Abstract
Background/Objectives: Lay Community Health Workers (CHWs) play a critical role in reducing mental health disparities, particularly among underserved and vulnerable populations, by bridging gaps in care and promoting mental well-being. This narrative review aimed to identify and characterize training programs designed for CHWs, with a focus on those targeting cancer patients and individuals with chronic conditions. Methods: A comprehensive literature search was conducted across databases including PubMed, EBSCOhost, Scielo, Redalyc, and Google Scholar. From an initial pool of 10,372 references, 27 relevant articles were selected, encompassing research articles, training materials, curricula, and other resources. Results: The identified training methods included role-playing, instructional videos, and manuals designed to equip CHWs with skills in mental health intervention, prevention, management, education, and stigma reduction. Training programs also incorporated evidence-based interventions and psychological skill training. This review highlights a notable gap in research on CHW-led interventions in cancer palliative care and mental health. Conclusions: The findings support the development of a specialized mental health training program tailored for CHWs working with cancer survivors, to enhance their capacity to address mental health challenges, reduce stigma, and promote psychological well-being. Future efforts involve developing a training intervention for CHWs to support the needs of cancer survivors.
1. Introduction
1.1. Background on Community Health Workers
Mental health disorders represent a critical global challenge due to their high prevalence, substantial impact on quality of life, and significant socio-economic burden [1]. Approximately 25% of individuals are estimated to experience at least one mental health or behavioral condition during their lifetime [2]. Depression, identified by the World Health Organization as a leading cause of global disease burden, disproportionately affects low- and middle-income countries [3]. The coexistence of multiple chronic conditions, including both physical and mental disorders, further complicates patient care and management [4].
Although there are effective treatments available, many people with mental health conditions still do not receive the care they need [5]. This gap in care is especially pronounced in underserved groups such as Hispanic communities, where access to quality mental health services is hindered by factors like stigma, poverty, and low levels of health literacy [6,7].
A critical factor contributing to the mental health treatment gap is the shortage of trained mental health providers [8]. To address this challenge, delegating primary prevention efforts to CHWs has been proposed as a strategy to expand service coverage and improve access to culturally competent care [9]. CHWs play a vital role within public health systems by bridging the gap between health care services and communities through outreach, education, and advocacy [10]. Their contributions to health literacy promotion, counseling, and social support have demonstrated effectiveness across various chronic conditions [11]. In mental health care, CHWs are pivotal in the early intervention of conditions such as anxiety, depression, and trauma, potentially preventing the progression to more severe outcomes and reducing dependence on emergency services [12]. Moreover, their efforts empower individuals and communities to adopt proactive health management strategies [13].
Given their established contributions to mental health care, it is equally important to consider the expanding role of CHWs in cancer, a disease that represents one of the most significant global public health burdens, with markedly unequal effects across populations. In 2022, approximately 20 million new cancer cases and 9.7 million deaths were reported worldwide [14]. In terms of absolute burden, countries with a high Human Development Index (HDI) are projected to experience the largest increase in incidence, with an additional 4.8 million new cases expected by 2050, compared to 2022 estimates. However, the proportional increase in incidence is most notable in countries with a low HDI (142% increase) and in countries with a medium HDI (99%). Similarly, cancer mortality in these countries is projected to nearly double by 2050 [14].
CHWs are trusted intermediaries between marginalized populations and health systems, enabling their participation to significantly increase early detection and adherence to cancer screening (particularly breast, cervical, and colorectal cancers), as well as reduce inequities [15,16]. They also play a critical role in advanced care by fostering supportive care practices, reducing hospitalizations, and encouraging advance care planning. CHWs have also demonstrated long-term effectiveness in improving chronic disease management and reducing health disparities among minority populations [17,18,19]. In mental health support, their involvement is associated with sustainable improvements in health behaviors and overall community well-being [16]. Recently, CHWs have been integrated into cancer care, contributing to prevention efforts and survivorship support. Programs leveraging CHWs to deliver culturally tailored education on cancer screening have significantly increased screening rates among minority populations [20,21].
Beyond prevention, CHWs contribute to managing the physical and psychological burden associated with cancer. Individuals with cancer and survivors report poorer health status, increased distress levels, and a higher prevalence of chronic conditions compared to individuals without a cancer history [22]. Factors such as limited social support, low socioeconomic status, and persistent treatment-related symptoms further exacerbate vulnerability [23]. Involvement of CHWs in mental health interventions—such as psychoeducation, peer support groups, and referrals—has demonstrated improvements in emotional well-being and quality of life among cancer survivors [24].
Moreover, CHWs serve as essential intermediaries, helping patients navigate complex health care systems, largely through the provision of informational/educational, instrumental/logistical, affective/emotional, and appraisal support [25,26]. Despite these well-documented benefits, significant gaps remain regarding their effectiveness in palliative or supportive care settings [27]. This highlights the urgent need for targeted training on complex health topics, such as mental health in the context of cancer, which remains insufficient. Outreach and dissemination strategies must consider cultural factors to enhance CHW engagement and training efficacy [28].
1.2. The Importance of Training Lay Community Members as Mental Health Workers
Community-based participatory research (CBPR) emerges as a crucial framework for addressing the challenge of translating research findings into real-world practice, particularly within CHW programs [29]. CBPR acknowledges the expertise of community members in co-creating knowledge aimed at promoting public health and health equity [30]. By actively involving communities, CBPR facilitates the dissemination of scientific knowledge to marginalized populations, bridging critical access gaps [29].
One of the key ongoing challenges is preparing a workforce that is adequately trained to deliver psychological interventions grounded in evidence [31]. To support this goal, it is essential that training programs and curricula be culturally adapted, allowing CHWs to build the core competencies needed to engage with their communities effectively. This approach fosters mental health equity and helps broaden access to services. Furthermore, evaluations of these programs should consider not only clinical outcomes but also factors such as community empowerment and the long-term sustainability of the interventions [29].
Although the role of CHWs in mental health care is well established, research on the most effective training strategies remains limited. Recognizing this gap, the present study seeks to review, analyze, and synthesize the best practices identified across studies involving CBPR, CHWs, mental health, and cancer care. The overarching goal is to strengthen community capacity by equipping CHWs with essential training and resources to proactively address cancer care and related health conditions.
1.3. Study Aims and Objectives
Narrative reviews play a crucial role in advancing knowledge within a discipline by identifying, analyzing, evaluating, and interpreting the body of research on a specific topic. The present narrative review examines the educational and training strategies designed to equip CHWs with primary prevention skills in mental health. These competencies are essential for enabling CHWs to identify, manage, and refer individuals diagnosed with cancer, as well as their caregivers, who may be at an elevated risk for developing mental health disorders. The objectives of this review are to identify published articles that describe training protocols for CHWs, define the essential skills required in cancer and mental health contexts, examine the didactic strategies employed, and assess the scope and outcome of existing training programs. Our future plan is to use these findings to develop mental health training for community health workers in cancer care.
2. Materials and Methods
2.1. Study Design
This study was a narrative review conducted to identify key characteristics of training materials designed to equip lay community members as CHWs. The Covidence platform (Veritas Health Innovation, Melbourne, Australia) was utilized to facilitate the review process. Given the high volume of literature published annually on this topic, a selective approach was taken, prioritizing studies based on methodological rigor, relevance to the research objective, and contribution to understanding the essential components of training programs for CHWs [32,33]. To ensure appropriate expertise in information retrieval, the team received training and direct guidance from an academic librarian. However, resource limitations did not allow for a librarian to be a permanent member of the research team. In addition, several team members had prior experience in conducting literature reviews and designing search strategies.
Although PRISMA guidelines were not strictly applied, given the narrative nature of this review, a flowchart was included to enhance clarity and methodological transparency. This review was carried out as a narrative review rather than a systematic review, because no formal quality appraisal of the included studies was performed with standardized instruments. Instead, the selection of studies was guided by their methodological transparency, their relevance to the aims of the review, and the extent to which they contributed to understanding training strategies for CHWs. This approach made it possible to bring together essential elements from diverse sources, while recognizing that the absence of a structured critical appraisal represents a methodological limitation.
2.2. Eligibility Criteria
This narrative review included experimental studies such as randomized controlled trials (RCTs), non-randomized controlled trials (NRCTs), and quasi-experimental studies (pre-post designs) that described training components, strategies, or skills related to mental health prevention and promotion for CHWs. Systematic reviews and meta-analyses addressing CHW training components or competencies were also considered eligible. Studies targeting adults aged 18 years or older who were working as CHWs and describing mental health training programs or interventions were included. Web-based sources providing information on CHW training components, curricula, strategies, or educational materials were also screened. Interventions incorporating a mental health component and targeting mental health conditions (such as substance use, depression, anxiety, caregiver burden, and dementia), chronic conditions (such as diabetes, cardiovascular disease, and Human Immunodeficiency Virus [HIV]), and cancer were eligible. Only articles published in English or Spanish were considered for inclusion.
2.3. Search Strategy
A comprehensive search strategy was developed to retrieve relevant studies addressing the training of CHWs in mental health and cancer care. Searches were conducted through PubMed, EBSCOhost, Scielo, Redalyc, and Google Scholar, covering the period from 17 November 2023 to 7 March 2024. No restrictions were placed on the publication year to ensure a thorough capture of foundational and recent literature. The search utilized a series of keyword combinations aligned with the study’s four specific aims. Keywords included combinations such as “training OR teaching” AND “community health worker” AND “mental health” AND “cancer”; “training OR teaching OR capacity building” AND “community health worker” AND “mental health” AND “cancer”; and “curriculums OR protocols” AND “mental health promotion” AND “community health workers” to identify studies focusing on training components. To explore mental health prevention and promotion skills, combinations like “mental health prevention OR mental health promotion skills” AND “mental health workers OR lay health workers OR health promoters” and “mental health” AND “community mental health workers” AND “protocols AND cancer” were used. For identifying didactic approaches and training strategies, the search included “didactics OR strategies” AND “training” AND “community mental health workers” AND “cancer”. Finally, to capture training specifically related to cancer care, the search incorporated the keywords “community mental health workers” AND “mental health training” AND “cancer”. This structured approach was designed to maximize the retrieval of the relevant literature for this narrative review. Alongside peer-reviewed publications, we also examined web-based materials and non-academic sources, such as program manuals and organizational reports, to identify relevant training resources that are not typically indexed in academic databases.
