Abstract
Background: Although improving the patient experience with care is being framed as part of value-based care, the economic and provider well-being impact of interventions for improving the patient experience has not been established. We aimed to synthesize the contemporary (2015–2024) empirical literature on the economic (e.g., costs, revenue) and other value-based impacts (e.g., provider well-being) of patient-experience improvement interventions. Methods: Systematic review using six databases of scientific literature (PubMed, EconLit, CINAHL, PsycINFO, DOAJ, and Scopus) supplemented by journal-specific and snowball searches following a registered study protocol (PROSPERO: CRD42022358337). Two independent reviewers performed eligibility decisions and quality appraisals of the study methods and economic assessments, when applicable; the latter was conducted using the Joanna Briggs Institute’s checklist for economic evaluations. Results: Out of 1317 unique references, nine were included. Four studies assessed the effectiveness of patient experience improvement interventions (e.g., provider communication training, discharge or transitional support) coupled with economic evaluations; these found statistically significant positive outcomes for both patient experience and economic dimensions—including reduced costs, improved revenue, or additional costs offset by increased revenue. Three additional studies on provider communication training also found statistically significant positive impacts on provider well-being (i.e., reduced burnout) and patient experience improvements. Conclusion: These findings shed light on the overall synergistic value of and business case for investments into developing patient experience improvement programs or activities. However, there is room for strengthening this body of knowledge in scope, volume, and method quality, including the need to study the impact on patient experience, provider well-being, health outcomes, and costs (i.e., the quadruple aim) in tandem.
1. Introduction
Patient experience encompasses a spectrum of valuable patient interactions within the healthcare system, such as easy access to information, timely appointments, and effective communication with healthcare providers [1]. A recent systematic review correlated improved patient experiences with better self-reported outcomes and reduced healthcare utilization [2]. Therefore, monitoring and enhancing patient experience, alongside other quality indicators, is crucial for advancing healthcare quality and value. To facilitate the monitoring of patient experience, the US Agency for Healthcare Research and Quality has established the Consumer Assessment of Healthcare Providers and Systems (CAHPS) program [3]. The CAHPS offers standardized patient experience measures, enabling routine monitoring and performance comparisons across providers. Of note, patient experience measures (or patient-reported experience measures) focus on how the patient experiences the service and care they receive, which conceptually differs from patient-reported outcome measures, which refer to any report that comes directly from the patient about their health condition, without interpretation by a clinician or anyone else [4,5]. Furthermore, patient experience measures conceptually differ from patient satisfaction measures, as the former rely on observable, modifiable aspects of care, while the latter are more subjective and influenced by patient expectations—hence with lower value for both quality assessment and improvement [6]. The routine use of the CAHPS or other patient experience measures can influence consumer choice and encourage quality improvement. For example, the Centers for Medicare & Medicaid Services (CMS) use CAHPS measures for case-mix adjusted public reporting of patient experience ratings, aligning with other quality indicators [7]. Furthermore, the CMS’s Hospital Value-Based Purchasing (VBP) Program, initiated in 2013, incorporates value-based incentives, including CAHPS-measured patient experience performance, to reward providers for key quality indicators [8].
Following value-based incentives and responding to market pressures such as customer loyalty, public reporting of patient experience data, online reviews, and social media accounts [9], healthcare systems and providers are actively striving to enhance their patient experience performance. To achieve this goal, healthcare organizations have various options. These include investments in patient experience improvement programs, engaging in quality improvement activities (e.g., in-service communication training [10]), and implementing new structures, such as patient experience offices [11], to support these improvement programs.
This review is developed from the standpoint that improving patient experience can lead to a return on investment. For example, improvements may lead to enhanced incentive payments under a value-based purchasing program and increased patient volume due to factors such as consumer loyalty, positive word-of-mouth marketing, or favorable online reviews [11,12]. In addition to potential financial returns, initiatives to enhance patient experience can positively impact provider engagement and well-being [13,14].
