Abstract
Introduction: Music is an intriguing but relatively under-researched intervention with many potential benefits for mechanically ventilated patients. The review aimed to assess the impact of listening to music as a non-pharmacological intervention on the physiological, psychological, and social responses of patients in an intensive care unit. Methods: The literature review was conducted in the fourth quarter of 2022. The overview included papers found in Science Direct, EBSCO, PubMed, Ovid, Scopus, and original research papers published in English meeting the PICOS criteria. Articles published between 2010 and 2022 meeting the inclusion criteria were included for further analysis. Results: Music significantly affects vital parameters: decreases the heart rate, blood pressure, and breathing; reduces pain intensity. The analyses confirmed that music affects anxiety levels, reduces sleep disturbances and delirium occurrence, and improves cognitive function. The effectiveness of the intervention is influenced by the choice of music. Conclusions: There is evidence of the beneficial effects of music on a patient’s physiological, psychological, and social responses. Music therapy is highly effective in reducing anxiety and pain and stabilizes physiological parameters, i.e., the heart rate and respiratory rate, after music sessions in mechanically ventilated patients. Studies show that music reduces agitation in confused patients, improves mood, and facilitates communication.
1. Introduction
Music is an intriguing but relatively under-researched intervention with many potential benefits for mechanically ventilated patients in an intensive care unit (ICU) [1]. During the treatment process, patients experience circadian rhythm changes and sleep disturbances and are at a high risk of delirium, an acute brain injury syndrome [2,3]. An intubated patient experiences pain, anxiety and physiological stress, fear of death, changes in the environment, and restriction of movement due to invasive and non-invasive monitoring [4]. The American Music Therapy Association defines music therapy as the use of personalized listening to music as a therapeutic tool by healthcare professionals, which can be conducted by a nurse or a nursing assistant after brief training [3,5,6,7].
Listening to music can be treated as a cheap, non-invasive, non-pharmacological method of reducing anxiety in patients. Music can have an analgesic effect, among others, by increasing the secretion of endorphins, peptide hormones produced in the central nervous system. Endorphins, in addition to relieving pain, also provide a feeling of bliss and euphoria [8,9]. It is used to reduce stress and anxiety and relieve pain, nausea, delirium, and depression [8]. Music can provide a balance between the mind, body, and soul. According to numerous studies, music experiences are effective and practiced as an integrative non-pharmacological intervention to support medicine by ICU nurses [8,9]. Without a doubt, nurses should be equipped with the clinical competences to meet patients’ needs and families’ expectations [10]. Recently, in nursing, music was identified as one of the contextual factors that can positively influence patients’ clinical outcomes by stimulating placebo effects and avoiding nocebo effects. The ideal example of this is when clinical nurses can improve patients’ symptoms and well-being by creating a comfortable environment [11,12,13]. Music can trigger emotional responses that improve the quality of life, but by the same token, music can also induce stress and aggressiveness. The use of complementary intervention improves concentration and also affects neuropsychological aspects, the effectiveness of which depends on individual preferences [14]. Some researchers recommend using original music to avoid the risk of negative emotions in patients and unpleasant memories after discharge from the hospital. Others, mainly in the perioperative period, advocate that providing music familiar to the patient enhances the positive emotional effects induced by listening [9]. The highest health benefits for intensive care patients are seen in the use of classical music. Some research suggests that classical and meditative music activate the left and right hemispheres of the brain. The simultaneous operation of the left and right hemispheres maximizes learning and remembering information. Heavy metal or techno music are not only ineffective but potentially dangerous and can lead to stress and/or life-threatening arrhythmias, especially in ICU patients [14]. Music tracks should have a slow rhythm, 60–80 beats/min., and be in sync with body rhythms; a calm environment should be provided with restricted light or eye mask usage [9]. The available analyses show that the issues of music therapy and medicine in the area of intensive care are still not fully understood. First, it is important to distinguish music therapy from musical intervention as a method of patients listening to music. Secondly, there is still not enough knowledge about how music improves the well-being of patients. Many of the analyzed studies have shown that this non-pharmacological intervention is very often carried out incorrectly. Thirdly, musical interventions for critically ill patients can promote rapid recovery from disease, but the inappropriate use of music can also increase anxiety and depression.
Aim
The review aimed to assess the impact of listening to music as a non-pharmacological intervention on the physiological, psychological, and social responses of patients in an intensive care unit.
2. Methods
2.1. Study Design
The literature review was conducted in the fourth quarter of 2022. This review was prepared on the recommendations of the Prisma 2020 Guidelines for scoping reviews [15,16]. Scoping reviews, a type of knowledge synthesis, follow a systematic approach to map evidence on a topic and identify the main concepts, theories, sources, and knowledge gaps [15].
2.2. Search Methods
The following databases were searched: Science Direct, EBSCO, PubMed, Ovid, and Scopus. The keywords used were “music”, “pain”, “intensive care”, “delirium”, or combinations of these using AND or OR operators. A total of 255 articles matching the primary search criteria were found, 160 of which were included in the further analysis, which included the verification of the availability of full-text versions and their compliance with the inclusion criteria. The last search was conducted on 8 January 2023. Finally, 18 articles published from 2010 to 2022 were submitted for our review. The review and qualification of articles for further analysis were possible after meeting the inclusion criteria.
