Citation Network Analysis of Nurse Staffing Research from the Past Two Decades: 2000–2022
Abstract
1. Background
2. Methods Section
2.1. Design and Data Collection
2.2. Analysis
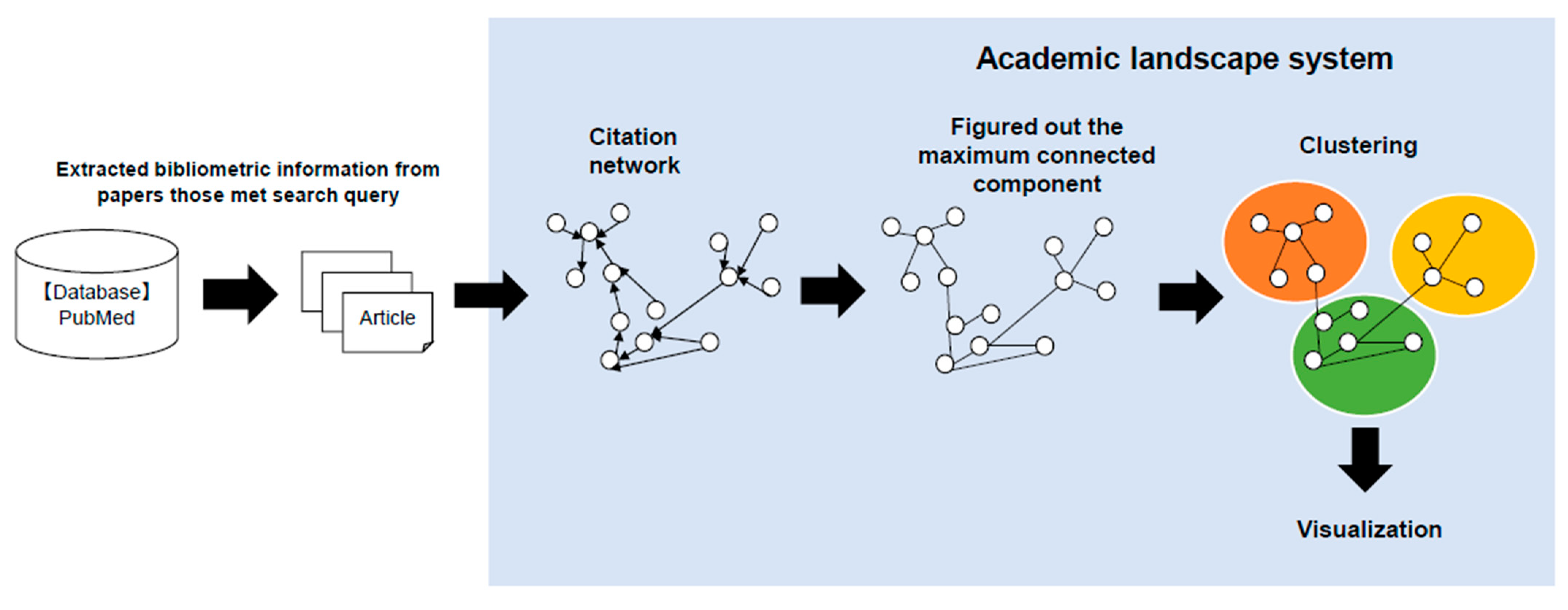
2.2.1. Citation Network Analysis
2.2.2. Analysis of Publication Trends, Authors, and Journals
3. Results
3.1. Global Publication Trends from 2000 to 2022
3.2. Analysis of Authors and Journals
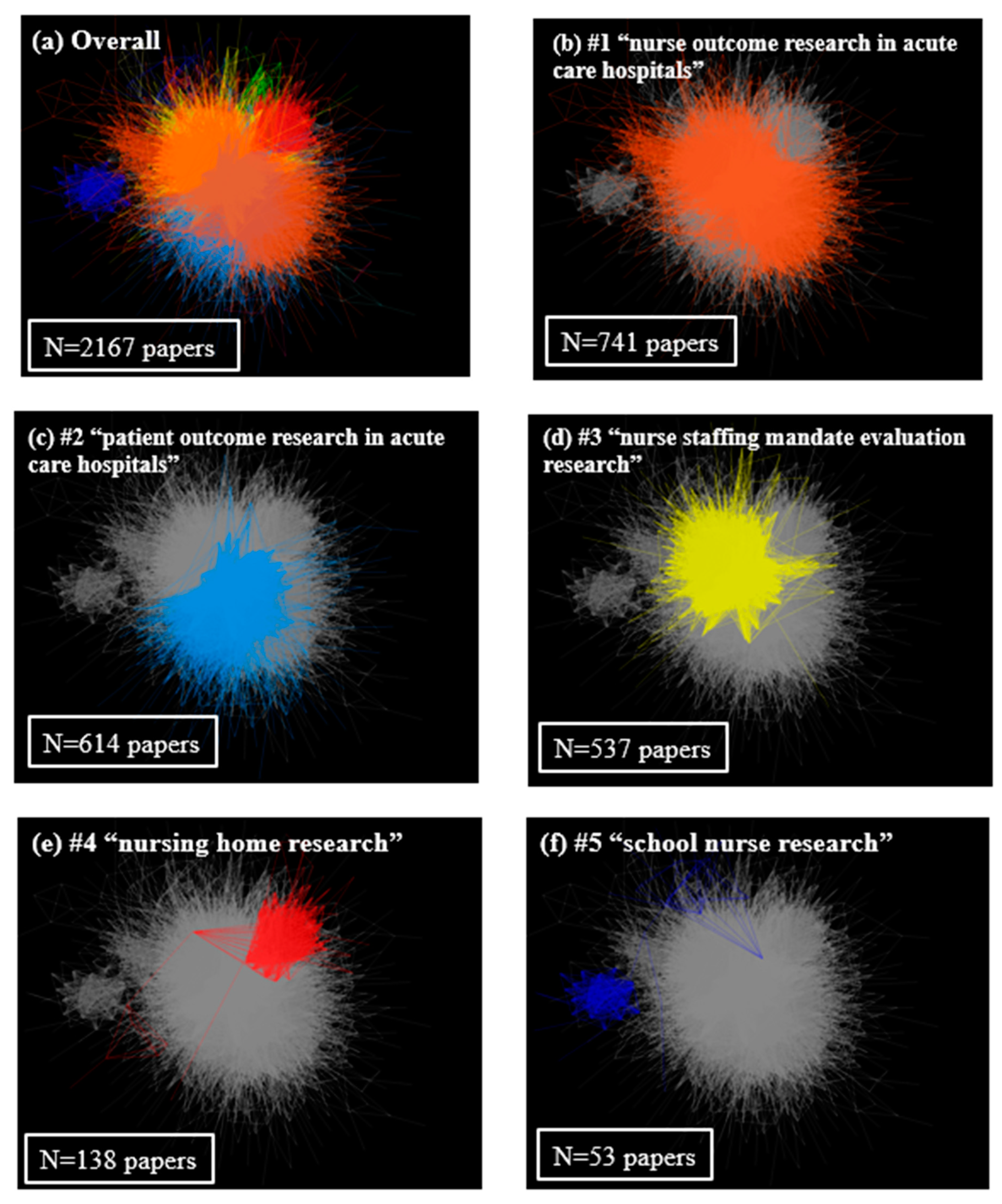
3.3. The Clustered Network Map of Co-Cited References
4. Discussion
4.1. Overall Publication Trends and Leading Authors and Journals from 2000 to 2022
4.2. Cluster by Citation Network Analysis
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Number of Articles That Met the Search Query | |
|---|---|
| “nurse staffing” | 26,194 |
| “nurse workload” | 8113 |
| “nurse workforce” | 18,801 |
| “nurses to patients” | 163,885 |
| “nurse to patients” | 163,885 |
| “nurse to patient” | 163,885 |
| “nurses-to-patients” | 163,885 |
| “nurse-to-patients” | 163,885 |
| “nurse-to-patient” | 414 |
| “patients to nurses” | 163,885 |
| “patient to nurses” | 163,885 |
| “patient to nurse” | 163,885 |
| “patients-to-nurses” | 163,885 |
| “patient-to-nurses” | 163,885 |
| “patient-to-nurse” | 171 |
| “nurses to beds” | 2357 |
| “nurse to beds” | 2357 |
| “nurse to bed” | 7235 |
| “nurses-to-beds” | 7235 |
| “nurse-to-beds” | 7235 |
| “nurse-to-bed” | 39 |
| number of nurses | 29,725 |
| “nurse staffing” [Title/Abstract] | 1752 |
| “nurse workload” [Title/Abstract] | 147 |
| “nurse workforce” [Title/Abstract] | 280 |
| “nurses to patients” [Title/Abstract] | 0 |
| “nurse to patients” [Title/Abstract] | 0 |
| “nurse to patient” [Title/Abstract] | 415 |
| “nurses-to-patients” [Title/Abstract] | 0 |
| “nurse-to-patients” [Title/Abstract] | 0 |
| “nurse-to-patient” [Title/Abstract] | 415 |
| “patients to nurses” [Title/Abstract] | 0 |
| “patient to nurses” [Title/Abstract] | 0 |
| “patient to nurse” [Title/Abstract] | 171 |
| “patients-to-nurses” [Title/Abstract] | 0 |
| “patient-to-nurses” [Title/Abstract] | 0 |
| “patient-to-nurse” [Title/Abstract] | 171 |
| “nurses to beds” [Title/Abstract] | 0 |
| “nurse to beds” [Title/Abstract] | 0 |
| “nurse to bed” [Title/Abstract] | 39 |
| “nurses-to-beds” [Title/Abstract] | 0 |
| “nurse-to-beds” [Title/Abstract] | 0 |
| “nurse-to-bed” [Title/Abstract] | 39 |
| “nurse staffing” [Title/Abstract] OR “nurse workload” [Title/Abstract] OR “nurse workforce” [Title/Abstract] OR “nurse to patient” [Title/Abstract] OR “patient to nurse” [Title/Abstract] OR “nurse to bed” [Title/Abstract] | 2563 |
| Cluster #1 | Cluster #2 | Cluster #3 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TERM | TFICF | TC | CC | TF | ICF | TERM | TFICF | TC | CC | TF | ICF | TERM | TFICF | TC | CC | TF | ICF | ||
| icu | 0.00171 | 652 | 4 | 0.00314 | 0.54407 | mortality | 0.00127 | 591 | 6 | 0.00344 | 0.36798 | staffing level | 0.00225 | 563 | 6 | 0.00611 | 0.36798 | ||
| nursing | 0.00130 | 2575 | 11 | 0.01239 | 0.10474 | patient outcome | 0.00104 | 398 | 5 | 0.00232 | 0.44716 | level | 0.00219 | 830 | 8 | 0.00901 | 0.24304 | ||
| intensive care | 0.00086 | 597 | 7 | 0.00287 | 0.30103 | hospital | 0.00103 | 2654 | 12 | 0.01545 | 0.06695 | nurse staffing level | 0.00171 | 352 | 5 | 0.00382 | 0.44716 | ||
| workforce | 0.00085 | 584 | 7 | 0.00281 | 0.30103 | level | 0.00089 | 627 | 8 | 0.00365 | 0.24304 | nurse staffing | 0.00116 | 1594 | 12 | 0.01730 | 0.06695 | ||
