Abstract
Population aging is causing increases in the numbers of chronic diseases, with the consequent need for changes in health systems to better assist patients with chronic conditions. A narrative review was conducted in this study with the objective of analysing the scientific evidence on the care and assistance provided by Case Management Nurses (CMNs) to chronic patients in primary healthcare. A total of 15 articles published in English, Spanish, and Portuguese were selected in the following databases: PubMed, Embase, Cochrane Library, Scopus, Dialnet, Cinahl, and Web of Science. In total, 46.6% of the studies showed the assistance provided by CMNs for chronic pathologies. Most of the articles selected (80%) considered that the assistance offered by case management nurses in relation to chronic diseases is effective, enabling cost reductions, which supposes benefits at the economic and political levels. It was concluded that CMNs have proven to be efficient in caring for people with chronic diseases, improving the quality of life of these people and their caregivers; therefore, they have a fundamental role in the PHC.
1. Introduction
Population aging is a major concern in terms of politics, citizenship, and health. There is an ongoing increase in expenses at the health level, especially in the consumption of medications and in hospital admissions. People over the age of 65 consume more than 50% of the medications sold; 80% of older adults take at least one medication a day and 45% are polymedicated, requiring more than three medications a day [1,2,3]. In addition, this population segment is generating ever-increasing expenses in drugs and health resources (more consultations and hospital admissions), ranking first in the United States in the consumption of medications at the global level, followed by Spain [2,3].
Chronic diseases are those with a prolonged evolution and multiple aetiologies that are not solved, causing a social burden both due to economic issues and dependence and disabling problems. Cardiac pathologies, stroke episodes, cancer, diabetes, and chronic respiratory diseases stand out among these ailments; they are responsible for approximately 74% of all deaths worldwide [4,5]. Approximately 41 million people die due to chronic diseases every year, and around 17 million do so before the age of 70. Among chronic diseases, those affecting the cardiovascular system cause 17.9 million deaths per year, followed by tumours (9.3 millions), chronic respiratory diseases (4.1 millions), and diabetes (2 million deaths, including those due to kidney diseases as a result of diabetes) [4,5]. Spain is locus to an increase in the number of chronic diseases and, consequently, to higher health-related expenses [6].
Chronic patients in complex situations are diagnosed with several chronic diseases, present a high vulnerability, and require comprehensive assistance due to the need for long-term, customised, and coordinated care [7,8]. These patients are characterised by using health services to a large extent, especially at the level of urgency services, and they normally require hospitalisation. In addition, they usually have increased dependence levels and are polymedicated; this is associated with increases in the risks of pharmacological interactions and related adverse effects, prescription and intake errors, deficient compliance, hospital readmissions, and mortality. Advanced age, loneliness due to lack of family support, and a high risk of falls are added to the aforementioned [9].
Chronic diseases also affect children and adolescents; therefore, it becomes indispensable for interventions targeted at families and communities to start as early as during PHC, in addition to the promotion of healthy lifestyles [10]. In this sense, taking into account that these ailments affect people of any age, previous studies point to the need to plan changes in health systems in order to better treat chronic diseases with actions such as improved accessibility, continuity, and more comprehensive assistance that considers lifestyles, with periodic physical activity and the suitable intake of certain nutrients standing out, as both can reduce the number of chronic diseases or mitigate the progression of some illnesses [11,12,13].
Chronic diseases have become one of the major epidemics at the global level; this is the result of various factors, such as increased life expectancy, lifestyle changes, and dietary habits. The importance of advanced practice lies in improving the assistance provided to chronic patients, standing out among alternative care methods [14]. We can highlight Case Management (CM) among them. This is a care modality targeted at people with high-intensity care needs, directed both at patients and at caregivers, with the objective of improving care continuity through multidisciplinary and interlevel coordination and integration [15].
Currently, Advanced Practice Nurse (APN) profiles with high professional competence have already been developed at the international level in countries such as the USA, the United Kingdom, Australia, and Canada, achieving reductions in mortality and readmission rates and improvements in quality of life [16]. The Autonomous Community of the Canary Islands (Spain) was a pioneer in implementing CM with the title of Liaison Nurse; this was expanded to other autonomous communities (Andalusia, Catalonia, Basque Country, Valencia, and Madrid). According to the Andalusian Health Quality Agency, CM has been considered as an APN in Andalusia (south of Spain); however, despite formal recognition of this figure in the assistance provided to patients, there is significant heterogeneity in the results from each autonomous community [17,18].