2.3. Inclusion and Exclusion Criteria
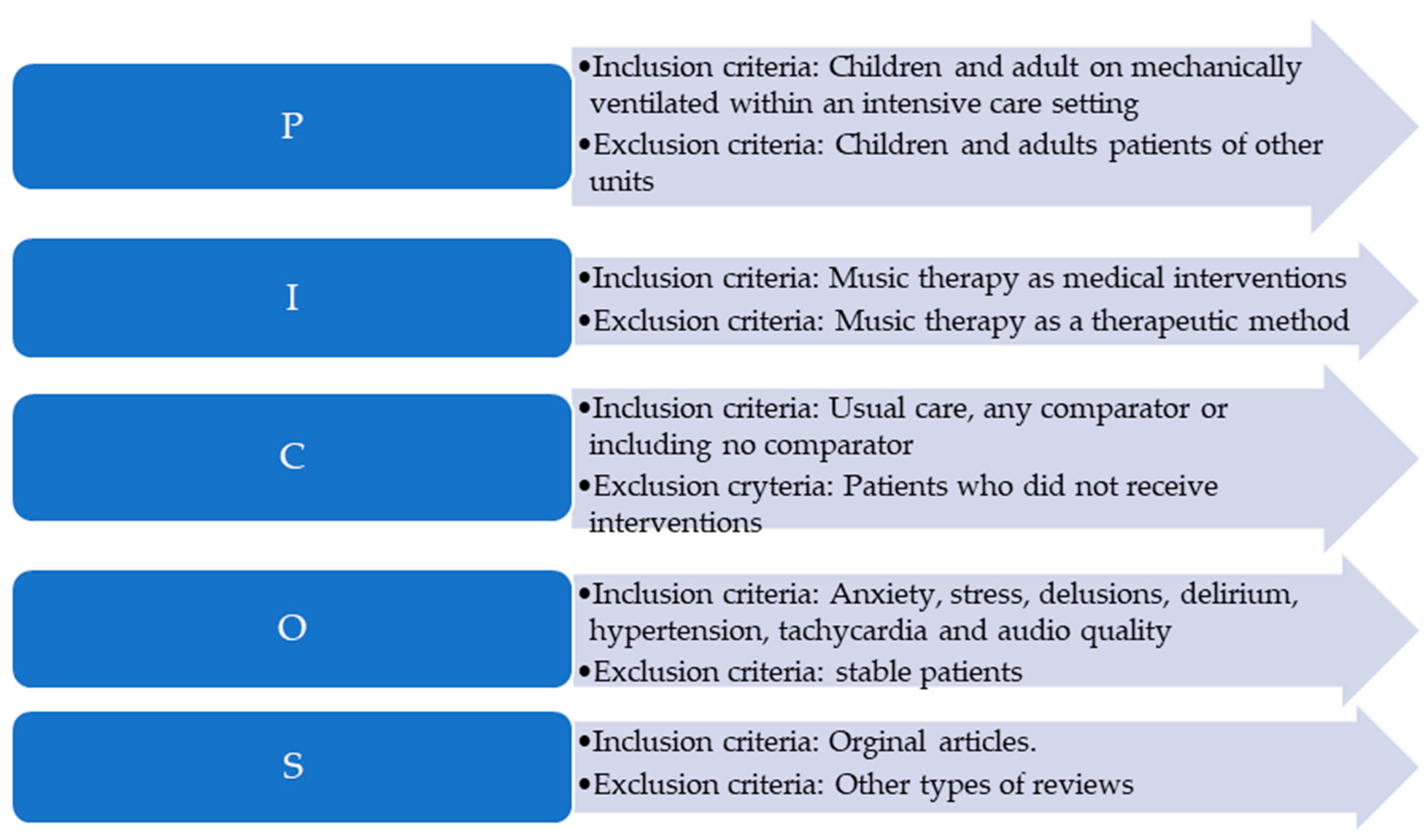
Papers published in English were included in the analysis. The inclusion and exclusion criteria were based on the PICOS classification and are further detailed in Figure 1.
Figure 1.
Inclusion and exclusion criteria (PICOS).
2.4. Data Extraction
Qualified articles meeting the inclusion criteria were analyzed by an independent reviewer with the following criteria: author, date of publication, the aim of the study, sample (study and control group), materials and methods, results, and implications for nursing practice. Finally, 18 qualitative articles meeting the PICOS criteria from two independent searches were included for further analysis.
2.5. Ethical Aspects
The consent of the bioethical commission was not needed to conduct a literature review due to the type of article.
2.6. Assessment of the Study Quality of the Included Studies
The screening of titles and abstracts was completed independently, then in duplicate, by two authors (M.L., D.B.). Any studies appearing to meet the inclusion criteria were retrieved as full-text articles. Two reviewers then read the full-text articles in their entirety to assess for eligibility, with decisions on inclusion and exclusion recorded according to the PICOS classification. Any disagreements were discussed with another reviewer.
