Advancements and Innovation Trends of Information Technology Empowering Elderly Care Community Services Based on CiteSpace and VOSViewer
Abstract
1. Introduction
1.1. Research Background and Motivation
1.2. Research Gap
1.3. Research Goals and Significance
- (1)
- To identify key individuals, institutions, and nations contributing to this field.
- (2)
- To develop a comprehensive research framework.
- (3)
- To suggest future research avenues and enhancement strategies.
2. Research Methods
2.1. Software Selection and Parameter Definition
2.2. Data Collection and Processing
2.3. Descriptive Statistical Analysis
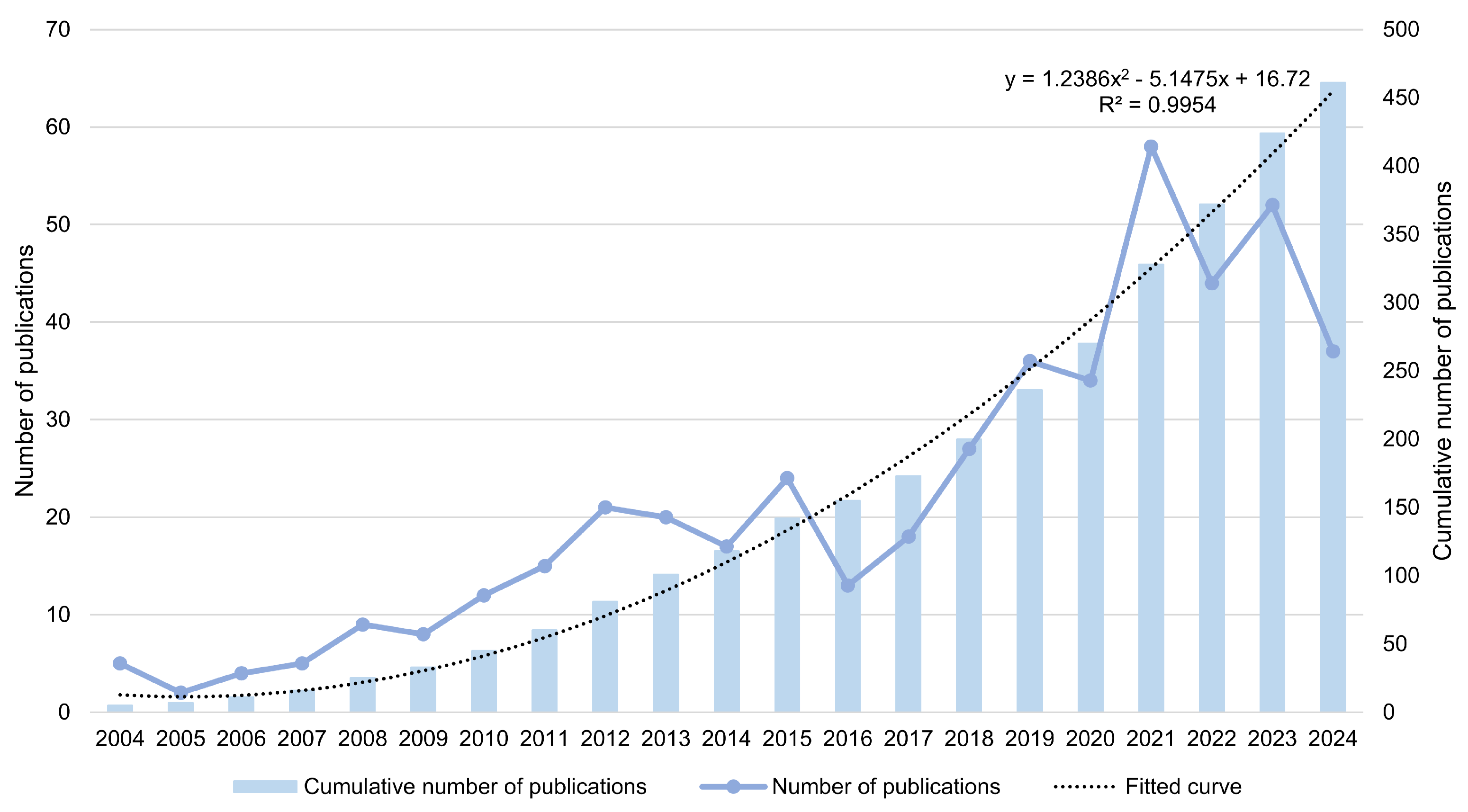
2.3.1. Quantitative Analysis
2.3.2. Category Analysis
2.3.3. Journal Analysis
3. Cooperation Analysis
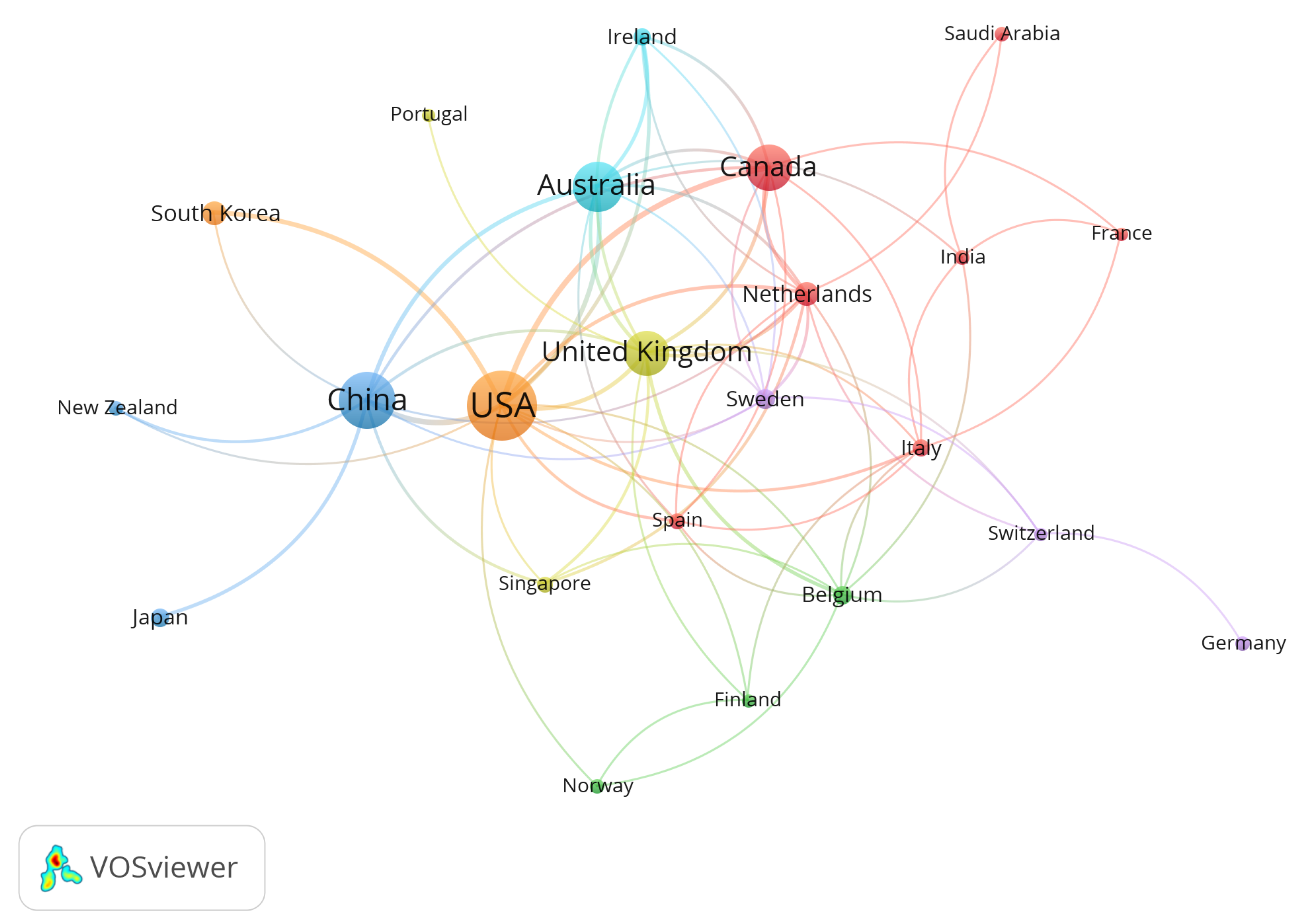
3.1. Country Cooperation
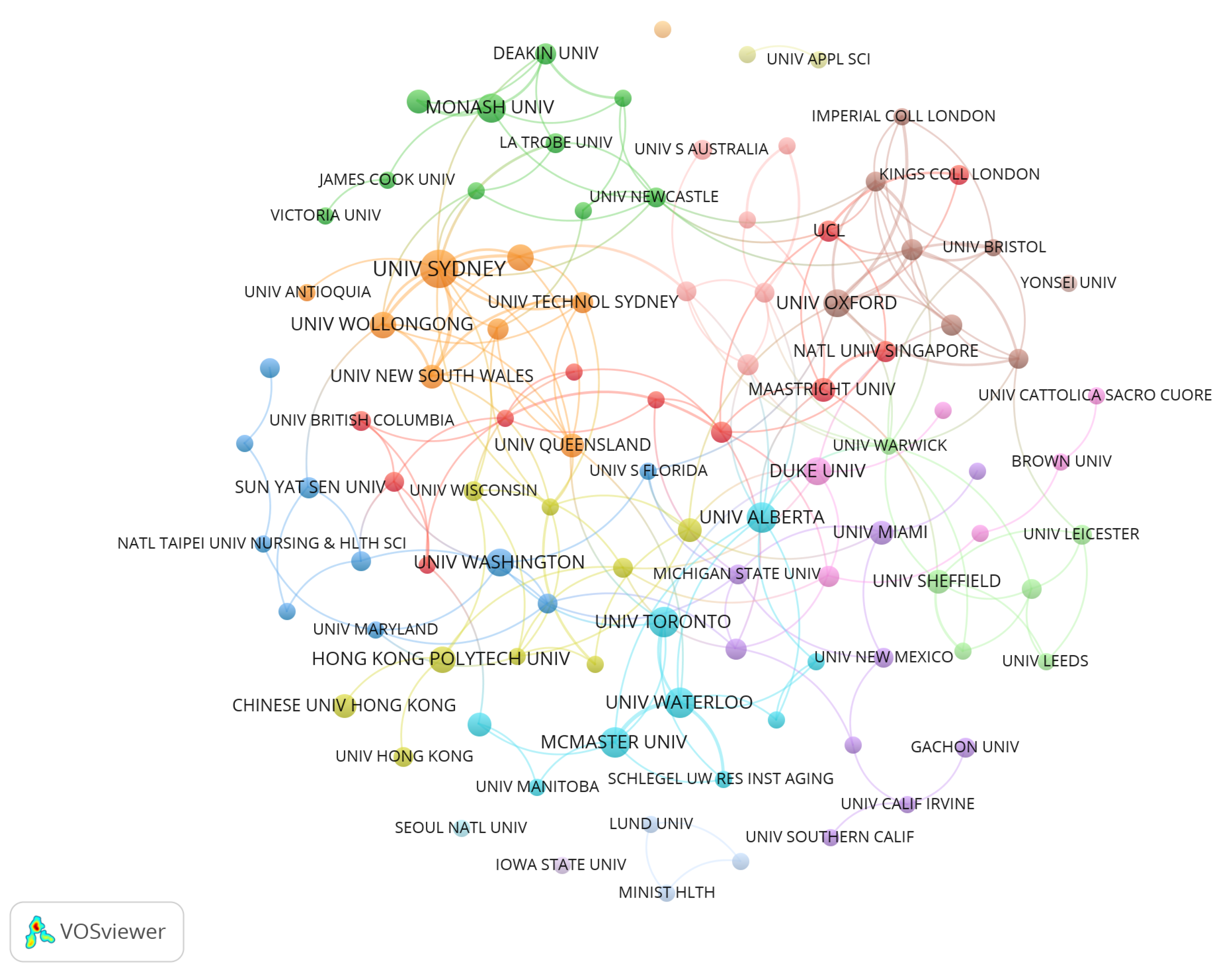
3.2. Institution Cooperation
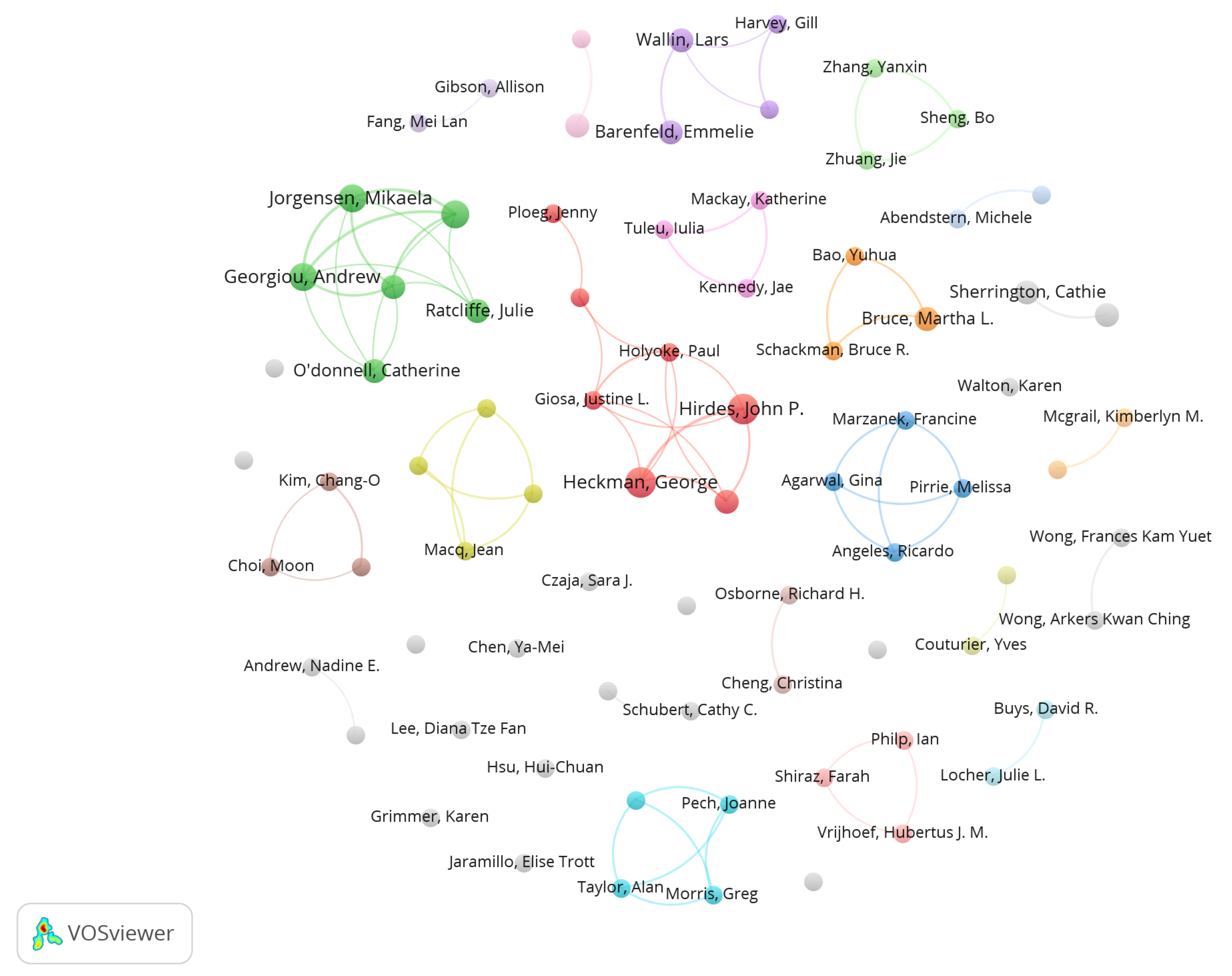
3.3. Author Cooperation
4. Keyword Analysis
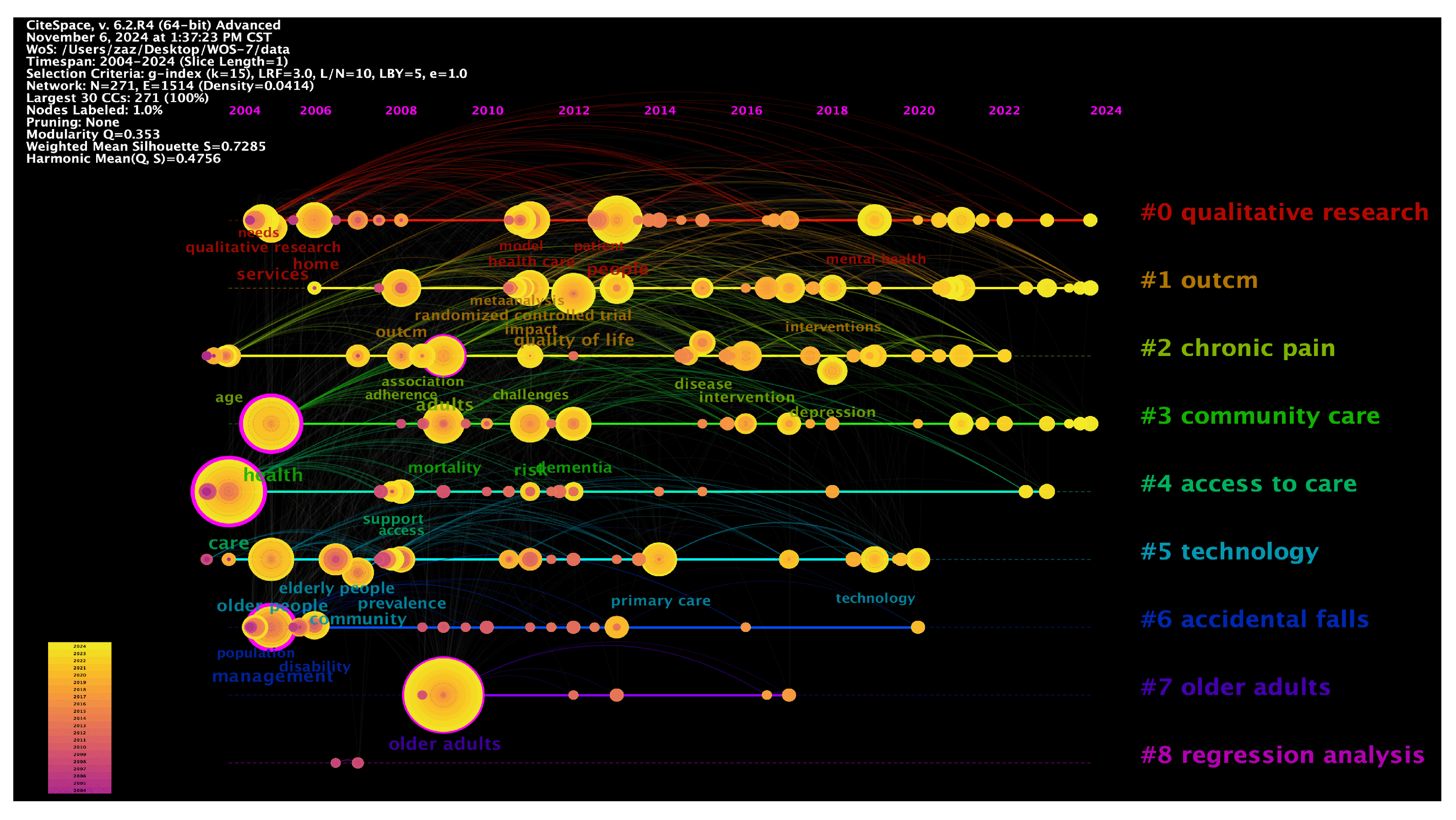
4.1. Keyword Co-Occurrence
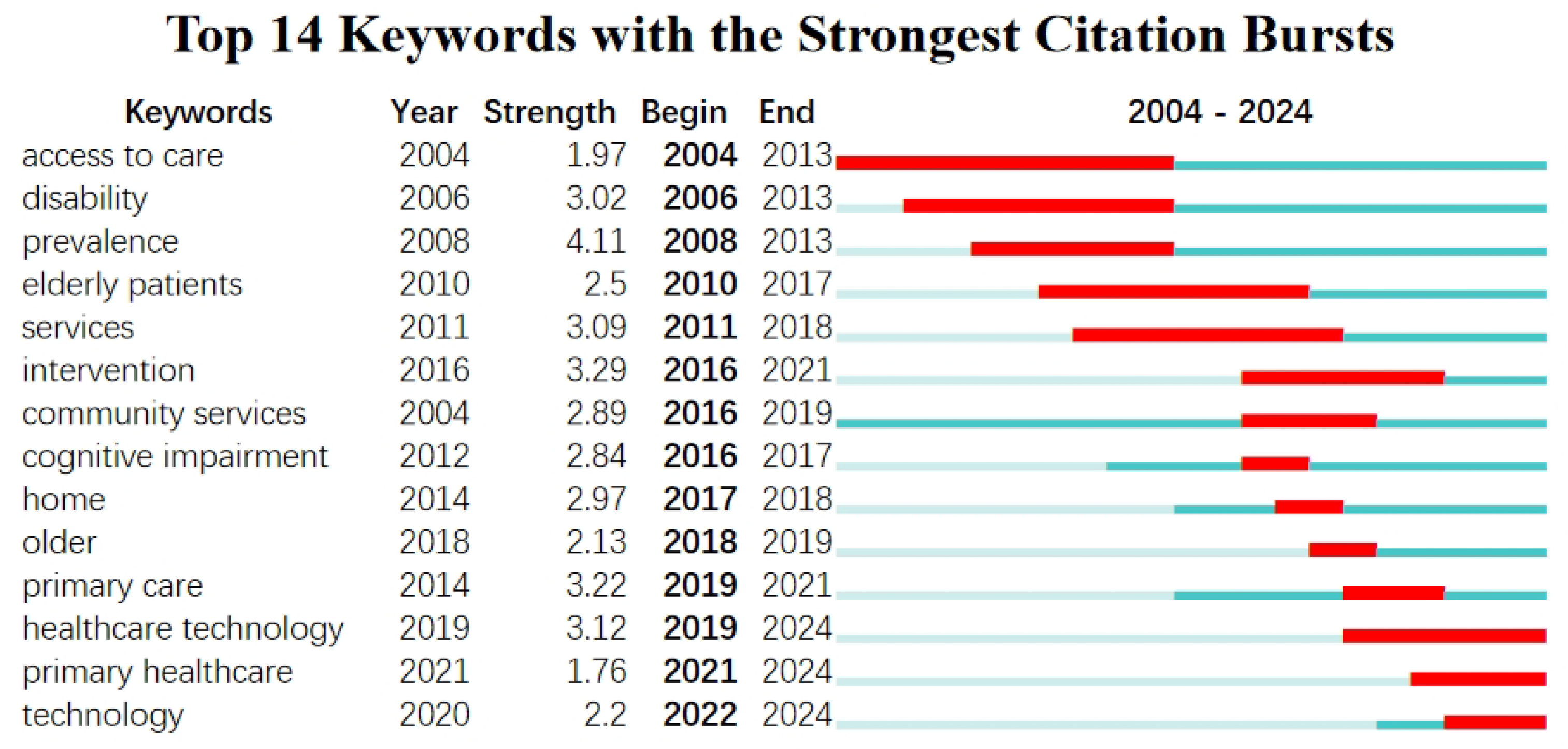
4.2. Keyword Emergence
5. Co-Citation Analysis
5.1. Journal Citation
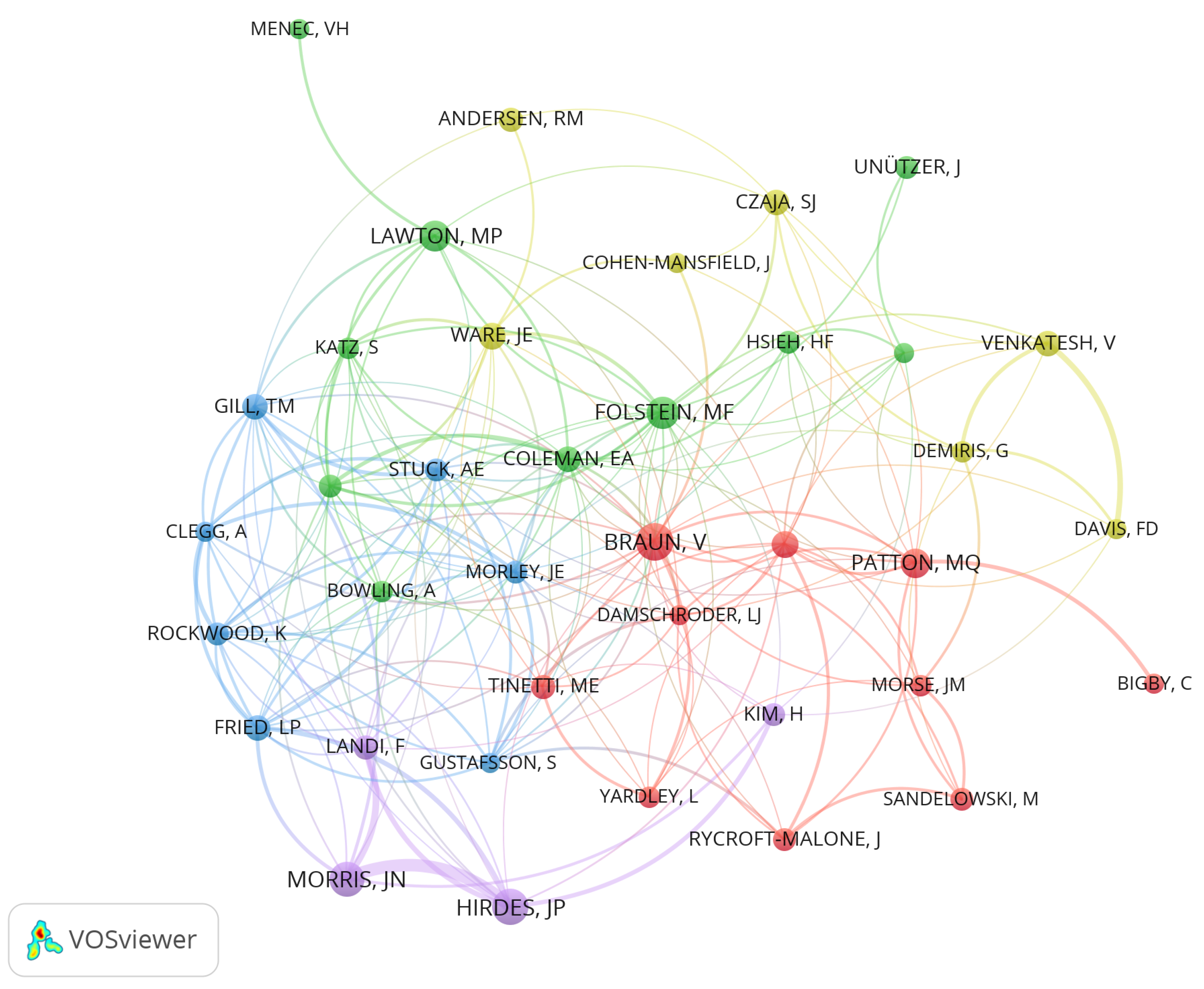
5.2. Author Citation
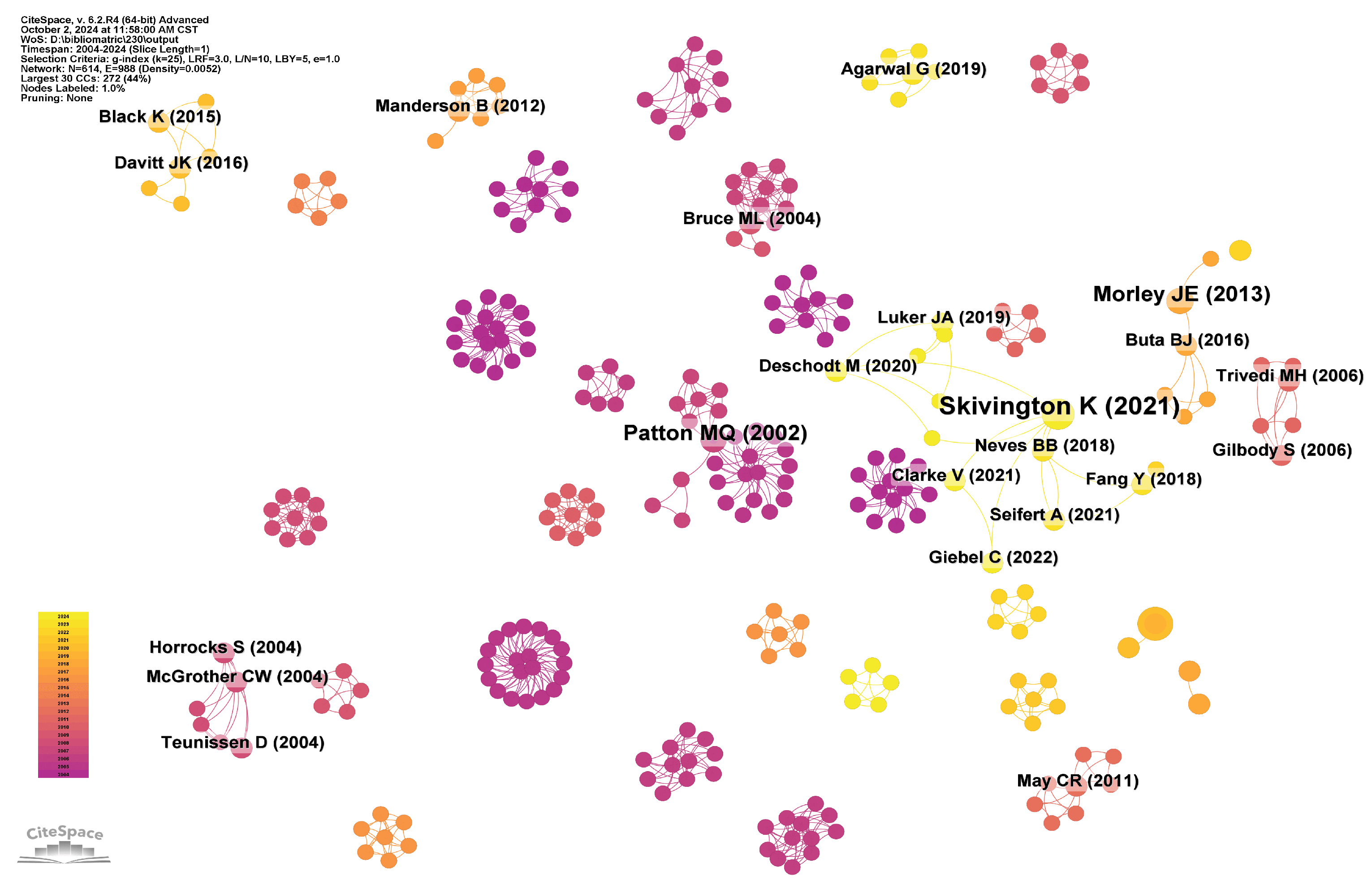
5.3. Document Citation
5.4. Cluster Analysis
- (1)
- Community care#3 Community care is an essential domain that entails improving the quality of life for older people through diverse technological methods, allowing them to enjoy their later years within a familiar community setting. Gustafson and colleagues investigated the influence of information and communication technology (ICT) on the quality of life of older people, examining