Abstract
Gait trainers are walking devices that provide additional trunk and pelvic support. The primary population of children using gait trainers includes children with cerebral palsy (CP) functioning at Gross Motor Function Classification System (GMFCS) levels IV and V. A recent systematic review found that evidence supporting the effectiveness of gait trainer interventions for children was primarily descriptive and insufficient to draw firm conclusions. A major limitation identified was the lack of valid, sensitive and reliable tools for measuring change in body structure and function, activity and participation outcomes. Twelve different clinical tools were identified in the systematic review and in this paper we review and discuss the evidence supporting their reliability, validity and clinical utility for use with children using gait trainers. We also describe seven additional clinical measurement tools that may be useful with this intervention and population. The Pediatric Evaluation of Disability Inventory (PEDI) rated highest across all areas at this time. Individualized outcome measures, such as the Canadian Occupational Performance Measure (COPM) and Goal Attainment Scaling and measuring user satisfaction with tools, such as the Quebec User Evaluation of Satisfaction with assistive Technology, show potential for gait trainer outcomes research. Spatiotemporal measures appear to be less useful than functional measures with this intervention and population. All tools would benefit from further development for use with children with CP functioning at GMFCS levels IV and V.
1. Introduction
Cerebral Palsy (CP) is the most prevalent diagnosis for children with significant motor impairments who are followed by physical and occupational therapists [1]. This diagnosis results in lifelong progressive deforming secondary sequellae, most likely as a direct result of immobility. One of the newest revealed pressing issues is that change in muscle physiology including the loss of stem (satellite) cells and increase in collagen and muscle stiffness may be a result of non-use [2].
The Gross Motor Function Classification System (GMFCS) [3] classifies children with CP according to their mobility level and need for assistive devices. Children classified as GMFCS levels IV and V are unable to walk with hand-held walkers due to lack of trunk/postural control, strength, range of motion (ROM) and balance. These children require more supportive walkers that provide additional trunk and pelvic support, as well as unweighting. These types of walkers are often referred to as gait trainers, but the term support walker is also found in the literature [4]. Following onset of independent ambulation, children at GMFCS levels I–III are unlikely to use gait trainers except for activities that are enhanced by a device that is hands-free and/or offers increased postural support with or without body weight support. The use of a gait trainer may be one methodology to increase activity and muscle use and thus decrease contracture and disuse weakness for children at GMFCS levels IV and V.
A recent systematic review of outcomes of gait trainer use in children [5] identified mainly descriptive evidence supporting a positive impact on walking distance, mobility level and ability to take steps. Some studies suggested a positive impact on bone mineral density and bowel function along with a variety of activity and participation outcomes, but overall the evidence was low level and strong conclusions could not be reached. This review identified a limited number of clinical measurement tools that have been used to evaluate impact of gait trainer interventions for children. The review suggests that lack of reliable sensitive outcome measures may be a factor contributing to lack of stronger intervention research in this area. However, outcome measurement was not the focus of this previous paper and no critical appraisal of the tools was conducted.
The purpose of this review is to summarize the clinical measurement tools available to assess outcomes relevant to children with CP who are functioning at GMFCS IV and V as these are primarily the population of children who are using gait trainers; to critically appraise the psychometric properties of these tools and to identify which International Classification of Functioning, Disability and Health (ICF) [6,7] domains they address. We defined a gait trainer as a walker that provides additional trunk and pelvic support and is designed to be used in typical home or school settings. Our specific clinical question was “For children aged 18 years or younger, with CP, what clinical measurement tools have been used to assess gait trainer outcomes; what additional clinical measurement tools may be appropriate for this intervention and population; what are their psychometric properties; and which ICF domains do they address?”
2. Materials and Methods
We built on the search that was completed for the systematic review [5] and updated it in January 2016. Databases included CINAHL; Medline; EMBASE; and EBM Reviews. Search terms included “gait trainer”, “supported walking”, “support walker”, “walking device”, “body weight support gait trainer”, “walker”, “supported ambulation” and “David Hart Walker”. Articles from the systematic review [5] were included if they provided a description of the clinical tools used and information on reliability, validity and/or clinical utility. We defined a clinical tool as one that could be used by a physical or occupational therapist in a family home or community, school or typical therapeutic setting. We specifically searched for tools that could be used for evaluative purposes rather than those designed to classify level of disability or discriminate between children with and without disabilities or delays. Outcome measures that require specialized medical or hospital-based equipment and are not able to be completed in a typical clinical environment were excluded, e.g., X-ray, bone mineral density scans, specialized gait analysis, etc. We included questionnaire-type assessments describing typical performance and designed to be completed by child or parent-proxy report. Capacity assessments completed by professional observation could include observation of physical abilities in real time or reviewing later via video-taping. Tempero-spatial measures could include use of a measuring tape or wheel, and stop-watch or video-camera, but would exclude specialized gait analysis that would require a gait lab setting or specialized camera or computer technology to complete. We excluded studies that did not provide detail on the clinical measurement tools or information on their psychometric properties.
In order to identify additional tools that might be appropriate for use with children with CP who use gait trainers, the search was expanded to include non-peer reviewed articles and conference proceeding submissions regarding children using gait trainers. We also searched for intervention studies involving other types of mobility interventions for children classified as GMFCS level IV and/or V and clinical tool development articles including children classified as GMFCS level IV and/or V. Search terms included “cerebral palsy” and “gait” or “walk* (* includes other word endings e.g. walker, walking, etc.)” in combination with terms such as “measure”, “tool” or “assess* (* includes other word endings such as assessment or assessed)”. We also hand searched for further articles including each of the tools identified in the electronic search by searching for them by name. We contacted known researchers and presenters on this topic in case there were other studies on these tools.
Knowing that a limited number of clinical tools have been used with gait trainer interventions, we also hand searched the reference lists of several systematic reviews of mobility and other motor interventions for children classified as GMFCS IV and V for potentially relevant tools. We purposely selected reviews of interventions that we considered to be commonly used by community-based therapists with our selected population, and that had some characteristics related to use of gait trainers. These included power mobility, adaptive seating, as well as supported walking and movement interventions that did not meet the inclusion criteria for the gait trainer systematic review [5], such as treadmill training or larger institutional or powered walking devices. We did not include reviews of general therapy interventions (e.g., Neurodevelopmental Therapy, Constraint induced movement therapy, Intensive motor therapies, etc.) or reviews of hippotherapy or aquatic therapy.
Reviews selected for hand-searching of reference lists were identified through the electronic search process using the search terms “cerebral palsy”, “power mobility”, “motor intervention”, “treadmill training”, “adaptive seating”, “participation” and “review”. All electronic searches were completed using the databases listed above. Any reviews identified in the electronic search were read full text to determine if they provided information on the clinical tools used in their included studies. If the studies included additional tools that had not previously been identified as having been used with gait trainer interventions, the individual articles were then read full-text.