In the next step, two reviewers (M.L., D.B.) independently performed quality appraisals using the tool developed by the Joanna Briggs Institute (JBI) [17]. The JBI’s approach to evidence-based healthcare is unique. The methods developed by the JBI were designed to provide authors with a comprehensive guide on how to conduct a systematic review and how to evaluate selected articles (JBI for manual synthesis https://jbi-global-wiki.refined.site/space/MANUAL, 15 December 2022). For this purpose, the JBI Critical Appraisal Checklist was used, which provides a checklist with 11 criteria (Q1–Q11). The questions in the checklist focused on the inclusion criteria of selected articles, the sources and resources of selected material, and what kind of methods were used in the study. The answers used are yes, no, unclear, or not applicable. The results of this evaluation are presented in Table 1. The results of the discussion were used as the final results for the quality appraisal of the included studies.

Table 1.
Critical appraisal results for included studies.
2.7. Data Analysis
The synthesis was carried out and presented graphically and as tables as appropriate. No meta-analysis was carried out.
2.8. Selection of the Source of Evidence
The review process was divided into three phases: 1. searching for relevant manuscripts using the search strategy in different databases; 2. including or excluding articles based on their abstracts and inclusion criteria; 3. checking for article relevance in full-text articles and preparing the literature review.
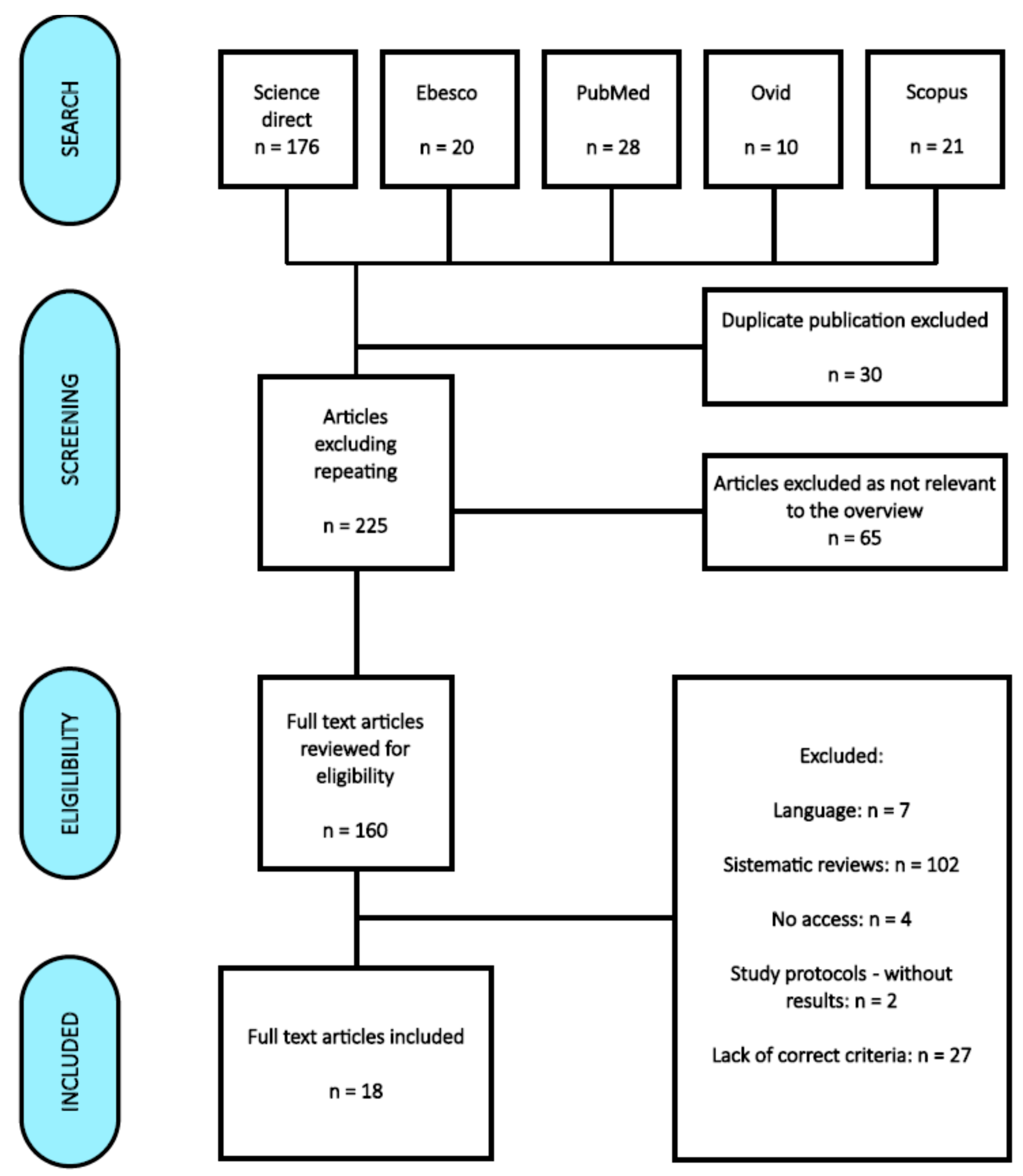
3. Results
A total of 256 publications were initially obtained from the databases: Science Direct—176, EBSCO—20, PubMed—28, Ovid—10, and Scopus—22. After discarding duplicates and selecting titles and abstracts, 128 were excluded. Ultimately, 18 articles were selected for review [3,7,9,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. The results are presented in Figure 2.
