Abstract
There is increasing attention to suicides that occur in view of others, as these deaths can cause significant psychological impact on witnesses. This study illuminates characteristics of witnessed suicides and compares characteristics of these deaths to non-witnessed suicides. We develop a codable definition of what constitutes witnessed (vs. non-witnessed) suicide. Our data include a sample of 1200 suicide descriptions from the 2003–2017 National Violent Death Reporting System (NVDRS). We first developed criteria to identify probable cases of witnessed suicide. The coding scheme achieved 94.5% agreement and identified approximately 10% (n = 125) of suicides as witnessed. Next, we examined differences between witnessed and non-witnessed suicides in demographics, manner of death, and social/environmental factors using bivariate Chi-squared tests, multivariate logistic regression, and ANOVA. Witnessed suicide decedents were significantly more likely than non-witnessed suicide decedents to be male, younger, and members of a sexual minority, and to have died in living spaces by means of a firearm. Two thirds of witnesses were strangers to the decedents, while 23.2% were romantic partners or ex-partners of the decedents. Our coding method offers a reliable approach to identify witnessed suicides. While witnessed suicides are relatively infrequent, these deaths have profound impact on witnesses. Articulating the features of witnessed suicides may contribute to identifying potential risk mitigation strategies.
1. Introduction
In 2021, there were an estimated 47,646 deaths due to suicide in the United States—a 4% increase from 2020 [1]. It has been estimated that for each suicide, 135 other people are affected by the death, and of those 22% experience subsequent guilt, anger, shock, and depression [2]. Although the majority of suicides occur in the decedent’s home while alone and in private areas (e.g., bedrooms, closets, and bathrooms), increasingly a subset of suicides take place within view of others, such as using a firearm in the presence of other people, jumping in front of trains or subways, or leaping from bridges [3,4]. This has been referred to as witnessed suicide [5,6]. Studies have found that 4–10% of suicides are witnessed [5,6,7,8,9]. Although relatively rare, their impact on witnesses can be profound [10,11,12,13]. Studies documenting the mental health state of “survivor-victims,” or those who have witnessed a suicide, have observed that these individuals commonly experience strong feelings of shame, guilt, and anger [5,6,14]. One study found that survivor-victims “are obsessed with thoughts of death, seeking reasons, casting blame, and often punishing themselves” [15].
Research on witnessed suicides has investigated their likely locations and circumstances, as well as characteristics of decedents and witnesses. For example, one study examined suicides from the Golden Gate Bridge, a widely known and very public location that averages 30 suicides a year [16]. These deaths are likely to be witnessed. Decedents who jumped typically have histories of psychiatric diagnoses including schizophrenia or psychosis [16,17,18]. Railway or subway locations also present another suicide location that is likely to be witnessed. A majority of decedents in railway- or subway-linked suicides have been found to also have previous psychiatric hospitalization and evidenced aberrant behaviors pre-death while on the station platform [19,20,21,22,23].
While witnessed suicides are often traumatic for the observer, they may also offer opportunities for interventions from observers. To that end, articulating common patterns of relationship between decedents and witnesses and identifying likely methods and locations of witnessed successful suicides as well as possible motivations of the decedent could contribute to preventative measures by identifying high risk situations [4]. In the current study, we develop a standardized definition of what constitutes witnessed (vs. non-witnessed suicide). Then, we apply our approach to identify decedent characteristics, location, and relationship to witnesses, employing narratives from the National Violent Death Reporting System (NVDRS). As our work is part of a larger study on identifying sexual orientation and characteristics of suicide in the NVDRS [24,25], we selected our sample, in part, on the NVDRS coded sexual orientation status of the decedent to ensure that our definition would be inclusive of the suicide circumstances of this population.
2. Materials and Methods
2.1. Data Source
We used information drawn from the 2003–2017 NVDRS. Established by the Centers for Disease Control and Prevention in 2002, the 2003–2017 NVDRS database includes reports from approximately 325,000 violent deaths. Over time, the NVDRS has incorporated reports from an increasing number of states, with 34 reporting in the 2017 year of the database [26]. The NVDRS is a compilation of both close-ended information (e.g., demographic information, decedent characteristics) and potentially two narrative reports written by a trained state-level public health worker, one summarizing law enforcement records and the other coroner/medical examiner files (LE/CME). Narratives can include information such as decedent demographics, place and cause of death, toxicology results, and method of death (see references for more details) [25,27]. This study was exempt from human subjects review.
