Mapping Research Trends on the Implications of Telemedicine for Healthcare Professionals: A Comprehensive Bibliometric Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
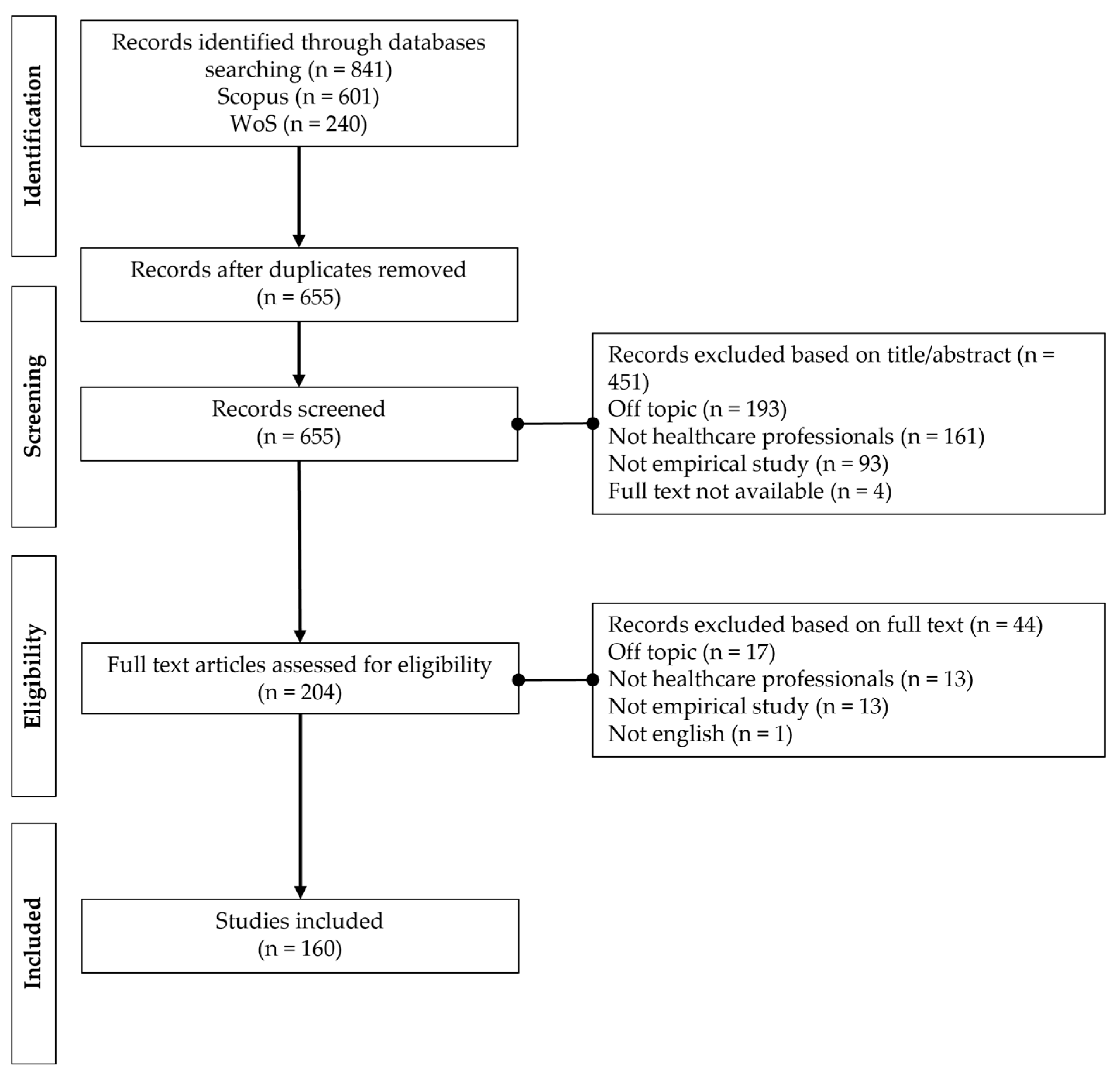
2.2. Inclusion and Exclusion Criteria
2.3. Screening Process
2.4. Data Analysis
3. Results
3.1. Data Description
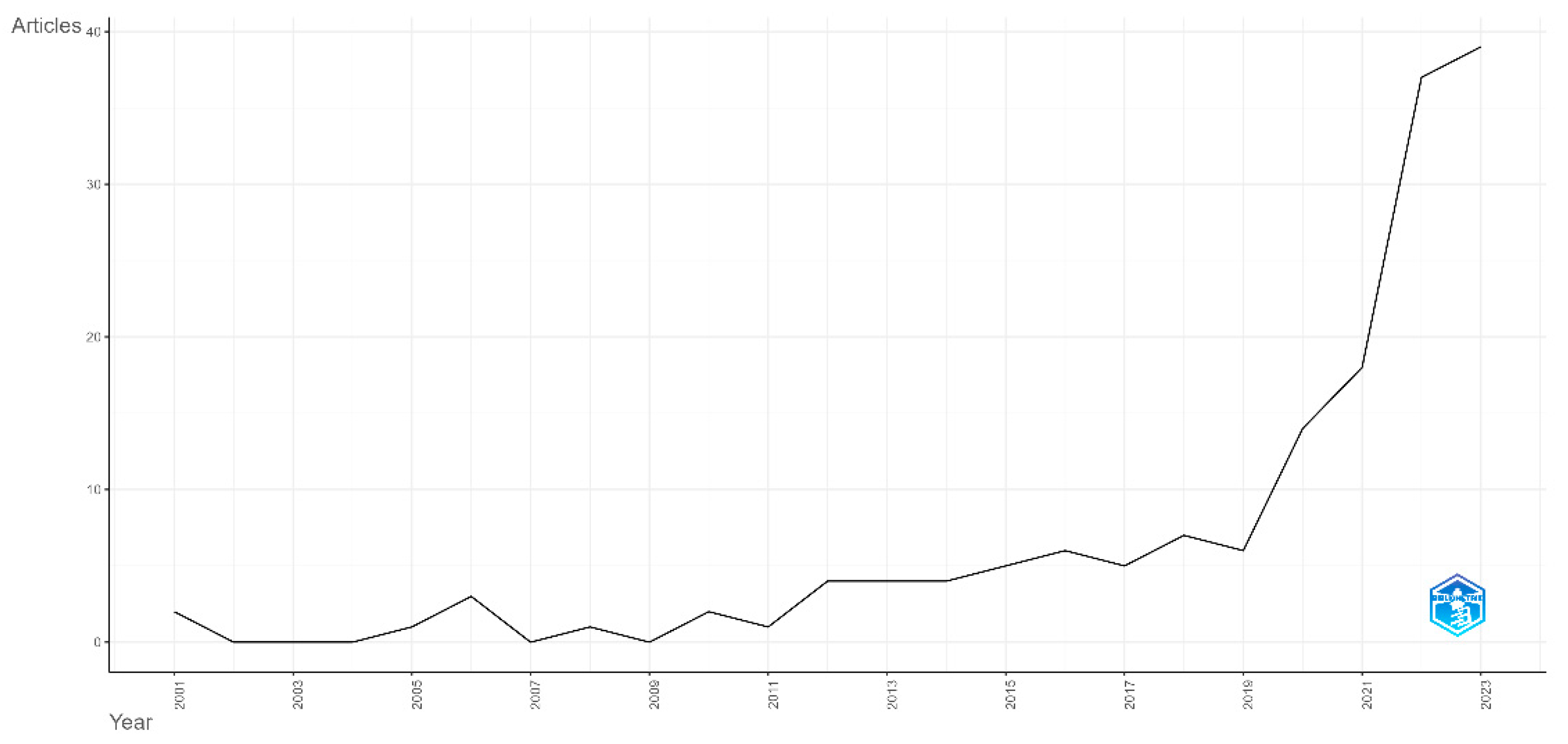
3.2. Global Publication Trends
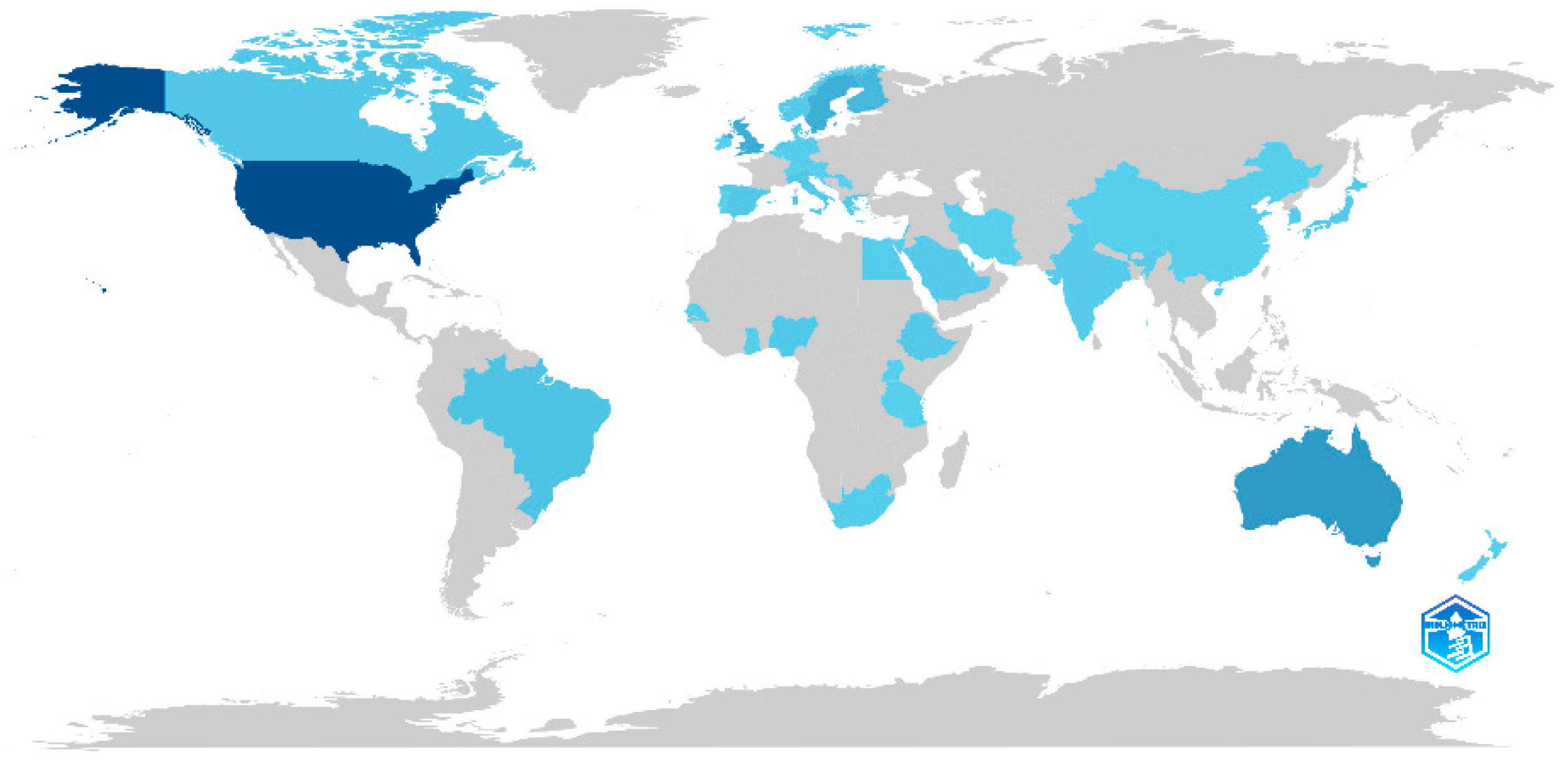
3.3. Most Relevant Journals, Articles, Countries and Affiliations
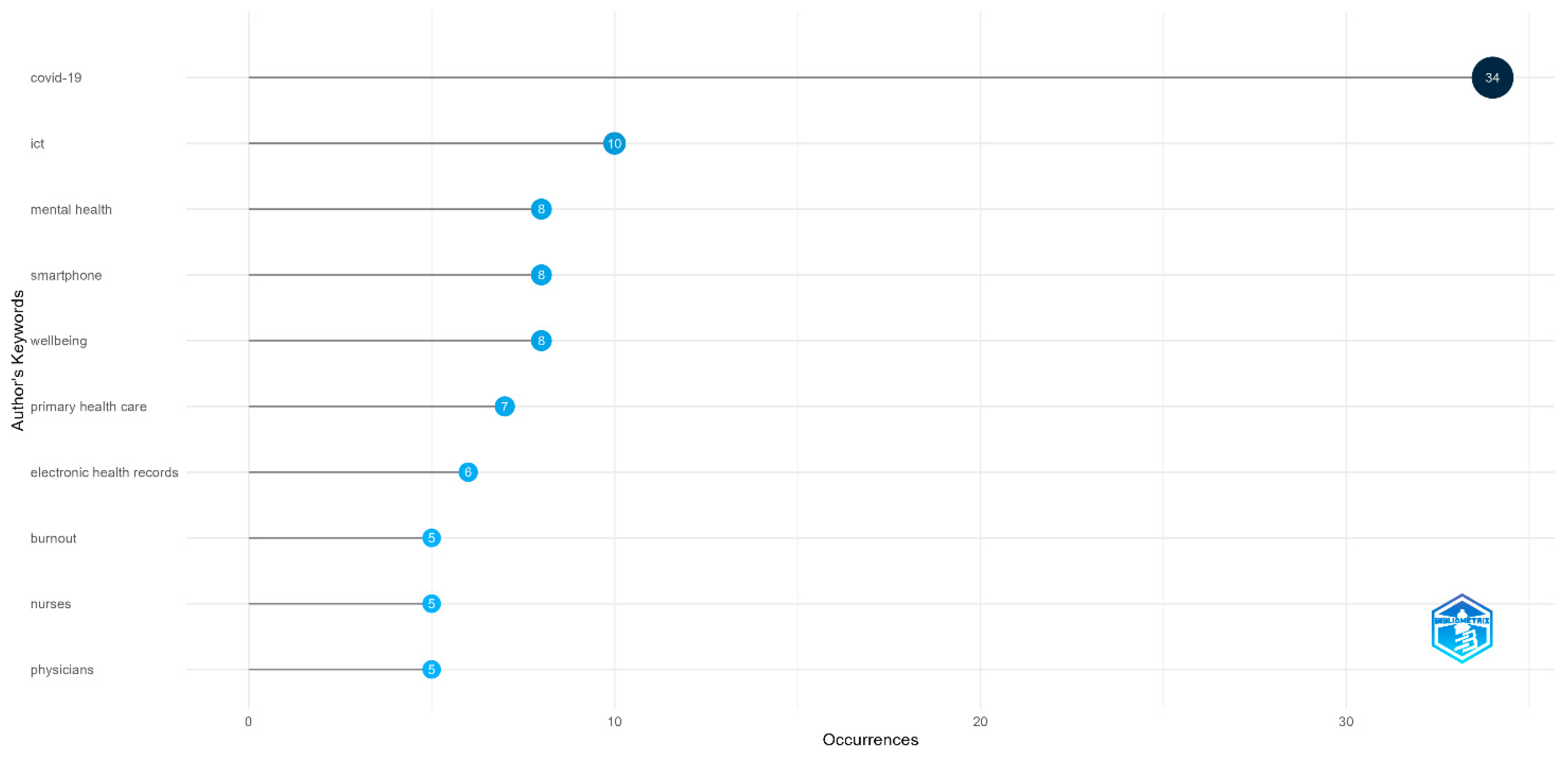
3.4. Most Relevant Words and Frequency over Time
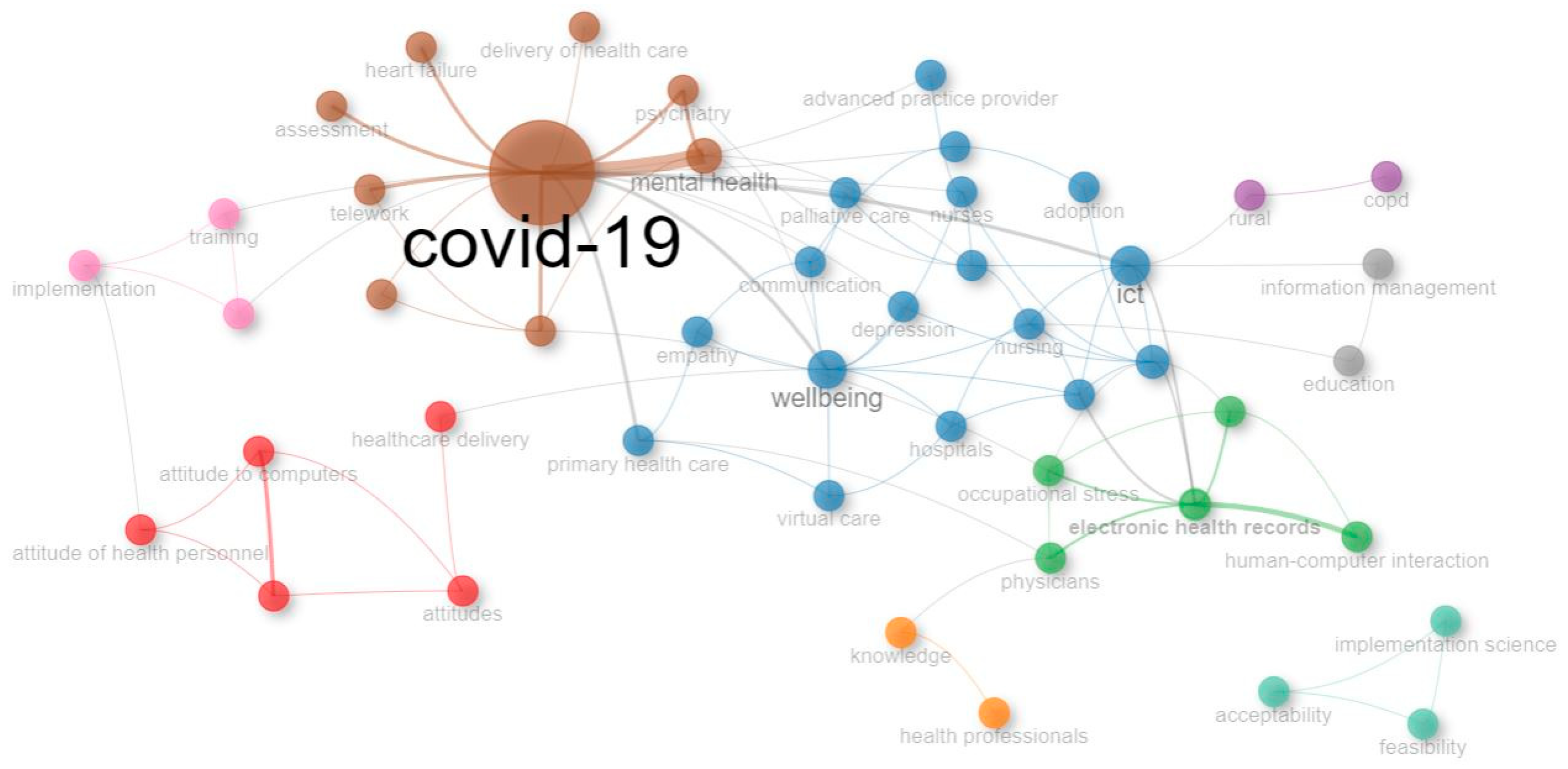
3.5. Co-Word Analysis
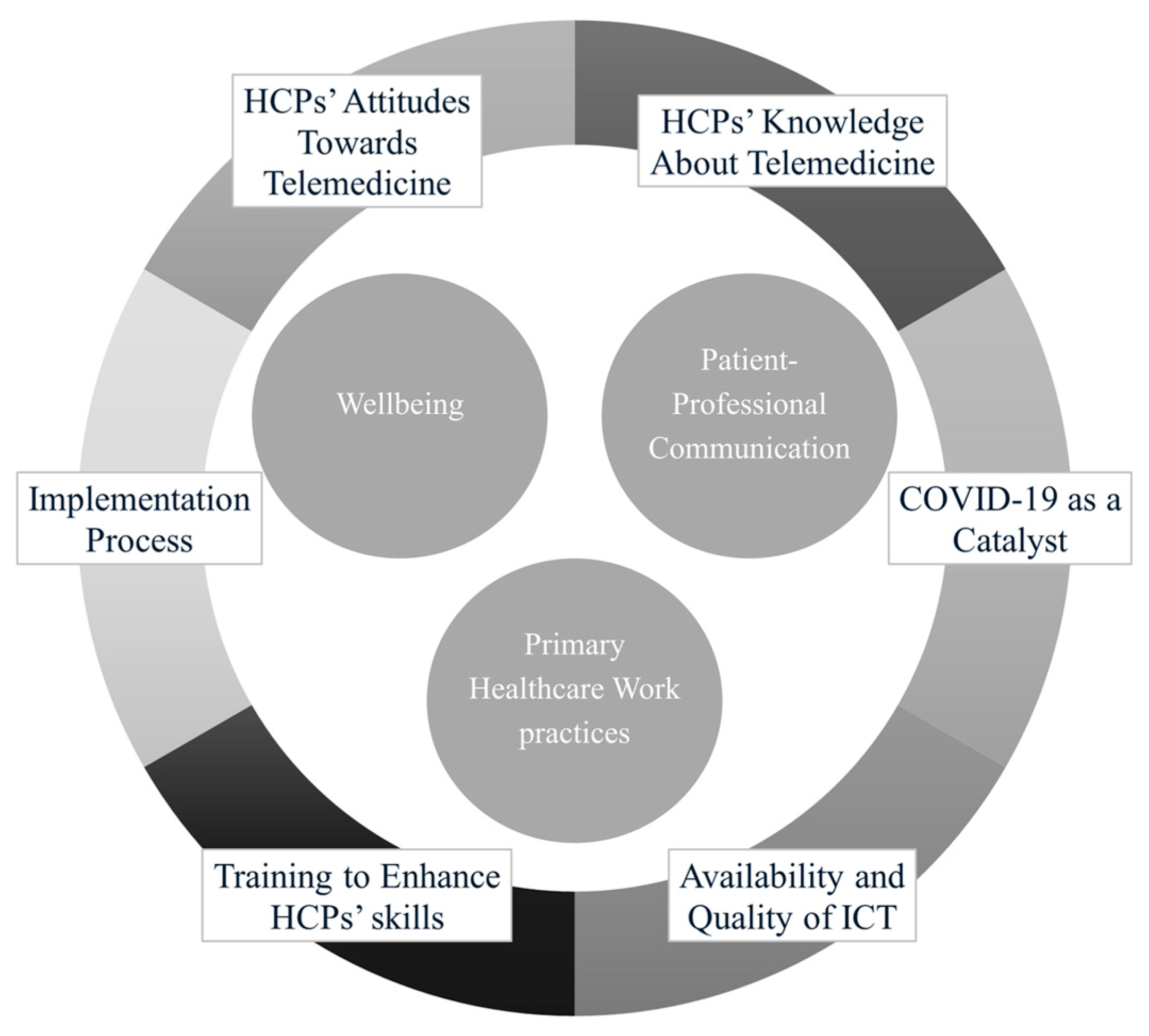
3.6. Thematic Analysis
4. Discussion
Implications for Practice
5. Conclusions
6. Suggestions for Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weißenfeld, M.M.; Goetz, K.; Steinhäuser, J. Facilitators and Barriers for the Implementation of Telemedicine from a Local Government Point of View—A Cross-Sectional Survey in Germany. BMC Health Serv. Res. 2021, 21, 919. [Google Scholar] [CrossRef]
- World Health Organization. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Tore, N.G.; Oskay, D.; Haznedaroglu, S. The Quality of Physiotherapy and Rehabilitation Program and the Effect of Telerehabilitation on Patients with Knee Osteoarthritis. Clin. Rheumatol. 2023, 42, 903–915. [Google Scholar] [CrossRef] [PubMed]
- Ezeamii, V.C.; Okobi, O.E.; Wambai-Sani, H.; Perera, G.S.; Zaynieva, S.; Okonkwo, C.C.; Ohaiba, M.M.; William-Enemali, P.C.; Obodo, O.R.; Obiefuna, N.G. Revolutionizing Healthcare: How Telemedicine Is Improving Patient Outcomes and Expanding Access to Care. Cureus 2024, 16, e63881. [Google Scholar] [CrossRef] [PubMed]
- Ohannessian, R.; Duong, T.A.; Odone, A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill. 2020, 6, e18810. [Google Scholar] [CrossRef] [PubMed]
- Ghildiyal, N.; Bangari, M. Telemedicine. Zero Contagion Risk and Enabler of Healthcare Fire Sales. Curr. Med. Res. Pract. 2023, 13, 26–31. [Google Scholar] [CrossRef]
- Bernuzzi, C.; Piccardo, M.A.; Marsilio, M.; Calcaterra, V.; Zuccotti, G.; Guglielmetti, C. Value Co-Creation in Telemedicine: A Qualitative Study of Pediatricians’ Expectations Regarding Telehomecare Implementation in an Italian Pediatric Hospital. J. Healthc. Leadersh. 2024, 16, 485–500. [Google Scholar] [CrossRef]
- World Health Organization. Transforming and Scaling up Health Professionals’ Education and Training: World Health Organization Guidelines 2013. In Transforming and Scaling up Health Professionals’ Education and Training: World Health Organization Guidelines; WHO: Geneva, Switzerland, 2013; p. 124. [Google Scholar]
- Scholze, A.; Hecker, A. Digital Job Demands and Resources: Digitization in the Context of the Job Demands-Resources Model. Int. J. Environ. Res. Public Health 2023, 20, 6581. [Google Scholar] [CrossRef]