Initially known as Liaison Nurses and later designated as CMNs (both names refer to the same professional profile), the CMN figure was implemented in Andalusia based on Decree No. 137/2002 of Support for Andalusian Families [19]. The CM services were expanded in 2009, including people with complex chronic problems as the target population, thus easing their access to healthcare, multidisciplinary interventions, care continuity guarantees, improved assistance provided to each person and their environment, and ensuring the protection of the patients’ rights and those of their care environments [20].
CM APNs are characterised for presenting a professional profile that provides health services and interventions enhanced with advanced capabilities that exert an influence on clinical health results. APNs have acquired a specialised knowledge base, skills in complex decision making, and clinical competencies for nurses’ expanded performance [18,19,20,21].
CM has evolved favourably and been considered as AP, showing a reduction in costs and improvements in care management [22,23]. In the Primary Health Care Strategy of the Andalusian 2020–2022 Strategic Plan, it was proposed to implement proactive follow-ups of complex chronic patients, prioritising the assistance provided to people with heart failure and Chronic Obstructive Pulmonary Disease (COPD) by the means of instruments that ease continuity and proactive follow-ups by the primary healthcare (PHC) team. The objective of this strategy is to improve quality of life, preventive assistance, and care customisation, as well as to decongest PHC and hospital care urgencies and reduce the number of hospital admissions/readmissions. In this Strategic Plan, the role of CM APNs is reinforced both in relation to people with complex chronic pathologies and in the home environment [24].
Given all of the aforementioned, the objective is to analyse the scientific evidence about the care and assistance provided by CMNs to chronic patients in PHC.
2. Materials and Methods
A narrative review of the scientific literature published between December 2022 and January 2023 was carried out following the recommendations set forth in the Cochrane Manual [25] and some of the indications included in the PRISMA report [26]. The following databases were consulted: PubMed, Embase, Cochrane Library, Scopus, Cinahl, Web of Science, and Dialnet.
The search strategy was as follows: chronic* AND (“liaison nurs*” OR “nurse liaison” OR “nurse case manager”) AND (“primary health care” OR “Primary Healthcare” OR “Primary Care”). The term Liaison Nurse (“liaison nurs*”, “nurse liaison”) was included, as this was the name initially given to CMNs (“Case Management Nurses”), corresponding to the same competencies and professional role.
The inclusion criteria were as follows: quantitative and/or qualitative research studies; reviews (bibliographic, systematic, and/or meta-analyses); materials related to case-management/liaison nurses and chronicity in PHC; and articles published in English, Spanish, and Portuguese. No time limits were applied in the searches. The exclusion criterion corresponded to studies that failed to present results, such as projects or programs.
In the first screening step, the eligible studies according to title and abstract were selected; subsequently, all duplicates were removed. Following the selection stage, the second screening was performed by the means of a critical full reading of the articles selected, taking into account agreement and applying the inclusion and exclusion criteria.
The data from the studies were extracted establishing the following elements: 1. Author, Year, and Locus; 2. Study: Type, Methodology, and Objective; 3. Sample (N), Gender, Age, and Period; and 4. Main findings. These data were included in a table following the recommendations provided by Del Pino et al. [27]. The data analysis was conducted through frequencies and percentages.
A total of 131 studies were initially identified, of which only 15 were finally selected (Figure 1).
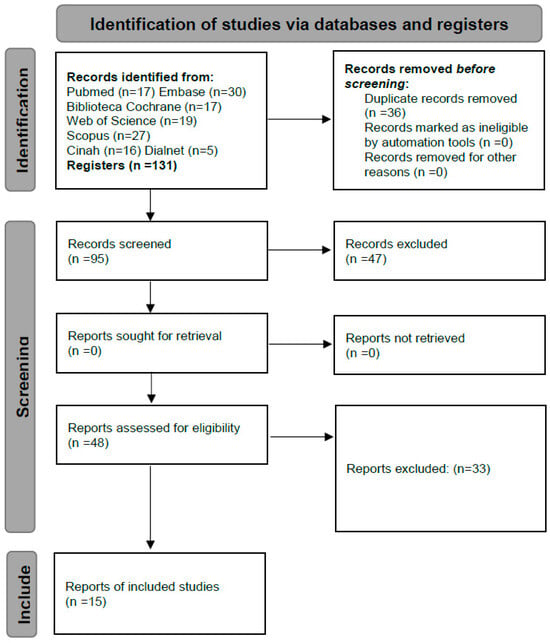
Figure 1.
