Abstract
Objectives: The purpose of this study was to evaluate the impact of endometriosis on various outcomes of in vitro fertilization (IVF), including live birth rates, clinical pregnancy rates, fertilization rates, and implantation rates, through a systematic review and meta-analysis. Methods: Systematic searches were carried out using PubMed, MEDLINE, Cochrane Central Register of Controlled Trials, Scopus, EMBASE, and Web of Science from January 2010 to November 2023. Studies comparing IVF outcomes in women with and without endometriosis were included. The primary outcome was live birth rate; secondary outcomes included clinical pregnancy, fertilization, and implantation rates. Data were extracted and analyzed using odds ratio (OR) and 95% confidence interval (CI) with fixed or random-effects models, depending on heterogeneity. Results: From 1340 studies initially identified, 40 studies met the inclusion criteria, encompassing 8970 women with endometriosis and 42,946 control participants. There were no significant differences between the endometriosis and control groups in terms of live birth rate (OR 1.03, 95% CI 0.75–1.41, p = 0.84), clinical pregnancy rate (OR 0.86, 95% CI 0.72–1.02, p = 0.1), or fertilization rate (OR 0.96, 95% CI 0.79–1.15, p = 0.64). However, endometriosis was associated with a significantly lower implantation rate (OR 0.85, 95% CI 0.74–0.97, p = 0.02). Conclusions: Endometriosis significantly negatively affects implantation rates in women undergoing IVF, despite the absence of significant differences in live birth, clinical pregnancy, and fertilization rates. Further research is needed to evaluate the impact of different stages of endometriosis on IVF outcomes and to develop optimized management protocols for these patients.
1. Introduction
Endometriosis is an inflammatory disorder characterized by the presence of endometrial tissue outside of the uterine cavity [1]. Women with endometriosis may experience a range of gynecological symptoms, including pelvic pain, dysmenorrhea, dyspareunia, and fertility issues [2].
It is estimated to affect about 10% of women of reproductive age. However, it may reach 25–40% among infertile women [3].
The high prevalence of endometriosis in the infertile population suggests a complex and multi-factorial role in infertility, which may affect ovarian reserve, ovulation, tubal anatomy, embryo quality, implantation, and pregnancy development [4]. As a consequence, the impact of endometriosis on embryo implantation is specifically difficult to highlight, and the exact mechanisms connecting endometriosis and infertility are still unclear and incompletely understood. Indeed the etiology of endometriosis remains incompletely elucidated to date. Its physiopathology is also debated. Its high prevalence in the infertile population (20–30%) underlines its very complex and multi-factorial role in infertility, affecting ovarian reserve, ovulation, tubal anatomy, embryo quality, implantation, and pregnancy development. Thus, the impact of endometriosis on embryo implantation is specifically difficult to highlight. While the relationship between infertility and severe/advanced stage endometriosis may be explained by the severe anatomical and functional abnormalities and lower ovarian reserve, the cause of infertility in the case of minimal or mild endometriosis is still unclear and remains a matter of debate [5].
The principal underlying cause of endometriosis related-infertility is most likely chronic pelvic inflammation. This inflammation can lead to increased levels of cytokines and macrophages in the peritoneal fluid of patients with endometriosis and has been linked to adverse effects on human reproduction [6,7,8,9]. Chronic inflammation can result in the formation of pelvic adhesions and scarring, distorting pelvic anatomy and leading to structural changes that may affect the normal functioning of reproductive organs. These adhesions might obstruct or alter the fallopian tubes, disrupt ovarian function, or hinder the release, movement, or transport of oocytes, thus impeding fertilization [10]. Other mechanisms that may explain reduced fertility include hormonal imbalances [11], uterine hyper- and dysperistalsis [12], and follicular loss along with intraovarian vascular injury due to ovarian stromal fibrosis [13,14]. Further endometriosis may induce immunological or hormonal abnormalities that by themselves may affect IVF outcomes [15,16].
IVF may be useful in bypassing some of the negative effects of endometriosis; however, women with endometriosis may still encounter infertility treatments [17].
Moreover, it is logical to predict that some of these causes cannot be avoided by using IVF, and there is an uncertainty if women affected by endometriosis may respond worse to IVF as compared to patients with other infertility causes. There is also a lack of agreement on how the severity of endometriosis affects IVF outcome and underscores the importance of investigating the relationship between endometriosis and IVF outcome.
Our objective was to quantify the impact of endometriosis on live birth, clinical pregnancy, fertilization, and implantation rates through a comprehensive meta-analysis, and the meta-analysis aimed to provide a thorough and evidence-based overview of how endometriosis affects various aspects of IVF, including live birth rates, pregnancy rates, and other relevant outcomes. This information can be valuable for clinicians, researchers, and patients in understanding the potential impact of endometriosis on fertility treatment outcomes and guiding clinical decision-making.
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
Systematic electronic database searches were carried out using PubMed, MEDLINE, Cochrane Central Register of Controlled Trials, Scopus, EMBASE, and Web of Science. The following keywords were searched for: fertilization in vitro, fertilization in vitro/methods, ART, ICSI, IVF, endometriosis, endometriosis/complications, endometriosis/pathology, endometrioma, DIE, outcome/s, pregnancy, pregnancy rate, and birth rate. Boolean operators including endometriosis and all the IVF outcomes were also searched. Only articles in the English language were included. The search was performed between January 2010 and November 2023. This study protocol is registered in the Prospero database (2023 CRD42023467215).