2.4. Study Selection
All studies identified through the search strategy underwent an initial screening process based on titles and abstracts to assess adherence to the inclusion criteria. Studies were excluded if they focused exclusively on formally trained mental health professionals, such as clinical psychologists, social workers, or nurses, or if they involved participants under 18 years of age. In addition, studies lacking detailed descriptions of the training protocols or those presented solely as narrative reviews without new empirical data were excluded. After the preliminary screening, full-text articles were reviewed to ensure that they met all eligibility criteria before being included in the final analysis. One of the main challenges encountered was that many of the initially captured studies were clinical trials or intervention studies that focused on patient outcomes or opinions rather than describing CHW training initiatives. In addition, a considerable number of excluded records consisted of narrative reviews, conference abstracts, commentaries, or studies unrelated to mental health training for CHWs. These were screened out to ensure that only empirical studies or detailed descriptions of training programs were included in the final analysis. Studies were considered eligible if they described training initiatives for community health workers. These initiatives had to be aimed at improving skills—in general, mental health promotion and prevention. They also had to include resources to support people with chronic conditions such as diabetes, HIV, or cancer, who experience comorbid mental health issues.
2.5. Data Extraction and Management
Data from the included studies were systematically extracted and organized using an Excel spreadsheet, version 2508 (Microsoft Corporation, Redmond, WA, USA). For each study, relevant information such as study ID, title, authors, geographic region, study characteristics, methodologies employed, participant demographics, and inclusion and exclusion criteria were documented. Web-based resources and gray literature sources were similarly cataloged to maintain consistency across data sources. This structured approach facilitated efficient organization and enabled a comparative analysis across the selected articles, ensuring a comprehensive synthesis of the key components, strategies, and educational frameworks described for community mental health worker training programs.
2.6. Data Analysis
Data extracted from the selected studies were analyzed using a descriptive and thematic synthesis approach. Studies were organized into categories (e.g., research articles, training curricula, web-based resources, protocols) to facilitate systematic examination. An inductive process was applied to identify themes directly from the content of the included studies, rather than from a predetermined set of codes. To ensure consistency, eight members of the research team independently reviewed the extracted data and reached consensus through discussion when discrepancies arose.
3. Results
3.1. Article Selection Process
A total of 16,701 publications were evaluated by independent reviewers using Covidence during the screening process (Figure 1). Of these, 6329 were identified as duplicates and removed. The remaining 10,372 references were considered potentially relevant and underwent title and abstract screening resulting in the exclusion of 10,201 articles that were not relevant to our study. A total of 171 articles proceeded to full-text review, of which 144 were excluded because they did not meet the inclusion criteria. Ultimately, 27 articles were included for comprehensive data extraction analysis. The main reasons for exclusion at the full-text stage were that many articles did not describe training components, focused on health professionals other than CHWs, or lacked empirical data. Additional records consisted of editorials or opinion pieces, which were also excluded. These were categorized as research articles (n = 16), training materials (n = 7), curricula (n = 1), and others (n = 3).
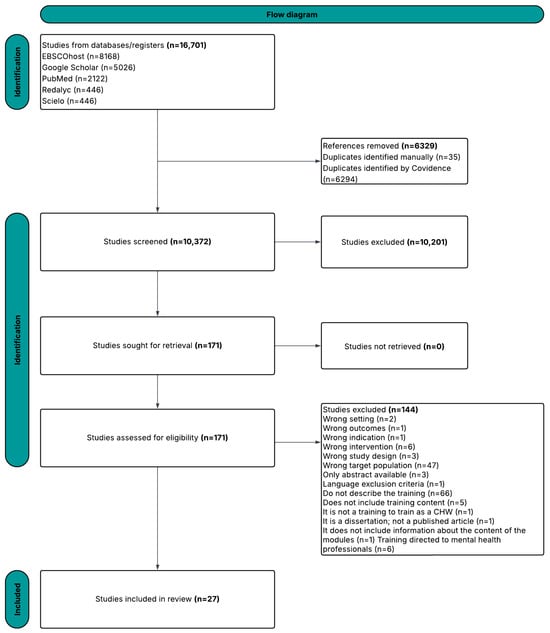
Figure 1.
Flow diagram illustrating the procedure for selecting work for inclusion in our study.
3.2. Training Components
In the 27 studies reviewed, we identified diverse training components for CHWs. These covered both mental health topics and different teaching strategies. Most studies (24 of 27) focused exclusively on mental health. This helped CHWs learn to recognize and address symptoms such as depression and anxiety, provide support, and refer people to medical care. Only three studies worked with populations facing chronic conditions, such as diabetes or HIV. These included content on mental health, but it was often treated as a secondary topic. In short, mental health and physical health were not addressed together and in a coordinated manner. Instead, they were kept separate. The most frequently reported component was mental health education, cited in 77.8% (n = 21) of the studies, emphasizing the foundational importance of disseminating knowledge in community-based mental health initiatives. Psychological intervention skill training was present in 44.4% (n = 12) of studies, often oriented toward equipping CHWs with practical tools for emotional support and behavioral management. A smaller subset (18.5%, n = 5) incorporated evidence-based intervention models, suggesting a growing, yet still limited, emphasis on standardized clinical approaches within community settings.
Additional training elements included family or caregiver-focused interventions (7.4%, n = 2), addressing health disparities (29.6%, n = 8), psychological first aid (22.2%, n = 6), and strategies to reduce mental health stigma (14.8%, n = 4). Moreover, 11.1% (n = 3) of studies provided content specifically focused on the role of CHWs in managing mental health issues, highlighting efforts to define and expand their scope of practice. Importantly, prevention strategies were addressed in 63.0% (n = 17) of the studies, indicating a strong emphasis on proactive care.
In terms of instructional methodology, instructional techniques were explicitly described in 33.3% (n = 9) of the studies. These included didactic sessions, interactive workshops, and experiential learning formats, although detailed reporting of teaching methods remained inconsistent across the literature. Together, these components underscore the heterogeneity of training approaches and content areas, while also revealing gaps in the systematic application of evidence-based models and instructional design.
3.3. Ethical and Pedagogical Approaches
This review highlighted various methods used to reinforce ethical principles and employ diverse teaching strategies in the training of CHWs. Ethical training commonly included content on research protections through CITI training, education on the Health Insurance Portability and Accountability Act (HIPAA), and instruction on the informed consent process both for CHWs during recruitment and for the individuals they serve.
Pedagogically, many programs incorporated didactic lectures, conferences, workshops, and classroom-based sessions, in addition to interactive tools such as games and case studies. Modeling strategies, particularly role-playing and the use of training manuals, were frequently employed to enhance engagement and learning outcomes. Audiovisual materials and educational aids were also used to support dynamic learning and accommodate various learning styles.
3.4. Instructional Strategies and Tools
The reviewed literature revealed a wide array of didactic approaches. The most frequently reported were role-playing (n = 5), videos (n = 4), manuals (n = 4), and presentations using PowerPoint, flipcharts, and brochures (n = 2). Other instructional methods included graphics and illustrations (n = 2), lectures (n = 2), case studies (n = 2), group work (n = 2), didactics (n = 2), supervision (n = 2), and field training (n = 2). Less commonly reported strategies involved virtual learning platforms such as Zoom (n = 1) and learning management systems like Canvas or Moodle (n = 1). Additional innovative methods included peer learning through pair activities, traditional classroom settings, games, case vignettes, software applications, video-based feedback, skills practice, and brainstorming—each of which was reported in one study.
3.5. Characteristics of Training Programs for Community Health Workers
3.5.1. Aim 1: Description of Training Components
The literature review revealed a range of materials implemented in training initiatives. These included research materials (59.3%, n = 16), training manuals or guides (25.9%, n = 7), curriculum documents (3.7%, n = 1), and other materials (11.1%, n = 3), such as program descriptions, training evaluations, and academic theses. Research materials were the most frequently utilized, followed by general training documents, with fewer instances of structured curricula or alternative formats.
Training programs were generally comprehensive and structured to provide CHWs with essential skills for supporting individuals with mental health needs in diverse contexts. Various training programs included components focused on crisis intervention, offering strategies for managing acute psychological symptoms such as suicidal ideation, panic attacks, and intense emotional distress. Case management training was also frequently reported and typically covered assessment, referral pathways, and follow-up procedures to maintain continuity of care. Programs placed a strong emphasis on the development of practical skills, utilizing techniques such as role-playing, case study analysis, and structured exercises in motivational interviewing, behavioral activation, and problem-solving.
Moreover, many programs integrated community engagement strategies, aiming to enhance mental health promotion, reduce stigma, and mobilize community-based resources. Administrative elements, including the refinement of training materials and the implementation of supervision and feedback systems, were also present to support training quality and worker preparedness. Overall, these components are not only foundational for theoretical understanding but are also critical in empowering CHWs to respond effectively to the complex psychosocial realities of the communities they serve.
