Abstract
Background/Objectives: Childhood obesity is a pressing global health issue. Addressing this multifaceted issue requires comprehensive interventions, particularly those improving social sustainability by strengthening support systems in families, schools, and communities. This scoping review explored interventions aimed at enhancing social sustainability to improve anthropometric outcomes in overweight and obese children. Methods: A literature search was conducted from 2 August to 1 September 2025 and included all studies published up to the latter date using PubMed, Scopus, Virtual Health Library, and Cochrane Library databases. Inclusion criteria were (a) children (2–12 y); (b) socially sustainable, family-, community-, or school-centered interventions targeting childhood obesity; (c) body weight, BMI (absolute or z-score), body fat, or waist circumference assessment; and (d) publication as a randomized controlled trial. Methodological quality was assessed using the 11-point PEDro scale. Results: Eleven studies were included (N = 39,902). Mean intervention duration was 27 months. BMI z-score and prevalence of overweight/obese children, assessed in 9 of 11 studies, were the most common anthropometric outcomes, followed by absolute BMI in 8 of 11 studies. Most studies were rated “fair” or “good” quality and indicated that school-, community- and family-oriented interventions may effectively improve anthropometric variables in pediatric obesity. Conclusions: Socially sustainable, multi-level interventions involving families, schools, and community systems appear to optimize anthropometric outcomes in childhood obesity by integrating health promotion into children’s daily social settings and reinforcing consistent, health-oriented norms and resources. Further studies employing independent, blinded evaluators, culturally sensitive components in interventions, and adequate participant adherence reports are required to enhance practical and clinical application.
1. Introduction
Childhood obesity has emerged as a critical global public health concern, recognized by the World Health Organization (WHO) as a growing epidemic [1]. According to WHO estimates, approximately 18%, or around 340 million, children aged ≥5 years were classified as overweight or obese in 2016 [1]. Definitions of overweight and obesity vary slightly across regions. The U.S. Centers for Disease Control and Prevention (CDC), for example, defines overweight as a body mass index (BMI) at or above the 85th percentile and below the 95th percentile for children of the same age and sex, while obesity is defined as a body mass index (BMI) at or above the 95th percentile [2]. In contrast, European guidelines typically classify individuals as overweight at or above the 85th percentile, and as obese at or above the 95th percentile, using similar age- and sex-specific BMI reference charts [3]. Regardless, the prevalence of childhood obesity is a major health concern, as excess body weight in early life often sets the stage for serious medical conditions traditionally associated with adulthood, including type 2 diabetes mellitus, hypertension, and hypercholesterolemia [4]. The physical health consequences of childhood obesity are extensive, encompassing cardiovascular complications, insulin resistance, metabolic syndrome, and a range of other conditions affecting the neurological, respiratory, musculoskeletal, hepatic, and renal systems [5]. Additionally, childhood obesity can significantly impact psychological well-being, contributing to low self-esteem, poor emotional and social functioning, and an overall reduced quality of life [6]. It is also linked to decreased academic performance [7] and significantly increases the risk of persistent obesity into adulthood [8], thereby posing serious health challenges in both developed and developing nations [4].
Obesity is a multifactorial condition influenced by a complex interplay of behavioral, environmental, socioeconomic, and genetic factors. Genetic predisposition contributes to obesity risk, particularly in cases where there is a family history of parental obesity [9]. Environmental key contributors include the increased intake of energy-dense, nutrient-poor foods; excessive consumption of sugar-sweetened beverages; and insufficient levels of physical activity [10]. Socioeconomic determinants, such as low parental education, urbanization, and the effects of modernization, also play a significant role in shaping dietary and lifestyle habits within families [10]. Moreover, sedentary behaviors, including prolonged screen time from television viewing and video gaming, have been strongly associated with the development of obesity in children [11]. In addition, the attitudes and perceptions of both children and their parents toward body weight, diet, and physical activity can significantly influence obesity-related behaviors and outcomes [11].