The population group of this study included women who had undergone or were undergoing IVF procedures; the study group was made up of women affected by endometriosis diagnosed either by ultrasound, MRI, or histologic examination, whereas the control group consisted of women without endometriosis.
The following articles were excluded: studies that had included women that had undergone treatment using donor oocytes or that had received surgical or medical treatment for endometriosis prior to ART; studies that did not provide full texts or lacked necessary data for analysis; studies without a control group; case reports or abstracts; studies limited to conference proceedings; and non-original or duplicate publications.
The primary outcome was live birth rate (LBR), which was determined as the number of deliveries resulting in a live newborn.
The secondary outcomes were as follows:
- (a)
- Clinical pregnancy rate (CPR), defined by the ultrasound visualization of an intrauterine gestational sac;
- (b)
- Fertilization rate (FR), defined as the percentage of transformation of micro injected oocytes into two pronuclei;
- (c)
- Implantation rate (IR): number of implanted embryos/number of embryos transferred.
CPR and LBR data were expressed as total number of ART patients considered in the study, and when this was not possible, we considered the data per transfer or per cycle.
2.2. Data Extraction and Quality Assessment
Two authors (IM and CP) reviewed all abstracts independently and selected the articles that fit the predefined selection criteria. Subsequently, the authors reviewed the full manuscripts of these selected publications to determine final inclusion or exclusion decisions. Any disagreements regarding the relevance of articles were settled through consensus or, if necessary, by consulting another reviewer (GR). Disagreement among authors was present only for 2 studies, which were re-reviewed with GR. The quality of the included studies was evaluated using the Newcastle–Ottawa scale, where each study is evaluated based on the selection of the study groups, the comparability of these groups, and the outcome of interests.
2.3. Statistical Analysis
An analysis of the ART outcomes of women with endometriosis compared to a control group was performed. Data were extracted from original studies; if raw data were not provided, we used the available data for calculations. From these indices, we derived corresponding odds ratios (ORs) and their 95% confidence intervals. Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines were observed in conducting this study. ORs from individual studies were combined using either a fixed-effects model or a random-effects model. The latter analysis was adopted when a high heterogeneity was found. Heterogeneity was assessed using I2 statistics and visually with forest plots. High heterogeneity was considered when I2 exceeded 50%. STATA version 13.1 (Stata Corp., College Station, TX, USA) was used for all statistical analyses.
3. Results
From the initial search, we identified 1340 studies (Figure 1, Prisma chart and Prisma checklist Supplementary Material). We conducted an initial screening of all titles and abstracts to evaluate their relevance to our study based on our predefined inclusion criteria. This screening process led to the exclusion of 1152 publications.
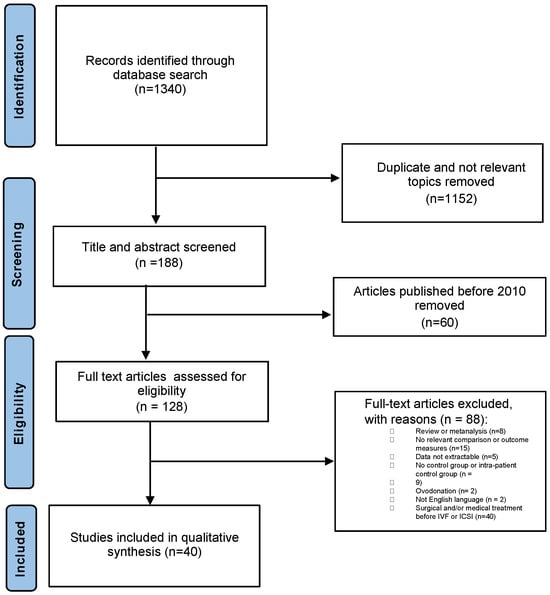
Figure 1.
Prisma chart showing study selection for systematic review on the effect of endometriosis on IVF treatment outcome.
Another set of 148 publications were excluded following a review of the entire texts of the remaining studies: (60 studies published before 2010, 15 without any relevant outcome measures, 7 concerning adenomyosis, 5 because data were not extractable from the studies, 8 were a review or meta-analysis, 9 had no control group or intra-patient control groups, 2 were about performing IVF with egg donation, 2 were not in the English language, and 40 were about patients that had undergone surgical or medical treatment before IVF (Supplementary Material).
Consequently, the systematic review included a total of 40 studies [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56] (Table 1).

Table 1.
General characteristics of the included studies.
The Newcastle–Ottawa Quality Assessment Scale scores for these studies are presented in Table 2. We analyzed data from 8970 women diagnosed with endometriosis and 42,946 control participants.

Table 2.
Newcastle–Ottawa Quality Assessment Scale of the included studies.
In Table 3, a summary of the results obtained is presented.

Table 3.
Data analysis summary.
3.1. Live Births
Information on live birth rates was available from 26 studies. In 15 of these studies, live birth rates were reported per total number of women undergoing IVF (study group n. 3210/8186 vs. control group n 7124/30,247). No significant difference in live birth rates between the endometriosis and control group was found (OR 1.03, 95% CI = 0.75–1.41, p = 0.84) (Figure 2). A high heterogeneity was observed among these studies, with an I2 value of 93.5% (95% CI = 91.3% to 94.9%).
