Abstract
Objective: The outbreak of COVID-19 brings an overload of physical and mental demands to healthcare professionals. Keeping healthcare professionals sustainable, engaged, and performing at their highest levels becomes critical and nonetheless difficult. The objective of this research is to link the literature on organizational climates, corporate social responsibility, safety science, and work engagement, and propose a research framework that investigates the factors influencing healthcare professionals’ engagement during COVID-19. Methodology: We propose that when healthcare workers’ career callings are triggered by COVID-19, it influences their perceptions of the work’s meaningfulness, which ultimately enhances their work engagement. We argue that creating a social responsibility climate and a safety climate inside the hospital facilitates the process of turning healthcare workers’ perceived work meaningfulness into work engagement. We collected data from 112 healthcare professionals, including nurses, doctors, and executive staff, from 16 wards in a public hospital in China to test our hypotheses. Results: Hierarchical linear regression analysis provided empirical support for our research model. We find that healthcare professionals’ career callings during COVID-19 enhanced their perceived work meaningfulness, which results in increased work engagement. Moreover, a social responsibility climate and a safety climate strengthens the link between work meaningfulness and work engagement among participants. Conclusions: Creating a social responsibility climate and a safety climate in the workplace are effective management approaches to realize healthcare workers’ feelings of work meaningfulness and turn them into work engagement.
1. Introduction
The COVID-19 pandemic created a global health crisis. After the outbreak of COVID-19, healthcare workers played a critical role in delivering timely healthcare service and around-the-clock treatment. Not only are they the ones who are racing against the clock and fighting at the frontline, but the whole profession is feeling a pull in the heart to help. The special period of the COVID-19 pandemic, on the one hand, incites healthcare workers’ sense of occupational calling and professional accountability; on the other hand, it forces them to engage themselves and perform under overloaded physical and mental demands [1]. Keeping healthcare workers sustainably engaged and performing their professional skills at the highest levels becomes critical and nonetheless difficult. Sustainable Human Resources Management (SHRM) research indicates that a series of human resource activities and practices may help organizations to achieve sustainable development goals and sustainable business outcomes [2]. Following this line of thought, in order to keep healthcare professionals’ work engagement sustainable under high work pace and demanding jobs during COVID-19, according to corporate operations, processes and deployment should be employed. Past research indicates that the organizational climate, which refers to the shared perceptions of employees regarding an organization’s policies, procedures, and practices, as well as the types of behavior that are rewarded and supported in work settings [3], plays a critical role in enhancing the organizational sustainability of enterprises. Furthermore, an organizational climate keeps humans thriving and sustainable at the individual level and influences the relational sustainability between team members [4,5,6]. In the current research, an organizational climate is proposed to be a strategic corporate operation that may help to keep healthcare workers sustainably engaged. We consider a social responsibility climate as well as a safety climate to be important during a crisis such as COVID-19. We choose these two organizational climates because a social responsibility climate indicates to employees the socially responsible actions they should take and what they should do for the benefit of the greater good [3,4] while a safety climate ensures that healthcare workers’ safety is a priority during treatment which could be perceived as background support during a crisis [4,6].
Past research indicates that during a crisis, people’s career calling may fluctuate during a short period of time [7,8]. We think the starting of COVID-19 offers good timing for studying healthcare workers’ career callings. Career calling, or occupational calling, is defined as “a transcending passion to use one’s talent and competencies toward a positive societal impact and a sense of meaningfulness is derived from the work in a chosen occupational domain” [1], and it becomes even more salient during the situation of COVID-19. Due to the severity of the pandemic, healthcare workers became warriors in society, and the huge amount of societal and professional demands greatly triggered an inherent career calling among them and urged them to focus and engage in their work [1,9]. This research aims to explore how healthcare professionals translate their career calling into work meaningfulness and then work engagement—a state where nurses connect with their work physically, cognitively, and emotionally [10]—during COVID-19. Furthermore, this research aims to demonstrate that building and maintaining a social responsibility climate and a safety climate in the workplace are important organizational operations to translate healthcare professionals’ work meaningfulness into work engagement.
1.1. Calling, Meaningfulness, and Work Engagement
Scholars theorize that a tripartite model of work orientation is such that people tend to see their work as a job, a career, or a calling [8,11]. People who tend to see their work as a job focus on the material benefits; people with a career orientation work for promotion and advancement. When people see their work as a calling, they work for the fulfillment brought by the work [12]. A severe situation of crisis, such as COVID-19, is able to incite nurses’ career calling [1]. When society is facing a crisis, it normally comes along with strained medical staff and strained healthcare professional services. The scarce medical resources and societal needs make nurses realize that their work is salient and in urgent need, so nurses tend to feel a pull in their hearts and feel fortunate to help meet those demands, and hence, tend to see their work as a calling [9]. When people see their work as a calling, they believe that their work contributes to the greater good and makes the world a better place [12]. In this case, during crisis, when healthcare workers feel a calling, they experience spiritual significance, personal fulfillment, and worldly impact, and hence, they are more likely to find their work meaningful [13,14,15,16].