3.5.2. Aim 2: Mental Health Prevention and Promotion Skills
Training programs for CHWs emphasize the development of a broad set of practical skills essential for delivering effective mental health support. A key foundational component across the reviewed programs was the ability to build and maintain supportive, trust-based relationships with clients. They also emphasize recognizing and addressing various mental health issues, as well as navigating mental health service systems effectively. CHWs are trained to engage empathetically, set achievable goals, and negotiate service agreements. They are also equipped to advocate for clients, mobilize community resources, and facilitate timely referrals when necessary. Skills such as understanding and applying crisis intervention techniques, managing suicide risk, and providing psychological first aid are integral parts of the training. Furthermore, CHWs are prepared to respond to various mental health emergencies, including identifying and addressing suicidal ideation, de-escalating panic attacks, and offering guidance following traumatic events. CHWs need core skills to effectively address mental health needs in their communities. High-quality training emphasizes client engagement, recognizing mental health concerns, navigating public and private services, and advocating for clients. These skills enable CHWs to build trust, deliver appropriate care, and empower community members to access available resources.
Training highlights the importance of the development of crisis intervention and mental health education, equipping CHWs to handle acute situations and promote mental well-being. Through the development of these skills, CHWs are better positioned to deliver comprehensive, empathetic, and culturally relevant mental health support to individuals and families in their communities.
3.5.3. Aim 3: Training Strategies for Community Health Workers
An analysis of the selected studies reveals that in-person training was the predominant method used for CHW instruction, accounting for 63.0% (n = 17) of the identified strategies. This modality was favored for its ability to foster the development of practical skills, encourage direct interaction, and provide immediate feedback elements deemed critical for CHWs working in community settings. In contrast, hybrid training approaches (combining in-person and online modalities) were reported in only 3.7% (n = 1), suggesting limited adoption despite their potential for flexibility and scalability.
Additionally, 22.2% (n = 6) of the studies did not specify the method of training delivery, indicating a gap in reporting and standardization across programs. Meanwhile, 11.1% (n = 3) utilized two or more delivery methods, highlighting the potential benefits of blended learning environments that draw on multiple instructional techniques. Of the three studies that reported the use of two or more instructional methods (11.1%), none were designed as comparative trials contrasting single versus multimodal approaches. Rather, the integration of strategies (e.g., integrating role-playing with manuals or video content) was used as a practical resource to increase participation, address different learning styles, and enhance knowledge retention. Therefore, the potential benefits are based on observations of practice and experience, not on comparative studies. The overall predominance of face-to-face formats underscores a preference for immersive, hands-on training that facilitates CHWs engagement and skill development within the communities they serve.
Didactic strategies in CHW training programs commonly included the use of manuals, presentations, graphics, illustrations, and video-based content. Six studies specifically referenced the use of manualized materials, which were adapted to various contexts and delivery formats [34,35,36,37,38,39]. For example, Chiumento et al. [34] adapted an individual intervention manual for group settings, incorporating content on psychoeducation, motivational interviewing, stress management, behavioral activation, and social support enhancement.
Didactic presentations were another frequently reported strategy, used to structure and deliver core content [37,38,40,41,42]. Uriarte et al. [40] described the use of slide-based curricula designed to scaffold complex content and avoid cognitive overload. Graphics and illustrations were employed to enhance accessibility and visual learning, as supported by Glenberg and Langston [43], who argued that visual aids help readers build mental models and improve comprehension [9,36,38,40,41].
Video content also played a prominent role in training programs [35,38,44,45,46]. Tyagi et al. [38] partnered with a local video production company to create a short, cultural platform accessible via smartphones and tablets.
Role-playing exercises were widely used across studies to develop communication skills and practical competencies [9,12,35,37,40,42,45,46]. These exercises were applied in various contexts, including mental health screening, cancer care communication, HIV interventions, and leadership development. For instance, within the MESA intervention, role-play activities helped participants apply coping strategies in simulated real-life scenarios, reinforcing both content knowledge and experiential learning.
Additional strategies included modeling, interactive lectures, group discussions, supervision site visits, and pair activities, as reported by Bordeaux-Rank [47], Shields-Zeeman et al. [45], and Uriarte et al. [40]. These methods facilitated knowledge retention and skill acquisition through dynamic and participatory leaning environments. For example, Moore-Monroy et al. [41] integrated tools such as Flip n Tell easel binders, anatomy visuals, and localized community resources to contextualize learning within structural health care barriers.
Beyond simulated exercises, several training programs incorporated real-word fieldwork to reinforce knowledge application. Malla et al. [44] emphasized clinical shadowing and hands-on sessions in outpatient settings, with instruction on risk management protocols and patient documentation. Similarly, Monton et al. [46] implemented a three-month curriculum combining synchronous and asynchronous learning with experiential field training, aiming to enhance CHWs’ competencies in palliative care.
Bordeaux-Rank [47] developed a five-day Training of Trainers program based on the Community-Based Psychological First Aid (CBPFA) model. This model emphasized community resilience and psychological support during emergencies. The training included interactive lectures and field-based activities, equipping CHWs with practical tools to deliver psychological first aid and make timely referrals for professional intervention.
3.6. Overview of Training Content and Structure
A synthesis of selected trainings interventions reveals a range of methodologies, implementation contexts, and target populations that illustrate the diverse applications of community-based mental health training programs (see Table 1). The summarized studies include quasi-experimental, qualitative, and mixed methods designs, implemented across diverse regions such as India, South Africa, and the United States. Target populations included rural CHWs, direct care personnel, and volunteer community educators, all of whom were engaged in strengthening local mental health capacities.

Table 1.
Summary of selected community-based mental health training programs.
Regarding training content, key components included evidence-based intervention models, instructional techniques, mental health education, and psychosocial interventions skills (see Table 2). Several programs also addressed prevention, stigma reduction, and health disparities. For instance, Taking Charge of My Life and Health focused on personal empowerment and self-care, while initiatives such as MESA and SONRISA offered culturally tailored approaches for promotoras and migrant communities. These trainings reflect a multidimensional framework aimed at building technical, psychoeducational, and community-oriented competencies among CHWs and other frontline actors.

Table 2.
Summary of key skills categories in reviewed training programs.
Overall, a comparison across interventions shows that programs combining didactic content with interactive strategies such as role-playing, case discussions, or field-based practice tended to report stronger improvements in CHWs’ knowledge, confidence, and communication skills. In contrast, training relying primarily on didactic lectures or printed manuals provided more limited evidence of sustained outcomes. This comparative perspective highlights the added value of experiential and participatory methods for strengthening CHWs’ mental health competencies.
4. Discussion
4.1. Summary of Findings Regarding Training Characteristics
The findings of this narrative review reveal that CHWs’ training programs are remarkably comprehensive and integrate a wide range of essential components for providing effective mental health support. This is evidenced by previous research highlighting the need for holistic training that includes theoretical foundations and practical tools for addressing community mental health challenges. The continued incorporation of research materials as core components in training design highlights a growing emphasis on evidence-based approaches. This is consistent with existing research advocating for the development of data-driven training to ensure effectiveness and contextual relevance.
The key components of the training identified, such as the detection of mental health needs in diverse populations, crisis intervention strategies (e.g., for suicidal ideation and panic attacks), and case management, reflect standard best practices reported in the community health literature. Additionally, the use of interactive methods like role-playing, case studies, and motivational interviewing coincides with findings from previous studies that suggest experiential learning improves skill acquisition and confidence among CHWs.
When comparing across studies, several patterns emerged. While many programs relied heavily on didactic lectures or printed manuals, interventions that combined didactic content with interactive strategies, such as role-playing, case discussions, or field-based practice tended to report stronger improvements in CHWs’ knowledge, confidence, and communication skills. This highlights the heterogeneity of approaches used across the literature and points to persistent gaps in the systematic use of evidence-based instructional models. These findings suggest that experiential and participatory methods may be especially valuable for strengthening CHWs’ mental health competencies and should be further prioritized in the design of future training initiatives.
4.2. Implications for Community Health Workers’ Training Programs
These results have significant implications for the structure and delivery of training programs for community health workers. By integrating a broad range of didactic and practical elements, the programs ensure that community health workers are prepared to address challenging mental health needs in their communities. Therefore, the focus on cultural competency is particularly relevant in multicultural contexts. This echoes previous research, which highlights the need for training that promotes culturally responsive care. This component will not only strengthen the therapeutic alliance but also help promote the accessibility and equity of mental health services.
The emphasis on community engagement, stigma reduction, and resource mobilization indicates a paradigm shift towards more proactive and community-centered models of mental health care. Furthermore, the attention to supervision, feedback mechanisms, and administrative refinement suggests a commitment to continuous quality improvement, which is essential for adapting to evolving community needs and maintaining the efficacy of interventions.
These findings are particularly relevant in settings affected by concurrent social and environmental stressors. One of the aims of this review was to support the design of training programs that strengthen the ability of CHWs to work effectively in settings where structural challenges amplify mental health needs. For example, in Puerto Rico following Hurricane Maria, medically vulnerable populations, such as cancer survivors, have faced additional barriers to access to care. This highlights the importance of training programs that prepare CHWs to respond effectively to crises and mental health needs within fragile infrastructures [52,53]. This is why addressing these vulnerabilities in training content ensures that community health workers are equipped to provide emotional support and community resilience during emergencies.
Taken together, these results suggest that future training efforts for CHWs should be guided by a structured framework that combines three key elements. First, culturally adapted didactic and interactive strategies such as role playing, case-based exercises, and audiovisuals tools appear to be more effective than lectures or manuals alone. Second, evaluation should not be limited to knowledge gains, but also include changes in confidence, attitudes, and community-level outcomes. Third, implementation factors such as supervision, ongoing support, and scalability through hybrid or digital platforms must be considered to ensure sustainability. Framing CHW training programs within these dimensions may enhance their impact and promote the integration of mental health support into cancer care.