Given the high prevalence and multifactorial nature of childhood obesity, a wide range of interventions have been designed and implemented to address excess body weight within this population. Some of these initiatives focus on modifying external factors that influence health behaviors through social sustainability [12,13], such as strengthening social support networks, improving access to health education, and fostering inclusive environments where young individuals feel valued and respected. These strategies often target the primary settings that shape children’s daily lives—most notably, the family [14], community [15], and school environments [16]—recognizing their critical role in promoting healthier lifestyles and long-term behavioral change. Previous reviews on this matter [17,18,19,20] have primarily explored the overall effectiveness of behavioral, nutritional, and physical activity programs, or the environmental and policy determinants of obesity prevention. However, these reviews have not specifically addressed how social sustainability components, including family, school, and community engagement, cultural adaptability, and long-term social equity, may shape the effectiveness and durability of such interventions. Furthermore, while prior evidence syntheses encompassed a wide range of study designs, none focused exclusively on randomized controlled trials (RCTs) explicitly incorporating socially sustainable frameworks. Consequently, an evidence gap remains regarding the methodological rigor and anthropometric impact of RCT-based interventions that embed principles of social sustainability in pediatric obesity management. This review aims to fill that gap by systematically identifying and appraising randomized evidence that connects socially sustainable strategies to measurable anthropometric outcomes in children, thereby offering novel insights into how equity, inclusivity, and community integration can enhance the long-term effectiveness of obesity interventions.
The purpose of this scoping review was to examine the state of the science on interventions improving social sustainability and targeting anthropometric outcomes in overweight and obese children. It was hypothesized that such interventions would be effective in enhancing anthropometric parameters such as body weight, BMI, and fat mass in this population.
2. Materials and Methods
This review was performed following the methodology of the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) statement [21] (Supplemental File S1). The review protocol can be assessed at https://archive.org/details/osf-registrations-nrbua-v1 (accessed on 10 October 2025). The population, concept and context (PCC) framework according to Arksey and O’Malley [22] was also employed to support the research question formulation (Table 1), which led to the following research question: “What is the existing evidence from RCTs on the effects of socially sustainable, family-, school-, or community-centered interventions on anthropometric outcomes in overweight and obese children?”

Table 1.
The population, concept, and context (PCC) framework used to guide the research question and inclusion criteria.
2.1. Eligibility Criteria
Studies were considered eligible for analysis when the following inclusion criteria were met: (a) published as a full-text manuscript; (b) inclusion of children (2–12 years of age) participants (Population (P)); (c) socially sustainable, family-, community- or school-centered interventions targeting childhood obesity (Intervention (I)); (d) inclusion of body weight, BMI (absolute or z-score), body fat or waist circumference assessment (Outcome (O)); (e) published as a RCT (Study Design (S)); and (f) available in English, Portuguese, or Spanish. Socially sustainable interventions were considered strategies or programs designed to achieve their outcomes while promoting equity, inclusivity, and long-term social well-being and community acceptance, ensuring benefits are maintained without exacerbating social inequalities. Systematic reviews, meta-analyses, case reports, book chapters, abstracts, and conference proceedings were excluded. Studies that employed pharmacological or other non-community, school- or family-centered interventions aimed at treating or preventing childhood obesity were excluded. Studies not addressing anthropometric outcomes in overweight or obese children were also excluded. No limitations were set on the year of publication.
2.2. Search Strategy
A systematic electronic search was conducted following the PICOS (Population, Intervention, Control, Outcome, Study Design) principle. The literature search was carried out from 2 August to 1 September 2025 and included all studies published up to the latter date while encompassing the following databases: PubMed, Scopus, Cochrane Library, and Virtual Health Library. As a part of a secondary search, the reference list in each full text was scanned for additional studies. The search strategy was initiated using a wide range of keywords and combinations, and refined every single time, making it more specific to ensure that only the most relevant articles were retrieved during the screening process. Several Medical Subject Headings (MeSH) terms were used to facilitate searching. This method resulted in a search strategy consisting of multiple combinations of keywords related to population, intervention, and outcome across databases (Table 2). The keywords and MeSH terms were combined with Boolean operators (“AND/OR”). The search strategy was independently conducted by two authors (RP and VSP) to reduce selection bias. The reviewers were not blinded to any of the studies’ details. Disagreements between the authors were resolved through mutual consensus, and any inter-reviewer disagreements were settled by consensus with a third investigator (RCGC).

Table 2.
Search strategy for the PubMed database.