Viewing healthcare through the lens of relationship-centered care, which recognizes the interdependence of patient–provider interactions [15,16], suggests that organizations fostering initiatives to improve patient experience may also elevate staff engagement, joy at work, and overall clinician well-being. If so, this contributes to the quadruple aim, which incorporates patient experience, cost, and provider experience alongside population health outcomes among the goals for quality improvement [17,18]. Furthermore, organizational initiatives emphasizing person-centered tenets can promote staff engagement and activation [19], reinforce a climate of compassionate and relational care, and ultimately improve provider well-being and staff retention [20,21].
However, the value of patient experience improvement activities has not been definitively established or systematically synthesized. While there are systematic reviews that aimed to link patient experiences to clinical safety and improved patient outcomes [2,22], there is a gap in the literature concerning the economic impact of patient experience improvement activities as well as the impact on provider well-being or other value-based outcomes.
We aimed to synthesize the contemporary (2015–2024) empirical literature on the economic (e.g., costs, revenue) and other value-based impacts (e.g., provider well-being) of patient experience improvement interventions. These findings aim to inform healthcare administrators about the potential supplementary value from investments in patient experience improvement activities.
2. Materials and Methods
2.1. Design
This study refers to a systematic review whose protocol was registered in the PROSPERO database (CRD42022358337). While this systematic review protocol focuses on both the effectiveness and value of health service interventions targeting improvements in patient experience, the systematic review described in this paper focuses on the value-based component. Reporting follows the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [23].
2.2. Eligibility Criteria
Our review addresses two key questions:
- (1)
- What is the economic impact on healthcare organizations of patient experience improvement interventions?
- (2)
- Are there additional value-based impacts, such as improved provider well-being/burnout or reduced healthcare utilization, arising from these interventions?
To answer both review questions, we included empirical studies (e.g., controlled experiments, longitudinal observational studies on the impact of a program/intervention, pre–post test designs) of all activities (e.g., service delivery and other in-service improvement interventions) targeting improvements in patient experience that also reported financial components or other value-based outcomes (e.g., burnout, readmission rates, healthcare utilization). For patient experience data (i.e., study outcomes), we included studies that used standardized patient experience assessments, including validated surveys or surveys that were externally collected and routinely used across providers, including for value-based reimbursement. We excluded studies that did not (1) use standardized measures or inferential statistics for evaluating the patient experience outcomes or (2) report any additional value-based outcomes (e.g., burnout-related healthcare utilization) or financial/economic outcomes (e.g., return on investment). For participants, we included health systems, organizations, providers, networks, settings, or service units, including any health professionals or staff. We excluded health service interventions exclusively delivered by students or clinicians-in-training. Those providing patient experience feedback could be the patient, family/informal caregivers, or any proxy respondents on the patient’s behalf. There were no limits placed on healthcare settings, geography, or health conditions. In addition, we had no requirement for a comparator (i.e., we included studies with inferential pre–post analysis). As planned in the protocol, we excluded studies not reported in English and those published before 2015, as we looked for contemporary evidence accessible to an international readership. Altogether, we covered the time period from 2015 through to 2024.
2.3. Search Process
Six scientific literature databases (PubMed/Medline, EconLit, CINAHL, PsycINFO, DOAJ, and Scopus) were searched using a combination of free-text words with indexed terms. We used terms for patient experience or terms related to methods of collecting or improving those experiences (e.g., experience-based codesign, experience rounding). These keywords were combined with a broad set of keywords on health service management and improvement approaches. No restriction was applied to country or health service type. The most recent search was updated until December 2024. Supplementary Table S1 provides details about the complete search.
The databases searches were complemented by targeted searches within specific peer-reviewed journals with a track record of publishing on patient experience activities. These journals include Patient Experience Journal, Journal of Patient Experience, Medical Care, and Health Expectations. NEJM Catalyst Innovations in Care Delivery was also searched for publications since January 2020, when the journal became peer-reviewed. Finally, we applied snowball strategies (e.g., author tracking, citation tracking) using the final included articles and any related systematic or scoping reviews, including those identified through the initial searches.