Work meaningfulness refers to the amount of significance people perceive in their work [12]. Healthcare workers’ jobs are widely perceived as meaningful but challenging, especially when confronting a worldly healthcare crisis, such as COVID-19. Past research indicates a link between career calling and work meaningfulness, which is particularly salient when the work is perceived as challenging. A severe crisis signals urgent societal needs, and nurses have strong feelings of obligation and responsibility to fully utilize their professional skills [17]. For example, Dobrow and colleagues in longitudinal research show that people with strong early career callings were more likely to pursue challenging careers professionally in adulthood [18]. We thus propose that during COVID-19, career calling is positively related to perceived work meaningfulness among healthcare workers.
Work meaningfulness is theorized to invoke people’s deeper consideration of purpose and significance [12]. Employees who experience psychological meaningfulness feel that they are receiving a return on investment in a currency of physical, cognitive, or emotional energy. Work meaningfulness may serve as a psychological driving force that makes nurses more energized, activated, and engaged in their work, and that is a high level of work engagement [19,20]. Past research shows that work meaningfulness influences important work outcomes, including work engagement, commitment, performance, job satisfaction, life satisfaction, and general health states [21]. We focus on healthcare professionals’ engagement because during COVID-19, due to the heavy workload, fast work pace, and high physical and mental demands, it was very often that healthcare professionals felt burnt out, depressed, or intended to quit [22]. When healthcare professionals find meaning in their work, they have a stronger intention to continue working as nurses [23]. Following this line of thought, we think that healthcare professionals who find their work meaningful not only would like to continue working as nurses, they are more likely to engage highly in their work. Past research shows that work meaningfulness invokes some of the most important outcomes in organizational studies, including work engagement [12]. We propose that this relationship is particularly salient among healthcare workers during COVID-19. Therefore, we propose the following two hypotheses:
Hypothesis 1 (H1).
Calling is positively related to work meaningfulness.
Hypothesis 2 (H2).
Work meaningfulness is positively related to work engagement.
1.2. Social Responsibility Climate and Safety Climate as Moderators
When healthcare workers are fighting at the frontline, they run the risk of being exposed to the virus and infected individuals, especially during a severe situation, such as COVID-19 [1]. According to a recent report, due to their exposure, a healthcare worker presented as one of the first reinfections reported in the world [24]. On the one hand, a situation of crisis brings about a high level of societal demands so nurses feel a sense of responsibility to assist with intensive caring needs; on the other hand, they feel worried because they have a high risk of being infected. Such worries and negative psychological states sometimes make healthcare workers distracted and hard to keep engaged. From a sustainable human resources management (HRM) perspective, we consider building a social responsibility climate and a safety climate in the workplace, which is a salient sustainable practice that potentially boosts nurses’ feelings of work meaningfulness, which strengthens their engagement and helps to strengthen the effect.
A social responsibility climate refers to “employees’ shared perceptions concerning organizational stakeholders’ values, expectations, and practices that emphasize the responsibility of individuals as a member in society” [25] (p. 667). Stakeholders of hospitals, especially in a situation of crisis, include wide groups of people, such as the hospital, co-workers, current patients, potential patients, the healthcare system, and society [26,27]. Healthcare workers’ feelings of social responsibility are discretionary and not explicitly recognized by the formal human resource systems [25]. In a unit with a social responsibility climate, healthcare workers are triggered to contribute because they feel the responsibility to help and to relieve the intensive societal needs [28]. Even though they are sometimes exhausted and depressed, a feeling of social responsibility may buffer their negative psychological states and pull them to engage. In this way, regarding nurses who perceive their job as significant to society (i.e., work meaningfulness) and would like to make the best use of their professional skills and capabilities to contribute, when they perceive a social responsibility climate in the workplace, they feel even more energized. We thus propose that a social responsibility climate boosts the effect of work meaningfulness on work engagement.