2.3. Study Coding and Data Extraction
All search results from databases were screened on title and abstract in Rayyan v.1.4.3, a computer software that facilitates and accelerates the work process in screening and selecting articles for inclusion in a systematic review. Studies were read and independently coded by two investigators (LVA and BHMB). The following data were extracted in an Excel template/spreadsheet: (a) author and year of publication; (b) descriptive information of participants’ characteristics, including the number of participants, age range, and nationality; (c) design (experimental groups/intervention and duration); (d) main results (compared to pre-intervention values). In the main results, primary outcomes included anthropometric data. Secondary outcomes were also extracted and included obesity-related behaviors, such as total amount of food intake, fruit ingestion, vegetable ingestion, fat ingestion, sugar-sweetened beverages ingestion, physical activity, and sedentary behavior. Whenever available, psychological variables were also extracted from the studies, such as quality of life (generally through the Pediatric Quality of Life Inventory, PedsQL), strengths and difficulties, and parental resource empowerment. In cases where studies lacked sufficient information regarding pre–post changes, the authors were contacted to provide the missing data. Whenever data were not acquired from authors, values were extracted from figures using WebPlotDigitizer v.5.2 online software, where applicable (https://apps.automeris.io/wpd/, accessed on 10 September 2025). Coding sheets were cross-checked between two reviewers (RP and VSP), with discussion and agreement over any observed differences, or if unresolved, adjudicated by a third independent reviewer (LVA).
2.4. Methodological Quality Assessment
For the assessment of methodological quality, the 11-point PEDro scale was used [23] and independently evaluated by two authors (RP and VSP). Discrepancies between reviewers were resolved by discussion, with a third independent reviewer consulted when consensus could not be reached (LVA). This scale is considered an internally valid and reliable tool for assessing the risk of bias for RCTs and clinical trials [19]. The PEDro scale consists of 11 items (yes/no questions). The first item assesses external validity and is not included in the total score. The items 2–11 assess internal validity; hence, the values of the PEDro scale range from 0 to 10. Results ranging from 9 to 10 were classified as “excellent”, 6 to 8 were classified as “good”, 4 to 5 were classified as “fair quality”, and 0 to 3 were classified as “poor quality”.
3. Results
3.1. Search Results
The search yielded 2241 (Pubmed, N = 1835; Cochrane Library, N = 316; Scopus, N = 24; Virtual Health Library, N = 66) possibly relevant references. From this number, 228 duplicates that appeared in one or more databases were excluded. After scrutinizing the abstracts and titles for relevance, we considered 44 full-texts appropriate for detailed review. A review of these studies revealed that only 11 studies [24,25,26,27,28,29,30,31,32,33,34] met all the inclusion criteria. Figure 1 presents a flow diagram of the search process. Ethics approval from the local institutional review board was noted in all the included studies.
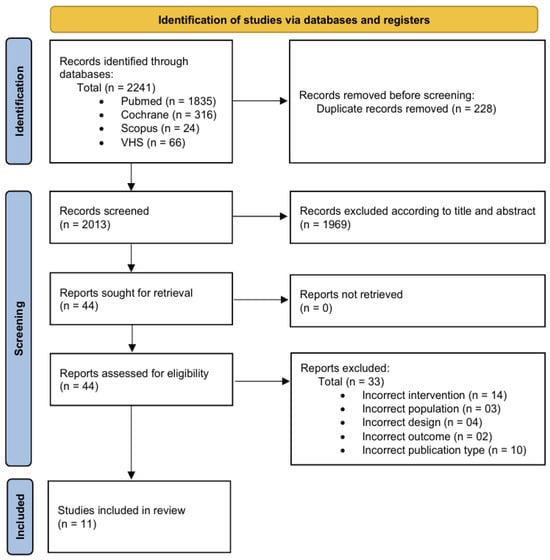
Figure 1.
Flow diagram of the search process.
3.2. Studies’ Description
The details of interventions from each study are presented in Table 3. The total number of participants across the studies was 39,902 participants, although one study alone was composed of 26,664 participants [26]. The total number of participants in control groups across the studies comprised 31,348 children, while experimental groups comprised 8554 participants. Studies’ duration lasted between 8 and 72 months (mean = 27 ± 20 months). Four studies employed exclusively community-centered programs [26,29,33,34]; three studies employed exclusively school-centered interventions [24,28,31]; two studies employed exclusively family-centered projects [30,32]; and two studies applied programs combining community-, school-, and family-orientation [25,27]. BMI z-score and percentage of overweight/obese children, evaluated in 8 out of 11 studies, were the most assessed anthropometric outcomes, followed by absolute BMI in 7 out of 11 studies. Seven studies reported a reduction in the percentage of overweight and/or obese children with socially sustainable interventions, while five reported a decrease in BMI z-score, three reported a decrease in absolute BMI, and one reported a reduction in fat mass percentage. In parallel, four studies did not detect any change in absolute BMI, while four and one studies reported, respectively, an absence of alteration in BMI z-score and percentage of overweight and/or obese children.

