Abstract
A monolayer of endothelial cells (ECs) lines the lumen of blood vessels and, as such, provides a semi-selective barrier between the blood and the interstitial space. Compromise of the lung EC barrier due to inflammatory or toxic events may result in pulmonary edema, which is a cardinal feature of acute lung injury (ALI) and its more severe form, acute respiratory distress syndrome (ARDS). The EC functions are controlled, at least in part, via epigenetic mechanisms mediated by histone deacetylases (HDACs). Zinc-dependent HDACs represent the largest group of HDACs and are activated by Zn2+. Members of this HDAC group are involved in epigenetic regulation primarily by modifying the structure of chromatin upon removal of acetyl groups from histones. In addition, they can deacetylate many non-histone histone proteins, including those located in extranuclear compartments. Recently, the therapeutic potential of inhibiting zinc-dependent HDACs for EC barrier preservation has gained momentum. However, the role of specific HDAC subtypes in EC barrier regulation remains largely unknown. This review aims to provide an update on the role of zinc-dependent HDACs in endothelial dysfunction and its related diseases. We will broadly focus on biological contributions, signaling pathways and transcriptional roles of HDACs in endothelial pathobiology associated mainly with lung diseases, and we will discuss the potential of their inhibitors for lung injury prevention.
1. Introduction
Acute lung injury (ALI) and its more severe manifestation, acute respiratory distress syndrome (ARDS), are triggered by a variety of external stimuli, ranging from bacterial or viral pneumonia and inhalation injuries (direct injury) to sepsis (indirect injury). As a result, dysfunction of the lung alveolar–capillary barrier, hyper-inflammation, atelectasis, pulmonary edema, hypoxia, and ultimately death can occur [,,,]. Despite a 27–45% mortality rate [], no pharmacological agents have been shown to improve outcomes in clinical trials in ARDS [,]. The current treatment guidelines rely on supportive management, including conservative use of fluids and airway maintenance, while controlling or resolving the inciting factor [,,]. New therapies targeting epithelial–endothelial barrier preservation may reduce vascular leak and have profound clinical benefits.
Endothelial cells (ECs) form the lining of all blood vessels and create a semi-selective barrier between blood and interstitium. Endothelial dysfunction has been previously identified as a prominent risk factor in cardiovascular diseases [] and ALI/ARDS [,]. Given the well-established understanding that SARS-CoV-2 or its spike protein causes endothelial dysfunction [], COVID-19 is widely recognized as an endothelial disease primarily affecting the microvasculature []. Overall, preventing EC barrier integrity is a critical clinical requirement for treating various acute and chronic lung diseases [,,].
Generally, the regulation of endothelial barrier integrity relies on an equilibrium between adhesive and contractile forces. Adhesive molecules present at the cell–cell and cell-matrix junctions provide EC barrier integrity and a scaffold for contractile machinery based on the actomyosin interaction; alterations at these junctions are primarily responsible for EC barrier disruption [,]. The tight interconnection between the endothelial cells is provided by the interaction of junctional proteins (occludins, zonula occludens-1 (ZO-1), catenins, and vascular endothelial cadherin (VE-cadherin), which are linked to the actin cytoskeleton of cells in its vicinity [,]. Consequently, any alterations in the dynamics of the actin cytoskeleton or/and the activation state of the EC contractile machinery can influence the stability of cell–cell junctions and may result in barrier dysfunction. Hence, the dysregulation of the endothelial barrier function is crucial (reviewed in [,]) in lung-related pathologies.
The tensegrity model proposed by Ingber and coworkers [] highlights how the interconnected cytoskeletal components experience tension and compression, allowing cells to sense mechanical forces via specialized mechanoreceptors. Such mechanoreceptors can be found in the lungs and are known as rapidly adapting receptors []. Various mechanosensors, such as ion channels, integrins, focal adhesions, and cytoskeletal complexes, enable cells to respond to both external and internal mechanical perturbations. This mechanism is crucial in cell functions like spreading, migration and overall cellular responses. For instance, endothelial cells in the microvasculature receive mechanical stretch through integrins from the capillary wall, while focal adhesions link the actin cytoskeleton to the cell’s interface with the extracellular matrix. They are vital players in regulating the integrity of the EC barrier as they provide additional tethering forces. ECs require cell–cell contact and enrolment of VE-cadherin-based junctional protein complex to convert the stretch into signals that promote their proliferation [] and to initiate mechanosensitive signaling cascades in the vascular endothelium [,].
Epigenetic mechanisms have recently been implicated as a significant regulator of endothelial barrier function [,,]. Histone post-translational modifications (PTMs) allow ECs to respond to intra- and extracellular stimuli []. One of the most prevalent reversible post-translational protein modifications is acetylation, or more correctly, Nε acetylation, and is governed by two classes of regulatory enzymes: (i) lysine acetyltransferases (KATs), also known as histone acetyltransferases (HATs). KATs/HATs facilitate the transfer of an acetyl group to a Lysine (Lys) residue, and (ii) lysine deacetylases (KDACs) or histone deacetylases (HDACs) catalyze the removal of acetyl groups. In simplified terms, these enzymes add or remove acetyl groups from histones. Their mode of action is illustrated in Figure 1. HDACs can be classified into two subgroups: zinc-dependent histone deacetylases (Class I, IIa, IIb, and IV HDACs) and NAD+-dependent sirtuins (Class III HDACs). It has been shown that HDACs from both subgroups can regulate EC function at various levels and by diverse mechanisms [,,]. Precise functional tuning of HDACs may be achieved by PTMs like phosphorylation, SUMOylation, etc. [,]. In addition to deacetylating histones, HDACs also deacetylate other non-histone proteins, which regulate cellular functions such as cytoskeletal polymerization and signal transduction [,]. A summary of the classification, structural features, and role of HDACs in EC function is provided in Table 1 [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]. The structural, functional, and inhibitory aspects of zinc-dependent HDACs have recently been reviewed by Porter and Christianson [].