- Qvarfordt, M.; Lagrosen, S. Healthcare Digitalisation and Its Association with Quality and Employee Health, a Mixed-Methods Study. Int. J. Workplace Health Manag. 2024, 17, 1–20. [Google Scholar] [CrossRef]
- Breton, M.; Sullivan, E.E.; Deville-Stoetzel, N.; McKinstry, D.; DePuccio, M.; Sriharan, A.; Deslauriers, V.; Dong, A.; McAlearney, A.S. Telehealth Challenges during COVID-19 as Reported by Primary Healthcare Physicians in Quebec and Massachusetts. BMC Fam. Pract. 2021, 22, 192. [Google Scholar] [CrossRef]
- Frennert, S.; Petersson, L.; Erlingsdottir, G. “More” Work for Nurses: The Ironies of EHealth. BMC Health Serv. Res. 2023, 23, 411. [Google Scholar] [CrossRef]
- Galle, A.; Semaan, A.; Huysmans, E.; Audet, C.; Asefa, A.; Delvaux, T.; Afolabi, B.B.; El Ayadi, A.M.; Benova, L. A Double-Edged Sword—Telemedicine for Maternal Care during COVID-19: Findings from a Global Mixed-Methods Study of Healthcare Providers. BMJ Glob. Health 2021, 6, e004575. [Google Scholar] [CrossRef] [PubMed]
- Garavand, A.; Aslani, N.; Nadri, H.; Abedini, S.; Dehghan, S. Acceptance of Telemedicine Technology among Physicians: A Systematic Review. Inform. Med. Unlocked 2022, 30, 100943. [Google Scholar] [CrossRef]
- Abdelghany, I.K.; AlMatar, R.; Al-Haqan, A.; Abdullah, I.; Waheedi, S. Exploring Healthcare Providers’ Perspectives on Virtual Care Delivery: Insights into Telemedicine Services. BMC Health Serv. Res. 2024, 24, 1. [Google Scholar] [CrossRef]
- Boksa, V.; Pennathur, P. Assessing Contributing and Mediating Factors of Telemedicine on Healthcare Provider Burnout. Health Policy Technol. 2024, 13, 100942. [Google Scholar] [CrossRef]
- Veiga, M.G.; Felizi, R.T.; Fernandes, C.E.; Oliveira, E. WhatsApp and Gynecologist-Patient Interaction: Development and Validation of a Questionnaire to Assess the Stress Perceived by the Doctor. Rev. Bras. Ginecol. Obs./RBGO Gynecol. Obstet. 2022, 44, 497–502. [Google Scholar] [CrossRef] [PubMed]
- West, C.P. Association of Resident Fatigue and Distress With Perceived Medical Errors. JAMA 2009, 302, 1294. [Google Scholar] [CrossRef]
- Baluszek, J.B.; Wiig, S.; Myrnes-Hansen, K.V.; Brønnick, K.K. Specialized Healthcare Practitioners’ Challenges in Performing Video Consultations to Patients in Nordic Countries—A Systematic Review and Narrative Synthesis. BMC Health Serv. Res. 2022, 22, 1432. [Google Scholar] [CrossRef]
- Chereka, A.A.; Mekonnen, G.B.; Yirsaw, A.N.; Mengistie, B.A.; Getachew, E.; Lakew, G.; Shibabaw, A.A.; Kitil, G.W. Attitudes towards Telemedicine Services and Associated Factors among Health Professionals in Ethiopia: A Systematic Review and Meta-Analysis. BMC Health Serv. Res. 2024, 24, 1505. [Google Scholar] [CrossRef]
- Ftouni, R.; AlJardali, B.; Hamdanieh, M.; Ftouni, L.; Salem, N. Challenges of Telemedicine during the COVID-19 Pandemic: A Systematic Review. BMC Med. Inform. Decis. Mak. 2022, 22, 207. [Google Scholar] [CrossRef]
- Rouidi, M.; Elouadi, A.; Hamdoune, A. Acceptance and Use of Telemedicine Technology by Health Professionals: Development of a Conceptual Model. Digit. Health 2022, 8, 205520762210816. [Google Scholar] [CrossRef]