| nursing care | 0.00084 | 582 | 7 | 0.00280 | 0.30103 | patient | 0.00080 | 4249 | 13 | 0.02473 | 0.03218 | staffing | 0.00092 | 2626 | 13 | 0.02850 | 0.03218 | ||
| workload | 0.00075 | 517 | 7 | 0.00249 | 0.30103 | icu | 0.00079 | 250 | 4 | 0.00145 | 0.54407 | patient outcome | 0.00084 | 174 | 5 | 0.00189 | 0.44716 | ||
| intensive care unit | 0.00073 | 413 | 6 | 0.00199 | 0.36798 | fall | 0.00078 | 246 | 4 | 0.00143 | 0.54407 | outcome | 0.00078 | 493 | 10 | 0.00535 | 0.14613 | ||
| care unit | 0.00069 | 479 | 7 | 0.00231 | 0.30103 | outcome | 0.00077 | 902 | 10 | 0.00525 | 0.14613 | relationship | 0.00077 | 237 | 7 | 0.00257 | 0.30103 | ||
| unit | 0.00066 | 942 | 10 | 0.00453 | 0.14613 | nursing | 0.00069 | 1135 | 11 | 0.00661 | 0.10474 | nursing | 0.00076 | 665 | 11 | 0.00722 | 0.10474 | ||
| level | 0.00066 | 562 | 8 | 0.00270 | 0.24304 | rate | 0.00067 | 475 | 8 | 0.00276 | 0.24304 | registered | 0.00065 | 199 | 7 | 0.00216 | 0.30103 | ||
| work | 0.00063 | 679 | 9 | 0.00327 | 0.19189 | surgical | 0.00066 | 252 | 5 | 0.00147 | 0.44716 | hospital | 0.00065 | 889 | 12 | 0.00965 | 0.06695 | ||
| job | 0.00062 | 429 | 7 | 0.00206 | 0.30103 | readmission | 0.00062 | 237 | 5 | 0.00138 | 0.44716 | registered nurse | 0.00064 | 195 | 7 | 0.00212 | 0.30103 | ||
| environment | 0.00061 | 522 | 8 | 0.00251 | 0.24304 | unit | 0.00060 | 700 | 10 | 0.00407 | 0.14613 | california | 0.00063 | 107 | 4 | 0.00116 | 0.54407 | ||
| critical care | 0.00058 | 221 | 4 | 0.00106 | 0.54407 | cost | 0.00056 | 317 | 7 | 0.00184 | 0.30103 | policy | 0.00063 | 157 | 6 | 0.00170 | 0.36798 | ||
| intensive | 0.00057 | 622 | 9 | 0.00299 | 0.19189 | data | 0.00055 | 646 | 10 | 0.00376 | 0.14613 | data | 0.00060 | 377 | 10 | 0.00409 | 0.14613 | ||
| work environment | 0.00056 | 261 | 5 | 0.00126 | 0.44716 | ratio | 0.00054 | 887 | 11 | 0.00516 | 0.10474 | mortality | 0.00059 | 148 | 6 | 0.00161 | 0.36798 | ||
| missed | 0.00056 | 259 | 5 | 0.00125 | 0.44716 | effect | 0.00052 | 298 | 7 | 0.00173 | 0.30103 | cost | 0.00058 | 178 | 7 | 0.00193 | 0.30103 | ||
| turnover | 0.00055 | 211 | 4 | 0.00102 | 0.54407 | ulcer | 0.00052 | 164 | 4 | 0.00095 | 0.54407 | staffing and patient | 0.00053 | 73 | 3 | 0.00079 | 0.66901 | ||
| care | 0.00051 | 3275 | 13 | 0.01576 | 0.03218 | associated | 0.00051 | 600 | 10 | 0.00349 | 0.14613 | effect | 0.00051 | 156 | 7 | 0.00169 | 0.30103 | ||
| quality | 0.00050 | 718 | 10 | 0.00346 | 0.14613 | surgery | 0.00051 | 195 | 5 | 0.00113 | 0.44716 | quality | 0.00050 | 317 | 10 | 0.00344 | 0.14613 | ||
| critical | 0.00049 | 279 | 6 | 0.00134 | 0.36798 | complication | 0.00050 | 158 | 4 | 0.00092 | 0.54407 | nurse staffing and patient | 0.00049 | 68 | 3 | 0.00074 | 0.66901 | ||
| infant | 0.00046 | 175 | 4 | 0.00084 | 0.54407 | workload | 0.00050 | 283 | 7 | 0.00165 | 0.30103 | unit | 0.00048 | 302 | 10 | 0.00328 | 0.14613 | ||
| outcome | 0.00045 | 638 | 10 | 0.00307 | 0.14613 | risk | 0.00047 | 334 | 8 | 0.00194 | 0.24304 | research | 0.00045 | 218 | 9 | 0.00237 | 0.19189 | ||
| job satisfaction | 0.00044 | 169 | 4 | 0.00081 | 0.54407 | pressure ulcer | 0.00047 | 149 | 4 | 0.00087 | 0.54407 | skill mix | 0.00045 | 93 | 5 | 0.00101 | 0.44716 | ||
| data | 0.00043 | 609 | 10 | 0.00293 | 0.14613 | odds | 0.00046 | 214 | 6 | 0.00125 | 0.36798 | association | 0.00043 | 207 | 9 | 0.00225 | 0.19189 | ||
| satisfaction | 0.00042 | 291 | 7 | 0.00140 | 0.30103 | hospital mortality | 0.00045 | 116 | 3 | 0.00068 | 0.66901 | evidence | 0.00043 | 205 | 9 | 0.00223 | 0.19189 | ||