Table 3.
Summary of the basic details from the included studies.
3.3. Methodological Quality
The PEDro score for the studies in this review ranged from 4 to 8 (mean = 5.5 ± 1.4), indicating “fair” to “good” methodological quality. Specifically, five studies were deemed to be of fair quality, and six studies were deemed to be of good quality. The details of quality analysis from each study are presented in Table 4. None of the articles received a score for Q5 and Q6, while only one received a score for Q7.

Table 4.
Studies’ quality through the 11-point Physiotherapy Evidence Database (PEDro) scale.
4. Discussion
A total of eleven RCTs were included in this review, comprising socially sustainable interventions targeting family, school, or community environments. Overall, the majority of trials reported beneficial anthropometric outcomes in pediatric obesity associated with socially sustainable interventions. The comparative efficacy between these approaches, however, remains inconclusive. Although the review did not definitively resolve which type of socially sustainable intervention model is superior, the collective evidence from the revised RCTs underscored meaningful insights into the efficacy of different components comprising socially sustainable interventions and their potential roles in the treatment of childhood obesity across diverse nationalities and settings.
4.1. School- and Community-Based Environmental Interventions
Several trials focused on environmental modifications at the school or community level. The pilot study by Warren and colleagues [24] evaluated a school-based intervention targeting 5- to 7-year-olds in Oxford, UK. Over approximately 14 months, children were randomly assigned to control, nutrition-only, physical activity–only, or combined arms. While all participants showed significant gains in nutrition knowledge, these did not translate into meaningful changes in overweight or obesity prevalence. Fruit and vegetable intake did increase modestly, but BMI remained unchanged, suggesting that improvements in knowledge and diet quality, while necessary, are insufficient by themselves to produce significant anthropometric changes.
In contrast, the “Romp & Chomp” intervention in Geelong, Australia (2004–2008), adopted a community-wide, multisetting approach focused on early childhood environments [26]. This multifaceted strategy, including community capacity building and environmental modifications in care and educational settings, yielded significant reductions in mean body weight, BMI, and BMI z-score among 3.5-year-olds, as well as a lower prevalence of overweight/obesity among both 2- and 3.5-year-old cohorts (reductions of 2.5 and 3.4 percentage points respectively, vs. ~0.7 percentage points in control groups). Behavioral changes reported by authors also included decreased consumption of packaged snacks and artificial fruit juice. These findings reflect the added potency of environmental strategies in achieving measurable outcomes in early childhood populations.
Likewise, the “LA Health” study [28] reported slight reductions in body fat among children exposed to school environmental modifications, though effect sizes were small and BMI z-score changes were not significant. Similarly, the “Fun ‘n Healthy in Moreland!” trial did not yield significant changes in BMI [31], though improvements in parameters other than anthropometric outcomes were demonstrated, such as in dietary behaviors, school policies, and child-reported wellbeing, as well as in the prevalence of overweight and obesity. On the other hand, a decrease in the prevalence of overweight and obesity was also observed in their control group [31]. In the same direction, the “Bright Start” trial in American Indian communities found no mean BMI differences, despite a 10% reduction in the prevalence of overweight, parallel to a significant increase in overweight prevalence in their control group, suggesting benefits in incidence prevention [27].
On the other hand, “Shape Up Somerville” showed significant reductions in BMI z-scores during its first year, attributed to broad community engagement and policy/environmental changes [25]. Likewise, the “TX CORD” trial reported that community-based programs with higher contact hours achieved greater short-term improvements in BMI and fat mass among underserved populations compared to primary care interventions [29], though sustaining effects remained a challenge. Finally, the “Children’s Healthy Living (CHL) Program”, across Pacific jurisdictions, achieved meaningful reductions in absolute BMI, BMI z-score, and overweight/obesity prevalence immediately post-intervention [33], while a sustained benefit was shown in overweight and obesity prevalence over six years [34]. These findings suggest that multilevel, culturally contextualized, and long-duration interventions are more likely to achieve measurable population-level effects than shorter-term, school-only approaches.