The reviews selected from this process included seating interventions [8], power mobility interventions [9], motor interventions [10], and treadmill training [11], as well as reviews of measurement tools suitable for children with CP [12], children using seating interventions [13], and children using power mobility [14]. The additional tools were only included based on agreement of the two reviewers if at least one study evidencing psychometric properties of these clinical tools and their use in measuring intervention outcomes with children with CP classified as GMFCS level IV or V was identified.
Data on included tools were extracted independently from identified articles by reviewers using the McMaster Outcome Measures Rating Form [15]. This tool was used to rate reliability and validity results as well as to provide information on clinical utility of the tools and to provide an overall utility rating. The McMaster Outcome Measures Rating Form provides a standardized form for recording the reliability, validity, responsiveness and clinical utility of tools. It also provides a means of recording ICF domains. Ratings of excellent, adequate and poor take into account the conduct of the studies as well as the psychometric results. Individual reliability coefficients are considered excellent if above 0.8, adequate at 0.6–0.79 and poor if less than 0.6.
Tools are considered to have excellent reliability if supported by more than 2 well-designed studies with adequate to excellent reliability values; adequate reliability if supported by 1–2 well-designed studies with adequate to excellent reliability ratings; and poor reliability if only supported by poorly designed studies or poor reliability ratings. Similarly, validity would be rated excellent if supported by more than two well-designed studies supporting the measure’s validity, adequate if supported by 1–2 well-designed studies and poor if the studies were poorly completed or did not support the measure’s validity. Responsiveness would be rated as excellent if more than two well-designed studies showed strong hypothesized relationships between changes on the measure and other measures of change on the same attribute; adequate if supported by 1–2 well-designed studies and poor if the studies were poorly completed or did not support the measures responsiveness. Clinical tools were rated adequate or excellent if these psychometric properties had been demonstrated with children functioning at GMFCS levels IV and/or V. Overall ratings also take into account clinical utility with this population.
3. Results
Eleven of the original 17 articles identified in the previous systematic review of gait trainer outcomes [5] were included in this new review specific to outcome measurement [16,17,18,19,20,21,22,23,24,25]. These articles described 12 different clinical measurement tools that have been used in gait trainer outcomes research with children functioning at GMFCS levels IV and V and provided information on the tools psychometric properties and clinical utility.
The tools include the 10-meter (10-m) walk test [26,27], 10-minute (10-min) walk test [27], Directional Mobility Assessment (DMA) [24,25], Gross Motor Function Measure (GMFM) [28], Pediatric Evaluation of Disability Inventory (PEDI) [29], Physical Abilities and Mobility Scale (PAMS) [30], School Function Assessment (SFA)—Travel subscale [31], Step/leg movement count [16,20,21,32], Step length and velocity footprint analysis [24,25], Top Down Motor Milestone Test (TDMMT) [33], Videoing indices of happiness [19,21], and the Functional Independence Measure for children (Wee FIM) [34,35].
In the expanded search, methodological studies providing further information on the Top Down Motor Milestone Test [33,36], use of the 10-m walk test with children with CP GMFCS levels I–III [37,38], and the PAMS [39] were identified. Only one gait trainer intervention study not included in the systematic review was identified [40]. It used the WeeFIM mobility scale [34,35] to discriminate between mobility function with and without a specialized gait trainer and orthotic device.
In the expanded search seven other clinical tools that have been used in mobility-related interventions with children with CP and appeared relevant to review regarding potential for use in gait trainer outcomes research were identified and agreed by two reviewers. All articles and tools were identified through the expanded electronic search and the hand search of the reference lists in the previously identified systematic reviews. These include: 6-min walk test [41]; Canadian Occupational Performance Measure (COPM) [42]; Early Activity Scale for Endurance (EASE) [43]; Goal Attainment Scaling (GAS) [44]; Matching Assistive Technology and Child (MATCH) [45]; Quebec User Evaluation of Satisfaction with assistive Technology 2.0 (QUEST 2.0) [46]; and the Supported Walker Ambulation Performance Scale (SWAPS) [47]. Figure 1 shows a flow diagram of the search.
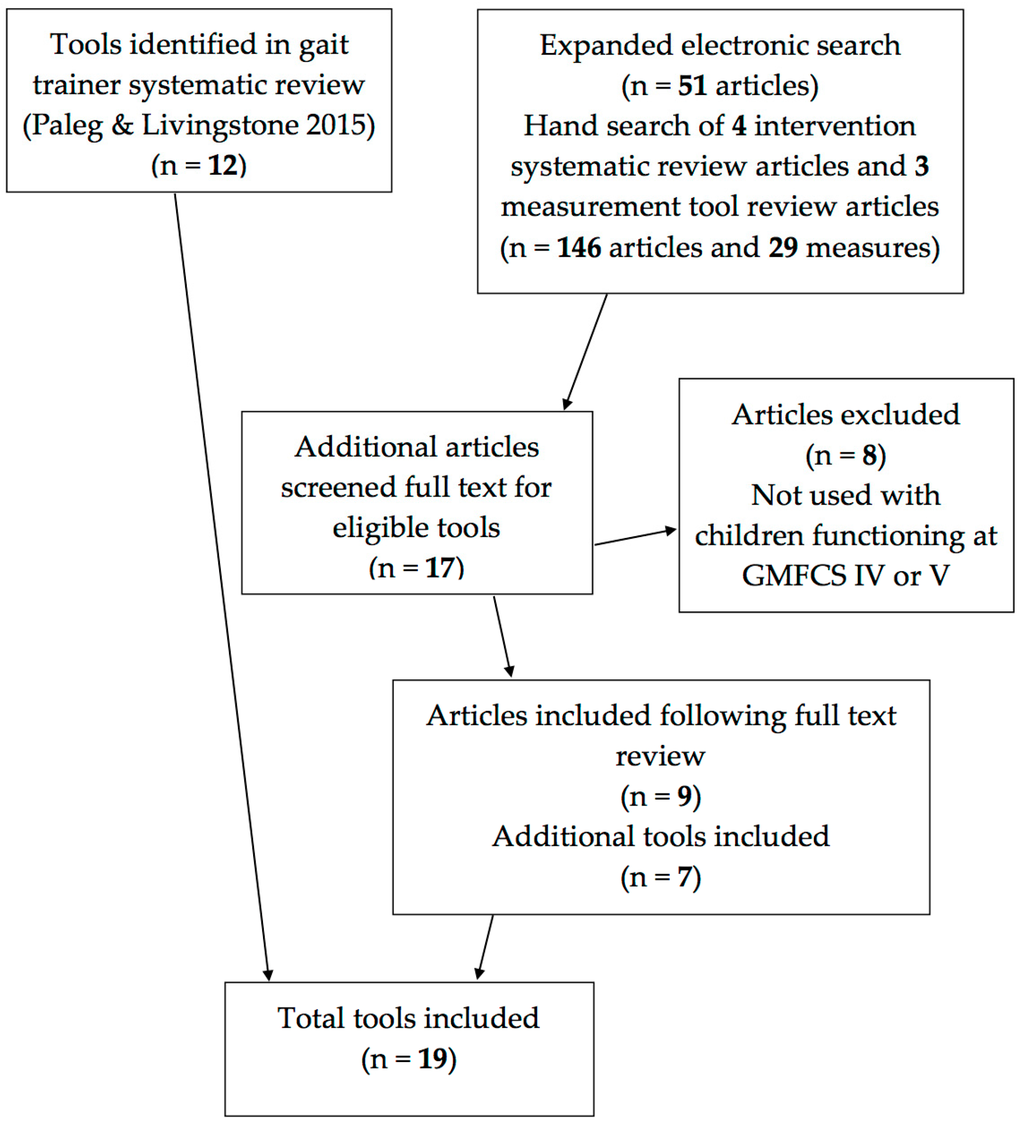
Figure 1.