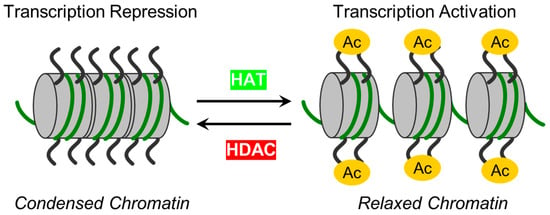
Figure 1.
The schematic illustrates enzymes responsible for reversible protein acetylation in the regulation of gene transcription. Two classes of regulatory enzymes, lysine acetyltransferases (KATs)/histone acetyltransferases (HATs) and lysine deacetylases (KDACs)/histone deacetylases (HDACs), govern the reversible post-translational Nε acetylation of Lys residues in proteins. While KATs/HATs facilitate the addition of acetyl group to Lys residues and promote chromatin unfolding (relaxed chromatin), thus facilitating the activation of transcription, KDACs/HDACs catalyze acetyl group removal from histone and non-histone targets and are responsible for chromatin condensation (repression of transcription).

Table 1.
Classification, structural features, and functions of zinc-dependent HDACs in vasculature.
Compelling evidence suggests that dysregulation of protein acetylation can ultimately promote the emergence of several diseases, including ALI. Therefore, maintaining the balance between the activities of HATs and HDACs is critical for vascular homeostasis []. A recent review by Shvedunova and Akhtar explored various dimensions of acetylation and deacetylation, including their diverse targets, rapid turnover, and sensitivity to the concentrations of co-factors like acetyl-CoA, acyl-CoA, and NAD+, highlighting their close relationship with metabolism and homeostasis [].
In addition to the direct de-acetylation of histones, HDACs play a role in epigenetic regulation as co-factors in many transcriptional processes [,]. Specific transcription factors mainly enlist them and are essential for maintaining vascular homeostasis and facilitating the development of blood vessels []. The dysregulation of HDAC expression and activity has been observed in numerous cardiovascular diseases like chronic obstructive pulmonary disease (COPD) [], asthma [], and cardiac hypertrophy []. Consequently, HDAC inhibitors have emerged as potential therapeutic targets to cope with these diseases [].
A growing body of evidence indicates that inhibition of zinc-dependent HDACs leads to the preservation of EC barrier function and can be beneficial for treating cardiovascular and inflammatory diseases [,]. However, the roles of individual HDACs in EC barrier regulation in vitro and in vivo are largely unspecified. In this review focusing on vascular pathobiology (mainly in ALI, ARDS, angiogenesis, and CVD), we discuss and highlight the importance of zinc-dependent HDACs in the maintenance and regulation of endothelial barrier integrity, mechanisms, and core signaling pathways modulating endothelial cell functions. Further, we provide an overview of current HDAC research, and we evaluate possible therapeutic approaches and treatment strategies involving HDAC inhibitors to improve EC dysfunction.
2. Zinc-Dependent HDACs: Classification, Functions, Regulations and Modulations
To date, 18 mammalian HDACs have been discovered. Initially, they were divided into four classes based on their homology to yeast HDACs, but later on they were subdivided into two major groups: (i) “classical” zinc-dependent enzymes, which require zinc ion (Zn2+) as a co-factor for their catalytic function (classes I, II, IV) and (ii) sirtuins (class III), which are nicotinamide adenine dinucleotide (NAD+)-dependent enzymes [,]. This review will focus on the role of the “classical” HDACs in endothelial pathobiology. For this group, the presence of Zn2+ in the active site of HDAC provides an appropriate conformation for the catalytic domain, thus facilitating interaction and deacetylation of the substrate []. Zn2+ allows a nucleophilic attack of the H2O molecule on the acetyl group, thus promoting the removal of the acetyl moiety []. Therefore, the presence of Zn2+ is essential for the proper folding and stability of “classical” HDACs and their enzymatic activity [,]. The main molecular and structural characteristics of Zn-dependent HDACs are provided in Figure 2 and Figure S1.
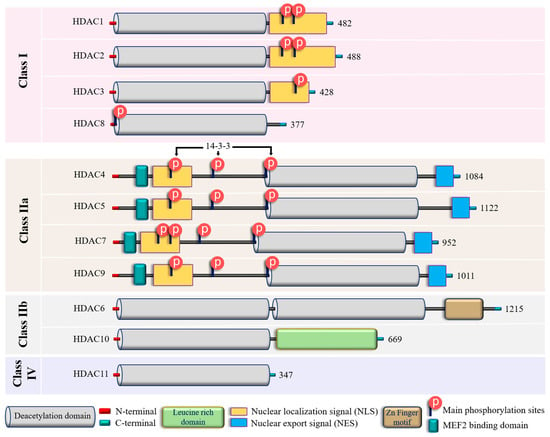
Figure 2.
Structural features of zinc-dependent HDACs. The schematic depicts the main structural peculiarities of zinc-dependent HDACs. See the text for further explanation. Additional information on HDACs secondary and tertiary structures is provided in Supplementary Figure S1.