Flowchart corresponding to the studies selected.
3. Results
3.1. Characteristics of the Studies
Among the studies selected, one of them employed a mixed methodology [28], two were qualitative [29,30], three were systematic reviews [31,32,33], and nine were quantitative studies [34,35,36,37,38,39,40,41,42]. Table 1 presents the characteristics of the studies selected.

Table 1.
Characteristics of the studies selected in the review.
3.2. Assistance Provided by CMNs to Chronic Patients and Caregivers in PHC
In total, 46.6% (N = 7) of the studies [30,32,33,34,37,41,42] evidenced the assistance provided by CMNs in the case of certain chronic pathologies, such as diabetes [33]; diabetes and arterial hypertension [41]; COPD [34]; diabetes, COPD, and coronary diseases [32]; and diabetes and behavioural health problems [30].
One study made a reference to assistance provided to women with chronic conditions in situations of vulnerability and frailty [35]. In turn, another one dealt with medically complex and frail children and young individuals with chronic health problems [38].
A mixed-methods study related the CM intervention in patients with chronic diseases to psychological distress and activation of the patients [28].
Twenty percent (N = 3) of the studies focused on care provided in urgency services and hospital admissions, relating these aspects to the satisfaction of the patients that had been assisted by CMNs [31,36,40].
Twenty percent (N = 3) of the studies selected [28,31,38] made specific references to the (family) caregivers of patients with chronic pathologies and the assistance they had received from CMNs.
3.3. CMNs’ Competencies and Effectiveness
Twenty percent (N = 2) of the articles selected considered that suitable training and certain professional competencies are necessary to hold CMN positions in relation to chronicity. The need for professional experience was also highlighted [31,33]. A clinical trial valued the effectiveness of a care model with the intervention of in-hospital Liaison Nurses and the PHC team [39].
The assistance provided by CMNs to chronic patients via telephone calls clearly proved to be effective in two studies (N = 2) [30,34]. Approximately 80% (N = 11) of the studies selected indicated that the assistance provided by CMNs was effective in relation to chronicity [28,29,31,32,34,36,37,38,39,40,41].
4. Discussion
The objective of this study was to analyse the scientific evidence about the care and assistance provided by CMNs to chronic patients in PHC. The main findings indicate that the assistance provided by CMNs is focused on chronic pathologies such as diabetes, arterial hypertension, COPD, coronary diseases, and behavioural health problems. Regarding the APNs’ competencies and effectiveness, the studies pointed out that the assistance provided by CMNs is effective in relation to chronicity [32].
4.1. Assistance Provided by CMNs to Chronic Patients and Caregivers in PHC
CMNs improved the arterial hypertension results and reduced the number of complications. Diabetes is better controlled with an integrated and multidisciplinary approach, and care management is a quality assurance component. They also assisted in reducing the glycated haemoglobin levels in diabetic patients [37,42], in addition to improving their waist circumference, Body Mass Index, and adherence to the treatment [41].
A study showed positive results in the assistance provided by CMNs to women with chronic diseases in situations of vulnerability and frailty, as well as in relation to medically complex and frail children and young individuals with chronic health problems, indicating increased satisfaction levels in the patients and their family caregivers [35].
The caregivers stated that they felt greater emotional and instrumental support through the assistance provided by CMNs, in addition to enhanced accessibility both at the in-person level and via telephone calls and home visits, which reduces psychological distress in many cases, thus providing improved safety. It is necessary to conduct studies with longer interventions led by CMNs in order to better show the assistance provided and the long-term results [15,28,31,38].