The other organizational climate we propose to be contextually important during COVID-19 is a safety climate. A safety climate refers to nurses’ shared perceptions of practices, policies, and procedures as well as the types of behavior that are rewarded and supported regarding the safety of their work environment [29]. COVID-19’s severity and influence never seem to decrease, and it is common that people are nervous and worried that they will be infected by the virus or infected individuals. This is even true for nurses who are frontline warriors and have the closest and most frequent interactions with COVID-19 patients [30]. Long-term worries and negative psychological states can make nurses distracted, depressed, and can make it hard to concentrate. In this case, a safety climate inside working units may work as a buffer, potentially creating a comparatively safe workplace by helping to relieve nurses’ psychological tension of being infected and offering them a sense of security when working. Past research shows that employees working in a safety climate have reduced stress, improved job performance and well-being, and improved work ability [31,32,33]. We thus consider a safety climate to be a key situational factor during the COVID-19 pandemic that can possibly enable nurses to turn their feelings of work meaningfulness into a focused, devoted, and absorbed state, as a safety climate strengthens the effect of work meaningfulness on work engagement. Combined, we propose the following hypotheses. Full research model is shown in Figure 1.
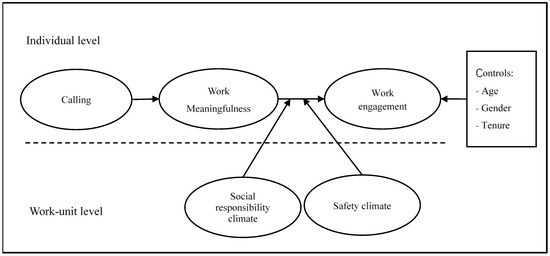
Figure 1.
Research model.
Hypothesis 3 (H3).
A social responsibility climate moderates the effect of work meaningfulness on work engagement, such that the effect is stronger when a social responsibility climate is high rather than low.
Hypothesis 4 (H4).
A safety climate moderates the effect of work meaningfulness on work engagement, such that the effect is stronger when a safety climate is high rather than low.
2. Materials and Methods
2.1. Sample and Procedures
We collected our data from nurses, doctors, and executive staff working in a public general hospital in a city located in Southwest China. The majority of participants were nurses from sixteen different wards across the hospital, including pediatrics, oncology, and clinical laboratory. Considering that the nurses and doctors have very busy hospital routines, we contacted the director of the hospital beforehand to obtain permission for our data collection.
We used paper-and-pencil questionnaires to collect data. The research protocol was approved by the Ethics Committee of Xi’an Jiaotong-Liverpool University. We included consent forms before the questionnaires and assured participants on the front cover of the questionnaire that their responses would be anonymous and kept confidential. Before we officially started the survey, we invited a friend, who used to be a nurse, to finish a pilot test, ensuring the wording used in the survey and the length of the survey were appropriate.
We initially invited 200 participants from the hospital to our survey. We aimed to invite all possible healthcare professionals in the hospital, but the director was worried that the working routines and efficiency might be affected during this process. After discussion, we agreed to send out 130 copies of questionnaires to participants who worked in the wards with a relatively low work pace. Executive staff in the hospital had more flexible work hours compared to nurses and doctors, so we invited them to our survey as well. The heads of each ward helped us to distribute the questionnaires to the participants. Informed consent was obtained from all subjects involved in the study.
We used a longitudinal design for the data collection. In the first wave, we collected all the variables in the research model except for work engagement. One week later, we invited the participants again and asked them to fill out a second wave with the measure of work engagement. This way, we could examine the effect of work meaningfulness on the sustainability of work engagement. We examined work engagement only one week after the predictors because healthcare professionals have a high work pace and job demands, especially during COVID-19, and things change fast. Past research took a one-year or a three-year gap when measuring the sustainability of engagement, while during COVID-19, it was not feasible and had little meaning [34,35]. After the 2 waves, we collected 112 completed questionnaires, with a response rate of 86.15% (95 nurses, 10 doctors, and 7 executive staff). Among all the participants, 84.82% were females. The mean age of participants was 32.13 years (standard deviation = 7.45). Participants reported having an average hospital tenure of 109.6 months (standard deviation = 101.4) and an average ward tenure of 62.67 months (standard deviation = 68.55).
2.2. Measures
We adopted existing measures for all of the variables in this study. We slightly modified some of the items to reflect the hospital context. The original questionnaire was prepared in English, and then translated into Chinese using standard back translation [36]. Respondents rated the measures on a 5-point Likert scale ranging from 1, “strongly disagree”, to 5, “strongly agree”.
Calling was measured by a six-item scale adapted from [25]. A sample item was “The work I do feels like my calling in life”. The Cronbach’s alpha of calling was 0.92.
Work meaningfulness was measured with a three-item scale from the second version of the Copenhagen Psychosocial Questionnaire [37]. Examples of the items include “My work is meaningful” and “I feel that the work I am doing is important”. The Cronbach’s alpha of calling was 0.87.
