Quality of Life, Physical Activity, and Mental and Physical Health Status in Croatian Middle-Aged and Elderly Population
Abstract
1. Introduction
1.1. Prevalence and Impact of Obesity and Chronic Disease in Croatia
1.2. Importance of the Lifestyle Factors and Functional Measures Like Handgrip Strength
1.3. Study Rationale and Objectives
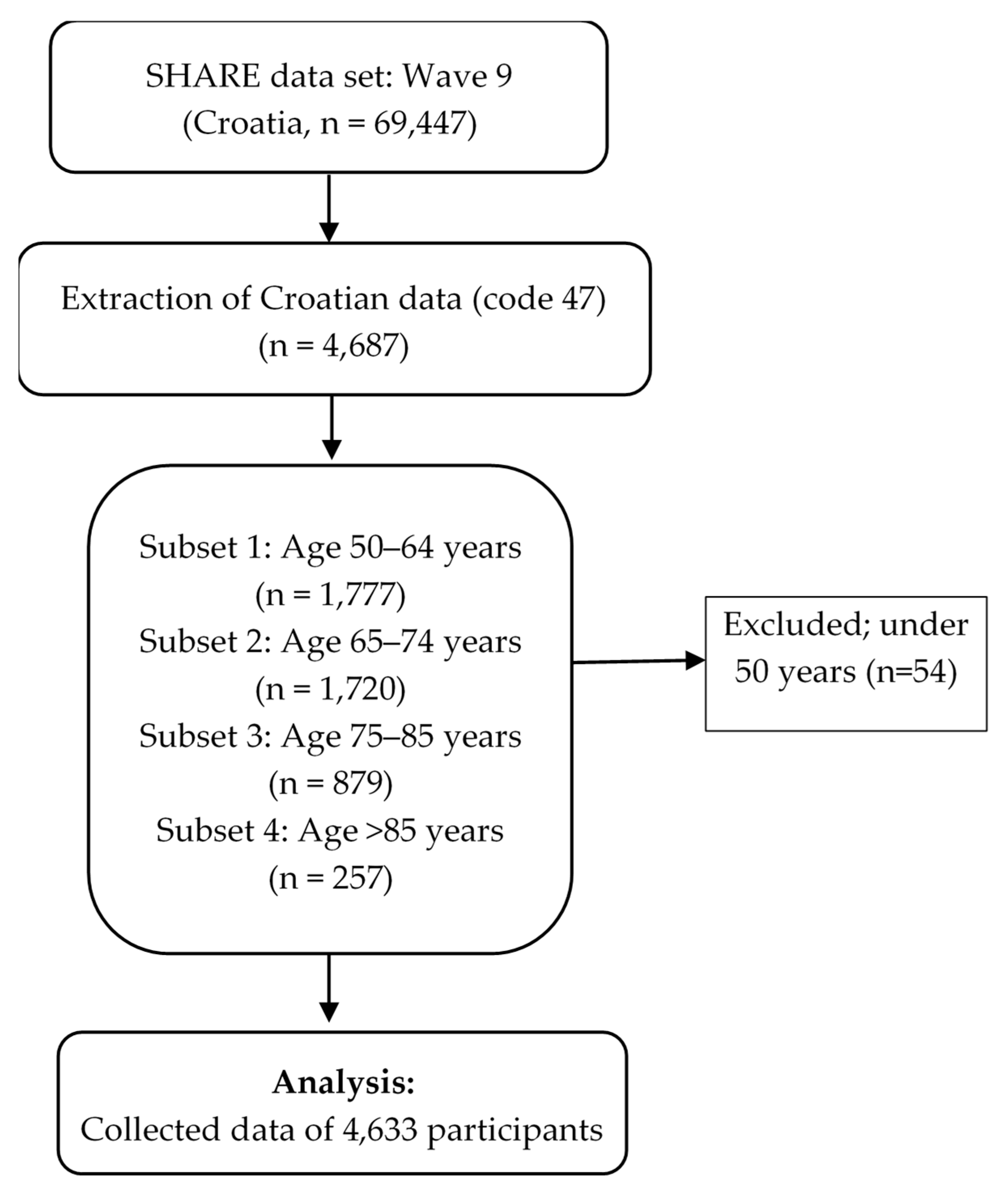
2. Materials and Methods
2.1. Data
2.2. Variables
Health-Related Indicators
2.3. Data Analysis
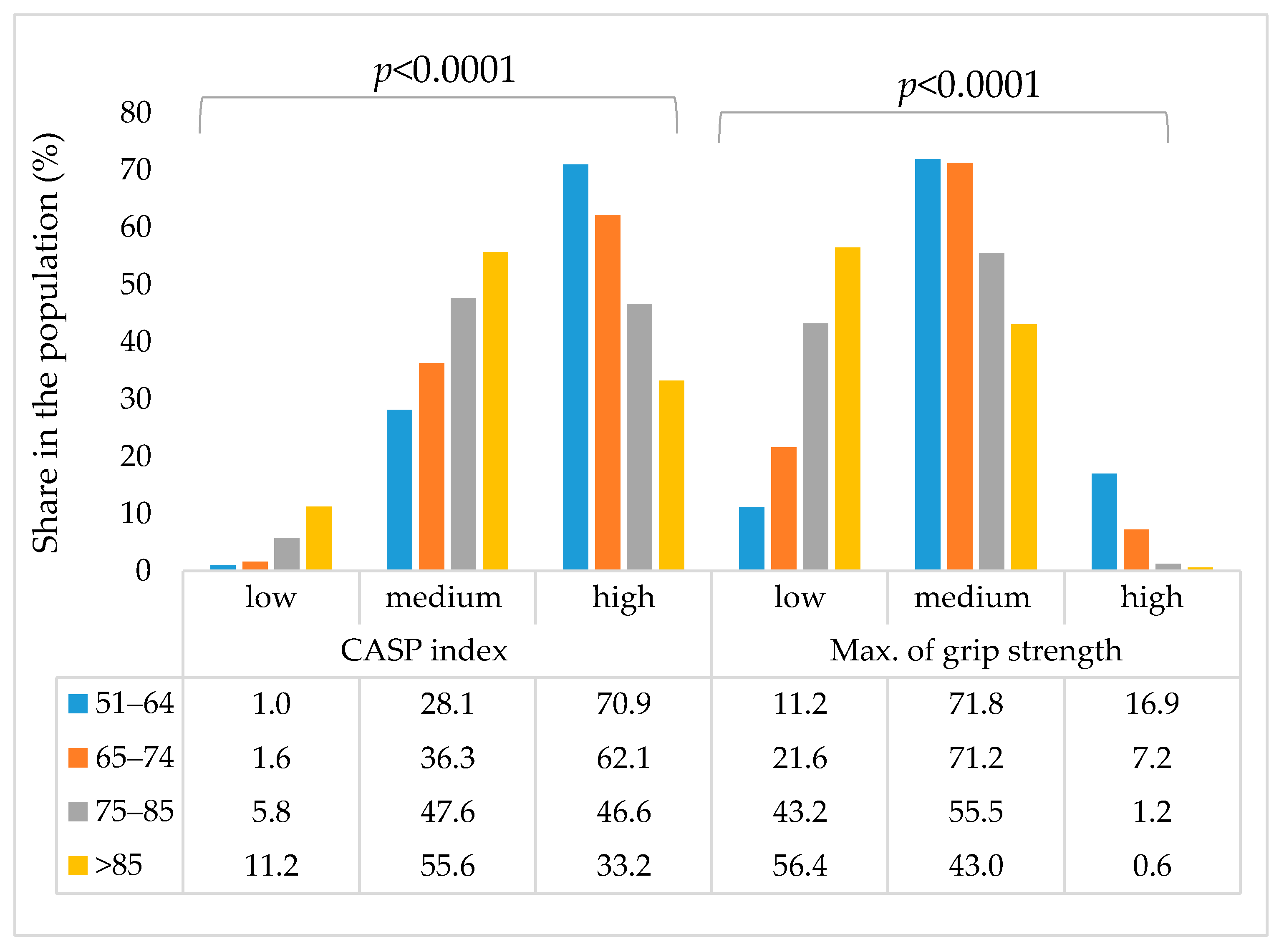
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BF | Body fat |
| BM | Body mass |
| BMI | Body mass index |
| CVD | Cardiovascular disease |
| CASP | Control, Autonomy, Self-realization, and Pleasure scale |
| CI | Confidence interval |
| EURO-D | depression symptoms scale used in European countries. The resulting scale consists of: depression, pessimism, suicidality, guilt, sleep, interest, irritability, appetite, fatigue, concentration (onreading or entertainment), enjoyment, and tearfulness |
| OR | Odds ratio |
| SPH | Self-perceived Health |
References
- European Commission. European Health Interview Survey (EHIS): Overweight and Obesity Indicators. 2019 Eurostat. Available online: https://ec.europa.eu/eurostat/web/microdata/european-health-interview-survey (accessed on 15 May 2025).
- Ministry of Health of the Republic of Croatia. Action Plan for Obesity Prevention 2024–2027. 2024. Available online: https://zdravlje.gov.hr/programi-i-projekti/nacionalni-programi-projekti-i-strategije/ostali-programi/akcijski-plan-za-prevenciju-debljine-2024-2027/6275 (accessed on 15 May 2025).
- WHO, World Health Organization. Obesity and Overweight. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 15 March 2025).