2.4. Selection of Papers and Data Extraction
Two independent reviewers were used for title-and-abstract screening and full-text selection; two rounds of discussion among the reviewers were sufficient to achieve agreement. The research team constructed a tailored data extraction table, which included data on (a) study characteristics (e.g., study design, objective, country, settings, measures used, analytic approaches), (b) interventions used and their impact on patient experience scores, (c) any economic analyses and their findings (i.e., on financial variables or indicators assessed, sources of these data, economic analysis type and methods used, and the results of these analyses), and (d) any additional analyses and findings on provider well-being/burnout or quality-of-care outcomes. Data extraction was performed by the lead author and then fully verified by another author for accuracy and completeness.
2.5. Quality Assessment (Risk-of-Bias Assessment)
We used a two-level quality assessment. First, we assessed the methodological quality of the overall study design according to design type. For controlled experiments, we used the Cochrane-suggested risk-of-bias criteria for Effective Practice and Organization of Care reviews. In turn, for pre–post and observational studies, we used quality assessment tools from the National Institutes of Health. Finally, for the studies that also contained economic assessments, we additionally used the Joanna Briggs Institute’s critical appraisal checklist for economic evaluations. Two independent reviewers performed each assessment, with a third reviewer involved in resolving any conflicts.
2.6. Data Synthesis
The study methods, indicators, and quantitative findings, with a focus on the economic and other value-based assessments, were then tabulated and narratively synthesized to address each review question. Due to the heterogeneity of contexts and study designs, meta-analysis was not possible.
3. Results
Figure 1 provides the PRISMA flowchart of this review. Out of the 1317 unique references, 144 full texts were assessed, and nine were included—all from the USA. Of the studies on patient experience that also assessed other value-based impacts, while some could focus on more than one impact type, five focused on economic impact, three on provider well-being/burnout, and four on healthcare utilization. Two studies that assessed readmission rates also assessed economic impacts, i.e., they fit in both categories.
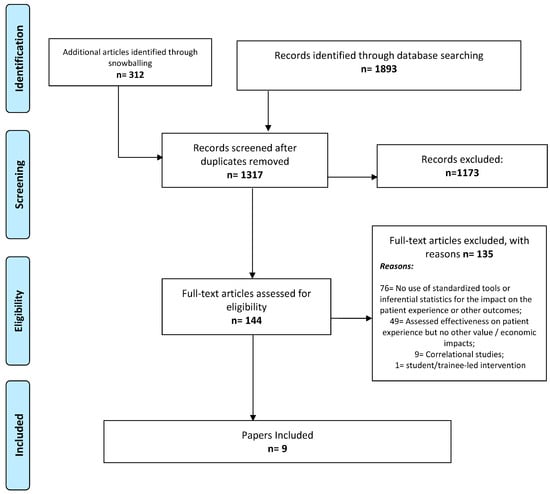
Figure 1.
PRISMA flowchart of the review.
The methodological quality of the economic impact evaluations ranged from a few methodological concerns, such as the use of estimated versus actual reimbursement [24], to a paper with no details about how the financial results were obtained [25]. Supplementary Tables S2 and S3 provide a synthesis of the methodological quality assessment of each study (for both the underlying study design and the economic evaluation component, where applicable) based on the respective quality assessment checklists. The key methodological features of each paper provide the context for the synthesized findings below for each review question.
3.1. Economic Impact of the Patient Experience Improvement Interventions
Table 1 provides synthesized details of the four studies on the improvement of patient experience that also assessed the economic impact—on costs, revenue, operating margin, or combinations of these. All these studies showed significant changes in at least some of their dimensions (e.g., in five of the 11 assessed items [24]).

Table 1.
The costs and benefits of interventions aimed at improving the patient experience of care, ordered by date of publication.
Below, we synthesize the economic findings and methods, organized by intervention type.