| registered | 0.00042 | 289 | 7 | 0.00139 | 0.30103 | lower | 0.00045 | 257 | 7 | 0.00150 | 0.30103 | safety | 0.00042 | 158 | 8 | 0.00171 | 0.24304 | ||
| mortality | 0.00041 | 234 | 6 | 0.00113 | 0.36798 | staffing level | 0.00044 | 205 | 6 | 0.00119 | 0.36798 | mix | 0.00041 | 126 | 7 | 0.00137 | 0.30103 | ||
| decision | 0.00035 | 163 | 5 | 0.00078 | 0.44716 | patient ratio | 0.00039 | 352 | 9 | 0.00205 | 0.19189 | model | 0.00035 | 169 | 9 | 0.00183 | 0.19189 | ||
| Cluster #4 | Cluster #5 | ||||||||||||||||||
| TERM | TFICF | TC | CC | TF | ICF | TERM | TFICF | TC | CC | TF | ICF | ||||||||
| nursing home | 0.00728 | 647 | 5 | 0.01627 | 0.44716 | school nurse | 0.01518 | 164 | 1 | 0.01324 | 1.14613 | ||||||||
| resident | 0.00433 | 385 | 5 | 0.00968 | 0.44716 | school | 0.00933 | 314 | 6 | 0.02535 | 0.36798 | ||||||||
| home | 0.00418 | 684 | 8 | 0.01720 | 0.24304 | student | 0.00395 | 90 | 4 | 0.00727 | 0.54407 | ||||||||
| nursing | 0.00223 | 845 | 11 | 0.02125 | 0.10474 | school nursing | 0.00305 | 33 | 1 | 0.00266 | 1.14613 | ||||||||
| facility | 0.00154 | 252 | 8 | 0.00634 | 0.24304 | mental | 0.00238 | 66 | 5 | 0.00533 | 0.44716 | ||||||||
| quality | 0.00127 | 345 | 10 | 0.00868 | 0.14613 | school nurse workload | 0.00231 | 25 | 1 | 0.00202 | 1.14613 | ||||||||
| home resident | 0.00116 | 69 | 3 | 0.00174 | 0.66901 | mental health | 0.00206 | 57 | 5 | 0.00460 | 0.44716 | ||||||||
| nursing home resident | 0.00116 | 69 | 3 | 0.00174 | 0.66901 | pmh | 0.00176 | 19 | 1 | 0.00153 | 1.14613 | ||||||||
| medicare | 0.00105 | 77 | 4 | 0.00194 | 0.54407 | health | 0.00169 | 200 | 11 | 0.01615 | 0.10474 | ||||||||
| level | 0.00105 | 171 | 8 | 0.00430 | 0.24304 | workforce | 0.00158 | 65 | 7 | 0.00525 | 0.30103 | ||||||||
| deficiency | 0.00096 | 85 | 5 | 0.00214 | 0.44716 | school health | 0.00157 | 17 | 1 | 0.00137 | 1.14613 | ||||||||
| chain | 0.00094 | 56 | 3 | 0.00141 | 0.66901 | workload | 0.00146 | 60 | 7 | 0.00484 | 0.30103 | ||||||||
| medicaid | 0.00093 | 83 | 5 | 0.00209 | 0.44716 | asthma | 0.00130 | 24 | 3 | 0.00194 | 0.66901 | ||||||||
| nursing facility | 0.00089 | 53 | 3 | 0.00133 | 0.66901 | epinephrine | 0.00111 | 12 | 1 | 0.00097 | 1.14613 | ||||||||
| life care | 0.00087 | 41 | 2 | 0.00103 | 0.84510 | psychiatric mental | 0.00102 | 11 | 1 | 0.00089 | 1.14613 | ||||||||
| registered | 0.00083 | 110 | 7 | 0.00277 | 0.30103 | psychiatric mental health | 0.00102 | 11 | 1 | 0.00089 | 1.14613 | ||||||||
| registered nurse | 0.00081 | 107 | 7 | 0.00269 | 0.30103 | school setting | 0.00102 | 11 | 1 | 0.00089 | 1.14613 | ||||||||
| rating | 0.00076 | 68 | 5 | 0.00171 | 0.44716 | adolescent | 0.00096 | 14 | 2 | 0.00113 | 0.84510 | ||||||||
| star | 0.00072 | 43 | 3 | 0.00108 | 0.66901 | school district | 0.00093 | 10 | 1 | 0.00081 | 1.14613 | ||||||||
| hprd | 0.00072 | 34 | 2 | 0.00086 | 0.84510 | school nurse staffing | 0.00093 | 10 | 1 | 0.00081 | 1.14613 | ||||||||
| staffing level | 0.00069 | 75 | 6 | 0.00189 | 0.36798 | public school | 0.00093 | 10 | 1 | 0.00081 | 1.14613 | ||||||||
| home quality | 0.00066 | 31 | 2 | 0.00078 | 0.84510 | school nurse workforce | 0.00093 | 10 | 1 | 0.00081 | 1.14613 | ||||||||
| nursing home quality | 0.00066 | 31 | 2 | 0.00078 | 0.84510 | anaphylaxis | 0.00093 | 10 | 1 | 0.00081 | 1.14613 | ||||||||
| profit | 0.00062 | 45 | 4 | 0.00113 | 0.54407 | allergy | 0.00093 | 10 | 1 | 0.00081 | 1.14613 | ||||||||
| state | 0.00060 | 125 | 9 | 0.00314 | 0.19189 | hop | 0.00093 | 10 | 1 | 0.00081 | 1.14613 | ||||||||