- Pi-Sunyer, F.X. Comorbidities of overweight and obesity: Current evidence and research issues. Med. Sci. Sports Exerc. 1999, 31 (Suppl. S11), S602–S608. [Google Scholar] [CrossRef]
- Fontaine, K.R.; Redden, D.T.; Wang, C.; Westfall, A.O.; Allison, D.B. Years of life lost due to obesity. JAMA 2003, 289, 187–193. [Google Scholar] [CrossRef]
- Mainous, A.G., III; Yin, L.; Wu, V.; Sharma, P.; Jenkins, B.; Saguil, A.A.; Nelson, D.S.; Orlando, F.A. Body Mass Index vs Body Fat Percentage as a Predictor of Mortality in Adults Aged 20–49 Years. Ann. Fam. Med. 2025, 23, 337–343. [Google Scholar] [CrossRef]
- Busebee, B.; Ghusn, W.; Cifuentes, L.; Acosta, A. Obesity: A Review of Pathophysiology and Classification. Mayo Clin. Proc. 2023, 98, 1842–1857. [Google Scholar] [CrossRef]
- Hurtado, A.M.D.; Acosta, A. Precision Medicine and Obesity. Gastroenterol. Clin. N. Am. 2021, 50, 127–139. [Google Scholar] [CrossRef]
- Bray, M.S.; Loos, R.J.F.; McCaffery, J.M.; Ling, C.; Franks, P.W.; Weinstock, G.M.; Snyder, M.P.; Vassy, J.L. Argus-Collins, T.; The Conference Working Group. NIH working group report-using genomic information to guide weight management: From universal to precision treatment. Obesity 2016, 24, 14–22. [Google Scholar] [CrossRef]
- Pigeyre, M.; Yazdi, F.T.; Kaur, Y.; Meyre, D. Recent progress in genetics, epigenetics and metagenomics unveils the pathophysiology of human obesity. Clin. Sci. 2016, 130, 943–986. [Google Scholar] [CrossRef] [PubMed]
- Heymsfield, S.B.; Wadden, T.A. Mechanisms, Pathophysiology, and Management of Obesity. N. Engl. J. Med. 2017, 376, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Locke, A.E.; Kahali, B.; Berndt, S.I.; Justice, A.E.; Pers, T.H.; Day, F.R.; Powell, C.; Vedantam, S.; Buchkovich, M.L.; Yanh, J.; et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 2015, 518, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, J.P. Epigenetics: Principles and practice. Dig. Dis. 2011, 29, 130–135. [Google Scholar] [CrossRef]
- Wahl, S.; Drong, A.; Lehne, B.; Loh, M.; Scott, W.R.; Kunze, S.; Tsai, P.C.; Ried, J.S.; Zhang, W.; Yang, Y.; et al. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature 2017, 541, 81–86. [Google Scholar] [CrossRef]
- Thorpe, K.E.; Yang, Z.; Long, K.M.; Garvey, W.T. The impact of weight loss among seniors on Medicare spending. Health Econ. Rev. 2013, 3, 7. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, S.R.; Nijpels, G.; Nilsson, P.M.; Nolan, J.J.; Gabriel, R.; Bobbioni-Harsch, E.; Mingrone, G.; Dekker, J.M.; for the Relationship Between Insulin Sensitivity and Cardiovascular Disease (RISC) Investigators. Low-grade chronic inflammation in the relationship between insulin sensitivity and cardiovascular disease (RISC) population: Associations with insulin resistance and cardiometabolic risk profile. Diabetes Care 2009, 32, 1295–1301. [Google Scholar] [CrossRef] [PubMed]
- Summers, S.A. Ceramides in insulin resistance and lipotoxicity. Prog. Lipid Res. 2006, 45, 42–72. [Google Scholar] [CrossRef]
- Sathyanarayana, P.; Barthwal, M.K.; Kundu, C.N.; Lane, M.E.; Bergmann, A.; Tzivion, G.; Rana, A. Activation of the Drosophila MLK by ceramide reveals TNF-alpha and ceramide as agonists of mammalian MLK3. Mol. Cell 2002, 10, 1527–1533. [Google Scholar] [CrossRef]
- Bays, H.E.; González-Campoy, J.M.; Bray, G.A.; Kitabchi, A.E.; Bergman, D.A.; Schorr, A.B.; Rodbard, H.W.; Henry, R.R. Pathogenic potential of adipose tissue and metabolic consequences of adipocyte hypertrophy and increased visceral adiposity. Expert Rev. Cardiovasc. Ther. 2008, 6, 343–368. [Google Scholar] [CrossRef]