4.2. Family-Based Interventions
More intensive clinical and family-centered strategies demonstrated consistent efficacy. The “Multi-Site Family-Based Treatment (FBT)” trial showed that enhanced social facilitation maintenance programs improved the prevalence of overweight children, but not BMI z-score relative to education controls, with treatment dose influencing efficacy [32]. Conversely, the “Connect for Health” trial demonstrated modest but significant BMI z-score improvements with enhanced primary care interventions [30], though the addition of personalized health coaching to families did not significantly augment effects.
4.3. General Overview
A central observation across the revised studies was the limited effect on BMI when interventions relied solely on educational or environmental changes of modest intensity and duration. Stronger effects appeared when programs integrated multiple components—school, family, and broader community systems—especially when maintained over time. Additionally, sustainability emerges as a critical factor: while many interventions showed short-term benefits, only the CHL Program demonstrated durable effects beyond the intervention period. Another recurring finding is that behavioral and environmental improvements (e.g., healthier diet, increased activity opportunities, policy changes) were often achieved even when anthropometric outcomes remained unchanged. These intermediate outcomes are meaningful in shaping supportive contexts for long-term obesity prevention and treatment, particularly in high-risk and underserved populations.
4.4. Limitations
Despite the broad diversity of populations studied across the trials (e.g., U.S. children, American Indian communities, Pacific Islanders), some of the studies were limited by modest sample sizes and relatively short intervention or follow-up periods. Heterogeneity in outcome measures and intervention intensity also impairs direct comparisons. In addition, one large-scale trial [26] alone accounted for more than two-thirds of all participants, which may have disproportionately influenced the overall synthesis and warrants caution when interpreting the findings.
A significant limitation identified across many of the studies included was the lack of consideration for cultural factors among participants, and as shown in Table 3, the studies were conducted across several distinct locations. Variables such as ethnicity, religious beliefs and practices, and neighborhood characteristics are well-documented to influence health behaviors and lifestyle choices in children and their families, factors that are closely linked to the prevalence of childhood obesity [35]. For example, a study by Chen et al. [36] demonstrated that culturally tailored, web-based behavioral interventions targeting Chinese American adolescents were more effective in promoting healthy lifestyle changes and reducing obesity risk. This finding underscores the importance of incorporating culturally sensitive components into intervention design to enhance both relevance and efficacy across diverse populations.
Furthermore, lack of adherence reports also emerged as a common limitation across all the studies. To enhance participant engagement, some researchers reported using different strategies, including email reminders, telephone follow-ups, and financial incentives. Nevertheless, one cannot assume that the adherence rate was necessarily high, especially since most of the reviewed studies included very long durations. In this sense, Novotny et al. [33] demonstrated in their first 24-month study that a multijurisdictional, multilevel, multicomponent community-based program was effective in improving anthropometric outcomes such as absolute BMI, BMI z-score, waist circumference, and the percentage of overweight and obese participants. On the other hand, during their 4-year follow-up [34], despite a sustained benefit still observed in overweight prevalence, no improvements were identified in absolute BMI and BMI z-score compared to the measurement taken after 24 months of intervention. In fact, a statistically significant increase in waist circumference was observed in the intervention group, suggesting limited long-term efficacy. These findings suggest that strategies need to be developed to maximize sustained engagement, thus optimizing and maintaining treatment efficacy.
Lastly, as shown in Table 4, none of the studies met items Q5 and Q6 of the PEDro scale, and only one met Q7. The absence of compliance with Q5 and Q6 is understandable in studies involving behavioral interventions (e.g., exercise training, specific diets), as blinding both the participants and the intervention providers is often impractical. However, the lack of compliance with Q7 is less justifiable, since it would have been feasible to assign outcome assessors blinded to the intervention type or experimental groups when evaluating anthropometric or other parameters. The absence of blinded assessors likely increased the risk of bias in most of the reviewed studies, underscoring the importance of employing blinded evaluators in future research to enhance methodological rigor. Moreover, although some of the included studies [24,26,27] did not explicitly state their eligibility criteria, all clearly targeted preschool and school-aged children and employed comparable intervention settings and outcome measures. Therefore, their inclusion does not compromise the generalizability of the findings. On the contrary, retaining these studies strengthens the representativeness of the evidence base by encompassing a broader range of socially sustainable, real-world interventions consistent with the review’s scope.