We first restricted the sample to deaths where the manner of death was determined to be suicide or homicide/suicide (n = 203,715). From this, we drew three samples: a systematic sample of 620 LGBT deaths described in Lyons et al. [24]; all deaths coded by the NVDRS as having a lesbian, gay, bisexual, or transgender (LGBT) identity not included in the Lyons et al. sample (n = 1028); and then a 10% simple random sample of the remaining suicide deaths (n = 20,376). From these deaths, we randomly selected 1200 for study. Coders were blind as to the original sexual orientation coding of the decedent.
2.2. Methods for Case Classification of Witnessed Suicide
2.2.1. Definition of Witnessed Suicide
The NVDRS does not code whether a suicide case is witnessed or non-witnessed. To develop criteria for case classification, five coders, all with previous training in suicide prevention, were tasked with developing a coding system. After reading subsets of the study narratives, they derived inclusion and exclusion criteria for case classification. In addition, they developed a coding sheet with examples to guide naïve coders. For this study, they defined a witnessed suicide as any suicide in which the decedent died in a location where an individual or individuals either observed the death as it happened or were highly likely to observe the suicide. Locations open to public access (i.e., commercial buildings, educational institutions, houses of worship, government buildings, healthcare facilities, and unobstructed open areas) were considered public areas with a high probability of individuals witnessing the suicide. Additionally, all cases where the method of death was a jump or fall from public areas, railroads, and subways was deemed a witnessed suicide. Furthermore, deaths arising in the context of Russian roulette games with more than one person were coded as witnessed suicides. Area locations with low likelihood of a witness observing the suicide, such as in the decedent’s own vehicle in a parking lot, obstructed public areas such as alleys, or private office spaces, were not included and would fall into non-witnessed suicides. Unless a witness was explicitly mentioned, all private residential areas and private rooms within public locations (i.e., areas only open to employees or staff, personal offices, closets, etc.) were not coded as witnessed suicide and were classified as non-witnessed cases. Cases in which an individual overheard the suicide occurring, such as a gunshot from a different room or over a phone call, were not included as witnessed but categorized as non-witnessed cases. Lastly, cases in which a witness observed an act of suicide such as swallowing pills were considered to be witnessed suicides.
2.2.2. Coding Procedures and Inter-rater Agreement
To arrive at a reliable coding scheme (see Table 1), narrative cases were randomly distributed in seven separate batches. The first 50 cases in Batch One served as training cases to develop coding criteria. Batch Two contained an additional 50 cases, Batch Three 200 cases, Batch Four 300 cases, Batch Five 98 cases, Batch Six 199 cases, and Batch Seven 203 cases, for a total of n = 1200 cases. Coders began with small batches, and then batches were increased in size. Batches sometimes varied based on the selection rubric that ensured cases from the three categories explained above. Each coder used binary coding (0, 1) to classify the presence or absence of witnessed suicide. A four out of five consensus was considered reliable to code the presence/absence of witnessed suicide. Following the coding of each batch, the coders received a report of their agreement/disagreement and reviewed cases with disagreements. Cases where four out of five coders subsequently agreed were deemed consensuses. To strengthen the reliability of the coding, discussions surrounding what classified a highly probably location evolved after discussing Batch Two. For example, locations of low obstruction (e.g., fewer cars, buildings, or trees) may still have a high or low probability of being in view of a witness depending on the foot traffic in that area.

Table 1.
Definition and coding for witnessed suicide using the NVDRS data 2003–2017.
After re-coding Batches One through Four based on refinement of locations, the definition of witnessed suicide was changed from a mandatory observation of the suicide to also include cases in which there was a high probability of observation. After coding all seven batches, the overall inter-rater agreement was still deemed inadequate, so the witnessed suicide locations were broadened to include types of locations from the Federal Bureau of Investigation (FBI) that are used to classify locations of active shooter incidents in the United States [28]. Coder agreement increased with this additional information. After all seven batches were coded, inter-rater agreement for two of the five coders stood out as consistently poor. These two were paired with coders who had high consistencies of coding. In these matched pairs, the inconsistent coder reviewed 25 cases, explained their rationale, and then to listened to the consistent coder’s view of the same case. This process provided the inconsistent coder with feedback and cognitively shifted understanding of the witnessed suicide criteria. Following this entire process, all coders returned to Batches One through Seven to recode any further disagreements; inter-rater reliability for witnessed suicide at this point reached 94.5% agreement. The agreement between the coders was measured using Fleiss’ kappa [29], which is commonly used for categorical outcomes with more than 2 raters. The calculation was performed using the “irr” package in R [30]. Fleiss’ kappa takes values between −1 and 1. Specifically, values between 0.41 and 0.6 are considered as moderate, values between 0.61 and 0.8 are considered as good, and values between 0.81 and 1 are considered as very good. The pattern of coding review is described in Figure 1.