4.3. Gaps in Cancer-Related CHW Training Programs
According to the findings and scope of this narrative review, there is a notable lack of published information on formal training programs specifically designed for CHWs that address the mental health needs of cancer patients, survivors, caregivers, and those at risk of psychological distress related to cancer. This gap must be addressed to develop and establish training programs capable of providing the necessary tools to meet the community-level needs of these groups. Training programs in mental health and cancer are essential for educating health professionals and communities on a comprehensive approach to these diseases. Such programs should include psycho-oncology, intervention techniques, stress management, and emotional support, enabling holistic care that enhances the quality of life for patients and their families. Additionally, they should promote interdisciplinary collaboration and a deeper understanding of how cancer and its treatment impact mental health, ensuring that professionals and CHWs are equipped to provide empathetic and effective palliative care to patients with cancer and their families.
4.4. Future Directions for Research and Practice
This review lays the groundwork for subsequent phases of the project, particularly the joint development of training materials. These are culturally adapted in collaboration with a Community Intervention Team. Future research should aim to evaluate the effectiveness of these training programs once implemented, including longitudinal evaluations of CHW performance, service delivery outcomes, and community mental health indicators. Furthermore, additional studies are needed to investigate the scalability and sustainability of these training models in diverse geographic and sociocultural contexts.
Practical examples, such as the Women’s Holistic Health (Salud Holística para la Mujer, SAHOM) program and the peer-led Nuevo Amanecer-II intervention, underscore the value of culturally tailored initiatives based on community-identified needs. Although SAHOM is not a training program per se, its participatory development process and holistic emphasis on emotional well-being illustrate how principles of cultural equity and community responsiveness can inform effective interventions. In contrast, the peer-led Nuevo Amanecer-II demonstrated the potential for integrating experiential learning, empathy, and sociocultural awareness into community-based psychosocial support models [54,55]. Future research should explore how such community-centered frameworks could be adapted and expanded to enhance the work of community health workers.
In addition to these cultural and participatory dimensions, this literature review also highlights a technological gap. Our analysis of 27 studies published between 1987 and 2023, showed that while training approaches have evolved from traditional and manualized methods toward digital formats in recent years (e.g., [56,57]), none incorporated artificial intelligence (AI), explainable AI (XAI), or intelligent training platforms. This absence may be explained by the relatively recent development of such technologies. Identifying this gap is crucial, as future research should examine how AI-driven tools, such as conversational agents, mobile-based screening, and adaptive e-learning platforms, might complement culturally tailored models, enhance individual adaptation, and support the long-term sustainability of CHW training programs in mental health.
5. Conclusions
5.1. Key Takeaways from the Narrative Review
The literature review provides insight into specific areas and topics, while highlighting knowledge gaps that remain to be explored [58]. A key finding of this narrative review was the identification of a substantial gap in the availability of training programs specifically designed to prepare CHWs to support people diagnosed with cancer and their caregivers. These programs should include components of prevention, assessment, identification, treatment, and referral to specialized care when necessary.
The review also identified and classified other training programs aimed at addressing chronic conditions such as diabetes, obesity, anxiety, and depression, among others. Additionally, it analyzed the most employed didactic strategies and assessed their frequency of implementation. According to our findings, the most used role-plays, instructional manuals, and didactic presentations were important. This lays the groundwork for future studies to determine which strategies are most appropriate for training health promoters in mental health and chronic conditions, such as cancer.
5.2. Importance of Ongoing Efforts in Training Community Health Workers
The importance of continuing efforts to train CHWs is underscored by current statistics and projections, which estimate that over 39.5% of the population will experience cancer, a condition that has both physical and mental health consequences [59]. There is a well-documented need for increased access to mental health services in both the United States and Puerto Rico. Given that Puerto Rico is frequently impacted by atmospheric events, seismic activity, and systemic challenges in health care infrastructure, it is crucial to implement strategies that empower communities to manage prevention, identification, treatment, and referral processes effectively.
5.3. Call for Further Research and Program Development
This narrative review enabled a rigorous and comprehensive exploration of the existing literature and revealed a clear gap in the development of training programs and research focused on CHWs who support individuals with comorbid cancer and mental health conditions, as well as their caregivers. This review offers a foundation for future projects aiming to design training models grounded in evidence-based recommendations and pedagogical strategies tailored to this specific context, with cultural sensitivity to the Puerto Rican population.
Considering Puerto Rico’s current epidemiological and sociopolitical context, it is important that professionals in psychology, public health, medicine, and related disciplines collaborate in the development of culturally and contextually appropriate programs. These initiatives should have the primary objective of empowering communities with the tools and resources necessary to respond autonomously and effectively to their specific health challenges, especially considering the limitations of traditional treatment and referral systems, which are often inaccessible to the population.
Author Contributions
Conceptualization, M.R.-R., N.T.-B., and E.M.C.-F.; methodology, M.R.-R., N.T.-N., and Z.R.-C.; software, J.D.-R., D.R.-A., and C.I.P.-V.; validation, J.D.-R., D.R.-A., and E.M.C.-F.; formal analysis, J.D.-R. and D.R.-A.; investigation, M.R.-R., J.D.-R., N.T.-B., N.T.-N., J.R.-G., J.M.-N., G.M.-Q., P.d.R.-R., G.L.-E., and Z.R.-C.; resources, G.N.A.-P. and E.M.C.-F.; data curation, M.R.-R., J.D.-R., N.T.-N., D.R.-A., J.R.-G., J.M.-N., G.M.-Q., P.d.R.-R., G.L.-E., and Z.R.-C.; writing—original draft preparation, M.R.-R., J.D.-R., N.T.-B., J.R.-G., and J.M.-N.; writing—review and editing, D.R.-A., G.M.-Q., P.d.R.-R., G.L.-E., Z.R.-C., C.C.-C., R.C.-M., P.C., J.J.-C., E.R.-S., G.N.A.-P., and E.M.C.-F.; visualization, M.R.-R., J.D.-R., and Z.R.-C.; supervision, Z.R.-C., C.C.-C., C.I.P.-V., and E.M.C.-F.; project administration, Z.R.-C. and C.C.-C.; funding acquisition, G.N.A.-P. and E.M.C.-F. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by a grant (U01CA290613; P30 CA008748) from the National Cancer Institute.
Institutional Review Board Statement
This project was revised and approved by the Ponce Health Sciences University-Ponce Research Institute Review Board (2303136895A001). It complies with the United States 45 Code of Federal Regulations part 46 (45 CFR 46) related to the Common Rule and human subject regulations.
Informed Consent Statement
Not applicable.
Data Availability Statement
This study is a narrative literature review. No new data were generated or analyzed in the course of this research. However, details regarding the search strategy, including the databases consulted and the selection process conducted via COVIDENCE, are available upon reasonable request. Interested researchers may contact the corresponding author for further information.
Acknowledgments
The author gratefully acknowledges all co-authors and the entire team of the Psycho-Oncology Research Lab, led by E.C.-F., for their invaluable support in overall project logistics. Their contributions were essential to making this project possible.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CHWs | Community Health Workers |
| CBPR | Community-based participatory Research |
| RCTs | Randomized Controlled Trials |
| NRCTs | Non-Randomized Controlled Trials |
| HIV | Human Immunodeficiency Virus |
| CBPFA | Community-based Psychological First Aid |
| HIPPA | Health Insurance Portability and Accountability Act |
| SAHOM | Salud Holística para la Mujer |
Appendix A

Table A1.
Selected community-based mental health training programs.
Table A1.
Selected community-based mental health training programs.
