Barriers and Facilitators of Using MyDispense from the Student Perspective: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
- 1.
- Primary research sources;
- 2.
- Published between January 2015 and January 2025;
- 3.
- Qualitative, quantitative and/or mixed-methods studies examining pharmacy students’ perceptions of MyDispense;
- 4.
- Published in English.
- 5.
- Reviews, conference abstracts, meta-analyses, commentary studies, grey literature;
- 6.
- Not published in English;
- 7.
- Not investigating the use of MyDispense;
- 8.
- Did not include a pharmacy student population.
2.3. Study Selection
2.4. Data Extraction and Synthesis
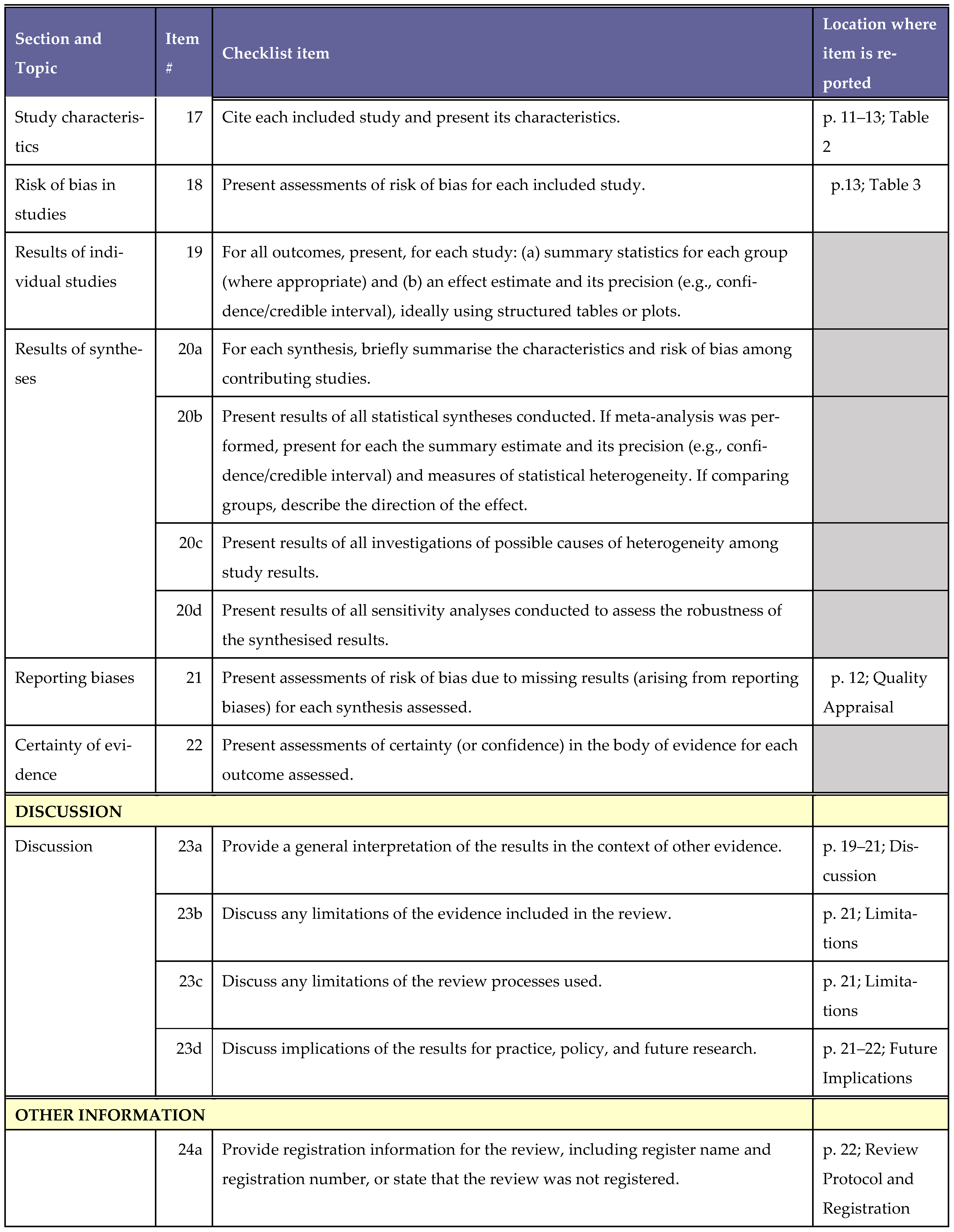
2.5. Quality Assessment of Included Studies
3. Results
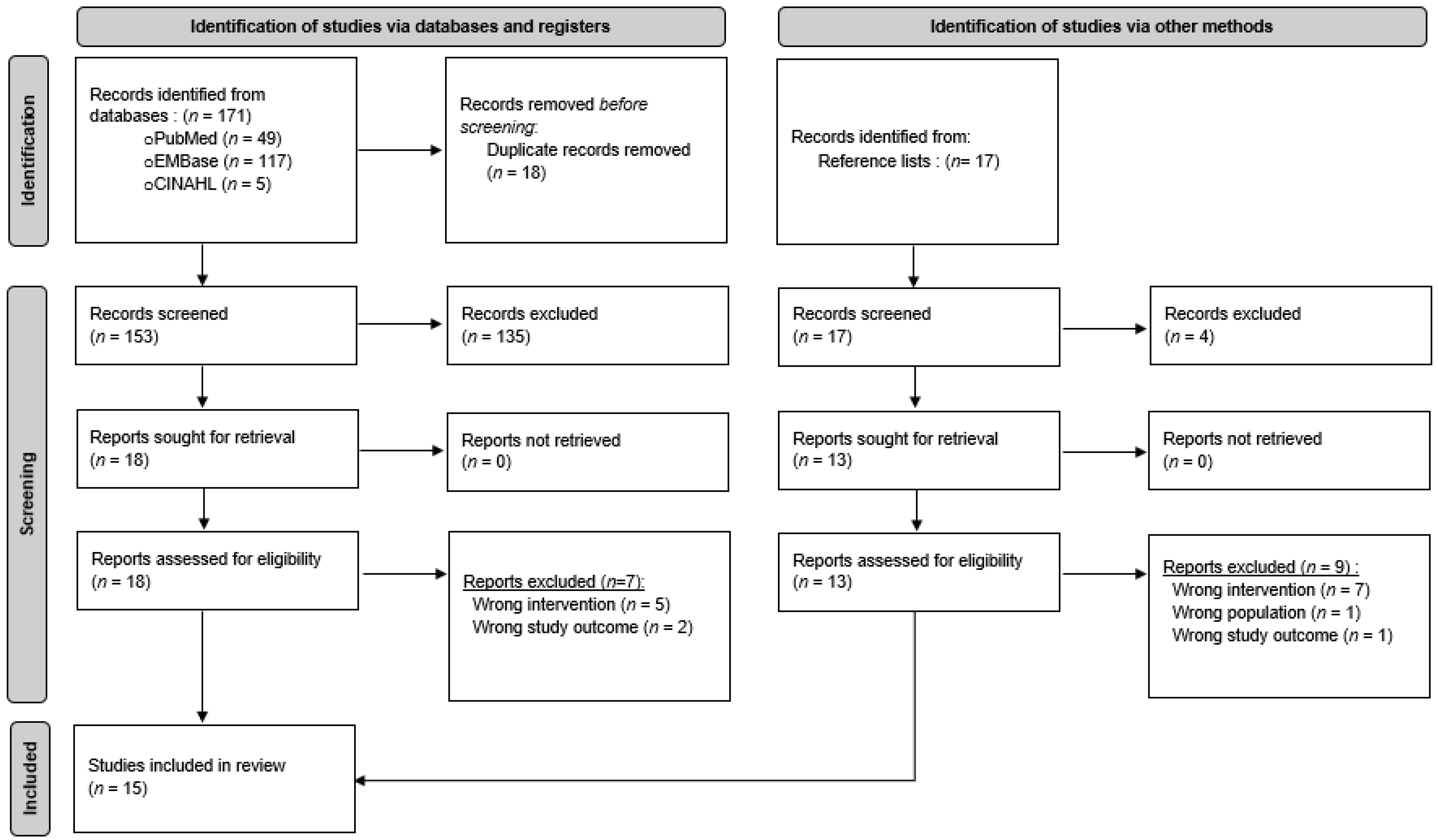
3.1. Studies Eligible for Inclusion
3.2. Characteristics of Included Studies
3.3. Summary of Identified Facilitators
3.3.1. Facilitator Theme I: Develops Competency
3.3.2. Facilitator Theme II: Accessibility
3.3.3. Facilitator Theme III: Engaging Learning Experience