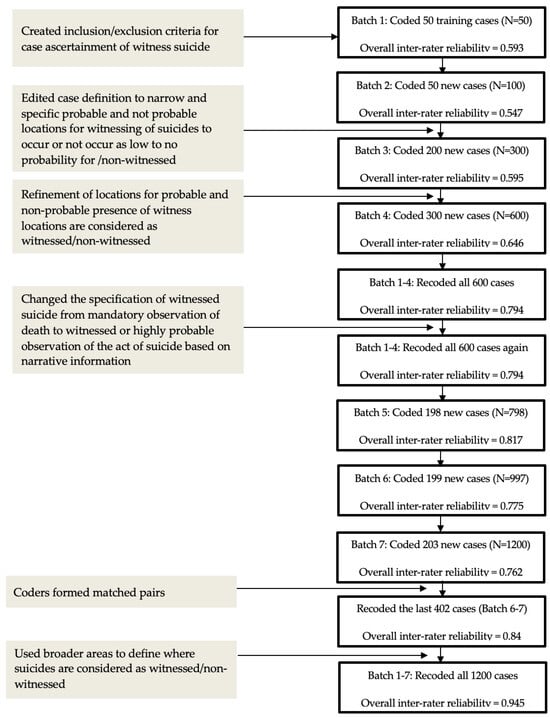
Figure 1.
Inter-rater agreement of coding for witnessed suicide using the National Violent Death Reporting System 2003–2017 narratives.
Of 1200 cases coded, 125 deaths were categorized as witnessed suicides. From the NVDRS narratives, we also coded decedents’ sex (male and female), sexual orientation (lesbian, gay, bisexual, heterosexual, and unknown or missing), transgender identity, and age as well as contextual variables including method of death (pills, fall, firearm, impact from vehicle (non-driver), impact from vehicle (driver), carbon monoxide poisoning, hanging, and stabbing/cutting), location of death (places of commerce, government buildings, open space, educational institutions/office spaces, houses of worship, and communal residences), and relationship of witness to the decedent (romantic (ex-)partner, blood relative, friend/acquaintance, and stranger). Narratives in which a witness was not explicitly mentioned, but where there was a probable presence of a witness, were coded as “stranger”.
We then compared our coding of these variables from the narratives to ones included in the NVDRS quantitative data that are coded by public health workers that prepare the files for the CDC. All of the variables above, with the exception of “relationship of the witness to the decedent,” are included in the NVDRS quantitative data file. Agreement between our coding of narratives on the variables above and the public health workers’ quantitative coding ranged from 98–100% with the exception of one variable essential to the witnessed suicide definition. The variable with lowest agreement (88%) was classification of a suicide occurring in an open space. For the analyses below, we use the original NVDRS variables as well as NVDRS public health coders’ designations for decedent’s race/ethnicity, educational attainment, marital status, military service history, and homeless status; whether financial problems appeared to have contributed to the death; whether the death occurred within one month of the decedent being released from or admitted to an institutional setting; suspected alcohol use in the hours preceding the incident; and, for decedents with a toxicology screen, blood alcohol content (BAC) and the use of marijuana and/or opiate drugs (toxicology results, however, are missing in over half of the cases).
2.2.3. Data Analytic Plan
Data analyses were conducted using R 4.0.2 (R Core Team, 2022) to investigate differences between suicides classified as witnessed and non-witnessed [31]. Initially, bivariate frequencies and percentages were computed. Chi-squared tests were used to compare features between witnessed and non-witnessed suicides while Fisher’s exact tests were used for some variables to accommodate sub-sample size(s) smaller than 5. Effect sizes from the Chi-squared tests are reported as Cramer’s V along with the Chi-squared statistics and their p-values. Then, a multivariate logistic regression was utilized to predict witness status, using the same variables as in the bivariate analyses as predictors. We report the adjusted odds ratio (OR) and 95% confidence intervals (CI), and we used the Wald Chi-squared test to determine the overall significance of each explanatory variable.