| Authors | Title | Year | Methodology/Study Desing | Target Audience | Country |
|---|---|---|---|---|---|
| Abadi, M. H., Drake, C., Richard, B. O., Schweinhart, A., Rychener, D., Shamblen, S. R., & Grimsgaard, S. N. [50] | An evaluation of the facilitator training to implement ‘Taking charge of my life and health’, a peer-led group program to promote self-care and patient empowerment in Veteran participants | 2020 | Quasi-experimental | Veteran peers | United States |
| Andreae, S. J., Andreae, L. J., Cherrington, A. L., Lewis, M., Johnson, E., Clark, D., & Safford, M. M. [60] | Development of a Community Health Worker-Delivered Cognitive Behavioral Training Intervention for Individuals with Diabetes and Chronic Pain | 2018 | Qualitative | Ten community members were trained and certified as CHWs. All were females, nine were African American, all had some college or a college degree, and five reported an income of USD 40,000 or more per year | United States |
| Armstrong, G., Kermode, M., Raja, S., Suja, S., Chandra, P., & Jorm, A. F. [9] | A mental health training program for community health workers in India: impact on knowledge and attitudes | 2011 | Quasi-experimental | Training participants were community health workers sourced through Gramina Abrudaya Seva Samstha (GASS), an NGO operating in Doddaballapur Taluk, Bangalore Rural District, Karnataka, India. The types of community health workers included Junior Health Assistants, Village Rehabilitation Workers, and ASHA workers | India |
| Bordeaux-Rank, J. A. [47] | Tribal Participatory Research with Community-based Psychological First Aid Training for Native Direct Care Staff: A Continuation Study | 2014 | Mixed Methods | Native American communities | United States |
| Chaudhary, A., Dosto, N., Hill, R., Lehmijoki-Gardner, M., Sharp, P., Daniel Hale, W., & Galiatsatos, P. [48] | Community Intervention for Syrian Refugees in Baltimore City: The Lay Health Educator Program at a Local Mosque | 2019 | Cohort study | Community members who would volunteer their time to learn about health care resources and information that could be utilized to aid refugees in their assimilation into the US healthcare system | United States |
| Cheffi, A., Harrison, S., & Stephan, A. [61] | Community Based Mental Health–A Training Guide for Community Providers | 2023 | Does not describe | Does not describe | |
| Edelblute, H. B., Clark, S., Mann, L., McKenney, K. M., Bischof, J. J., & Kistler, C. [42] | Promotoras across the border: a pilot study addressing depression in Mexican women impacted by migration | 2014 | Quasi-experimental | Mexican immigrant women in the US | Mexico |
| Gormley, M., Loughran, C., Conte, J., & Dunn Navarra, A. M. [35] | Trends in U.S. HIV Peer Health Worker Training Strategies and Approaches: A Scoping Review of the Literature | 2023 | Scoping Review | U.S. HIV peer health workers | United States |
| Hofmann-Broussard, C., Armstrong, G., Boschen, M. J., & Somasundaram, K. V. [62] | A mental health training program for community health workers in India: Impact on recognition of mental disorders, stigmatizing attitudes and confidence. | 2016 | Experimental/non-randomized controlled trial | Rural India | India |
| Hossain, D., Gorman, D., Eley, R., & Coutts, J [63] | Farm Advisors’ reflections on Mental Health First Aid training | 2009 | Quasi-experimental | Thirty-two farm advisors working in Southern Queensland, Australia, who attended MHFA training | Australia |
| Malla, A., Margoob, M., Iyer, S., Joober, R., Lal, S., Thara, R., Mushtaq, H., & Mansouri, B. I. [44] | A Model of Mental Health Care Involving Trained Lay Health Workers for Treatment of Major Mental Disorders Among Youth in a Conflict-Ridden, Low-Middle Income Environment: Part I Adaptation and Implementation | 2019 | Qualitative | Recruited and trained 40 LHWs (18 males and 22 females) from villages within the Ganderbal district | India |
| McCabe, O. L., Marum, F., Mosley, A., Gwon, H. S., Langlieb, A., Everly, G. S., Jr, Kaminsky, M. J., & Links, J. M. [64] | Community capacity-building in disaster mental health resilience: a pilot study of an academic/faith partnership model | 2012 | Mixed Methods | Faith communities, participants representing Christian, Jewish, and Muslim FBOs, respectively | United States |
| Michael, A., Thirumoorthy, A., Girish, N., & Sivakumar, P. T. [65] | Training Community health workers in geriatric mental health: Process of manual development and pilot testing findings | 2018 | Quasi-experimental | Interviews (n = 23) used a semi-structured interview guide prepared by the researchers, and the study included geriatric mental health professionals, experts from non-governmental organizations, primary health center physicians, Taluk Officers, CHWs, community members, and the elderly. The semi structured questionnaire used was different for each group of key informants. Five health workers from one of the primary health centers under the BBMP south were the participants in the pilot. The Mental Health Literacy Survey Questionnaire was used to assess the difference between pre- and post-assessments | India |
| Paramasivam, R., Elangovan, A. R., Amudhan, S., Kommu, J. V. S., Haridas, H., & Sriramalu, S. B. [66] | Intervention-based mental health training for community level workers in India—A systematic review | 2022 | Systematic Review | CHWs and mental health | India |
| Quinnett P. G. [56] | The Certified QPR Pathfinder Training Program: A Description of a Novel Public Health Gatekeeper Training Program to Mitigate Suicidal Ideation and Suicide Deaths | 2023 | Qualitative | Person with a high risk of suicide | United States |
| Reinschmidt, K. M., & Chong, J. [51] | SONRISA: a curriculum toolbox for promotores to address mental health and diabetes. | 2005 | Qualitative | Promotores (community health workers) who work with Hispanic clients to prevent or manage diabetes | Latin America United States |
| Reinschmidt, K. M., Philip, T. J., Alhay, Z. A., Braxton, T., & Jennings, L. A. [57] | Training Community Health Workers to Address Disparities in Dementia Care: A Case Study from Oklahoma With National Implications | 2023 | Quasi-experimental | Older population in Oklahoma City | United States |
| Robertson, M. N., DeShong, H. L., Steen, J. S., Buys, D. R., & Nadorff, M. R. [67] | Mental health first aid training for Extension agents in rural communities | 2021 | Mixed Methods | Rural communities, farmers | United States |
| Ryan, A. S., & Epstein, I. [68] | Mental health training for Southeast Asian refugee resettlement workers | 1987 | Mixed Methods | Southeast Asian workers, refugees, refugee community support network in northeastern USA. | United States |
| Shields-Zeeman, L., Pathare, S., Walters, B. H., Kapadia-Kundu, N., & Joag, K. [45] | Promoting wellbeing and improving access to mental health care through community champions in rural India: the Atmiyata intervention approach | 2017 | Mixed Methods | Two populations experiencing varying levels of distress: people with emotional stress and/or common mental health problems and people with severe mental illness | India |
| Sibeko, G., Milligan, P. D., Roelofse, M., Molefe, L., Jonker, D., Ipser, J., Lund, C., & Stein, D. J. [49] | Piloting a mental health training programme for community health workers in South Africa: an exploration of changes in knowledge, confidence and attitudes | 2018 | Mixed Methods | Community health workers | South Africa |
| Smith, M. V., & Kruse-Austin, A. [13] | A gender-informed model to train community health workers in maternal mental health | 2015 | Quasi-experimental | Mothers living in the city of New Haven | United States |
| Stacciarini, J. M., Rosa, A., Ortiz, M., Munari, D. B., Uicab, G., & Balam, M. [69] | Promotoras in mental health: a review of English, Spanish, and Portuguese literature | 2012 | Mixed Methods | Community health workers | Western Countries |
| Tyagi, V., Khan, A., Siddiqui, S., Kakra Abhilashi, M., Dhurve, P., Tugnawat, D., Bhan, A., & Naslund, J. A. [38] | Development of a Digital Program for Training Community Health Workers in the Detection and Referral of Schizophrenia in Rural India | 2023 | Qualitative | Rural India | India |
| Weaver, A., & Lapidos, A. [70] | Mental Health Interventions with Community Health Workers in the United States: A Systematic Review | 2018 | Systematic Review | Systematic review of mental health interventions with CHWs in the United States | United States |
| Wennerstrom, A., Vannoy, S. D., 3rd, Allen, C. E., Meyers, D., O’Toole, E., Wells, K. B., & Springgate, B. F. [12] | Community-based participatory development of a community health worker mental health outreach role to extend collaborative care in post-Katrina New Orleans | 2011 | Qualitative | Community to address post-disaster mental health disparities | United States |
| Wright, J., & Chiwandira, C. [71] | Building capacity for community mental health care in rural Malawi: Findings from a district-wide task-sharing intervention with village-based health workers. | 2016 | Qualitative | Zomba district of southern Malawi. Consists of villages of 200–1000 people, small trading centers, and one urban center in Zombatown. The HSAs’ brief biomedical training and accessibility within local populations mean they have experience navigating differing perspectives of causation of and treatment for health problems | Malawi |

Table A2.
Key skill categories in reviewed training programs.
Table A2.
Key skill categories in reviewed training programs.
| Reference of Article | Training Name | Training Skills Categories |
|---|---|---|
| Abadi, M. H., Drake, C., Richard, B. O., Schweinhart, A., Rychener, D., Shamblen, S. R., & Grimsgaard, S. N. (2020). An evaluation of the facilitator training to implement ‘Taking charge of my life and health’, a peer-led group program to promote self-care and patient empowerment in Veteran participants. Patient education and counseling, S0738-3991(20)30332-3. Advance online publication. https://doi.org/10.1016/j.pec.2020.06.014 [50] | “Taking charge of my life and Health”—a peer-led program | Evidence-based intervention models, roles of CMHWs in helping to prevent or manage mental health issues, psychological intervention skills training, prevention |
| Andreae, S. J., Andreae, L. J., Cherrington, A. L., Lewis, M., Johnson, E., Clark, D., & Safford, M. M. (2018). Development of a Community Health Worker-Delivered Cognitive Behavioral Training Intervention for Individuals With Diabetes and Chronic Pain. Family & community health, 41(3), 178–184. https://doi.org/10.1097/FCH.0000000000000197 [60] | Does not describe the name of the training/intervention | Roles of CMHWs in helping to prevent or manage mental health issues |
| Armstrong, G., Kermode, M., Raja, S., Suja, S., Chandra, P., & Jorm, A. F. (2011). A mental health training program for community health workers in India: impact on knowledge and attitudes. International journal of mental health systems, 5(1), 17. https://doi.org/10.1186/1752-4458-5-17 [9] | Does not describe the name of the training/intervention | Instructional techniques, mental health education, prevention, psychological first aid |
| Bordeaux-Rank, J. A. (2014). Tribal participatory research with community-based psychological first aid training for Native direct care staff: A continuation study. ProQuest Dissertations Publishing. [47] | Community-based psychological first aid training | Instructional techniques; psychological intervention skills training |