the potential application of ICT in community care via a randomized controlled trial [5]. Furthermore, Taylor and colleagues concentrated on home telemedicine video conferencing, analyzing the perceptions and efficacy of this technology in delivering community care services [7]. Northwood and colleagues used a group concept mapping methodology to investigate the application of electronic health tools (interRAI Check-Up Self Report) in facilitating the integrated health and social care of older people and their caregivers within the community [84]. This tool can integrate health information, enhance care efficiency, and, via multidisciplinary team collaboration, deliver more comprehensive and compassionate care services for older adults. Rahmawati Riana et al. demonstrated the function of community health workers in managing hypertension in older people [128], emphasizing the significance of community care in managing chronic diseases.While IT has helped communities address various elderly care issues, numerous challenges in caring for older adults persist due to social factors. For instance, considerable challenges arise in domains such as the prevalence and acceptance of technology [10], cross-cultural differences, and service compatibility [129]. To effectively address these challenges, it is essential to enhance the user experience design of IT by thoroughly considering the cognitive capacities, cultural contexts, and usage patterns of older individuals, thereby improving their satisfaction and the efficacy of elderly care services.
- (2)
- Access to careImproving the accessibility of medical and nursing services for older people (#4 Access to care) is a core issue. Numerous studies have explored this topic from different perspectives, and some of these studies have integrated IT to provide more convenient and efficient health services for older people. Soran and others indicated that computerized telephone monitoring systems are superior to conventional care in reducing healthcare costs for elderly patients with heart failure [6]. Moreover, Chiu Kuang and colleagues in Taiwan further confirmed the feasibility of remote monitoring of the health status of older people at home [8]. These studies enhance the ability of older people to access medical services, reduce healthcare costs, and improve the efficiency of medical resource utilization.Despite the increasing number of studies on the accessibility of medical and nursing services, there are still many areas that need improvement. For instance, Gao Li and others have explored the inadequacies in the integration of health resources for the elderly [130]. Meanwhile, Hogeveen Sophie and colleagues investigated the challenges faced by the elderly in accessing healthcare services [131]. These studies indicate that the elderly still face a series of issues regarding the accessibility of healthcare services, including insufficient service integration and coordination, low acceptance of technology, a significant digital divide, uneven resource distribution, and variations in service quality. To effectively address these challenges, it is urgently necessary for the government, society, and service providers to strengthen cooperation and promote the application of information technology in elderly community services, thereby facilitating the continuous development and improvement of services.