| case | 0.00058 | 77 | 7 | 0.00194 | 0.30103 | psychiatric | 0.00083 | 23 | 5 | 0.00186 | 0.44716 | ||||||||
| effect | 0.00056 | 74 | 7 | 0.00186 | 0.30103 | policy | 0.00077 | 26 | 6 | 0.00210 | 0.36798 | ||||||||
| relationship | 0.00055 | 73 | 7 | 0.00184 | 0.30103 | academic outcome | 0.00074 | 8 | 1 | 0.00065 | 1.14613 | ||||||||
| life | 0.00045 | 60 | 7 | 0.00151 | 0.30103 | nursing | 0.00068 | 80 | 11 | 0.00646 | 0.10474 | ||||||||
References
- World Health Organization. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- National Quality Forum. National Voluntary Consensus Standards for Nursing-Sensitive Care: An Initial Performance Measure Set; National Quality Forum: Washington, DC, USA, 2004. [Google Scholar]
- Aiken, L.H.; Clarke, S.P.; Sloane, D.M. Hospital Staffing, Organization, and Quality of Care: Cross-National Findings. Nurs. Outlook 2002, 50, 187–194. [Google Scholar] [CrossRef]
- Needleman, J.; Buerhaus, P.; Mattke, S.; Stewart, M.; Zelevinsky, K. Nurse-Staffing Levels and the Quality of Care in Hospitals. N. Engl. J. Med. 2002, 346, 1715–1722. [Google Scholar] [CrossRef]
- Pearson, A.; Pallas, L.O.; Thomson, D.; Doucette, E.; Tucker, D.; Wiechula, R.; Long, L.; Porritt, K.; Jordan, Z. Systematic Review of Evidence on the Impact of Nursing Workload and Staffing on Establishing Healthy Work Environments. Int. J. Evid. Based Healthc. 2006, 4, 337–384. [Google Scholar]
- Kane, R.L.; Shamliyan, T.A.; Mueller, C.; Duval, S.; Wilt, T.J. The Association of Registered Nurse Staffing Levels and Patient Outcomes: Systematic Review and Meta-Analysis. Med. Care 2007, 45, 1195–1204. [Google Scholar] [CrossRef]
- Twigg, D.; McCullough, K. Nurse Retention: A Review of Strategies to Create and Enhance Positive Practice Environments in Clinical Settings. Int. J. Nurs. Stud. 2014, 51, 85–92. [Google Scholar] [CrossRef]
- Griffiths, P.; Ball, J.; Drennan, J.; Dall’Ora, C.; Jones, J.; Maruotti, A.; Pope, C.; Recio Saucedo, A.; Simon, M. Nurse Staffing and Patient Outcomes: Strengths and Limitations of the Evidence to Inform Policy and Practice. A Review and Discussion Paper Based on Evidence Reviewed for the National Institute for Health and Care Excellence Safe Staffing Guideline Development. Int. J. Nurs. Stud. 2016, 63, 213–225. [Google Scholar]
- Bae, S. Intensive Care Nurse Staffing and Nurse Outcomes: A Systematic Review. Nurs. Crit. Care 2021, 26, 457–466. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Saville, C.; Rubbo, B.; Turner, L.; Jones, J.; Griffiths, P. Nurse Staffing Levels and Patient Outcomes: A Systematic Review of Longitudinal Studies. Int. J. Nurs. Stud. 2022, 134, 104311. [Google Scholar] [CrossRef]
- Blume, K.S.; Dietermann, K.; Kirchner-Heklau, U.; Winter, V.; Fleischer, S.; Kreidl, L.M.; Meyer, G.; Schreyögg, J. Staffing Levels and Nursing-Sensitive Patient Outcomes: Umbrella Review and Qualitative Study. Health Serv. Res. 2021, 56, 885–907. [Google Scholar] [CrossRef]
- Spetz, J. California’s Minimum Nurse-to-Patient Ratios: The First Few Months. J. Nurs. Adm. 2004, 34, 571–578. [Google Scholar] [CrossRef]
- Mark, B.A.; Harless, D.W.; Spetz, J.; Reiter, K.L.; Pink, G.H. California’s Minimum Nurse Staffing Legislation: Results from a Natural Experiment. Health Serv. Res. 2013, 48, 435–454. [Google Scholar] [CrossRef]
- The New York State Senate. Assembly Bill A2954 Enacts the “Safe Staffing for Quality Care Act”; The New York State Senate: Albany, NY, USA, 2019.
- Gerdtz, M.F.; Nelson, S. 5-20: A Model of Minimum Nurse-to-Patient Ratios in Victoria, Australia. J. Nurs. Manag. 2007, 15, 64–71. [Google Scholar] [CrossRef]