3. Results
3.1. Decedent Characteristics of Witnessed Suicide
The majority of the suicide decedents were male, between the age of 26 and 64 years, and non-Hispanic white, and about half had finished high school or completed some college (see Table 2). Decedents of witnessed suicide were also more likely to be homeless compared to decedents of non-witnessed suicide (4.0% vs. 0.7%). A common method of death regardless of being a witnessed or non-witnessed suicide was via firearms (42.4% vs. 42.0%). Falling was a prominent method in witnessed suicide (23.2%) vs. 0.2% in non-witnessed suicide. Witnessed suicides were also less likely to occur in living spaces than non-witnessed suicides (44.8% vs. 76.9%) and more likely to occur in public open spaces (33.6% vs. 8.1%). Based on the Cramer’s V values, age categories, race and ethnicity groups, and highest level of education are considered as having statistically significant association with the presence of witnessed suicide.

Table 2.
Characteristics by presence/absence of witnessed suicide for quantitative data from the 2003–2017 National Violent Death Reporting System (NVDRS) sample (n = 1200).
Generalized Variance Inflation Factor (GVIF) is small for all the predictors in our final logistic regression, indicating no violation of the no-collinearity assumption. Results from the Wald Chi-squared tests indicate that witnessed and non-witnessed suicides differed significantly in decedents’ ages and sexual orientations, and there is marginally significant association shown between highest level of education and witnessed suicide, while controlling for other predictors in the model (see Table 3). Based on the logistic regression results, in comparison to decedents whose highest levels of education were high school or less, decedents who received some college education were less likely to be classified as a witnessed suicide.

Table 3.
Predictors of witnessed suicide deaths in the 2003–2017 National Violent Death Reporting System (NVDRS) sample (n = 1200). The overall significance of each predictor was determined using ANOVA.
Decedents of witnessed suicides and non-witnessed suicides also significantly differed in the primary type of weapon and means involved. Suicides involving falling were more likely to be witnessed as opposed to non-witnessed. Locations of the suicides also varied; witnessed suicides were more likely to occur in public spaces—including open space, supervised public space, and transportation. Such interpretation is made based on the effect sizes, as these particular odds ratios are not statistically significant. Finally, marijuana use was significantly more likely to be present in witnessed suicides as compared to non-witnessed suicides.
Additional Characteristics from Narratives
In 42 (33.6%) of the witnessed suicide incidents, the decedents actively sought to suicide in front of a witness, while in the other 83 (66.4%) incidents, the presence of the witness(es) was incidental. Investigation regarding the relationship of witnesses to decedents determined that two thirds of witnesses were strangers to the decedents, while 23.2% were romantic partners or ex-partners. The remainder were relatives or friends/acquaintances.
4. Discussion
While witnessed suicides are relatively rare in comparison to non-witnessed suicides, their impact on those who witness the death can be powerful and enduring [4,5,6,15,32]. In the current study, we developed criteria and a reliable coding scheme to classify suicides for being witnessed or not using information available in the law enforcement and medical/coroner narratives contained within the 2003–2017 NVDRS. Using these classifications, we showed that the majority of witnessed suicide decedents are much younger than decedents from non-witnessed suicides. They are also more likely to be classified as lesbian, gay, or bisexual as opposed to no classification for sexual orientation status. Our deliberate inclusion of LGBT cases may provide some insights into the necessity for further research on sexual orientation as a risk indicator for witnessed suicide. The Interpersonal Theory of Suicide asserts that there are three criteria that must be present for one to have a heightened risk of suicide: (1) perceived burdensomeness, (2) thwarted belongingness, and (3) capability for suicide [33]. Previous studies have demonstrated that sexual minorities feel more isolated than their heterosexual counterparts, which meets the element for thwarted belongingness [34]. Additionally, in both the McDowell et al. (1994) and Ooi et al. (2020) studies, perceived abandonment/isolation and use of firearms were significant factors in witnessed suicides [4,8]. As such, not only does the isolation reported by LGBT individuals increase their risk of suicide, but it may also increase their risk of witnessed suicide, specifically. It is also the case that young LGBT individuals may be more likely to be at risk for homelessness or transient living arrangements particularly in early years of coming out, which may also contribute to witnessed suicide occurrence [35]. Further research would be necessary to confirm this possibility [36]. Given the discrimination and rejection experienced by LGBT populations [34,37,38], further explorations of this theme warrant attention.