- (3)
- TechnologyThe application of technology is a key driver for upgrading and optimizing services. Among the various technologies, telemedicine, intelligent assistance systems, and digital tools are particularly significant. These technologies provide more comprehensive and personalized services for older adults through various methods. Chiu Kuang et al. and Taylor et al. demonstrated that remote monitoring technology can effectively monitor and care for the health status of older people [7,130]. Both studies demonstrated that this technology enhances the efficiency of medical services and significantly improves the quality of life for older individuals. Furthermore, the study by Fan et al. shows that compared to traditional in-person medical consultations, health chatbots improve the efficiency of self-diagnosis among older persons by 40% [132]. This research provides empirical evidence for the clinical implementation of health chatbots. Regarding intelligent assistance systems, Gustafson et al. demonstrated the effectiveness and comprehensiveness of information and communication technology (ICT) in improving the quality of life for older people [5]. Moreover, Northwood et al. used electronic health tools to integrate health and social care information, enhancing collaboration among interdisciplinary teams to deliver more comprehensive and compassionate care for older people within the community [84]. In the field of artificial intelligence applications, a study by Ghosh et al. proposed the “FEEL” framework, which achieves federated learning through edge-IoMT devices, reducing the risk of data breaches by 89%. This framework provides a secure foundation for multi-institutional collaborative community health networks [133]. Moreover, Lima et al. provided personalized companionship through multimodal emotion recognition, significantly alleviating anxiety in dementia patients [134]. Furthermore, Wilmink et al. found that an AI-driven health platform, combined with wearable devices, can reduce the risk of falls by 32%, providing key clinical evidence for technology-based preventive interventions [135]. These digital tools improve care efficiency and ensure that empathy in care is preserved by standardizing assessment technologies during their implementation.Despite the significant potential these technologies show in eldercare community services, many challenges need to be addressed. Wong et al. and Fan et al. indicated that the high complexity of system development results in a lack of user-friendliness and interface accessibility, leading to limited acceptance among older people [132,136]. Moreover, Vergouw et al. noted that older individuals often encounter difficulties when using applications and lack access to professional guidance [137]. Additionally, the research by Wilmink et al. also indicates that issues with the comfort of wearable devices can lead users to discontinue their use [135]. These studies illustrate that future technology needs to balance precise monitoring and user experience, continuously enhancing the informational empowerment and service quality of eldercare community services through technological innovation and service optimization.
- (4)
- Older adults#7 Research concerning older adults has attracted significant attention. These studies aim to improve the quality of life for older people, augment their autonomy, and enhance their social interaction abilities. Wong and colleagues examined the technological acceptance of the Intelligent Comprehensive Interactive Care (ICIC) system among older people [136]. The research indicated that older people strongly accepted the system, suggesting its potential utility in community elder care services. Furthermore, Gell Nancy M. and associates examined technology usage trends among older people with and without disabilities [109]. This research offers significant references for developing technological products and services tailored to the varied needs of older people. Kim and colleagues developed a healthcare service system tailored for older adults [138]. Their research demonstrated that the system markedly enhanced the accessibility and quality of healthcare services for older people. Furthermore, Askari Marjan and colleagues concentrated on the usage intentions of older Dutch people concerning medical applications [139]. This research provides significant insights for developing medical applications tailored to the requirements of older people in the Netherlands.Although there have been some advancements in IT to address the challenges older people face in recent years, several issues remain insufficiently addressed. Jamerson et al. noted that older adults encounter various challenges in medication management attributable to cognitive decline [140]. Furthermore, Kim and associates indicated that older people face challenges adapting to and embracing new technological paradigms [138]. Furthermore, the integration of information technology with elder care services requires careful consideration of its profound ethical and social implications. Firstly, the collection of sensitive health data poses risks to privacy and data security [141,142]. Secondly, the digital divide caused by disparities in digital literacy and economic resources may exacerbate inequality and social exclusion among the elderly population [143,144]. Excessive reliance on technology may also weaken the necessary interpersonal interactions within care services [145]. In addition, ensuring the autonomy and informed consent of older adults when their data is used presents a significant challenge, particularly for those with cognitive impairments [146,147]. Therefore, in parallel with technological innovation, establishing a robust ethical framework, adopting inclusive design principles, and engaging in ongoing social dialogue is crucial for the equitable and responsible development of information technology in elder care services.
6. Future Research Directions
- (1)
- Conduct in-depth research on smart elderly care and health technology.Innovations in senior care and health technology are the current research hotspots. Future research should focus on developing intelligent technologies for elderly care, with a particular emphasis on AI-driven health monitoring, age-friendly technology design, and blockchain for data security [148,149]. Big data and artificial intelligence enable the real-time monitoring and analysis of health data for older people, offering more accurate health management solutions. Furthermore, the advancement of Internet of Things technology will lead to a greater integration of smart homes and wearable devices into the daily lives of older people, significantly improving their quality of life and convenience. Nonetheless, as intelligent care for older people and health technology continue to be refined, potential challenges must be addressed. The maturity and stability of technology require enhancement, and disparities exist in the technology acceptance and usage proficiency among older adults. Furthermore, data security and privacy protection are paramount, requiring the implementation of robust data protection measures to safeguard the personal information of older people.
- (2)
- Research on an Integrated Community-Based Elderly Care Service System.Integrated community care requires coordination of cross-departmental resources. Referring to relevant reports from the Australian government, the World Health Organization, and other institutions, in the future, we should focus on standardizing service workflows and digital needs assessment tools, as well as eliminating resource duplication [150,151,152]. Furthermore, this study suggests that community services should emphasize integration, enhancement, standardization, and the judicious distribution of resources. First, service content necessitates integration and optimization, encompassing medical care, rehabilitation, caregiving, and entertainment, with tailored services provided to address the distinct needs of older adults. Second, comprehensive assessments of the needs of older people can enhance service strategies, including advancements in healthcare, telemedicine, and ongoing care services. Third, the standardization and normalization of service processes should be advanced by instituting uniform service standards and procedures to enhance service efficiency and quality. Finally, the judicious allocation and distribution of service resources must be accomplished, enhancing the utilization of human, material, and informational assets to minimize expenses while increasing efficiency. Although research on integrated community-based elderly care service systems has progressively increased in recent years, their implementation has encountered numerous challenges. Integrating service resources requires enhancement, as specific resources are duplicated or squandered. Conversely, the standardization and normalization of service processes are insufficient, resulting in cumbersome and inefficient workflows. Moreover, the professional qualifications of service personnel are inconsistent, requiring enhanced skills training and practical experience to improve their competencies.
- (3)
- Research on Interdisciplinary Collaboration and Information Sharing.The research of eldercare community services is progressively transitioning from a singular medical domain to a multidisciplinary comprehensive inquiry. However, interdisciplinary collaboration must still be based on WHO interoperability standards and integrate ICN’s nurse-led coordination model, which involves developing collaborative platforms, nurse-led information hubs, and breaking down information silos [148,149,152]. In the future, the innovation and implementation of interdisciplinary collaboration models will emerge as a focal point of research, encompassing the exploration of cooperative mechanisms and models across various disciplines and evaluating the efficacy of collaboration. Furthermore, developing and enhancing information-sharing platforms for older people is essential for facilitating information exchange and collaborative efforts among diverse departments and institutions. Moreover, the implementation and advancement of IT present extensive opportunities for the sector. Emerging technologies such as blockchain and artificial intelligence can facilitate the advanced development of eldercare community service systems. Despite interdisciplinary collaboration and information sharing being considered fundamental research directions in this domain, significant challenges persist. The disparities in research methodologies and epistemologies across various disciplines augment the intricacy of interdisciplinary collaboration. Conversely, information-sharing mechanisms remain underdeveloped, with information silos presenting a significant challenge, thereby requiring immediate improvement in the standardization and regulation of information exchange.
- (4)
- Precise policies and financial support.Precise policies and financial support are essential for developing information-driven elderly community services. Policy-making should draw on the WHO’s policy maturity assessment tool and refer to effective policies of many governments, focusing on dynamic policy adaptation, public–private investment framework, and performance monitoring indicators [150,151,152]. Moreover, novel mechanisms and models for financing elderly services should be implemented, including the creation of dedicated funds and the integration of social capital through various approaches to provide economic assistance for advancing elderly services. Furthermore, assessing and overseeing the efficacy of policies and financial assistance is essential. Regular evaluations clarify the outcomes of policy implementation and financial assistance, enabling the identification and resolution of existing issues. An intelligent elderly information system should be developed according to local requirements to document the health and service data of senior citizens in the area, thereby enhancing the efficiency of community elderly services. Nonetheless, specific chain reactions may transpire during the ongoing optimization of policies. The formulation and implementation of policies exhibit delays and incompatibility issues, as specific policies fail to keep pace with the rapid development of information-driven elderly community services. Conversely, the mechanisms and models for financial support remain imperfect, where issues such as inefficient fund utilization and insufficient oversight are still prevalent. Moreover, inadequate emphasis on policies and financial support by certain localities and institutions may hinder the effectiveness of implementation.
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ye, L.; van Grieken, A.; Alhambra-Borrás, T.; Zhou, S.; Clough, G.; Markaki, A.; Bilajac, L.; Raat, H. Interplay of physical, psychological, and social frailty among community-dwelling older adults in five european countries: A longitudinal study. J. Urban Health 2024, 101, 730–739. [Google Scholar] [CrossRef] [PubMed]
- Mueller, A.; Hoefling, H.A.; Muaremi, A.; Praestgaard, J.; Walsh, L.C.; Bunte, O.; Huber, R.M.; Fürmetz, J.; Keppler, A.M.; Schieker, M.; et al. Continuous digital monitoring of walking speed in frail elderly patients: Noninterventional validation study and longitudinal clinical trial. JMIR MHealth UHealth 2019, 7, e15191. [Google Scholar] [CrossRef]
- Willard, S.; Cremers, G.; Man, Y.P.; van Rossum, E.; Spreeuwenberg, M.; de Witte, L. Development and testing of an online community care platform for frail older adults in the Netherlands: A user-centred design. BMC Geriatr. 2018, 18, 87. [Google Scholar] [CrossRef] [PubMed]
- Schubert, C.C.; Penney, L.S.; Schwartzkopf, A.L.; Damush, T.M.; Preddie, A.; Flemming, S.; Myers, J.; Myers, L.J.; Perkins, A.J.; Zhang, Y.; et al. Expanding Access to Comprehensive Geriatric Evaluation via Telehealth: Development of Hybrid-Virtual Home Visits. J. Gen. Intern. Med. 2024, 39, 36–43. [Google Scholar] [CrossRef]
- Gustafson, D.H.; McTavish, F.; Gustafson, D.H.; Mahoney, J.E.; Johnson, R.A.; Lee, J.D.; Quanbeck, A.; Atwood, A.K.; Isham, A.; Veeramani, R.; et al. The effect of an information and communication technology (ICT) on older adults’ quality of life: Study protocol for a randomized control trial. Trials 2015, 16, 191. [Google Scholar] [CrossRef] [PubMed]
- Soran, O.Z.; Feldman, A.M.; Piña, I.L.; Lamas, G.A.; Kelsey, S.F.; Selzer, F.; Pilotte, J.; Lave, J.R. Cost of medical services in older patients with heart failure: Those receiving enhanced monitoring using a computer-based telephonic monitoring system compared with those in usual care: The heart failure home care trial. J. Card. Fail. 2010, 16, 859–866. [Google Scholar] [CrossRef]
- Taylor, A.; Morris, G.; Pech, J.; Rechter, S.; Carati, C.; Kidd, M.R. Home telehealth video conferencing: Perceptions and performance. JMIR MHealth UHealth 2015, 3, e4666. [Google Scholar] [CrossRef] [PubMed]
- Chiu, K.H.; Yang, Y.Y. Remote monitoring of health status of the elderly at home in Taiwan. Telemed. E-Health 2010, 16, 717–726. [Google Scholar] [CrossRef]
- Wilson, D.J.; Mitchell, J.M.; Kemp, B.J.; Adkins, R.H.; Mann, W. Effects of assistive technology on functional decline in people aging with a disability. Assist. Technol. 2009, 21, 208–217. [Google Scholar] [CrossRef]
- Choi, K.S.; Chan, S.H.; Ho, C.L.; Matejak, M. Development of a healthcare information system for community care of older adults and evaluation of its acceptance and usability. Digit. Health 2022, 8, 20552076221109083. [Google Scholar] [CrossRef]
- Cheek, J.; Ballantyne, A.; Roder-Allen, G. Factors influencing the decision of older people living in independent units to enter the acute care system. J. Clin. Nurs. 2005, 14, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Wormald, H.; Waters, H.; Sleap, M.; Ingle, L. Participants’ perceptions of a lifestyle approach to promoting physical activity: Targeting deprived communities in Kingston-upon-Hull. BMC Public Health 2006, 6, 202. [Google Scholar] [CrossRef] [PubMed]
- Cheek, J.; Ballantyne, A.; Byers, L.; Quan, J. From retirement village to residential aged care: What older people and their families say. Health Soc. Care Community 2007, 15, 8–17. [Google Scholar] [CrossRef]
- Company, T.B.R. Elderly Care Services Global Market Report 2025—By Service Type. Available online: https://www.thebusinessresearchcompany.com/report/elderly-care-services-global-market-report#:~:text=The%20elderly%20care%20services%20market%20size%20has%20grown%20strongly%20in,(CAGR)%20of%208.4%25 (accessed on 25 April 2025).