- Öztürk, O.; Kocaman, R.; Kanbach, D.K. How to Design Bibliometric Research: An Overview and a Framework Proposal. Rev. Manag. Sci. 2024, 18, 3333–3361. [Google Scholar] [CrossRef]
- Donthu, N.; Kumar, S.; Mukherjee, D.; Pandey, N.; Lim, W.M. How to Conduct a Bibliometric Analysis: An Overview and Guidelines. J. Bus. Res. 2021, 133, 285–296. [Google Scholar] [CrossRef]
- Aria, M.; Cuccurullo, C. Bibliometrix: An R-Tool for Comprehensive Science Mapping Analysis. J. Informetr. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Fusco, F.; Marsilio, M.; Guglielmetti, C. Co-Production in Health Policy and Management: A Comprehensive Bibliometric Review. BMC Health Serv. Res. 2020, 20, 504. [Google Scholar] [CrossRef]
- Mukherjee, D.; Lim, W.M.; Kumar, S.; Donthu, N. Guidelines for Advancing Theory and Practice through Bibliometric Research. J. Bus. Res. 2022, 148, 101–115. [Google Scholar] [CrossRef]
- Montazeri, A.; Mohammadi, S.; M. Hesari, P.; Ghaemi, M.; Riazi, H.; Sheikhi-Mobarakeh, Z. Preliminary Guideline for Reporting Bibliometric Reviews of the Biomedical Literature (BIBLIO): A Minimum Requirements. Syst. Rev. 2023, 12, 239. [Google Scholar] [CrossRef]
- Ball, R.; Tunger, D. Science Indicators Revisited—Science Citation Index versus SCOPUS: A Bibliometric Comparison of Both Citation Databases. Inf. Serv. Use 2007, 26, 293–301. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Callon, M.; Courtial, J.P.; Laville, F. Co-Word Analysis as a Tool for Describing the Network of Interactions between Basic and Technological Research: The Case of Polymer Chemsitry. Scientometrics 1991, 22, 155–205. [Google Scholar] [CrossRef]
- Cobo, M.J.; López-Herrera, A.G.; Herrera-Viedma, E.; Herrera, F. Science Mapping Software Tools: Review, Analysis, and Cooperative Study among Tools. J. Am. Soc. Inf. Sci. Technol. 2011, 62, 1382–1402. [Google Scholar] [CrossRef]
- Hennemann, S.; Beutel, M.E.; Zwerenz, R. Ready for EHealth? Health Professionals’ Acceptance and Adoption of EHealth Interventions in Inpatient Routine Care. J. Health Commun. 2017, 22, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Katzman, J.G.; Comerci, G.; Boyle, J.F.; Duhigg, D.; Shelley, B.; Olivas, C.; Daitz, B.; Carroll, C.; Som, D.; Monette, R.; et al. Innovative Telementoring for Pain Management: Project ECHO Pain. J. Contin. Educ. Health Prof. 2014, 34, 68–75. [Google Scholar] [CrossRef]
- Villani, D.; Grassi, A.; Cognetta, C.; Toniolo, D.; Cipresso, P.; Riva, G. Self-Help Stress Management Training through Mobile Phones: An Experience with Oncology Nurses. Psychol. Serv. 2013, 10, 315–322. [Google Scholar] [CrossRef]
- Maguire, R.; Ream, E.; Richardson, A.; Connaghan, J.; Johnston, B.; Kotronoulas, G.; Pedersen, V.; McPhelim, J.; Pattison, N.; Smith, A.; et al. Development of a Novel Remote Patient Monitoring System. Cancer Nurs. 2015, 38, E37–E47. [Google Scholar] [CrossRef]