In a meta-analysis study, it was shown that CMNs ease care continuity and prevent hospital admissions. The CM model is focused on people with complex and long-term conditions (chronicity). The individuals treated indicated positive experiences and improved their quality of life, fostering self-management and personal accountability [29].
In relation to the number of urgency consultations, some studies [31,36,40] evidenced a reduction in the use of in-hospital emergency services among patients assisted by CMNs, in addition to fewer hospital admissions and increased satisfaction levels due to the care provided by CMNs, both in patients and in caregivers. The aforementioned is in line with other studies outside of this review, which suggests that patients with chronic pathologies are characterised by significantly resorting to health services, especially urgency consultations and hospital admissions, which is a reason why CMN interventions can contribute to reducing health expenses [9,15].
PHC nurses believe that the assistance provided by CMNs benefits patients and caregivers alike. However, they consider it necessary to improve the communication channels and mechanisms among them in order to achieve better interprofessional coordination between PHC nurses and CMNs. This would suppose an improvement in teamwork and, therefore, an enhancement in terms of human and material resources. Care continuity is fundamental in the nursing process: it is for this reason that CMNs should perform evaluations and follow-ups to improve care quality [23,36,43].
The Andalusian 2020–2023 Strategic Plan prioritises the assistance provided to groups of patients affected by chronic diseases with a prolonged evolution by the means of instruments that allow for proactive follow-ups at the PHC level, through care plans, objectives, and evaluations shared with the patients via useful tools such as the following: Clip-Salud, which fosters tele and video consultations and using professionals’ voicemails and emails; the App Salud Andalucía; and the development of telemedicine [24].
4.2. CMNs’ Competencies and Effectiveness
The assistance that CMNs provide to patients reduces the habitual complications usually presented by COPD patients, in addition to simultaneously reducing the number of hospitalisations [34]. Furthermore, significantly positive results have been evidenced in patients with chronic pathologies such as diabetes, COPD, and coronary diseases in relation to objective clinical measures, quality of life and functionality, patient satisfaction, adherence to the treatment, self-care, and the use of services. In this sense, with the Primary Care Strategy, Andalusia has initiated proactive follow-ups of patients with chronic pathologies (COPD and heart failure), strengthening the role of CMNs in relation to people with complex chronic diseases [24,32].
CMNs serve as educators, counsellors, and case managers, showing positive and effective results in telephone follow-ups and email messages. They are active participants in the process of identifying patients that require care after hospital discharge, performing a coordinating role in the process and turning out to be key actors for patient- and family-centred assistance [29,42,44].
A randomised clinical trial proposed valuing the effectiveness of a care model comprising an Internist and in-hospital Liaison Nurse, with subsequent follow-ups at the PHC level; it also reflected that this intervention was not adequate for all groups of patients. It was not efficient in patients over the age of 80; however, those aged less than 80 years old with at least three chronic diseases managed to reduce the costs in relation to consultations with urgency services and hospitalisations [39].
Through the assistance provided by CMNs in the PHC scope, improvements have been achieved in patients’ clinical conditions in relation to care quality and efficiency, as well as improvements in terms of efficacy in the use of the resources and the quality and compliance of the process. Weaknesses have also been noticed, as good-quality research studies are required in relation to the use of specific result indicators, classification of CM services, and expanded populations, offering a better-quality service that provides more customised care [45].
Two studies suggested that CMNs need special training to be able to offer effective assistance. Therefore, mandatory and continuous training is required, as well as methods to evaluate competencies and measures for ongoing control in terms of safety and quality. Regarding chronic diseases, these nurses need training in advanced practices related to chronicity. Communication skills and professional experience are also important [33]. Managers should take into account that CMNs need to have ample professional experience, knowledge about the health system and intra- and extra-hospital resources, in addition to competencies that allow them to know each patient, family, and the improvements for the health conditions in depth [44].
CMNs are nurses with advanced practice nursing (APN) competencies, which improve chronic patients’ health [31]. This is in line with other studies not discussed in this review, where CMNs have been considered as effective and efficient APNs [22,23]; in addition, it has been stated that APNs possess specialised knowledge, as well as skills in complex decision making and clinical competencies [21].