- Fontanesi, J.; Shefer, A.M.; Fishbein, D.B.; Bennett, N.M.; De Guire, M.; Kopald, D.; Holcomb, K.; Stryker, D.W.; Coleman, M.S. Operational conditions affecting the vaccination of older adults. Am. J. Prev. Med. 2004, 26, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Onder, G.; Landi, F.; Gambassi, G.; Liperoti, R.; Soldato, M.; Catananti, C.; Finne-Soveri, H.; Katona, C.; Carpenter, I.; Bernabei, R.; et al. Association between pain and depression among older adults in Europe: Results from the Aged in Home Care (AdHOC) project: A cross-sectional study. J. Clin. Psychiatry 2005, 66, 982–988. [Google Scholar] [CrossRef]
- Coll-Planas, L.; Kron, M.; Sander, S.; Rißmann, U.; Becker, C.; Nikolaus, T. Accidental falls among community-dwelling older adults. Z. Für Gerontol. Und Geriatr. 2006, 39, 277–282. [Google Scholar] [CrossRef]
- Shipton, D.; Glazier, R.H.; Guan, J.; Badley, E.M. Effects of use of specialty services on disease-modifying antirheumatic drug use in the treatment of rheumatoid arthritis in an insured elderly population. Med Care 2004, 42, 907–913. [Google Scholar] [CrossRef]
- Ngwakongnwi, E.; Hemmelgarn, B.; Quan, H. Documentation of preventive screening interventions by general practitioners: A retrospective chart audit. BMC Fam. Pract. 2010, 11, 21. [Google Scholar] [CrossRef]
- Della Mea, V.; Popescu, M.H.; Gonano, D.; Petaros, T.; Emili, I.; Fattori, M.G. A communication infrastructure for the health and social care internet of things: Proof-of-concept study. JMIR Med Informatics 2020, 8, e14583. [Google Scholar] [CrossRef]
- Sheeran, T.; Rabinowitz, T.; Lotterman, J.; Reilly, C.F.; Brown, S.; Donehower, P.; Ellsworth, E.; Amour, J.L.; Bruce, M.L. Feasibility and impact of telemonitor-based depression care management for geriatric homecare patients. Telemed. E-Health 2011, 17, 620–626. [Google Scholar] [CrossRef]
- Aggar, C.; Sorwar, G.; Seton, C.; Penman, O.; Ward, A. Smart home technology to support older people’s quality of life: A longitudinal pilot study. Int. J. Older People Nurs. 2023, 18, e12489. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chau, K.Y.; Liu, X.; Wan, Y. The progress of smart elderly care research: A scientometric analysis based on CNKI and WOS. Int. J. Environ. Res. Public Health 2023, 20, 1086. [Google Scholar] [CrossRef]
- Czaja, S.J.; Sharit, J.; Lee, C.C.; Nair, S.N.; Hernández, M.A.; Arana, N.; Fu, S.H. Factors influencing use of an e-health website in a community sample of older adults. J. Am. Med Informatics Assoc. 2013, 20, 277–284. [Google Scholar] [CrossRef]
- Sheng, B.; Huang, L.; Wang, X.; Zhuang, J.; Tang, L.; Deng, C.; Zhang, Y. Identification of knee osteoarthritis based on bayesian network: Pilot study. JMIR Med Informatics 2019, 7, e13562. [Google Scholar] [CrossRef]
- Lam, H.Y.; Ho, G.T.S.; Mo, D.Y.; Tang, V. Enhancing data-driven elderly appointment services in domestic care communities under COVID-19. Ind. Manag. Data Syst. 2021, 121, 1552–1576. [Google Scholar] [CrossRef]
- Zhou, M.; Zha, F.; Liu, F.; Zhou, J.; Liu, X.; Li, J.; Yang, Q.; Zhang, Z.; Xiong, F.; Hou, D.; et al. Long-term care status for the elderly with different levels of physical ability: A cross-sectional survey in first-tier cities of China. BMC Health Serv. Res. 2023, 23, 953. [Google Scholar] [CrossRef] [PubMed]
- Dai, B. The old age health security in rural China: Where to go? Int. J. Equity Health 2015, 14, 119. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Hamilton, M.; Peisah, C.; Anstey, K.J.; Sinclair, C. Navigating community-based aged care services from the consumer perspective: A scoping review. Gerontol. 2024, 64, gnad017. [Google Scholar] [CrossRef]
- Matthew-Maich, N.; Harris, L.; Ploeg, J.; Markle-Reid, M.; Valaitis, R.; Ibrahim, S.; Gafni, A.; Isaacs, S. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: A scoping review. JMIR MHealth UHealth 2016, 4, e5127. [Google Scholar] [CrossRef]
- Wang, W.; Lu, C. Visualization analysis of big data research based on Citespace. Soft Comput. 2020, 24, 8173–8186. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inf. Sci. Technol. 2006, 57, 359–377. [Google Scholar] [CrossRef]
- Oladinrin, O.; Gomis, K.; Jayantha, W.M.; Obi, L.; Rana, M.Q. Scientometric analysis of global scientific literature on aging in place. Int. J. Environ. Res. Public Health 2021, 18, 12468. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Yao, Q.; An, N. The Evolution, Hotspots, and Trends in Research on Facilities of Combined Medical and Nursing Care for the Elderly. Buildings 2022, 12, 2132. [Google Scholar] [CrossRef]
- Ding, X.; Yang, Z. Knowledge mapping of platform research: A visual analysis using VOSviewer and CiteSpace. Electron. Commer. Res. 2022, 22, 787–809. [Google Scholar] [CrossRef]
- Liao, J.; Cui, X.; Kim, H. Mapping a decade of smart homes for the elderly in web of science: A scientometric review in citespace. Buildings 2023, 13, 1581. [Google Scholar] [CrossRef]
- Guo, P.; Tian, W.; Li, H.; Zhang, G.; Li, J. Global characteristics and trends of research on construction dust: Based on bibliometric and visualized analysis. Environ. Sci. Pollut. Res. 2020, 27, 37773–37789. [Google Scholar] [CrossRef]
- Yenişehir, S. Artificial intelligence based on falling in older people: A bibliometric analysis. Aging Med. 2024, 7, 162–170. [Google Scholar] [CrossRef]
- Hong, Y.K.; Wang, Z.Y.; Cho, J.Y. Global research trends on smart homes for older adults: Bibliometric and scientometric analyses. Int. J. Environ. Res. Public Health 2022, 19, 14821. [Google Scholar] [CrossRef]
- Research, M. Charticulator. Available online: https://donghaoren.org/charticulator/ (accessed on 25 April 2025).
- Lab, S. Scimago Graphica. Available online: https://www.graphica.app/ (accessed on 25 April 2025).
- Pranckutė, R. Web of Science (WoS) and Scopus: The titans of bibliographic information in today’s academic world. Publications 2021, 9, 12. [Google Scholar] [CrossRef]
- Moral-Muñoz, J.A.; Herrera-Viedma, E.; Santisteban-Espejo, A.; Cobo, M.J. Software tools for conducting bibliometric analysis in science: An up-to-date review. Prof. De La Inf. 2020, 29, e290103. [Google Scholar] [CrossRef]
- Brusco, M.; Nazeran, H. Digital phonocardiography: A PDA-based approach. In Proceedings of the The 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; IEEE: Piscataway Township, NJ, USA, 2004; Volume 1, pp. 2299–2302. [Google Scholar] [CrossRef]
- Loane, D.; Flanagan, G.; De Siun, A.; Mc Namara, E.; Kenny, S. Nutrition in the community–an exploratory study of oral nutritional supplements in a health board area in Ireland. J. Hum. Nutr. Diet. 2004, 17, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Kim, I.; Lee, S.; Yu, S. Information and Communication Technology-Based Application for Cognitive Behavioral Therapy among Community-Dwelling Older Adults with Insomnia: Development and Validation Study. Healthcare 2024, 12, 106. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Park, S.; Cho, M.h.; Kang, J.W.; Kim, M.; Choi, S.; Kim, S.g.; Choi, J.h.; Han, K.; Kim, C.O.; et al. Development of a web-based care networking system to support visiting healthcare professionals in the community. BMC Health Serv. Res. 2023, 23, 1427. [Google Scholar] [CrossRef] [PubMed]
- McGill, A.; Salehi, V.; McCloskey, R.; Smith, D.; Veitch, B. Mapping the way: Functional modelling for community-based integrated care for older people. Health Res. Policy Syst. 2024, 22, 103. [Google Scholar] [CrossRef]
- Xue, C.; Xu, L.; Yang, K.; Wang, J.; Xie, X.; Zhou, W.; Liu, Q.; Deng, R.; Wang, L. Evaluating the effectiveness and feasibility of a digital health intervention to community-based rehabilitation in older adults: A cluster randomized controlled trial study protocol. Digit. Health 2024, 10, 20552076241252648. [Google Scholar] [CrossRef] [PubMed]
- Tungu, M.; Sirili, N.; Frumence, G.; Kagaigai, A.; Anaeli, A.; Mwangu, M.A.; Kiwara, A.D. Health care prioritization process for the elderly in rural Tanzania under decentralized system: Prospects and challenges. PLoS ONE 2024, 19, e0304243. [Google Scholar] [CrossRef]
- Liu, S.; Wang, Y.; Zhou, D.; Kang, Y. Two-step floating catchment area model-based evaluation of community care facilities’ spatial accessibility in Xi’an, China. Int. J. Environ. Res. Public Health 2020, 17, 5086. [Google Scholar] [CrossRef]
- Choi, N.G.; DiNitto, D.M. Internet use among older adults: Association with health needs, psychological capital, and social capital. J. Med Internet Res. 2013, 15, e2333. [Google Scholar] [CrossRef]
- Gazni, A.; Sugimoto, C.R.; Didegah, F. Mapping world scientific collaboration: Authors, institutions, and countries. J. Am. Soc. Inf. Sci. Technol. 2012, 63, 323–335. [Google Scholar] [CrossRef]
- McQuown, C.M.; Snell, K.T.; Abbate, L.M.; Jetter, E.M.; Blatnik, J.K.; Ragsdale, L.C. Telehealth for geriatric post-emergency department visits to promote age-friendly care. Health Serv. Res. 2023, 58, 16–25. [Google Scholar] [CrossRef]
- Zhou, B.; Deng, Q.; Zhou, S.; Zhuo, D. Health care in future community: Innovatively discover and respond to the needs of today’s seniors. Front. Public Health 2023, 11, 1302493. [Google Scholar] [CrossRef]
- Ma, Y.; Zou, G.; Shin, J.h.; Kang, Y.; Gao, S.; Siu, K.W.M.; Zhang, S. Locating community-based comprehensive service facilities for older adults using the GIS-NEMA method in Harbin, China. J. Urban Plan. Dev. 2021, 147, 05021010. [Google Scholar] [CrossRef]
- Robinson, E.; Dickins, M.; Lad, L.; Beard, S.; McGill, D.; Hayes, J.; Fabri, A.M.; Wade, H.; Meyer, C.; Lowthian, J.A. Adaptation and Implementation of a Volunteer-Delivered, Telephone-Based, Social Support Program HOW-RU? During the COVID-19 Pandemic: A Pragmatic Study. Gerontol. 2024, 64, gnae034. [Google Scholar] [CrossRef] [PubMed]
- Steiner-Lim, G.Z.; Karamacoska, D.; Abramov, G.; Dubois, S.; Harley, A.; McDonald, K.; Hohenberg, M.I. “I’m On My Own, I Need Support”: Needs Assessment of Community Aged Care Services. Int. J. Integr. Care 2023, 23, 14. [Google Scholar] [CrossRef]
- Crocker, T.F.; Ensor, J.; Lam, N.; Jordão, M.; Bajpai, R.; Bond, M.; Forster, A.; Riley, R.D.; Andre, D.; Brundle, C.; et al. Community based complex interventions to sustain independence in older people: Systematic review and network meta-analysis. bmj 2024, 384, e077764. [Google Scholar] [CrossRef] [PubMed]
- Iris, M.; Ridings, J.W.; Conrad, K.J. The development of a conceptual model for understanding elder self-neglect. Gerontol. 2010, 50, 303–315. [Google Scholar] [CrossRef]