- Moeckli, J.; Cram, P.; Cunningham, C.; Reisinger, H.S. Staff Acceptance of a Telemedicine Intensive Care Unit Program: A Qualitative Study. J. Crit. Care 2013, 28, 890–901. [Google Scholar] [CrossRef] [PubMed]
- Vehko, T.; Hyppönen, H.; Puttonen, S.; Kujala, S.; Ketola, E.; Tuukkanen, J.; Aalto, A.-M.; Heponiemi, T. Experienced Time Pressure and Stress: Electronic Health Records Usability and Information Technology Competence Play a Role. BMC Med. Inform. Decis. Mak. 2019, 19, 160. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Asch, S.; Vilendrer, S.; Thomas, S.C.; Bajra, R.; Barman, L.; Edwards, L.M.; Filipowicz, H.; Giang, L.; Jee, O.; et al. Qualitative Assessment of Rapid System Transformation to Primary Care Video Visits at an Academic Medical Center. Ann. Intern. Med. 2020, 173, 527–535. [Google Scholar] [CrossRef]
- Bolier, L.; Ketelaar, S.M.; Nieuwenhuijsen, K.; Smeets, O.; Gärtner, F.R.; Sluiter, J.K. Workplace Mental Health Promotion Online to Enhance Well-Being of Nurses and Allied Health Professionals: A Cluster-Randomized Controlled Trial. Internet Interv. 2014, 1, 196–204. [Google Scholar] [CrossRef]
- Grünloh, C.; Cajander, Å.; Myreteg, G. “The Record Is Our Work Tool!”—Physicians’ Framing of a Patient Portal in Sweden. J. Med. Internet Res. 2016, 18, e167. [Google Scholar] [CrossRef]
- Ruiz Morilla, M.D.; Sans, M.; Casasa, A.; Giménez, N. Implementing Technology in Healthcare: Insights from Physicians. BMC Med. Inform. Decis. Mak. 2017, 17, 92. [Google Scholar] [CrossRef]
- Escobar, O.R.; Leone, D.; Malafronte, P.; Mele, S. The Effect of Telemedicine on Patients’ Wellbeing: A Systematic Review. J. Innov. Econ. Manag. 2021, 35, 9–31. [Google Scholar] [CrossRef]
- Widyanty, W.; Oktasari, D.P.; Riyanto, S.; Nusraningrum, D.; Damayanti, S.; Sumaedi, S.; Bakti, I.G.M.Y.; Dinaseviani, A.; Prasetya, P.; Fahlevi, M. Employee Green Behavior: Mapping Knowledge Structures and Future Directions. Cogent Bus. Manag. 2025, 12, 2440814. [Google Scholar] [CrossRef]
- Werkmeister, B.J.; Haase, A.M.; Fleming, T.; Officer, T.N. Experiences of the COVID-19 Lockdown and Telehealth in Aotearoa New Zealand: Lessons and Insights from Mental Health Clinicians. Int. J. Environ. Res. Public Health 2023, 20, 4791. [Google Scholar] [CrossRef]
- Boe Danbjørg, D.; Wagner, L.; Rønde Kristensen, B.; Clemensen, J. Nurses’ Experience of Using an Application to Support New Parents after Early Discharge: An Intervention Study. Int. J. Telemed. Appl. 2015, 2015, 1–10. [Google Scholar] [CrossRef]
- Sävenstedt, S.; Sandman, P.O.; Zingmark, K. The Duality in Using Information and Communication Technology in Elder Care. J. Adv. Nurs. 2006, 56, 17–25. [Google Scholar] [CrossRef]
- Fernemark, H.; Skagerström, J.; Seing, I.; Ericsson, C.; Nilsen, P. Digital Consultations in Swedish Primary Health Care: A Qualitative Study of Physicians’ Job Control, Demand and Support. BMC Fam. Pract. 2020, 21, 241. [Google Scholar] [CrossRef]