- Kern, P.A.; Ranganathan, S.; Li, C.; Wood, L.; Ranganathan, G. Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am. J. Physiol. Endocrinol. Metab. 2001, 280, E745–E751. [Google Scholar] [CrossRef]
- Shi, H.; Kokoeva, M.V.; Inouye, K.; Tzameli, I.; Yin, H.; Flier, J.S. TLR4 links innate immunity and fatty acid-induced insulin resistance. J. Clin. Investig. 2006, 116, 3015–3025. [Google Scholar] [CrossRef]
- Xu, H.; Barnes, G.T.; Yang, Q.; Tan, G.; Yang, D.; Chou, C.J.; Sole, J.; Nichols, A.; Ross, J.S.; Tartaglia, L.A.; et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J. Clin. Investig. 2003, 112, 1821–1830. [Google Scholar] [CrossRef]
- Rocha, V.Z.; Folco, E.J.; Sukhova, G.; Shimizu, K.; Gotsman, I.; Vernon, A.H.; Libby, P. Interferon-gamma, a Th1 cytokine, regulates fat inflammation: A role for adaptive immunity in obesity. Circ. Res. 2008, 103, 467–476. [Google Scholar] [CrossRef] [PubMed]
- Stratford, S.; DeWald, D.B.; Summers, S.A. Ceramide dissociates 3′-phosphoinositide production from pleckstrin homology domain translocation. Biochem. J. 2001, 354 Pt 2, 359–368. [Google Scholar] [CrossRef]
- Aguirre, V.; Uchida, T.; Yenush, L.; Davis, R.; White, M.F. The c-Jun NH(2)-terminal kinase promotes insulin resistance during association with insulin receptor substrate-1 and phosphorylation of Ser(307). J. Biol. Chem. 2000, 275, 9047–9054. [Google Scholar] [CrossRef] [PubMed]
- Magkos, F.; Su, X.; Bradley, D.; Fabbrini, E.; Conte, C.; Eagon, J.C.; Varela, J.E.; Brunt, E.M.; Patterson, B.W.; Klein, S. Intrahepatic diacylglycerol content is associated with hepatic insulin resistance in obese subjects. Gastroenterology 2012, 142, 1444–1446.e2. [Google Scholar] [CrossRef]
- Klop, B.; Elte, J.W.; Cabezas, M.C. Dyslipidemia in obesity: Mechanisms and potential targets. Nutrients 2013, 5, 1218–1240. [Google Scholar] [CrossRef]
- Rocha, V.Z.; Libby, P. Obesity, inflammation, and atherosclerosis. Nat. Rev. Cardiol. 2009, 6, 399–409. [Google Scholar] [CrossRef]
- Wilson, P.W.; D’Agostino, R.B.; Sullivan, L.; Parise, H.; Kannel, W.B. Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch. Intern. Med. 2002, 162, 1867–1872. [Google Scholar] [CrossRef]
- Doyev, R.; Axelrod, R.; Keinan-Boker, L.; Shimony, T.; Goldsmith, R.; Nitsan, L.; Dichtiar, R.; Sinai, T. Energy Intake Is Highly Associated with Handgrip Strength in Community-Dwelling Elderly Adults. J. Nutr. 2021, 151, 1249–1255. [Google Scholar] [CrossRef] [PubMed]
- Maltarić, M.; Ruščić, P.; Kolak, M.; Bender, D.V.; Kolarić, B.; Ćorić, T.; Hoejskov, P.S.; Bošnir, J.; Kljusurić, J.G. Adherence to the Mediterranean Diet Related to the Health Related and Well-Being Outcomes of European Mature Adults and Elderly, with an Additional Reference to Croatia. Int. J. Environ. Res. Public Health 2023, 20, 4893. [Google Scholar] [CrossRef] [PubMed]
- Go, Y.J.; Lee, D.C.; Lee, H.J. Association between handgrip strength asymmetry and falls in elderly Koreans: A nationwide population-based cross-sectional study. Arch. Gerontol. Geriatr. 2021, 96, 104470. [Google Scholar] [CrossRef]
- Chua, K.Y.; Lim, W.-S.; Lin, X.; Yuan, J.-M.; Koh, W.-P. Handgrip Strength and Timed-Up-and-Go (TUG) Test are Predictors of Short-Term Mortality in Older Adults. J. Nutr. Health Aging 2020, 24, 371–378. [Google Scholar] [CrossRef]
- Gruber, S.; Wagner, M.; Batta, F. SHARE: Scales and Multi-Item Indicators. 2024. Available online: https://www.researchgate.net/publication/382256208_Scales_and_Multi-Item_Indicators#fullTextFileContent (accessed on 15 March 2025).