Social responsibility climate was measured with a three-item scale from [25]. Examples of the items include “In my opinion, my workplace is socially responsible” and “In my opinion, my workplace is genuinely concerned to improve the well-being of society”. The Cronbach’s alpha of calling was 0.91. We aggregated individual-level data to the ward level, so we justified the aggregation by assessing the intra-class correlation coefficients, ICC(1) and ICC(2). The ICC(1) for a social responsibility climate was 0.12, and the ICC(2) was 0.53, indicating that we could aggregate the data.
Safety climate was measured with a six-item scale from [38]. Examples of the items include “Health professionals are told when they do not follow good safety practices” and “The safety of health professionals is a high priority with management where I work”. The Cronbach’s alpha of calling was 0.91. The ICC(1) for safety climate was 0.11, and the ICC(2) was 0.49.
Work engagement was measured using the Utrecht Work Engagement Scale (UWES) developed in [39]. This measure included three subscales of work engagement: vigor, dedication, and absorption. Vigor was assessed with six items (e.g., “When I get up in the morning, I feel like going to work”). Dedication was measured with five items (e.g., “I am enthusiastic about my work”). Absorption was assessed with six items (e.g., “Time flies when I am working”). Respondents rated work engagement on a 5-point Likert scale ranging from 1, “never”, to 5, “always”. Cronbach’s alpha of work engagement was 0.93.
Control variables. Considering that age, gender, and tenure in hospital could have an influence on health professionals’ work engagement, and past research indicated that these demographics may influence employees’ work engagement (e.g., [40,41]), we included participants’ age, gender, and organizational tenure as control variables. Age and organizational tenure were continuous variables. Gender was a dummy variable, where 0 represented female and 1 represented male.
2.3. Analytic Strategy
Our research model is multilevel in nature with participants nested in wards and because calling, work meaningfulness, and work engagement are individual-level constructs. A social responsibility climate and safety climate are ward-level constructs, so we conducted hierarchical linear modeling (HLM) analyses to test our hypotheses. HLM explicitly takes into account the nested data structure and simultaneously estimates the impact of factors at different levels and on individual-level outcomes.
3. Results
3.1. Descriptive Statistics
Table 1 presents the characteristics of participants. Table 2 presents the means, standard deviations, and correlations among the variables. Internal consistency reliabilities are presented on the diagonal.

Table 1.
Subject characteristics.

Table 2.
Means, standard deviations, correlations, and internal consistency reliability.
3.2. Hierarchical Linear Modeling Results
Before we performed the HLM analysis, we tested the normality of all the variables in the model. The chi-squares of the Skewness-Kurtosis tests of work engagement, calling, work meaningfulness, social responsibility climate, and safety climate were 0.44 (p > 0.05), 2.76 (p > 0.05), 6.13 (p < 0.05), 3.48 (p > 0.05), and 0.10 (p > 0.05), indicating that almost all the variables are normally distributed. We performed these tests using the sktest in Stata 14.0.
To perform the HLM, we first entered all the control variables and the predictor, calling, into the model as shown in Model 1 in Table 3. Then, we entered work meaningfulness, social responsibility climate, and their cross-level interactions in Model 2 and Model 3. Lastly, we entered safety climate and its cross-level interactions with work meaningfulness in Model 4 and Model 5. Table 3 presents the analytical results.

Table 3.
Hierarchical linear modeling results: the effects of work meaningfulness, social responsibility climate, and safety climate on work engagement.
Hypothesis 1 predicted that calling is positively related to work meaningfulness. Ordinary least square regression results, as shown in Model 1 in Table 3, revealed that calling was positively related to work meaningfulness (b = 0.49, p = 0.000). Therefore, Hypothesis 1 was supported.
Hypothesis 2 proposed that work meaningfulness is positively related to work engagement. HLM results shown in Model 2 in Table 3 revealed that work meaningfulness was positively related to work engagement (b = 0.31, p = 0.000). Therefore, Hypothesis 2 was supported.
Hypothesis 3 proposed that a social responsibility climate moderates the effect of work meaningfulness on work engagement, such that the effect is stronger when a social responsibility climate is high rather than low. The HLM results in Model 3 demonstrate a significant interaction between work meaningfulness and a social responsibility climate (b = 0.13, p = 0.03). We probed the interaction between work meaningfulness and the social responsibility climate by taking one standard deviation above and below the mean to indicate high and low levels. As shown in Figure 2, the simple slopes revealed that the effect of work meaningfulness on work engagement was stronger when a social responsibility climate was high (r = 0.44, p = 0.000) rather than low (r = 0.23, p = 0.000). Therefore, Hypothesis 3 was supported.