- Björndell, C.; Premberg, Å. Physicians’ Experiences of Video Consultation with Patients at a Public Virtual Primary Care Clinic: A Qualitative Interview Study. Scand. J. Prim. Health Care 2021, 39, 67–76. [Google Scholar] [CrossRef]
- Rothwell, E.; Ellington, L.; Planalp, S.; Crouch, B. Exploring Challenges to Telehealth Communication by Specialists in Poison Information. Qual. Health Res. 2012, 22, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Sigesmund, D.; Coe, J.B.; Khosa, D.; Moore, I.C. Veterinarians Are Reluctant to Recommend Virtual Consultations to a Fellow Veterinarian. J. Am. Vet. Med. Assoc. 2023, 261, 1820–1828. [Google Scholar] [CrossRef]
- Brandt, C.J.; Isidora Søgaard, G.; Clemensen, J.; Søndergaard, J.; Bo Nielsen, J. Determinants of Successful Ehealth Coaching for Consumer Lifestyle Changes: Qualitative Interview Study among Health Care Professionals. J. Med. Internet Res. 2018, 20, e237. [Google Scholar] [CrossRef]
- Amuasi, J.H.; Agbogbatey, M.K.; Sarfo, F.S.; Beyuo, A.; Duah, K.; Agasiya, P.; Arthur, A.; Appiah, L.; Nguah, S.B.; Bockarie, A.; et al. Feasibility, Acceptability, and Appropriateness of a Mobile Health Stroke Intervention among Ghanaian Health Workers. J. Neurol. Sci. 2022, 439, 120304. [Google Scholar] [CrossRef]
- Piay-Fernández, N.; Stenbacka, E.; Jaramillo, M.C.; Guerrero, G.; Solano Rodríguez, A.A.; Montenegro, P.; Moreno, D.C.; Cleeve, A. Implementing Medical Abortion through Telemedicine in Colombia: A Qualitative Study. Sex. Reprod. Health Matters 2023, 31, 2236780. [Google Scholar] [CrossRef] [PubMed]
- Lerret, S.M.; Nuccio, S.; Compton, A.; Keegan, M.; Rapala, K. Nurses’ Experiences and Perspectives of the Telehealth Working Environment and Educational Needs. J. Contin. Educ. Nurs. 2023, 54, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Benwell, N.; Hird, K.; Thomas, N.; Furness, E.; Fear, M.; Sweetman, G. Effectiveness and Efficiency of Training in Digital Healthcare Packages: Training Doctors to Use Digital Medical Record Keeping Software. Aust. Health Rev. 2017, 41, 479–484. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Eriksen, S.; Dahler, A.M.; Øye, C. The Informal Way to Success or Failure? Findings from a Comparative Case Study on Video Consultation Training and Implementation in Two Danish Hospitals. BMC Health Serv. Res. 2023, 23, 1135. [Google Scholar] [CrossRef]
- Bautista, C.A.; Huang, I.; Stebbins, M.; Floren, L.C.; Wamsley, M.; Youmans, S.L.; Hsia, S.L. Development of an Interprofessional Rotation for Pharmacy and Medical Students to Perform Telehealth Outreach to Vulnerable Patients in the COVID-19 Pandemic. J. Interprof. Care 2020, 34, 694–697. [Google Scholar] [CrossRef]
- Bernuzzi, C.; Sommovigo, V.; Setti, I. The Role of Resilience in the Work-Life Interface: A Systematic Review. Work 2022, 73, 1147–1165. [Google Scholar] [CrossRef]