In addition to their homology to yeast counterparts, “classical” zinc-dependent HDACs can be distinguished based on their structural features, subcellular locations and active mechanisms (Figure 2 and Figure S1; Supplementary Table S1). Class I HDACs (HDAC1, HDAC2, HDAC3, and HDAC8) have high homology to the yeast RPD3 gene [,,] and are characterized by the presence of the conservative catalytic domain with N-and C-terminal extensions. The latter includes a Nuclear Localization Sequence (NLS) with regulatory phosphorylation sites (for HDAC1, HDAC2, and HDAC3) (Figure 2). These HDACs are ubiquitous enzymes that are primarily localized in the nucleus and have high catalytic activity against histones [,]. In addition, they can be involved in chromatin remodeling as an enzymatically active subunit of multi-protein complexes (functional interactomes), which include other HDACs and transcription factors [,]. Class II HDACs are homologous to the Hda1 gene [,] and can be present in both the nucleus and the cytoplasm. Compared to class I enzymes, they are more spatiotemporally regulated with more evident tissue and cell-restricted expression patterns [,] (Table 1). They are subdivided into class IIa and IIb subclasses (Figure 2). Class IIa HDACs (HDAC4, HDAC5, HDAC7, and HDAC9) are characterized by a unique N-terminal extension, which includes a binding site for the transcription factor MEF2, NLS, and three conservative phosphorylation sites. These sites regulate HDAC critically with a 14-3-3 protein chaperones, and 14-3-3 are responsible for cytoplasmic sequestration []. Additionally, class IIa HDACs have a C-terminal extension, which contains a Nuclear Export Signal (NES) (Figure 2). Therefore, class IIa HDACs can shuttle between the nucleus and cytoplasm. They primarily act as co-repressors of transcriptional events in the nucleus and have minimal deacetylase activity on acetylated histones [,,]. However, cumulative evidence indicated they can deacetylase non-histone proteins [,] (Table 1). Class IIb HDACs (HDAC6 and HDAC10) possess two tandem deacetylase domains. However, in the case of HDAC10, the C-terminal (or Leu-rich) domain is truncated and lacks its enzymatic activity [,,] (Figure 2). Unlike HDAC6, which is usually a cytoplasmic deacetylase, HDAC10 resides in both the nucleus and cytoplasm [,] (Table 1). HDAC11 is the only member of class IV HDACs and has a catalytic core homology with both class I and II enzymes. It is characterized by short N- and C-terminal extension and a unique ability to deacetylase fatty acids []. HDAC11 defatty-acylase activity is about 10,000 times more efficient than its deacetylase activity [].
Initially, HDACs were discovered as enzymes that catalyze the removal of ε-N-acetyl groups from histones, modulating gene transcription (Figure 1). Later research revealed that HDACs can deacetylate non-histone proteins such as p53, signal transducers and activators of transcription (STAT3), E2F1, heat shock protein 90 (Hsp90), and NF-κB [] (Table 1). The deacetylation process driven by HDACs executes chromatin compaction and transcriptional repression, while histone acetylation accelerates chromatin accessibility and triggers the activation of gene transcription [] (Figure 1). The acetylation and deacetylation of proteins may impact the target proteins’ stability, activity, localization, and interactions []. The reversible protein acetylation may indirectly affect other PTMs through mechanisms like crosstalk between PTMs, protein-protein interactions, recruitment of modifying enzymes, etc. In short, zinc-dependent HDACs are evolutionally conserved enzymes that epigenetically regulate gene expression in numerous cellular pathways (reviewed in [,]). Reversible protein acetylation and other PTMs, like phosphorylation, methylation, ubiquitination, etc., are the core mechanisms regulating protein function []. A large body of evidence indicates that the vast majority of signaling cascades involved in cell cycle progression, proliferation, apoptosis, survival, differentiation, development, angiogenesis, and inflammatory actions are regulated by the zinc-dependent HDACs [,,].
3. Zinc-Dependent HDACs in Endothelial Function
3.1. Class I HDACs: HDAC1, HDAC2, HDAC3, and HDAC8
Emerging evidence implied that zinc-dependent HDACs are actively involved in the function as well as in the dysfunction of the endothelial lining [,]. However, the role of specific HDAC subtypes remains incompletely defined and somewhat contradictory. For example, a recent study demonstrated that nuclear class I HDACs—HDAC1 and HDAC2, but not nuclear/cytoplasmic HDAC3—are involved in lung microvascular EC barrier dysfunction induced by lipopolysaccharide (LPS) via the suppression of Sox18 gene expression []. However, another study demonstrated that the pharmacological inhibition of HDAC1, HDAC2, and HDAC3 leads to EC barrier dysfunction in mice and increased lung vascular leak by suppression of EC Roundabout4 (Robo4) receptor expression []. In addition, published data demonstrated that specific inhibition of HDAC1, HDAC2, and HDAC3 induces F-actin stress fibers in Human Umbilical Vein ECs (HUVECs) and suggested that down-regulation of these HDACs is involved in Bacillus anthracis lethal toxin (LT)-induced HUVEC barrier dysfunction []. Further, one group demonstrated that the overexpression of HDAC2 in human aortic ECs mitigated the oxidized low-density lipoprotein (OxLDL)-mediated vascular dysfunction induced by endothelial Arginase 2 (Arg2). This occurred via the direct binding of HDAC2 with the Arg2 promotor [], and protects against EC dysfunction and atherogenesis induced by oxidized lipids in mice []. A study from another group indicated that upregulation of HDAC2 promotes EC dysfunction in mice and humans via repressing the expression of Manganese superoxide dismutase (MnSOD), thus increasing oxidative stress []. In addition, pro-inflammatory cytokines like TNF-α and IL-1β induce inflammation and EC dysfunction, at least in part, via down-regulation of RNAse1 in an HDAC2-dependent manner in HUVECs []. Interestingly, the known EC barrier-enhancing lipid mediator, sphingosine-1-phosphate (S1P) [], can bind to HDAC1 and HDAC2 and inhibit their enzymatic activity []. Thus, the involvement of class I HDACs in endothelial function may be agonist- and tissue-specific. Accordingly, a recent review highlighted the regulatory role of a class I HDAC, HDAC1, as an environmental sensor that drives functions of ECs like inflammatory and NO signaling, redox balance, and angiogenesis in an agonist-specific manner [].