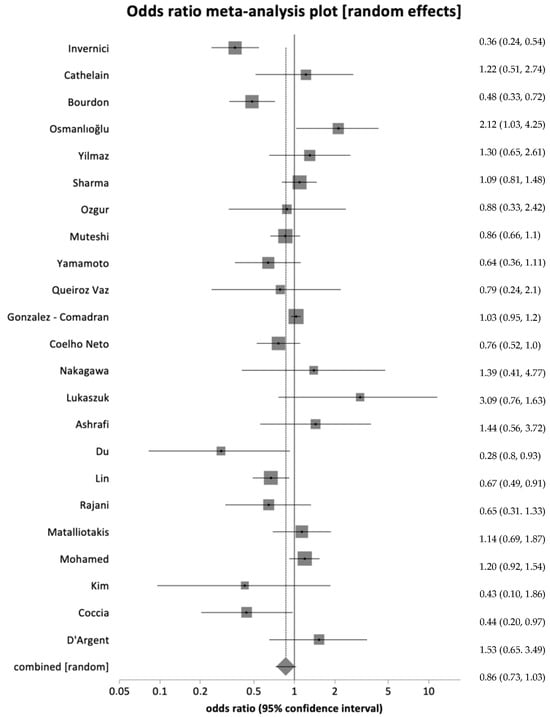
Figure 2.
Forest plot showing live birth rate per total number of women with no significant difference in live birth rates across groups [17,19,20,23,28,31,32,33,34,36,37,38,41,45,46,47,50,51,52,53,54,55,56].
When combining results from four studies that evaluated live birth per transfer (study group n. 274/748 vs. control group n 942/2483), no difference in live birth rate was observed between the two groups (OR 0.93, 95% CI = 0.78–1.10, p = 0.388) (Supplementary Figure S1). The I2 value was 0% (95% CI = 0% to 67.9%).
When pooling results from seven studies that reported live birth per cycle (study group n. 398/435 vs. control group n. 270/7462), no significant difference was observed in live birth rate (OR 0.99, 95% CI = 0.86–1.15, p = 0.89) (Supplementary Figure S2). The I2 value was 0% (95% CI = 0% to 58.5%), suggesting low heterogeneity among the studies.
3.2. Clinical Pregnancies
Data on the clinical pregnancy rate were available in 30 studies. In 23 of these, pregnancy rate was expressed per total number of women undergoing IVF (study group n. 1833/6552 vs. control group n. 9716/34,691). After combining the data, no difference in clinical pregnancy rates was found between the endometriosis and control groups (OR 0.86, 95% CI = 0.72–1.02, p = 0.098) (Figure 3). A high heterogeneity was observed, with an I2 value of 72.5% (95% CI = 56.2% to 80.9%).
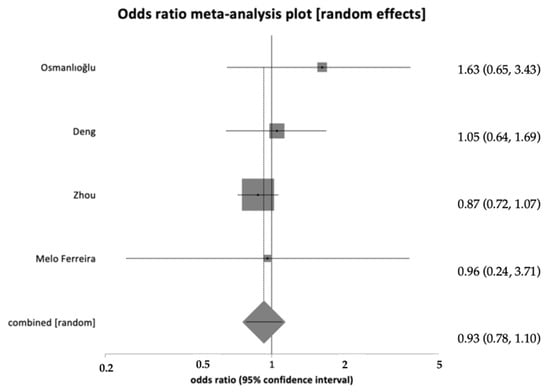
Figure 3.
Forest plot showing clinical pregnancy per total number of women with no significant difference in live birth rates across groups [23,24,25,29].
When pooling data from four studies that evaluated clinical pregnancy per transfer (study group n. 345/759 vs. control group n 996/1856), no difference in clinical pregnancy rates was observed (OR 0.91, 95% CI = 0.76–1.09, p = 0.29) (Supplementary Figure S3). The I2 value was 0% (95% CI = 0% to 67.9%), indicating minimal variability among the studies.
Combining data from three studies that described clinical pregnancy per cycle as an outcome (study group n. 271/990 vs. control group n 505/1571) also showed no statistically significant difference (OR 0.95, 95% CI = 0.76–1.17, p = 0.61) (Supplementary Figure S4). The I2 value was 0% (95% CI = 0% to 72.9%), indicating a low heterogeneity.
3.3. Fertilization Rate
Fertilization rate data, defined as the number of fertilized oocytes per number of metaphase II oocytes, were extracted from eight studies (study group: 4153 out of 5661; control group: 43,979 out of 62,972). No difference in fertilization rates was found (OR = 0.96, 95% CI = 0.79–1.15, p = 0.64) (Figure 4). A significant heterogeneity was indicated by an I2 value of 80.5% (95% CI = 57.6% to 88.5%).
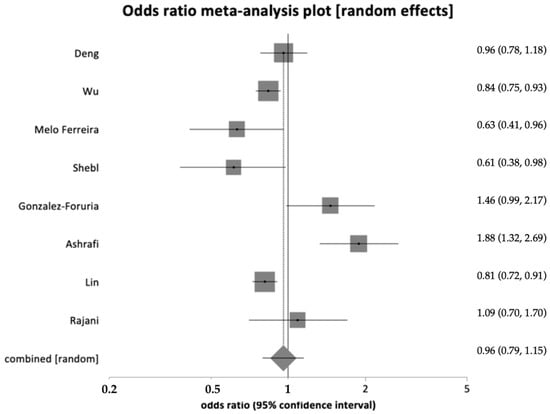
Figure 4.
Forest plot showing fertilization rate with no significant difference in live birth rates across groups [24,26,30,35,36,46,50,51].
