Abstract
Background: It is not known whether intensive care unit (ICU) patients’ family members realistically assess patients’ health status. Objectives: The aim was to investigate the agreement between family and intensivists’ assessment concerning changes in patient health, focusing on family members’ resilience and their perceptions of decision making. Methods: For each ICU patient, withdrawal criteria were assessed by intensivists while family members assessed the patient’s health development and completed the Connor–Davidson Resilience Scale and the Self-Compassion Scale. Six months after ICU discharge, follow-up contact was established, and family members gave their responses to two hypothetical scenarios. Results: 162 ICU patients and 189 family members were recruited. Intensivists’ decisions about whether a patient met the withdrawal criteria had 75,9% accuracy for prediction of survival. Families’ assessments were statistically independent of intensivists’ opinions, and resilience had a significant positive effect on the probability of agreement with intensivists. Six months after discharge, family members whose relatives were still alive were significantly more likely to consider that the family or patient themselves should be involved in decision-making. Conclusions: Resilience is related to an enhanced probability of agreement of the family with intensivists’ perceptions of patients’ health progression. Family attitudes in hypothetical scenarios were found to be significantly affected by the patient’s actual health progression.
1. Introduction
Intensive care units (ICUs) are for patients with medical conditions that imminently threaten their survival. Being hospitalized in ICU means that the patient’s physical health has suffered excessive and possibly irreversible damage [1]. Additionally, the generally unexpected admission of a patient to the ICU can be particularly frightening and distressing for their loved ones [2]. Higher levels of anxiety, depression, and stress during admission are commonly reported in the literature [3], while post-traumatic stress disorder and complicated grief occur after discharge [4]. Nonetheless, family members are seen as an integral part of the healthcare process and the need for good collaboration should always be considered.
The most important decision made during an ICU stay is often whether to use life-support devices to prolong life, or to discontinue life support and place more emphasis on comfort measures, given that further intervention is futile [5]. To make such a decision as objectively as possible, intensivists have been extensively and thoroughly trained to ensure that their judgment is based on globally recognized health indicators that objectively determine the patient’s clinical picture.
Under these circumstances, it is common for the patients not to be able to express their wishes to the medical team [6]. The role of family members is very important, as they are called upon not to express their own opinion on whether the patient’s life should be further mechanically assisted, but the patient’s own view, based on their perception of the patient’s personality and character, or after relevant discussions with the patient prior to admission to the ICU. It is not clearly known whether patients’ relatives realistically assess the patient’s status of health [6,7]. In fact, an unrealistic perception of the patient’s condition on the part of loved ones leads to tension and feelings of unease about the decision to withdraw life support, reflected in overall satisfaction with healthcare system performance [3,8,9].
Moreover, little is known about the factors that influence the patient’s family members when asked to make end-of-life decisions on the patient’s behalf. In this context, the concepts of mental resilience and self-compassion have been implicated as potential factors in the psychological well-being of families in the ICU, including the subject’s ability to succeed despite the adversities they face in life [10] and the subject’s ability to have a warm, caring, empathetic, and non-judgmental orientation towards the self at times of suffering and failure [11,12]. Specifically, our group found that self-compassion and mental resilience were highlighted as the two psychological traits that explain the overall psychological distress experienced by attendants in the ICU environment [13].
It is essential to examine the factors influencing the realistic view formed by the patient’s relatives, because these directly relate to the quality of communication with medical staff and the overall experience in the ICU. Therefore, the question arises whether these two characteristics are also related to the attendant’s increased ability to assess realistically the patient’s state of health and to agree with the intensivist’s opinion.
A primary aim of the present study was to fill this research gap by examining whether demographic variables, resilience, and self-compassion also influence family members’ realistic view of the patients’ health. Then, we considered the post-ICU attitudes of family members, and examined whether realistic attitudes during the experienced situation were related to the belief that the family should participate in decision-making in other hypothetical situations, and whether the evolution of the patient’s health played an important role. In doing so, we also assessed the validity of hypothetical scenarios as tools for identifying attitudes and perceptions, and their usefulness as policy-making tools.
2. Materials and Methods
2.1. Participants and Study Design
A cross-sectional study was conducted using a quantitative methodology, to evaluate psychological impact on relatives of critically ill patients. The data were collected in two time periods from 2019 to 2021; the first took place during the patient’s hospitalization in the ICU of our tertiary university hospital, while the second took place six months after the patient’s ICU discharge.
A total of 162 patients and their 189 family members, i.e., spouse, child, parent, or other, were recruited and agreed to participated in the study. Family members of patients with elective postoperative admission or brain death or who died within 1 week after admission were excluded from the study. Oral informed consent was obtained from family members and the study was approved by the Ethics Committee of the University Hospital of Ioannina.