Homelessness, falls, public open spaces, and transportation are all risk factors for witnessed suicide because the element that ties these disparate matters together is the fact that they inherently occur where others are likely to see them. Similarly, falling from heights, being in public open spaces, and driving a vehicle occur in locations where there is a high probability of being seen by another person.
Suicide via firearm was the most likely method for both witnessed and unwitnessed suicides. However, suicide through jumping or falling was the second most likely method of death for witnessed suicides, and the use of vehicle-related means was the third most likely method to be used. This differs from national statistics, which indicate the second and third most likely means of suicide-related deaths are suffocation and drug poisoning, respectively [1,39,40].
While the NVDRS narratives are somewhat limited in their description of witnesses and the relationship of witnesses to the decedent, previous studies have found that romantic partners are the most likely witnesses to a suicide [5,8]. Here, however, we found the majority of witnesses of NVDRS suicides were strangers, followed by romantic partners or ex-partners. This divergence could be due to our definition of witnessed suicide, which includes probable witnesses, as compared to existing studies, which specify only recorded witnesses. Our focus on locations where witnessed suicides are likely to occur—bridges, trains, and subway stations—may have increased the prevalence of strangers witnessing these deaths. Train and subway conductors, metal workers who attempt bridge rescues, and hotel staff for example are accidental bystanders. Location of suicide is an overlooked variable in suicidology, but yet it offers some insights into occupations of rescuers who are likely to be exposed to witnessed suicides [41,42]. Knowledge of locations in suicides increases knowledge of lethality and risk of being an unintended witness [43,44]. Studies have documented the impact of suicide in occupations such as first responders, mental health professionals, and others [45,46], but less attention has been paid to inadvertent bystanders who by virtue of their occupations may be exposed to the emotional distress of witnessing a suicide. There is a growing focus by suicide prevention and response agencies to “witness survivors” [47,48] and by suicide researchers seeking to address the mental health consequences of suicides [49,50], as well as public awareness of those who have had this experience and its impact on their mental health [51,52]. All three of these groups call for the need for greater attention to “suicide witness survivors”.
Results of our study also provide a case definition that can be applied to what a witnessed vs. non-witnessed suicide is, allowing researchers’ consistency in research approaches on the topic. Our coding system, if employed by large databases such as violent deaths at the local, state, or federal levels, could aid in identifying circumstances of particular occupations that may require specific training and resources to mitigate mental health consequences. In addition, following the efforts of New Hampshire’s Connect program identifying ways to reach those individuals who may be witnesses to get them into treatment if needed could be beneficial [47].
Results from this study should be contextualized by some of its limitations. First, only 1200 cases were selected for study on the assumption that witnessed suicide characteristics are randomly distributed and common in the data. A larger sample may have identified additional characteristics. Additionally, witnessed suicide is a relatively under-studied topic; thus, definitions of witnessed suicide are not well established. Compared to existing definitions, our definition of witnessed suicide includes locations identified as highly likely for a witness to be present and excludes non-visual forms of witnessing (e.g., overhearing a gunshot, being present via phone, etc.) [4,8]. These differences in the definition could impact the results and, subsequently, the implications and knowledge drawn from them. An additional limitation of the study is the NVDRS narratives themselves; the narratives are often short, terse, or nondescriptive of many death circumstances. Thus, our study coders coded conservatively. Despite these limitations, we were able to produce a coding schema with good inter-rater agreement that can identify cases of witnessed suicide from death narratives. Our inclusion of a subsample of LGBT individuals has verified that this approach can work with this vulnerable population.
5. Conclusions
In sum, investigating the nature of witnessed suicide and documenting its frequency and associated characteristics is possible given better methods for classifying these deaths. Identifying locations and occupations in which there are unintended mental health consequences from witnessed suicides provides an opportunity to address the risk for particular occupations [43]. In this study, we tested and developed a definition as well as reliable methods for coding witnessed suicides in the NVDRS. These coding criteria can be integrated into public health mortality surveillance systems. As the United States tries to reach its goal of zero suicides, it is important that we not overlook any methods for improvement of the use of suicide data that can decrease suicide and its associated morbidity.