- Oliver, A.; Sentandreu-Mañó, T.; Tomás, J.M.; Fernández, I.; Sancho, P. Quality of Life in European Older Adults of SHARE Wave 7: Comparing the Old and the Oldest-Old. J. Clin. Med. 2021, 10, 2850. [Google Scholar] [CrossRef]
- Ma, R.; Zhang, C.; Xu, W. The Moderating Role of Control Strategies on the Relationship between Negative Emotions and QoL in the Elderly: A Longitudinal Study. Int. J. Ment. Health Promot. 2025, 27, 470–483. [Google Scholar] [CrossRef]
- Smolić, Š.; Međimurec, P.; Čipin, I.; Mudražija, S.; Mustač, D.; Fabijančić, M. The hidden crisis: Classifying unmet healthcare needs in European older adults during COVID-19. Eur. J. Ageing 2025, 22, 31. [Google Scholar] [CrossRef]
- Li, Y.; Song, H. The association between sports social capital and cognitive health: A longitudinal study of middle-aged and elderly adults in China. SSM-Popul. Health 2025, 30, 101778. [Google Scholar] [CrossRef]
- Hwang, J.-H.; Kim, Y.-J. Neighborhood Effect on Elderly Depression in Republic of Korea. Int. J. Environ. Res. Public Health 2023, 20, 5200. [Google Scholar] [CrossRef]
- Moriya, S.; Muramatsu, T.; Tei, K.; Nakamura, K.; Muramatsu, M.; Notani, K.; Inoue, N. Relationships between oral conditions and physical performance in a rural elderly population in Japan. Int. Dent. J. 2009, 59, 369–375. [Google Scholar] [CrossRef]
- Albitar, M.M.; Maya, S.; Al Ashabia, K.K.; Hamzeh, G.; Kakaje, A. Modifiable Risk Factors for Stroke in Syria: A Nationwide Multi-centre Case-Control Study. Sci. Rep. 2024, 15, 115. [Google Scholar] [CrossRef]
- Viadel, A.; Laguna, L.; Tárrega, A. Digging into the roots of discomfort and difficult eating: Understanding elderly oral capabilities. Food Res. Int. 2025, 213, 116544. [Google Scholar] [CrossRef] [PubMed]
- Maltarić, M.; Kolak, M.; Kolarić, B.; Vranešić Bender, D.; Gajdoš Kljusurić, J. Cross-European Patterns of Obesity: Where Does Croatia Stand?—Descriptive Analysis of Waves 2015–2022 of the Survey of Health, Ageing and Retirement in Europe (SHARE) Including Adults Aged Over 50. Obesities 2025, 5, 66. [Google Scholar] [CrossRef]
- Ginnerup-Nielsen, E.; Christensen, R.; Heitmann, B.L.; Altman, R.D.; March, L.; Woolf, A.; Bliddal, H.; Henriksen, M. Prognostic value of illness perception on changes in knee pain among elderly individuals: Two-year results from the Frederiksberg Cohort study. Osteoarthr. Cartil. Open 2023, 5, 100403. [Google Scholar] [CrossRef] [PubMed]
- Berrington de Gonzalez, A.; Hartge, P.; Cerhan, J.R.; Flint, A.J.; Hannan, L.; MacInnis, R.J.; Moore, S.C.; Tobias, G.S.; Anton-Culver, H.; Freeman, L.B.; et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 2010, 363, 2211–2219. [Google Scholar] [CrossRef]
- Lyall, D.M.; Celis-Morales, C.; Ward, J.; Iliodromiti, S.; Anderson, J.J.; Gill, J.M.R.; Smith, D.J.; Ntuk, U.E.; Mackay, D.F.; Holmes, M.V.; et al. Association of Body Mass Index With Cardiometabolic Disease in the UK Biobank: A Mendelian Randomization Study. JAMA Cardiol. 2017, 2, 882–889. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Ford, E.S.; Bowman, B.A.; Dietz, W.H.; Vinicor, F.; Bales, V.S.; Marks, J.S. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003, 289, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Nathan, D.M. Long-term complications of diabetes mellitus. N. Engl. J. Med. 1993, 328, 1676–1685. [Google Scholar] [CrossRef] [PubMed]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Schaan, B.; Stuck, S.; Zuber, S. Data Resource Profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). Int. J. Epidemiol. 2013, 42, 992–1001. [Google Scholar] [CrossRef] [PubMed]