Within the first two days after patient admission, the Glasgow coma score (GSC), the acute physiology, age and chronic health evaluation score (APACHE), and the simplified acute physiology score (SAPS) were assessed by ICU physicians. When the medical status and the prognosis of the patient were clarified, the director of the department together with the 3 most experienced intensivists completed a brief screening questionnaire describing whether the patient met any of eight criteria for withdrawal of treatment, along with a single direct question as to whether the patient would eventually survive. Then, 7–10 days after patient’s admission to the ICU and in the knowledge of the intensivists’s assessment of the patient’s health status, the relatives were asked to complete a multiple-choice questionnaire. For each family member, gender, age, type of relationship, and their assessment of the health progression of their relative were recorded on a five-point Likert scale (1: hopeless to 5: hopeful).
Additionally, each family member completed the Connor–Davidson resilience scale (CD-RISC) [14] and the self-compassion scale (SCS) [12]. The CD-RISC consists of 25 items that are answered on a 5-point frequency scale (0 to 4). CD-RISC’s total score ranges from 0 to 100, with higher scores indicating greater perceived resilience [14]. The SCS consists of 26 questions answered on a 5-point frequency scale (1 to 5), and the total score is calculated as the overall mean after 13 of the score values are reversed [12]. The total score reflects self-compassion as defined as a dynamic balance between compassionate and uncompassionate ways in which individuals respond emotionally to pain and failure, cognitively understand their predicament, and pay attention to suffering [12].
Six months after each patient’s ICU discharge, telephone follow-up contact was established with 153/189 (81%) of participants, all of whom had close contacts with a patient. During this telephone interview, family members answered four questions about two hypothetical clinical scenarios: one with a conscious and competent patient being able to comprehend his actual state of health, and one with an unconscious patient who cannot participate in medical decisions that affecting him. In both scenarios, the first question assessed whether the patient’s family should be involved in the decision to withdraw life support measures, while the second question aimed to capture the family member’s opinion about who should be responsible for making the decision. The two scenarios were taken from a previous study [15] and translated into Greek with minor changes in the responses, allowing independent selection of all those involved in the decision-making process.
2.2. Statistical Analysis
The Chi-square test of independence was applied to evaluate whether two nominal or ordinal variables were statistically independent. Analysis of variance was applied to quantify the differences between more than two groups, while Tukey’s b test was employed to highlight the homogeneous groups. To elucidate the similarities between respondents’ answers in the hypothetical scenarios, the distances between pairs of binary variables were computed using the Dice coefficient of similarity (known also as the Czekanowski or Sorensen measure) [16]. Then, a hierarchical cluster analysis was applied to provide an indicative grouping of similar responses. A logistic regression model was applied to test whether demographic factors, resilience, and self-compassion affected agreement between family members’ and intensivists’ assessments, and a second logistic model was applied in order to test whether agreement in assessment and the progression of patient’s health affected respondents’ perceptions in analogous scenarios.
A two-sided level of significance of 0.05 was set for all statistical tests. The data were analyzed using SPSS statistical package (version 21) and R statistical language [17].
3. Results
3.1. Sample Characteristics
The demographic sample characteristics for family members and patients are presented in Table 1. The mean age of family members was 46.5 (SD 11.4 years) and the corresponding figure for the patients was 64.4 (SD 17.2 years). Among the family members, 111 (58.7%) were women; the corresponding figure for the patients was 52 (32.1%).

Table 1.
Family members’ and patients’ characteristics.
3.2. Intensivists Criteria for Withdrawing Life-Sustaining Treatment
Among the 162 patients admitted to the ICU, 46 (28.4%) met the intensivists’ criteria for treatment withdrawal. Lack of future quality of life and futility of treatment were the dominant clinical assessments. Meanwhile, hospital costs were not regarded as a withdrawal criterion for any patient, while age was considered a criterion for six patients (M = 78.7 years, SD = 3.8) (Table 2).

Table 2.
Intensivists’ criteria for withdrawal or non-escalation of support measures.
The 46 patients that met the withdrawal criteria were significantly older (73.3 ± 11.5 vs. 60.9 ± 17.8, p < 0.001) than the others, they were characterized by significantly higher SAPS scores (54.7 ± 13.8 vs. 39.1 ± 12.7, p < 0.001) and APACHE scores (21.5 ± 5.7 vs. 15.9 ± 5.8, p < 0.001), and significantly lower GCS scores (7.0 ± 3.0 vs. 10.1 ± 3.5, p < 0.001). During ICU hospitalization, 25/46 passed away, with the remaining 21 patients at ICU discharge presenting severe disability regarding feeding (nasogastric tube or gastrostomy), breathing (tracheostomy), or mobility (hemiplegia, tetraplegia, critical care myopathy). Six months after ICU hospitalization, nine patients were still alive with little (7) or moderate (2) health recovery, and unable to live autonomously. Overall, the accuracy of the physician’s classification (PAC) concerning patient’s survival was 75.9% during hospitalization, and 71% six months after hospitalization (Table 3).