The nuclear/cytoplasmic enzymes HDAC3 and HDAC8 also regulate EC function in cell- and agonist-specific fashion. In human lung microvascular ECs (HL-MVECs), LPS modestly but significantly increases HDAC3 activity. Inhibition of HDAC 3 (in tandem with HDAC6) protects against LPS-induced EC barrier dysfunction in vitro and in vivo, apparently via acetylation and suppression of heat shock protein 90 (Hsp90) chaperone function and attenuation of RhoA activity []. Accordingly, the downregulation of HDAC3 protects blood-brain barrier (BBB) integrity in oxygen-glucose deprivation/reoxygenation states by promoting PPARγ activation [] in brain ECs. It prevents BBB leakage in type II diabetic mice via activation of the nuclear factor erythroid 2 (NFE2)-related factor 2 (Nrf2) [], which controls the cellular resistance to oxidants []. It has also been found that the mitigation of HDAC3 combats Type 2 diabetes mellitus-induced endothelial dysfunction via the Keap1-Nrf2-Nox4 signaling pathway [].
However, HDAC3 plays a somewhat contrasting role in atherosclerosis development, which is tightly linked with endothelial dysfunction []. While HDAC3 is critical for maintaining endothelial layer integrity in the areas of disturbed flow in atherosclerosis [], its up-regulation is involved in inflammatory responses in HUVECs and pharmacologic inhibition of HDAC3 mitigates the development of atherosclerotic lesions in mice []. Interestingly, distinct roles for class I and IIa HDACs in regulating gene expression and EC signaling in response to disturbed flow were noted [], thus highlighting the functional differences between HDACs.
While the role of HDAC8 in EC function is mainly unknown, emerging evidence demonstrated the association of this enzyme with cytoskeletal proteins responsible for smooth muscle contractility, such as α-actin [] and cortactin []. The latter protein actively participates in EC barrier regulation (reviewed by Bandela et al. []). However, the role of HDAC8-mediated cortactin deacetylation in EC barrier regulation remains to be elucidated.
3.2. Class IIa HDACs: HDAC4, HDAC5, HDAC7, and HDAC9
These HDACs have a more restricted expression patterns compared to class I HDACs and some unique structural and functional features (listed in Figure 2), which allow them to shuttle between the nucleus and the cytoplasm. They are recognized for their involvement in endothelial cell migration, angiogenesis, inflammation, and embryonic development [,,]. Recently published data indicated that the pan-class IIa inhibitor, TMP269, improves EC barrier function in an LPS-induced murine ALI model in vivo and in HLMVECs in vitro []. Since this inhibitor selectively binds to the catalytic site of class IIa HDACs [], this data suggested that the catalytic activity of this HDAC group may play a role in EC barrier regulation despite the minimal activity against acetylated histones []. The effect of TMP269 can be attributed to the activation of the Rho pathway, which may occur, at least in part, via de-repression of adapter protein ArgBP2 (Arg-binding protein 2) transcription []. However, the role of individual class IIa HDACs, as well as the role of nuclear/cytoplasmic shuttling, was not specified.
HDAC4, a “gold standard” in class IIa HDACs research, is linked to early stress response in pulmonary fibrosis. At the same time, HDAC2 is responsible for chronic progression, suggesting that these HDACs may regulate gene expression of pro-inflammatory cytokines and fibronectin in concert []. Additionally, by triggering autophagy, HDAC4 regulates vascular inflammation []. The activation of HDAC4 prevented endothelial dysfunction in diabetes []. A transcription factor, specificity protein-1, i.e., SP1, reduces intestinal barrier dysfunction, oxidative stress, and inflammatory response after sepsis by upregulating HDAC4 while inhibiting the high mobility group box one protein (HMGB1) expression []. Long noncoding RNA cancer susceptibility candidate 11 (lncRNA CASC11) alleviates ox-LDL-induced injury (inflammation and apoptosis) in coronary microvascular ECs, at least in part, by stabilizing HDAC4 []. Therefore, while the information on the involvement of HDAC4 in EC barrier regulation is limited, published data suggests that HDAC4 may have an anti-inflammatory and barrier-protective role in ECs.
Vascular endothelial growth factor and its receptor (VEGF and VEGFR, respectively) are primary drivers of angiogenesis in ECs [,]. There is a direct correlation between HDAC4 phosphorylation and VEGF signaling. The HDAC4 phosphorylation can improve the motility of ECs. Insights on phosphorylated HDAC4 in angiogenesis are provided by Liu et al. []. Nox4 oxidizes HDAC4 and enhances its phosphorylation; thus, this cascade facilitates proper tube formation by ECs []. HDAC4, HDAC5, and HDAC6 control VEGFR-2 expression [], and its deacetylation in ECs directly impact EC function []. In a study conducted by Urbich et al., HDAC5 was recognized as a suppressor of angiogenic gene expression in HUVECs []. Consistently, HDAC5 impairs angiogenesis in scleroderma ECs []. Recent data indicated that HDAC5 may be involved in LPS-induced inflammatory responses in human pulmonary artery ECs (HPAECs) [].