Flow chart of the search.
3.1. Tool Identification
3.2. Tool Characteristics
Table 1 provides a summary of the measurement properties of the clinical tools included in this review. Readers are directed to the published systematic review [5] for evaluation of the evidence provided in the gait trainer intervention studies. A number of the included tools merited poor McMaster Outcome Measure [15] ratings, as psychometric properties have not been established for children with CP functioning at GMFCS levels IV and V.

Table 1.
Psychometric properties.
See Appendix A for a brief summary of the six intervention and three methodological or tool development studies providing information on additional clinical tools that have been used with children functioning at GMFCS levels IV and/or V and may have utility for evaluating outcomes of gait trainer interventions.
3.3. Reliability
Studies that measured step or leg movement counts, or indices of happiness [16,19,20,21,32] all reported excellent inter-rater reliability with % agreement ranging from 90%–100%. Timed walking tests such as the 10-m walk test have excellent test-retest reliability [26,70] and acceptable inter-rater reliability [70] in adults with neurological impairments. However, the reliability of the three included spatiotemporal tests (10-m walk test [26,27]; 10 min-walk test [27]; 6-min walk test [41]) has not been confirmed for children functioning at GMFCS levels IV or V.
Functional measures, such as the PEDI [29] and GMFM [28], are reported to have excellent inter, intra and test-retest reliability with children with CP, but evaluation of all the articles published on these widely known measures is beyond the scope of this paper. The COPM [42] was rated as having adequate reliability due to the limited number of studies relevant to the specific population being considered in this paper whereas GAS [44] is reported to have excellent reliability with children at all GMFCS levels.
3.4. Validity
Face and content validity is evident for most of the included measures but only the most relevant examples are listed in the table in the interests of space. Some measures used factor analysis (e.g., SFA [31]) while others (e.g., SWAPS [47]) were developed through expert consensus. The SWAPS [47] and DMA [24,25] demonstrate construct (convergent) validity with a moderate correlation with the GMFM [28]. The PAMS [30,39] demonstrates moderate to strong correlation with the WeeFIM [34,35]. Discriminative validity is demonstrated by some measures (e.g., EASE [43]) being able to discriminate between GMFCS levels [43] and others (e.g., WeeFIM [34,35]) being able to discriminate between mobility levels with and without a specific mobility device [40]. However, this does not indicate that a measure is suitable for evaluative purposes with this population.
3.5. Responsiveness and Sensitivity to Change
Limited information was available for the majority of tools identified. Responsiveness indicates that a measure is able to detect clinically meaningful change and sensitivity or the ability to detect any change is an important first step. Although the GMFM [28] is reported to have good responsiveness to change in children with CP regardless of GMFCS level, many of the items cannot be completed by children using gait trainers and therefore it is limited in its utility for assessing change related to gait trainer interventions. The PEDI [29] has been found to be sensitive to change in children with CP and a scaled score change of 11 points is thought to represent a clinically important change in an inpatient population [71]. The COPM [42] has been shown to be sensitive to change in children with mild CP (GMFCS I and II equivalent) although parents have rated a significant increase in independence in children with severe CP (GMFCS IV and V equivalent) using power mobility [61].
The 10-m walk test [26,27] has been heavily studied with adult populations and a change of more than 0.5 s is thought to be greater than measurement error [70]. However, studies with children with CP suggest much greater variability between assessments with differences as great as 17 s [37] and 10 s [38] being measured in children functioning at GMFCS level III. Since no studies have compared measurement properties of the 10-m walk test [26,27] with children at GMFCS level IV and V, it is unclear whether or not greater variability between performances would be present in this population.
3.6. Clinical Utility
Table 2 provides a summary of the clinical utility of all the measures identified in this review. Clinical utility was rated using the McMaster Outcome Measures rating form and includes consideration of the clarity of the instructions, format, time needed to complete, need for specialized training or equipment, availability of the measure and instruction manual as well as cost. Consideration of usefulness for children using gait trainers would also include whether or not the measure can be used with the child in the gait trainer or not. Excellent overall utility indicates that the tool has adequate to excellent clinical utility, is easily available and has excellent reliability and validity. Adequate overall utility indicates that the tool has adequate to excellent clinical utility, is easily available and has adequate to excellent reliability and validity. Poor overall utility indicates that the tool has poor clinical utility for this population or intervention, is not easily available or has poor reliability and validity. A poor score in any of these factors would result in an overall score of poor overall utility.

Table 2.
Clinical Utility and Usefulness of all included tools.
Several outcome measures identified are freely available and require little specialized equipment other than a tape measure or stop watch. Counting steps or positive affect instances from video or at the time are easily accomplished in clinical practice and ways to increase reliability are included in the relevant articles [16,19,20,21,32]. Detailed instructions for administration of the 10-m [26,27] and 10-min [27] walk tests are provided in the citing article [23]. In addition, detailed instructions for use with adult patients with stroke or spinal cord injury and video support materials are available online [72].
The GMFM [28] and PEDI [29] are commonly available in pediatric therapy settings, but the SFA [31] is costly and its purchase in order to use only one subscale may be prohibitive. The PAMS [30,39] appears to be a useful measure for tracking smaller changes in positioning and mobility function and tolerance in an inpatient population, but is not freely available. The DMA [24,25] was developed specifically for children with CP using gait trainers but has had limited development on its psychometric properties and is also not freely available for use. In contrast, the SWAPS scoring and administration detail, is provided in an appendix to the article [47].
The GMFM-88 [28] is most sensitive to change for children at GMFCS levels IV and V because of the increased number of test items in domains A and B. If clinicians choose to use the GMFM-66 [73] they should note that orthotics and assistive devices cannot be used during testing. The updated Gross Motor Ability Estimator (GMAE-2) software must be used (available for free, download at www.canchild.ca) and the GMFM-66 and percentiles can never be “hand-scored”. However, the usefulness of the GMFM [28] for gait trainer outcomes is questionable given that function in the gait trainer cannot be directly assessed.
4. Discussion
This review has identified 12 different clinical measures that have been used to measure outcomes with children diagnosed with CP functioning at GMFCS levels IV and V who use gait trainers. An additional seven measures have been used in assessment of mobility interventions with children functioning at GMFCS levels IV and V and have been evaluated regarding their potential for use in future gait trainer intervention research. The majority of tools identified address the ICF domain of activity despite the recent emphasis on maximizing participation for children with motor impairments [76].