Table 3.
Patients’ survival at ICU discharge and 6 months later, and survival prediction.
3.3. Family Members’ Agreement with Intensivists Concerning Patient’s Health
About half of the 189 respondents (86, 45.5%) were overly optimistic about the patient’s health progress (Table 4). The subjective optimism expressed by the patients’ family members was statistically independent of the intensivist’s evaluation (c2(4) = 6.279, p = 0.179). The family members were divided into three categories according to their assessments, in comparison with the those of the intensivists. The first category comprised family members who did not expect a positive change in the patient’s health, while the doctors insisted on the continuation of life support (N = 38). The second group contained the family members who perceived the patient’s state of health in agreement with the intensivist’s perception (N = 108), and the third category included family members who expected a positive development in the patient’s health while the intensivists suggested withdrawal of life support (N = 36). Overall, 74 (40.7%) of the respondents were not in agreement with intensivists’ judgments about changes in the health of their relative (Table 4).

Table 4.
Family members’ assessment of the progress of patient health and comparison to the intensivists’ assessment.
The mean resilience score for the total sample of family members was 70.8 (SD = 14.4) analogous to the general Greek population (MP = 70.2, SD = 11.4) [18]. The mean score for self-compassion was 3.3 (SD = 0.5), considered moderate (2.5 to 3.5) due to the lack of clinical norms or scores to suggest that an individual has high or low self-compassion [19].
Logistic regression was carried out to quantify the effects of the patients’ age and gender, family members’ age and gender, staying with the patient, resilience, and self-compassion in terms of the agreement between the attendant’s and intensivist’s assessment of the patient’s health. The logistic model was statistically significant (omnibus test of model coefficients: c2(8) = 19.432, p = 0.013), being able to predict correctly 66.7% of the observations (sensitivity 81.6%, specificity 45.1%, 2-log likelihood = −215.865, McFadden’s pseudo R squared = 0.083) (Table 5).

Table 5.
Logistic prediction model of agreement between attendants’ and intensivists’ assessments.
The attendant’s resilience (B = 0.031, ExpB = 1.032, 95% C.I. 1.005–1.060, p = 0.022), had a significant effect on the probability of agreement concerning the patient’s health. Specifically, an additional score of one on the resilience scale corresponded to 1.032 times greater likelihood that the respondent agreed with the intensivist’s view of the patient’s health. In particular, those who agreed were characterized by a significantly higher resilience score (MNA = 68.0 vs. MAG = 73.0, t(172) = 2.402, p = 0.017).
The effect of the patient’s age on realism was marginally rejected at the 0.05 level (B = −0.020, ExpB = 0.980, 95% C.I. 0.960–1.000, p = 0.050), suggesting a noteworthy but not significant effect. In this context, it is worth noting that the statistically significant difference between patient age in the two groups (MNA = 68.0 vs. MAG = 60.6, t(172) = 2.775, p = 0.006).
3.4. Family Participation in the Theoretical Scenarios, 6 Months after the ICU Experience
At the second sampling timeperiod, among the 153 family members that responded to the study, 13 were parents, 31 were spouses, 18 were brothers, and 91 were offspring. In both hypothetical scenarios, most of the respondents favored family participation in decision making (Scenario 1: 78, 51.0%, Scenario 2: 109, 71.2%) (Table 6).

Table 6.
The hypothetical clinical scenarios.
A logistic regression analysis was applied to test the effects of patient’s age, agreement with intensivists during hospitalization, and survival of the patient on the probability of considering family or patient responsible for the withdrawal decision. The logistic model was statistically significant (Omnibus Test of Model Coefficients: c2(5) = 12.888, p = 0.024), being able to predict 66.7% of the observations correctly (sensitivity 93.9%, specificity 18.2%, −2-log likelihood = −186.966, Nagelkerke pseudo R squared = 0.111) (Table 7).

Table 7.
Effects of patients’ characteristics on family/patient selection in the two theoretical scenarios.