More than 80% of the studies selected in the review mentioned that, through the assistance they provide, CMNs can reduce health expenses, which supposes a benefit at the economic and political levels; it is for this reason that research studies should be encouraged to understand these costs in depth, so that this can translate into improvements in health systems at the global level. Therefore, it is important to enhance the CMN figure for assistance to be provided to chronic patients [28,29,31,32,34,36,37,38,39,40,41]. In this sense, we should take into account population aging and the increases in chronic diseases, as these imply increased health expenses in the future [1,2,6].
4.3. Opportunities and Barriers
Among the opportunities available, we can highlight that primary healthcare CMN interventions provide a better health literacy and self-management of care in people affected by chronic health problems [35]. This leads to better control of certain chronic diseases, including hypertension, diabetes, and chronic obstructive pulmonary disease [34,37,41,42].
Among the barriers, specific training, advanced practice competencies, and professional experience are considered as necessary for primary healthcare CMNs to provide effective and quality care for people with chronic diseases [33].
4.4. Added Value of this Study
The study highlights the work performed by primary healthcare CMNs through outpatient follow-up, which allows for improved healthcare and reduced healthcare costs, in addition to improving care for caregivers [31,38].
People tended by CMNs reported positive experiences and an improvement in their quality of life [29,31], as well as a decrease in the use of emergency services [31,36,40]. This study highlights the importance of interlevel coordination by the primary healthcare CMN [30].
4.5. Areas for Research Expansion and Suggestions for Future Developments
In relation to future research, studies on primary healthcare CMN interventions are needed to assess long-term health outcomes [28], taking into account the specific characteristics of patients [39].
Based on the results of this review, research studies on other prevalent chronic diseases should be considered [32,41].
Advanced practice profiles, such as primary healthcare CMNs, should be investigated to encourage the development of these figures [32].
Regarding the limitations of this review, one is that an assessment of the quality of the selected studies was not carried out, and another limitation is that only studies in English, Spanish, and Portuguese were included.
5. Conclusions
Healthcare models need to adapt to the new needs caused by the increases in complex chronic diseases, which affect people of any age and require special care from the PHC level. CMNs prepare customised management plans, evaluate social environments and lifestyles, and empower patients; all of this generates improvements in the quality of life of chronic patients and their caregivers. In addition, they have proven to be effective through ongoing assistance and interlevel and interdisciplinary coordination. Finally, we should state that new health organisation models, such as APNs (including CMNs), are required to achieve more effective and efficient results. Deeper implementation of the CMN figure should be sought, in addition to tools that allow for assessing and evaluating the work performed by these professionals.
Author Contributions
Conceptualisation, M.J.M.-G., R.D.D.-C. and M.D.G.-M.; methodology and formal analysis, R.D.D.-C. and M.D.G.-M.; resources, M.J.M.-G.; writing—original draft, R.D.D.-C. and M.D.G.-M.; visualization, R.D.D.-C., M.D.G.-M. and M.J.M.-G.; supervision, M.D.G.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not additional data available.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Arjona, C.R.; Criado, J.; Sánchez, L. Enfermedades crónicas y consumo de fármacos en mayores de 65 años. Med. Gen. 2002, 47, 684–695. Available online: https://semg.info/mgyf/medicinageneral/revista_47/pdf/684-695.pdf (accessed on 20 February 2022).
- Abades, M.; Rayón, E. Aging in Spain: A challenge or social problem? Gerokomos 2012, 23, 151–155. [Google Scholar] [CrossRef]
- Morales, A.; Aguilar, J.M.; Padilla, D.; Rocamora, P.; López, R. Consumo farmacológico y salud en personas mayors. Int. J. Dev. Educ. Psychol. 2018, 4, 235. Available online: https://www.redalyc.org/journal/3498/349857603023/349857603023.pdf (accessed on 1 March 2022).
- World Health Organization. ICD-11 2022 Release. 2022. Available online: https://www.who.int/es/news/item/11-02-2022-icd-11-2022-release (accessed on 22 February 2022).
- Robledo, R.; Escobar, F.A. Las Enfermedades Crónicas no Transmisibles en Colombia. Universidad Nacional de Colombia, Facultad de Medicina. 2010. Available online: https://repositorio.unal.edu.co/handle/unal/31438 (accessed on 2 March 2022).