3.1.1. Discharge Support
Two studies focused on this intervention type (Table 1). A controlled before-and-after study with historical controls and adjustment for price changes found that a telephone-based transitional support cost an additional $430 per patient compared to usual care. The increased cost was statistically significant in both the univariate and multivariate models (p < 0.01 and p = 0.03, respectively). However, the same models showed no significant changes for hospital margin (p = 0.25 and p = 0.23, respectively) [24], suggesting that improved revenues were offsetting the increased cost of the intervention.
The study found that communication training for the surgeons (n = 56) of a children’s hospital increased hospital revenue (payments by 25% and charges by 21%) after adjusting for yearly price changes. In the same study, a small, controlled subgroup analysis (surgeons; n = 8) showed that payments and charges increased further (by 71% and 113%, respectively) for the plastic surgeons who received communication training, while revenue decreased for the surgeons who did not receive the training [10].
3.1.2. Patient Experience Office
Finally, we included a secondary analysis (i.e., an observational, retrospective, comparative study) of the financial impact of adding and operating a patient experience office within a healthcare organization’s structure, applied to a national sample of 132 hospitals [11]. Of note, a patient experience office is a formal, cross-departmental organizational unit dedicated to assessing, analyzing, and optimizing the entire patient journey and patient experience performance of a healthcare organization. The study found a 1.4% reduction in operating costs for each added year of the office’s operation. The article also reported that supplementary key informant interviews revealed that the associated positive financial results are likely a result of efficiency in communication training, improved outcomes, greater patient volumes, and better value-based reimbursements [11]. Altogether, these results suggest a potential positive financial impact for organizations that run patient experience offices and continue doing so over time.
3.2. Other Value-Based Impacts of Patient Experience Improvement Interventions
Seven studies on the improvement of patient experience with care also assessed other value-based impacts, such as provider well-being/burnout (n = 3) and readmission rates (n = 4). Of note, two of the latter [24,25] also assessed economic impacts and, therefore, have some components described in Table 1.
3.2.1. Provider Well-Being/Burnout Outcomes
Table 2 summarizes the three studies assessing the impact of patient experience improvement interventions on provider well-being or burnout, all using a pre–post design and employing physician communication training interventions. Two pre–post studies were relatively large (physicians trained = 104 [26] and 947 [14]), and the smaller study (physicians trained = 30) was part of a randomized controlled trial (RCT)—i.e., a pre–post study for the burnout outcomes and RCT for the patient experience outcomes [13].

Table 2.
Well-being outcomes from interventions aimed at improving the patient experience of care, ordered by date of publication.
All three studies found positive impacts on the patient experience of care, although the smaller study found them only for patient experience scores (i.e., not on percentile ranks, among peer providers) [13]. All three also found improvements in provider well-being or burnout. The smaller study found significant improvements in two of the subscales of the Maslach Burnout Inventory [13], while the largest found gains for all three subscales, with improvements on two subscales sustained after three months [14]. Finally, the remaining study found statistically significant positive impacts on three out of five burnout subscales measured with the Professional Fulfillment Index (Table 3), although not if Bonferroni corrections were applied (supplementary Table S2) [26].

Table 3.
Healthcare utilization outcomes from interventions aimed at improving the patient experience of care, ordered by date of publication.
3.2.2. Healthcare Utilization (e.g., Readmission Rates, Emergency Room Visits)
Table 3 describes four studies on improving the patient experience with post-discharge support or transitional care that also assessed the intervention’s impact on readmission rates.
One study found statistically significant impacts on healthcare utilization in the planned analyses. In a pragmatic randomized controlled trial of transitional care, no significant between-group differences in healthcare utilization (outpatient visits, hospitalizations, emergency room visits) were found within 60 days [27]. In a controlled before-and-after study of telephone-based post-discharge support, no significant between-group difference was found for 90-day readmissions (p = 0.21) [24]. In the pre–post study of discharge support, no significant differences in readmission rates were found [25]. Finally, a case–control study found no effects on readmission outcomes from a pharmacist-led, pre- and post-discharge education and medication reconciliation intervention; only in an unplanned subgroup analysis (for the post-discharge component) did the study find pre–post reductions on 30-day readmission rates: 17.3–12.4% (p = 0.007) [28].