A significant interaction between the patient’s age and his or her health condition was identified (Wald W = 6.873, df = 2, p = 0.032). Specifically, as the age of patients increased, respondents whose relatives were still alive and lived autonomously were significantly more likely to consider the patient himself or the family as those who should be involved in decision making. In contrast, in cases where the patient had died, as the age of their deceased relatives increased the respondents tended to hesitate to declare the family responsible for decision making in the theoretical scenarios (Figure 1).
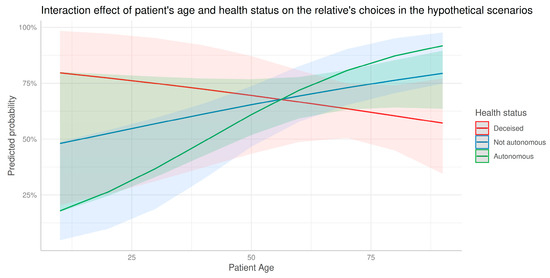
Figure 1.
Interaction effect of age and health status on family members’ selections in the hypothetical scenarios. Predicted probability refers to the probability of a response that the patient himself or the family should be involved in the decision-making.
4. Discussion
Withdrawal of life-sustaining therapy, while not a strictly documented procedure, is an ethically acceptable practice in western ICUs. For example, in the Ethicus-2 study, a prospective observational study of 199 ICUs in 36 countries involving 87,951 patients who were admitted to ICU over a 6-month period, 12,850 (14.6%) patients died, with treatment limitations (withholding or withdrawing life-sustaining treatment) occurring frequently (80.9%). Common factors associated with treatment limitation included patient’s age and chronic disease, together with the presence of country-specific end-of-life legislation [20,21]. The decision to withdraw extensive supportive care is made by ICU physicians, based on measurable indicators of physical functioning and objective observations of vital signs. As most critically ill patients lack decision-making capacity and family members often serve as surrogate decision makers, decisions about the end of life should involve the family. Unfortunately, not only do data about true family participation in end-of-life decisions remain scarce, but end-of-life communication with families or surrogates varies markedly in different global regions; according to the Ethicus-2 study, discussion with family occurred only in 46.4% of cases in southern Europe, while in northern and central Europe percentages were significantly higher at 95.0% and 74.9.%, respectively [22,23]. For Greece, data are even more limited. In a national Greek study conducted across 18 multidisciplinary Greek ICUs dating back to 2015, 71.4% of 149 doctors and 59.8% of 320 nurses responded that families were not actively involved in discussion of life-sustaining treatment, confirming that in Greece fear of litigation is still considered a major barrier to properly informing the patients’ relatives about end-of-life decisions [24]. Since no clear, discontinuation criteria are defined in other countries either, the final decision always lies with the physicians, and is usually based on their experience and training [25]. However, making life-or-death decisions for another person is never an inconsequential decision for physicians, as reflected in increased burnout and distress among medical staff [26] and less empathetic and more cynical behaviour towards ICU patients [27]. In this regard, the present study suggests that the psychological pressure faced by medical staff does not affect their assessment of whether patients meet the withdrawal criteria. Poor quality of life in future and futility of treatment were found to be the most important criteria for the discontinuation of life-sustaining measures, while patients’ gender or age as well as treatment costs did not significantly influence the decision. It was also found that ICU physician assessment accurately assesses patients’ chances of survival during their hospital stay and in the immediate future. It is worth mentioning that in the Ethicus-2 study, 20% of patients with treatment limitations eventually survived the hospital stay, and the percentage in the earlier Ethicus-1 study (1999–2000) was even lower [20,21].
On a different note, in the burdensome environment of an ICU, members of the patient’s family are in a vulnerable position where depressive symptoms [28,29] and higher risk of anxiety and stress-related disorders are commonly reported [30]. Given this great psychological pressure, it is not surprising that for out of ten family members did not realistically assess the health progression of their relatives in ICU. In particular, the fact that the psychological symptoms of the family members were independent of the severity of the patient’s condition is supported by the findings of previous research [31].
Nevertheless, a realistic view is always necessary, because unjustified optimism makes it difficult to adjust to the loss of a loved one, promotes feelings of meaninglessness, and can lead to painful after-experiences in the ICU. This was demonstrated in the study by Sjökvist et al. [15], where the general public stated that they preferred greater influence from patients and families compared with intensive-care physicians in decisions to withdraw life support. The results of the present study further clarify these differences by highlighting mental resilience as the trait that determines the consent of family members to intensivists’ assessments. That is, this study further demonstrates the importance of resilience, previously shown in the study by Stamou et al. [13], as a psychological trait that reduces the overall psychological burden of ICU attendants.