3.3.4. Facilitator Theme IV: Safe Learning Environment
3.4. Summary of Identified Barriers
3.4.1. Barrier Theme I: Learning Curve
3.4.2. Barrier Theme II: IT Issues
3.4.3. Barrier Theme III: Limited Realism and Applications
3.5. Quality Appraisal
4. Discussion
4.1. Limitations
4.2. Future Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
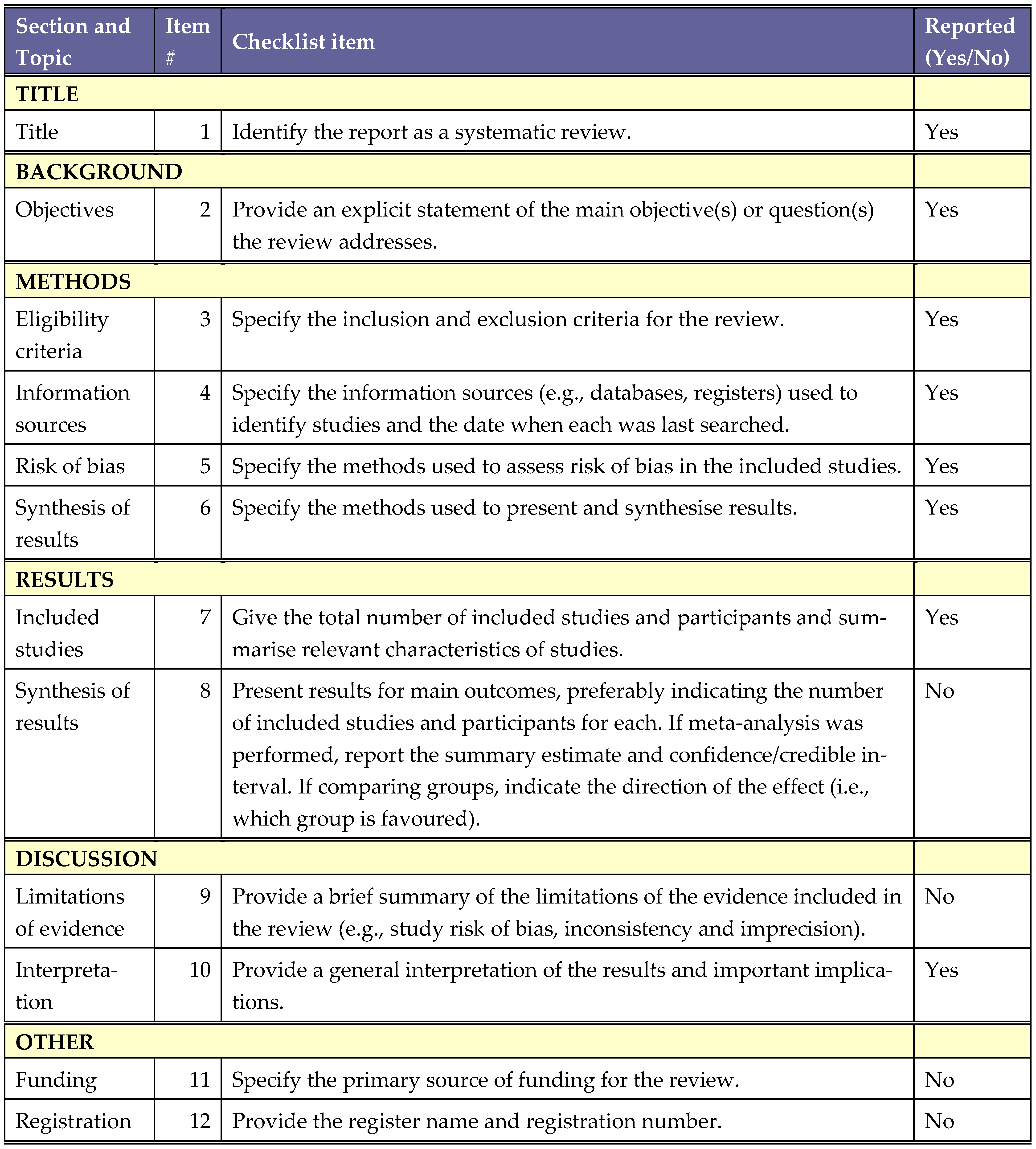
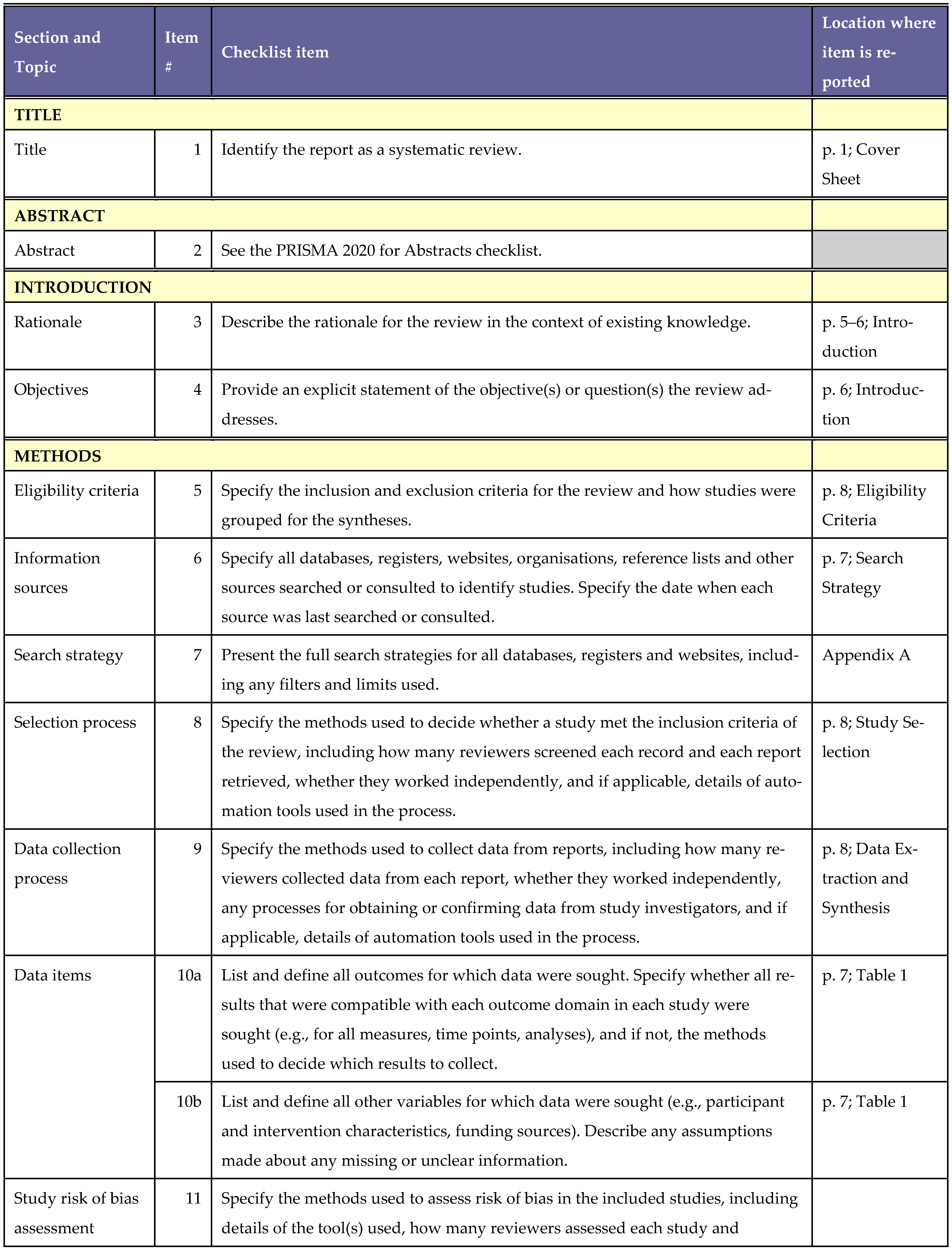
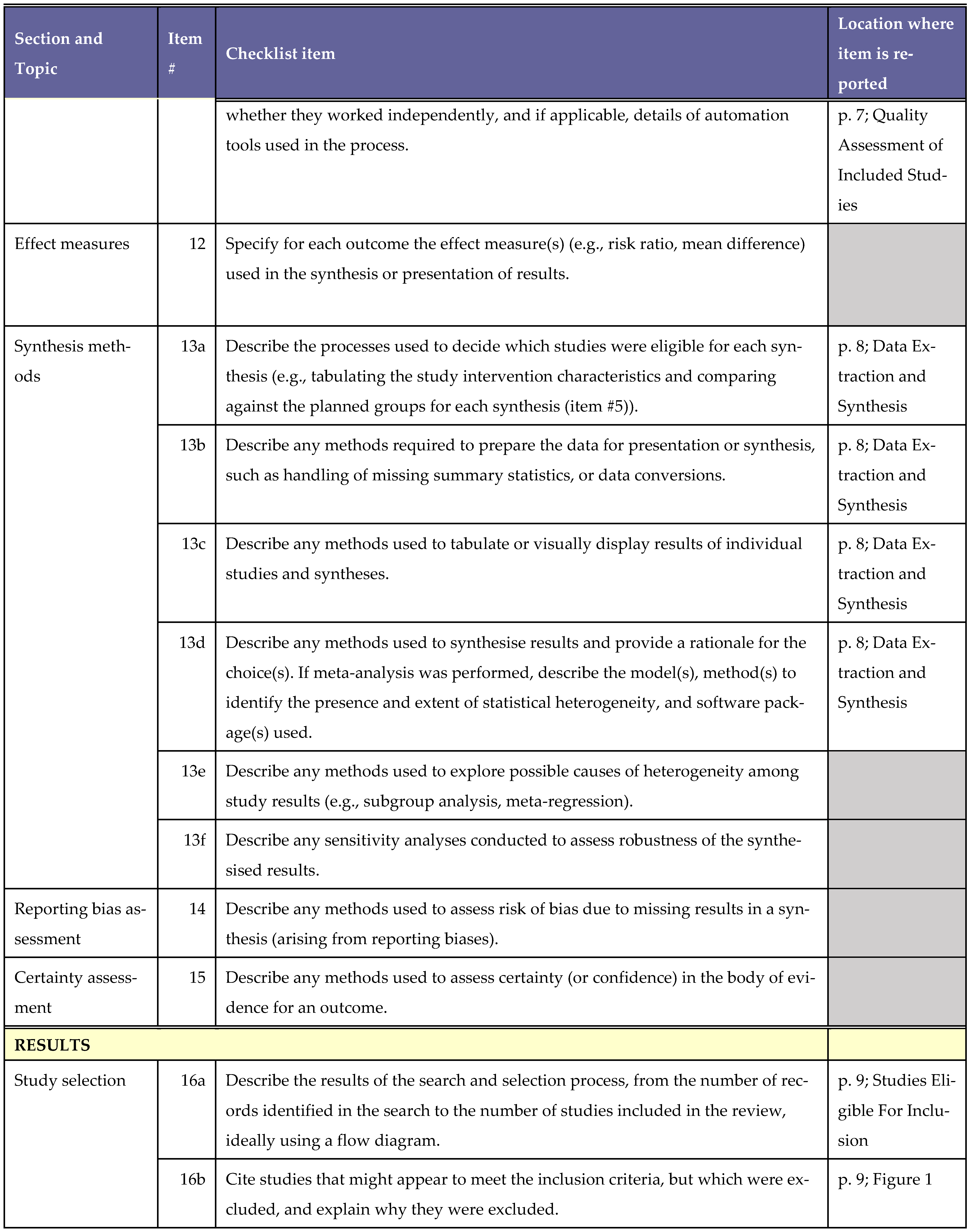
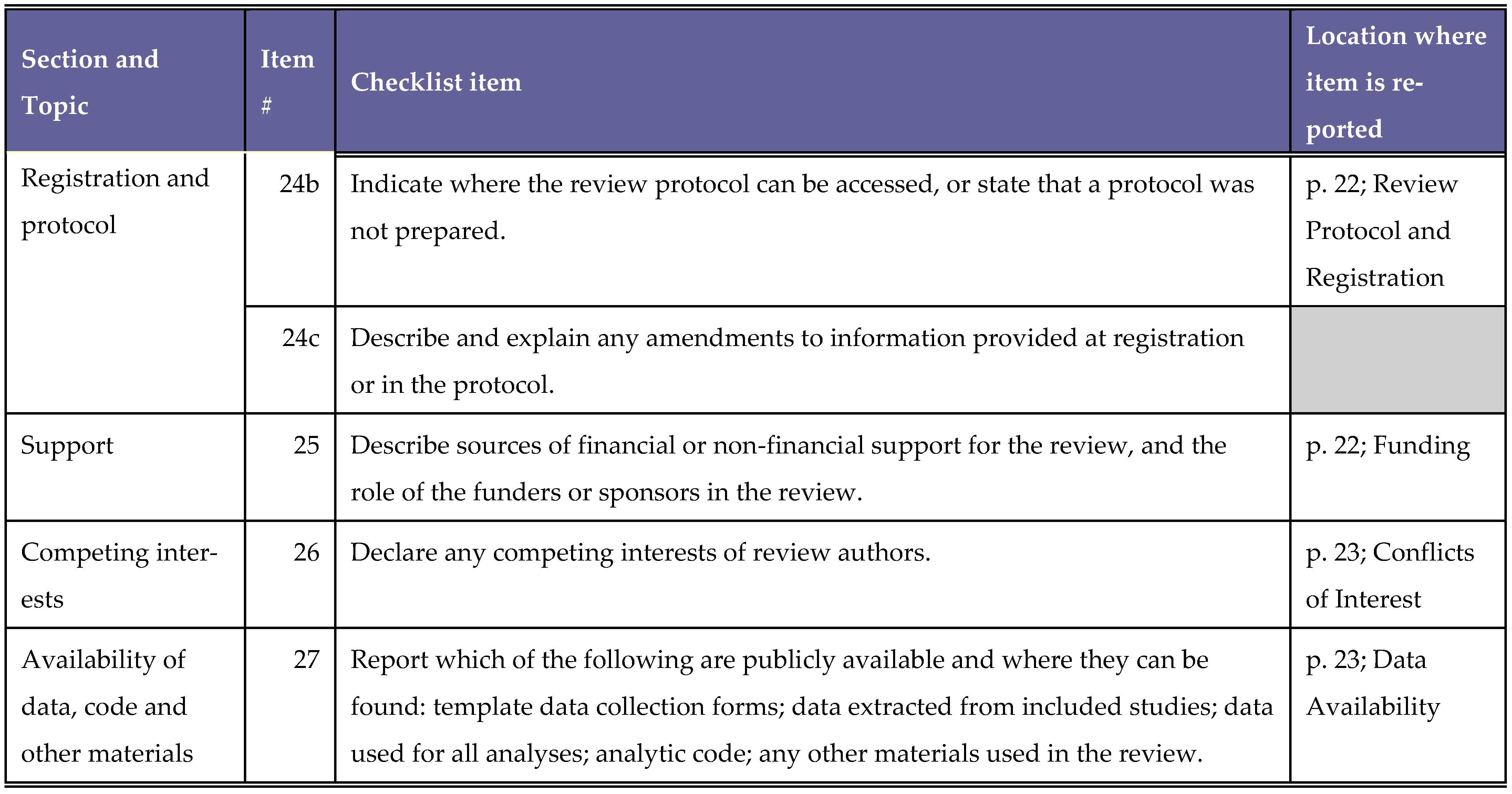
Appendix A. PRISMA Checklist
Appendix B. Search Strategy
| Database | Date of Search | Search Strings | Terms Used | Results |
|---|---|---|---|---|
| PubMed | 28 January 2025 | S1 | (perception[MeSH Terms]) OR (attitude[MeSH Terms])) OR (facilitator)) OR (enabler)) OR (barrier)) OR (obstacle)) OR (challenge) | 4,224,261 |
| S2 | (“MyDispense”) OR (computer simulation[MeSH Terms])) OR (patient simulations[MeSH Terms])) OR (educational technologies[MeSH Terms])) OR (“virtual patient simulator”[tiab:~3])) OR (“dispensing simulation”) | 440,869 | ||