Author Contributions
Conceptualization, V.M.M. and M.G.; coding development, M.G., V.N., J.R., A.E., Y.L., and M.B.; coding consultation, A.A.-K.; formal analysis, X.Z. and S.D.C.; writing—original draft preparation, J.R., V.M.M., and S.D.C.; writing—review and editing, A.A.-K., J.G.F., S.D.C., and V.M.M.; funding acquisition, V.M.M. and S.D.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by grants from the National Institute of Mental Health (MH115344), the National Institute of Minority Health and Health Disparities (MD006923), and the National Science Foundation Graduate Research Fellowship Program (DGE-1650604).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data for this study comes from the National Violent Death Reporting System Restricted Access Database (RAD), which is accessible to eligible researchers through agreement with the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
Acknowledgments
We would like to thank Ung Lik Teng, Colette Franz, Sherry Shi, Amir Bayat, Jessica Mangano, Chase Kapler, and Khang Tran for their assistance.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Curtin, S.C.; Garnett, M.F.; Ahmad, F.B. Provisional numbers and rates of suicide by month and demographic characteristics: United States, 2021. Natl. Vital Stat. Rep. 2021, 24, 60–84. [Google Scholar]
- Cerel, J.; Brown, M.M.; Maple, M.; Singleton, M.; Van de Venne, J.; Moore, M.; Flaherty, C. How many people are exposed to suicide? Not six. Suicide Life Threat. Behav. 2019, 49, 529–534. [Google Scholar] [CrossRef]
- Meyer, C.; Irani, T.; Hermes, K.; Yung, B. Explaining Suicide: Patterns, Motivations, and What Notes Reveal; Academic Press: London, UK, 2017. [Google Scholar]
- Ooi, T.H.; Irani, T.H.; Hermes, K.A.; Meyer, C.L. Deconstructing witnessed suicide: A portrait of those who die by suicide in front of others. Curr. Psychol. 2020, 28, 6481–6489. [Google Scholar] [CrossRef]
- Andress, V.R.; Corey, D.M. Survivor-victims: Who discovers or witnesses suicide? Psychol. Rep. 1978, 42, 759–764. [Google Scholar] [CrossRef]
- Agjei, R.O.; Kolog, E.A.; Dei, D.; Tengey, Y.T. Emotional impact of suicide on active witnesses: Predicting with machine learning. Adv. Sci. Technol. Eng. Syst. J. 2018, 3, 501–509. [Google Scholar] [CrossRef]
- Dorpat, T.; Ripley, H.A.A. A study of suicide in the Seattle area. Compr. Psychiatry 1963, 4, 117–123. [Google Scholar] [CrossRef]
- McDowell, C.P.; Rothberg, J.M.; Koshes, R.J. Witnessed suicides. Suicide Life Threat. Behav. 1994, 24, 213–223. [Google Scholar] [CrossRef]
- Padosch, S.A.; Schmidt, P.H.; Madea, B. Planned complex suicide by self-poisoning and a manipulated blank revolver: Remarkable findings due to multiple gunshot wounds and self-made wooden projectiles. J. Forensic Sci. 2003, 48, 1371–1378. [Google Scholar] [CrossRef]
- Zhao, C.; Zou, Y.; Cao, L. Traumatic stress disorder in witnesses to a suicide. Chin. Ment. Health J. 2006, 20, 252–255. [Google Scholar]
- Limosin, F.; Loze, J.; Cothereau, C.; Beaurepaire, C.D.; Payan, C.; Conso, F.; Hautecouverture, S.; Rouillon, F. A prospective study of the psychological effects of “person under train” incident on drivers. J. Psychiatr. Res. 2006, 40, 755–761. [Google Scholar] [CrossRef]
- Cothereau, C.; Beaurepaire, C.D.; Payan, C.; Cambou, J.P.; Rouillon, F.; Conso, F. Professional and medical outcomes for French train drivers after “person under train” accidents: Three-year follow up study. Occup. Environ. Med. 2004, 61, 488–494. [Google Scholar] [CrossRef] [PubMed]
- PTSD, UK. Causes of PTSD: Witnessing a Suicide. n.d. Available online: https://www.ptsduk.org/causes-of-ptsd-witnessing-a-suicide/ (accessed on 10 January 2023).