- Findlay, L.; Kellett, R.; Lubbe, S.; Wand, A.P. Pathways to community living in practice: Local development and adaptation within an older peoples mental health service. Australas. Psychiatry 2023, 31, 824–829. [Google Scholar] [CrossRef] [PubMed]
- Willging, C.E.; Sommerfeld, D.H.; Jaramillo, E.T.; Lujan, E.; Bly, R.S.; Debenport, E.K.; Verney, S.P.; Lujan, R. Improving Native American elder access to and use of health care through effective health system navigation. BMC Health Serv. Res. 2018, 18, 464. [Google Scholar] [CrossRef]
- Marra, K.V.; Wagley, S.; Kuperwaser, M.C.; Campo, R.; Arroyo, J.G. Care of older adults: Role of primary care physicians in the treatment of cataracts and macular degeneration. J. Am. Geriatr. Soc. 2016, 64, 369–377. [Google Scholar] [CrossRef]
- Murray, E.; Burns, J.; May, C.; Finch, T.; O’Donnell, C.; Wallace, P.; Mair, F. Why is it difficult to implement e-health initiatives? A qualitative study. Implement. Sci. 2011, 6, 6. [Google Scholar] [CrossRef]
- Iliffe, S.; Kharicha, K.; Harari, D.; Swift, C.; Goodman, C.; Manthorpe, J. User involvement in the development of a health promotion technology for older people: Findings from the SWISH project. Health Soc. Care Community 2010, 18, 147–159. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, M.F.; Davagnino, J.; Hastings, S.N.; Sloane, R.; Kamholz, B.; Twersky, J. Preliminary data from the Caring for Older Adults and Caregivers at Home (COACH) program: A care coordination program for home-based dementia care and caregiver support in a Veterans Affairs medical center. J. Am. Geriatr. Soc. 2015, 63, 1203–1208. [Google Scholar] [CrossRef] [PubMed]
- Gustavson, A.M.; Falvey, J.R.; LeDoux, C.V.; Stevens-Lapsley, J.E. Stakeholder and data-driven fall screen in a program of all-inclusive care for the elderly: Quality improvement initiative. J. Geriatr. Phys. Ther. 2022, 45, 154–159. [Google Scholar] [CrossRef]
- Dixon, B.E.; Schwartzkopf, A.L.; Guerrero, V.M.; May, J.; Koufacos, N.S.; Bean, A.M.; Penrod, J.D.; Schubert, C.C.; Boockvar, K.S. Regional data exchange to improve care for veterans after non-VA hospitalization: A randomized controlled trial. BMC Med Informatics Decis. Mak. 2019, 19, 125. [Google Scholar] [CrossRef]
- Hirdes, J.P.; Morris, J.N.; Perlman, C.M.; Saari, M.; Betini, G.S.; Franco-Martin, M.A.; van Hout, H.; Stewart, S.L.; Ferris, J. Mood Disturbances Across the Continuum of Care Based on Self-Report and Clinician Rated Measures in the interRAI Suite of Assessment Instruments. Front. Psychiatry 2022, 13, 787463. [Google Scholar] [CrossRef] [PubMed]
- Giosa, J.L.; Saari, M.; Holyoke, P.; Hirdes, J.P.; Heckman, G.A. Developing an evidence-informed model of long-term life care at home for older adults with medical, functional and/or social care needs in Ontario, Canada: A mixed methods study protocol. BMJ Open 2022, 12, e060339. [Google Scholar] [CrossRef]
- Ludlow, K.; Westbrook, J.; Jorgensen, M.; Lind, K.E.; Baysari, M.T.; Gray, L.C.; Day, R.O.; Ratcliffe, J.; Lord, S.R.; Georgiou, A.; et al. Co-designing a dashboard of predictive analytics and decision support to drive care quality and client outcomes in aged care: A mixed-method study protocol. BMJ Open 2021, 11, e048657. [Google Scholar] [CrossRef]
- Siette, J.; Georgiou, A.; Jorgensen, M.; O’Donnell, C.; Westbrook, J. Integrating social engagement instruments into Australian community aged care assessments to enhance service provision. Health Soc. Care Community 2018, 26, 810–818. [Google Scholar] [CrossRef]
- Foebel, A.D.; Hirdes, J.P.; Heckman, G.A. Caregiver status affects medication adherence among older home care clients with heart failure. Aging Clin. Exp. Res. 2012, 24, 718–721. [Google Scholar] [CrossRef]
- Brett, L.; Jorgensen, M.; Myton, R.; Georgiou, A.; Westbrook, J.I. Characteristics of older Australian community aged care clients who fall: Incidents reported by care staff. Health Soc. Care Community 2022, 30, 469–475. [Google Scholar] [CrossRef]
- Jorgensen, M.; Siette, J.; Georgiou, A.; Warland, A.; Westbrook, J. Modeling the association between home care service use and entry into residential aged care: A cohort study using routinely collected data. J. Am. Med Dir. Assoc. 2018, 19, 117–121. [Google Scholar] [CrossRef]
- King, G.; O’Donnell, C.; Boddy, D.; Smith, F.; Heaney, D.; Mair, F.S. Boundaries and e-health implementation in health and social care. BMC Med Informatics Decis. Mak. 2012, 12, 100. [Google Scholar] [CrossRef] [PubMed]
- Gregory, D. Healthcare Goes Digital: Designing for the Convergence of the Digital and Physical Environment—Implications for Design Professionals. Herd: Health Environ. Res. Des. J. 2022, 15, 43–48. [Google Scholar] [CrossRef]
- Zwack, C.C.; Haghani, M.; Hollings, M.; Zhang, L.; Gauci, S.; Gallagher, R.; Redfern, J. The evolution of digital health technologies in cardiovascular disease research. NPJ Digit. Med. 2023, 6, 1. [Google Scholar] [CrossRef]
- Blasi, F.; Caiani, E.G.; Cereda, M.G.; Donetti, D.; Montorsi, M.; Panella, V.; Panina, G.; Pelagalli, F.; Speroni, E. Six drivers to face the XXI century challenges and build the new healthcare system:“La Salute in Movimento” Manifesto. Front. Public Health 2022, 10, 876625. [Google Scholar] [CrossRef]
- Lievevrouw, E.; Marelli, L.; Van Hoyweghen, I. Weaving EU digital health policy into national healthcare practices. The making of a reimbursement standard for digital health technologies in Belgium. Soc. Sci. Med. 2024, 346, 116620. [Google Scholar] [CrossRef] [PubMed]
- Iakovleva, T.; Oftedal, E.; Bessant, J. Changing role of users—innovating responsibly in Digital Health. Sustainability 2021, 13, 1616. [Google Scholar] [CrossRef]
- Chen, X.; Chen, J.; Wu, D.; Xie, Y.; Li, J. Mapping the research trends by co-word analysis based on keywords from funded project. Procedia Comput. Sci. 2016, 91, 547–555. [Google Scholar] [CrossRef]
- Sedighi, M. Application of word co-occurrence analysis method in mapping of the scientific fields (case study: The field of Informetrics). Libr. Rev. 2016, 65, 52–64. [Google Scholar] [CrossRef]
- Northwood, M.; Saari, M.; Heckman, G.; Alexander, T.; Eastway, B.; Gerantonis, P.; Gillies, D.; Gregg, S.; McKinnon Wilson, J.; Morrison, A.; et al. Use of an electronic wellness instrument in the integrated health and social care of older adults: A group concept mapping study. BMC Health Serv. Res. 2024, 24, 864. [Google Scholar] [CrossRef]
- Cui, L.; Tong, Z.; Wang, R.; Fang, X.; Liu, L. Using an internet-based platform to provide online and offline healthcare services for discharged patients. BMC Nurs. 2024, 23, 486. [Google Scholar] [CrossRef] [PubMed]
- Jaramillo, E.T. Place-based strengths and vulnerabilities for mental wellness among rural minority older adults: An intervention development study protocol. BMJ Open 2024, 14, e088348. [Google Scholar] [CrossRef]
- Jiang, Z.; Liu, H.; Deng, J.; Ye, Y.; Li, D. Influence of intergenerational support on the mental health of older people in China. PLoS ONE 2024, 19, e0299986. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Dong, L. Payment Behavioral Response Mechanisms for All-Age Retrofitting of Older Communities: A Study among Chinese Residents. Behav. Sci. 2023, 13, 925. [Google Scholar] [CrossRef] [PubMed]
- Tao, X.; Jiang, W.; Wang, J.; Yang, S. Aged Care Projects Evaluation Research Based on the Self-Adaptive Consensus Emergence Model Driven by the Social Learning Mechanism. Expert Syst. Appl. 2024, 238, 121699. [Google Scholar] [CrossRef]
- Sharma, P.; Dilip, T.; Mishra, U.S.; Kulkarni, A. The lifetime risk of developing type II diabetes in an urban community in Mumbai: Findings from a ten-year retrospective cohort study. BMC Public Health 2023, 23, 1673. [Google Scholar] [CrossRef]
- Chang, Y.C.; Chang, S.C.; Chung, K.P.; Tu, Y.K.; Chen, Y.M. Development of a long-term care service integration self-assessment tool. J. Interprofessional Care 2024, 38, 807–817. [Google Scholar] [CrossRef]
- Balqis-Ali, N.Z.; Jawahir, S.; Chan, Y.M.; Lim, A.W.Y.; Azlan, U.W.; Shaffie, S.S.M.; Fun, W.H.; Lee, S.W.H. The impact of long-term care interventions on healthcare utilisation among older persons: A scoping review of reviews. BMC Geriatr. 2024, 24, 484. [Google Scholar] [CrossRef]
- Fan, L.; Xiong, Y.; Peng, Y. Assessing accessible travel satisfaction in old communities: A SEM study. Buildings 2024, 14, 1273. [Google Scholar] [CrossRef]
- Choi, H.K.; Lee, K.; Lee, S.H. Developmental study on “Smart Silver Care”: A mobile application to alleviate loneliness in older adults within the community. Healthcare 2023, 11, 2376. [Google Scholar] [CrossRef]
- Gao, F.; Languille, C.; Karzazi, K.; Guhl, M.; Boukebous, B.; Deguen, S. Efficiency of fine scale and spatial regression in modelling associations between healthcare service spatial accessibility and their utilization. Int. J. Health Geogr. 2021, 20, 22. [Google Scholar] [CrossRef] [PubMed]
- Foebel, A.; Hirdes, J.; Heckman, G.; Tyas, S.; Tjam, E. A profile of older community-dwelling home care clients with heart failure in Ontario. Health Promot. Chronic Dis. Prev. Can. 2011, 31, 49–57. Available online: https://pubmed.ncbi.nlm.nih.gov/21466754/ (accessed on 25 April 2025). [CrossRef]
- Helstrom, A.; Haratz, J.; Chen, S.; Benson, A.; Streim, J.; Oslin, D. Telephone-based management of chronic pain in older adults in an integrated care program. Int. J. Geriatr. Psychiatry 2018, 33, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.C.; Chiu, H.L.; Liu, D.; Chan, P.T.; Tseng, J.; Chen, R.; Niu, S.F.; Chou, K.R. Effect of interactive cognitive motor training on gait and balance among older adults: A randomized controlled trial. Int. J. Nurs. Stud. 2018, 82, 121–128. [Google Scholar] [CrossRef]
- Nakrem, S.; Solbjør, M.; Pettersen, I.N.; Kleiven, H.H. Care relationships at stake? Home healthcare professionals’ experiences with digital medicine dispensers—A qualitative study. BMC Health Serv. Res. 2018, 18, 26. [Google Scholar] [CrossRef]
- Tong, C.E.; Franke, T.; Larcombe, K.; Sims Gould, J. Fostering inter-agency collaboration for the delivery of community-based services for older adults. Br. J. Soc. Work 2018, 48, 390–411. [Google Scholar] [CrossRef]
- Zhou, J.; Walker, A. The need for community care among older people in China. Ageing Soc. 2016, 36, 1312–1332. [Google Scholar] [CrossRef]
- Deborah, O.M.L.; Chiu, M.Y.L.; Cao, K. Geographical accessibility of community health assist scheme general practitioners for the elderly population in Singapore: A case study on the elderly living in housing development board flats. Int. J. Environ. Res. Public Health 2018, 15, 1988. [Google Scholar] [CrossRef]