- McHugh, M.D.; Aiken, L.H.; Sloane, D.M.; Windsor, C.; Douglas, C.; Yates, P. Effects of Nurse-to-Patient Ratio Legislation on Nurse Staffing and Patient Mortality, Readmissions, and Length of Stay: A Prospective Study in a Panel of Hospitals. Lancet 2021, 397, 1905–1913. [Google Scholar] [CrossRef]
- Morioka, N.; Tomio, J.; Seto, T.; Kobayashi, Y. The Association between Higher Nurse Staffing Standards in the Fee Schedules and the Geographic Distribution of Hospital Nurses: A Cross-Sectional Study using Nationwide Administrative Data. BMC Nurs. 2017, 16, 25. [Google Scholar] [CrossRef]
- Shin, S.; Park, J.D.; Shin, J.H. Improvement Plan of Nurse Staffing Standards in Korea. Asian Nurs. Res. 2020, 14, 57–65. [Google Scholar] [CrossRef]
- Ball, J.E.; Griffiths, P. Consensus Development Project (CDP): An Overview of Staffing for Safe and Effective Nursing Care. Nurs. Open 2022, 9, 872–879. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Safe Staffing for Nursing in Adult Inpatient Wards in Acute Hospitals (SG1); National Institute for Health and Care Excellence: London, UK, 2014. [Google Scholar]
- Assaye, A.M.; Wiechula, R.; Schultz, T.J.; Feo, R. Impact of Nurse Staffing on Patient and Nurse Workforce Outcomes in Acute Care Settings in Low- and Middle-Income Countries: A Systematic Review. JBI Evid. Synth. 2021, 19, 751–793. [Google Scholar] [CrossRef]
- Imam, A.; Obiesie, S.; Aluvaala, J.; Maina, J.M.; Gathara, D.; English, M. Identifying Gaps in Global Evidence for Nurse Staffing and Patient Care Outcomes Research in Low/Middle-Income Countries: An Umbrella Review. BMJ Open 2022, 12, e064050. [Google Scholar] [CrossRef]
- Spilsbury, K.; Hewitt, C.; Stirk, L.; Bowman, C. The Relationship between Nurse Staffing and Quality of Care in Nursing Homes: A Systematic Review. Int. J. Nurs. Stud. 2011, 48, 732–750. [Google Scholar] [CrossRef]
- Clemens, S.; Wodchis, W.; McGilton, K.; McGrail, K.; McMahon, M. The Relationship between Quality and Staffing in Long-Term Care: A Systematic Review of the Literature 2008–2020. Int. J. Nurs. Stud. 2021, 122, 104036. [Google Scholar] [CrossRef]
- Royal College of Nursing. Mandatory of Nuse Staffing Levels; Royal College of Nursing: London, UK, 2012. [Google Scholar]
- Murrells, T.; Ball, J.; Maben, J.; Ashworth, M.; Griffiths, P. Nursing Consultations and Control of Diabetes in General Practice: A Retrospective Observational Study. Br. J. Gen. Pract. 2015, 65, 642. [Google Scholar] [CrossRef][Green Version]
- Zengul, F.D.; Oner, N.; Ozaydin, B.; Hall, A.G.; Berner, E.S.; Cimino, J.J.; Lemak, C.H. Mapping 2 Decades of Research in Health Services Research, Health Policy, and Health Economics Journals. Med. Care 2022, 60, 264–272. [Google Scholar] [CrossRef]
- Dong, J.; Wei, W.; Wang, C.; Fu, Y.; Li, Y.; Li, J.; Peng, X. Research Trends and Hotspots in Caregiver Studies: A Bibliometric and Scientometric Analysis of Nursing Journals. J. Adv. Nurs. 2020, 76, 2955–2970. [Google Scholar] [CrossRef]
- Yang, W.; Liu, Y.; Zeng, T.; Wang, Y.; Hao, X.; Yang, W.; Wang, H. Research Focus and Thematic Trends in Magnet Hospital Research: A Bibliometric Analysis of the Global Publications. J. Adv. Nurs. 2021, 77, 2012–2025. [Google Scholar] [CrossRef]
- Chang, C.; Gau, M.; Tang, K.; Hwang, G. Directions of the 100 most Cited Nursing Student Education Research: A Bibliometric and Co-Citation Network Analysis. Nurse Educ. Today 2021, 96, 104645. [Google Scholar] [CrossRef]