Figure 2.
PRISMA flow diagram [8].
Of the 18 included studies, 13 (72.22%) of them were reports of randomized controlled trials or pilot-controlled trials. One paper was a pilot study, and one was a cross-sectional intervention. Other studies were based on the pretest and post-test design. The last study included in the systematic review was a retrospective cohort study.
The literature review was aimed at investigating and presenting the current state of knowledge on supporting the treatment of ICU patients with music based on scientific publications. Table 2 presents a summary of the main results of the review. The last literature review presenting an analysis of articles approximating the topic of music therapy in an ICU was published in 2010 [18]; thus, one of the inclusion criteria was the year of publication. Subsequent studies provide an opportunity to better understand the effect of music on the patient, as its impact is still unrecognized [19,20].

Table 2.
Synthesis of qualitative findings for a literature review in the field of music and medicine.
A detailed synthesis of the qualitative findings is presented in Table 2.
3.1. Demographic Data
Most of the included studies were conducted in the United States of America (n = 9). Other countries mentioned in the included articles were: India, Australia, Taiwan, Switzerland, Columbia, Turkey, China, Iran, and France.
3.2. Characteristics of the Study Population
A total of 1598 participants were included in 18 studies. One study focused on relatives of ICU patients. The mean age of the patient population included in the study was 60 years old. In seven manuscripts, the authors did not provide detailed information about the patient’s age. Scales that were used to assess patient reactions to music intervention were: the Richmond Agitation and Sedation Scale (n = 4), the Likert scale (n = 2), and the Glasgow Coma Scale (n = 3). Other scales were: the Chinese version of the Spielberger State-Trait Anxiety Scale, the Hospital Anxiety and Depression Scale (HADS), the Facial Anxiety Scale, the Critical Care Pain Observation Tool, the Numeric Rating Scale, and the Visual Analog Scale. Six of the eighteen included articles (33.3%) indicated that nursing staff could and should include patients listening to music in their nursing interventions (Table 2).
3.3. Types of Music Therapies
It is important to distinguish between forms of treatment with music because therapeutic music listening is very often confused with music therapy, as these two terms are not the same. “Therapeutic music listening should not be confused with music therapy”. The first form of music used in the form of music therapy can only be conducted by a certified music therapist, while therapeutic music listening is conducted by nurses, among others, through patients listening to music on headphones or volunteers playing live music [21]. Golino et al., 2019, in their publication, present a juxtaposition of the terms music therapy and music listening [3]. Browning et al. and Buzzi et al. point out that therapeutic music listening can be conducted by staff without training since such training in order to play music to patients is not necessary. The authors also found that playing music to patients from a player is far less expensive than using individual headsets for each patient [29,33].
3.4. The Impact of Music on the Physiological, Psychological, and Social Responses of Patients in an Intensive Care Unit
Studies by Golino et al., Seyffert et al., Khan et al., Ettenberger et al., and Johnson K. et al. indicate that music has a significant effect on vital signs and decreases the heart rate, blood pressure, and respiration [3,19,21]. On the other hand, Ettenberger et al., Lee et al., and Johnson et al. confirmed that music can reduce pain and anxiety levels [21,23,24], as well as reduce sleep disturbances [21,25] and have a relaxing effect and regulate breathing [22]. Studies by Dallı et al., Browning et al., and Jawaharani et al. emphasize that music therapy reduces the incidence of delirium [25,29,30], and Yekefallah et al. pointed out that it can improve cognitive function [32]; in addition, it can result in reduced costs of drug treatment [26]. Some studies have shown that music therapy has a positive effect on vital signs, except for diastolic pressure [20,23,31], and can accelerate heart rate [20]. Cousin et al. also proved that music helps young patients (children) communicate better, and all subjects showed improvement in coping with stress during hospitalization [31]. The effectiveness of interventions is influenced by the choice of music [31]. The available analysis also shows that there are studies that do not indicate that music therapy in an ICU has any benefit for patients [27,28].
4. Discussion
The analysis of selected articles made it possible to present the impact of music on the physiological, psychological, and social spheres of life of patients from intensive care units with various ailments, at different ages, with the use of different forms of treatment with the help of music. In everyday life, medical teams strive to improve patient care. Focusing on the patient is of crucial importance in the quality of care, especially since post-ICU symptoms such as anxiety, depression, or post-traumatic stress disorder (PTSD) may occur up to 90 days after an ICU stay [9]. Music therapy is a new therapeutic tool accepted by most patients [34,35]. However, before music therapy is applied, attention should be paid to the available forms of therapy and the possibilities of their implementation in the hospital ward. The analyzed publications indicate that therapeutic music listening is very often confused with music therapy, and these are not the same [3,21]. Only therapeutic music listening can be implemented by nursing personnel [21].