The literature suggests that HDAC7 is perhaps the most distinct of all class IIa HDACs []. For example, unlike other class IIa HDACs, it may primarily be localized in the cytosol in specific cell types []. Further, the pro- or anti-angiogenic function of HDAC7 is dependent upon its cellular localization []. The role of HDAC7 in endothelial permeability remains controversial. While a recent study implicated the involvement of HDAC7 in E. coli-induced ALI in mice [], the classical work of Dr. Olson’s group demonstrated that HDAC7 maintains vascular endothelial integrity during embryogenesis via downregulation of the expression of matrix metalloproteinase 10 (MMP-10) []. The small interfering RNA (siRNA)-based knockdown of Filamin B can reduce VEGF-induced HDAC7 cytosolic accumulation, repressing MMP-10 and NUR 77 genes and inhibiting VEGF-mediated vascular permeability []. A peptide (7A) derived from HDAC7 was reported as a driver for vascular regeneration through phosphorylation of 14-3-3γ []. In addition, the maintenance of the vascular lumen is dependent on the phosphatase 2A/HDAC7/ArgBP2 pathway, which controls the endothelial cytoskeletal dynamics and cell-matrix adhesion in zebrafish and cultured HUVECs []. Data from the literature indicates that dephosphorylation of HDAC7 by myosin light chain (MLC) phosphatase (MLCP) regulates nuclear import of HDAC7 in thymocytes, suggesting the role of MLCP/HDAC7 crosstalk in cytoskeletal remodeling in non-muscle cells []. MLCP plays a vital role in EC cytoskeletal remodeling, leading to EC barrier strengthening [,]. However, the role of HDAC7 in regulating MLCP activity/EC barrier function is unknown. It was shown that ectopically expressed HDAC7 complexes with β-catenin and 14-3-3 retain β-catenin in the cytoplasm, thus inhibiting HUVEC proliferation []. On the contrary, a recent study demonstrated that upregulation of HDAC7 increased β-catenin acetylation at Lys 49 accompanied by decreased phosphorylation at Ser 45, thus facilitating its nuclear import and proliferation in lung cancer cell lines [], suggesting a cell-specific role of HDAC7 in the regulation of cell growth.
While the role of HDAC9 in lung endothelial function is largely unknown, it was shown that it can worsen endothelial injury in a cerebral ischemia/reperfusion model via increasing inflammatory activity and endothelial barrier dysfunction []. HDAC9 was identified as a responsible factor since it triggered the IκBα/NF-κB and MAPKs signaling pathways, leading to the promotion of brain ischemic injury [], and it was involved in brain EC injury associated with intracranial aneurism by repressing miR 34a expression []. Interestingly, HDAC9 may play a pro- or anti-inflammatory role, depending on the cell type investigated []. Therefore, the role of class IIa HDACs in endothelial function is complex and apparently tissue- and agonist-specific.
3.3. Class IIb HDACs: HDAC6 and HDAC10
HDAC6 is known for its effects on cytoskeletal dynamics and cell–cell junctions as well as for regulation of EC mechanosensing and permeability [,,,,]. As demonstrated by studies conducted by Gao et al. [] and Zhang et al. [], HDAC6 controls cell motility by governing tubulin and actin networks. HDAC6 is directly deacetylated α-tubulin at Lys 40 [], thus promoting MT disassembly in human pulmonary ECs []. However, it may affect MT dynamics independently from its deacetylase activity []. It is also demonstrated that HDAC6 plays a regulatory role in endothelial cell migration and angiogenesis via deacetylation of the actin-binding protein cortactin []. In addition, HDAC6 stimulates angiogenesis through polarization and migration of vascular ECs in a microtubule end-binding protein 1 (EB1)-dependent fashion []. The involvement of HDAC6 in EC barrier regulation is well documented due, at least in part, to the discovery of HDAC6-specific inhibitors (reviewed by Zhang et al., []). In many cases, downregulation or pharmacological inhibition of HDAC6 attenuates the increase in EC permeability induced by pro-inflammatory agonists or edemagenic microorganisms [,,,,,]. However, mechanisms are varied and may be agonist-specific. They may include microtubule destabilization accompanied by deacetylation of tubulin [,,] and β-catenin, followed by disruption of adherens junctions [] and activation of Rho-mediated contractile machinery [,]. In particular, Staphylococcus aureus-induced EC inflammation and barrier dysfunction is mediated by an increased level of reactive oxygen species (ROS), with subsequent HDAC6 activation followed by MT destabilization, which triggers the activation of the nucleotide exchange factor GEF-H1/Rho pathway []. In addition, recent data suggests that HDAC6 may activate Rho by either deacetylation (inhibition) of Rho GDP-dissociation inhibitor (RhoGDI) or upregulation of ArgBP2 expression [,]. ROS-mediated HDAC6 activation accompanied by HDAC6 phosphorylation at Ser 22 is involved in the disruption of EC barrier integrity induced by cigarette smoke []. Collectively, this data supported the multifaceted role of HDAC6 in EC barrier dysfunction. However, recently published data demonstrates that in primary HLMVECs derived from neonatal lungs and in a neonatal murine model of sepsis, downregulation of HDAC6 exacerbates LPS-induced pro-inflammatory responses via upregulation of canonical toll-like receptor (TLR) signaling, suggesting an anti-inflammatory role of HDAC6 in the development of lung pathology during systemic sepsis []. Therefore, the role of HDAC6 in various ALI models requires further investigation.