| Variable | Frequency n (%) |
|---|---|
| Gender | |
| Male | 2040 (43.5) |
| Female | 2647 (56.5) |
| Age (years) | |
| 50–64 | 1777 (37.9) |
| 65–74 | 1720 (36.7) |
| 75–85 | 879 (18.8) |
| >85 | 257 (5.5) |
| Living with partner | 1677 (35.8) |
| Retired | 2994 (63.4) |
| Normal Body mass index (kg/m2) | 1280 (27.3) |
| Leisure and Sport Activities | Age Group | p-Value * | |||
|---|---|---|---|---|---|
| 51–64 | 65–74 | 75–85 | >85 | ||
| Activities in the last year: | |||||
| done voluntary or charity work | 6.3 | 3.6 | 1.7 | 0.4 | <0.0001 |
| attended an educational or training course | 4.4 | 0.9 | 0.2 | 0.0 | <0.0001 |
| gone to a sport, social or other kind of club | 12.3 | 10.1 | 4.8 | 1.2 | <0.0001 |
| taken part in a political or community-related organization | 2.7 | 2.6 | 1.7 | 0.4 | <0.0001 |
| read books, magazines or newspapers | 50.3 | 49.5 | 42.7 | 28.0 | <0.0001 |
| did word or number games (crossword puzzles /Sudoku./etc.) | 24.2 | 24.9 | 20.3 | 12.6 | <0.0001 |
| played cards or games such as chess | 19.2 | 15.7 | 8.3 | 3.7 | <0.0001 |
| Sports or activities that are vigorous | |||||
| More than once a week | 47.0 | 30.6 | 17.1 | 5.4 | <0.0001 |
| Once a week | 14.6 | 14.0 | 12.3 | 3.9 | |
| One to three times a month | 14.7 | 16.3 | 12.9 | 5.4 | |
| Hardly ever, or never | 23.4 | 39.0 | 57.1 | 84.8 | |
| Physical inactivity | |||||
| Other | 96.6 | 93.3 | 81.8 | 61.9 | <0.0001 |
| Never vigorous nor moderate physical activity | 3.0 | 6.5 | 17.4 | 37.7 | |
| Frequency of Consumption | Age Group | p-Value * | |||
|---|---|---|---|---|---|
| 51–64 | 65–74 | 75–85 | >85 | ||
| Dairy products | |||||
| Every day | 47.9 | 49.4 | 51.3 | 58.8 | 0.1759 |
| 3–6 times a week | 26.1 | 25.6 | 25.1 | 23.7 | |
| Twice a week | 12.1 | 12.9 | 13.2 | 8.9 | |
| Once a week | 5.8 | 5.4 | 4.8 | 4.3 | |
| Less than once a week | 7.6 | 6.5 | 4.8 | 3.9 | |
| Legumes or eggs | |||||
| Every day | 10.5 | 10.5 | 8.8 | 8.2 | <0.0001 |
| 3–6 times a week | 30.2 | 32.2 | 31.2 | 30.7 | |
| Twice a week | 36.6 | 34.3 | 34.2 | 29.6 | |
| Once a week | 18.0 | 18.6 | 17.9 | 16.7 | |
| Less than once a week | 4.2 | 4.1 | 7.2 | 14.4 | |
| Meat, fish or poultry | |||||
| Every day | 54.3 | 52.6 | 44.4 | 46.3 | 0.0018 |
| 3–6 times a week | 37.5 | 39.0 | 44.0 | 42.0 | |
| Twice a week | 5.6 | 6.1 | 7.4 | 7.0 | |
| Once a week | 1.5 | 1.5 | 1.6 | 3.1 | |
| Less than once a week | 0.5 | 0.6 | 1.7 | 1.2 | |
| Fruits or vegetables | |||||
| Every day | 78.8 | 79.1 | 76.0 | 81.3 | 0.0118 |
| 3–6 times a week | 14.3 | 15.5 | 15.6 | 13.6 | |
| Twice a week | 4.0 | 3.1 | 5.3 | 3.9 | |
| Once a week | 2.1 | 1.5 | 0.8 | 0.8 | |
| Less than once a week | 0.3 | 0.5 | 1.5 | 0.0 | |
| Health Parameter | Age Group | p-Value * | |||
|---|---|---|---|---|---|
| 51–64 | 65–74 | 75–85 | >85 | ||
| Number of chronic diseases | |||||
| 0 | 31.6 | 16.4 | 7.2 | 7.4 | <0.0001 |
| 1 | 28.1 | 25.1 | 21.3 | 22.2 | |
| 2 | 20.9 | 24.5 | 25.0 | 21.0 | |
| 3+ | 19.0 | 33.7 | 45.6 | 49.0 | |
| CVDs and diabetes | |||||
| Heart attack: ever diagnosed/currently having | 8.7 | 14.2 | 20.1 | 26.5 | <0.0001 |
| High blood pressure or hypertension: ever diagnosed/currently having | 38.1 | 57.4 | 66.1 | 66.1 | <0.0001 |