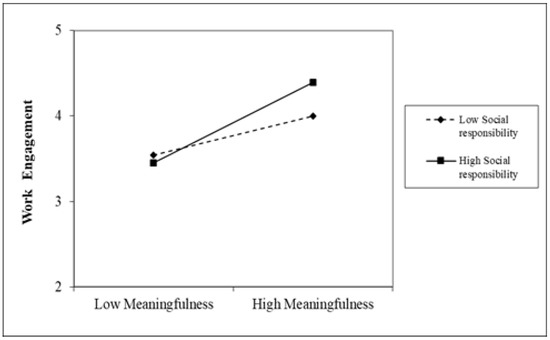
Figure 2.
Simple slopes for the interaction between work meaningfulness and social responsibility climate on work engagement.
Hypothesis 4 proposed that a safety climate moderates the effect of work meaningfulness on work engagement, such that the effect is stronger when a safety climate is high rather than low. The results in Model 5 demonstrate a significant interaction between work meaningfulness and a safety climate (b = 0.15, p = 0.01). We probed the interaction between work meaningfulness and safety climate by taking one standard deviation above and below the mean to indicate high and low levels. As shown in Figure 2 and Figure 3, the simple slopes indicated that the effect of work meaningfulness on work engagement was stronger when the safety climate was high (r = 0.48, p = 0.000) rather than low (r = 0.21, p = 0.000). Therefore, Hypothesis 4 was supported.
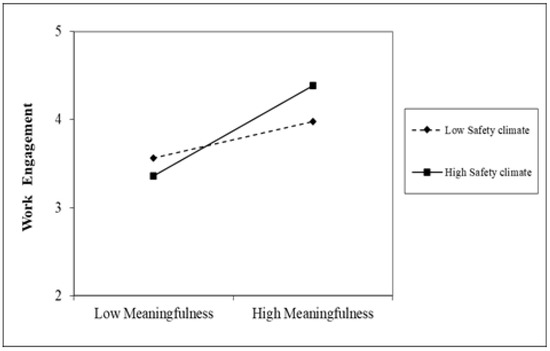
Figure 3.
Simple slopes for the interaction between work meaningfulness and safety climate on work engagement.
4. Discussion
This research links the literature on organizational climate, corporate social responsibility, safety science, and work engagement, and examines a research framework that aims to keep health professionals’ work engagement sustainable during COVID-19. We find that during COVID-19, the societal and professional demands triggered health professionals’ feelings of career calling, and such callings made them have an enhanced feeling of work meaningfulness—they are helping, they are saving lives, and they are contributing to the greater good—which results in enhanced engagement. Our results further show that during this special period, a social responsibility climate and safety climate serve as situational boosters that strengthen the above link and enable corporations to achieve sustainable engagement among healthcare workers. Below, we discuss the theoretical and practical implications of our findings.
4.1. Theoretical and Practical Implications
This study makes contributions to the existing literature in the following ways. First, in hoping that the turning period of COVID-19 would arrive soon, healthcare professionals were confronted with overloaded demands that require both physical and mental engagement at a high level [1]. Even so, keeping health professionals sustainably engaged receives limited research attention [34]. Grounded in the broad literature of sustainable HRM, this research seeks to uncover mechanisms that help to achieve the sustainable engagement of healthcare professionals [42]. As shown in Table 3, we find that when a sense of calling is invoked during COVID-19, it positively influences healthcare professionals’ feelings of work meaningfulness, which in turn leads to work engagement. We link research on organizational climates, which reflects the practices, procedures, and policies in an organization, with sustainable HRM research and bridge these two bodies of literature in the context of COVID-19. Our results in Table 3 show that a social responsibility climate and safety climate strengthen the effect of work meaningfulness on work engagement. We demonstrate that building a social responsibility climate and safety climate are indeed effective practices and can be utilized as management strategies to maintain sustainable performance and the engagement of healthcare professionals (as shown in Figure 2 and Figure 3).
Second, this research highlights the importance of organizations’ practices in creating a socially responsible and safe workplace in hospitals. As COVID-19 brings a fast work pace, overloaded professional demands, and unbearable physical and psychological pressure [43], a socially responsible and safe workplace to some extent relieves the pressure, calms the workers, and offers inner motivation to overcome the difficulties. Our results indicate that when healthcare workers find their jobs meaningful and would like to make a contribution, a socially responsible and safe working environment would help to keep them sustainably engaged and potentially realize their eagerness to contribute.
Third, past research shows that COVID-19 incites high levels of career calling from healthcare professionals [44,45]. This research demonstrates that it is indeed true when a whole society depends on this important group of people. This research further shows that depending only on the inner calling of healthcare workers is not enough to achieve sustainable outcomes because a career calling is not stable, and it fluctuates due to high demands, work pace, and pressure [46]. Our results indicate that hospitals and managers in hospitals should make efforts to trigger this inner calling and translate the inner calling into important work outcomes through policy making [46]. Our results in Table 3 and Figure 2 and Figure 3 show that creating effective organizational climates with regard to social responsibility and safety would be such an important effort.