- DePierro, J.; Marin, D.B.; Sharma, V.; Costello, Z.; Starkweather, S.; Katz, C.L.; Lim, S.; Charney, D.S. Developments in the First Year of a Resilience-Focused Program for Health Care Workers. Psychiatry Res. 2021, 306, 114280. [Google Scholar] [CrossRef]
- Lee, D.; Lee, W.J.; Choi, S.-H.; Jang, J.-H.; Kang, D.-H. Long-Term Beneficial Effects of an Online Mind-Body Training Program on Stress and Psychological Outcomes in Female Healthcare Providers. Medicine 2020, 99, e21027. [Google Scholar] [CrossRef]
- Maniaci, M.J.; Maita, K.; Torres-Guzman, R.A.; Avila, F.R.; Garcia, J.P.; Eldaly, A.; Forte, A.J.; Matcha, G.; Pagan, R.; Paulson, M.R. Provider Evaluation of a Novel Virtual Hybrid Hospital at Home Model. Int. J. Gen. Med. 2022, 15, 1909–1918. [Google Scholar] [CrossRef]
- Brault, M.E.; Laudermith, A.; Kroll-Desrosiers, A. Telemedicine During COVID-19 Response: A Welcome Shift for Younger Female Healthcare Workers. J. Gen. Intern. Med. 2023, 38, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Haines, K.J.; Sawyer, A.; McKinnon, C.; Donovan, A.; Michael, C.; Cimoli, C.; Gregory, M.; Berney, S.; Berlowitz, D.J. Barriers and Enablers to Telehealth Use by Physiotherapists during the COVID-19 Pandemic. Physiotherapy 2023, 118, 12–19. [Google Scholar] [CrossRef] [PubMed]
- White, J.; Byles, J.; Walley, T. The Qualitative Experience of Telehealth Access and Clinical Encounters in Australian Healthcare during COVID-19: Implications for Policy. Health Res. Policy Syst. 2022, 20, 9. [Google Scholar] [CrossRef] [PubMed]
- Saukkonen, P.; Elovainio, M.; Virtanen, L.; Kaihlanen, A.-M.; Nadav, J.; Lääveri, T.; Vänskä, J.; Viitanen, J.; Reponen, J.; Heponiemi, T. The Interplay of Work, Digital Health Usage, and the Perceived Effects of Digitalization on Physicians’ Work: Network Analysis Approach. J. Med. Internet Res. 2022, 24, e38714. [Google Scholar] [CrossRef]
- Elareed, H.R.; Elroby, F.A.; Adly, E.S.; Mohamed Lotfy, A.M. Knowledge and Moral Attitude toward Telemedicine among Egyptian Physicians. J. Public Health (Bangkok) 2023, 33, 933–940. [Google Scholar] [CrossRef]
- George, P.P.; Edathotty, T.T.; Gopikrishnan, S.; Prasanth, P.S.; Mathew, S.; Mohammed Ameen, A.A. Knowledge, Awareness, and Attitude among Practicing Orthodontist on Teledentistry during COVID Pandemic in Kerala: A Cross-Sectional Survey. J. Pharm. Bioallied Sci. 2021, 13, S846–S850. [Google Scholar] [CrossRef]
- Morony, S.; Weir, K.; Duncan, G.; Biggs, J.; Nutbeam, D.; Mccaffery, K.J. Enhancing Communication Skills for Telehealth: Development and Implementation of a Teach-Back Intervention for a National Maternal and Child Health Helpline in Australia. BMC Health Serv. Res. 2018, 18, 162. [Google Scholar] [CrossRef]
- Phillips, Z.; Wong, L.; Crotty, K.; Horlick, M.; Johnston, R.; Altshuler, L.; Zabar, S.; Jay, M.; Dembitzer, A. Implementing an Experiential Telehealth Training and Needs Assessment for Residents and Faculty at a Veterans Affairs Primary Care Clinic. J. Grad. Med. Educ. 2023, 15, 456–462. [Google Scholar] [CrossRef]