| S3 | ((students[MeSH Terms]) OR (pharmacy students[MeSH Terms])) | 185,856 | ||
| S4 | ((pharmacy[MeSH Terms]) OR (pharmacy education[MeSH Terms])) | 26,507 | ||
| S5 | S1 AND S2 AND S3 AND S4 | 49 |
| Database | Date of Search | Search Strings | Terms Used | Results |
|---|---|---|---|---|
| CINAHL | 28 January 2025 | S1 | (MM “Attitude”) OR “beliefs” OR “views” OR “opinions” OR “barriers” OR “challenges” OR “obstacles” OR “facilitators” OR “enablers” | 567,858 |
| S2 | “Mydispense” OR “patient simulation” OR “virtual simulation” OR “computer simulation” OR “simulation” N2 (“patient” OR “virtual” OR “dispensing”) | 27,672 | ||
| S3 | (MH “Students”) OR (MH “Students, Pharmacy”) | 22,056 | ||
| S4 | (MH “Education, Pharmacy”) OR “pharmacy” | 13,743 | ||
| S5 | S1 AND S2 AND S3 AND S4 | 5 |
| Database | Date of Search | Search Strings | Terms Used | Results |
|---|---|---|---|---|
| Embase | 28 January 2025 | S1 | ‘attitude’/de OR ‘attitude’ OR ‘beliefs’/de OR ‘beliefs’ OR ‘perception’/de OR ‘perception’ OR ‘challenge’/de OR ‘challenge’ OR ‘obstacles’/de OR ‘obstacles’ OR ‘barriers’/de OR ‘barriers’ OR ‘facilitator’/de OR ‘facilitator’ OR enablers | 2,003,993 |
| S2 | ‘mydispense’ OR ‘computer simulation’/exp OR ‘computer simulation’ OR ‘patient simulation’/exp OR ‘patient simulation’ OR ((virtual OR patient OR dispensing) NEAR/2 simulation) | 197,410 | ||
| S3 | ‘student’/exp OR ‘student’ OR ‘pharmacy student’/exp OR ‘pharmacy student’ | 617,087 | ||
| S4 | ‘pharmacy’/exp OR pharmacy OR ‘pharmacy education’/exp OR ‘pharmacy education’ | 1,299,905 | ||
| S5 | S1 AND S2 AND S3 AND S4 | 117 |
References
- Pharmaceutical Society of Ireland (PSI). Accreditation Standards for the Five Year Master’s Degree Programmes in Pharmacy; Pharmaceutical Society of Ireland (PSI): Dublin, Ireland, 2023; Available online: https://www.psi.ie/education-and-training/training-become-pharmacist-ireland/accreditation-and-standards-0 (accessed on 20 March 2025).