Only one measure (PEDI [29]) has demonstrated reliability, validity and responsiveness to change in children with CP at GMFCS levels IV and V and appears to have utility for use with gait trainer outcomes research. While the GMFM [28] has excellent psychometric properties, its usefulness in gait trainer outcome research is limited. In the short term, significant change in PEDI [29] mobility level was demonstrated from use of the Hart walker in two studies [17,24]. However, it was only over the longer-term [25] that reduced need for caregiver assistance in social function and self-care skills were measured. Similarly, one study investigating effects of 12 sessions of treadmill training in children aged 2.5–3.9 years at GMFCS levels I–IV [77] also measured change in mobility level and need for caregiver assistance in mobility activities, but not in self-care skills. However, Jones and colleagues [78] measured significant change in mobility skills and reduced need for caregiver assistance in mobility and self-care tasks in subjects versus controls following 12 months power mobility intervention in children at GMFCS levels IV and V aged 14–30 months. This suggests that the PEDI [29] may be more useful as a measure of change in mobility level in shorter-term intervention studies. Impact on participation or environmental factors may only be measured in more longitudinal research and requires further exploration.
Walking (and supported/assisted stepping) remains a primary long-term goal for parents of children with CP, despite the fact that their children often see walking as exercise rather than functional mobility [79]. Many of the outcomes measured in gait trainer research focus on increasing number of steps, increasing walking speed or endurance, or quality of stepping. Most methodological articles exploring psychometric properties of gait and walking assessment tools are focused on children functioning at GMFCS levels I–III. Walking endurance tests, such as the 10-min walk test [27], have not established validity, reliability or responsiveness for children functioning at GMFCS levels IV and V.
Clinical experience suggests that many children who use gait trainers would not be able to complete this task, and perhaps the 6-min walk test [41] maybe a more appropriate length of time. However, this measure has not been used in gait trainer research and use with only a few children at GMFCS level IV has been demonstrated in studies investigating body-weight support treadmill training [77] and robotic step training [80]. One study [43] states that the 6-min walk test [41] is not valid for young children who walk with walking aids following pilot testing with children at GMFCS III. For children who are just learning to walk with assistive device, their movements are slow and labored in comparison with floor mobility and therefore may not be a valid representation of tolerance for physical activity.
This same study described the development of the Early Activity Scale for Endurance (EASE) [43], a parent-report measure of endurance for physical activity developed for use with children at all GMFCS levels. The study measured a moderate correlation with the 6-min walk test [41] for children at GMFCS I and II. They state that walking tests such as the 6-min walk test [41] are not appropriate for children under three years of age due to difficulties in following the directions. However, Mattern-Baxter [77] used the 6-min walk test [41] and the 10-m walk test [26,27] with children aged 2.5–3.9 years and report children with gait trainers being able to complete both tests at follow-up. Children needed directional locks on gait trainers as they were unable to steer, but could step forward. The EASE [43] was found to have construct validity and test-retest reliability for children at all GMFCS levels and to be a feasible and low burden method of assessing tolerance of and endurance for physical activity. However, responsiveness has not been established so it is unknown if it could be used to measure increase in endurance for physical activity following an intervention. In addition, it has a wide minimal detectible change of eight points, due to wide variability in scores.
The DMA [24,25] directly assesses functional use of the gait trainer and has initial documentation of face, content and construct validity, however it is unfortunately not available for use in practice. The SWAPS [47] can be adapted to assess level of support and stepping in a gait trainer, although in the initial development studies children were supported by an adult. Other studies [68,69] have used this measure to assess function of children with CP at GMFCS III or possibly IV using a walker or gait trainer. Inter-rater reliability testing has been completed and it is freely available for use in clinical practice. For children whose gait velocity is less than 50% of typical, clinical measures are more appropriate and sensitive to change than spatiotemporal gait measures [81,82]. There are no published gait lab studies including children at GMFCS IV and V although gait lab studies, with EMG and 3D motion analysis are considered to be the gold standard in gait analysis [83].
Improving participation in meaningful life activities is being stressed as a major focus in current pediatric rehabilitation [76]. For many children functioning at GMFCS levels IV and V, gait trainers are primarily a means of increasing activity and participation rather than as a means of training gait or progression towards independent walking. A lack of measures sensitive to measure change in functional activity and participation goals has been identified for children using gait trainers [5]. In a review of appropriate participation measures for children with CP, Sakzewski [12] suggests that the COPM [42] and GAS [44] are worth considering. The COPM [42] has been successfully used to measure significant improvement in self-selected participation goals following robot-assisted gait training [84] in a study that included one child at GMFCS IV. The COPM [42] has also been used to measure increase in independence or progress in self-selected activity goals in effectiveness research for adaptive seating [60] and power mobility [61].
Environmental and personal factors are other important influences on use of assistive technology [85]. The QUEST 2.0 [46] has been widely used to measure user satisfaction with a variety of different assistive technologies in many different populations. Although it does not have reliability, validity or responsiveness established for children with CP functioning at GMFCS IV or V, it has been previously used with parents of children with CP whose children were using a power mobility intervention [75,86]. Device acceptability is thought to be an important factor influencing device adoption and abandonment. Parents generally rated a high level of acceptability of power mobility device features other than size, weight and transportability [75]. When considering acceptability of gait trainers environmental factors, such as location of use may be influential. If the device is primarily being used in a therapeutic or educational setting, impressions of care staff may be more influential, but parent views may be more important to collect if the device is primarily going to be used in the home setting.
There are a number of limitations to be considered in this review. Although we expanded beyond peer-reviewed journals to grey literature, it was challenging to search conference proceedings and studies may have been missed. Although the term gait trainer is widely used and known particularly in the United States, other terms are used in other countries and this made the electronic search challenging. Using more generic terms such as “walker” generates a wide range of citations and was difficult to narrow down.
Since the number of tools that have been used in gait trainer interventions is limited, we attempted to identify other measures that might be useful in future gait trainer intervention research. However, searching for all potential measures that could be used with this population, would have made the search unmanageable. Instead, we chose to limit our search to an electronic search for systematic reviews of interventions that we considered likely to include children with CP, GMFCS IV and V. We have identified the specific reviews that we used as a source to hand search for additional measures and studies in order to increase replicability of our methods, but recognize that some studies or measures may have been missed.
However, a large-scale comprehensive review of interventions for children with CP [87] that did not meet our inclusion criteria also identified the same reviews on treadmill training [11] and adaptive seating [8] as providing the highest level of evidence published on these interventions. In addition, another review of gait related outcomes [88] and a review of walking ability measures published since our search took place [89], failed to suggest any additional measures that had been used in intervention studies with children functioning at GMFCS IV and V.
Some of the clinical tools identified in this review (e.g., GMFM, PEDI, COPM, GAS) have been widely used with other populations and interventions and it was not within the scope of this paper to evaluate all the studies published on these tools. As a result some of the table results are listed as a summary of ratings based on the data retrieved from the articles we included. We attempted to retrieve the studies relevant to children with CP GMFCS levels IV and V but had to rely on evidence related to children classified as GMFCS I–III, other disabilities or adult research in some instances.