Along with HDAC6, HDAC10 plays an essential role in Hsp90-mediated proteasomal degradation and regulation of VEGF receptors []. A recent study demonstrated that HDAC10 promotes angiogenesis in HUVECs via the PTPN22/ERK axis []. In some cell types, up-regulation of HDAC10 is linked to pro-inflammatory responses [,]. However, the downregulation of HDAC10 exacerbates NLRP3-mediated inflammatory responses in intracerebral hemorrhage (ICH)-induced injury []. Further, a newly published study demonstrated that nebulized inhalation of HDAC10 attenuates oxidative stress, inflammation, and pulmonary fibrosis in a murine model of silicosis, suggesting an anti-inflammatory role of HDAC10 in lung injury []. The role of HDAC10 in lung EC barrier function remains to be elucidated.
3.4. Class IV HDAC: HDAC11
HDAC11 is the most recently discovered zinc-dependent HDAC [] and the only member of class IV HDACs with some unique features (listed in Figure 2). The high expression of HDAC11 is associated with poor prognosis in non-small cell lung cancer []. HDAC11 is also critically involved in metabolic diseases, including obesity and diabetes (reviewed in []). In particular, acetaldehyde and the NF-κB pathways regulate the levels of HDAC11 in alcoholic liver disease. Further, the downregulation of HDAC11 decreased IL-10 levels, which increased TNF-α levels, thus promoting inflammation []. Accordingly, recent studies demonstrated that TNF-α increases the expression of HDAC11 in HUVECs, resulting in the activation of NLRP3/caspase-1/GSDMD and caspase-3/GSDME signaling cascades and culminating in pyroptosis, an inflammatory type of cell death involved in atherosclerosis [,]. Proteinase-activated Receptor-2 (PAR2)-induced HUVECs barrier compromise involves repression of VE-cadherin expression via upregulation of HDAC11 []. This data supported the involvement of HDAC11 in inflammatory responses and EC barrier compromise. Interestingly, the initial characterization of HDAC11 revealed that the enzyme co-immunoprecipitates with HDAC6, suggesting the formation of a functional complex []. However, the role (if any) of a potential HDAC11/HDAC6 interaction in EC function requires further investigation.
4. EC-Mediated Central Signaling Cascades and Their Regulation by Zinc-Dependent HDACs
Zinc-dependent HDACs contribute to vascular pathobiology through multiple mechanisms, such as impairing the production of nitric oxide (NO), increasing oxidative stress, triggering severe inflammatory cascades, differentiation, proliferation, apoptosis, altering integrity of ECs, modulating vascular tone and angiogenesis [,,,]. Broadly simplified links between HDACs and vascular regulatory mechanisms are presented in Figure 3. The engagement of class I HDACs in overall cellular proliferation, differentiation, and development is reviewed by Reichert et al. []. Class I and II HDACs were studied in ECs with regard to inflammation, oxidation, and proliferation-related signaling cascades and mRNA, i.e., gene expression studies, and interpreted as prominent therapeutic targets in EC dysfunction [].
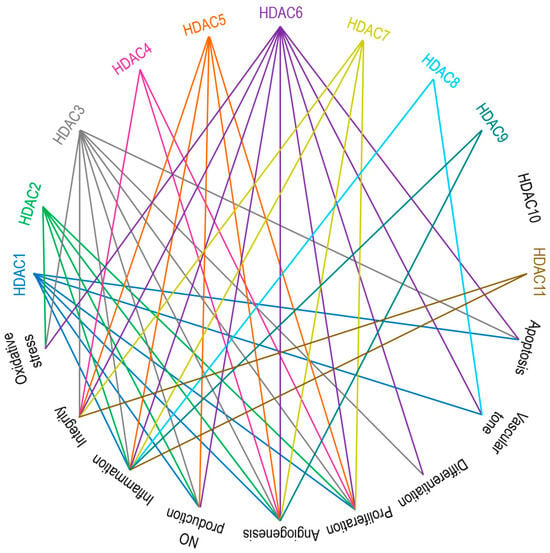
Figure 3.
Main endothelial signaling pathways mediated by zinc-dependent HDACs. HDAC1, HDAC3, and HDAC6 are involved in apoptosis. HDAC1, HDAC6, and HDAC8 are responsible for vascular tone. HDAC3 and HDAC6 control cell differentiation. HDACs 1 to 7 participate in cell proliferation. Except for HDAC8, HDAC10, and HDAC11, all other zinc-dependent HDACs drive angiogenesis. HDAC1, HDAC2, HDAC3, HDAC5, and HDAC6 regulate NO production. Aside from HDAC4 and HDAC10, the rest of the zinc-dependent HDACs are involved in inflammatory responses. HDACs 3 to 7 and HDAC11 are the key players accounting for the regulation of cell integrity. HDAC2, HDAC3, and HDAC6 are contributors to oxidative stress. See the text for further explanations and references.
In particular, HDACs can epigenetically modulate the activity of regulators (cyclins, cyclin-dependent kinases, p53, etc.) involved in cell cycle progression and proliferation [,]. Under pathological circumstances (e.g., stress, injury, hypoxia, etc.), ECs tend to migrate and proliferate, thus disturbing EC barrier integrity [,]. HDAC1 to HDAC7 are active participants in these pathomechanisms []. Accordingly, HDAC inhibitors, such as SAHA (suberoylanilide hydroxamic acid, vorinostat) [], trichostatin A (TSA), apicidin [], and tubacin [], were reported to overcome barrier dysfunction and restrict EC proliferation. Interestingly, in cancer cell lines, HDAC3 and HDAC8 downregulate the expression of SIRT7, thus facilitating proliferation [,] and suggesting a possible crosstalk between zinc-dependent and NAD+-dependent (class III) HDACs in the regulation of cell proliferation.