3.4. Implantation Rate
Data on implantation rates, defined as successful implantations per total number of embryos transferred, were available in 10 studies (study group: 406 out of 2032; control group: 3573 out of 11,120). Heterogeneity was limited, with an I2 value of 37.5% (95% CI = 0% to 68.9%) (Figure 5). Pooling the results from these ten studies showed a statistically significant reduction in implantation rates (OR = 0.85, 95% CI = 0.74–0.97, p = 0.02).
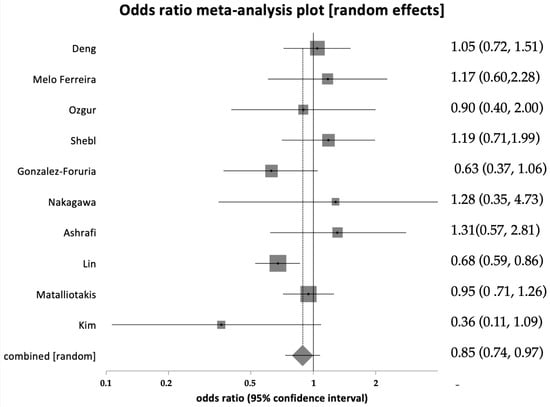
Figure 5.
Forest plot showing implantation rate significantly lower in women with endometriosis [24,30,32,35,36,41,46,50,52].
4. Discussion
4.1. Main Findings
This systematic review and meta-analysis indicate that endometriosis among patients undergoing IVF/ICSI, regardless of its stage, does not significantly impact live birth, clinical pregnancy, and fertilization rates when compared to other causes of infertility. However, a notable reduction in implantation rate was observed in women with endometriosis.
4.2. Strengths and Limitations
One major strength of this study is its restriction of our analysis to studies published from 2010 onwards, minimizing the influence of outdated IVF techniques. Furthermore, we selected only studies in which women with endometriosis had not undergone any previous surgical or medical treatments for this condition. We adopted the Newcastle–Ottawa Quality Assessment Scale to ensure that high-quality studies with a low bias were included. As a consequence, the inclusion of recent research and the strict selection criteria enhanced the quality of the analysis.
However, the main limitation was the lack of differentiation between different grades of endometriosis, potentially increasing heterogeneity. Similarly, it was not possible to stratify women according to their characteristics (e.g., age, BMI) and IVF protocols that similarly may increase heterogenicity. Nevertheless, clinical heterogeneity is common in meta-analyses and does not necessarily affect generalizability more than individual studies do [58]. Other limitations concerned data presentation variability as some studies did not report the number of patients included but only the number of cycles, where some studies reported IVF results after a certain number of cycles while others only followed one cycle. Moreover, the diagnosis of endometriosis was not performed the same way in all studies (either by laparoscopy or ultrasound). This may affect the correct diagnosis and classification of endometriosis since deep endometriosis lesions may be missed with ultrasound in the absence of a high level of expertise of sonographers. Similarly, we cannot exclude the small form of endometriosis in the control group due to the limitations of the non-invasive technique in their diagnosis.
Further, the concomitant association with adenomyosis, a potential risk factor of decreased implantation, was not evaluated in the studies considered [59]. Similarly, the association with other causes of infertility (such as both male and female factors) that may affect IVF outcome independently by endometriosis could not be extracted by the studies considered. Finally, it cannot be ignored that the patients of some studies might have received medical or surgical therapy without being reported.
4.3. Interpretation
In this systematic review and meta-analysis, which included 40 studies, we compared 8970 infertile women with endometriosis and 42,946 controls with other causes of infertility. Our findings suggest that endometriosis at all stages does not impact major fertility outcomes such as live birth, clinical pregnancy, and fertilization rates but is associated with a decreased implantation rate. These results align with the findings of Qu et al. [60], who also found a significant difference in implantation rate among women undergoing IVF/ICSI with or without endometriosis. They also demonstrated that the endometriosis and control group had similar pregnancy, live birth, and fertilization rates. Unlike our study, their exclusion criteria were less stringent (the single criterion of exclusion was egg donation), potentially weakening their findings. To mitigate this, we carefully selected studies that excluded patients who had undergone any previous medical or surgical interventions.
The reduction in the implantation rate of women with endometriosis is of interest. This finding may have a triple etiology: reduced oocyte and embryo quality, endometrial receptivity defect, and an altered interaction between the embryo and the endometrium. Our analysis did not allow us to differentiate the role of these potential factors, and it is not possible to disregard that this may play a different role in each woman.
A limitation of our study is the lack of differentiation by disease stage. Harb et al. [60] found over a decade ago that severe endometriosis (stages III/IV) is associated with a reduction in implantation and clinical pregnancy rates, with a trend towards reduced live births that did not reach statistical significance, whereas mild endometriosis (stage I/II) did not seem to affect these outcomes. However, their study included publications from 1985, and IVF techniques have evolved since then, which is why we included only studies from 2010 onwards.
Our study shows that endometriosis is associated with a reduced implantation rate. Successful implantation involves coordinated interactions between a receptive endometrium and a fertilized oocyte, suggesting multiple causal links between endometriosis and reduced implantation rates [61]. Abnormal inflammatory factors in women with endometriosis can lead to a hormonal imbalance, affecting estradiol secretion and progesterone resistance [10], which, in turn, may modify endometrial receptivity. Additionally, ectopic endometrial tissue in these women shows significant biochemical and ultrastructural differences from normal tissue [62]. Further, women with endometriosis may have a lower implantation rate due to oocyte and consequent embryo quality or different [63]. These findings could have clinical implications and justify the development of personalized pre-implantation protocols for women with endometriosis scheduled for IVF. Future research agenda will include the search for a specific genetic profile of women with endometriosis and a transcriptomic analysis of the endometrium leading to targeted treatments on the individual mechanism inducing endometriosis-related infertility.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare12232435/s1, List of excluded studies, Prisma checklist, Supplementary Figures S1–S4.