- Chiang, H.; Lee, H.; Hung, Y.; Chien, T. Classification and Citation Analysis of the 100 Top-Cited Articles on Nurse Resilience using Chord Diagrams: A Bibliometric Analysis. Medicine 2023, 102, e33191. [Google Scholar] [CrossRef]
- Shekelle, P.G. Nurse-Patient Ratios as a Patient Safety Strategy: A Systematic Review. Ann. Intern. Med. 2013, 158, 404–409. [Google Scholar] [CrossRef]
- Kajikawa, Y.; Ohno, J.; Takeda, Y.; Matsushima, K.; Komiyama, H. Creating an Academic Landscape of Sustainability Science: An Analysis of the Citation Network. Sustain. Sci. 2007, 2, 221–231. [Google Scholar] [CrossRef]
- Newman, M.E.J. Coauthorship Networks and Patterns of Scientific Collaboration. Proc. Natl. Acad. Sci. USA 2004, 101 (Suppl. 1), 5200–5205. [Google Scholar] [CrossRef]
- Fortunato, S. Community Detection in Graphs. Phys. Rep. 2010, 486, 75–174. [Google Scholar] [CrossRef]
- Kajikawa, Y.; Hashimoto, M.; Sakata, I.; Takeda, Y.; Matsushima, K. Academic Landscape of Innovation Research and National Innovation System Policy Reformation in Japan and the United States. Int. J. Innov. Technol. Manag. 2009, 9, 1250044. [Google Scholar]
- Ball, J.E.; Murrells, T.; Rafferty, A.M.; Morrow, E.; Griffiths, P. ‘Care left undone’ during nursing shifts: Associations with workload and perceived quality of care. BMJ Qual. Saf. 2014, 23, 116–125. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sermeus, W.; Van den Heede, K.; Sloane, D.M.; Busse, R.; McKee, M.; Bruyneel, L.; Rafferty, A.M.; Griffiths, P.; Moreno-Casbas, M.T.; et al. Patient safety, satisfaction, and quality of hospital care: Cross-sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ Clin. Res. 2012, 344, e1717. [Google Scholar] [CrossRef]
- Rafferty, A.M.; Clarke, S.P.; Coles, J.; Ball, J.E.; James, P.; McKee, M.; Aiken, L.H. Outcomes of variation in hospital nurse staffing in English hospitals: Cross-sectional analysis of survey data and discharge records. Int. J. Nurs. Stud. 2007, 44, 175–182. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Cimiotti, J.P.; Clarke, S.P.; Flynn, L.; Seago, J.A.; Spetz, J.; Smith, H.L. Implications of the California Nurse Staffing Mandate for Other States. Health Serv. Res. 2010, 45, 904–921. [Google Scholar] [CrossRef]
- Sochalski, J.; Konetzka, R.T.; Zhu, J.; Volpp, K. Will mandated minimum nurse staffing ratios lead to better patient outcomes? Med. Care 2008, 46, 606–613. [Google Scholar] [CrossRef]
- Spetz, J.; Harless, D.W.; Herrera, C.N.; Mark, B.A. Using Minimum Nurse Staffing Regulations to Measure the Relationship between Nursing and Hospital Quality of Care. Med. Care Res. Rev. 2013, 70, 380–399. [Google Scholar] [CrossRef]
- Hyer, K.; Thomas, K.S.; Branch, L.G.; Harman, J.S.; Johnson, C.E.; Weech-Maldonado, R. The influence of nurse staffing levels on quality of care in nursing homes. Gerontologist 2011, 51, 610–616. [Google Scholar] [CrossRef]
- Werner, R.M.; Konetzka, R.T.; Polsky, D. The Effect of Pay-for-Performance in Nursing Homes: Evidence from State Medicaid Programs. Health Serv. Res. 2013, 48, 1393–1414. [Google Scholar] [CrossRef]
- Li, Y.; Cai, X.; Wang, M. Social media ratings of nursing homes associated with the experience of care and “Nursing Home Compare” quality measures. BMC Health Serv. Res. 2019, 19, 260. [Google Scholar] [CrossRef]