- Di Toro, A. Smart Elderly Care in China: A Preliminary Overview. In Italian Forum of Ambient Assisted Living; Springer: Berlin/Heidelberg, Germany, 2024; pp. 507–523. [Google Scholar] [CrossRef]
- Wang, H.; Chen, H.; Wang, Y. Analysis of Hot Topics Regarding Global Smart Elderly Care Research—1997–2021. China CDC Wkly. 2024, 6, 157. [Google Scholar] [CrossRef]
- Yang, C.H.; Chen, Y.C.; Hsu, W.; Chen, Y.H. Evaluation of smart long-term care information strategy portfolio decision model: The national healthcare environment in Taiwan. Ann. Oper. Res. 2023, 326, 505–536. [Google Scholar] [CrossRef]
- Papa, A.; Mital, M.; Pisano, P.; Del Giudice, M. E-health and wellbeing monitoring using smart healthcare devices: An empirical investigation. Technol. Forecast. Soc. Chang. 2020, 153, 119226. [Google Scholar] [CrossRef]
- Muzny, M.; Henriksen, A.; Giordanengo, A.; Muzik, J.; Grøttland, A.; Blixgård, H.; Hartvigsen, G.; Årsand, E. Wearable sensors with possibilities for data exchange: Analyzing status and needs of different actors in mobile health monitoring systems. Int. J. Med Informatics 2020, 133, 104017. [Google Scholar] [CrossRef]
- Cascajares, M.; Alcayde, A.; Salmerón-Manzano, E.; Manzano-Agugliaro, F. The bibliometric literature on Scopus and WoS: The medicine and environmental sciences categories as case of study. Int. J. Environ. Res. Public Health 2021, 18, 5851. [Google Scholar] [CrossRef] [PubMed]
- Gell, N.M.; Rosenberg, D.E.; Demiris, G.; LaCroix, A.Z.; Patel, K.V. Patterns of technology use among older adults with and without disabilities. Gerontol. 2015, 55, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Canham, S.L.; Fang, M.L.; Battersby, L.; Woolrych, R.; Sixsmith, J.; Ren, T.H.; Sixsmith, A. Contextual factors for aging well: Creating socially engaging spaces through the use of deliberative dialogues. Gerontol. 2018, 58, 140–148. [Google Scholar] [CrossRef]
- Philip, K.E.; Alizad, V.; Oates, A.; Donkin, D.B.; Pitsillides, C.; Syddall, S.P.; Philp, I. Development of EASY-Care, for brief standardized assessment of the health and care needs of older people; with latest information about cross-national acceptability. J. Am. Med Dir. Assoc. 2014, 15, 42–46. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Burrows, A.B.; Morris, J.N.; Simon, S.E.; Hirdes, J.P.; Phillips, C. Development of a minimum data set-based depression rating scale for use in nursing homes. Age Ageing 2000, 29, 165–172. [Google Scholar] [CrossRef]
- Morris, J.N.; Fries, B.E.; Mehr, D.R.; Hawes, C.; Phillips, C.; Mor, V.; Lipsitz, L.A. MDS cognitive performance scale©. J. Gerontol. 1994, 49, M174–M182. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontol. 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Liu, X.; Glänzel, W.; De Moor, B. A hierarchical and optimal clustering of WoS journal database by hybrid information. In Proceedings of the ISSI, Durban, South Africa, 4–7 July 2011; pp. 485–496. [Google Scholar] [CrossRef]
- Skivington, K.; Matthews, L.; Simpson, S.A.; Craig, P.; Baird, J.; Blazeby, J.M.; Boyd, K.A.; Craig, N.; French, D.P.; McIntosh, E.; et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. bmj 2021, 374, n2061. [Google Scholar] [CrossRef]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef]
- Morley, J.E.; Vellas, B.; Van Kan, G.A.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.; Doehner, W.; Evans, J.; et al. Frailty consensus: A call to action. J. Am. Med Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef]
- Bruce, M.L.; Ten Have, T.R.; Reynolds, C.F., 3rd; Katz, I.I.; Schulberg, H.C.; Mulsant, B.H.; Brown, G.K.; McAvay, G.J.; Pearson, J.L.; Alexopoulos, G.S. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. JAMA 2004, 291, 1081–1091. [Google Scholar] [CrossRef]
- May, C.R.; Finch, T.L.; Cornford, J.; Exley, C.; Gately, C.; Kirk, S.; Jenkings, K.N.; Osbourne, J.; Robinson, A.L.; Rogers, A.; et al. Integrating telecare for chronic disease management in the community: What needs to be done? BMC Health Serv. Res. 2011, 11, 131. [Google Scholar] [CrossRef] [PubMed]
- Manderson, B.; McMurray, J.; Piraino, E.; Stolee, P. Navigation roles support chronically ill older adults through healthcare transitions: A systematic review of the literature. Health Soc. Care Community 2012, 20, 113–127. [Google Scholar] [CrossRef] [PubMed]
- McGrother, C.W.; Donaldson, M.M.K.; Shaw, C.; Matthews, R.J.; Hayward, T.A.; Dallosso, H.M.; Jagger, C.; Clarke, M.; Castleden, C.M.; MRC Incontinence Study Team. Storage symptoms of the bladder: Prevalence, incidence and need for services in the UK. BJU Int. 2004, 93, 763–769. [Google Scholar] [CrossRef]
- Horrocks, S.; Somerset, M.; Stoddart, H.; Peters, T.J. What prevents older people from seeking treatment for urinary incontinence? A qualitative exploration of barriers to the use of community continence services. Fam. Pract. 2004, 21, 689–696. [Google Scholar] [CrossRef]
- Davitt, J.K.; Madigan, E.A.; Rantz, M.; Skemp, L. Aging in community: Developing a more holistic approach to enhance older adults’ well-being. Res. Gerontol. Nurs. 2016, 9, 6–13. [Google Scholar] [CrossRef]
- Trivedi, M.H.; Rush, A.J.; Wisniewski, S.R.; Nierenberg, A.A.; Warden, D.; Ritz, L.; Norquist, G.; Howland, R.H.; Lebowitz, B.; McGrath, P.J.; et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: Implications for clinical practice. Am. J. Psychiatry 2006, 163, 28–40. [Google Scholar] [CrossRef]
- Rahmawati, R.; Bajorek, B. Peer Reviewed: A Community Health Worker–Based Program for Elderly People with Hypertension in Indonesia: A Qualitative Study, 2013. Prev. Chronic Dis. 2015, 12, E175. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Liu, C.; Song, Y.; Sörensen, S. Adaptation and Validation of the Preparation for Future Care Needs Scale for Chinese Older Adults in Hong Kong. Gerontol. 2022, 62, e357–e368. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Wang, B.; Yang, X.; Pan, Y.; Feng, W.; Pei, X.; Fan, Y.; Liu, B. Can the organization of health resource integration be analyzed in terms of the current state of unmet demand for health services? take the health needs of the elderly in a place in zhejiang province, china, as an example. BMC Prim. Care 2022, 23, 288. [Google Scholar] [CrossRef]
- Hogeveen, S.; Hirdes, J.P.; Heckman, G.; Keller, H. Determinants of access of frail, community-residing older adults to geriatricians in Ontario. J. Am. Geriatr. Soc. 2023, 71, 2810–2821. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Chao, D.; Zhang, Z.; Wang, D.; Li, X.; Tian, F. Utilization of self-diagnosis health chatbots in real-world settings: Case study. J. Med Internet Res. 2021, 23, e19928. [Google Scholar] [CrossRef]
- Ghosh, S.; Ghosh, S.K. Feel: Federated learning framework for elderly healthcare using edge-iomt. IEEE Trans. Comput. Soc. Syst. 2023, 10, 1800–1809. [Google Scholar] [CrossRef]
- Lima, M.R.; Wairagkar, M.; Gupta, M.; y Baena, F.R.; Barnaghi, P.; Sharp, D.J.; Vaidyanathan, R. Conversational affective social robots for ageing and dementia support. IEEE Trans. Cogn. Dev. Syst. 2021, 14, 1378–1397. [Google Scholar] [CrossRef]
- Wilmink, G.; Dupey, K.; Alkire, S.; Grote, J.; Zobel, G.; Fillit, H.M.; Movva, S. Artificial intelligence–powered digital health platform and wearable devices improve outcomes for older adults in assisted living communities: Pilot intervention study. JMIR Aging 2020, 3, e19554. [Google Scholar] [CrossRef]
- Wong, A.M.; Chang, W.H.; Ke, P.C.; Huang, C.K.; Tsai, T.H.; Chang, H.T.; Shieh, W.Y.; Chan, H.L.; Chen, C.K.; Pei, Y.C. Technology acceptance for an Intelligent Comprehensive Interactive Care (ICIC) system for care of the elderly: A survey-questionnaire study. PLoS ONE 2012. [Google Scholar] [CrossRef]
- Vergouw, J.W.; Smits-Pelser, H.; Kars, M.C.; van Houwelingen, T.; van Os-Medendorp, H.; Kort, H.; Bleijenberg, N. Needs, barriers and facilitators of older adults towards eHealth in general practice: A qualitative study. Prim. Health Care Res. Dev. 2020, 21, e54. [Google Scholar] [CrossRef]
- Kim, Y.S.; Lee, J.; Moon, Y.; Kim, H.J.; Shin, J.; Park, J.M.; Uhm, K.E.; Kim, K.J.; Yoo, J.A.; Oh, Y.K.; et al. Development of a senior-specific, citizen-oriented healthcare service system in South Korea based on the Canadian 48/6 model of care. BMC Geriatr. 2020, 20, 32. [Google Scholar] [CrossRef] [PubMed]
- Askari, M.; Klaver, N.S.; van Gestel, T.J.; van de Klundert, J. Intention to use medical apps among older adults in the Netherlands: Cross-sectional study. J. Med Internet Res. 2020, 22, e18080. [Google Scholar] [CrossRef] [PubMed]
- Jamerson, B.D.; Fillenbaum, G.G.; Sloane, R.; Morey, M.C. A new method of identifying characteristics of needing help to take medications in an older representative community-dwelling population: The Older Adults Medication Assist Scale. J. Am. Geriatr. Soc. 2016, 64, 1195–1202. [Google Scholar] [CrossRef] [PubMed]
- Yamout, Y.; Yeasar, T.S.; Iqbal, S.; Zulkernine, M. Beyond smart homes: An in-depth analysis of smart aging care system security. ACM Comput. Surv. 2023, 56, 1–35. [Google Scholar] [CrossRef]
- Zhang, X.; Gao, X.; Wu, D.; Xu, Z.; Wang, H. The Role of Big Data in Aging and Older People’s Health Research: A Systematic Review and Ecological Framework. Sustainability 2021, 13, 11587. [Google Scholar] [CrossRef]
- Huxhold, O.; Hees, E.; Webster, N.J. Towards bridging the grey digital divide: Changes in internet access and its predictors from 2002 to 2014 in Germany. Eur. J. Ageing 2020, 17, 271–280. [Google Scholar] [CrossRef]
- Yang, J.; Du, P. Gender, capital endowment and digital exclusion of older people in China. Ageing Soc. 2021, 41, 2502–2526. [Google Scholar] [CrossRef]
- Tuisku, O.; Parjanen, S.; Hyypiä, M.; Pekkarinen, S. Managing changes in the environment of human–robot interaction and welfare services. Inf. Technol. Manag. 2024, 25, 1–18. [Google Scholar] [CrossRef]
- Wangmo, T.; Lipps, M.; Kressig, R.W.; Ienca, M. Ethical concerns with the use of intelligent assistive technology: Findings from a qualitative study with professional stakeholders. BMC Med. Ethics 2019, 20, 98. [Google Scholar] [CrossRef]
- Zhu, J.; Shi, K.; Yang, C.; Niu, Y.; Zeng, Y.; Zhang, N.; Liu, T.; Chu, C.H. Ethical issues of smart home-based elderly care: A scoping review. J. Nurs. Manag. 2022, 30, 3686–3699. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Strategy on Digital Health 2020–2025. Available online: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (accessed on 25 April 2025).