- Godfrey, E.M.; Fiastro, A.E.; Jacob-Files, E.A.; Coeytaux, F.M.; Wells, E.S.; Ruben, M.R.; Sanan, S.S.; Bennett, I.M. Factors Associated with Successful Implementation of Telehealth Abortion in 4 United States Clinical Practice Settings. Contraception 2021, 104, 82–91. [Google Scholar] [CrossRef]
- Busso, M.; Gonzalez, M.P.; Scartascini, C. On the Demand for Telemedicine: Evidence from the COVID-19 Pandemic. Health Econ. 2022, 31, 1491–1505. [Google Scholar] [CrossRef]
- Shaver, J. The State of Telehealth Before and After the COVID-19 Pandemic. Prim. Care Clin. Off. Pract. 2022, 49, 517–530. [Google Scholar] [CrossRef]
- Bernuzzi, C. Exploring Patient Role From Compliance To Engagement In Telemedicine: A Comparative Bibliometric Analysis Across Psychology And Medicine. Humanit. Soc. Sci. Commun. 2025. under revision. [Google Scholar]
- Zeng, N.; Liu, M.-C.; Zhong, X.-Y.; Wang, S.-G.; Xia, Q.-D. Knowledge Mapping of Telemedicine in Urology in the Past 20 Years: A Bibliometric Analysis (2004–2024). Digit. Health 2024, 10, 20552076241287460. [Google Scholar] [CrossRef] [PubMed]
- Waqas, A.; Teoh, S.H.; Lapão, L.V.; Messina, L.A.; Correia, J.C. Harnessing Telemedicine for the Provision of Health Care: Bibliometric and Scientometric Analysis. J. Med. Internet Res. 2020, 22, e18835. [Google Scholar] [CrossRef]
- Fisk, M.; Livingstone, A.; Pit, S.W. Telehealth in the Context of COVID-19: Changing Perspectives in Australia, the United Kingdom, and the United States. J. Med. Internet Res. 2020, 22, e19264. [Google Scholar] [CrossRef]
- Sampat, B.; Drummond, M. Another Special Relationship? Interactions between Health Technology Policies and Health Care Systems in the United States and the United Kingdom. J. Health Polit. Policy Law. 2011, 36, 119–139. [Google Scholar] [CrossRef]
- Laukka, E.; Huhtakangas, M.; Heponiemi, T.; Kujala, S.; Kaihlanen, A.-M.; Gluschkoff, K.; Kanste, O. Health Care Professionals’ Experiences of Patient-Professional Communication Over Patient Portals: Systematic Review of Qualitative Studies. J. Med. Internet Res. 2020, 22, e21623. [Google Scholar] [CrossRef]
- Zeng, J.; Gao, Y.; Hou, C.; Liu, T. The Impact of Doctor–Patient Communication on Medication Adherence and Blood Pressure Control in Patients with Hypertension: A Systematic Review. PeerJ 2024, 12, e18527. [Google Scholar] [CrossRef] [PubMed]
- Horwood, C.; Luthuli, S.; Mapumulo, S.; Haskins, L.; Jensen, C.; Pansegrouw, D.; McKerrow, N. Challenges of Using E-Health Technologies to Support Clinical Care in Rural Africa: A Longitudinal Mixed Methods Study Exploring Primary Health Care Nurses’ Experiences of Using an Electronic Clinical Decision Support System (CDSS) in South Africa. BMC Health Serv. Res. 2023, 23, 30. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425. [Google Scholar] [CrossRef]