Types and forms of music therapies
Although therapeutic music listening can be used in everyday clinical practice and has beneficial effects for ICU patients of all ages, it is not always used. Various forms of using music were used in the researched original papers. In studies by Cooke et al., Lee et al., and Johnson et al., patients listened to music on headphones connected to a portable CD player or an MP3 player [23,24,27]. Some authors confirmed that music should have a slow tempo and low volume because the processes taking place in the brain during its playback have a calming effect [23]. In addition, Khan et al. used three different forms of supporting the patients’ treatment and showed that slow-tempo music was the best [20].
The choice of musical instruments is also important. Chiasson et al. conducted a music therapy session using a harp played by a professional harpist [28]. In the study by Cousin et al., a certified music therapist used different instruments, including the allophone, ukulele, and kalimba [31]. Playing live music on musical instruments requires the employment of qualified musicians or music therapists, which is associated with additional costs. As noted by Browning et al. and Buzzi et al., 2022, music played on a device by the ward staff does not require training and is a cheaper solution [29,33]. The use of this form of musical intervention also has a positive effect on improving the patients’ vital parameters: patients listening to music with a slow tempo on headphones had an improvement in heart rate and systolic blood pressure [24]. Patient participation in the musical intervention also affects decreases in self-reported pain and respiratory rate [3].
The impact of music on the physiological, psychological, and social responses of patients in an intensive care unit.
Supporting treatment with the use of music applies to patients in various clinical conditions. A specific musical intervention conducted in the study by Buzzi et al. by musicians and music therapists decreased the heart rate in pediatric patients [33]. Music therapy interventions may also reduce anxiety and pain in critically ill children [31].
The results of the collected studies often do not show a statistically significant effect on the improvement of a patient’s condition. The lack of dependence may be due to the small size of the study group. Despite this, some publications showed a positive impact of music on the physiological sphere of patients’ lives by improving vital parameters such as heart rate, respiratory rate, anxiety levels, blood pressure, and pain [3,20,24]. Han L. et al. showed that a music session stabilized vital signs in invasively ventilated patients [18]. One 20–30 min session of musical intervention can relieve pain in patients [36]. According to Cousin et al., music therapy is a method that can be successfully used in an intensive care unit and is accompanied by a high level of recognition not only by the families of patients staying at the ICU but, above all, by the staff working there [31].
The second issue is that there are still unrecognized ways to measure/test a patient’s mental or social sphere. The effects of music on the mental and social spheres have been assessed based on patients’ reported and observed reactions/parameters: better communication, calmness or agitation, coping with stress, and alertness [30,31].
A study by Chahal et al. found that 85% of patients admitted to an ICU experienced anxiety, and similarly, Castillo et al. showed that 82% of patients experienced anxiety, but the music therapy used was highly effective in reducing anxiety and stabilizing physiological parameters among those in the experimental group at post-test compared to the conventional social care group, which received no intervention beyond routine care [37,38]. Han et al. showed that even a single session of music significantly reduced anxiety in patients compared to those who did not receive music [18]. Mechanically ventilated patients who had music played on headphones by nurses had reduced stress and anxiety [23].
Patient participation in guided music therapy reduces pain, lowers elevated vital signs, and speeds up recovery processes after discharge from intensive care. When it comes to music cognition, the current results are particularly relevant to studies on aesthetic preferences, style or genre preferences, and musical choices [39]. The brain activation data revealed that broad limbic and paralimbic regions related to emotion, as well as reward circuits, are significantly more active for familiar music compared to unfamiliar music. Smaller areas in the cingulate cortex and frontal lobe, including the motor cortex and Broca’s area, were found to be more active in response to liked versus disliked music. Therefore, familiarity appears to be a key factor in listeners’ emotional engagement with music, as shown by the fMRI data [40].
Recent research on empathy and aggression from a music therapy perspective highlights the importance of participants’ subjective worldviews when it comes to experiencing empathy. Similarly, the influence of music therapists’ spiritual or religious beliefs on their perception of empathy further complicates the situation, indicating that divergent meanings of empathy can be found not only among healthcare users but also among healthcare professionals [41].
5. Limitations
The study has several limitations. First was the methodological quality of the presented research. All included articles were original studies and met the PICOS inclusion criteria. Unfortunately, after the evaluation process, we can say that there was no standardized tool to measure the effect of music therapy on patients’ well-being. Some researchers used the Glasgow Coma Scale, others the CAM-ICU, CPOT scales, or physiologic parameters. This was the main difficulty in comparing and generalizing the results. Another barrier refers to the intervention used. Some authors used music therapy, while other research projects focused on patient-direct music therapy (PDMT). Music sessions in the articles included in the review process last from 15 to even 60 min, which differs from the American Music Therapy Association recommendations. All patients included in the studies were adults; the study groups of individual components were not differentiated. In some publications, the presence of a control group was indicated. In other observations, the research had a more qualitative nature.
The last limitation was that this review only included studies available in English, and the review could be replicated in other languages for comparison and wider representation.
6. Implications for Nursing Practice
Influencing the patient with music is not an entirely new method in medicine, although, in an intensive care unit setting, this form of influencing the patient is a return to the tenets of holistic medicine, that is, one that combines the work of the body with the work of the mind. Analyses of available studies have confirmed the benefits of therapeutic music listening.