Moreover, resilience, as commonly defined as the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress, is highlighted as a key feature facilitating the transition from the initial emotional distress experienced by family members in the ICU to a sense of regained control [13]. As one such key feature, resilience provides family members with the right conditions to seek and create meaning in their situation and gives them purpose in contributing to their relative’s recovery. Therefore, an appropriate collaborative approach should be developed between family members and healthcare professionals, to address the patient’s needs while providing emotional and psychosocial support to their families [32]. Specifically, it is suggested that initiatives aiming to strengthen mental resilience will help relatives’ agreement with the opinions of critical care physicians, enhance quality of communication, reduce feelings of frustration and dissatisfaction from intensivists as well as relatives, and improve the overall satisfaction of the patient’s companions about the care their loved one receives [33,34].
After hospitalization in the ICU, most surviving patients require constant and long-term care and are unable to care for themselves. This situation, commonly referred to as post-intensive care syndrome (PICS), can affect the patient’s body, thoughts, feelings, and mental state [35]. Of course, this also puts strain on the family environment, both psychologically and financially. In the context of the two theoretical scenarios, caregivers of a surviving patient were reluctant to attribute family responsibility for life-sustaining decisions as their patients aged, a finding that indicates that their personal experiences strongly influenced the responses to the theoretical scenarios. It might be argued that positive health progress appears to predispose respondents to family involvement, while poor progress or the death of a loved one appears to reduce the desire to involve the family in life-support decisions affecting the ICU patient. Overall, a biased attitude was evident in our study, with personal experiences strongly influencing responses to theoretical scenarios. We found that the death of the patient distances the caregiving relative from the traumatic event of their family member’s hospitalization in the ICU. Furthermore, results indicated a limited validity of these instruments as decision-making aids with regard to the involvement of the family in withdrawal decisions in the ICU environment.
There is ample evidence in the current literature that family members desire a more active role in end-of-life decision-making, in order to communicate patient’s wishes [36]. There is also consensus that end-of-life decisions should be viewed as shared decisions, with shared responsibility between the care team, the patient, and the family [37]. In this context, it is of paramount importance for intensivists to provide patients and their families with reliable information to help them decide whether withdrawal of life-support measures is the appropriate medical option [38]. Complete and comprehensible information about the medical data supporting the discontinuation of patient support could help loved ones to resolve their doubts about the treatment being offered, to understand the futility of the treatment, and to appreciate the severely reduced quality of life that awaits the patient if they survive after ICU [39]. Although the crucial need for complete and accurate information for family members of ICU patients has been widely reported [40,41] this factor seems to be underestimated by caregivers [42]. Since treatment futility is a rather vague concept and various attempts have been made to resolve this problem [43,44,45], there is a need for improvement in the communication skills of ICU staff so they can better distinguish and describe to relatives the individual aspects of treatment futility. With regard to the goal of family consent to the doctors’ decisions, an additional initiator could be the family’s right to additional patient care, which has also been described in the literature as a demand [44]. This opportunity would allow family members to experience the situation, recognize the futility of treatment, and create personal meaning for the potential loss of their loved one, making the loss gentler for them. Especially in the current context of COVID-19 with the noted shortage of ICU beds worldwide, better communication skills and methods between family members and caregivers will enable faster decisions and allow medical staff to provide medical care and hospitalization to people who need it most [45,46].
To the best of our knowledge, this is the first study to examine personal experience and resilience in relation to family members’ realistic views of ICU patient health as factors influencing attitudes towards end-of-life decisions.The use of disease severity scores such as GSC, APACHE, and SAPS to compare against family views is one of this study’s strengths.
Our study had some limitations. First, our results reported responses from one single ICU; hence their lack of generalizability should not be ignored. Second, family members who declined to participate at the second phase of the study i.e., six months after the ICU experience, may have reported different attitudes and perceptions. Furthermore, we did not assess post-ICU distress symptoms or post-ICU resilience and are therefore unable to justify the role played by such factors in long-term attitudes towards end-of-life decisions. Finally, since the data for the hypothetical scenarios were collected six months after ICU experience, the possibility of recall bias cannot be ruled out.
5. Conclusions
Family members of patients admitted to ICU have increased needs in terms of assurance, proximity, and information, and these requirements should be carefully considered by ICU staff [2]. The results of our study indicate that resilience as a personality trait was associated with an increased likelihood of agreement between family members and physicians’ perceptions of the patient’s health. Thus, it is suggested that mental resilience initiatives can help family members to adapt well to the overwhelming experiences in ICU and to recognize the situation pragmatically. In particular, the development of a philosophy of family-centred care should be a priority, with formal assessment of families taking place shortly after admission, followed by development of an appropriate care plan [47]. From this perspective, a collaborative approach between family members and medical staff will enhance the quality of communication, reduce feelings of frustration and dissatisfaction among physicians and relatives, and improve overall satisfaction with the care received.