Author Contributions
Conceptualization, I.M. and G.R.; writing—original draft preparation, I.M., Z.P.P. and C.P.; writing—review and editing, G.R., I.M., D.D.M., A.G., L.M., F.D., G.R., G.M., F.G. and M.C.; visualization, Z.P.P., I.M. and C.P.; supervision, G.R. and I.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Available from the authors at reasonable request.
Acknowledgments
This study was performed as part of the Master thesis of I.M. (Continuing Education in the Biotechnology of Human Assisted Reproduction and Embryology Universitat de València, Spain).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Johnson, N.P.; Hummelshoj, L.; Adamson, G.D.; Keckstein, J.; Taylor, H.S.; Abrao, M.S.; Bush, D.; Kiesel, L.; Tamimi, R.; Sharpe-Timms, K.L.; et al. World Endometriosis Society consensus on the classification of endometriosis. Hum. Reprod. 2017, 32, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256. [Google Scholar] [CrossRef]
- Ozkan, S.; Murk, W.; Arici, A. Endometriosis and infertility: Epidemiology and evidence-based treatments. Ann. N. Y. Acad. Sci. 2008, 1127, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Boucher, A.; Brichant, G.; Gridelet, V.; Nisolle, M.; Ravet, S.; Timmermans, M.; Henry, L. Implantation Failure in Endometriosis Patients: Etiopathogenesis. J. Clin. Med. 2022, 11, 5366. [Google Scholar] [CrossRef]
- Muzii, L.; DITucci, C.; Galati, G.; Mattei, G.; Chinè, A.; Cascialli, G.; Palaia, I.; Benedetti Panici, P. Endometriosis-associated infertility: Surgery or IVF? Minerva Obs. Gynecol. 2021, 73, 226–232. [Google Scholar] [CrossRef] [PubMed]
- De Ziegler, D.; Borghese, B.; Chapron, C. Endometriosis and infertility: Pathophysiology and management. Lancet 2010, 376, 730–738. [Google Scholar] [CrossRef]
- Wang, X.M.; Ma, Z.Y.; Song, N. Inflammatory cytokines IL-6, IL-10, IL-13, TNF-α and peritoneal fluid flora were associated with infertility in patients with endometriosis. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 2513–2518. [Google Scholar] [CrossRef]
- Hogg, C.; Horne, A.W.; Greaves, E. Endometriosis-Associated Macrophages: Origin, Phenotype, and Function. Front. Endocrinol. 2020, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Jeljeli, M.; Riccio, L.G.C.; Chouzenoux, S.; Moresi, F.; Toullec, L.; Doridot, L.; Nicco, C.; Bourdon, M.; Marcellin, L.; Santulli, P.; et al. Macrophage Immune Memory Controls Endometriosis in Mice and Humans. Cell Rep. 2020, 33, 108325. [Google Scholar] [CrossRef]
- Coccia, M.E.; Nardone, L.; Rizzello, F. Endometriosis and Infertility: A Long-Life Approach to Preserve Reproductive Integrity. Int. J. Environ. Res. Public. Health 2022, 19, 6162. [Google Scholar] [CrossRef]
- Marquardt, R.M.; Kim, T.H.; Shin, J.H.; Jeong, J.W. Progesterone and Estrogen Signaling in the Endometrium: What Goes Wrong in Endometriosis? Int. J. Mol. Sci. 2019, 20, 3822. [Google Scholar] [CrossRef] [PubMed]
- Leyendecker, G.; Kunz, G.; Wildt, L.; Beil, D.; Deininger, H. Uterine hyperperistalsis and dysperistalsis as dysfunctions of the mechanism of rapid sperm transport in patients with endometriosis and infertility. Hum. Reprod. 1996, 11, 1542–1551. [Google Scholar] [CrossRef]
- Sanchez, A.M.; Viganò, P.; Somigliana, E.; Panina-Bordignon, P.; Vercellini, P.; Candiani, M. The distinguishing cellular and molecular features of the endometriotic ovarian cyst: From pathophysiology to the potential endometrioma-mediated damage to the ovary. Hum. Reprod. Update. 2014, 20, 217–230. [Google Scholar] [CrossRef]
- Pirtea, P.; de Ziegler, D.; Ayoubi, J.M. Endometrial receptivity in adenomyosis and/or endometriosis. Fertil Steril. 2023, 119, 741–745. [Google Scholar] [CrossRef]
- Abramiuk, M.; Grywalska, E.; Małkowska, P.; Sierawska, O.; Hrynkiewicz, R.; Niedźwiedzka-Rystwej, P. The Role of the Immune System in the Development of Endometriosis. Cells. 2022, 11, 2028. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.G.; Lenk, E.E.; Lebovic, D.I.; Shu, Y.; Yu, J.; Taylor, R.N. Pathogenesis of endometriosis: Interaction between Endocrine and inflammatory pathways. Best. Pract. Res. Clin. Obstet. Gynaecol. 2018, 50, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Invernici, D.; Reschini, M.; Benaglia, L.; Somigliana, E.; Galati, G.; La Vecchia, I.; Vigano’, P.; Vercellini, P. The impact of endometriosis on IVF efficacy: Qualitative and quantitative assessment of ovarian response and embryo development. Reprod. Biomed. Online. 2022, 45, 275–281. [Google Scholar] [CrossRef]