This study offers significant practical implications for management. Our results demonstrate the significant impact of calling on the perception of work meaningfulness and sustainable engagement among healthcare workers. In order to realize such an important link, this research indicates that hospitals should endeavor to emphasize a social responsibility climate to healthcare workers and try to make effective policies and practices with regard to safety in hospitals to offer a feeling of security and safety to healthcare workers. These are important management practices because the severity and scope of COVID-19 are huge and broad, and internal supporting practices from the hospitals are key to maintain and promote inner motivation for frontline healthcare workers [44,45,46].
4.2. Limitations
We are aware of the limitations of this study. First, we collected our second wave data only one week after the first wave to measure the sustainability of work engagement, which was much shorter than previous studies (e.g., [34,44]). Although COVID-19 was a special time, future research could use a longer lag to test the sustainability of healthcare workers’ engagement. Second, we collected all of the variables from one source—healthcare professionals— and although there was a time lag between predictors and outcomes, it is hard for us to draw causal inferences. Third, the results of this study lack external validity given its particularity in the timing of data collection (the outbreak of COVID-19 in China) and location (not far from Wuhan). We, therefore, should be careful if we would like to draw conclusions from the results in a different context.
5. Conclusions
Grounded in the broad literature of sustainable HRM, this research links the literature on organizational climate, corporate social responsibility, safety science, career calling, and work engagement. Situated in the context of COVID-19, this research investigates the relationship between healthcare professionals’ career calling, work meaningfulness, and work engagement. The results demonstrate that creating a social responsibility climate and safety climate in the workplace are effective management approaches to realize healthcare workers’ feelings of work meaningfulness and turn them into work engagement. The present research indicates the importance of creating a socially responsible and secure workplace for healthcare workers, especially during COVID-19.
Author Contributions
Conceptualization, B.D. and T.M.; methodology, T.M.; writing—original draft, T.M.; writing—review and editing, B.D.; supervision, B.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Xi’an Jiaotong-Liverpool University.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be requested from the first author.
Acknowledgments
We deeply thank anonymous reviewers for their insightful suggestions and constructive comments. We are grateful to the editors for their guidance and time for our manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhu, Y.; Chen, T.; Wang, J.; Wang, M.; Johnson, R.E.; Jin, Y. How critical activities within COVID-19 intensive care units increase nurses’ daily occupational calling. J. Appl. Psychol. 2021, 106, 4–14. [Google Scholar] [CrossRef]
- Kramar, R. Sustainable human resource management: Six defining characteristics. Asia Pac. J. Hum. Resour. 2022, 60, 146–170. [Google Scholar] [CrossRef]
- Reichers, A.E.; Schneider, B. Climate and culture: An evolution of constructs. In Organizational Climate and Culture; Schneider, B., Ed.; Jossey-Bass: San Francisco, CA, USA, 1990; pp. 5–39. [Google Scholar]
- Geiger, L. Leading towards Well-Being: Exploring Organizational Climate, Leadership and Individual Factors That Relate to Thriving at Work; Pepperdine University ProQuest LLC: Ann Arbor, MI, USA, 2013. [Google Scholar]
- Srisathan, W.A.; Ketkaew, C.; Naruetharadhol, P. The intervention of organizational sustainability in the effect of organizational culture on open innovation performance: A case of Thai and Chinese SMEs. Cogent Bus. Manag. 2020, 7, 1717408. [Google Scholar] [CrossRef]
- Zanasi, C.; Rota, C. Sustainable Relations in International Development Cooperation Projects: The Role of Human Resource Management and Organizational Climate; Federal Reserve Bank of St. Louis: St. Louis, MO, USA, 2010. [Google Scholar]