Furthermore, family members’ perceptions of the patient’s health progress are related to their psychological characteristics, while the way they responded to the two hypothetical scenarios was related to their patient’s health progress (Supplementary Table S1). Therefore, it is cautioned that family members may have difficulty separating what they feel is best from what they believe the patient would think best [48]. It is suggested that the involvement of family members in important decisions regarding the patient life-support should be required of physicians working in critical care, while it appears that the ultimate decision should remain the sole responsibility of medical staff. However, we believe our findings merit further investigation with increased consideration given to the communication skills between ICU staff and family members; a factor that we did not examine herein.
Finally, the appropriateness of hypothetical scenarios for ascertaining citizens’ perceptions is not supported, or at least their more cautious use and careful interpretation of the responses is suggested, which should consider the respondents’ recent exposure to relevant traumatic events as well as the trajectory of these events.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare11030345/s1. Supplementary Table S1: Proximity matrix of the answers to the four questions in the two hypothetical scenarios (Dice measure).
Author Contributions
Conceptualization, V.K, M.G. and P.S.; methodology, V.K., G.P. and E.D; software, M.G. and E.D.; validation, V.K., G.P. and D.T.; investigation, P.S.; writing—original draft preparation, P.S., D.T and E.D.; writing—review and editing, V.K., G.P. and M.G.; visualization, M.G. and E.D.; supervision, V.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University Hospital of Ioannina (protocol code 3263, 1 February 2019).
Informed Consent Statement
Oral informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
Naum Konstantina and Evaggelos Ioannou for administrative support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Maki, D.G.; Crnich, C.J.; Safdar, N. Nosocomial Infection in the Intensive Care Unit. In Critical Care Medicine; Elsevier: Amsterdam, The Netherlands, 2008; pp. 1003–1069. [Google Scholar] [CrossRef]
- Alsharari, A.F. The needs of family members of patients admitted to the intensive care unit. Patient Prefer. Adherence 2019, 13, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Abdul Halain, A.; Tang, L.Y.; Chong, M.C.; Ibrahim, N.A.; Abdullah, K.L. Psychological distress among the family members of Intensive Care Unit (ICU) patients: A scoping review. J. Clin. Nurs. 2022, 31, 497–507. [Google Scholar] [CrossRef] [PubMed]
- Cameron, J.I.; Chu, L.M.; Matte, A.; Tomlinson, G.; Chan, L.; Thomas, C.; Friedrich, J.O.; Mehta, S.; Lamontagne, F.; Levasseur, M.; et al. One-Year Outcomes in Caregivers of Critically Ill Patients. N. Engl. J. Med. 2016, 374, 1831–1841. [Google Scholar] [CrossRef] [PubMed]
- Myatra, S.N.; Salins, N.; Iyer, S.; Macaden, S.C.; Divatia, J.V.; Muckaden, M.; Kulkarni, P.; Simha, S.; Mani, R.K. End-of-life care policy: An integrated care plan for the dying: A Joint Position Statement of the Indian Society of Critical Care Medicine (ISCCM) and the Indian Association of Palliative Care (IAPC). Indian J. Crit. Care Med. 2014, 18, 615–635. [Google Scholar] [CrossRef]
- Adams, J.A.; Anderson, R.A.; Docherty, S.L.; Tulsky, J.A.; Steinhauser, K.E.; Bailey, D.E., Jr. Nursing strategies to support family members of ICU patients at high risk of dying. Heart Lung 2014, 43, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Akdeniz, M.; Yardımcı, B.; Kavukcu, E. Ethical considerations at the end-of-life care. SAGE Open Med. 2021, 9, 20503121211000918. [Google Scholar] [CrossRef]
- McAdam, J.L.; Puntillo, K. Symptoms experienced by family members of patients in intensive care units. Am. J. Crit. Care 2009, 18, 200–209, quiz 210. [Google Scholar] [CrossRef]
- Myhren, H.; Ekeberg, Ø.; Stokland, O. Satisfaction with communication in ICU patients and relatives: Comparisons with medical staffs’ expectations and the relationship with psychological distress. Patient Educ. Couns. 2011, 85, 237–244. [Google Scholar] [CrossRef]