The music played, to bring the best therapeutic benefits, should be a slow tempo with a low volume, not exceeding 65 dB. Many authors confirm that therapeutic music listening can and should be incorporated into nursing interventions as part of non-pharmacological treatments for both pain and delirium. Contrary to appearances, the use of this method does not require specialized, expensive equipment or many nursing staff. All that is required is a short training course, access to a radio, and scheduling a 20–30 min music session that can be repeated four times a day. Nursing staff who would like to incorporate a therapeutic music listening program can refer to the American Music Therapy Association’s detailed rules and guidelines for conducting such activities. The association recommends that during ongoing music sessions, when evaluating the effectiveness of ongoing activities, staff should closely observe patients’ behavior and responses, including the presence of tears, physical responses (movement), verbal expression, eye contact, and changes in breathing or muscle tone. Only by carefully observing and noting changes in the patient’s observation chart will there be a real opportunity to assess the effectiveness of the activities carried out. Undoubtedly, it is worthwhile to deepen the topic of the impact and benefits of using music in the intensive care unit setting, especially since the use of therapeutic music listening as one of the few intervention methods is very well-received by the medical community, but also by the families of patients.
7. Conclusions
Analyses have given evidence of the beneficial effects of music on the physiological, psychological, and social responses of patients. Music therapy is highly effective in reducing anxiety and pain and stabilizing physiological parameters, i.e., the heart rate and the respiratory rate in mechanically ventilated patients. Studies show that music reduces agitation in confused patients, improves mood, and facilitates communication. Conducting music therapy is very well-received not only by staff working in an intensive care unit but also by family members who visit patients.
Author Contributions
Conceptualization, W.M.-D.; methodology, W.M.-D.; analysis, M.L. and D.B.; writing—original draft preparation, M.L., D.B. and W.M.-D.; writing—review and editing, M.L., D.B., K.K.-J. and W.M.-D.; visualization, W.M.-D., K.K.-J. and W.M.-D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable. The article was written as part of the Journal Club Nursing project.
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors declare that the data of this research are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| AMTA | The American Music Therapy Association |
| BP | Blood Pressure |
| CAM-ICU | Confusion Assessment Method in Intensive Care Unit |
| CAM-ICU-7 | Confusion Assessment Method in Intensive Care Unit 7 |
| CG | Control Group |
| CPOT | Critical Care Pain Observation Tool |
| DBP | Diastolic Blood Pressure |
| FAS | Facial Anxiety Scale |
| GCS | Glasgow Coma Scale |
| HADS | Hospital Anxiety and Depression Scale |
| HR | Heart Rate |
| HT | Head Trauma |
| ICU | Intensive Care Unit |
| LOC | Level of Consciousness |
| MAR | Music-Assisted Relaxation |
| MT | Music Therapy |
| NIV | Non-invasive ventilation |
| NRS | Numeric Rating Scale |
| PDM | Patient-Directed Music |
| PDMI | Patient-Directed Music Intervention |
| PDMT | Patient-Direct Music Therapy |
| PHQ-9 | Patient Health Questionnaire-9 |
| PTSD | The Post-Traumatic Stress Disorder |
| RASS | Richmond Agitation-Sedation Scale |
| SBP | Systolic Blood Pressure |
| VAS | Visual Analogue Scale |
References
- Gullick, J.G.; Kwan, X.X. Patient-directed music therapy reduces anxiety and sedation exposure in mechanically-ventilated patients: A research critique. Aust. Crit. Care 2015, 28, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Chahal, J.K.; Sharma, P.; Sulena Rawat, H.C.L. Effect of music therapy on ICU induced anxiety and physiological parameters among ICU patients: An experimental study in a tertiary care hospital in India. Clin. Epidemiol. Glob. Health 2021, 11, 10071. [Google Scholar] [CrossRef]
- Golino, A.J.; Leone, R.; Gollenberg, A.; Christopher, C.; Stanger, D.; Davis, T.M.; Anthony Meadows, A.; Zhang, Z.; Friesen, M.A. Impact of an Active Music Therapy Intervention on Intensive Care Patients. Am. J. Crit. Care 2019, 28, 48–55. [Google Scholar] [CrossRef] [PubMed]
- DellaVolpe, J.D.; Huang, D.T. Is there a role for music in the ICU? Crit. Care 2015, 19, 17. [Google Scholar] [CrossRef]
- AMTA. About Music Therapy. Available online: https://www.musictherapy.org/about/musictherapy/ (accessed on 2 March 2023).
- Manchaster Music School. What Is Music Therapy? Available online: https://mcmusicschool.org/what-is-music-therapy/ (accessed on 2 March 2023).