- Atkinson, J.; Rombaut, B.; Pozo, A.; Rekkas, D.; Veski, P.; Hirvonen, J.; Bozic, B.; Skowron, A.; Mircioiu, C.; Marcincal, A.; et al. The production of a framework of competences for pharmacy practice in the European Union. Pharmacy 2014, 2, 161–174. [Google Scholar] [CrossRef]
- Hall, K.; Musing, E.; Miller, D.A.; Tisdale, J.E. Experiential training for pharmacy students: Time for a new approach. Can. J. Hosp. Pharm. 2012, 65, 285. [Google Scholar] [CrossRef]
- Gaba, D.M. The future vision of simulation in health care. Qual. Saf. Health Care 2004, 13, i2. [Google Scholar] [CrossRef]
- McBane, S.; Alavandi, P.; Allen, S.; Bingham, A.; Dang, Y.; Elmes, A.; Fallon, J.M.; Herman, A.; Januszka, J.; Peddi, A.N.; et al. Overview of implementation and learning outcomes of simulation in pharmacy education. J. Am. Coll. Clin. Pharm. 2023, 6, 528–554. [Google Scholar] [CrossRef]
- Crea, K.A. Practice skill development through the use of human patient simulation. Am. J. Pharm. Educ. 2011, 75, 188. [Google Scholar] [CrossRef]
- Lin, K.; Travlos, D.V.; Wadelin, J.W.; Vlasses, P.H. Simulation and introductory pharmacy practice experiences. Am. J. Pharm. Educ. 2011, 75, 209. [Google Scholar] [CrossRef]
- Lloyd, M.; Watmough, S.; Bennett, N. Simulation-based training: Applications in clinical pharmacy. Clin. Pharm. 2018, 10, 3–10. [Google Scholar] [CrossRef]
- Bernaitis, N.; Baumann-Birkbeck, L.; Alcorn, S.; Powell, M.; Arora, D.; Anoopkumar-Dukie, S. Simulated patient cases using DecisionSim™ improves student performance and satisfaction in pharmacotherapeutics education. Curr. Pharm. Teach. Learn. 2018, 10, 730–735. [Google Scholar] [CrossRef]
- Cavaco, A.M.; Madeira, F. European pharmacy students’ experience with virtual patient technology. Am. J. Pharm. Educ. 2012, 76, 106. [Google Scholar] [CrossRef]
- Han, H.; Resch, D.; Kovach, R. Educational technology in medical education. Teach. Learn. Med. 2013, 25, S39–S43. [Google Scholar] [CrossRef]
- Maarek, J.-M. Benefits of Active Learning Embedded in Online Content Material Supporting a Flipped Classroom. In Proceedings of the 2018 ASEE Annual Conference & Exposition Proceedings, Salt Lake City, UT, USA, 24–27 June 2018; ASEE Conferences: Salt Lake City, UT, USA, 2018; p. 29845. [Google Scholar]
- Dimock, M. Where Millennials End and Generation Z Begins|Pew Research Center. Washington, DC, USA. 2019. Available online: https://www.pewresearch.org/shortreads/2019/01/17/where-millennials-end-and-generation-z-begins/ (accessed on 21 March 2025).
- Shatto, B.; Erwin, K. Teaching Millennials and Generation Z: Bridging the Generational Divide. Creat. Nurs. 2017, 23, 24–28. [Google Scholar] [CrossRef]
- Salem, S.; Cooper, J.; Schneider, J.; Croft, H.; Munro, I. Student Acceptance of Using Augmented Reality Applications for Learning in Pharmacy: A Pilot Study. Pharmacy 2020, 8, 122. [Google Scholar] [CrossRef]
- Schneider, J.; Patfield, M.; Croft, H.; Salem, S.; Munro, I. Introducing Augmented Reality Technology to Enhance Learning in Pharmacy Education: A Pilot Study. Pharmacy 2020, 8, 109. [Google Scholar] [CrossRef]
- Coyne, L.; Merritt, T.A.; Parmentier, B.L.; Sharpton, R.A.; Takemoto, J.K. The past, present, and future of virtual reality in pharmacy education. Am. J. Pharm. Educ. 2019, 83, 7456. [Google Scholar] [CrossRef]
- Mak, V.; Fitzgerald, J.; Holle, L.; Vordenberg, S.E.; Kebodeaux, C. Meeting pharmacy educational outcomes through effective use of the virtual simulation MyDispense. Curr. Pharm. Teach. Learn. 2021, 13, 739–742. [Google Scholar] [CrossRef]
- Marriott, J.L. Use and evaluation of “virtual” patients for assessment of clinical pharmacy undergraduates. Pharm. Educ. 2007, 7, 341–349. [Google Scholar] [CrossRef]
- Thompson, J.; White, S.; Chapman, S. Virtual patients as a tool for training pre-registration pharmacists and increasing their preparedness to practice: A qualitative study. PLoS ONE 2020, 15, e0238226. [Google Scholar] [CrossRef]
- Seybert, A.L.; Smithburger, P.L.; Benedict, N.J.; Kobulinsky, L.R.; Kane-Gill, S.L.; Coons, J.C. Evidence for simulation in pharmacy education. J. Am. Coll. Clin. Pharm. 2019, 2, 686–692. [Google Scholar] [CrossRef]
- Monash University. MyDispense Melbourne, Australia. Faculty of Pharmacy and Pharmaceutical Sciences, Monash University. 2025. Available online: https://info.mydispense.monash.edu/ (accessed on 21 March 2025).
