Modeling the Impact of Tele-Health on Accessibility and Equity of Medical Resources in Metropolitan Cities in China
Abstract
1. Introduction
2. Methods
2.1. Data
2.2. Model Assumptions
- Assumption 1: Patients’ offline access to medical resources is mainly influenced by distance, i.e., the transportation time to the hospitals. This assumption can be observed among many elderly patients with chronic diseases, and has been justified in [21] from a large-scale analysis on accessibility to medical facilities in China.
- Assumption 2: Offline treatment for chronic diseases is provided by community hospitals, with some cases being referred to tertiary A hospitals. Online consultations are offered by tertiary A hospitals. This assumption is aligned with the standard introduced in [22] for the service objective of community hospitals.
- Assumption 3: Medical resources are quantified by the consultation time of physicians. Each physician has a fixed daily working time, and the proportion allocated to online consultations cannot exceed a given limit. The proportion of physicians specializing in chronic diseases is the same across all hospitals. A monograph [23] explicitly considers the physicians’ working hours (such as consultations/hour) as a key input variable for medical service production, which justifies the assumption.
- Assumption 4: The residents’ tendency to seek online treatment is divided into two types according to the offline access to medical resources in the district, namely, the district with good and poor access to offline medical treatment. It has been observed that patients living in areas with good accessibility to offline medical services are more likely to choose offline visits, while those living in areas with poor accessibility to offline medical services are more inclined to use online medical services.
2.3. Analysis Model
- Step 1: The area of concern for a physician in hospital j is defined as the region that encompasses all residential divisions k within a traveling distance threshold from hospital j, where superscript is used to denote tertiary A hospitals (mainly for acute diseases) and community hospitals (typically for chronic diseases). The physician-to-population ratio at location j, defined as , is calculated aswhere is the numbers of physicians in hospital j, and is the population of residential division k, and is the distance between the hospital and the residential division.
- Step 2: For residential division k, the hospitals within the travel time threshold are identified, and the physician-to-population ratio in these hospitals are summed together to obtain .By performing an identity transformation, we obtain the accessibility measure for division k to hospital type x.where H and P are the numbers of hospitals and residential divisions, respectively. is a function of traveling distance . For chronic disease, most elderly patients are sensitive to the distances between their residential divisions and community hospitals; i.e., their willingness to visit medical facilities is decreasing with respect to longer distance. Thus, a distance-based decaying function can be introduced aswhere, according to [28,29], for Chinese cities, is suitable.
- Step 3: For some patients with chronic diseases, after visiting community hospitals, they may need additional visits and treatment at tertiary A hospitals through the hierarchical referral system. To characterize this, a referral rate r is introduced to indicate the proportion of patients making additional visit to tertiary A hospitals so that is replaced by a more comprehensive accessibility measure including referrals, as follows:where the first part characterizes the patients staying in community hospitals without referring, and the second part is for those being referred to tertiary A hospitals. Here, L denotes the number of tertiary A hospitals, and represents the medical resource in tertiary A hospital i.
- Step 4: To address online visits, the accessibility model considers patients with chronic diseases who prefer to seek online healthcare services. Note that, for internet-based service, geographical distance ceases to be a determining factor. Consequently, can be treated as a constant for all patients, effectively eliminating this variable from consideration, as follows:where superscript v denotes online visits, represents the online consultation preference from residents with chronic diseases in division k, and indicates the medical resource in tertiary A hospital i dedicated to online services.