- Bonanno, G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef]
- Gilbert, P. The Compassionate Mind; Robinson: Torrance, CA, USA, 2009. [Google Scholar]
- Neff, K.D. The Development and Validation of a Scale to Measure Self-Compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Stamou, P.; Gouva, M.; Konstanti, Z.; Papathanasiou, A.; Koulouras, V.; Papathanakos, G. Psychological Factors Affecting the Family’s Satisfaction of Patients in an Intensive Care Unit: The Dominant Role of Self-Compassion and Resilience. Open J. Nurs. 2022, 12, 334–348. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Sjökvist, P.; Nilstun, T.; Svantesson, M.; Berggren, L. Withdrawal of life support--who should decide? Differences in attitudes among the general public, nurses and physicians. Intensive Care Med. 1999, 25, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Dice, L.R. Measures of the Amount of Ecologic Association Between Species. Ecology 1945, 26, 297–302. [Google Scholar] [CrossRef]
- RC Team. Core. R: A Language and Environment for Statistical Computing; RC Team: Vienna, Austria, 2018. [Google Scholar]
- Tsigkaropoulou, E.; Douzenis, A.; Tsitas, N.; Ferentinos, P.; Liappas, I.; Michopoulos, I. Greek Version of the Connor-Davidson Resilience Scale: Psychometric Properties in a Sample of 546 Subjects. In Vivo 2018, 32, 1629–1634. [Google Scholar] [CrossRef]
- Neff, K.D. Self-Compassion: Theory, Method, Research, and Intervention. Annu. Rev. Psychol. 2023, 74, 193–218. [Google Scholar] [CrossRef]
- Avidan, A.; Sprung, C.L.; Schefold, J.C.; Ricou, B.; Hartog, C.S.; Nates, J.L.; Jaschinski, U.; Lobo, S.M.; Joynt, G.M.; Lesieur, O.; et al. Variations in end-of-life practices in intensive care units worldwide (Ethicus-2): A prospective observational study. Lancet Respir. Med. 2021, 9, 1101–1110. [Google Scholar] [CrossRef]
- Sprung, C.L.; Cohen, S.L.; Sjokvist, P.; Baras, M.; Bulow, H.H.; Hovilehto, S.; Ledoux, D.; Lippert, A.; Maia, P.; Phelan, D.; et al. End-of-life practices in European intensive care units: The Ethicus Study. Jama 2003, 290, 790–797. [Google Scholar] [CrossRef]
- Hartog, C.S.; Maia, P.A.; Ricou, B.; Danbury, C.; Galarza, L.; Schefold, J.C.; Soreide, E.; Bocci, M.G.; Pohrt, A.; Sprung, C.L.; et al. Changes in communication of end-of-life decisions in European ICUs from 1999 to 2016 (Ethicus-2)—A prospective observational study. J. Crit. Care 2022, 68, 83–88. [Google Scholar] [CrossRef]
- Feldman, C.; Sprung, C.L.; Mentzelopoulos, S.D.; Pohrt, A.; Hartog, C.S.; Danbury, C.; Weiss, M.; Avidan, A.; Estella, A.; Joynt, G.M.; et al. Global Comparison of Communication of End-of-Life Decisions in the ICU. Chest 2022, 162, 1074–1085. [Google Scholar] [CrossRef]
- Ntantana, A.; Matamis, D.; Savvidou, S.; Marmanidou, K.; Giannakou, M.; Gouva, Μ.; Nakos, G.; Koulouras, V. The impact of healthcare professionals’ personality and religious beliefs on the decisions to forego life sustaining treatments: An observational, multicentre, cross-sectional study in Greek intensive care units. BMJ Open 2017, 7, e013916. [Google Scholar] [CrossRef]
- Phua, J.; Joynt, G.M.; Nishimura, M.; Deng, Y.; Myatra, S.N.; Chan, Y.H.; Binh, N.G.; Tan, C.C.; Faruq, M.O.; Arabi, Y.M.; et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern. Med. 2015, 175, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Curtis, J.R.; Vincent, J.L. Ethics and end-of-life care for adults in the intensive care unit. Lancet 2010, 376, 1347–1353. [Google Scholar] [CrossRef] [PubMed]
- Kompanje, E.J.O. Burnout, boreout and compassion fatigue on the ICU: It is not about work stress, but about lack of existential significance and professional performance. Intensive Care Med. 2018, 44, 690–691. [Google Scholar] [CrossRef] [PubMed]
- Bolosi, M.; Peritogiannis, V.; Tzimas, P.; Margaritis, A.; Milios, K.; Rizos, D.V. Depressive and Anxiety Symptoms in Relatives of Intensive Care Unit Patients and the Perceived Need for Support. J. Neurosci. Rural. Pract. 2018, 9, 522–528. [Google Scholar] [CrossRef]