- Riera, L. El etiquetado de pacientes en atención primaria. El caso de la cronicidad. Aten. Prim. 2017, 49, 508–509. [Google Scholar] [CrossRef] [PubMed]
- Miguélez, A.; Casado, M.I.; Company, M.C.; Balboa, E.; Font, M.A.; Román, I. Advanced practice in case management: An essential element in the new complex chronicity care model. Enferm. Clín. 2019, 29, 99–106. [Google Scholar] [CrossRef]
- Viña, M.; Román, I. The role of the geriatric nurse specialist as a key response in the care of the elderly, chronicity, complex chronicity and its consequences on dependence. Enferm. Clín. 2019, 29, 381–384. [Google Scholar] [CrossRef] [PubMed]
- Contel, J.C.; Muntané, B.; Camp, L. La atención al paciente crónico en situación de complejidad: El reto de construir un escenario de atención integrada. Aten. Prim. 2012, 44, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Flores, B.; Aceituno, J. Planes de prevención de enfermedades crónicas no transmisibles en niños y adolescentes. Rev. Pediatr. Aten. Prim. 2021, 23, 143–153. Available online: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1139-76322021000200006 (accessed on 15 June 2022).
- Bruins, M.J.; Van Dael, P.; Eggersdorfer, M. The Role of Nutrients in Reducing the Risk for Noncommunicable Diseases During Aging. Nutrients 2019, 11, 85. [Google Scholar] [CrossRef]
- Capodaglio, E.M. Physical activity, tool for the prevention and management of chronic diseases. G. Ital. Med. Lav. Ergon. 2018, 40, 106–119. Available online: https://pubmed.ncbi.nlm.nih.gov/30480395/ (accessed on 10 April 2022).
- Del Brutto, O.H.; Mera, R.M.; Zambrano, M.; Del Brutto, V.J. El Proyecto de Atahualpa: Protocolo, definiciones operacionales y diseño inicial. Rev. Ecuat. Neurol. 2017, 26, 95–100. Available online: http://scielo.senescyt.gob.ec/scielo.php?script=sci_arttext&pid=S2631-25812017000100095 (accessed on 25 April 2022).
- Morales-Asencio, J.M.; Martin-Santos, F.J.; Morilla-Herrera, J.C.; Fernández-Gallego, M.C.; Celdrán-Mañas, M.; Navarro-Moya, F.J.; Rodríguez-Salvador, M.M.; Muñoz-Ronda, F.J.; Gonzalo-Jiménez, E.; Carrasco, A.M. Design of a case management model for people with chronic disease (Heart Failure and COPD). Phase I: Modeling and identification of the main components of the intervention through their actors: Patients and professionals (DELTA-icE-PRO Study). BMC Health Serv. Res. 2010, 10, 324. [Google Scholar] [CrossRef] [PubMed]
- Caldararo, A.M.; Graña, M.E.; López, M.; Maestre, L.; Martín, P.; Morales, I.; Nebot Fernández, C.; Pérez Casado, S.; Rico Merino, M.; Ríos Gómez, M.T. Guía de Recomendaciones Prácticas en Enfermería: Terapias Respiratorias en el Ámbito Domiciliario. Fontán G y Rico M. (Coordinadores); IM&C: Madrid, Spain, 2023; Available online: https://www.consejogeneralenfermeria.org/profesion/guias-clinicas/send/160-guias-clinicas/2579-terapias-respiratorias (accessed on 28 September 2023).
- Lafuente, N.; Fernández, S.; Rodríguez, S.; Casado, M.I.; Morales, J.M.; Ramos, A.J. Competency development of nurses in the public health system of Andalusia. Clin. Enferm. 2019, 29, 83–89. [Google Scholar] [CrossRef] [PubMed]
- López, M.; Puente, J. Institutionalization of the case management nurse in Spain. Comparative analysis of health systems of the Spanish autonomous communities. Enferm. Clín. Engl. Ed. 2019, 29, 107–118. [Google Scholar] [CrossRef]
- Prácticas Avanzadas. Servicio Andaluz de Salud. Consejería de Salud y Consumo. Junta de Andalucía. 2019. Available online: https://www.sspa.juntadeandalucia.es/servicioandaluzdesalud/el-sas/planes-marco-y-estrategias/estrategia-de-cuidados-de-andalucia/practicas-avanzadas (accessed on 20 December 2022).