The McMaster Outcome Measures Rating Form [15] was used with all studies but ratings take into account whether the studies had included our identified population or an alternate population. Reliability, validity and responsiveness can only be established in regard to a specific population or setting [90,91] and therefore only studies including children functioning at GMFCS levels IV and V were considered when rating properties as excellent, adequate or poor. Tools may have demonstrated good psychometric properties with another population but could be rated as poor for CP, or poor for GMFCS IV and V.
We considered using an additional quality rating such as the Consensus-based Standards for the selection of health status Measurement Instruments (COSMIN) [92,93], but the sample size requirement for this tool means that almost all the studies included in this review would automatically receive a poor or fair rating, regardless of the conduct of the study. As a result, we determined that this rating would not provide any additional information to assist readers in discriminating between measures. Instead, we chose to divide Table 2 into sections to clarify the tools most useful for gait trainer research, for which specific populations, and which tools required further development, but recognize that this is a qualitative rating based on the consensus of the two reviewers.
5. Conclusions
Lack of sensitive outcomes measures has been identified as a factor in low evidence quality ratings in gait trainer outcomes research. In this study we identified 17 potential tools with the PEDI [29] attaining the highest ratings in all categories. The COPM [42] and GAS [44] show potential for measuring progress on individually selected activity and participation goals while the SWAPS [47] may be adapted to measure progress in mobility or gait function within the gait trainer. The QUEST 2.0 [46] may be beneficial for exploring user satisfaction in comparing different gait trainer features and function with different children. Gait trainer interventions have a multi-dimensional impact while, at this point, most tools have been used to measure activity level outcomes. A more comprehensive outcomes framework [94] should be used to assist in measuring and understanding contextual and functional factors, as well as including activity and participation outcomes that are meaningful to families and children. Further development of all potential tools used with children functioning at GMFCS levels IV and V is warranted.
Author Contributions
Roslyn Livingstone conceived and designed this review; Roslyn Livingstone and Ginny Paleg equally performed the review and analyzed the data; Roslyn Livingstone and Ginny Paleg both wrote the paper. Roslyn Livingstone was responsible for the bibliography and formatting. Both authors have read and approved the final manuscript.
Conflicts of Interest
Roslyn Livingstone declares no conflicts of interest. Ginny Paleg is a paid educational consultant for Prime Engineering, manufacturer of the KidWalk gait trainer. No funding was received for this manuscript and this relationship did not influence the paper in any way.
Abbreviations
| COPM | Canadian Occupational Performance Measure |
| CP | Cerebral Palsy |
| DMA | Directional Mobility Assessment |
| EASE | Early Activity Scale for Endurance |
| GAS | Goal Attainment Scaling |
| GMFCS | Gross Motor Function Classification System |
| GMFM | Gross Motor Function Measure |
| ICF | International Classification of Functioning, Disability and Health |
| MATCH | Matching Assistive Technology and Child |
| PAMS | Physical Abilities Mobility Scale |
| PEDI | Pediatric Evaluation of Disability Inventory |
| QUEST 2.0 | Quebec User Evaluation of Satisfaction with Technology |
| SFA | School Function Assessment |
| SWAPS | Supported Walker Ambulation Scale |
| TDMMT | Top Down Motor Milestone Test |
| Wee FIM | Functional Independence Measure for Children |
Appendix A. Studies Providing Evidence for Use of Additional Tools to Measure Outcomes of Motor Interventions with Children at GMFCS IV and V

| Study | Design | Intervention | Participants & Sample | Clinical Tools |
|---|---|---|---|---|
| Benedict et al., 1999 [86] | Cross-sectional | Assistive Technology | 21 families; 19 CP, 2 metabolic; 2–4 years; 1 PWC user (GMFCS IV) | PEDI [29] QUEST 2.0 [46] |
| Bottos et al., 2001 [61] | Case series | Power Mobility | 25 children with CP, (GMFCS IV or V) 3–8 years | COPM [42] |
| Malouin et al., 1997 [47] | Tool development | NA | 3 expert PT’s 9 children with CP 1.3–2.3 years. GMFCS levels unclear—4 quadriplegic | SWAPS [47] |
| Mattern-Baxter et al., 2009 [77] | Cohort without control | Treadmill training | 6 children with CP 2.5–3.9 years Including 2 at GMFCS IV | 6-min walk test [41] 10-m walk test [26,27] PEDI [29] GMFM-66 [73] |
| Meyer-Heim et al., 2009 [80] | Single Subject Research Design | Robot-assisted treadmill training | 22 children with CP mean 8.6 years (4.6–11.7 years). Including 4 at GMFCS IV | 6 min walk test [41] 10 m walk test [26,27] GMFM-66 [73] |
| Reid et al., 1999 [60] | Single Subject Research Design | Rigid pelvic stabilizer | 6 children with CP GMFCS IV; 8–12 years. Rated with caregiver | COPM [42] |
| Steenbeek et al., 2011 [65] | Methodological | Multi-disciplinary rehabilitation | 23 children with CP GMFCS I–V 2–13 years. Included 5 at GMFCS V and 4 at GMFCS IV | GAS [44] PEDI [29] GMFM-66 [73] |
| Tefft et al., 2011 [75] | Cohort without control | Power Mobility | Parents of 23 children; 18–72 mos. 13 CP (GMFCS IV or V), 10 other | MATCH [45] QUEST 2.0 [46] |
| Westcott-McCoy et al., 2012 [43] | Tool development | Not Appropriate | 69 children GMFCS IV and 92 GMFCS V—Construct validity 8 children GMFCS V—Test-retest reliability study 13 children GMFCS I and 1 GMFCS II—convergent reliability with 6 min walk test | EASE [43] 6-min walk test [41] |
References
- Hanna, S.E.; Bartlett, D.J.; Rivard, L.M.; Russell, D.J. Reference curves for the Gross Motor Function Measure: Percentiles for clinical description and tracking over time among children with cerebral palsy. Phys. Ther. 2008, 88, 596–607. [Google Scholar] [CrossRef] [PubMed]
- Dayanidhi, S.; Dykstra, P.B.; Lyubasyuk, V.; McKay, B.R.; Chambers, H.G.; Lieber, R.L. Reduced satellite cell number in situ in muscular contractures from children with cerebral palsy. J. Orthop. Res. 2015, 33, 1039–1045. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Low, S.A.; McCoy, S.W.; Beling, J.; Adams, J. Pediatric physical therapists’ use of support walkers for children with disabilities: A nationwide survey. Pediatr. Phys. Ther. 2011, 23, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Paleg, G.; Livingstone, R. Outcomes of gait trainer use in home and school settings for children with motor impairments: A systematic review. Clin. Rehabil. 2015, 28, 1077–1091. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability & Health (ICF); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health—Children and Youth; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Chung, J.; Evans, J.; Lee, C.; Rabbani, Y.; Roxborough, L.; Harris, S.R. Effectiveness of adaptive seating on sitting posture and postural control in children with cerebral palsy. Pediatr. Phys. Ther. 2008, 20, 303–317. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, R.; Field, D. Systematic review of power mobility outcomes for infants, children and adolescents with mobility limitations. Clin. Rehabil. 2014, 28, 954–964. [Google Scholar] [CrossRef] [PubMed]
- Houwen, S.; Van der Putten, A.; Vlaskamp, C. A systematic review of the effects of motor interventions to improve motor, cognitive, and/or social functioning in people with severe or profound intellectual disabilities. Res. Dev. Disabil. 2014, 35, 2093–2116. [Google Scholar] [CrossRef] [PubMed]
- Zwicker, J.G.; Mayson, T.A. Effectiveness of treadmill training in children with motor impairments: An overview of systematic reviews. Pediatr. Phys. Ther. 2010, 22, 361–377. [Google Scholar] [CrossRef] [PubMed]
- Sakzewski, L.; Boyd, R.; Ziviani, J. Clinimetric properties of participation measures for 5 to 13 year old children with cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2007, 49, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Field, D.; Livingstone, R. Clinical tools that measure sitting posture, seated postural control or functional abilities in children with motor impairments: A systematic review. Clin. Rehabil. 2013, 27, 994–1004. [Google Scholar] [CrossRef] [PubMed]
- Field, D.A.; Miller, W.C.; Ryan, S.E.; Jarus, T.; Abundo, A. Measuring participation for children and youth with power mobility needs: A systematic review of potential health measurement tools. Arch. Phys. Med. Rehabil. 2015, 97, 462–477. [Google Scholar] [CrossRef] [PubMed]
- Law, M. Outcome Measures Rating Form Guidelines. Available online: http://www.canchild.ca/en/canchildresources.resources.measguid.pdf (accessed on 7 May 2016).