- Van Hooff, M.; McFarlane, A.C.; Baur, J.; Abraham, M.; Barnes, D.J. The stressor Criterion-A1 and PTSD: A matter of opinion? J. Anxiety Disord. 2009, 23, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Shneidman, E.S. Postvention and the Survivor-Victim. In Deaths of Man; The New York Times Book Quadrangle: New York, NY, USA, 1973; pp. 33–41. [Google Scholar]
- Blaustein, M.; Fleming, A. Suicide from the Golden Gate Bridge. Am. J. Psychiatry 2009, 166, 1111–1116. [Google Scholar] [CrossRef] [PubMed]
- Cantor, C.H.; Hill, M.A.; McLachlan, E.K. Suicide and related behaviour from river bridges. Br. J. Psychiatry 1989, 155, 829–835. [Google Scholar] [CrossRef] [PubMed]
- de Moore, G.M.; Robertson, A.R. Suicide attempts by firearms and by leaping from heights: A comparative study of survivors. Am. J. Psychiatry 1999, 156, 1425–1431. [Google Scholar] [CrossRef]
- San Too, L.; Milner, A.; Bugeja, L.; McClure, R. The socio-environmental determinants of railway suicide: A systematic review. BMC Public Health 2014, 14, 20. [Google Scholar] [CrossRef]
- Guggenheim, F.G.; Weisman, A.D. Suicide in the subway: Publicly witnessed attempts of 50 cases. J. Nerv. Ment. Dis. 1972, 155, 404–409. [Google Scholar] [CrossRef]
- Mishara, B.L.; Bardon, C.; Dupont, S. Can CCTV identify people in public transit stations who are at risk of attempting suicide? An analysis of CCTV video recordings of attempters and a comparative investigation. BMC Public Health 2016, 16, 1245. [Google Scholar] [CrossRef]
- Lukaschek, K.; Baumert, J.; Ladwig, K.H. Behaviour patterns preceding a railway suicide: Explorative study of German federal police officers’ experiences. BMC Public Health 2011, 11, 620. [Google Scholar] [CrossRef]
- Mackenzie, J.; Borrill, J.; Hawkins, E.; Fields, B.; Kruger, I.; Noonan, I.; Marzano, L. Behaviours preceding suicides at railway and underground locations: A multimethodological qualitative approach. BMJ Open 2018, 8, e021076. [Google Scholar] [CrossRef]
- Lyons, B.H.; Walters, M.L.; Jack, S.P.D.; Petrosky, E.; Blair, J.M.; Ivey-Stephenson, A.Z. Suicides among lesbian and gay male individuals: Findings from the National Violent Death Reporting System. Am. J. Prev. Med. 2019, 56, 512–521. [Google Scholar] [CrossRef]
- Arseniev-Koehler, A.; Cochran, S.; Mays, V.; Chang, K.; Foster, J.G. Integrating topic modeling and word embedding to characterize violent deaths. Proc. Natl. Acad. Sci. USA 2022, 119, e2108801119. [Google Scholar] [CrossRef] [PubMed]
- Paulozzi, L.J.; Mercy, J.; Frazier, L.; Annest, J.L. CDC’s National Violent Death Reporting System: Background and methodology. Inj. Prev. 2004, 10, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. National Violent Death Reporting System (NVDRS). CDC. 2021. Available online: https://www.cdc.gov/violenceprevention/datasources/nvdrs/index.html (accessed on 10 January 2023).
- Blair, J.P.; Schweit, K.W. A Study of Active Shooter Incidents, 2000–2013; Texas State University; Federal Bureau of Investigation, U.S. Department of Justice: Washington, DC, UA, 2014. Available online: https://www.fbi.gov/file-repository/active-shooter-study-2000-2013-1.pdf/view (accessed on 10 January 2023).
- Fleiss, J.L.; Cohen, J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ. Psychol. Meas. 1973, 33, 613–619. [Google Scholar] [CrossRef]
- Gamer, M.; Lemon, J.; Fellows, I.; Singh, P. irr: Various Coefficients of Inter-rater Reliability and Agreement. R Package Version 0.84.1. 2019. Available online: https://CRAN.R-project.org/package=irr (accessed on 24 August 2023).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 10 December 2022).