- Decreto 137/2002, de 30 de Abril, de Apoyo a las Familias Andaluzas. Boletín Oficial de la Junta de Andalucía, Número 52 de 04/05/2002. Available online: https://www.juntadeandalucia.es/boja/2002/52/1 (accessed on 22 October 2022).
- Casado, M.I.; Cuevas, M.; González, F.; Martín, F.J.; Morillas, J.C.; Perteguer, I.; Toral, I.; Modelo de Gestión de Casos del Servicio Andaluz de Salud. Guía de Reorientación de las Prácticas Profesionales de la Gestión de Casos en el Servicio Andaluz de Salud. 2017. Available online: https://www.sspa.juntadeandalucia.es/servicioandaluzdesalud/sites/default/files/sincfiles/wsas-media-pdf_publicacion/2021/mgc_modelo_gestion_casos.pdf (accessed on 10 March 2023).
- Schober, M.; Lehwaldt, D.; Rogers, M.; Steinke, M.; Turale, S.; Pulcini, J.; Rousse, J.; Stewart, D. Directrices de Enfermería de Práctica Avanzada 2020. Consejo Internacional de Enfermeras. 2020. Available online: https://www.icn.ch/system/files/documents/2020-04/ICN_APN%20Report_ES_WEB.pdf (accessed on 30 November 2022).
- Feyereisen, S.; Puro, N.; Thomas, C.; McConnell, W. A new kind of gatekeeper: The increasing prevalence of Advanced Practice Nurses as case managers in US hospitals. Health 2021, 25, 596–612. [Google Scholar] [CrossRef] [PubMed]
- Sastre, P.; Morales, J.M.; Sesé, A.; Bennasar, M.; Fernández, J.C.; De Pedro, J. Advanced Practice Nursing Competency Assessment Instrument (APNCAI): Clinimetric validation. BMJ Open 2017, 7, e013659. [Google Scholar] [CrossRef] [PubMed]
- Estrategia Atención Primaria. Plan Estratégico 2020–2022.Servicio Andaluz de Salud. Consejería de Salud y Consumo. 2020. Available online: https://www.sspa.juntadeandalucia.es/servicioandaluzdesalud/el-sas/planes-marco-y-estrategias/estrategia-atencion-primaria-plan-estrategico-2020-2022 (accessed on 10 June 2023).
- Higgins, J.; Thomas, J.; Cochrane Handbook for Systematic Reviews of Interventions. 22 August 2023. Available online: https://training.cochrane.org/handbook (accessed on 11 October 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Del Pino, R.; Frías, A.; Palomino, P.A. La revisión sistemática cuantitativa en enfermería. Rev. Iberoam. Enferm. Comunitaria 2014, 7, 24–40. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=6336945 (accessed on 5 September 2022).
- Hudon, C.; Chouinard, M.C.; Dubois, M.F.; Roberge, P.; Loignon, C.; Tchouaket, É.; Lambert, M.; Hudon, É.; Diadiou, F.; Bouliane, D. Case Management in Primary Care for Frequent Users of Health Care Services: A Mixed Methods Study. Ann. Fam. Med. 2018, 16, 232–239. [Google Scholar] [CrossRef]
- Askerud, A.; Conder, J. Patients’ experiences of nurse case management in primary care: A meta-synthesis. Aust. J. Prim. Health 2017, 23, 420–428. [Google Scholar] [CrossRef]
- Kahn, L.S.; Fox, C.H.; Carrington, J.; Desai, U.; Bartlett, D.P.; Lyle, H.; Kowalski, M. Telephonic nurse case management for patients with diabetes and mental illnesses: A qualitative perspective. Chronic Illn. 2009, 5, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Doménech-Briz, V.; Romero, R.G.; de Miguel-Montoya, I.; Juárez-Vela, R.; Martínez-Riera, J.R.; Mármol-López, M.I.; Verdeguer-Gómez, M.V.; Sánchez-Rodríguez, Á.; Gea-Caballero, V. Results of Nurse Case Management in Primary Heath Care: Bibliographic Review. Int. J. Environ. Res. Public Health 2020, 17, 9541. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, D.; Hayter, M. Structured review: Evaluating the effectiveness of nurse case managers in improving health outcomes in three major chronic diseases. J. Clin. Nurs. 2009, 18, 2978–2992. [Google Scholar] [CrossRef]