| High blood cholesterol: ever diagnosed/currently having | 17.4 | 26.3 | 23.9 | 20.2 | <0.0001 |
| Stroke: ever diagnosed/currently having | 2.6 | 4.8 | 9.0 | 8.2 | <0.0001 |
| Diabetes or high blood sugar: ever diagnosed/currently having | 10.0 | 19.8 | 21.6 | 15.6 | <0.0001 |
| Self-perceived health—US version (SPUUS) | |||||
| Excellent | 10.9 | 5.3 | 2.7 | 1.6 | <0.0001 |
| Very good | 22.9 | 15.1 | 7.3 | 3.9 | |
| Good | 38.0 | 41.3 | 30.5 | 24.5 | |
| Fair | 19.6 | 24.2 | 34.4 | 34.6 | |
| Poor | 8.1 | 13.7 | 24.5 | 35.4 | |
| SPHUS-2 | |||||
| Very good/excellent | 33.7 | 20.4 | 10.0 | 5.4 | <0.0001 |
| Less than very good | 65.8 | 79.2 | 89.3 | 94.6 | |
| EURO-D caseness | |||||
| No | 78.9 | 76.3 | 63.2 | 45.9 | <0.0001 |
| Yes | 21.1 | 23.7 | 36.8 | 54.1 | |
| Parts of EURO-D (12 symptoms) | |||||
| Depression | 30.0 | 32.6 | 41.4 | 42.8 | <0.0001 |
| Pessimism | 14.4 | 17.2 | 28.0 | 41.2 | <0.0001 |
| Suicidality | 3.6 | 4.7 | 9.0 | 12.5 | <0.0001 |
| Guilt | 4.6 | 4.0 | 4.0 | 3.5 | <0.0001 |
| Sleep | 24.8 | 29.9 | 34.9 | 44.0 | <0.0001 |
| Interest | 7.8 | 9.6 | 15.5 | 24.5 | <0.0001 |
| Irritability | 26.4 | 25.3 | 28.4 | 30.4 | <0.0001 |
| Appetite | 6.1 | 7.8 | 9.6 | 17.9 | <0.0001 |
| Fatigue | 29.1 | 36.6 | 47.9 | 63.0 | <0.0001 |
| Concentration | 13.7 | 18.0 | 28.2 | 42.4 | <0.0001 |
| Enjoyment | 8.1 | 10.3 | 15.6 | 24.5 | <0.0001 |
| Tearfulness | 19.6 | 21.0 | 23.9 | 25.3 | <0.0001 |
| Observed Variable | Medium | p-Value | Low | p- Value | ||
|---|---|---|---|---|---|---|
| B | OR (% CI) | B | OR (% CI) | |||
| Activities | ||||||
| done voluntary or charity work | −0.46 | 0.63 (0.28–1.42) | 0.267 | −0.54 | 0.59 (0.21–1.67) | 0.316 |
| attended an educational or training course | −0.32 | 0.73 (0.24–2.16) | 0.567 | −0.16 | 0.86 (0.2–3.57) | 0.830 |
| gone to a sport, social or other kind of club | −0.55 | 0.58 (0.38–0.89) | 0.013 | −0.48 | 0.62 (0.32–1.21) | 0.163 |
| taken part in a political or community-related organization | −0.19 | 0.83 (0.36–1.89) | 0.651 | 0.15 | 1.16 (0.32–4.21) | 0.817 |
| read books, magazines or newspapers | 0.33 | 1.4 (0.96–2.04) | 0.084 | 0.22 | 1.25 (0.77–2.04) | 0.368 |
| did word or number games (crossword puzzles/Sudoku/etc.) | 0.07 | 1.07 (0.69–1.66) | 0.772 | 0.02 | 1.02 (0.58–1.79) | 0.953 |
| played cards or games such as chess | −0.30 | 0.74 (0.5–1.1) | 0.141 | −0.58 | 0.56 (0.3–1.04) | 0.066 |
| No additional sport activities | 0.37 | 1.45 (1.23–1.7) | 0.000 | 0.66 | 1.94 (1.59–2.37) | 0.000 |
| Physical inactivity | 0.13 | 1.14 (0.39–3.3) | 0.807 | 0.53 | 1.7 (0.52–5.63) | 0.382 |
| Dietary intake | ||||||
| Dairy products | −0.04 | 0.96 (0.83–1.11) | 0.614 | −0.01 | 0.99 (0.82–1.19) | 0.907 |
| Legumes and eggs | −0.15 | 0.86 (0.72–1.03) | 0.098 | −0.25 | 0.78 (0.62–0.97) | 0.024 |
| Meat, fish and poultry | 0.13 | 1.14 (0.86–1.51) | 0.375 | 0.11 | 1.12 (0.8–1.56) | 0.509 |
| Fruit and vegetable | 0.05 | 1.06 (0.83–1.35) | 0.660 | −0.01 | 0.99 (0.72–1.36) | 0.934 |
| CVDs and diabetes | ||||||
| Heart attack: ever diagnosed/currently having | −0.35 | 0.71 (0.39–1.27) | 0.248 | 0.04 | 1.04 (0.51–2.15) | 0.911 |
| High blood pressure or hypertension: ever diagnosed/currently having | 0.42 | 1.52 (0.99–2.34) | 0.054 | 0.45 | 1.57 (0.92–2.69) | 0.101 |
| High blood cholesterol: ever diagnosed/currently having | −0.31 | 0.73 (0.43–1.23) | 0.239 | −0.32 | 0.72 (0.38–1.37) | 0.323 |