- Chen, J.-P.; Zhang, Y.-Y.; Jin, J.-N.; Ying, Y.; Song, Z.-M.; Xu, Q.-Q.; Tu, M.-X.; Ye, X.-H.; Tang, H.-N.; Ni, F.-D.; et al. Effects of Dysregulated Glucose Metabolism on the Occurrence and ART Outcome of Endometriosis. Eur. J. Med. Res. 2023, 28, 305. [Google Scholar] [CrossRef]
- Cathelain, A.; Simon, V.; Wattier, J.M.; Robin, G.; Ramdane, N.; Decanter, C.; Plouvier, P.; Rubod, C. Pain Assessment in Women with or without Endometriosis during the IVF Process: A Prospective Study. Reprod. BioMedicine Online 2023, 47, 103250. [Google Scholar] [CrossRef]
- Bourdon, M.; Alwohaibi, A.; Maignien, C.; Marcellin, L.; Chargui, A.; Pocate Cheriet, K.; Patrat, C.; Chapron, C.; Santulli, P. IVF/ICSI Outcomes After a Freeze-All Strategy: An Observational Cohort Study. Reprod. Sci. 2023, 30, 2283–2291. [Google Scholar] [CrossRef]
- Li, Y.; Wang, N.; Jing, Y.; He, J.; Li, F.; Zhang, X. Down-Regulation of the FTO Gene in Follicular Fluid of Infertile Women with Ovarian Endometriosis. Gynecol. Endocrinol. 2023, 39, 2269273. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yi, Y.-C.; Guu, H.-F.; Chen, Y.-F.; Kung, H.-F.; Chang, J.-C.; Chen, L.-Y.; Chuan, S.-T.; Chen, M.-J. Impact of Adenomyosis and Endometriosis on IVF/ICSI Pregnancy Outcome in Patients Undergoing Gonadotropin-Releasing Hormone Agonist Treatment and Frozen Embryo Transfer. Sci. Rep. 2023, 13, 6741. [Google Scholar] [CrossRef] [PubMed]
- Osmanlıoğlu, Ş.; Berker, B.; Aslan, B.; Şükür, Y.E.; Özmen, B.; Sönmezer, M.; Atabekoğlu, C.S.; Aytaç, R. Presence of Endometrioma Does Not Impair Embryo Quality and Assisted Reproductive Technology (ART) Cycle Outcome in Diminished Ovarian Reserve (DOR) Patients. Reprod. Sci. 2023, 30, 1540–1547. [Google Scholar] [CrossRef]
- Deng, Y.; Ou, Z.; Yin, M.; Chen, Z.; Chen, S.; Sun, L. Does Current Ovarian Endometrioma Increase the Time for DOR Patients to Reach Live Birth in IVF? BMC Pregnancy Childbirth 2022, 22, 324. [Google Scholar] [CrossRef]
- Zhou, L.; Wang, L.; Geng, Q.; Zhang, H.; Xu, S.; Diao, L.; Zeng, Y.; Mo, M.; Li, L. Endometriosis Is Associated with a Lowered Cumulative Live Birth Rate: A Retrospective Matched Cohort Study Including 3071 in Vitro Fertilization Cycles. J. Reprod. Immunol. 2022, 151, 103631. [Google Scholar] [CrossRef]
- Wu, Y.; Yang, R.; Lan, J.; Lin, H.; Jiao, X.; Zhang, Q. Ovarian Endometrioma Negatively Impacts Oocyte Quality and Quantity But Not Pregnancy Outcomes in Women Undergoing IVF/ICSI Treatment: A Retrospective Cohort Study. Front. Endocrinol. 2021, 12, 739228. [Google Scholar] [CrossRef] [PubMed]
- Boucret, L.; Bouet, P.-E.; Riou, J.; Legendre, G.; Delbos, L.; Hachem, H.E.; Descamps, P.; Reynier, P.; May-Panloup, P. Endometriosis Lowers the Cumulative Live Birth Rates in IVF by Decreasing the Number of Embryos but Not Their Quality. J. Clin. Med. 2020, 9, 2478. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, N.; Ceran, M.U.; Ugurlu, E.N.; Gulerman, H.C.; Ustun, Y.E. Impact of Endometrioma and Bilaterality on IVF/ICSI Cycles in Patients with Endometriosis. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 101839. [Google Scholar] [CrossRef]
- Feichtinger, M.; Nordenhök, E.; Olofsson, J.I.; Hadziosmanovic, N.; Rodriguez-Wallberg, K.A. Endometriosis and Cumulative Live Birth Rate after Fresh and Frozen IVF Cycles with Single Embryo Transfer in Young Women: No Impact beyond Reduced Ovarian Sensitivity—A Case Control Study. J. Assist. Reprod. Genet. 2019, 36, 1649–1656. [Google Scholar] [CrossRef]
- Ferreira, E.M.; Giorgi, V.S.I.; Rodrigues, J.K.; De Andrade, A.Z.; Junior, A.A.J.; Navarro, P.A. Systemic Oxidative Stress as a Possible Mechanism Underlying the Pathogenesis of Mild Endometriosis-Related Infertility. Reprod. BioMedicine Online 2019, 39, 785–794. [Google Scholar] [CrossRef]