- Singh, P. Maintaining work motivation during trying times. In International Terrorism and Threats to Security: Managerial and Organizational Challenges; Burke, R., Cooper, C.L., Eds.; Edward Elgar: Cheltenham, UK, 2008; pp. 219–231. [Google Scholar]
- Wrzesniewski, A.; McCauley, C.; Rozin, P.; Schwartz, B. Jobs, careers, and callings: People’s relations to their work. J. Res. Personal. 1997, 31, 21–33. [Google Scholar] [CrossRef]
- Gatto, M. Nursing at ground zero: A life-changing experience. J. N. Y. State Nurses’ Assoc. 2002, 33, 5–9. [Google Scholar]
- Kahn, W.A. Psychological Conditions of Personal Engagement and Disengagement at Work. Acad. Manag. J. 1990, 33, 692–724. [Google Scholar] [CrossRef]
- Bellah, R.N.; Madsen, R.; Sullivan, W.M.; Swidler, A.; Tipton, S.M. Habits of the Heart; Harper & Row: New York, NY, USA, 1985. [Google Scholar]
- Rosso, B.D.; Dekas, K.H.; Wrzesniewski, A. On the meaning of work: A theoretical integration and review. Res. Organ. Behav. 2010, 30, 91–127. [Google Scholar] [CrossRef]
- Berg, J.M.; Grant, A.M.; Johnson, V. When Callings Are Calling: Crafting Work and Leisure in Pursuit of Unanswered Occupational Callings. Organ. Sci. 2010, 21, 973–994. [Google Scholar] [CrossRef]
- Dobrow, S. Extreme subjective career success: A new integrated view of having a calling. Acad. Manag. Proc. 2004, 2004, B1–B6. [Google Scholar] [CrossRef]
- Grant, A.M. The significance of task significance: Job performance effects, relational mechanisms, and boundary conditions. J. Appl. Psychol. 2008, 9, 108–124. [Google Scholar] [CrossRef]
- Wrzesniewski, A. Finding positive meaning in work. In Positive Organizational Scholarship: Foundations of a New Discipline; Cameron, K.S., Dutton, J.E., Quinn, R.E., Eds.; Berrett-Koehler Publishers: San Francisco, CA, USA, 2003; pp. 296–308. [Google Scholar]
- Zhao, W.W.; Liu, X.; Zhang, H. Family Embeddedness and Medical Students’ Interest for Entrepreneurship as an Alternative Career Choice: Evidence from China. Front. Psychol. 2021, 11, 593235. [Google Scholar] [CrossRef] [PubMed]
- Dobrow, R.S.; Heller, D. Follow your heart or your head? A longitudinal study of the facilitating role of calling and ability in the pursuit of a challenging career. J. Appl. Psychol. 2015, 100, 695–712. [Google Scholar] [CrossRef]
- Kahn, W.A.; Heaphy, E.D. Relational contexts of personal engagement at work. In Employee Engagement in Theory and Practice; Truss, C., Delbridge, R., Soane, E., Alfes, K., Shantz, A., Eds.; Routledge: London, UK, 2014; pp. 163–179. [Google Scholar]
- May, D.R.; Gilson, R.L.; Harter, L.M. The psychological conditions of meaningfulness, safety and availability and the engagement of the human spirit at work. J. Occup. Organ. Psychol. 2004, 77, 11–37. [Google Scholar] [CrossRef]
- Allan, B.A.; Batz-Barbarich, C.; Sterling, H.M.; Tay, L. Outcomes of meaningful work: A meta-analysis. J. Manag. Stud. 2019, 56, 500–528. [Google Scholar] [CrossRef]
- Ding, B.; Liu, W.; Tsai, S.; Gu, D.; Bian, F.; Shao, X. Effect of Patient Participation on Nurse and Patient Outcomes in Inpatient Healthcare. Int. J. Environ. Res. Public Health 2019, 16, 1344. [Google Scholar] [CrossRef] [PubMed]
- Shacklock, K.; Brunetto, Y. The intention to continue nursing: Work variables affecting three nurse generations in Australia. J. Adv. Nurs. 2012, 68, 36–46. [Google Scholar] [CrossRef]
- Guedes, A.R.; Oliveira, M.S.; Tavares, B.M.; Luna-Muschi, A.; Lazari, C.D.S.; Montal, A.C.; de Faria, E.; Maia, F.L.; Barboza, A.D.S.; Leme, M.D.; et al. Reinfection rate in a cohort of healthcare workers over 2 years of the COVID-19 pandemic. Sci. Rep. 2023, 13, 712. [Google Scholar] [CrossRef]
- Yim, F.H.; Fock, H.K. Social Responsibility Climate as a Double-Edged Sword: How Employee-Perceived Social Responsibility Climate Shapes the Meaning of Their Voluntary Work? J. Bus. Ethics 2013, 114, 665–674. [Google Scholar] [CrossRef]
- Dong, S.-Z.; Yang, L.; Ding, B.; Wu, C.-H.; Shao, X.-F. Pricing Strategy with Customers’ Privacy Concerns in Smart-X Systems. Enterp. Inf. Syst. 2020, 16, 445–471. [Google Scholar] [CrossRef]
- Liu, B.; Guo, S.; Ding, B. Technical Blossom in Medical Care: The Influence of Big Data Platform on Medical Innovation. Int. J. Environ. Res. Public Health 2020, 17, 516. [Google Scholar] [CrossRef] [PubMed]