2.4. Optimization Model
3. Results
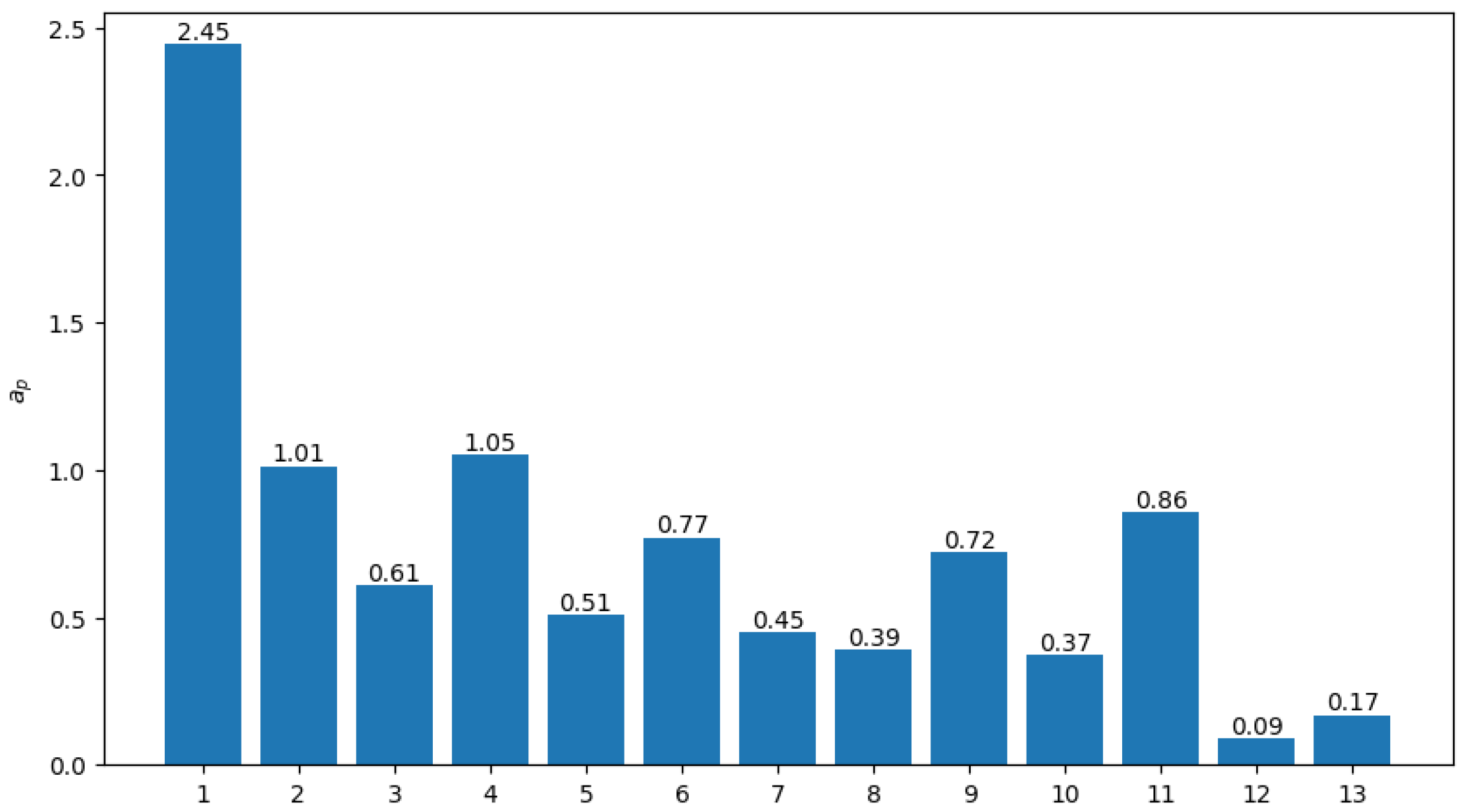
3.1. Accessibility Assessment
3.2. Optimization Analysis
4. Discussion
4.1. Benefits and Potentials
4.2. Barriers and Difficulties
4.3. Limitations and Extensions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 2SFCA | two-step floating catchment area |
| i2SFCA-TH | improved two-step floating catchment area method with tele-health |
| EHR | electronic health record |
References
- National Bureau of Statistics of China. Communique of the Seventh National Population Census (No. 8); National Bureau of Statistics of China: Beijing, China, 2021.
- Zhang, H. Beijing Now a Moderately Aging Society, to Become Severely Aging by 2035. Global Times, 2 September 2022. [Google Scholar]
- Textor, C. Age Distribution of the Population in Shanghai, China 2015–2023. 2024. Available online: https://www.statista.com/statistics/1130402/china-shanghai-population-distribution-by-broad-age-group/ (accessed on 17 August 2025).