- Shiferaw, K.B.; Mengiste, S.A.; Gullslett, M.K.; Zeleke, A.A.; Tilahun, B.; Tebeje, T.; Wondimu, R.; Desalegn, S.; Mehari, E.A. Healthcare Providers’ Acceptance of Telemedicine and Preference of Modalities during COVID-19 Pandemics in a Low-Resource Setting: An Extended UTAUT Model. PLoS ONE 2021, 16, e0250220. [Google Scholar] [CrossRef] [PubMed]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating Barriers to Adopting Telemedicine Worldwide: A Systematic Review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [CrossRef] [PubMed]


| Dataset Features | ||
|---|---|---|
| General information | Timespan | 2001:2023 |
| Journals | 119 | |
| Documents | 160 | |
| Annual growth rate (%) | 14.46 | |
| Average citations per document | 14.03 | |
| Average citations per year per doc | 3.83 | |
| References | 4895 | |
| Document contents | Author’s keywords | 600 |
| Authors | Authors | 905 |
| n | Highest Percentile (Source: Scopus) | |
|---|---|---|
| Journal of Medical Internet Research | 10 | Health Informatics |
| BMC Health Services Research | 7 | Health Policy |
| International Journal of Environmental Research And Public Health | 6 | / |
| BMC Medical Informatics And Decision Making | 4 | / |
| BMJ Open | 3 | General Medicine |
| Plos One | 3 | Multidisciplinary |
| Telemedicine Reports | 3 | Medicine (miscellaneous) |
| Australian Journal of Primary Health | 2 | / |
| Frontiers in Digital Health | 2 | / |
| Health Informatics Journal | 2 | Health Informatics |
| Ranking | Article | Number of Citations | Number of Citations per Year |
|---|---|---|---|
| 1 | Hennemann et al. [33] | 123 | 15.38 |
| 2 | Katzman et al. [34] | 94 | 8.55 |
| 3 | Villani et al. [35] | 85 | 7.08 |
| 4 | Maguire et al. [36] | 81 | 8.1 |
| 5 | Moeckli et al. [37] | 71 | 1.39 |
| 6 | Vehko et al. [38] | 67 | 11.16 |
| 7 | Srinivasan et al. [39] | 62 | 12.4 |
| 8 | Bolier et al. [40] | 61 | 5.54 |
| 9 | Grünloh et al. [41] | 55 | 6.11 |
| 10 | Ruiz Morilla et al. [42] | 54 | 6.75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernuzzi, C.; Piccardo, M.A.; Guglielmetti, C. Mapping Research Trends on the Implications of Telemedicine for Healthcare Professionals: A Comprehensive Bibliometric Analysis. Healthcare 2025, 13, 1149. https://doi.org/10.3390/healthcare13101149
Bernuzzi C, Piccardo MA, Guglielmetti C. Mapping Research Trends on the Implications of Telemedicine for Healthcare Professionals: A Comprehensive Bibliometric Analysis. Healthcare. 2025; 13(10):1149. https://doi.org/10.3390/healthcare13101149
Chicago/Turabian StyleBernuzzi, Chiara, Maria Adele Piccardo, and Chiara Guglielmetti. 2025. "Mapping Research Trends on the Implications of Telemedicine for Healthcare Professionals: A Comprehensive Bibliometric Analysis" Healthcare 13, no. 10: 1149. https://doi.org/10.3390/healthcare13101149
APA StyleBernuzzi, C., Piccardo, M. A., & Guglielmetti, C. (2025). Mapping Research Trends on the Implications of Telemedicine for Healthcare Professionals: A Comprehensive Bibliometric Analysis. Healthcare, 13(10), 1149. https://doi.org/10.3390/healthcare13101149