In apoptosis and cell survival pathways, HDACs affect the expression of pro-apoptotic and anti-apoptotic genes, thus maintaining the equilibrium between cell death and survival signals []. Apoptosis has been linked to several cardiovascular diseases, and a positive correlation between an increased EC apoptosis and the development and progression of cardiovascular diseases has been established [,,,]. In a HUVEC model of disturbed flow (atherosclerosis), β-catenin positively regulates endothelial nitric oxide synthase (eNOS) activity and anti-apoptotic gene expression []. In turn, β-catenin activity and cellular location are controlled by HDAC7 in HUVECs, suggesting the involvement of HDACs in β-catenin-mediated EC proliferation and survival []. HDAC1 and HDAC2 modulate the expression of endothelial VCAM-1 and atherogenesis by mechanisms that downregulate the methylation of the GATA6 promoter by blocking STAT3 acetylation []. HDACs are considered an epigenetic factor in the modulation of vascular endothelium-related atherosclerosis and flow []. MicroRNA-200b-3p can induce EC apoptosis in atherosclerosis by encountering HDAC4 []. The involvement of HDACs in atherosclerosis, emphasizing the regulation of endothelial cell function, is reviewed by Chen et al. [].
Cellular differentiation, development processes, and angiogenesis (VEGF and its receptors) are also epigenetically controlled by HDACs []. Hrgovic et al. explained that the anti-angiogenic action of HDAC inhibitors like TSA, sodium butyrate (But), and valproic acid (VPA) by VE-cadherin-dependent mechanism suppresses VEGFR-2 expression []. HDAC1, HDAC4, HDAC5, and HDAC6-mediated suppression is a crucial target for anti-angiogenic drug development.
Inflammatory events promote injury, vascular dysfunction, and a breach in EC barrier integrity. Most of the time, the inflammation and its regulation are HDAC-dependent [,,]. In particular, HDACs modulate the expression of genes encoding inflammatory cytokines, chemokines, and adhesion molecules, thereby affecting the inflammatory cascades, including the NF-κB pathway [,,,]. In 2019, Bedenbender et al. elucidated how inflammatory cytokines hindered the equilibrium of endothelial RNase1-eRNA homeostasis, which buffers against different vascular pathologies []. They reported that the inflammatory stimulation of ECs facilitates HDAC2 activation, which subsequently leads to H4 and H3K27 deacetylation (within the promoter region of RNASE1). The vascular architecture disturbs the vascular inflammation (TNF-α) driven by HDAC1, HDAC2, HDAC3, HDAC5, HDAC6, HDAC7, HDAC8, HDAC9, and HDAC11 [,,]. The functional roles of HDACs in CVD-related inflammations are reviewed by Kulthinee et al. [].
ROS, oxidative stress, and uncoupling of endothelial nitric oxide synthase (eNOS) are the critical components for inducing endothelial dysfunction []. HDAC2, HDAC3, and HDAC6 are associated with oxidative stress/ROS production []. HDAC4/HDAC5-HMGB1 mediated signaling, facilitated by the activity of NADPH oxidase, plays a vital role in cerebral ischemia/reperfusion injury or ischemic stroke []. HDACs like HDAC1, HDAC2, HDAC3, HDAC5, and HDAC6 and their inhibitors were shown to modulate NO production [].
5. Therapeutic Targeting of Zinc-Dependent HDACs in Lung Injury
The broad relationship between zinc-dependent HDACs and their inhibitors is shown in Figure 4. A deeper understanding of the structural features, selectivity and capability of various HDAC inhibitors was reviewed by Roche and Bertrand []. These authors have summarized the advancements made by chemists in designing more specific and effective compounds and distinguished their behavior within target molecules. Briefly, HDAC inhibitors are subdivided into four classes based on their chemical structure: hydroxamate, cyclic peptide, benzamide, and aliphatic acids (Figure 4). TSA, belinostat, panobinostat, and vorinostat (SAHA) belong to the hydroxamate class. Among these, pan-HDAC inhibitors, such as TSA and vorinostat, are canonical zinc-dependent HDAC inhibitors that inhibit HDAC1 to HDAC9 with about equal potency []. Depsipeptide belongs to the cyclic peptide class. Inhibitors classified as benzamides, MS-275 (etinostat) and MGCD0103 (mocetinostat) are usually considered to target HDAC1, HDAC2, HDAC3, and HDAC8 (class I HDACs). 4-Phenylbutyric acid (phenylbutyrate), sodium butyrate (sodium salt of butyric acid), and valproic acid (valproate) are characterized as aliphatic acids (Figure 4). In general, zinc-dependent histone deacetylase inhibitors share similar pharmacophores that consist of three essential components: a cap group, a linker, and a zinc-binding domain.
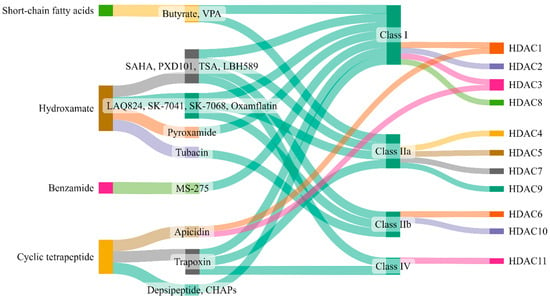
Figure 4.