- Jakab, I.; Howard, M.C. Art therapy with a 12-year-old girl who witnessed suicide and developed school phobia. Psychother. Psychosom. 1969, 17, 309–324. [Google Scholar] [CrossRef] [PubMed]
- Van Orden, K.A.; Witte, T.K.; Cukrowicz, K.C.; Braithwaite, S.; Selby, E.A.; Joiner, T.E. The Interpersonal Theory of Suicide. Psychol. Rev. 2010, 117, 575–600. [Google Scholar] [CrossRef] [PubMed]
- Aparicio-Garcia, M.E.; Diaz-Ramiro, E.M.; Rubio-Valdehita, S.; Lopez-Nunez, M.I.; Garcia-Nieto, I. Protective factors, risk of violence and discrimination and mental health indicators of young LGB people. Int. J. Environ. Res. Public Health 2022, 19, 14401. [Google Scholar] [CrossRef]
- Fraser, B.; Pierse, N.; Chisholm, E.; Cook, H. LGBTIQ+ Homelessness: A Review of the Literature. Int. J. Environ. Res. Public Health 2019, 16, 2677. [Google Scholar] [CrossRef]
- Ormiston, C.K. LGBTQ Youth Homelessness: Why We Need to Protect Our LGBTQ Youth. LGBT Health 2022, 9, 217–221. [Google Scholar] [CrossRef]
- Mays, V.M.; Cochran, S.D. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. AJPH 2001, 91, 1869–1876. [Google Scholar] [CrossRef]
- Gmelin, J.H.; Vries, Y.A.D.; Baams, L.; Aguilar-Gaxiola, S.; Alonso, J.; Borges, G.; Bunting, B.; Cardoso, G.; Florescu, S.; Gureje, O.; et al. Increased risks for mental disorders among LGB individuals: Cross-national evidence from the World Mental Health Surveys. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 2319–2332. [Google Scholar] [CrossRef] [PubMed]
- Hedegaard, H.; Curtin, S.C.; Warner, M. Suicide rates in the United States continue to increase. In NCHS Data Brief; National Center for Health Statistics: Hyattsville, MD, USA, 2018. [Google Scholar]
- Pettrone, K.; Curtin, S.C. Urban-rural differences in suicide rates, by sex and three leading methods: United States, 2000–2018. In NCHS Data Brief; National Center for Health Statistics: Hyattsville, MD, USA, 2020; pp. 1–8. [Google Scholar] [PubMed]
- Wasserman, I.M.; Stack, S. Lethal locations: An application of opportunity theory to motel suicide, a research note. Death Stud. 2008, 32, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Mishara, B.L. Railway and metro suicides: Understanding the problem and prevention potential. Crisis 2007, 28, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Weisman, A.D.; Worden, W. Risk-rescue rating in suicide assessment. Arch. Gen. Psychiatry 1972, 26, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Zarkowski, P.; Avery, D. Hotel room suicide. Suicide Life Threat. Behav. 2011, 36, 578–581. [Google Scholar] [CrossRef]
- Lyra, R.L.; McKenzie, S.K.; Every-Palmer, S.; Jenkin, G. Occupational exposure to suicide: A review of research on the experiences of mental health professionals and first responders. PLoS ONE 2021, 16, e0251038. [Google Scholar] [CrossRef] [PubMed]
- Hom, M.A.; Stanley, I.H.; Spencer-Thomas, S.; Joiner, T.E. Exposure to suicide and suicide bereavement among women firefighters: Associated suicidality and psychiatric symptoms. J. Clin. Psychol. 2018, 74, 2219–2237. [Google Scholar] [CrossRef]
- Greenleaf, C. New Approaches to Helping the Witness to A Suicide: The Suicide Witness Survivor Outreach Program of NAMI New Hampshire. Available online: https://theconnectprogram.org/wp-content/uploads/2018/11/witnesssurvivor-final.pdf (accessed on 23 August 2023).
- Witnesses—Support after Suicide. Available online: https://supportaftersuicide.org.uk/i-didnt-know-the-person/ (accessed on 23 August 2023).
- Cerel, J.; Maple, M.; van de Venne, J.; Moore, M.; Flaherty, C.; Brown, M. Exposure to Suicide in the Community: Prevalence and Correlates in One U.S. State. Public Health Rep. 2016, 131, 100–107. [Google Scholar] [CrossRef]
- Harper, C.R. Witnessing Community Violence, Gun Carrying, and Associations with Substance Use and Suicide Risk Among High School Students—Youth Risk Behavior Survey, United States, 2021. MMWR Suppl. 2023, 72, 22–28. [Google Scholar] [CrossRef]
- Robb, A. How A Public Suicide Harms the People Who See It. Available online: https://www.theatlantic.com/health/archive/2018/05/witnessing-stranger-suicide/561257/ (accessed on 23 August 2023).
- Bardon, C.; Dargis, L.; Mishara, B. Evaluation of the implementation of a railway critical incident management and support protocol to help train drivers cope with accidents and suicides. J. Occup. Environ. Med. 2021, 63, e495–e504. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).