- Park, J.; Goldberg, D.W. A Review of Recent Spatial Accessibility Studies That Benefitted from Advanced Geospatial Information: Multimodal Transportation and Spatiotemporal Disaggregation. ISPRS Int. J. Geo-Inf. 2021, 10, 532. [Google Scholar] [CrossRef]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Wang, F. Measurement, Optimization, and Impact of Health Care Accessibility: A Methodological Review. Ann. Assoc. Am. Geogr. 2012, 102, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Tao, Z.; Cheng, Y.; Liu, J. Hierarchical two-step floating catchment area (2SFCA) method: Measuring the spatial accessibility to hierarchical healthcare facilities in Shenzhen, China. Int. J. Equity Health 2020, 19, 164. [Google Scholar] [CrossRef] [PubMed]
- Langford, M.; Higgs, G.; Fry, R. Multi-modal two-step floating catchment area analysis of primary health care accessibility. Health Place 2016, 38, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Spatial accessibility to primary care and physician shortage area designation: A case study in Illinois with GIS approaches. In Geographic Information Systems and Health Applications; IGI Global: Hershey, PA, USA, 2003; pp. 261–279. [Google Scholar]
- Delamater, P.L. Spatial accessibility in suboptimally configured health care systems: A modified two-step floating catchment area (M2SFCA) metric. Health Place 2013, 24, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Dai, D.; Wang, F. Geographic disparities in accessibility to food stores in southwest Mississippi. Environ. Plan. B Plan. Des. 2011, 38, 659–677. [Google Scholar] [CrossRef]
- McGrail, M.R.; Humphreys, J.S. Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Appl. Geogr. 2014, 54, 182–188. [Google Scholar] [CrossRef]
- Neutens, T. Accessibility, equity and health care: Review and research directions for transport geographers. J. Transp. Geogr. 2015, 43, 14–27. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Outline of the Healthy China 2030 Plan; National Health Commission of the People’s Republic of China: Beijing, China, 2016.
- Liu, D.; Sun, Y. The Impact of “Internet Plus Healthcare” on the Traditional Healthcare Industry. Chin. J. Res. Hosp. 2017, 4, 7–11. [Google Scholar]
- Thaker, D.A.; Monypenny, R.; Olver, I.; Sabesan, S. Cost savings from a telemedicine model of care in northern Queensland, Australia. Med. J. Aust. 2013, 199, 414–417. [Google Scholar] [CrossRef] [PubMed]
- LeRouge, C.M.; Garfield, M.J.; Hevner, A.R. Patient perspectives of telemedicine quality. Patient Prefer. Adherence 2014, 2015, 25–40. [Google Scholar] [CrossRef] [PubMed]
- General Office of the State Council. Guiding Opinions on Promoting High-Quality Development of Public Hospitals; General Office of the State Council: Beijing, China, 2021. [Google Scholar]
- Ma, N.; Qiu, Y.; Wei, G. Practice and Analysis of Internet Healthcare Promoting Changes in Diagnosis and Treatment Models. Chin. J. Hosp. Adm. 2020, 36, 726–729. [Google Scholar]
- Tangshan Municiple People’s Government. Statistics Yearbook of Tangshan 2023; Tangshan Municiple People’s Government: Tangshan, China, 2024.
- Yin, C.; He, Q.; Liu, Y.; Chen, W.; Gao, Y. Inequality of public health and its role in spatial accessibility to medical facilities in China. Appl. Geogr. 2018, 92, 50–62. [Google Scholar] [CrossRef]
- The General Office of the National Health Commission. Issues the Basic Standards for Community Hospitals Notice on the Key Points of the Core System for Medical Quality and Safety (Trial); The General Office of the National Health Commission: Beijing, China, 2019.