- Shao, J.; Zhang, T.; Wang, H.; Tian, Y. Corporate Social Responsibility and Consumer Emotional Marketing in Big Data Era: A Mini Literature Review. Front. Psychol. 2022, 13, 2483. [Google Scholar] [CrossRef]
- Zohar, D.; Tenne-Gazit, O. Transformational leadership and Group Interaction as Climate Antecedents: A social network analysis. J. Appl. Psychol. 2008, 93, 744–757. [Google Scholar] [CrossRef]
- Liang, C.; Gu, D.; Tao, F.; Jain, H.K.; Zhao, Y.; Ding, B. Influence mechanism of patient-accessible HIS implementation on doctor-patient relationships: A service fairness perspective. Inf. Manag. 2017, 54, 57–72. [Google Scholar] [CrossRef]
- Chowdhury, S.K.; Endres, M.L. The impact of client variability on nurses’ occupational strain and injury: Cross-level moderation by safety climate. Acad. Manag. J. 2010, 53, 182–198. [Google Scholar] [CrossRef]
- Larsson, A.; Karlqvist, L.; Westerberg, M.; Gard, G. Identifying work ability promoting factors for home care aides and assistant nurses. BMC Musculoskelet Disord. 2012, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- McGhan, G.; Ludlow, N.C.; Rathert, C.; McCaughey, D. Variations in Workplace Safety Climate Perceptions and Outcomes across Healthcare Provider Positions. J. Healthc. Manag. 2020, 65, 202–215. [Google Scholar] [CrossRef]
- Consiglio, C.; Borgogni, L.; Di Tecco, C.; Schaufeli, W.B. What makes employees engaged with their work? the role of self-efficacy and employee’s perceptions of social context over time. Career Dev. Int. 2016, 21, 125–143. Available online: https://www.proquest.com/scholarly-journals/what-makes-employees-engaged-with-their-work-role/docview/1781724996/se-2 (accessed on 20 January 2022). [CrossRef]
- Lisbona, A.; Palaci, F.; Salanova, M.; Frese, M. The effects of work engagement and self-efficacy on personal initiative and performance. Psicothema 2018, 30, 89–96. [Google Scholar] [PubMed]
- Brislin, R.W. Translation and content analysis of oral and written material. In Handbook of Cross-Cultural Psychology: Methodology; Triandis, H.C., Berry, J.W., Eds.; Allyn and Bacon: Boston, MA, USA, 1980; pp. 389–444. [Google Scholar]
- Pejtersen, J.H.; Kristensen, T.S.; Borg, V.; Bjorner, J.B. The second version of the Copenhagen Psychosocial Questionnaire. Scand. J. Public Health 2010, 38, 8–24. [Google Scholar] [CrossRef] [PubMed]
- Hahn, S.; Murphy, L.R. A short scale for measuring safety climate. Saf. Sci. 2008, 46, 1047–1066. [Google Scholar] [CrossRef]
- Schaufeli, W.; Salanova, M.; Gonzalez-Roma, V.; Bakker, A. The Measurement of Engagement and Burnout: A Two Sample Confirmatory Factor Analytic Approach. J. Happiness Stud. 2002, 3, 71–92. [Google Scholar] [CrossRef]
- Zhang, L.; Farndale, E. Workforce age profile effects on job resources, work engagement and organizational citizenship behavior. Pers. Rev. 2021, 51, 194–209. [Google Scholar] [CrossRef]
- Goštautaitė, B.; Bučiūnienė, I. Work engagement during life-span: The role of interaction outside the organization and task significance. J. Vocat. Behav. 2015, 89, 109–119. [Google Scholar] [CrossRef]
- Nagarajan, R.; Ravikumar, A.S.; Reio, T.G.; Elangovan, R.; Parayitam, S. The COVID-19 impact on employee performance and satisfaction: A moderated moderated-mediation conditional model of job crafting and employee engagement. Hum. Resour. Dev. Int. 2022, 25, 600–630. [Google Scholar] [CrossRef]
- Liu, D.; Chen, Y.; Li, N. Tackling the negative impact of COVID-19 on work engagement and taking charge: A multi-study investigation of frontline health workers. J. Appl. Psychol. 2021, 106, 185. [Google Scholar] [CrossRef] [PubMed]
- Szilvassy, P.; Širok, K. Importance of work engagement in primary healthcare. BMC Health Serv. Res. 2022, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- De-la-Calle-Durán, M. Employee engagement and wellbeing in times of COVID-19: A proposal of the 5Cs model. Int. J. Environ. Res. Public Health 2021, 18, 5470. [Google Scholar] [CrossRef]
- Trougakos, J.P.; Chawla, N.; McCarthy, J.M. Working in a pandemic: Exploring the impact of COVID-19 health anxiety on work, family, and health outcomes. J. Appl. Psychol. 2020, 105, 1234–1245. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).