- Tetuan, T.M.; Akagi, C.G. The effects of budget, delegation, and other variables on the future of school nursing. J. Sch. Nurs. 2004, 20, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Daughtry, D.; Engelke, M.K. Demonstrating the relationship between school nurse workload and student outcomes. J. Sch. Nurs. 2018, 34, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Best, N.C.; Nichols, A.O.; Waller, A.E.; Zomorodi, M.; Pierre-Louis, B.; Oppewal, S.; Travers, D. Impact of school nurse ratios and health services on selected student health and education outcomes: North Carolina, 2011–2016. J. Sch. Health 2021, 91, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, P.; Saville, C.; Ball, J.E.; Jones, J.; Monks, T.; Safer Nursing Care Tool Study Team. Beyond Ratios—Flexible and Resilient Nurse Staffing Options to Deliver Cost-Effective Hospital Care and Address Staff Shortages: A Simulation and Economic Modelling Study. Int. J. Nurs. Stud. 2021, 117, 103901. [Google Scholar] [CrossRef]
- Ball, J.; Day, T.; Murrells, T.; Dall’Ora, C.; Rafferty, A.M.; Griffiths, P.; Maben, J. Cross-Sectional Examination of the Association between Shift Length and Hospital Nurses Job Satisfaction and Nurse Reported Quality Measures. BMC Nurs. 2017, 16, 26. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Ejebu, O.; Griffiths, P. Because They’re Worth it? A Discussion Paper on the Value of 12-H Shifts for Hospital Nursing. Hum. Resour. Health 2022, 20, 36. [Google Scholar] [CrossRef]
- Griffiths, P.; Saville, C.; Ball, J.; Jones, J.; Pattison, N.; Monks, T.; Safer Nursing Care Study Group. Nursing Workload, Nurse Staffing Methodologies and Tools: A Systematic Scoping Review and Discussion. Int. J. Nurs. Stud. 2020, 103, 103487. [Google Scholar] [CrossRef]
- Griffiths, P.; Saville, C.; Ball, J.; Culliford, D.; Pattison, N.; Monks, T. Performance of the Safer Nursing Care Tool to Measure Nurse Staffing Requirements in Acute Hospitals: A Multicentre Observational Study. BMJ Open 2020, 10, e035828. [Google Scholar] [CrossRef]
- Zhu, R.; Wang, Y.; Wu, R.; Meng, X.; Han, S.; Duan, Z. Trends in High-Impact Papers in Nursing Research Published from 2008 to 2018: A Web of Science-Based Bibliometric Analysis. J. Nurs. Manag. 2020, 28, 1041–1052. [Google Scholar] [CrossRef]
- Sermeus, W.; Aiken, L.H.; Van den Heede, K.; Rafferty, A.M.; Griffiths, P.; Moreno-Casbas, M.T.; Busse, R.; Lindqvist, R.; Scott, A.P.; Bruyneel, L.; et al. Nurse Forecasting in Europe (RN4CAST): Rationale, Design and Methodology. BMC Nurs. 2011, 10, 6. [Google Scholar] [CrossRef]
- European Commission. Final Report Summary—RN4CAST (Nurse Forecasting: Human Resources Planning in Nursing); European Commission: Brussels, Belgium, 2017.
- Lawless, J.; Couch, R.; Griffiths, P.; Burton, C.; Ball, J. Towards Safe Nurse Staffing in England’s National Health Service: Progress and Pitfalls of Policy Evolution. Health Policy 2019, 123, 590–594. [Google Scholar] [CrossRef]
- Lake, E.T. Development of the Practice Environment Scale of the Nursing Work Index. Res. Nurs. Health 2002, 25, 176–188. [Google Scholar] [CrossRef]
- Di Giulio, P.; Clari, M.; Conti, A.; Campagna, S. The Problems in the Interpretation of the Studies on the Relationship between Staffing and Patients’ Outcomes: The Case of the RN4CAST Studies. Assist. Inferm. Ric. 2019, 38, 138–145. [Google Scholar]
- Twigg, D.E.; Whitehead, L.; Doleman, G.; El-Zaemey, S. The Impact of Nurse Staffing Methodologies on Nurse and Patient Outcomes: A Systematic Review. J. Adv. Nurs. 2021, 77, 4599–4611. [Google Scholar] [CrossRef]
- European Commission. Germany: Improving Staffing and Workforce Availability in Healthcare and Long-Term Care; European Commission: Brussels, Belgium, 2018.