| Chaudhary, A., Dosto, N., Hill, R., Lehmijoki-Gardner, M., Sharp, P., Daniel Hale, W., & Galiatsatos, P. (2019). Community Intervention for Syrian Refugees in Baltimore City: The Lay Health Educator Program at a Local Mosque. Journal of religion and health, 58(5), 1687–1697. https://doi.org/10.1007/s10943-019-00893-9 [48] | The Lay Health Educator Program Curriculum | Mental health education; prevention |
| Cheffi, A., & Harrison, S. (2023). Community-based mental health (CBMH) training guide. IFRC Reference Centre for Psychosocial Support. Copenhagen, Denmark. [61] | Community-Based Mental Health a Training Guide for Community Providers | Instructional techniques, mental health education, prevention, training aimed at reducing health disparities |
| Edelblute, H. B., Clark, S., Mann, L., McKenney, K. M., Bischof, J. J., & Kistler, C. (2014). Promotoras across the border: a pilot study addressing depression in Mexican women impacted by migration. Journal of immigrant and minority health, 16(3), 492–500. https://doi.org/10.1007/s10903-012-9765-5 [42] | Mujeres en Solidaridad Apoyándose (MESA) | Instructional techniques, psychological intervention skills training, prevention |
| McCabe, O. L., Marum, F., Mosley, A., Gwon, H. S., Langlieb, A., Everly, G. S., Jr., Kaminsky, M. J., & Links, J. M. (2012). Community capacity-building in disaster mental health resilience: A pilot study of an academic/faith partnership model. International Journal of Emergency Mental Health, 14(2), 112–122. [64] | Does not describe the name of the training/intervention | Mental health education, psychological intervention skills training |
| Gormley, M., Loughran, C., Conte, J., & Dunn Navarra, A. M. (2023). Trends in U.S. HIV Peer Health Worker Training Strategies and Approaches: A Scoping Review of the Literature. The Journal of the Association of Nurses in AIDS Care: JANAC, 34(4), 331–348. https://doi.org/10.1097/JNC.0000000000000415 [35] | Does not describe the name of the training/intervention | Prevention; instructional techniques |
| Hofmann-Broussard, C., Armstrong, G., Boschen, M. J., & Somasundaram, K. V. (2016). A mental health training program for community health workers in India: impact on recognition of mental disorders, stigmatizing attitudes and confidence. International Journal of Culture and Mental Health, 10(1), 62–74. https://doi.org/10.1080/17542863.2016.1259340 [62] | Does not describe the name of the training/intervention | Mental health education, training aimed at reducing health disparities, training aimed at reducing stigma |
| Hossain, D., Gorman, D., Eley, R., & Coutts, J. (2009). Farm Advisors’ reflections on Mental Health First Aid training. Australian E-Journal for the Advancement of Mental Health, 8(1), 105–111. https://doi.org/10.5172/jamh.8.1.105 [63] | Mental health first aid training | Prevention; instructional techniques; mental health education |
| Malla, A., Margoob, M., Iyer, S., Joober, R., Lal, S., Thara, R., Mushtaq, H., & Mansouri, B. I. (2019). A Model of Mental Health Care Involving Trained Lay Health Workers for Treatment of Major Mental Disorders Among Youth in a Conflict-Ridden, Low-Middle Income Environment: Part I Adaptation and Implementation. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 64(9), 621–629. https://doi.org/10.1177/0706743719839318 [44] | Does not describe the name of the training/intervention | Prevention; Instructional techniques; mental health education |
| Michael, A., Thirumoorthy, A., Girish, N., & Sivakumar, P. T. (2018). Training Community health workers in geriatric mental health: Process of manual development and pilot testing findings. Asian journal of psychiatry, 38, 12–15. https://doi.org/10.1016/j.ajp.2018.10.017 [65] | Does not describe the name of the training/intervention | Prevention |
| Paramasivam, R., Elangovan, A. R., Amudhan, S., Kommu, J. V. S., Haridas, H., & Sriramalu, S. B. (2022). Intervention-based mental health training for community level workers in India -A systematic review. Journal of family medicine and primary care, 11(4), 1237–1243. https://doi.org/10.4103/jfmpc.jfmpc_1134_21 [66] | Does not describe the name of the training/intervention | Mental health education; prevention; psychological intervention skills training; psychological first aids |
| Quinnett P. G. (2023). The Certified QPR Pathfinder Training Program: A Description of a Novel Public Health Gatekeeper Training Program to Mitigate Suicidal Ideation and Suicide Deaths. Journal of prevention (2022), 44(6), 813–824. https://doi.org/10.1007/s10935-023-00748-w [56] | Pathfinder QPR Gatekeeper Training Program | Prevention; mental health education; psychological first aid |
| Reinschmidt, K. M., & Chong, J. (2005). SONRISA: a curriculum toolbox for promotores to address mental health and diabetes. Preventing chronic disease, 4(4), A101. [51] | Sonrisa | Evidence-based intervention models; roles of CMHWs in helping to prevent or manage mental health issues; mental health education; prevention. |
| Reinschmidt, K. M., Philip, T. J., Alhay, Z. A., Braxton, T., & Jennings, L. A. (2023). Training Community Health Workers to Address Disparities in Dementia Care: A Case Study From Oklahoma With National Implications. The Journal of ambulatory care management, 46(4), 272–283. https://doi.org/10.1097/JAC.0000000000000470 [57] | Dementia Training for CHW | Mental health education; training aimed at reducing health disparities |
| Robertson, M. N., DeShong, H. L., Steen, J. S., Buys, D. R., & Nadorff, M. R. (2021). Mental health first aid training for Extension agents in rural communities. Suicide & life-threatening behavior, 51(2), 301–307. https://doi.org/10.1111/sltb.12705 [67] | Mental Health First Aid (MHFA) | Mental health education; psychological first aid; psychological intervention skill training |
| Ryan, A. S., & Epstein, I. (1987). Mental health training for Southeast Asian refugee resettlement workers. International Social Work, 30(2), 185-198. https://doi.org/10.1177/002087288703000209 (Original work published 1987) [68] | Does not describe the name of the training/intervention | Mental health education; evidence-based intervention models; psychological intervention skills training; interventions for family caregivers; training aimed at reducing health disparities |
| Shields-Zeeman, L., Pathare, S., Walters, B. H., Kapadia-Kundu, N., & Joag, K. (2017). Promoting wellbeing and improving access to mental health care through community champions in rural India: the Atmiyata intervention approach. International journal of mental health systems, 11, 6. https://doi.org/10.1186/s13033-016-0113-3 [45] | Atmiyata program | Instructional techniques, psychological intervention skill training, mental health education |
| Sibeko, G., Milligan, P.D., Roelofse, M. et al. Piloting a mental health training programme for community health workers in South Africa: an exploration of changes in knowledge, confidence and attitudes. BMC Psychiatry 18, 191 (2018). https://doi.org/10.1186/s12888-018-1772-1 [49] | Does not describe the name of the training/intervention | Mental health education; prevention; psychological intervention skill training |
| Smith, M. V., & Kruse-Austin, A. (2015). A gender-informed model to train community health workers in maternal mental health. Evaluation and program planning, 51, 59–62. https://doi.org/10.1016/j.evalprogplan.2014.12.008 [13] | Does not describe the name of the training/intervention | Instructional techniques, mental health education, prevention, training aimed at reducing health disparities |
| Stacciarini, J. M., Rosa, A., Ortiz, M., Munari, D. B., Uicab, G., & Balam, M. (2012). Promotoras in mental health: a review of English, Spanish, and Portuguese literature. Family & community health, 35(2), 92–102. https://doi.org/10.1097/FCH.0b013e3182464f65 [69] | Does not describe the name of the training/intervention | Mental health education |
| Tyagi, V., Khan, A., Siddiqui, S., Kakra Abhilashi, M., Dhurve, P., Tugnawat, D., Bhan, A., & Naslund, J. A. (2023). Development of a Digital Program for Training Community Health Workers in the Detection and Referral of Schizophrenia in Rural India. The Psychiatric quarterly, 94(2), 141–163. https://doi.org/10.1007/s11126-023-10019-w [38] | The content of the digital training program was adapted from the COPSI (Community care for People with Schizophrenia in India) program manual | Instructional techniques, mental health education, prevention, training aimed at reducing stigma, training aimed at reducing health disparities |
| Weaver, A., & Lapidos, A. (2018). Mental Health Interventions with Community Health Workers in the United States: A Systematic Review. Journal of health care for the poor and underserved, 29(1), 159–180. https://doi.org/10.1353/hpu.2018.0011 [70] | Does not describe the name of the training/intervention | Mental health education; evidence-based intervention models; prevention; psychological intervention skill training |
| Wennerstrom, A., Vannoy, S. D., 3rd, Allen, C. E., Meyers, D., O’Toole, E., Wells, K. B., & Springgate, B. F. (2011). Community-based participatory development of a community health worker mental health outreach role to extend collaborative care in post-Katrina New Orleans. Ethnicity & disease, 21 (3 Suppl 1), S1–51. [12] | The REACH NOLA Mental Health Infrastructure and Training Project (MHIT) | Instructional techniques, psychological intervention skills training, mental health education, prevention, training aimed at reducing health disparities |
| Wright, J., & Chiwandira, C. (2016). Building capacity for community mental health care in rural Malawi: Findings from a district-wide task-sharing intervention with village-based health workers. The International journal of social psychiatry, 62(6), 589–596. https://doi.org/10.1177/0020764016657112 [71] | Mental Health in Zomba (MHiZ) Project | Mental health education, evidence-based intervention models, psychological first aid, prevention, psychological intervention skill training, interventions for family/caregivers, training aimed at reducing stigma, training aimed at reducing health disparities |
References
- World Health Organization, Regional Office for Europe. Mental Health: Facing the Challenges, Building Solutions: Report from the WHO European Ministerial Conference; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2005; Available online: https://iris.who.int/handle/10665/326566 (accessed on 12 June 2024).
- Ramírez, F.; Misol, R.; Bentata, L.; Alonso, M.; Campayo, J.; Franco, C.; Velázquez, S. Recomendaciones para la prevención de los trastornos de la salud mental en atención primaria. Aten. Primaria 2014, 46, 59–74. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. Depression and Other Common Mental Disorders; WHO: Geneva, Switzerland, 2017. [Google Scholar][Green Version]
- Hills, W.; Hills, K. Virtual treatments in an integrated primary care-behavioral health practice: An overview of synchronous telehealth services to address rural-urban disparities in mental health care. Med. Sci. Pulse 2019, 13, 54–59. [Google Scholar] [CrossRef]
- World Health Organization. Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings; WHO: Geneva, Switzerland, 2010; Available online: https://apps.who.int/iris/handle/10665/250239 (accessed on 17 June 2024).