4. Discussion
This review synthesizes the recent peer-reviewed literature spanning 2015–2024, focusing on the synergistic value-based assessments of patient experience improvement interventions. Emphasis was placed on economic impacts, provider well-being, and healthcare utilization outcomes. The synthesized interventions focused on provider communication training or post-discharge and transitional support. These interventions showed effectiveness in improving selected dimensions of patient experience and were coupled with either fiscal neutrality (e.g., costs offset by improved revenue [24]) or positive financial returns, such as improved revenue [10]. Reduced healthcare utilization was not found in the target outcomes of studies on discharge and transitional care processes [24,25,27,28]. Nonetheless, these processes resulted in economic benefits [25] or neutrality [24]. These results align with secondary correlational studies, demonstrating positive associations of patient experience scores with health organizations’ financial performance [25,29,30].
From a broader value-based perspective, interventions targeting provider communication have been shown to yield gains in provider well-being and reduce burnout [13,14,26]. Through the lens of relationship-centered care, it is hypothesized that improving patient–provider communication can positively impact patient as well as provider experiences, which are viewed as dynamically interconnected [15]. The improvement mechanism may involve fostering staff engagement with compassionate and relational care, contrasting with instrumental organizational climates that can negatively affect provider well-being and sense of accomplishment [19,20,21,31,32].
Initiatives for improving patient–provider communication may have a high synergistic potential and even potentially contribute to all four components of a value-based perspective focused on the quadruple aim: population health, cost, patient experience, and provider well-being [17,18]. Here, we found that these initiatives are associated with positive financial results, patient experience, and provider well-being, and synergistically so. In turn, in the broader literature, better patient experience scores have been correlated with improved self-reported patient health outcomes [2], including through enhanced shared decision-making [33]. Therefore, an enhanced value proposition may apply to organizational activities that aim to improve patient–provider communication.
Additionally, enhancing provider well-being can offer significant value to healthcare organizations grappling with challenges in recruiting, retaining, and maintaining an engaged and productive staff. High vacancy and turnover rates entail various costs, including recruitment and retention expenses, continual retraining of new staff, the inability to meet heightened demands due to staff shortages, and potential risks to reliability resulting from uncoordinated team processes [17,34]. Notably, the potential benefits of these factors were not assessed or quantified in the reviewed literature and may be further avenues for research.
Similarly, the literature did not explore the potential reduction in litigation costs despite the plausibility of such benefits. Improved communication practices, a frequent determinant of litigation, could lead to diminished legal costs or malpractice premiums [35]. Lastly, there were no included studies on patient experience improvement activities beyond provider communication or post-discharge support (e.g., real-time patient experience feedback [36,37]). Exploring these avenues could provide further opportunities to investigate the synergistic value of activities aimed at enhancing patient experience.
While the literature primarily focuses on the United States, this trend may stem from a combination of factors. The CMS’s Value-Based Purchasing program offers incentives to U.S. health providers based on quality and patient experience metrics, potentially motivating health organizations in the U.S. to invest in and study patient experience improvement activities. However, caution must be taken regarding the generalizability of the results from this review to other contexts, where the same incentives and returns may not apply. Additionally, the U.S. operates under a consumer-based healthcare delivery system, where consumers’ choices for providers are influenced by lived patient experiences, word-of-mouth recommendations, online reviews, and comparison websites [9]. This dynamic places the financial strength of healthcare organizations at risk based on their performance in patient experience. Consequently, these incentives are likely drivers for increasing organizational investments in patient experience improvement structures and activities in the U.S. [11], fostering an enhanced interest in studying the business case for such investments.