- Watts, S.A.; Lucatorto, M. A review of recent literature—Nurse case managers in diabetes care: Equivalent or better outcomes compared to primary care providers. Curr. Diab. Rep. 2014, 14, 504. [Google Scholar] [CrossRef]
- Casas, A.; Troosters, T.; Garcia-Aymerich, J.; Roca, J.; Hernández, C.; Alonso, A.; del Pozo, F.; de Toledo, P.; Antó, J.M.; Rodríguez-Roisín, R.; et al. Integrated care prevents hospitalisations for exacerbations in COPD patients. Eur. Respir. J. 2006, 28, 123–130. [Google Scholar] [CrossRef]
- Cook, C.L.; Hall, A.G.; Garvan, C.S.; Kneipp, S.M. A Public Health Nursing Model Assists Women Receiving Temporary Assistance for Needy Families Benefits to Identify a Usual Source of Primary Care. Care Manag. J. 2015, 16, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Crane, S.; Collins, L.; Hall, J.; Rochester, D.; Patch, S. Reducing utilization by uninsured frequent users of the emergency department: Combining case management and drop-in group medical appointments. J. Am. Board Fam. Med. 2012, 25, 184–191. [Google Scholar] [CrossRef]
- Gabbay, R.A.; Añel-Tiangco, R.M.; Dellasega, C.; Mauger, D.T.; Adelman, A.; Van Horn, D.H.A. Diabetes Nurse Case Management and Motivational Interviewing for Change (DYNAMIC): Results of a 2-year Randomized Controlled Pragmatic Trial. J. Diabetes 2013, 5, 349–357. [Google Scholar] [CrossRef]
- Gordon, J.B.; Colby, H.H.; Bartelt, T.; Jablonski, D.; Krauthoefer, M.L.; Havens, P. A tertiary care-primary care partnership model for medically complex and fragile children and youth with special health care needs. Arch. Pediatr. Adolesc. Med. 2007, 161, 937–944. [Google Scholar] [CrossRef]
- Lanzeta, I.; Mar, J.; Arrospide, A. Cost-utility analysis of an integrated care model for multimorbid patients based on a clinical trial. Gac. Sanit. 2016, 30, 352–358. [Google Scholar] [CrossRef]
- Mallitt, K.A.; Mcnab, J.; Hughes, R.; Fernyhough, J.; Paterson, J.; O’Halloran, D. Reducing emergency department presentations among chronically ill patients in Western Sydney: A key role for coordinated primary care. Aust. J. Prim. Health 2017, 23, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Mattei, A.T.; de Fátima, M.; Castanho, R.; Perez, J.; Molina, R. Nursing case management for people with hypertension in primary health care: A randomized controlled trial. Res. Nurs. Health 2020, 43, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Watts, S.A.; Sood, A. Diabetes nurse case management: Improving glucose control: 10 years of quality improvement follow-up data. Appl. Nurs. Res. 2016, 29, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Peña, R.; Ortego-Maté, C.; Amo-Setién, F.J.; Silió-García, T.; Casasempere-Satorres, A.; Sarabia-Cobo, C. Implementing a Care Pathway for Complex Chronic Patients from a Nursing Perspective: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 6324. [Google Scholar] [CrossRef]
- Reig-Garcia, G.; Suñer-Soler, R.; Mantas-Jiménez, S.; Bonmatí-Tomas, A.; Malagón-Aguilera, M.C.; Bosch-Farré, C.; Gelabert-Viella, S.; Juvinyà-Canal, D. Assessing Nurses Satisfaction with Continuity of Care and the Case management Model as an Indicator of Quality of Care in Spain. Int. J. Environ. Res. Public Health 2021, 18, 6609. [Google Scholar] [CrossRef]
- Gisele, K.A.; Bernardino, E.; Lapierre, J.; Dallaire, C. Activities of liaison nurses at hospital discharge: A strategy for continuity of care. Rev. Lat. Am. Enfermagem. 2019, 27, e3162. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).