- St John, B.; McDonald, L.; Stafford, A. Addressing mental health literacy in Hispanic populations. J. Health Disparities Res. Pract. 2021, 14, 45–53. [Google Scholar]
- Varas-Díaz, N.; Santos-Figueroa, A.; Polanco-Frontera, N.; Cajigas-Vargas, I.; Rivera Díaz, M.; Lugo Candelas, C.I.; Rosario-Hernández, E.; Rivera-Segarra, E. Desarrollo de una Escala para Medir el Estigma Relacionado a Problemas de Salud Mental en Puerto Rico. Rev. Puertorriqueña Psicol. 2012, 23, 107–118. [Google Scholar]
- Mugisha, J.; Abdulmalik, J.; Hanlon, C.; Petersen, I.; Lund, C.; Upadhaya, N.; Ahuja, S.; Shidhaye, R.; Mntambo, N.; Alem, A. Health systems context(s) for integrating mental health into primary health care in six Emerald countries: A situation analysis. Int. J. Ment. Health Syst. 2017, 11, 7. [Google Scholar] [CrossRef]
- Armstrong, G.; Kermode, M.; Raja, S.; Suja, S.; Chandra, P.; Jorm, A.F. A mental health training program for community health workers in India: Impact on knowledge and attitudes. Int. J. Ment. Health Syst. 2011, 5, 17. [Google Scholar] [CrossRef] [PubMed]
- American Public Health Association. Support for Community Health Workers to Increase Health Access and to Reduce Health Inequities. 2009. Available online: https://www.apha.org/policy-and-advocacy/public-health-policy-briefs/policy-database/2014/07/09/14/19/support-for-community-health-workers-to-increase-health-access-and-to-reduce-health-inequities (accessed on 20 June 2024).
- Swider, S. Outcome effectiveness of community health workers: An integrative literature review. Public Health Nurs. 2002, 19, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Wennerstrom, A.; Vannoy, S.D.; Allen, C.E.; Meyers, D.; O’Toole, E.; Wells, K.B.; Springgate, B.F. Community-based participatory development of a community health worker mental health outreach role to extend collaborative care in post-Katrina New Orleans. Ethn. Dis. 2011, 21, S1. [Google Scholar] [PubMed]
- Smith, M.V.; Kruse-Austin, A. A gender-informed model to train community health workers in maternal mental health. Eval. Program Plan. 2015, 51, 59–62. [Google Scholar] [CrossRef]
- World Health Organization. (n.d.). Global Cancer Burden Growing, Amidst Mounting Need for Services. Available online: https://www.who.int/news/item/01-02-2024-global-cancer-burden-growing--amidst-mounting-need-for-services (accessed on 20 June 2024).
- Van Iseghem, T.; Jacobs, I.; Vanden Bossche, D.; Delobelle, P.; Willems, S.; Masquillier, C.; Decat, P. The role of community health workers in primary healthcare in the WHO-EU region: A scoping review. Int. J. Equity Health 2023, 22, 134. [Google Scholar] [CrossRef]
- Mistry, S.K.; Harris, E.; Harris, M. Community Health Workers as Healthcare Navigators in Primary Care Chronic Disease Management: A Systematic Review. J. Gen. Intern. Med. 2021, 36, 2755–2771. [Google Scholar] [CrossRef]
- Cummings, D.M.; Lutes, L.D.; Littlewood, K.; DiNatale, E.; Hambidge, B.; Schulman, K. EMPOWER: A randomized trial using community health workers to deliver a lifestyle intervention program in African American women with Type 2 diabetes: Design, rationale, and baseline characteristics. Contemp. Clin. Trials 2013, 36, 147–153. [Google Scholar] [CrossRef]
- Wells, K.B.; Sherbourne, C.D.; Miranda, J.; Tang, L.; Benjamin, B.; Duan, N. The cumulative effects of quality improvement for depression on outcome disparities over 9 years: Results from a randomized, controlled group-level trial. Med. Care 2007, 45, 1052–1059. [Google Scholar] [CrossRef]
- Andrews, J.O.; Felton, G.; Wewers, M.E.; Heath, J. Use of community health workers in research with ethnic minority women. J. Nurs. Scholarsh. 2004, 36, 358–365. [Google Scholar] [CrossRef]
- West Rasmus, E.K.; Pineda-Reyes, F.; Tamez, M.; Westfall, J.M. Promotores de salud and community health workers: An annotated bibliography. Fam. Community Health 2012, 35, 172–182. [Google Scholar] [CrossRef] [PubMed]
- Götze, H.; Taubenheim, S.; Dietz, A.; Lordick, F.; Mehnert, A. Comorbid conditions and health-related quality of life in long-term cancer survivors-associations with demographic and medical characteristics. J. Cancer Surviv. Res. Pract. 2018, 12, 712–720. [Google Scholar] [CrossRef] [PubMed]
- Shahid, S.; Teng, T.H.; Bessarab, D.; Aoun, S.; Baxi, S.; Thompson, S.C. Factors contributing to delayed diagnosis of cancer among Aboriginal people in Australia: A qualitative study. BMJ Open 2016, 6, e010909. [Google Scholar] [CrossRef] [PubMed]
- Carreira, H.; Williams, R.; Müller, M.; Harewood, R.; Stanway, S.; Bhaskaran, K. Associations between breast cancer survivorship and adverse mental health outcomes: A systematic review. J. Natl. Cancer Inst. 2018, 110, 1311–1327. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, T.R.; Wang, X.S.; Cleeland, C.S. The impact of cancer-related symptoms on patient outcomes. Cancer 2021, 127, 448–456. [Google Scholar]
- Ashing-Giwa, K.T.; Padilla, G.; Tejero, J.; Kim, J. Cancer survivorship and quality of life: A qualitative study of African American cancer survivors. Oncol. Nurs. Forum 2022, 49, 68–77. [Google Scholar]
- Nguyen, T.-U.N.; Tran, J.H.; Kagawa-Singer, M.; Foo, M.A. A qualitative assessment of community-based breast health navigation services for Southeast Asian women in Southern California: Recommendations for developing a navigator training curriculum. Am. J. Public Health 2011, 101, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.I.; Kapphahn, K.; Dewland, M.; Aguilar, V.; Sanchez, B.; Sisay, E.; Murillo, A.; Smith, K.; Park, D.J. Effect of a Community Health Worker Intervention on Acute Care Use, Advance Care Planning, and Patient-Reported Outcomes Among Adults with Advanced Stages of Cancer: A Randomized Clinical Trial. JAMA Oncol. 2022, 8, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Kelley, S.F.; DeCourtney, C.; Owens, X. Behavioral Health Aides in Rural Alaska: Their Experience in Caring for Alaska Native Cancer Survivors. J. Cancer Educ. 2014, 29, 642–648. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.N.; Matthew, R.A.; Orpinas, P. Design, implementation, and evaluation of community health worker training programs in Latinx communities: A scoping review. J. Community Psychol. 2023, 51, 382–405. [Google Scholar] [CrossRef] [PubMed]
- Stanley, D.; Marshall, Z.; Lazarus, L.; LeBlanc, S.; Heighton, T.; Preater, B.; Tyndall, M. Harnessing the power of community-based participatory research: Examining knowledge, action, and consciousness in the PROUD study. Soc. Work Public Health 2015, 30, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Muke, S.S.; Shrivastava, R.D.; Mitchell, L.; Khan, A.; Murhar, V.; Tugnawat, D.; Shidhaye, R.; Patel, V.; Naslund, J.A. Acceptability and feasibility of digital technology for training community health workers to deliver brief psychological treatment for depression in rural India. Asian J. Psychiatry 2019, 45, 99–106. [Google Scholar] [CrossRef]
- Utilidad y tipos de revisión de literatura Usefulness and types of literature review. Available online: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1988-348X2015000200002&lng=en (accessed on 17 June 2024).