- Sharma, S.; Bathwal, S.; Agarwal, N.; Chattopadhyay, R.; Saha, I.; Chakravarty, B. Does Presence of Adenomyosis Affect Reproductive Outcome in IVF Cycles? A Retrospective Analysis of 973 Patients. Reprod. BioMedicine Online 2019, 38, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Ozgur, K.; Bulut, H.; Berkkanoglu, M.; Coetzee, K. Reproductive Outcomes of Segmented In Vitro Fertilization in Patients Diagnosed with Endometriomas. J. Minim. Invasive Gynecol. 2018, 25, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Muteshi, C.M.; Ohuma, E.O.; Child, T.; Becker, C.M. The Effect of Endometriosis on Live Birth Rate and Other Reproductive Outcomes in ART Cycles: A Cohort Study. Hum. Reprod. Open 2018, 2018, hoy016. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, A.; Johnstone, E.B.; Bloom, M.S.; Huddleston, H.G.; Fujimoto, V.Y. A Higher Prevalence of Endometriosis among Asian Women Does Not Contribute to Poorer IVF Outcomes. J. Assist. Reprod. Genet. 2017, 34, 765–774. [Google Scholar] [CrossRef]
- Shebl, O.; Sifferlinger, I.; Habelsberger, A.; Oppelt, P.; Mayer, R.B.; Petek, E.; Ebner, T. Oocyte Competence in in Vitro Fertilization and Intracytoplasmic Sperm Injection Patients Suffering from Endometriosis and Its Possible Association with Subsequent Treatment Outcome: A Matched Case–Control Study. Acta Obstet. Gynecol. Scand. 2017, 96, 736–744. [Google Scholar] [CrossRef] [PubMed]
- González-Comadran, M.; Schwarze, J.E.; Zegers-Hochschild, F.; Souza, M.D.C.B.; Carreras, R.; Checa, M.Á. The Impact of Endometriosis on the Outcome of Assisted Reproductive Technology. Reprod. Biol. Endocrinol. 2017, 15, 8. [Google Scholar] [CrossRef]
- Queiroz Vaz, G.; Evangelista, A.V.; Almeida Cardoso, M.C.; Gallo, P.; Erthal, M.C.; Pinho Oliveira, M.A. Frozen Embryo Transfer Cycles in Women with Deep Endometriosis. Gynecol. Endocrinol. 2017, 33, 540–543. [Google Scholar] [CrossRef]
- Coelho Neto, M.A.; de P. Martins, W.; da Luz, C.M.; Jianini, B.T.G.M.; Ferriani, R.A.; Navarro, P.A. Endometriosis, Ovarian Reserve and Live Birth Rate Following In Vitro Fertilization/Intracytoplasmic Sperm Injection. Rev. Bras. Ginecol. Obstet. 2016, 38, 218–224. [Google Scholar] [CrossRef]
- Senapati, S.; Sammel, M.D.; Morse, C.; Barnhart, K.T. Impact of Endometriosis on in Vitro Fertilization Outcomes: An Evaluation of the Society for Assisted Reproductive Technologies Database. Fertil. Steril. 2016, 106, 164–171.e1. [Google Scholar] [CrossRef]
- González-Foruria, I.; Peñarrubia, J.; Borràs, A.; Manau, D.; Casals, G.; Peralta, S.; Creus, M.; Ferreri, J.; Vidal, E.; Carmona, F.; et al. Age, Independent from Ovarian Reserve Status, Is the Main Prognostic Factor in Natural Cycle in Vitro Fertilization. Fertil. Steril. 2016, 106, 342–347.e2. [Google Scholar] [CrossRef]
- Nakagawa, K.; Hisano, M.; Sugiyama, R.; Yamaguchi, K. Measurement of Oxidative Stress in the Follicular Fluid of Infertility Patients with an Endometrioma. Arch. Gynecol. Obstet. 2016, 293, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Coelho Neto, M.A.; Martins, W.P.; Lima, M.L.S.; Barbosa, M.A.P.; Nastri, C.O.; Ferriani, R.A.; Navarro, P.A. Ovarian Response Is a Better Predictor of Clinical Pregnancy Rate Following Embryo Transfer than Is Thin Endometrium or Presence of an Endometrioma: Thin Endometrium, Endometrioma and Clinical Pregnancy. Ultrasound Obstet. Gynecol. 2015, 46, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Borges, E., Jr.; Braga, D.P.A.F.; Setti, A.S.; Vingris, L.S.; Figueira, R.C.S.; Iaconelli, A., Jr. Endometriosis Affects Oocyte Morphology in Intracytoplasmic Sperm Injection Cycles. JBRA Assist. Reprod. 2015, 19, 235–240. [Google Scholar] [CrossRef]
- Polat, M.; Boynukalın, F.K.; Yaralı, İ.; Esinler, İ.; Yaralı, H. Endometriosis Is Not Associated with Inferior Pregnancy Rates in in Vitro Fertilization: An Analysis of 616 Patients. Gynecol. Obstet. Invest. 2014, 78, 59–64. [Google Scholar] [CrossRef]
- Łukaszuk, K.; Kunicki, M.; Liss, J.; Bednarowska, A.; Jakiel, G. Probability of Live Birth in Women with Extremely Low Anti-Müllerian Hormone Concentrations. Reprod. BioMedicine Online 2014, 28, 64–69. [Google Scholar] [CrossRef][Green Version]
- Ashrafi, M.; Fakheri, T.; Kiani, K.; Sadeghi, M.; Akhoond, M.R. Impact of the Endometrioma on Ovarian Response and Pregnancy Rate in in Vitro Fertilization Cycles. Int. J. Fertil. Steril. 2014, 8, 29–34. [Google Scholar] [PubMed]