- Smith, M.A.; Mohammad, R.A.; Benedict, N. Use of virtual patients in an advanced therapeutics pharmacy course to promote active, patient-centered learning. Am. J. Pharm. Educ. 2014, 78, 125. [Google Scholar] [CrossRef]
- Phanudulkitti, C.; Kebodeaux, C.; Vordenberg, S.E. Use of the virtual simulation Tool ‘MyDispense’ by pharmacy programs in the United States. Am. J. Pharm. Educ. 2022, 86, ajpe8827. [Google Scholar] [CrossRef]
- Gharib, A.M.; Peterson, G.M.; Bindoff, I.K.; Salahudeen, M.S. Potential barriers to the implementation of computer-based simulation in pharmacy education: A systematic review. Pharmacy 2023, 11, 86. [Google Scholar] [CrossRef]
- McDowell, J.; Styles, K.; Sewell, K.; Trinder, P.; Marriott, J.; Maher, S.; Naidu, S. A simulated learning environment for teaching medicine dispensing skills. Am. J. Pharm. Educ. 2016, 80, 11. [Google Scholar] [CrossRef]
- Gharib, A.M.; Peterson, G.M.; Bindoff, I.K.; Salahudeen, M.S. Exploring barriers to the effective use of computer-based simulation in pharmacy education: A mixed-methods case study. Front. Med. 2024, 11, 1448893. [Google Scholar] [CrossRef]
- Beshir, S.A.; Mohamed, A.P.; Soorya, A.; Sir Loon Goh, S.; Moussa El-Labadd, E.; Hussain, N.; Said, A.S.A. Virtual patient simulation in pharmacy education: A systematic review. Pharm. Educ. 2022, 22, 954–970. [Google Scholar] [CrossRef]
- Khera, H.K.; Mannix, E.; Moussa, R.; Mak, V. MyDispense simulation in pharmacy education: A scoping review. J. Pharm. Policy Pract. 2023, 16, 110. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Waghel, R.C.; Wilson, J.A. Exploring community pharmacy work experience impact on errors and omissions performance and MyDispense perceptions. Curr. Pharm. Teach. Learn. 2025, 17, 102235. [Google Scholar] [CrossRef]
- Rude, T.A.; Eukel, H.N.; Ahmed-Sarwar, N.; Burke, E.S.; Anderson, A.N.; Riskin, J.; Caldas, L.M. An introductory over-the-counter simulation for first-year pharmacy students using a virtual pharmacy. Am. J. Pharm. Educ. 2023, 87, ajpe8940. [Google Scholar] [CrossRef]
- Tabulov, C.; Vascimini, A.; Ruble, M. Using a virtual simulation platform for dispensing pediatric prescriptions in a community-based pharmaceutical skills course. Curr. Pharm. Teach. Learn. 2023, 15, 1052–1059. [Google Scholar] [CrossRef]
- Deneff, M.; Holle, L.M.; Fitzgerald, J.M.; Wheeler, K. A novel approach to pharmacy practice law instruction. Pharmacy 2021, 9, 75. [Google Scholar] [CrossRef]
- Ambroziak, K.; Ibrahim, N.; Marshall, V.D.; Kelling, S.E. Virtual simulation to personalize student learning in a required pharmacy course. Curr. Pharm. Teach. Learn. 2018, 10, 750–756. [Google Scholar] [CrossRef]
- Ferrone, M.; Kebodeaux, C.; Fitzgerald, J.; Holle, L. Implementation of a virtual dispensing simulator to support US pharmacy education. Curr. Pharm. Teach. Learn. 2017, 9, 511–520. [Google Scholar] [CrossRef]
- Shin, J.; Tabatabai, D.; Boscardin, C.; Ferrone, M.; Brock, T. Integration of a Community Pharmacy Simulation Program into a Therapeutics Course. Am. J. Pharm. Educ. 2018, 82, 6189. [Google Scholar] [CrossRef]
- Phanudulkitti, C.; Leelakanok, N.; Nakpun, T.; Kittisopee, T.; Farris, K.B.; Vordenberg, S.E. Impacts of the dispensing program(MyDispense®) on pharmacy students’ learning outcomes with relevant perceptions: A quasi-intervention study. Thai J. Pharm. Sci. 2024, 48, 4. [Google Scholar] [CrossRef]
- Al-Diery, T.; Hejazi, T.; Al-Qahtani, N.; ElHajj, M.; Rachid, O.; Jaam, M. Evaluating the use of virtual simulation training to support pharmacy students’ competency development in conducting dispensing tasks. Curr. Pharm. Teach. Learn. 2024, 16, 102199. [Google Scholar] [CrossRef]
- Nguyen, K.T.; Dao, M.L.; Nguyen, K.N.; Nguyen, H.N.; Nguyen, H.T.; Nguyen, H.Q. Perception of learners on the effectiveness and suitability of MyDispense: A virtual pharmacy simulation and its integration in the clinical pharmacy module in Vietnam. BMC Med. Educ. 2023, 23, 790. [Google Scholar] [CrossRef]
- Amatong, A.J.; Asentista, H.; Diasnes, C.M.; Erispe, K.D.; Malintad, K.; Paderog, H.G.; Pangolima, Y.F.; Toledo, K.A.; Turtal, L.F.; Faller, D.E. Learners’ perceptions on MyDispense virtual simulation in the Philippines. Int. J. Innov. Res. Sci. Eng. Technol. 2022, 7, 1627–1636. [Google Scholar]
- Amirthalingam, P.; Hamdan, A.M.; Veeramani, V.P.; Ali, M.A.S. A comparison between student performances on objective structured clinical examination and virtual simulation. Pharm. Educ. 2022, 22, 466–473. [Google Scholar] [CrossRef]
- Dameh, M. A Report of Second Year Pharmacy Students’ Experience after Using a Virtual Dispensing Program. J. Pharma. Care Health Sys. 2015, S2. [Google Scholar] [CrossRef]
- Slater, N.; Mason, T.; Micallef, R.; Ramkhelawon, M.; May, L. Enabling Access to Pharmacy Law Teaching during COVID-19: Student Perceptions of MyDispense and Assessment Outcomes. Pharmacy 2023, 11, 44. [Google Scholar] [CrossRef]
- Miller, G.E. The assessment of clinical skills/competence/performance. Acad. Med. 1990, 65, S63–S67. [Google Scholar] [CrossRef]
- Benedict, N.; Smithburger, P.; Donihi, A.C.; Empey, P.; Kobulinsky, L.; Seybert, A.; Waters, T.; Drab, S.; Lutz, J.; Farkas, D.; et al. Blended simulation progress testing for assessment of practice readiness. Am. J. Pharm. Educ. 2017, 81, 14. [Google Scholar] [CrossRef]
- De Almeida Neto, A.C.; Benrimoj, S.I.; Kavanagh, D.J.; Boakes, R.A. Novel educational training program for community pharmacists. Am. J. Pharm. Educ. 2000, 64, 302–306. [Google Scholar] [CrossRef]
- Seybert, A.L.; Kobulinsky, L.R.; McKaveney, T.P. Human patient simulation in a pharmacotherapy course. Am. J. Pharm. Educ. 2008, 72, 37. [Google Scholar] [CrossRef]
- Gharib, A.M.; Bindoff, I.K.; Peterson, G.M.; Salahudeen, M.S. Exploring global perspectives on the use of computer-based simulation in pharmacy education: A survey of students and educators. Front. Pharmacol. 2024, 15, 1494569. [Google Scholar] [CrossRef]
- DeLucenay, A.; Conn, K.; Corigliano, A. An evaluation of the impact of immediate compared to delayed feedback on the development of counselling skills in pharmacy students. Pharm. Educ. 2017, 17, 322. [Google Scholar]
- Steuber, T.D.; Janzen, K.M.; Walton, A.M.; Nisly, S.A. Assessment of learner metacognition in a professional pharmacy elective course. Am. J. Pharm. Educ. 2017, 81, 6034. [Google Scholar] [CrossRef]
- Durand, E.; Kerr, A.; Kavanagh, O.; Crowley, E.; Buchanan, B.; Bermingham, M. Pharmacy students’ experience of technology-enhanced learning during the COVID-19 pandemic. Explor. Res. Clin. Soc. Pharm. 2023, 9, 100206. [Google Scholar] [CrossRef]
- Henning, K.; Ey, S.; Shaw, D. Perfectionism, the impostor phenomenon and psychological adjustment in medical, dental, nursing and pharmacy students. Med. Educ. 1998, 32, 456–464. [Google Scholar] [CrossRef]