- Heiderscheit, A.; Johnson, K.; Chlan, L.L. Analysis of Preferred Music of Mechanically Ventilated Intensive Care Unit Patients Enrolled in a Randomized Controlled Trial. J. Integr. Complement Med. 2022, 28, 517–529. [Google Scholar] [CrossRef]
- Wilkins, M.K.; Moore, M.L. Music intervention in the intensive care unit: A complementary therapy to improve patient outcomes. Evid.-Based Nurs. 2004, 7, 103–104. [Google Scholar] [CrossRef]
- Messika, J.; Kalfon, P.; Ricard, J.D. Adjuvant therapies in critical care: Music therapy. Intensive Care Med. 2018, 44, 1929–1931. [Google Scholar] [CrossRef]
- Palese, A.; Cadorin, L.; Testa, M.; Geri, T.; Colloca, L.; Rossettini, G. Contextual factors triggering placebo and nocebo effects in nursing practice: Findings from a national cross-sectional study. J. Clin. Nurs. 2019, 28, 1966–1978. [Google Scholar] [CrossRef]
- Edwards, R.R.; Dworkin, R.H.; Turk, D.C.; Angst, M.S.; Dionne, R.; Freeman, R.; Hansson, P.; Haroutounian, S.; Arendt-Nielsen, L.; Attal, N.; et al. Patient phenotyping in clinical trials of chronic pain treatments: IMMPACT recommendations. Pain Rep. 2021, 6, e896. [Google Scholar] [CrossRef]
- Palese, A.; Ambrosi, E.; Stefani, F.; Zenere, B.A.; Saiani, L. The activities/tasks performed by health care aids in hospital settings: A mixed-methods study. Assist. Inferm. Ric. 2019, 38, 6–14. [Google Scholar] [CrossRef]
- Palese, A.; Longhini, J.; Danielis, M. To what extent Unfinished Nursing Care tools coincide with the discrete elements of The Fundamentals of Care Framework? A comparative analysis based on a systematic review. J. Clin. Nurs. 2021, 30, 239–265. [Google Scholar] [CrossRef]
- Trappe, H.J. Role of music in intensive care medicine. Int. J. Crit. Illn. Inj. Sci. 2012, 2, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- PRISMA. PRISMA-ScR-Fillable-Checklist. Available online: http://www.prisma-statement.org/documents/PRISMA-ScR-Fillable-Checklist_11Sept2019.pdf (accessed on 17 March 2023).
- Aromataris, E.; Fernandez, R.; Godfrey, C.; Holly, C.; Khalil, H.; Tungpunkom, P. The Joanna Briggs Institute Reviewers’ Manual 2014 Methodology for JBI Umbrella Reviews; The Joanna Briggs Institute: Adelaide, Australia, 2014. [Google Scholar]
- Han, L.; Li, J.P.; Sit, J.W.; Chung, L.; Jiao, Z.Y.; Ma, W.G. Effects of music intervention on physiological stress response and anxiety level of mechanically ventilated patients in China: A randomised controlled trial. J. Clin. Nurs. 2010, 19, 978–987. [Google Scholar] [CrossRef] [PubMed]
- Seyffert, S.; Moiz, S.; Coghlan, M.; Balozian, P.; Nasser, J.; Rached, E.A.; Jamil, Y.; Naqvi, K.; Rawlings, L.; Perkins, A.J.; et al. Decreasing delirium through music listening (DDM) in critically ill, mechanically ventilated older adults in the intensive care unit: A two-arm, parallel-group, randomized clinical trial. Trials 2022, 23, 576. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.H.; Xu, C.; Purpura, R.; Durrani, S.; Lindroth, H.; Wang, S.; Gao, S.; Heiderscheit, A.; Chlan, L.; Boustani, M.; et al. Decreasing Delirium through Music: A Randomized Pilot Trial. Am. J. Crit. Care 2020, 29, e31–e38. [Google Scholar] [CrossRef] [PubMed]
- Ettenberger, M.; Maya, R.; Salgado-Vasco, A.; Monsalve-Duarte, S.; Betancourt-Zapata, W.; Suarez-Cañon, N.; Prieto-Garces, S.; Marín-Sánchez, J.; Gómez-Ortega, V.; Valderrama, M. The Effect of Music Therapy on Perceived Pain, Mental Health, Vital Signs, and Medication Usage of Burn Patients Hospitalized in the Intensive Care Unit: A Randomized Controlled Feasibility Study Protocol. Front. Psychiatry 2021, 12, 714209. [Google Scholar] [CrossRef] [PubMed]
- Ames, N.; Shuford, R.; Yang, L.; Moriyama, B.; Frey, M.; Wilson, F.; Sundaramurthi, T.; Gori, D.; Mannes, A.; Ranucci, A.; et al. Music Listening Among Postoperative Patients in the Intensive Care Unit: A Randomized Controlled Trial with Mixed-Methods Analysis. Integr. Med. Insights 2017, 12, 1178633717716455. [Google Scholar] [CrossRef]
- Lee, C.H.; Lee, C.Y.; Hsu, M.Y.; Lai, C.L.; Sung, Y.H.; Lin, C.Y.; Lin, L.Y. Effects of Music Intervention on State Anxiety and Physiological Indices in Patients Undergoing Mechanical Ventilation in the Intensive Care Unit. Biol. Res. Nurs. 2017, 19, 137–144. [Google Scholar] [CrossRef]