- Barnes, S.B.; Whinnery, K.W. Effects of Functional Mobility Skills Training for Young Students with Physical Disabilities. Except. Child. 2002, 68, 313–324. [Google Scholar] [CrossRef]
- Eisenberg, S.; Zuk, L.; Carmeli, E.; Katz-Leurer, M. Contribution of stepping while standing to function and secondary conditions among children with cerebral palsy. Pediatr. Phys. Ther. 2009, 21, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Farrell, E.; Naber, E.; Geigle, P. Description of a multifaceted rehabilitation program including overground gait training for a child with cerebral palsy: A case report. Physiother. Theory Pract. 2010, 26, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Lancioni, G.; Nirbhay, N.; O’Reilly, F.; Campodonico, F.; Oliva, O.; Vigo, C. Promoting walker-assisted step responses by an adolescent with multiple disabilities through automatically delivered stimulation. J. Vis. Impair. Blind 2005, 99, 109–113. [Google Scholar]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; Oliva, D.; Scalini, L.; Castagnaro, F.; Di Bari, M. Promoting foot-leg movements in children with multiple disabilities through the use of support devices and technology for regulating contingent stimulation. Cogn. Process. 2007, 8, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; Oliva, D.; Piazzolla, G.; Pidala, S.; Smaldone, A.; Manfredi, F. Automatically Delivered Stimulation for Walker-Assisted Step Responses: Measuring its Effects in Persons with Multiple Disabilities. J. Dev. Phys. Disabil. 2007, 19, 1–13. [Google Scholar] [CrossRef]
- Van der Putten, A.; Vlaskamp, C.; Reynders, K.; Nakken, H. Children with profound intellectual and multiple disabilities: The effects of functional movement activities. Clin. Rehabil. 2005, 19, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Willoughby, K.L.; Dodd, K.J.; Shields, N.; Foley, S. Efficacy of partial body weight-supported treadmill training compared with overground walking practice for children with cerebral palsy: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2010, 91, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Wright, F.V.; Belbin, G.; Slack, M.; Jutai, J. An evaluation of the David Hart Walker Orthosis: A new assistive device for children with Cerebral Palsy. Physiother. Can. 1999, 51, 280–291. [Google Scholar]
- Wright, F.V.; Jutai, J.W. Evaluation of the longer-term use of the David Hart Walker Orthosis by children with cerebral palsy: A 3-year prospective evaluation. Disabil. Rehabil. Assist. Technol. 2006, 1, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.D.; Goldie, P.A.; Hill, K.D. Systematic and random error in repeated measurements of temporal and distance parameters of gait after stroke. Arch. Phys. Med. Rehabil. 1997, 78, 725–729. [Google Scholar] [CrossRef]
- Pirpiris, M.; Wilkinson, A.J.; Rodda, J.; Nguyen, T.C.; Baker, R.J.; Nattrass, G.R.; Graham, H.K. Walking speed in children and young adults with neuromuscular disease: Comparison between two assessment methods. J. Pediatr. Orthop. 2003, 23, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.; Rosenbaum, P.; Cadman, D.; Gowland, C.; Hardy, S.; Jarvis, S. The Gross Motor Function Measure: A means to evaluate the effects of physical therapy. Dev. Med. Child Neurol. 1989, 31, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Haley, S.; Coster, W.; Ludlow, L. Pediatric Evaluation of Disability Inventory: Development, Standardization and Administration Manual; New England Medical Center Publications: Boston, MA, USA, 1992. [Google Scholar]
- Suskauer, S.; Slomine, B.; Salorio, C.; Bradley, E.; Madigan, L.; Sesma, H.; Christensen, J. The physical abilities and mobility scale. J. Head Trauma Rehabil. 2006, 21, 420–420. [Google Scholar] [CrossRef]
- Coster, W.; Deeney, T.; Haltiwanger, J.; Haley, S. School Function Assessment (SFA) User’s Manual; PsychCorp: San Antonio, TX, USA, 1998. [Google Scholar]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; Oliva, D.; Campodonico, F.; Buono, S. Walker devices and microswitch technology to enhance assisted indoor ambulation by persons with multiple disabilities: Three single-case studies. Res. Dev. Disabil. 2013, 34, 2191–2199. [Google Scholar] [CrossRef] [PubMed]
- Van der Putten, A.; Vlaskamp, C.; Reynders, K.; Nakken, H. Movement skill assessment in children with profound multiple disabilities: A psychometric analysis of the Top Down Motor Milestone Test. Clin. Rehabil. 2005, 19, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.C.; Bode, R.K.; Granger, C.V.; Heinemann, A.W. Psychometric Properties and Developmental Differences in Children’s ADL Item Hierarchy. Am. J. Phys. Med. Rehabil. 2005, 84, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Uniform Data System for Medical Rehabilitation: WeeFIM System Clinical Guide, 5th ed.; University of Buffalo: New York, NY, USA, 1998.