- Du, Y.-B.; Gao, M.-Z.; Shi, Y.; Sun, Z.-G.; Wang, J. Endocrine and Inflammatory Factors and Endometriosis-Associated Infertility in Assisted Reproduction Techniques. Arch. Gynecol. Obstet. 2013, 287, 123–130. [Google Scholar] [CrossRef]
- Benaglia, L.; Bermejo, A.; Somigliana, E.; Faulisi, S.; Ragni, G.; Fedele, L.; Garcia-Velasco, J.A. In Vitro Fertilization Outcome in Women with Unoperated Bilateral Endometriomas. Fertil. Steril. 2013, 99, 1714–1719. [Google Scholar] [CrossRef]
- Benaglia, L.; Bermejo, A.; Somigliana, E.; Scarduelli, C.; Ragni, G.; Fedele, L.; Garcia-Velasco, J.A. Pregnancy Outcome in Women with Endometriomas Achieving Pregnancy through IVF. Hum. Reprod. 2012, 27, 1663–1667. [Google Scholar] [CrossRef]
- Lin, X.-N.; Wei, M.-L.; Tong, X.-M.; Xu, W.-H.; Zhou, F.; Huang, Q.-X.; Wen, G.-F.; Zhang, S.-Y. Outcome of in Vitro Fertilization in Endometriosis-Associated Infertility: A 5-Year Database Cohort Study. Chin. Med. J. 2012, 125, 2688–2693. [Google Scholar]
- Rajani, S.; Chattopadhyay, R.; Goswami, S.K.; Ghosh, S.; Sharma, S.; Chakravarty, B. Assessment of Oocyte Quality in Polycystic Ovarian Syndrome and Endometriosis by Spindle Imaging and Reactive Oxygen Species Levels in Follicular Fluid and Its Relationship with IVF-ET Outcome. J. Hum. Reprod. Sci. 2012, 5, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Matalliotakis, I.M.; Sakkas, D.; Illuzzi, J.; Matalliotaki, C.; Arici, A. Implantation Rate Remains Unaffected in Women with Endometriosis Compared to Tubal Factor Infertility. J. Endometr. 2011, 3, 86–92. [Google Scholar] [CrossRef]
- Mohamed, A.M.F.; Chouliaras, S.; Jones, C.J.P.; Nardo, L.G. Live Birth Rate in Fresh and Frozen Embryo Transfer Cycles in Women with Endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 156, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Ahn, J.; Kim, S.; Chae, H.; Kang, B. Effects on in Vitro Fertilization–Embryo Transfer Outcomes of Vascular Endothelial Growth Factor Receptor-1, -2 and -3 in Eutopic Endometrial Tissue of Women with Endometriosis. J. Obs. Gynaecol. 2011, 37, 1631–1637. [Google Scholar] [CrossRef]
- Coccia, M.E.; Rizzello, F.; Mariani, G.; Bulletti, C.; Palagiano, A.; Scarselli, G. Impact of Endometriosis on in Vitro Fertilization and Embryo Transfer Cycles in Young Women: A Stage-dependent Interference. Acta Obs. Gynecol. Scand. 2011, 90, 1232–1238. [Google Scholar] [CrossRef]
- Mathieu d’Argent, E.; Coutant, C.; Ballester, M.; Dessolle, L.; Bazot, M.; Antoine, J.-M.; Daraï, E. Results of First in Vitro Fertilization Cycle in Women with Colorectal Endometriosis Compared with Those with Tubal or Male Factor Infertility. Fertil. Steril. 2010, 94, 2441–2443. [Google Scholar] [CrossRef]
- Thompson, S.G. Why sources of heterogeneity in meta-analysis should be investigated. BMJ 1994, 309, 1351–1355. [Google Scholar] [CrossRef]
- Cozzolino, M.; Tartaglia, S.; Pellegrini, L.; Troiano, G.; Rizzo, G.; Petraglia, F. The Effect of Uterine Adenomyosis on IVF Outcomes: A Systematic Review and Meta-analysis. Reprod. Sci. 2022, 29, 3177–3193. [Google Scholar] [CrossRef]
- Qu, H.; Du, Y.; Yu, Y.; Wang, M.; Han, T.; Yan, L. The effect of endometriosis on IVF/ICSI and perinatal outcome: A systematic review and meta-analysis. J. Gynecol. Obstet. Hum. Reprod. 2022, 51, 102446. [Google Scholar] [CrossRef]
- Harb, H.M.; Gallos, I.D.; Chu, J.; Harb, M.; Coomarasamy, A. The effect of endometriosis on in vitro fertilisation outcome: A systematic review and meta-analysis. BJOG 2013, 120, 1308–1320. [Google Scholar] [CrossRef]
- Bulun, S.E.; Cheng, Y.H.; Pavone, M.E.; Xue, Q.; Attar, E.; Trukhacheva, E.; Tokunaga, H.; Utsunomiya, H.; Yin, P.; Luo, X.; et al. Estrogen receptor-beta, estrogen receptor-alpha, and progesterone resistance in endometriosis. Semin. Reprod. Med. 2010, 28, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Selam, B.; Arici, A. Implantation defect in endometriosis: Endometrium or peritoneal fluid. J. Reprod. Fertil. Suppl. 2000, 55, 121–128. [Google Scholar] [PubMed]
- Goyri, E.; Kohls, G.; Garcia-Velasco, J. IVF stimulation protocols and outcomes in women with endometriosis. Best. Pract. Res. Clin. Obstet. Gynaecol. 2024, 92, 102429. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).