5. Conclusions
Across diverse pediatric populations and settings, childhood obesity management requires comprehensive, multi-component strategies. School- and family-based programs achieved notable improvements in dietary behaviors and physical activity opportunities; however, their effects on anthropometric outcomes were generally small or inconsistent. More intensive, multilevel community-based interventions produced greater short-term improvements in anthropometric parameters, yet sustaining these benefits over time remains challenging. These results underscore that scalable and equitable solutions to childhood obesity must integrate efforts across schools, families, healthcare systems, and communities, with long-term investment to support sustainability and health promotion.
Future research should aim to strengthen adherence, reduce socioeconomic disparities, and extend intervention benefits beyond short-term gains toward lasting improvements in child health. To enhance practical and clinical application, studies should incorporate (a) blinded research personnel to reduce assessment bias; (b) culturally sensitive components to ensure relevance and engagement; and (c) adequate reporting of participant adherence to inform fidelity and reproducibility.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare13222932/s1, Supplemental File S1: Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Author Contributions
Conceptualization, B.H.M.B. and R.G.C.; data curation, R.d.P., V.d.S.P. and L.V.A.; formal analysis, R.d.P. and V.d.S.P.; investigation, R.d.P., V.d.S.P. and L.V.A.; methodology, R.d.P., V.d.S.P. and L.V.A.; software, B.H.M.B.; validation, R.d.P., V.d.S.P., L.V.A., B.H.M.B. and R.G.C.; resources, B.H.M.B. and R.G.C.; writing—original draft preparation, R.d.P. and V.d.S.P.; writing—review and editing, V.d.S.P., L.V.A., B.H.M.B. and R.G.C.; visualization, R.d.P., V.d.S.P., L.V.A., B.H.M.B. and R.G.C.; supervision, B.H.M.B. and R.G.C.; project administration, B.H.M.B. and R.G.C.; funding acquisition, B.H.M.B. and R.G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by scholarships for productivity in research provided by the Individual Research Program of our university (grant number #7-02-1202/2024), the National Council for Scientific and Technological Development (CNPq; grant number #313009/2025-2), the Cesumar Institute of Science, Technology and Innovation, and the Araucaria Foundation for Support of Scientific and Technological Development. These funding sources were not involved in the conduct of the research and/or preparation of the article.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable as no datasets were generated and/or analysed for this study.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| BMI | Body Mass Index |
| WHO | World Health Organization |
| CDC | Centers for Disease Control and Prevention |
| RCT | Randomized Controlled Trial |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| VHL | Virtual Health Library |
| PedsQL | Pediatric Quality of Life Inventory |
| PEDro | Physiotherapy Evidence Database Scale |
| SBP | Systolic Blood Pressure |
| DBP | Diastolic Blood Pressure |
| SDQ | Strengths and Difficulties Questionnaire |
References
- World Health Organization. Obesity and Overweight. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 27 September 2025).
- Zhang, X.; Liu, J.; Ni, Y.; Yi, C.; Fang, Y.; Ning, Q.; Shen, B.; Zhang, K.; Liu, Y.; Yang, L.; et al. Global Prevalence of Overweight and Obesity in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2024, 178, 800–813. [Google Scholar] [CrossRef]
- Garrido-Miguel, M.; Oliveira, A.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Pozuelo-Carrascosa, D.P.; Soriano-Cano, A.; Martínez-Vizcaíno, V. Prevalence of Overweight and Obesity among European Preschool Children: A Systematic Review and Meta-Regression by Food Group Consumption. Nutrients 2019, 11, 1698. [Google Scholar] [CrossRef] [PubMed]