- International Council of Nurses. ICN Position Statement on Digital Health. Adopted by the ICN Board of Directors. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC11638528/ (accessed on 25 April 2025).
- Australian Digital Health Agency. National Digital Health Strategy 2023–2028. Budget Allocation: AUD 325.7 Million. Available online: https://www.digitalhealth.gov.au/sites/default/files/documents/national-digital-health-strategy-2023-2028.pdf (accessed on 25 April 2025).
- World Health Organization. Global Report on Digital Health. Available online: https://iris.who.int/bitstream/handle/10665/373581/9789240081949-eng.pdf (accessed on 25 April 2025).
- Centers for Disease Control and Prevention. Global Health Security Strategy 2022. Available online: https://www.cdc.gov/global-health/media/pdfs/GDHS_Strategy2022_REV_508.pdf (accessed on 25 April 2025).





| Topic | Search Terms |
|---|---|
| Information | Information OR Information Technology Integration OR |
| Computerization OR Digitalization OR Automation OR Electronic | |
| Data Processing OR Data Processing OR Information Management | |
| OR Information Systems Development OR Software Development | |
| OR Hardware Integration | |
| Pension | Pension OR Old-age OR Endowment OR Senior OR Retirement |
| OR Elderly Care OR Aged Elderly Service OR Superannuation | |
| OR Nursing OR Old Age | |
| Community | Community Service OR Community-based Services OR |
| Communal Services OR Community-service OR | |
| Community-based Service |
| Rank | Journals | Numbers | Country | IF(JCR2023) |
|---|---|---|---|---|
| 1 | BMJ OPEN | 24 | United Kingdom | 2.4 |
| 2 | BMC HEALTH SERVICES RESEARCH | 19 | United Kingdom | 2.7 |
| 3 | BMC GERIATRICS | 17 | United Kingdom | 3.4 |
| 4 | HEALTH & SOCIAL CARE IN THE COMMUNITY | 11 | United Kingdom | 2.0 |
| 5 | JOURNAL OF THE AMERICAN GERIATRICS SOCIETY | 10 | USA | 4.3 |
| 6 | FRONTIERS IN PUBLIC HEALTH | 10 | Switzerland | 3.0 |
| 7 | BMC PUBLIC HEALTH | 9 | United Kingdom | 3.5 |
| 8 | GERONTOLOGIST | 8 | USA | 4.6 |
| 9 | JOURNAL OF MEDICAL INTERNET RESEARCH | 8 | Canada | 5.8 |
| 10 | PLOS ONE | 7 | USA | 2.9 |
| Rank | Country | Numbers | Citations | Average Citations | H-Index |
|---|---|---|---|---|---|
| 1 | USA | 129 | 2684 | 20.81 | 30 |
| 2 | China | 86 | 762 | 8.86 | 15 |
| 3 | Australia | 68 | 801 | 11.78 | 16 |
| 4 | Canada | 57 | 723 | 12.68 | 16 |
| 5 | United Kingdom | 53 | 1128 | 21.28 | 19 |
| 6 | Netherlands | 16 | 353 | 22.06 | 11 |
| 7 | South Korea | 15 | 148 | 9.87 | 7 |
| 8 | Sweden | 11 | 169 | 15.36 | 6 |
| 9 | Belgium | 9 | 165 | 18.33 | 6 |
| 10 | Japan | 9 | 49 | 5.44 | 4 |
| Rank | Organization | Numbers | Citations | Average Citations | H-Index |
|---|---|---|---|---|---|
| 1 | UNIVERSITY OF SYDNEY | 16 | 216 | 13.50 | 7 |
| 2 | UNIVERSITY OF CALIFORNIA SYSTEM | 13 | 250 | 19.23 | 7 |
| 3 | UNIVERSITY OF LONDON | 13 | 485 | 37.31 | 10 |
| 4 | US DEPARTMENT OF VETERANS AFFAIRS | 13 | 156 | 12.00 | 7 |
| 5 | VETERANS HEALTH ADMINISTRATION VHA | 13 | 156 | 12.00 | 7 |
| 6 | FLINDERS UNIVERSITY SOUTH AUSTRALIA | 11 | 100 | 9.09 | 5 |
| 7 | MONASH UNIVERSITY | 11 | 61 | 5.55 | 5 |
| 8 | UNIVERSITY OF TORONTO | 11 | 84 | 7.64 | 4 |
| 9 | GERIATRIC RESEARCH EDUCATION CLINICAL CENTER | 10 | 173 | 17.30 | 7 |
| 10 | MCMASTER UNIVERSITY | 10 | 143 | 14.30 | 6 |
| Rank | Author | Numbers | Citations | Average Citations | H-Index |
|---|---|---|---|---|---|
| 1 | Hirdes, John | 5 | 52 | 10.40 | 3 |
| 2 | Heckman, George A. | 5 | 50 | 10.00 | 3 |
| 3 | Georgiou, Andrew | 4 | 48 | 12.00 | 3 |
| 4 | Jorgensen, Mikaela | 4 | 48 | 12.00 | 3 |
| 5 | Westbrook, Johanna | 4 | 48 | 12.00 | 3 |
| 6 | O’Donnell, Catherine | 3 | 202 | 67.33 | 3 |
| 7 | Bruce, Martha L. | 3 | 97 | 32.33 | 3 |
| 8 | Bleijenberg, Nienke | 3 | 79 | 26.33 | 2 |
| 9 | Wallin, Lars | 3 | 74 | 24.67 | 2 |
| 10 | Siette, Joyce | 3 | 45 | 15.00 | 3 |
| Rank | Cited Journals | Citations | Country | IF(JCR2023) |
|---|---|---|---|---|
| 1 | JAM GERIATR SOC | 417 | USA | 4.3 |
| 2 | GERONTOLOGIST | 231 | USA | 4.6 |
| 3 | JAMA-J AM MED ASSOC | 193 | USA | 63.1 |
| 4 | BMC HEALTH SERV RES | 172 | United Kingdom | 2.7 |
| 5 | AGE AGEING | 170 | United Kingdom | 6.0 |
| 6 | LANCET | 168 | United Kingdom | 98.4 |
| 7 | SOC SCI MED | 164 | United Kingdom | 4.9 |
| 8 | BMC GERIATR | 158 | United Kingdom | 3.4 |
| 9 | PLOS ONE | 157 | USA | 2.9 |
| 10 | BMJ-BRIT MED J | 145 | United Kingdom | 93.6 |
| Rank | Cited Authors | Total Link Strength | Citations |
|---|---|---|---|
| 1 | BRAUN, V | 44 | 34 |
| 2 | HIRDES, JP | 141 | 30 |
| 3 | MORRIS, JN | 142 | 28 |
| 4 | FOLSTEIN, MF | 47 | 25 |
| 5 | LAWTON, MP | 30 | 22 |
| 6 | PATTON, MQ | 35 | 20 |
| 7 | CRESWELL, JW | 34 | 18 |
| 8 | WARE, JE | 30 | 18 |
| 9 | COLEMAN, EA | 39 | 16 |
| 10 | VENKATESH, V | 33 | 16 |
| Rank | Title | Journal | Author(s) | Citations |
|---|---|---|---|---|
| 1 | A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance [118] | BMJ-BRITISH MEDICAL JOURNAL | Skivington K | 4 |
| 2 | Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019 [119] | LANCET | Cieza A | 4 |
| 3 | Frailty Consensus: A Call to Action [120] | JOURNAL OF THE AMERICAN MEDICAL DIRECTORS ASSOCIATION | Morley JE | 3 |
| 4 | Reducing suicidal ideation and depressive symptoms in depressed older primary care patients—A randomized controlled trial [121] | JAMA-JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION | Bruce ML | 2 |
| 5 | Integrating telecare for chronic disease management in the community: What needs to be done? [122] | BMC HEALTH SERVICES RESEARCH | May CR | 2 |
| 6 | Navigation roles support chronically ill older adults through healthcare transitions: a systematic review of the literature [123] | HEALTH & SOCIAL CARE IN THE COMMUNITY | Manderson B | 2 |
| 7 | Storage symptoms of the bladder: prevalence, incidence and need for services in the UK [124] | BJU INTERNATIONAL | McGrother CW | 2 |
| 8 | What prevents older people from seeking treatment for urinary incontinence? A qualitative exploration of barriers to the use of community continence services [125] | FAMILY PRACTICE | Horrocks S | 2 |
| 9 | Aging in Community Developing a More Holistic Approach to Enhance Older Adults’ Well-Being [126] | RESEARCH IN GERONTOLOGICAL NURSING | Davitt JK | 2 |
| 10 | Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: Implications for clinical practice [127] | AMERICAN JOURNAL OF PSYCHIATRY | Trivedi MH | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Shao, Z.; Tian, Z.; Chen, J. Advancements and Innovation Trends of Information Technology Empowering Elderly Care Community Services Based on CiteSpace and VOSViewer. Healthcare 2025, 13, 1628. https://doi.org/10.3390/healthcare13131628
Wang Y, Shao Z, Tian Z, Chen J. Advancements and Innovation Trends of Information Technology Empowering Elderly Care Community Services Based on CiteSpace and VOSViewer. Healthcare. 2025; 13(13):1628. https://doi.org/10.3390/healthcare13131628
Chicago/Turabian StyleWang, Yanxiu, Zichun Shao, Zhen Tian, and Junming Chen. 2025. "Advancements and Innovation Trends of Information Technology Empowering Elderly Care Community Services Based on CiteSpace and VOSViewer" Healthcare 13, no. 13: 1628. https://doi.org/10.3390/healthcare13131628
APA StyleWang, Y., Shao, Z., Tian, Z., & Chen, J. (2025). Advancements and Innovation Trends of Information Technology Empowering Elderly Care Community Services Based on CiteSpace and VOSViewer. Healthcare, 13(13), 1628. https://doi.org/10.3390/healthcare13131628