- Rose, L.; Muttalib, F.; Adhikari, N.K.J. Psychological Consequences of Admission to the ICU: Helping Patients and Families. Jama 2019, 322, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Jezierska, N. Psychological reactions in family members of patients hospitalised in intensive care units. Anaesthesiol. Intensive Ther. 2014, 46, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Kourti, M.; Christofilou, E.; Kallergis, G. Anxiety and depression symptoms in family members of ICU patients. Av. Enfermería 2015, 33, 47–54. [Google Scholar] [CrossRef]
- Wong, P.; Liamputtong, P.; Koch, S.; Rawson, H. Searching for meaning: A grounded theory of family resilience in adult ICU. J. Clin. Nurs. 2019, 28, 781–791. [Google Scholar] [CrossRef]
- Rawal, G.; Yadav, S.; Kumar, R. Post-intensive Care Syndrome: An Overview. J. Transl. Int. Med. 2017, 5, 90–92. [Google Scholar] [CrossRef]
- Lind, R.; Lorem, G.F.; Nortvedt, P.; Hevrøy, O. Family members’ experiences of “wait and see” as a communication strategy in end-of-life decisions. Intensive Care Med. 2011, 37, 1143–1150. [Google Scholar] [CrossRef]
- Thompson, B.T.; Cox, P.N.; Antonelli, M.; Carlet, J.M.; Cassell, J.; Hill, N.S.; Hinds, C.J.; Pimentel, J.M.; Reinhart, K.; Thijs, L.G. Challenges in end-of-life care in the ICU: Statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003: Executive summary. Crit. Care Med. 2004, 32, 1781–1784. [Google Scholar] [CrossRef]
- Shin, K.; Mok, J.H.; Lee, S.H.; Kim, E.J.; Seok, N.R.; Ryu, S.S.; Ha, M.N.; Lee, K. The current status of medical decision-making for dying patients in a medical intensive care unit: A single-center study. Korean J. Crit. Care Med. 2014, 29, 160–165. [Google Scholar] [CrossRef]
- Bailey, J.J.; Sabbagh, M.; Loiselle, C.G.; Boileau, J.; McVey, L. Supporting families in the ICU: A descriptive correlational study of informational support, anxiety, and satisfaction with care. Intensive Crit. Care Nurs. 2010, 26, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Hinkle, J.L.; Fitzpatrick, E. Needs of American relatives of intensive care patients: Perceptions of relatives, physicians and nurses. Intensive Crit. Care Nurs. 2011, 27, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, G.F.; Kirby, A.S. The perspective of families of the critically ill patient: Their needs. Curr. Opin. Crit Care 2006, 12, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Bijttebier, P.; Vanoost, S.; Delva, D.; Ferdinande, P.; Frans, E. Needs of relatives of critical care patients: Perceptions of relatives, physicians and nurses. Intensive Care Med. 2001, 27, 160–165. [Google Scholar] [CrossRef]
- Youngner, S.J. Who defines futility? Jama 1988, 260, 2094–2095. [Google Scholar] [CrossRef]
- Schneiderman, L.J.; Jecker, N.S.; Jonsen, A.R. Medical futility: Its meaning and ethical implications. Ann. Intern. Med. 1990, 112, 949–954. [Google Scholar] [CrossRef]
- Wilkinson, D.J.; Savulescu, J. Knowing when to stop: Futility in the ICU. Curr. Opin. Anaesthesiol. 2011, 24, 160–165. [Google Scholar] [CrossRef]
- Keenan, A.; Joseph, L. The needs of family members of severe traumatic brain injured patients during critical and acute care: A qualitative study. Can. J. Neurosci. Nurs. 2010, 32, 25–35. [Google Scholar] [PubMed]
- Huynh, T.N.; Kleerup, E.C.; Raj, P.P.; Wenger, N.S. The opportunity cost of futile treatment in the ICU*. Crit. Care Med. 2014, 42, 1977–1982. [Google Scholar] [CrossRef] [PubMed]
- Mathews, K.S.; Durst, M.S.; Vargas-Torres, C.; Olson, A.D.; Mazumdar, M.; Richardson, L.D. Effect of Emergency Department and ICU Occupancy on Admission Decisions and Outcomes for Critically Ill Patients. Crit. Care Med. 2018, 46, 720–727. [Google Scholar] [CrossRef]
- McKiernan, M.; McCarthy, G. Family members’ lived experience in the intensive care unit: A phemenological study. Intensive Crit. Care Nurs. 2010, 26, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Schenker, Y.; Crowley-Matoka, M.; Dohan, D.; Tiver, G.A.; Arnold, R.M.; White, D.B. I don’t want to be the one saying ‘we should just let him die’: Intrapersonal tensions experienced by surrogate decision makers in the ICU. J. Gen. Intern. Med. 2012, 27, 1657–1665. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).