- Karnik, S.; Kanekar, A. Childhood obesity: A global public health crisis. Int. J. Prev. Med. 2012, 3, 1–7. [Google Scholar]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; So, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Mond, J.; Van den Berg, P.; Boutelle, K.; Hannan, P.; Neumark-Sztainer, D. Obesity, body dissatisfaction, and emotional well-being in early and late adolescence: Findings from the project EAT study. J. Adolesc. Health 2011, 48, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Hagman, E.; Danielsson, P.; Brandt, L.; Svensson, V.; Ekbom, A.; Marcus, C. Childhood obesity, obesity treatment outcome, and achieved education: A prospective cohort study. J. Adolesc. Health 2017, 61, 508–513. [Google Scholar] [CrossRef]
- Biro, F.M.; Wien, M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010, 91, 1499–1505. [Google Scholar] [CrossRef]
- Angoorani, P.; Heshmat, R.; Ejtahed, H.S.; Motlagh, M.E.; Ziaodini, H.; Taheri, M.; Aminaee, T.; Shafiee, G.; Godarzi, A.; Qorbani, M.; et al. The association of parental obesity with physical activity and sedentary behaviors of their children: The CASPIAN-V study. J. Pediatr. 2018, 94, 410–418. [Google Scholar] [CrossRef]
- An, R.; Shen, J.; Yang, Q.; Yang, Y. Impact of built environment on physical activity and obesity among children and adolescents in China: A narrative systematic review. J. Sport Health Sci. 2019, 8, 153–169. [Google Scholar] [CrossRef]
- Braithwaite, I.; Stewart, A.W.; Hancox, R.J.; Beasley, R.; Murphy, R.; Mitchell, E.A.; ISAAC Phase Three Study Group. The worldwide association between television viewing and obesity in children and adolescents: Cross sectional study. PLoS ONE. 2013, 8, e74263. [Google Scholar] [CrossRef]
- He, G.; Cerin, E.; Huang, W.Y.; Wong, S.H. Understanding neighborhood environment related to Hong Kong children’s physical activity: A qualitative study using nominal group technique. PLoS ONE. 2014, 9, e106578. [Google Scholar] [CrossRef]
- Skouteris, H.; Cox, R.; Huang, T.; Rutherford, L.; Edwards, S.; Cutter-Mackenzie, A. Promoting obesity prevention together with environmental sustainability. Health Promot. Int. 2014, 29, 454–462. [Google Scholar] [CrossRef][Green Version]
- Sacher, P.M.; Kolotourou, M.; Chadwick, P.M.; Cole, T.J.; Lawson, M.S.; Lucas, A.; Singhal, A. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity 2010, 18, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Benjamin Neelon, S.E.; Namenek Brouwer, R.J.; Østbye, T.; Evenson, K.R.; Neelon, B.; Martinie, A.; Bennett, G. A community-based intervention increases physical activity and reduces obesity in school-age children in North Carolina. Child. Obes. 2015, 11, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, N.; Nagpal, N.; Zieve, H.; Vyas, A.; Tatum, J.; Ramos, M.; Team KiPOW!; McCarter, R., Jr.; Lucas, C.T.; Mietus-Snyder, M. A School-Based Intervention Using Health Mentors to Address Childhood Obesity by Strengthening School Wellness Policy. Prev. Chronic Dis. 2019, 16, 154. [Google Scholar] [CrossRef]
- Ernest, D.K.; Onugha, E.A.; Singh, B.; Sharma, S.V.; Dave, J.M. A Scoping Review of the Social Determinants of Pediatric and Adolescent Obesity. Int. J. Pediatr. 2025, 28, 8871022. [Google Scholar] [CrossRef] [PubMed]
- Brown, V.; Moodie, M.; Sultana, M.; Hunter, K.E.; Byrne, R.; Zarnowiecki, D.; Seidler, A.L.; Golley, R.; Taylor, R.W.; Hesketh, K.D.; et al. A scoping review of outcomes commonly reported in obesity prevention interventions aiming to improve obesity-related health behaviors in children to age 5 years. Obes. Rev. 2022, 23, e13427. [Google Scholar] [CrossRef]
- Chia, A.; Ong, J.; Bundele, A.; Lim, Y.W. Social entrepreneurship in obesity prevention: A scoping review. Obes. Rev. 2022, 23, e13378. [Google Scholar] [CrossRef]
- Wang, X.; Ammerman, A.; Orr, C.J. Family-based interventions for preventing overweight or obesity among preschoolers from racial/ethnic minority groups: A scoping review. Obes. Sci. Pract. 2021, 8, 371–386. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Warren, J.M.; Henry, C.J.; Lightowler, H.J.; Bradshaw, S.M.; Perwaiz, S. Evaluation of a pilot school programme aimed at the prevention of obesity in children. Health Promot. Int. 2003, 18, 287–296. [Google Scholar] [CrossRef]