- Tedla, J.S.; Ganesan, S.; Katragadda, S. Inter-rater reliability of the Top Down Motor Milestone Test: A cross-sectional study. Clin. Rehabil. 2009, 23, 725–729. [Google Scholar] [CrossRef] [PubMed]
- Thompson, P.; Beath, T.; Bell, J.; Jacobson, G.; Phair, T.; Salbach, N.M.; Wright, F.V. Test-retest reliability of the 10-metre fast walk test and 6-minute walk test in ambulatory school-aged children with cerebral palsy. Dev. Med. Child Neurol. 2008, 50, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Graser, J.V.; Letsch, C.; Van Hedel, H.J.A. Reliability of timed walking tests and temporo-spatial gait parameters in youths with neurological gait disorders. BMC Neurol. 2016, 16, 15. [Google Scholar] [CrossRef] [PubMed]
- Trovato, M.K.; Bradley, E.; Slomine, B.S.; Salorio, C.F.; Christensen, J.R.; Suskauer, S.J. Physical abilities and mobility scale: Reliability and validity in children receiving inpatient rehabilitation for acquired brain injury. Arch. Phys. Med. Rehabil. 2013, 94, 1335–1341. [Google Scholar] [CrossRef] [PubMed]
- Kuenzle, C.; Brunner, R. The effects of the Norsk Funktion-walking orthosis on the walking ability of children with cerebal palsy and severe gait impairment. J. Prosthet. Orthot. 2009, 21, 138–144. [Google Scholar] [CrossRef]
- Maher, C.; Williams, L.; Olds, T. The six-minute walk test for children with cerebral palsy. Int. J. Rehabil. Res. 2008, 31, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Law, M.; Baptiste, S.; Carswell, A.; McColl, M.; Polatajko, H.; Pollock, N. Canadian Occupational Performance Measure, 2nd ed.; Canadian Association of Occupational Therapists: Toronto, ON, Canada, 1994. [Google Scholar]
- Westcott McCoy, S.; Yocum, A.; Bartlett, D.J.; Mendoza, J.; Jeffries, L.; Chiarello, L.; Palisano, R.J. Development of the Early Activity Scale for Endurance for children with cerebral palsy. Pediatr. Phys. Ther. 2012, 24, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Kiresuk, T.; Smith, A.; Cardillo, J. Goal Attainment Scaling: Application, Theory and Measurement; Lawrence Erlbaum Associates: Hillscale, NJ, USA, 1994. [Google Scholar]
- Scherer, M. Matching Assistive Technology & Child (MATCH. A Process and Series of Assessments for Selecting and Evaluating Technologies Used by Infants and Young Children; The Institute for Matching Person & Technology: Webster, NY, USA, 1998. [Google Scholar]
- Demers, L.; Weiss-Lambrou, R.; Ska, B. The Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST Version 2.0), 2000. Available online: http://www.midss.ie/sites/default/files/questmanual_final_electronic20version_0.pdf (accessed on 7 May 2016).
- Malouin, F.; Richards, C.; Menier, C.; Dumas, F.; Marcoux, S. Supported walker ambulation performance scale (SWAPS): Development of an outcome measure of locomotor status in children with cerebral palsy. Pediatr. Phys. Ther. 1997, 9, 48–53. [Google Scholar] [CrossRef]
- Dodd, K.J. Partial body-weight-supported treadmill training can improve walking in children with cerebral palsy: A clinical controlled trial. Dev. Med. Child Neurol. 2007, 49, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.; Kim, M. Reliability and responsiveness of the gross motor function measure-88 in children with cerebral palsy. Phys. Ther. 2013, 93, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Wright, F.; Boschen, K. Use of the Pediatric Evaluation of Disability Inventory to detect change in functional status in children with cerebral palsy. Physiother. Can. 1996, 48 (Suppl. 2), 1–6. [Google Scholar]
- Nichols, D.; Case-Smith, J. Reliability and Validity of the Pediatric Evaluation of Disability Inventory. Pediatr. Phys. Ther. 1996, 8, 15–24. [Google Scholar] [CrossRef]
- Iyer, L.V.; Haley, S.M.; Watkins, M.P.; Dumas, H.M. Establishing minimal clinically important differences for scores on the pediatric evaluation of disability inventory for inpatient rehabilitation. Phys. Ther. 2003, 83, 888–898. [Google Scholar] [PubMed]
- Wright, F.V.; Boschen, K.; Jutai, J. Exploring the comparative responsiveness of a core set of outcome measures in a school-based conductive education programme. Child Care Health Dev. 2005, 31, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Wright, F.; Liu, G.; Milne, F. Reliability of the measurement of time-distance parameters of gait: A comparison in children with juvenile rheumatoid arthritis and children with cerebral palsy. Physiother. Can. 1999, 15, 191–200. [Google Scholar]
- Nsenga Leunkeu, A.; Shephard, R.J.; Ahmaidi, S. Six-minute walk test in children with cerebral palsy gross motor function classification system levels I and II: Reproducibility, validity, and training effects. Arch. Phys. Med. Rehabil. 2012, 93, 2333–2339. [Google Scholar] [CrossRef] [PubMed]
- Cusick, A.; Lannin, N.A.; Lowe, K. Adapting the Canadian Occupational Performance Measure for use in a paediatric clinical trial. Disabil. Rehabil. 2007, 29, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Verkerk, G.J.Q.; Wolf, M.J.M.; Louwers, A.M.; Meester-Delver, A.; Nollet, F. The reproducibility and validity of the Canadian Occupational Performance Measure in parents of children with disabilities. Clin. Rehabil. 2006, 20, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Wallen, M.A.; Ziviani, J.M. Canadian Occupational Performance Measure: Impact of blinded parent-proxy ratings on outcome. Can. J. Occup. Ther. 2012, 79, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Cusick, A.; McIntyre, S.; Novak, I.; Lannin, N.; Lowe, K. A comparison of goal attainment scaling and the Canadian Occupational Performance Measure for paediatric rehabilitation research. Pediatr. Rehabil. 2006, 9, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Reid, D.; Rigby, P.; Ryan, S. Functional impact of a rigid pelvic stabilizer on children with cerebral palsy who use wheelchairs: users’ and caregivers’ perceptions. Pediatr. Rehabil. 1999, 3, 101–118. [Google Scholar] [PubMed]
- Bottos, M.; Bolcati, C.; Sciuto, L.; Ruggeri, C.; Feliciangeli, A. Powered wheelchairs and independence in young children with tetraplegia. Dev. Med. Child Neurol. 2001, 43, 769–777. [Google Scholar] [CrossRef] [PubMed]
- Carswell, A.; McColl, M.A.; Baptiste, S.; Law, M.; Polatajko, H.; Pollock, N. The Canadian Occupational Performance Measure: A research and clinical literature review. Can. J. Occup. Ther. 2004, 71, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Steenbeek, D.; Ketelaar, M.; Lindeman, E.; Galama, K.; Gorter, J.W. Interrater Reliability of Goal Attainment Scaling in Rehabilitation of Children With Cerebral Palsy. Arch. Phys. Med. Rehabil. 2010, 91, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Law, L.S.H.; Dai, M.O.; Siu, A. Applicability of goal attainment scaling in the evaluation of gross motor changes in children with cerebral palsy. Hong Kong Physiother. J. 2004, 22, 22–28. [Google Scholar] [CrossRef]
- Steenbeek, D.; Gorter, J.W.; Ketelaar, M.; Galama, K.; Lindeman, E. Responsiveness of Goal Attainment Scaling in comparison to two standardized measures in outcome evaluation of children with cerebral palsy. Clin. Rehabil. 2011, 25, 1128–1139. [Google Scholar] [CrossRef] [PubMed]
- Demers, L.; Weiss-Lambrou, R.; Ska, B. Item analysis of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST). Assist. Technol. 2000, 12, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Demers, L.; Weiss-lambrou, R.; Ska, B. The Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0): An overview and recent progress. Technol. Disabil. 2002, 14, 101–105. [Google Scholar]
- Kurz, M.J.; Stuberg, W.; Dejong, S.; Arpin, D.J. Overground body-weight-supported gait training for children and youth with neuromuscular impairments. Phys. Occup. Ther. Pediatr. 2013, 33, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Stuberg, W.; DeJong, S.; Kelly, M. Gait training using partial body weight support during over ground walking in individuals with developmental disabilities. Pediatr. Phys. Ther. 2004, 16, 65–66. [Google Scholar]
- Watson, M.J. Refining the ten-metre walking test for use with neurologically impaired people. Physiother 2002, 88, 386–397. [Google Scholar] [CrossRef]
- Haley, S.M.; Coster, W.I.; Kao, Y.C.; Dumas, H.M.; Fragala-Pinkham, M.A.; Kramer, J.M.; Ludlow, L.H.; Moed, R. Lessons from use of the Pediatric Evaluation of Disability Inventory: Where do we go from here? Pediatr. Phys. Ther. 2010, 22, 69–75. [Google Scholar] [CrossRef] [PubMed]
- SCIRE Project. Available online: http://www.scireproject.com/outcome-measures-new/10-m-walking-test-10-mwt# (accessed on 26 July 2016).