5. Limitations
These results should be taken with caution, apart from the generalizability outside of the U.S. context. The volume of the literature was not large, and controlled study designs were rare. In addition, we did not conduct a meta-analysis due to the heterogeneity of interventions, contexts, and study designs. We only covered English-language peer-reviewed literature, while many economic analyses of patient experience improvement activities may be in the grey literature or even in unpublished, internal analyses. Many health sector contexts, such as primary care settings and safety-net hospitals, were not adequately represented in the reviewed literature. Furthermore, the economic analyses exhibited a spectrum of methodological rigor, ranging from no substantive risks of bias to a complete underreporting of methods, resulting in significant variability. Collectively, these methodological weaknesses and variations in study designs pose challenges to the robustness of the body of knowledge derived from this review.
6. Conclusions
The findings of this review, based on the literature from the U.S. context, underscore the potential financial and employee well-being benefits associated with investments in activities targeting and effectively achieving improvements in patient experiences with care. These results contribute to the value-based argument for healthcare administrators to prioritize investments in patient experience improvement activities, with a particular emphasis on enhancing patient–provider communication.
However, it is essential to approach these findings with caution, considering the substantive potential for strengthening this body of knowledge in terms of scope, volume, and methodological quality. Opportunities exist for incorporating additional economic variables, such as malpractice litigation costs and factors secondary to employee engagement and retention. Additionally, further research could explore the impact on the quadruple aim, encompassing patient experience, provider well-being, clinical effectiveness, and costs, particularly when examined in tandem.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare13131622/s1, Table S1: Full search strategy per scientific database. Table S2: Study design and methodological weaknesses based on the respective quality assessment checklists for the studies responding to the first study question. Table S3: Study design and respective methodological weaknesses based on quality assessment checklists for the studies responding to the second review question.
Author Contributions
T.S.J.: Conceptualization; Methodology; Investigation; Data curation; Project administration; Writing—original draft. D.L.: Investigation; Data curation; Validation; Writing—review & editing. B.Z.S.: Data curation; Validation; Writing—review & editing. M.Z.: Data curation; Validation; Writing—review & editing. J.S.: Data curation; Validation; Writing—review & editing. A.W.H.: Conceptualization; Methodology; Writing—review & editing. A.D.: Conceptualization; Methodology; Writing—review & editing. N.J.: Conceptualization; Methodology; Writing—review & editing. All authors have read and agreed to the published version of the manuscript.
Funding
Tiago S. Jesus completed part of this work and Manrui Zhang the totally of this work under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR; 90ARHF0003). NIDILRR is a center within the Administration for Community Living (ACL), U.S. Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, or HHS, and the reader should not assume endorsement by the U.S. federal government. Dr Jesus initiated this work with the Northwestern University’s affiliation (under the grant support mentioned) and the work was completed with The Ohio State University’s affiliation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Agency for Healthcare Research and Quality. What Is Patient Experience? Rockville, MD [December 2022]. Available online: https://www.ahrq.gov/cahps/about-cahps/patient-experience/index.html (accessed on 12 April 2024).
- Navarro, S.; Ochoa, C.Y.; Chan, E.; Du, S.; Farias, A.J. Will Improvements in Patient Experience with Care Impact Clinical and Quality of Care Outcomes? A Systematic Review. Med. Care. 2021, 59, 843–856. [Google Scholar] [CrossRef] [PubMed]
- Agency for Healthcare Research and Quality. The CAHPS Program Rockville, MD [December 22]. Available online: https://www.ahrq.gov/cahps/about-cahps/cahps-program/index.html (accessed on 12 April 2024).
- Food and Drug Administration. Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims; FDA: Silver Spring, MD, USA, 2009.
- Kingsley, C.; Patel, S. Patient-reported outcome measures and patient-reported experience measures. BJA Educ. 2017, 17, 137–144. [Google Scholar] [CrossRef]
- Friedel, A.L.; Siegel, S.; Kirstein, C.F.; Gerigk, M.; Bingel, U.; Diehl, A.; Steidle, O.; Haupeltshofer, S.; Andermahr, B.; Chmielewski, W.; et al. Measuring Patient Experience and Patient Satisfaction-How Are We Doing It and Why Does It Matter? A Comparison of European and U.S. American Approaches. Healthcare 2023, 11, 797. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Medicare.gov. Find & Compare Providers Near You 2022 [Cited 2022 December 21]. Available online: https://www.medicare.gov/care-compare/ (accessed on 12 April 2024).