- Economos, C.D.; Hyatt, R.R.; Goldberg, J.P.; Must, A.; Naumova, E.N.; Collins, J.J.; Nelson, M.E. A community intervention reduces BMI z-score in children: Shape Up Somerville first year results. Obesity 2007, 15, 1325–1336. [Google Scholar] [CrossRef]
- de Silva-Sanigorski, A.M.; Bell, A.C.; Kremer, P.; Nichols, M.; Crellin, M.; Smith, M.; Sharp, S.; de Groot, F.; Carpenter, L.; Boak, R.; et al. Reducing obesity in early childhood: Results from Romp & Chomp, an Australian community-wide intervention program. Am. J. Clin. Nutr. 2010, 91, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Story, M.; Hannan, P.J.; Fulkerson, J.A.; Rock, B.H.; Smyth, M.; Arcan, C.; Himes, J.H. Bright Start: Description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity 2012, 20, 2241–2249. [Google Scholar] [CrossRef]
- Williamson, D.A.; Champagne, C.M.; Harsha, D.W.; Han, H.; Martin, C.K.; Newton, R.L., Jr.; Sothern, M.S.; Stewart, T.M.; Webber, L.S.; Ryan, D.H. Effect of an environmental school-based obesity prevention program on changes in body fat and body weight: A randomized trial. Obesity 2012, 20, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Butte, N.F.; Hoelscher, D.M.; Barlow, S.E.; Pont, S.; Durand, C.; Vandewater, E.A.; Liu, Y.; Adolph, A.L.; Pérez, A.; Wilson, T.A.; et al. Efficacy of a Community- Versus Primary Care-Centered Program for Childhood Obesity: TX CORD RCT. Obesity 2017, 25, 1584–1593. [Google Scholar] [CrossRef]
- Taveras, E.M.; Marshall, R.; Sharifi, M.; Avalon, E.; Fiechtner, L.; Horan, C.; Gerber, M.W.; Orav, E.J.; Price, S.N.; Sequist, T.; et al. Comparative Effectiveness of Clinical-Community Childhood Obesity Interventions: A Randomized Clinical Trial. JAMA Pediatr. 2017, 171, e171325. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.; Gibbs, L.; Tadic, M.; Ukoumunne, O.C.; Magarey, A.; Okely, A.D.; de Silva, A.; Armit, C.; Green, J.; O’Connor, T.; et al. Cluster randomised trial of a school-community child health promotion and obesity prevention intervention: Findings from the evaluation of fun ‘n healthy in Moreland! BMC Public Health 2017, 18, 92. [Google Scholar] [CrossRef]
- Wilfley, D.E.; Saelens, B.E.; Stein, R.I.; Best, J.R.; Kolko, R.P.; Schechtman, K.B.; Wallendorf, M.; Welch, R.R.; Perri, M.G.; Epstein, L.H. Dose, Content, and Mediators of Family-Based Treatment for Childhood Obesity: A Multisite Randomized Clinical Trial. JAMA Pediatr. 2017, 171, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Novotny, R.; Davis, J.; Butel, J.; Boushey, C.J.; Fialkowski, M.K.; Nigg, C.R.; Braun, K.L.; Leon Guerrero, R.T.; Coleman, P.; Bersamin, A.; et al. Effect of the Children’s Healthy Living Program on Young Child Overweight, Obesity, and Acanthosis Nigricans in the US-Affiliated Pacific Region: A Randomized Clinical Trial. JAMA Netw. Open 2018, 1, e183896. [Google Scholar] [CrossRef] [PubMed]
- Novotny, R.; Yamanaka, A.B.; Butel, J.; Boushey, C.J.; Dela Cruz, R.; Aflague, T.; Coleman, P.; Shallcross, L.; Fleming, T.; Wilkens, L.R. Maintenance Outcomes of the Children’s Healthy Living Program on Overweight, Obesity, and Acanthosis Nigricans Among Young Children in the US-Affiliated Pacific Region: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2214802. [Google Scholar] [CrossRef] [PubMed]
- Baskin, M.L.; Tipre, M.; Richardson, M. Culturally-Relevant Obesity Interventions: African American Children and Adolescents. In Families, Food, and Parenting; Francis, L.A., McHale, S.M., King, V., Glick, J.E., Eds.; National Symposium on Family Issues; Springer: Cham, Switzerland, 2021; Volume 11. [Google Scholar]
- Chen, J.L.; Weiss, S.; Heyman, M.B.; Cooper, B.; Lustig, R.H. The efficacy of the Web-based childhood obesity prevention program in Chinese American adolescents: Web ABC Study. J. Adolesc. Health 2011, 49, 148–154. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).