- Centers for Medicare & Medicaid Services. Nursing Homes Medicare and Medicaid Programs; Reform of Requirements for Long-Term Care Facilities; Centers for Medicare & Medicaid Services: Baltimore, MD, USA, 2022. [Google Scholar]
- Centers for Medicare & Medicaid Services. Five-Star Quality Rating System; Centers for Medicare & Medicaid Services: Baltimore, MD, USA, 2023. [Google Scholar]
- Moricca, M.L.; Grasska, M.A.; BMarthaler, M.; Morphew, T.; Weismuller, P.C.; Galant, S.P. School Asthma Screening and Case Management: Attendance and Learning Outcomes. J. Sch. Nurs. 2013, 29, 104–112. [Google Scholar] [CrossRef]
- Engelke, M.K.; Swanson, M.; Guttu, M. Process and Outcomes of School Nurse Case Management for Students with Asthma. J. Sch. Nurs. 2014, 30, 196–205. [Google Scholar] [CrossRef]
- Dolatowski, R.; Endsley, P.; Hiltz, C.; Johansen, A.; Maughan, E.; Minchella, L.; Trefry, S. School Nurse Workload—ZStaffing for Safe Care: Position Statement. NASN Sch. Nurse 2015, 30, 290–293. [Google Scholar]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: Strengths and Weaknesses. FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef]
- Belikov, A.V.; Belikov, V.V. A Citation-Based, Author- and Age-Normalized, Logarithmic Index for Evaluation of Individual Researchers Independently of Publication Counts. F1000Res 2015, 4, 884. [Google Scholar] [CrossRef]

| Author | Number of Articles | Affiliation | Country | |
|---|---|---|---|---|
| Linda H. Aiken | 95 | University of Pennsylvania | USA |  |
| Douglas M. Sloane | 51 | University of Pennsylvania | USA |  |
| Peter Griffiths | 44 | University of Southampton | UK |  |
| Matthew D. McHugh | 36 | University of Pennsylvania | USA |  |
| Joanne Spetz | 27 | University of California, San Francisco | USA |  |
| Sean P. Clarke | 27 | McGill University, Quebec | Canada |  |
| Charlene Harrington | 25 | University of California, San Francisco | USA |  |
| Walter Sermeus | 23 | KU Leuven-University of Leuven | Belgium |  |
| Eileen T. Lake | 22 | University of Pennsylvania | USA |  |
| Christine Duffield | 21 | University of Technology Sydney/Edith Cowan University | Australia |  |
| Jeannie P. Cimiotti | 20 | Emory University, Georgia | USA |  |
| Kathleen Rice Simpson | 19 | Mercy Hospital, Missouri | USA |  |
| Barbara A. Mark | 19 | University of North Carolina at Chapel Hill | USA |  |
| Jane Ball | 18 | University of Southampton | UK |  |
| Peter I. Buerhaus | 18 | Montana State University | USA |  |
| Jack Needleman | 18 | University of California, Los Angeles, San Francisco | USA |  |
| Koen Van den Heede | 17 | KU Leuven-University of Leuven | Belgium |  |
| David W. Harless | 16 | Virginia Commonwealth University | USA |  |
| Vincent S. Staggs | 15 | University of Missouri-Kansas City, Missouri | USA |  |
| Luk Bruyneel | 13 | KU Leuven-University of Leuven | Belgium |  |
| Anne Marie Rafferty | 13 | King’s College London | UK |  |
| Journal Title | Number of Articles | Journal Impact Factor in 2021 |
|---|---|---|
| Journal of Nursing Administration | 88 | 1.806 |
| Journal of Nursing Management | 85 | 4.682 |
| International Journal of Nursing Studies | 81 | 6.612 |
| Journal of Advanced Nursing | 52 | 3.057 |
| Nursing Economics | 49 | 1.193 |
| Medical Care | 47 | 3.178 |
| Health Services Research | 45 | 3.734 |
| Journal of Clinical Nursing | 43 | 4.423 |
| Nursing Standard | 43 | no data |
| Journal of Nursing Scholarship | 33 | 3.928 |
| Policy, Politics & Nursing Practice | 33 | no data |
| Journal of Nursing Care Quality | 29 | 1.728 |
| Health Affairs | 29 | 9.048 |
| BMJ Open | 23 | 3.007 |
| International Nursing Review | 23 | 3.384 |
| American Journal of Nursing | 22 | 2.577 |
| MCN: The American Journal of Maternal-Child Nursing | 21 | 1.753 |
| Nursing Research | 19 | 2.364 |
| Nursing Outlook | 19 | 3.315 |
| Nursing Times | 19 | no data |
| Journal of the American Geriatrics Society | 19 | 7.538 |
| Modern Healthcare | 19 | no data |
| Cluster Name | Keywords (TF-ICF) | Examples of Included Papers |
|---|---|---|
| #1 “nurse outcome research in acute care hospital” | ICU (0.00171), workforce (0.00085), nursing care (0.00084), workload (0.00075), work environment (0.00056), missed (0.00056) | [3,37] |
| #2 “patient outcome research in acute care hospitals” | mortality (0.00127), patient outcome (0.00104), hospital (0.00103), patient (0.00080), fall (0.00078), outcome (0.00077) | [4,38,39] |
| #3 “nurse staffing mandate evaluation research” | staffing level (0.00225), patient outcome (0.00084), hospital (0.00065), registered nurse (0.00064), California (0.00063), policy (0.00063) | [40,41,42] |
| #4 “nursing home research” | nursing home (0.00728), resident (0.00433), medicare (0.00105), deficiency (0.00096), Medicaid (0.00093), nursing facility (0.00089) | [43,44,45] |
| #5 “school nurse research” | school nurse (0.01518), school (0.00933), student (0.00395), mental (0.00238), school nurse workload (0.00231), asthma (0.00130) | [46,47,48] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morioka, N.; Ochi, M.; Okubo, S.; Moriwaki, M.; Hayashida, K.; Sakata, I.; Kashiwagi, M. Citation Network Analysis of Nurse Staffing Research from the Past Two Decades: 2000–2022. Healthcare 2023, 11, 3050. https://doi.org/10.3390/healthcare11233050
Morioka N, Ochi M, Okubo S, Moriwaki M, Hayashida K, Sakata I, Kashiwagi M. Citation Network Analysis of Nurse Staffing Research from the Past Two Decades: 2000–2022. Healthcare. 2023; 11(23):3050. https://doi.org/10.3390/healthcare11233050
Chicago/Turabian StyleMorioka, Noriko, Masanao Ochi, Suguru Okubo, Mutsuko Moriwaki, Kenshi Hayashida, Ichiro Sakata, and Masayo Kashiwagi. 2023. "Citation Network Analysis of Nurse Staffing Research from the Past Two Decades: 2000–2022" Healthcare 11, no. 23: 3050. https://doi.org/10.3390/healthcare11233050
APA StyleMorioka, N., Ochi, M., Okubo, S., Moriwaki, M., Hayashida, K., Sakata, I., & Kashiwagi, M. (2023). Citation Network Analysis of Nurse Staffing Research from the Past Two Decades: 2000–2022. Healthcare, 11(23), 3050. https://doi.org/10.3390/healthcare11233050