- Elliott, M.N.; Beckett, M.K.; Lehrman, W.G.; Cleary, P.; Cohea, C.W.; Giordano, L.A.; Goldstein, E.H.; Damberg, C.L. Understanding the Role Played by Medicare’s Patient Experience Points System in Hospital Reimbursement. Health Aff. 2016, 35, 1673–1680. [Google Scholar] [CrossRef] [PubMed]
- Adams, C.; Walpola, R.; Schembri, A.M.; Harrison, R. The ultimate question? Evaluating the use of Net Promoter Score in healthcare: A systematic review. Health Expect. Int. J. Public Particip. Health Care Health Policy 2022, 25, 2328–2339. [Google Scholar] [CrossRef] [PubMed]
- Abu-Ghname, A.; Davis, M.J.; Shook, J.E.; Reece, E.M.; Hollier, L.H., Jr. Press Ganey: Patient-Centered Communication Drives Provider and Hospital Revenue. Plast. Reconstr. Surg. 2021, 147, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Sharma, L.; Chandrasekaran, A.; Bendoly, E. Does the Office of Patient Experience Matter in Improving Delivery of Care? Prod. Oper. Manag. 2020, 29, 833–855. [Google Scholar] [CrossRef] [PubMed]
- Boissy, A. Getting to Patient-Centered Care in a Post–Covid-19 Digital World: A Proposal for Novel Surveys, Methodology, and Patient Experience Maturity Assessment. NEJM Catalyst. 2020, 1–12. [Google Scholar] [CrossRef]
- Congiusta, S.; Ascher, E.M.; Ahn, S.; Nash, I.S. The Use of Online Physician Training Can Improve Patient Experience and Physician Burnout. Am. J. Med. Qual. 2020, 35, 258–264. [Google Scholar] [CrossRef]
- Boissy, A.; Windover, A.K.; Bokar, D.; Karafa, M.; Neuendorf, K.; Frankel, R.M.; Merlino, J.; Rothberg, M.B. Communication Skills Training for Physicians Improves Patient Satisfaction. J. Gen. Intern. Med. 2016, 31, 755–761. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beach, M.C.; Inui, T. Relationship-centered care. A constructive reframing. J. Gen. Intern. Med. 2006, 21 (Suppl. S1), S3–S8. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jesus, T.S.; Papadimitriou, C.; Bright, F.A.; Kayes, N.M.; Pinho, C.S.; Cott, C.A. Person-Centered Rehabilitation Model: Framing the Concept and Practice of Person-Centered Adult Physical Rehabilitation Based on a Scoping Review and Thematic Analysis of the Literature. Arch. Phys. Med. Rehabil. 2022, 103, 106–120. [Google Scholar] [CrossRef] [PubMed]
- Bodenheimer, T.; Sinsky, C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014, 12, 573–576. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fitzpatrick, B.; Bloore, K.; Blake, N. Joy in Work and Reducing Nurse Burnout: From Triple Aim to Quadruple Aim. AACN Adv. Crit. Care 2019, 30, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Howell, T.G.; Mylod, D.E.; Lee, T.H.; Shanafelt, T.; Prissel, P. Physician Burnout, Resilience, and Patient Experience in a Community Practice: Correlations and the Central Role of Activation. J. Patient Exp. 2019, 7, 1491–1500. [Google Scholar] [CrossRef]
- Porter, T.H.; Rathert, C.; Ishqaidef, G.; Simmons, D.R. System justification theory as a foundation for understanding relations among toxic health care workplaces, bullying, and psychological safety. Health Care Manag. Rev. 2024, 49, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Rathert, C.; Vogus, T.; Hearld, L.R. Psychological work climates and health care worker well-being. Health Care Manag. Rev. 2024, 49, 85. [Google Scholar] [CrossRef] [PubMed]