- Barry Issenberg, S.; Mcgaghie, W.C.; Petrusa, E.R.; Lee Gordon, D.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med. Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef]
- Bindoff, I.; Ling, T.; Bereznicki, L.; Westbury, J.; Chalmers, L.; Peterson, G.; Ollington, R. A computer simulation of community pharmacy practice for educational use. Am. J. Pharm. Educ. 2014, 78, 168. [Google Scholar] [CrossRef]
- Wenzheng, W.; Lingmin, Y. The relationship between digital literacy and academic performance of college students in blended learning: The mediating effect of learning adaptability. Adv. Educ. Technol. Psychol. 2023, 7, 77–87. [Google Scholar] [CrossRef]
- Al-Dahir, S.; Bryant, K.; Kennedy, K.B.; Robinson, D.S. Online virtual-patient cases versus traditional problem-based learning in advanced pharmacy practice experiences. Am. J. Pharm. Educ. 2014, 78, 76. [Google Scholar] [CrossRef]
- Duffull, S.; Peterson, A.; Chai, B.; Cho, F.; Opoku, J.; Sissing, T.; Smith, D.; Tongskul, T.; Wilby, K. Exploring a scalable real-time simulation for interprofessional education in pharmacy and me. MedEdPublish 2020, 9, 240. [Google Scholar] [CrossRef]
| PICO | Definitions |
|---|---|
| Population (P) | Pharmacy Students |
| Intervention (I) | Any study that collects pharmacy students’ opinion, perception, satisfaction or attitudes on using MyDispense in a recognised pharmacy course |
| Comparison (C) | Any type of study, i.e., with/without a comparison group |
| Outcomes (O) | Pharmacy students’ perceptions on the barriers and facilitators to using MyDispense |
| Author (Year); Country | Description of Study Design | Study Participants | Study Outcomes | Method(s) of Data Collection | Identified Barrier(s) | Identified Facilitator(s) |
|---|---|---|---|---|---|---|
| Waghel et al. (2025) USA [34] | Prospective, mixed methods, comparative study Cross-sectional | Y1 PharmD students enrolled in a pharmacy skills lab course (n = 71) | To evaluate the correlation between previous pharmacy experience and performance on MyDispense E&O activities To evaluate students perceptions of MyDispense | Post-intervention questionnaire investigating prior pharmacy experience and MyDispense perceptions | Initial learning curve to use software IT incompatibilities | Provides high fidelity learning interactive environment Provides immediate feedback Easy to navigate |
| Phanudulkitti et al. (2024) Thailand [20] | Quasi-intervention study with two rounds Longitudinal | Y4 Pharmacy students enrolled in a Pharmacotherapeutic I course (n = 136) | To evaluate MyDispense impact on pharmacy students’ learning outcomes To evaluate students perceptions along with instructors views of MyDispense | A five part mixed methods survey Part three comprised of five closed-ended questions about MyDispense perceptions and one item for additional student feedback | Learning how to use software initially | Can practice dispensing skills at any time or place Provides feedback instantly at end of exercises |
| Al-Diery et al. (2024) Qatar [42] | Quantitative, prospective study Longitudinal | Y1 pharmacy students enrolled in a Professional Skills II course (n = 55) | To evaluate impact of MyDispense on students self-reported reaction, learning and accuracy in dispensing tasks | Pre-post intervention seven-point Likert scale surveys based on Kirkpatricks Model | Does not stimulate true patient-practitioner interactions | Offers immediate feedback Allows for practice in a safe virtual dispensing environment |
| Nguyen et al. (2023) Vietnam [43] | Mixed methods study with two phases Longitudinal | Y4 and Y5 pharmacy students enrolled at UMP Vietnam (n = 69) Pharmacists with at least one year clinical practice experience (n = 23) | To investigate learners’ perspectives on effectiveness of MyDispense in learning dispensing skills To investigate the suitability of MyDispense integration into clinical pharmacy curriculums in Vietnam | Online five-point Likert scale questionnaire (phase 1) Semi-structured interview (phase II) | Complicated learning process of software Inconsistent quality of product images | High degree of user interactivity Ability to self-learn by immediate feedback Diverse medication database |
| Rude et al. (2023) USA [35] | Quantitative, prospective study Longitudinal | Y1 PharmD students enrolled at NDSU and VCU (n = 142) | To assess the impact of a MyDispense simulation on students knowledge and confidence of OTC medications To assess overall student perceptions of the MyDispense activity | Pre-post activity survey with closed-ended demographic, confidence and knowledge-based questions with a five modified-scale perception questions in the post-survey. | May not be as effective as traditional learning methods | Effective way to learn new information Encourages active thinking |
| Tabulov et al. (2023) USA [36] | Quantitative, prospective study Longitudinal | Y1 PharmD students enrolled in a pharmaceutical skills 1 course (n = 64) | To describe a paediatric simulation on MyDispensecompleted by first year students To review student perceptions on confidence and knowledge learned after using MyDispense simulation | Pre-post online questionnaire with yes/no items and a five-point Likert scale | Initial learning curve with the software is timely which may impact student engagement with MyDispense | Low-stakes environment that allows students to make mistakes without harm More realistic than paper-based case learning |
| Slater et al. (2023) United Kingdom [47] | Mixed methods, prospective study Cross-sectional | Y2 MPharm students enrolled in a pharmacy law and ethics module (n = 147) | To evaluate the impact of MyDispense simulation on assessment performance To evaluate student perceptions of MyDispense | Online post-simulation 24 item survey consisting of closed-ended and Likert-scale questions aswell as open-ended questions. | Software layout could be improved Difficulties navigating software initially | Highly accessible and can practice dispensing skills from home Provides opportunity to repeat exercises |
| Faller et al. (2022) Philippines [44] | Mixed methods, retrospective study Cross-sectional | Filipino pharmacy students from four universites that implemented MyDispense into their pharmacy cirricula (n = 322) | To determine learners level of perception of MyDispense | Online three-part survey including demographics, five-point Likert scale and open-ended questions on student perceptions of the software | IT and web connectivity issues | High-fidelity learning environment without patient harm |
| Amirthalingam et al. (2022) Saudi Arabia [45] | Mixed-methods, prospective study Cross-sectional | Y4 pharmacy students enrolled in an Introductory Pharmacy Practice Experience 2 course (n = 69) | To compare pharmacy students performance on MyDispense vs in-person OSCEs To explore students perceptions of MyDispense | Post-simulation questionnaire with a five-point Likert scale and open-ended questions | Can be complicated to use Robotic in nature | Helps improve patient communication skills Enhances student confidence in patient care |