| Stroke: ever diagnosed/currently having | −0.33 | 0.72 (0.3–1.72) | 0.459 | 0.28 | 1.32 (0.45–3.85) | 0.608 |
| Diabetes or high blood sugar: ever diagnosed/currently having | 0.11 | 1.12 (0.65–1.94) | 0.688 | 0.06 | 1.07 (0.54–2.11) | 0.855 |
| Number of chronic diseases | 0.13 | 1.14 (0.89–1.44) | 0.300 | 0.27 | 1.31 (0.99–1.73) | 0.058 |
| EURO-D | ||||||
| Depression | 0.04 | 1.04 (0.6–1.8) | 0.890 | 0.13 | 1.14 (0.6–2.2) | 0.686 |
| Pessimism | 0.29 | 1.34 (0.8–2.24) | 0.271 | 0.29 | 1.34 (0.71–2.52) | 0.370 |
| Suicidality | −0.32 | 0.73 (0.24–2.23) | 0.581 | 0.53 | 1.7 (0.49–5.89) | 0.405 |
| Guilt | −1.27 | 0.28 (0.12–0.68) | 0.005 | −1.08 | 0.34 (0.12–0.98) | 0.045 |
| Sleep | 0.14 | 1.15 (0.69–1.91) | 0.594 | −0.12 | 0.89 (0.48–1.64) | 0.704 |
| Interest | 0.02 | 1.02 (0.48–2.18) | 0.959 | 0.05 | 1.05 (0.43–2.55) | 0.913 |
| Irritability | −0.33 | 0.72 (0.44–1.19) | 0.204 | −0.63 | 0.54 (0.29–0.99) | 0.048 |
| Appetite | −0.27 | 0.76 (0.34–1.72) | 0.510 | −0.32 | 0.72 (0.28–1.88) | 0.508 |
| Fatigue | −0.03 | 0.97 (0.61–1.54) | 0.903 | 0.35 | 1.41 (0.81–2.48) | 0.225 |
| Concentration | 0.20 | 1.22 (0.66–2.24) | 0.521 | 0.65 | 1.91 (0.94–3.89) | 0.073 |
| Enjoyment | −0.12 | 0.88 (0.46–1.71) | 0.711 | 0.03 | 1.03 (0.46–2.3) | 0.934 |
| Tearfulness | −0.31 | 0.73 (0.34–1.58) | 0.430 | −0.16 | 0.85 (0.37–1.98) | 0.712 |
| Euro-D (yes) | 0.25 | 1.29 (0.54–3.06) | 0.563 | 0.07 | 1.07 (0.39–2.96) | 0.891 |
| CASP, low | 1.82 | 6.17 (0.08–481.4) | 0.413 | 4.63 | 10.15 (0.71–14.58) | 0.068 |
| CASP, medium | 1.18 | 3.26 (0.44–24.25) | 0.249 | 2.33 | 10.28 (0.99–16.26) | 0.051 |
| CASP, high | 1.23 | 3.41 (0.5–23.07) | 0.209 | 2.30 | 9.99 (1.08–92.77) | 0.043 |
| Sphus1 | 0.20 | 1.22 (0.9–1.66) | 0.201 | 0.35 | 1.42 (0.98–2.06) | 0.061 |
| Sphus2 | −0.28 | 0.75 (0.39–1.46) | 0.402 | −0.13 | 0.88 (0.38–2.03) | 0.757 |
| BMI | 0.60 | 0.55 (0.33–0.9) | 0.017 | 0.84 | 0.43 (0.24–0.78) | 0.005 |
| Retired | 0.01 | 1.01 (0.98–1.04) | 0.615 | 0.02 | 1.02 (0.98–1.05) | 0.367 |
| Marital status | 0.08 | 1.08 (0.95–1.23) | 0.222 | 0.33 | 1.39 (1.21–1.6) | <0.001 |
| Education level | −0.06 | 0.94 (0.88–1) | 0.061 | −0.09 | 0.91 (0.84–0.99) | 0.021 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maltarić, M.; Kolak, M.; Bender, D.V.; Gajdoš Kljusurić, J.; Kolarić, B. Quality of Life, Physical Activity, and Mental and Physical Health Status in Croatian Middle-Aged and Elderly Population. Healthcare 2025, 13, 2931. https://doi.org/10.3390/healthcare13222931
Maltarić M, Kolak M, Bender DV, Gajdoš Kljusurić J, Kolarić B. Quality of Life, Physical Activity, and Mental and Physical Health Status in Croatian Middle-Aged and Elderly Population. Healthcare. 2025; 13(22):2931. https://doi.org/10.3390/healthcare13222931
Chicago/Turabian StyleMaltarić, Manuela, Mirela Kolak, Darija Vranešić Bender, Jasenka Gajdoš Kljusurić, and Branko Kolarić. 2025. "Quality of Life, Physical Activity, and Mental and Physical Health Status in Croatian Middle-Aged and Elderly Population" Healthcare 13, no. 22: 2931. https://doi.org/10.3390/healthcare13222931
APA StyleMaltarić, M., Kolak, M., Bender, D. V., Gajdoš Kljusurić, J., & Kolarić, B. (2025). Quality of Life, Physical Activity, and Mental and Physical Health Status in Croatian Middle-Aged and Elderly Population. Healthcare, 13(22), 2931. https://doi.org/10.3390/healthcare13222931