- Doyle, C.; Lennox, L.; Bell, D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013, 3, e001570. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schreiter, N.A.; Fisher, A.; Barrett, J.R.; Acher, A.; Sell, L.; Edwards, D.; Leverson, G.; Joachim, A.; Weber, S.M.; Abbott, D.E. A telephone-based surgical transitional care program with improved patient satisfaction scores and fiscal neutrality. Surgery 2021, 169, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Thum, A.; Ackermann, L.; Edger, M.B.; Riggio, J. Improving the Discharge Experience of Hospital Patients Through Standard Tools and Methods of Education. J. Healthc. Qual. Promot. Excell. Healthc. 2022, 44, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Altamirano, J.; Kline, M.; Schwartz, R.; Fassiotto, M.; Maldonado, Y.; Weimer-Elder, B. The effect of a relationship-centered communication program on patient experience and provider wellness. Patient Educ. Couns. 2022, 105, 1988–1995. [Google Scholar] [CrossRef] [PubMed]
- LaBedz, S.L.; Prieto-Centurion, V.; Mutso, A.; Basu, S.; Bracken, N.E.; Calhoun, E.A.; DiDomenico, R.J.; Joo, M.; Pickard, A.S.; Pittendrigh, B.; et al. Pragmatic Clinical Trial to Improve Patient Experience Among Adults During Transitions from Hospital to Home: The PArTNER study. J. Gen. Intern. Med. 2022, 37, 4103–4111. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- March, K.L.; Peters, M.J.; Finch, C.K.; Roberts, L.A.; McLean, K.M.; Covert, A.M.; Twilla, J.D. Pharmacist Transition-of-Care Services Improve Patient Satisfaction and Decrease Hospital Readmissions. J. Pharm. Pract. 2022, 35, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Akinleye, D.D.; McNutt, L.A.; Lazariu, V.; McLaughlin, C.C. Correlation between hospital finances and quality and safety of patient care. PLoS ONE 2019, 14, e0219124. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Richter, J.P.; Muhlestein, D.B. Patient experience and hospital profitability: Is there a link? Health Care Manag. Rev. 2017, 42, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Jesus, T.S.; Stern, B.Z.; Struhar, J.; Deutsch, A.; Heinemann, A.W. The use of patient experience feedback in rehabilitation quality improvement and codesign activities: Scoping review of the literature. Clin Rehabil. 2023, 37, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Jesus, T.S.; Papadimitriou, C.; Pinho, C.S.; Hoenig, H. Key Characteristics of Rehabilitation Quality Improvement Publications: Scoping Review From 2010 to 2016. Arch. Phys. Med. Rehabil. 2018, 99, 1141–1148.e4. [Google Scholar] [CrossRef] [PubMed]
- Elwyn, G.; Frosch, D.L.; Kobrin, S. Implementing shared decision-making: Consider all the consequences. Implement. Sci. IS 2016, 11, 114. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coulmont, M.; Roy, C.; Dumas, L. Does the Planetree patient-centered approach to care pay off?: A cost-benefit analysis. Health Care Manag. 2013, 32, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.S.; Miller, T.; Daniels, C.; Paine, M.; Gresh, B.; Betz, A.L. Creating the Exceptional Patient Experience in One Academic Health System. Acad. Med. 2016, 91, 338–344. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jesus, T.S.; Struhar, J.; Zhang, M.; Lee, D.; Stern, B.Z.; Heinemann, A.W.; Jordan, N.; Deutsch, A. Near real-time patient experience feedback with data relay to providers: A systematic review of its effectiveness. Int. J. Qual. Health Care 2024, 36, mzae053. [Google Scholar] [CrossRef] [PubMed]
- Khanbhai, M.; Flott, K.; Darzi, A.; Mayer, E. Evaluating Digital Maturity and Patient Acceptability of Real-Time Patient Experience Feedback Systems: Systematic Review. J. Med. Internet Res. 2019, 21, e9076. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).