- Hernández Sampieri, R.; Fernández Collado, C.; Baptista Lucio, P. Fundamentos de Metodología de la Investigación, 4th ed.; McGraw-Hill: New York, NY, USA, 2006. [Google Scholar]
- Chiumento, A.; Hamdani, S.U.; Khan, M.N.; Dawson, K.; Bryant, R.A.; Sijbrandij, M.; Rahman, A. Evaluating effectiveness and cost-effectiveness of a group psychological intervention using cognitive behavioral strategies for women with common mental disorders in conflict-affected rural Pakistan: Study protocol for a randomized controlled trial. Trials 2017, 18, 190. [Google Scholar] [CrossRef]
- Gormley, M.; Loughran, C.; Conte, J.; Navarra, A.M.D. Trends in US HIV peer health worker training strategies and approaches: A scoping review of the literature. J. Assoc. Nurses AIDS Care 2023, 34, 331–348. [Google Scholar] [CrossRef]
- Islam, N.S.; Zanowiak, J.M.; Wyatt, L.C.; Chun, K.; Lee, L.; Kwon, S.C.; Trinh-Shevrin, C. A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J. Community Health 2013, 38, 1030–1041. [Google Scholar] [CrossRef]
- Cruz-Correa, M.; Cordero, F.; Betancourt, J.P.; Diaz-Algorri, Y.; Lopez, S.M.; Rivera, M.; Rodriguez-Quilichini, S. Implementation and outcomes of a community-based educational program for colorectal cancer prevention in Hispanics. J. Fam. Med. Dis. Prev. 2016, 2, 42. [Google Scholar] [CrossRef]
- Tyagi, V.; Khan, A.; Siddiqui, S.; Kakra Abhilashi, M.; Dhurve, P.; Tugnawat, D.; Bhan, A.; Naslund, J.A. Development of a digital program for training community health workers in the detection and referral of schizophrenia in rural India. Psychiatr. Q. 2023, 94, 141–163. [Google Scholar] [CrossRef]
- Springgate, B.F.; Wennerstrom, A.; Meyers, D.; Allen, C.E., III; Vannoy, S.D.; Bentham, W.; Wells, K.B. Building community resilience through mental health infrastructure and training in post-Katrina New Orleans. Ethn. Dis. 2011, 21 (Suppl. S1), S1–S29. [Google Scholar]
- Uriarte, J.A.; Cummings, A.D.; Lloyd, L.E. An instructional design model for culturally competent community health worker training. Health Promot. Pract. 2014, 15 (Suppl. S1), 56S–63S. [Google Scholar] [CrossRef] [PubMed]
- Moore-Monroy, M.; Wilkinson-Lee, A.M.; Verdugo, L.; Lopez, E.; Paez, L.; Rodriguez, D.; Wilhelm, M.; Garcia, F. Addressing the information gap: Developing and implementing a cervical cancer prevention education campaign grounded in principles of community-based participatory action. Health Promot. Pract. 2013, 14, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Edelblute, H.B.; Clark, S.; Mann, L.; McKenney, K.M.; Bischof, J.J.; Kistler, C. Promotoras across the border: A pilot study addressing depression in Mexican women impacted by migration. J. Immigr. Minor. Health 2014, 16, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Glenberg, A.M.; Langston, W.E. Comprehension of illustrated texts: Pictures help to build mental models. J. Mem. Lang. 1992, 31, 129–151. [Google Scholar] [CrossRef]
- Malla, A.; Margoob, M.; Iyer, S.; Joober, R.; Lal, S.; Thara, R.; Mushtaq, H.; Mansouri, B.I. A model of mental health care involving trained lay health workers for treatment of major mental disorders among youth in a conflict-ridden, low-middle income environment: Part I adaptation and implementation. Can. J. Psychiatry 2019, 64, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Shields-Zeeman, L.; Pathare, S.; Walters, B.H.; Kapadia-Kundu, N.; Joag, K. Promoting wellbeing and improving access to mental health care through community champions in rural India: The Atmiyata intervention approach. Int. J. Ment. Health Syst. 2017, 11, 6. [Google Scholar] [CrossRef]
- Monton, O.; Abou-Zamzam, A.; Fuller, S.; Barnes-Malone, T.; Siddiqi, A.; Woods, A.; Patton, J.; Ibe, C.A.; Johnston, F.M. Palliative Care Curriculum and Training Plan for community health workers. BMJ Support. Palliat. Care 2023, 14, e2972–e2976. [Google Scholar] [CrossRef]
- Bordeaux-Rank, J.A. Tribal Participatory Research with Community-Based Psychological First Aid Training of Trainers on the Rosebud: A Follow-Up Study. Ph.D. Thesis, University of South Dakota, Sioux Falls, SD, USA, 2017. [Google Scholar]
- Chaudhary, A.; Dosto, N.; Hill, R.; Lehmijoki-Gardner, M.; Sharp, P.; Daniel Hale, W.; Galiatsatos, P. Community intervention for Syrian refugees in Baltimore City: The Lay Health Educator Program at a local mosque. J. Relig. Health 2019, 58, 1687–1697. [Google Scholar] [CrossRef]
- Sibeko, G.; Milligan, P.D.; Roelofse, M.; Molefe, L.; Jonker, D.; Ipser, J.; Stein, D.J. Piloting a mental health training programme for community health workers in South Africa: An exploration of changes in knowledge, confidence and attitudes. BMC Psychiatry 2018, 18, 191. [Google Scholar] [CrossRef] [PubMed]
- Abadi, M.H.; Drake, C.; Richard, B.O.; Schweinhart, A.; Rychener, D.; Shamblen, S.R.; Grimsgaard, S.N. An evaluation of the facilitator training to implement ‘Taking charge of my life and health’, a peer-led group program to promote self-care and patient empowerment in Veteran participants. Patient Educ. Couns. 2020, 103, 2489–2498. [Google Scholar] [CrossRef]
- Reinschmidt, K.M.; Chong, J. SONRISA: A curriculum toolbox for promotores/community health workers to address mental/emotional health issues associated with diabetes. Prev. Chronic Dis. 2005, 4, A101. [Google Scholar]
- Rodriguez-Rabassa, M.; Hernandez, R.; Rodriguez, Z.; Colon-Echevarria, C.B.; Maldonado, L.; Tollinchi, N.; Torres-Marrero, E.; Mulero, A.; Albors, D.; Perez-Morales, J.; et al. Impact of a natural disaster on access to care and biopsychosocial outcomes among Hispanic/Latino cancer survivors. Sci. Rep. 2020, 10, 10376. [Google Scholar] [CrossRef] [PubMed]
- Community-Based Mental Health (CBMH). Training Guide; IFRC Reference Centre for Psychosocial Support: Copenhagen, Denmark, 2023. [Google Scholar]
- Castro-Figueroa, E.M.; Torres-Blasco, N.; Rodriguez-Subašić, W.C.; Padilla, N.; Toro-Morales, Y.; Beauchamp, A.; González, K.; Costas-Muñiz, R. A Holistic and Community-Based Service Program Promoting Mental Health among Latina Breast Cancer Survivors and Informal Caregivers. J. Health Care Poor Underserved 2023, 34, 823–832. [Google Scholar] [CrossRef] [PubMed]
- Nápoles, A.M.; Santoyo-Olsson, J.; Stewart, A.L.; Ortiz, C.; Samayoa, C.; Torres-Nguyen, A.; Palomino, H.; Coleman, L.; Urias, A.; Gonzalez, N.; et al. Nuevo Amanecer-II: Results of a randomized controlled trial of a community-based participatory, peer-delivered stress management intervention for rural Latina breast cancer survivors. Psycho-Oncol. 2020, 29, 1802–1814. [Google Scholar] [CrossRef] [PubMed]
- Quinnett, P.G. The certified QPR pathfinder training program: A description of a novel public health gatekeeper training program to mitigate suicidal ideation and suicide deaths. J. Prev. 2023, 44, 813–824. [Google Scholar] [CrossRef]
- Reinschmidt, K.M.; Philip, T.J.; Alhay, Z.A.; Braxton, T.; Jennings, L.A. Training Community Health Workers to Address Disparities in Dementia Care: A Case Study from Oklahoma with National Implications. The Journal of Ambulatory Care Management. J. Ambul. Care Manag. 2023, 46, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Zillmer, J.G.V.; Díaz-Medina, B.A. Revisión Narrativa: Elementos que la constituyen y sus potencialidades. J. Nurs. Health 2018, 8, e188101. [Google Scholar] [CrossRef]
- Instituto Nacional del Cáncer (NIH). Estadísticas Sobre el Cáncer. 2024. Available online: https://www.cancer.gov/espanol/cancer/naturaleza/estadisticas (accessed on 24 December 2024).
- Andreae, S.J.; Andreae, L.J.; Cherrington, A.L.; Lewis, M.; Johnson, E.; Clark, D.; Safford, M.M. Development of a Community Health Worker–Delivered Cognitive Behavioral Training Intervention for Individuals with Diabetes and Chronic Pain. Fam. Community Health 2018, 41, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Cheffi, A.; Harrison, S. Community-Based Mental Health: A Training Guide for Community Providers. IFRC Reference Centre for Psychosocial Support. 2023. Available online: https://mhpsshub.org/resource/community-based-mental-health-a-training-guide-for-community-provider (accessed on 17 June 2024).
- Hofmann-Broussard, C.; Armstrong, G.; Boschen, M.J.; Somasundaram, K.V. A mental health training program for community health workers in India: Impact on recognition of mental disorders, stigmatizing attitudes and confidence. Int. J. Cult. Ment. Health 2017, 10, 62–74. [Google Scholar] [CrossRef]
- Hossain, D.; Gorman, D.; Eley, R.; Coutts, J. Farm Advisors’ reflections on Mental Health First Aid training. Aust. E-J. Adv. Ment. Health 2009, 8, 105–111. [Google Scholar] [CrossRef]
- McCabe, O.L.; Marum, F.; Mosley, A.; Gwon, H.S.; Langlieb, A.; Everly, G.S.; Kaminsky, M.J., Jr.; Links, J.M. Community capacity-building in disaster mental health resilience: A pilot study of an academic/faith partnership model. International Journal of Emerg. Ment. Health 2012, 14, 112–122. [Google Scholar]
- Michael, A.; Thirumoorthy, A.; Girish, N.; Sivakumar, P.T. Training Community health workers in geriatric mental health: Process of manual development and pilot testing findings. Asian J. Psychiatry 2018, 38, 12–15. [Google Scholar]
- Paramasivam, R.; Elangovan, A.R.; Amudhan, S.; Kommu, J.V.S.; Haridas, H.; Sriramalu, S.B. Intervention-based mental health training for community level workers in India—A systematic review. J. Fam. Med. Prim. Care 2022, 11, 1237–1243. [Google Scholar]
- Robertson, M.N.; DeShong, H.L.; Steen, J.K.S.; Buys, D.R.; Nadorff, M.R. Mental health first aid training for Extension agents in rural communities. Suicide Life-Threat. Behav. 2021, 51, 301–307. [Google Scholar] [CrossRef]
- Ryan, A.S.; Epstein, I. Mental health training for Southeast Asian refugee resettlement workers. Int. Soc. Work. 1987, 30, 185–198. [Google Scholar] [CrossRef]
- Stacciarini, J.M.R.; Rosa, A.; Ortiz, M.; Munari, D.B.; Uicab, G.; Balam, M. Promotoras in mental health: A review of English, Spanish, and Portuguese literature. Fam. Community Health 2012, 35, 92–102. [Google Scholar]
- Weaver, A.; Lapidos, A. Mental health interventions with community health workers in the United States: A systematic review. J. Health Care Poor Underserved 2018, 29, 159–180. [Google Scholar] [CrossRef]
- Wright, J.; Chiwandira, C. Building capacity for community mental health care in rural Malawi: Findings from a district-wide task-sharing intervention with village-based health workers. Int. J. Soc. Psychiatry 2016, 62, 589–596. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).