| Deneff et al. (2021) USA [37] | Two year, mixed methods, prospective study Cross-sectional | Y3 PharmD students enrolled in a pharmacy law and ethics course in 2017 (n = 38) and 2018 (n = 28) | To evaluate the utility of and student perceptions on the usefulness of MyDispense for pharmacy law instruction | A qualitative survey with a series of close-ended questions graded on a four- and five-point Likert Scale in 2017 and 2018 respectively and open ended questions; | Challenges learning software cases without a tutorial Some pharmacy law exercises may not be suitable for MyDispense | More engaging than traditional classroom teaching |
| Ambroziak et al. (2018) USA [38] | Prospective, quantitative, comparative study Longitudinal | Y1 PharmD students enrolled in a Pharmacy Practice Skills 1 course (n = 85) | To implement MyDispense cases into Pharmacy Practice Skills 1 To assess student perceptions of their learning using MyDispense | Pre simulation survey investigating prior pharmacy experience Post simulation survey investigating perceptions of MyDispense using open and closed ended questions | Learning how to navigate program | Effective tool to learn dispensing skills e.g. analysing prescriptions |
| Ferrone et al. (2017) USA [39] | Prospective, mixed methods study Cross-sectional | Y1 and Y3 PharmD students enrolled in UCSF, UConn, STLCOP (n =241) | To implement MyDispense simulation into US pharmacy curricula To assess student satisfaction of the MyDispense simulation | Post-simulation survey with a five-point Likert scale, demographic query on pharmacy experience and open-ended questions on perceptions | Can be difficult to learn at first May need to be adapted for different regions to be more realistic in nature | Straightforward to learn Affords opportunity to learn and make mistakes without harming patients More realistic than paper based cases |
| Shin et al. (2016) USA [40] | Comparative, quantitative study Longitudinal | Y2 PharmD students enrolled in a Therapeutics II course (n = 117) | To demonstrate feasibility of integrating MyDispense into a therapeutics course To measure students perceptions on MyDispense and its impact on their learning | Pre-case and post-case tests Three post-intervention quantitative surveys consisting of 10 to 17 items | Limited capacity to simulate interactions with prescribers and patients | Provides immediate feedback Can practice cases at any time or place Provides safe, low stakes practice environment |
| McDowell et al. (2016) Australia [26] | Retrospective, mixed methods study Cross-sectional | Y1 BPharm students enrolled in PAC1311 and PAC1322 modules at Monash University (n = 199) | To develop MyDispense for students to learn dispensing skills in a low-stakes environment To explore student perceptions of MyDispens as a learning tool | 38 item survey with five point Likert-scale questions and open ended questions | User interface is not responsive Technical and server connectivity issues | Learning support that allows “safe” dispensing without patient harm Stimulating learning environment |
| Dameh (2015) UAE [46] | Prospective, mixed-methods study Cross-sectional | Y2 female pharmacy students enrolled at FCHS (n = 33) | To report pharmacy students’ experience after using MyDispense | Survey consisting of five point Likert-Scale and open ended questions on student perceptions Focus group discussion to allow students to elaborate perceptions | Technical issues cause student frustration | Highly accessible and user friendly to students Gives dispensing practice prior to working in real-life scenarios |
| Category of Study Designs | MMAT Quality Criteria | Waghel et al. (2025) [34] | Phanudulikitti et al. (2024) [20] | Al-Diery et al. (2024) [42] | Nguyen et al. (2023) [43] | Rude et al. (2023) [35] | Tabulov et al. (2023) [36] | Slater et al. (2023) [47] | Faller et. al. (2022) [44] | Amirthalingm et al. (2022) [45] | Deneff et al. (2021) [37] | Ambroziak et. al. (2018) [38] | Ferrone et al. (2017) [39] | Shin et al. (2016) [40] | McDowell et al. (2016) [26] | Dameh et al. (2016) [46] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Qualitative | 1.1 | Y | Y | N/A | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | N/A | Y | Y |
| 1.2 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | |||||
| 1.3 | Y | CT | Y | Y | Y | Y | Y | CT | Y | Y | CT | |||||
| 1.4 | Y | Y | Y | Y | Y | Y | CT | CT | Y | Y | N | |||||
| 1.5 | CT | Y | Y | Y | Y | Y | Y | CT | Y | Y | N | |||||
| Quantitative Randomized Controlled Trials (RCTs) | 2.1 | N/A | Y | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Y | N/A | N/A |
| 2.2 | N | Y | ||||||||||||||
| 2.3 | Y | Y | ||||||||||||||
| 2.4 | N | N | ||||||||||||||
| 2.5 | Y | Y | ||||||||||||||
| Quantitative non-randomized | 3.1 | N/A | N/A | Y | N/A | Y | Y | N/A | N/A | N/A | N/A | N/A | N/A | Y | N/A | N/A |
| 3.2 | Y | Y | CT | Y | ||||||||||||
| 3.3 | Y | Y | CT | Y | ||||||||||||
| 3.4 | CT | CT | Y | Y | ||||||||||||
| 3.5 | Y | Y | Y | Y | ||||||||||||
| Quantitative descriptive | 4.1 | Y | N/A | N/A | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | N/A | Y | Y |
| 4.2 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||||||
| 4.3 | Y | Y | Y | CT | Y | Y | CT | Y | Y | Y | ||||||
| 4.4 | Y | Y | Y | Y | CT | CT | Y | Y | Y | CT | ||||||
| 4.5 | Y | Y | Y | Y | Y | Y | CT | Y | Y | N | ||||||
| Mixed Methods | 5.1 | Y | Y | N/A | Y | N/A | N/A | Y | Y | Y | Y | Y | Y | N/A | Y | Y |
| 5.2 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | CT | |||||
| 5.3 | Y | Y | Y | Y | Y | Y | Y | CT | Y | Y | N | |||||
| 5.4 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | CT | |||||
| 5.5 | Y | N | Y | Y | Y | Y | Y | CT | Y | Y | N |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collins, O.; McCarthy, R.; Sahm, L.J. Barriers and Facilitators of Using MyDispense from the Student Perspective: A Systematic Review. Pharmacy 2025, 13, 158. https://doi.org/10.3390/pharmacy13060158
Collins O, McCarthy R, Sahm LJ. Barriers and Facilitators of Using MyDispense from the Student Perspective: A Systematic Review. Pharmacy. 2025; 13(6):158. https://doi.org/10.3390/pharmacy13060158
Chicago/Turabian StyleCollins, Owen, Ruth McCarthy, and Laura J. Sahm. 2025. "Barriers and Facilitators of Using MyDispense from the Student Perspective: A Systematic Review" Pharmacy 13, no. 6: 158. https://doi.org/10.3390/pharmacy13060158
APA StyleCollins, O., McCarthy, R., & Sahm, L. J. (2025). Barriers and Facilitators of Using MyDispense from the Student Perspective: A Systematic Review. Pharmacy, 13(6), 158. https://doi.org/10.3390/pharmacy13060158