- Folland, S.; Goodman, A.C.; Stano, M.; Danagoulian, S. The Economics of Health and Health Care; Routledge: London, UK, 2024. [Google Scholar]
- Berndt, D.J.; Fisher, J.W.; Rajendrababu, R.V.; Studnicki, J. Measuring healthcare inequities using the Gini index. In Proceedings of the 36th Hawaii International Conference on System Sciences–2003 Measuring Healthcare Inequities using the Gini Index, Big Island, HI, USA, 6–9 January 2003. [Google Scholar]
- Liao, Z. The Analysis of Basic Public Service Supply Regional Equalization in China’s Provinces—Based on the Theil Index Evaluation. IOP Conf. Ser. Earth Environ. Sci. 2017, 100, 012106. [Google Scholar] [CrossRef]
- Witthayapipopsaku, W.; Cetthakriku, N.; Suphanchaimat, R.; Noree, T.; Sawaengdee, K. Equity of health workforce distribution in Thailand: An implication of concentration index. Risk Manag. Healthc. Policy 2019, 14, 13–22. [Google Scholar] [CrossRef] [PubMed]
- San Sebastian, M.; Mosquera, P.; Ng, N.; Gustafsson, P. Health care on equal terms? Assessing horizontal equity in health care use in Northern Sweden. Eur. J. Public Health 2017, 27, 637–643. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Chen, W. Measuring Spatial Accessibility to Health Care Facilities Based on Potential Model. Prog. Geogr. 2009, 28, 848. [Google Scholar]
- Yue, J. Research on Evaluation and Optimization Model of Urban Medical Resource Allocation from Spatial Perspective. Ph.D. Dissertation, Huazhong University of Science and Technology, Wuhan, China, 2021. [Google Scholar]
- Gini, C. Variabilita e Mutabilita; C. Cuppini: Cambridge, MA, USA, 1912. [Google Scholar]
- Ni, Z.J.; Qian, Y. Research on the evolutionof public attitudes towards telemedicine in China—Multi-period analysis of Weibo text data. Oper. Res. Fuzzy Syst. 2024, 14, 466–477. [Google Scholar]
- China Internet Network Information Center (CNNIC). The 53rd Statistical Report on China’s Internet Development; China Internet Network Information Center (CNNIC): Beijing, China, 2024. [Google Scholar]
- Deloitte. Internet Hospitals in China: The New Step into Digital Healthcare; Deloitte: London, UK, 2024. [Google Scholar]
- Rongxu-Boyi Program. 2022 China E-Hospital Development Research Report; Shanghai Jiaotong University: Shanghai, China, 2022. [Google Scholar]
- Zhang, X.; Liu, R.; Huang, E.; Hu, X.; Zhang, H.; Han, T.; He, S.; Tu, W.; Xu, R.; Chen, Z.; et al. E-Health High Quality Development Research Report; Eight Clock Health News, Jianwen Group: Shanghai, China, 2023. [Google Scholar]
- Beijing Municipal Bureau of Statistics, Survey Office of the National Bureau of Statistics in Beijing. 2022 Survey Report on Usability and Attitude to Smart Phones Among Elderly People; Beijing Municipal Bureau of Statistics, Survey Office of the National Bureau of Statistics in Beijing: Beijing, China, 2022.
- Khan, M.; Mehran, M.T.; Haq, Z.U.; Ullah, Z.; Naqvi, S.R.; Ihsan, M.; Abbass, H. Applications of artificial intelligence in COVID-19 pandemic: A comprehensive review. Expert Syst. Appl. 2021, 185, 115695. [Google Scholar] [CrossRef] [PubMed]
- Postigo, A. Regulatory Barriers in Implementing Digital Health Interventions; ARTNeT Working Paper Series No. 231; ESCAP: Bangkok, Thailand, 2023. [Google Scholar]


| Division # | Residents ≥ 60 | Residents with Chronic Diseases |
|---|---|---|
| 1 | 9126 | 1061 |
| 2 | 13,301 | 3285 |
| 3 | 16,786 | 3463 |
| 4 | 676 | 146 |
| 5 | 12,190 | 2288 |
| 6 | 15,535 | 5820 |
| 7 | 8251 | 4190 |
| 8 | 10,680 | 4394 |
| 9 | 18,283 | 4074 |
| 10 | 22,544 | 6070 |
| 11 | 26,678 | 6762 |
| 12 | 847 | 3731 |
| 13 | 16,479 | 9349 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Weng, L.; Li, J. Modeling the Impact of Tele-Health on Accessibility and Equity of Medical Resources in Metropolitan Cities in China. Healthcare 2025, 13, 2105. https://doi.org/10.3390/healthcare13172105
Wang Q, Weng L, Li J. Modeling the Impact of Tele-Health on Accessibility and Equity of Medical Resources in Metropolitan Cities in China. Healthcare. 2025; 13(17):2105. https://doi.org/10.3390/healthcare13172105
Chicago/Turabian StyleWang, Qing, Leqi Weng, and Jingshan Li. 2025. "Modeling the Impact of Tele-Health on Accessibility and Equity of Medical Resources in Metropolitan Cities in China" Healthcare 13, no. 17: 2105. https://doi.org/10.3390/healthcare13172105
APA StyleWang, Q., Weng, L., & Li, J. (2025). Modeling the Impact of Tele-Health on Accessibility and Equity of Medical Resources in Metropolitan Cities in China. Healthcare, 13(17), 2105. https://doi.org/10.3390/healthcare13172105