- Russell, D.; Rosenbaum, P.; Avery, L.; Lane, M. The Gross Motor Function Measure (GMFM-66 and GMFM-88) User’s Manual; Cambridge University Press: Cambridege, UK, 2002. [Google Scholar]
- Steenbeek, D.; Ketelaar, M.; Galama, K.; Gorter, J.W. Goal attainment scaling in paediatric rehabilitation: A report on the clinical training of an interdisciplinary team. Child Care Health Dev. 2008, 34, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Tefft, D.; Guerette, P.; Furumasu, J. The impact of early powered mobility on parental stress, negative emotions, and family social interactions. Phys. Occup. Ther. Pediatr. 2011, 31, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.J.; Chiarello, L.A.; King, G.A.; Novak, I.; Stoner, T.; Fiss, A. Participation-based therapy for children with physical disabilities. Disabil. Rehabil. 2012, 34, 1041–1052. [Google Scholar] [CrossRef] [PubMed]
- Mattern-Baxter, K.; Bellamy, S.; Mansoor, J.K. Effects of intensive locomotor treadmill training on young children with cerebral palsy. Pediatr. Phys. Ther. 2009, 21, 308–318. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.; McEwen, I.; Neas, B. Effects of power wheelchairs on the development and function of young children with severe motor impairments. Pediatr. Phys. Ther. 2012, 24, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Gibson, B.E.; Teachman, G.; Wright, V.; Fehlings, D.; Young, N.L.; McKeever, P. Children’s and parents’ beliefs regarding the value of walking: Rehabilitation implications for children with cerebral palsy. Child Care Health Dev. 2012, 38, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Heim, A.; Ammann-Reiffer, C.; Schmartz, A.; Schaefer, J.; Sennhauser, F.H.; Heinen, F.; Knecht, B.; Dabrowski, E.; Borggraefe, I. Improvement of walking abilities after robotic-assisted locomotion training in children with cerebral palsy. Arch. Dis. Child 2009, 94, 615–620. [Google Scholar] [CrossRef] [PubMed]
- Richards, C.L.; Malouin, F.; Dumas, F.; Marcoux, S.; Lepage, C.; Menier, C. Early and intensive treadmill locomotor training for young children with cerebral palsy: A feasibility study. Pediatr. Phys. Ther. 1997, 9, 158–165. [Google Scholar] [CrossRef]
- Drouin, L.M.; Malouin, F.; Richards, C.L.; Marcoux, S. Correlation between the gross motor function measure scores and gait spatiotemporal measures in children with neurological impairments. Dev. Med. Child Neurol. 1996, 38, 1007–1019. [Google Scholar] [CrossRef] [PubMed]
- Carty, C.P.; Walsh, H.P.J.; Gillett, J.G.; Phillips, T.; Edwards, J.M.; Boyd, R.N. The effect of femoral derotation osteotomy on transverse plane hip and pelvic kinematics in children with cerebral palsy: A systematic review and meta-analysis. Gait Posture 2014, 40, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, A.S.; Homburg, M.; Warken, B.; Auffermann, H.; Koerte, I.; Berweck, S.; Jahn, K.; Heinen, F.; Borggraefe, I. Prospective controlled cohort study to evaluate changes of function, activity and participation in patients with bilateral spastic cerebral palsy after Robot-enhanced repetitive treadmill therapy. Eur. J. Paediatr. Neurol. 2014, 18, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Scherer, M.J.; Craddock, G. Matching Person & Technology ({MPT}) assessment process. Technol. Disabil. 2002, 14, 125–132. [Google Scholar]
- Benedict, R.; Lee, J.; Marrujo, S.; Farel, A. Assistive devices as an early childhood intervention: Evaluating outcomes. Technol. Disabil. 1999, 11, 79–90. [Google Scholar]
- Novak, I.; McIntyre, S.; Morgan, C.; Campbell, L.; Dark, L.; Morton, N.; Stumbles, E.; Wilson, S.; Goldsmith, S. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev. Med. Child Neurol. 2002, 55, 885–910. [Google Scholar] [CrossRef] [PubMed]
- Amman-Reiffer, C.; Bastiaenen, C.H.G.; De Bie, R.A.; Van Hedel, H.J.A. Measurement properties of gait-related outcomes in youth with neuromuscular diagnoses: A systematic review. Phys. Ther. 2014, 94, 1067–1082. [Google Scholar] [CrossRef] [PubMed]
- Himoru, N.; Hirokazu, A.; Nishibu, H.; Seino, T.; Mori, M. Easy to use clinical measures of walking ability in children and adolescents with cerebral palsy: A systematic review. Disabil. Rehabil. 2016. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Andresen, E.M. Criteria for assessing the tools of disability outcomes research. Arch. Phys. Med. Rehabil. 2000, 81, S15–S20. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; Prinsen, C.A.C.; Ricci Garotti, M.G.; Suman, A.; De Vet, H.C.W.; Mokkink, L.B. The quality of systematic reviews of health-related outcome measurement instruments. Qual. Life Res. 2016, 25, 767–779. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Terwee, C.B.; Stratford, P.W.; Alonso, J.; Patrick, D.L.; Riphagen, I.; Knol, D.L.; Bouter, L.M.; DeVet, H.C.W. Evaluation of the methodological quality of systematic reviews of health status measurement instruments. Qual. Life Res. 2009, 18, 313–333. [Google Scholar] [CrossRef] [PubMed]
- Fuhrer, M.J.; Jutai, J.W.; DeRuyter, F.A. A framework for the conceptual modelling of assistive technology device outcomes. Disabil. Rehabil. 2003, 25, 1243–1251. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).