- Johnson, K.; Fleury, J.; McClain, D. Music intervention to prevent delirium among older patients admitted to a trauma intensive care unit and a trauma orthopaedic unit. Intensive Crit. Care Nurs. 2018, 47, 7–14. [Google Scholar] [CrossRef]
- Dallı, Ö.E.; Yıldırım, Y.; Aykar, F.Ş.; Kahveci, F. The effect of music on delirium, pain, sedation and anxiety in patients receiving mechanical ventilation in the intensive care unit. Intensive Crit. Care Nurs. 2022, 2, 103348. [Google Scholar] [CrossRef] [PubMed]
- Chlan, L.L.; Heiderscheit, A.; Skaar, D.J.; Neidecker, M.V. Economic Evaluation of a Patient-Directed Music Intervention for ICU Patients Receiving Mechanical Ventilatory Support. Crit. Care Med. 2018, 46, 1430–1435. [Google Scholar] [CrossRef] [PubMed]
- Cooke, M.; Chaboyer, W.; Schluter, P.; Foster, M.; Harris, D.; Teakle, R. The effect of music on discomfort experienced by intensive care unit patients during turning: A randomized cross-over study. Int. J. Nurs. Pract. 2010, 16, 125–131. [Google Scholar] [CrossRef]
- Chiasson, A.; Linda Baldwin, A.; McLaughlin, C.; Cook, P.; Sethi, G. The effect of live spontaneous harp music on patients in the intensive care unit. Evid. Based Complement Altern. Med. 2013, 2013, 428731. [Google Scholar] [CrossRef] [PubMed]
- Browning, S.G.; Watters, R.; Thomson-Smith, C. Impact of Therapeutic Music Listening on Intensive Care Unit Patients: A Pilot Study. Nurs. Clin. N. Am. 2020, 55, 557–569. [Google Scholar] [CrossRef]
- Jawaharani, A.; Acharya, S.; Kumar, S.; Gadegone, A.; Raisinghani, N. The effect of music therapy in critically ill patients admitted to the intensive care unit of a tertiary care center. J. Datta Meghe Inst. Med. Sci. Univ. 2019, 14, 320–325. [Google Scholar] [CrossRef]
- Cousin, V.L.; Colau, H.; Barcos-Munoz, F.; Rimensberger, P.C.; Polito, A. Parents’ Views with Music Therapy in the Pediatric Intensive Care Unit: A Retrospective Cohort Study. Children 2022, 9, 958. [Google Scholar] [CrossRef]
- Yekefallah, L.; Namdar, P.; Azimian, J.; Dost Mohammadi, S.; Mafi, M. The effects of musical stimulation on the level of consciousness among patients with head trauma hospitalized in intensive care units: A randomized control trial. Complement Ther. Clin. Pract. 2021, 42, 101258. [Google Scholar] [CrossRef]
- Buzzi, F.; Yahya, N.B.; Gambazza, S.; Binda, F.; Galazzi, A.; Ferrari, A.; Crespan, S.; Al-Atroushy, H.A.; Cantoni, B.M.; Laquintana, D.; et al. Use of Musical Intervention in the Pediatric Intensive Care Unit of a Developing Country: A Pilot Pre–Post Study. Children 2022, 9, 455. [Google Scholar] [CrossRef]
- Li, D.; Yao, Y.; Chen, J.; Xiong, G. The effect of music therapy on the anxiety, depression and sleep quality in intensive care unit patients: A protocol for systematic review and meta-analysis. Medicine 2022, 101, e28846. [Google Scholar] [CrossRef]
- Liu, K.; Wang, J.; Ma, Z.; Chen, B.; Wang, L.; Gong, J.; Wang, R. Non-pharmacological Treatment of Intensive Care Unit Delirium. Am. J. Nurs. Sci. 2019, 8, 119–128. [Google Scholar] [CrossRef]
- Chen, Y.-F.; Chang, M.-Y.; Chow, L.-H.; Ma, W.-F. Effectiveness of Music-Based Intervention in Improving Uncomfortable Symptoms in ICU Patients: An Umbrella Review. Int. J. Environ. Res. Public Health 2021, 18, 11500. [Google Scholar] [CrossRef] [PubMed]
- Uyar, M.; Akın Korhan, E. The effect of music therapy on pain and anxiety in intensive care patients. Agri 2011, 23, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Castillo, M.I.; Cooke, M.; Macfarlane, B.; Aitken, L.M. Factors associated with anxiety in critically ill patients: A prospective observational cohort study. Int. J. Nurs. Stud. 2016, 60, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, T.; Sedlmeier, P.; Städtler, C.; Huron, D. The psychological functions of music listening. Front. Psychol. 2013, 4, 511. [Google Scholar] [CrossRef]
- Pereira, C.S.; Teixeira, J.; Figueiredo, P.; Xavier, J.; Castro, S.L.; Brattico, E. Music and emotions in the brain: Familiarity matters. PLoS ONE 2011, 6, e27241. [Google Scholar] [CrossRef]
- Ettenberger, M.; Calderón Cifuentes, N.P. Intersections of the arts and art therapies in the humanization of care in hospitals: Experiences from the music therapy service of the University Hospital Fundación Santa Fe de Bogotá, Colombia. Front. Public Health 2022, 10, 1020116. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).