Zinc-dependent HDACs and their inhibitors. This figure (made at SankeyMATIC.com) illustrates four distinct classes of HDAC inhibitors: aliphatic acids, hydroxamate, benzamide, and cyclic peptide. Among these, trichostatin A (TSA), belinostat, panobinostat, and vorinostat are hydroxamate inhibitors, with TSA being the most extensively studied. Depsipeptide falls within the cyclic peptide class. Notably, the inhibitors MS-275 (etinostat) and MGCD0103 (mocetinostat) target HDAC1, HDAC2, HDAC3, and HDAC8, classified as class I HDACs, and are categorized as benzamides. Aliphatic acids encompass 4-phenylbutyric acid (phenyl butyrate), sodium butyrate (sodium salt of butyric acid), and valproic acid (valproate).
The potential role of HDAC inhibitors as therapeutic agents in the treatment of a wide variety of diseases has been established (reviewed by Li et al. [] in 2019 and Li et al. [] in 2022). HDACs have recently been suggested as promising potential targets for treating cardiac diseases []. HDAC inhibitors are also reviewed in treating sepsis and inflammatory pulmonary diseases [,]. Table 2 summarizes broad knowledge of the role of HDAC inhibitors in lung pathobiology [,,,,,,,,,,,,,,,,,,,]. Emerging evidence demonstrated that ALI/ARDS is regulated (not entirely but at least partially) by HDACs [,,]. However, the information on the involvement of specific HDAC-mediated signaling pathways in ALI/ARDS is limited and based primarily on the effect of semi-selective HDAC inhibitors on ALI manifestations in murine models.

Table 2.
Zinc-dependent HDACs inhibitors in lung pathobiology.
It was demonstrated that treatment with a broad-spectrum inhibitor of zinc-dependent HDACs, valproate [], administrated 30 min or 3 h after Escherichia coli (E. coli) infection attenuates pro-inflammatory responses in mouse lungs. However, administration of the same inhibitor at 4 h, 6 h, or 9 h after E. coli did not affect lung injury, suggesting a limited therapeutic window for this treatment [,]. Accordingly, the therapeutic index of valproate is reported to be narrow in both mice and humans due to side effects and toxicity [].
Recently, Kasotakis and co-workers [] reported that TSA can effectively mitigate lung inflammation and improve the survival rate of mice infected with E. coli. Surprisingly, the E. coli-induced injury in murine lungs is accompanied by decreased transcription of several HDAC genes, i.e., HDAC2, HDAC7, and HDAC8, but increased the expression of HDAC7 at the protein level. Further, TSA selectively decreased HDAC7 mRNA after an E. coli insult and attenuated E. coli-induced HDAC7 at the protein level. These discrepancies are discussed in more detail in the form of a letter to the editor []. Notably, the mechanisms by which TSA attenuates lung injury in E. coli-induced murine pneumonia are unclear. TSA was suggested to attenuate lung injury induced by mechanical ventilation/bleomycin insult in mice via inhibition of HDAC4/Akt signaling. However, TSA selectivity towards HDAC4 has not been described []. TSA and SAHA attenuate ventilator-induced lung injury in rats []. In addition, literature data indicated that another broad-spectrum HDAC inhibitor, sodium butyrate (SB), attenuates LPS-induced lung injury in mice []. Both TSA and SB are effective against intrapulmonary inflammation and promote survival in murine sepsis [].
The nuclear HDAC1 and HDAC2 participation in the endothelial barrier compromise in vitro and lung injury in an LPS murine model was recently evaluated []. Selective inhibition of HDAC1 and HDAC2, but not HDAC3, attenuates LPS-induced hyper-permeability in HLMVECs, likely through the preservation of Sox 18 expression, which LPS downregulates. Further, the HDAC1 inhibitor, tacedinaline, preserves Sox 18 expression and attenuates LPS-induced ALI in mice. Therefore, this study suggested that HDAC1 and HDAC2 act as transcription repressors, which drive the downregulation of Sox18 transcription induced by LPS, thus compromising the integrity of the pulmonary EC barrier. Therefore, selective HDAC1/HDAC2 inhibition may benefit ALI/ARDS treatment.
A recent study suggested that the chemical constituent of Azadirachta indica, Nimbolide, inhibits LPS-induced ALI in mice via suppression of oxidative stress and inflammatory responses, at least, in part, via inhibition of nuclear translocation of NF-κB and HDAC3 in alveolar epithelial cells []. Another study reported that selective inhibition of HDAC3 by the RGFP966 compound suppresses the expression of pro-inflammatory cytokines (such as IL-6, IL-1β, and IL-12β) in macrophages via inhibiting activity of NF-κB and attenuated lung injury manifestations in murine lung slices treated with LPS/IFNγ []. Interestingly, HDAC3 in macrophages may regulate the expression of pro-inflammatory genes in vitro and in mice in a dichotomous manner, with HDAC3 activity suppressing LPS-induced signaling. At the same time, the recruitment of HDAC3 by LPS activates the expression of pro-inflammatory genes independently from HDAC3 catalytic activity []. Therefore, specific precautions should be taken to generate HDAC3-specific inhibitors for treating lung inflammation and injury by targeting HDAC3 enzymatic activity []. While combined inhibition of HDAC3 and HDAC6 (by RGFP-966 and tubastatin, respectively) attenuates LPS-induced ALI in mice [], a recent study demonstrated that MS-275 compound (entinostat), inhibits HDAC1, HDAC2, and HDAC3 activities [], suppresses Robo4 expression by inhibiting HDAC3 in ECs and enhances EC permeability and lung vascular leakage in mice [].
Selective HDAC6 inhibition by tubastatin attenuates LPS-induced deacetylation of α-tubulin and β-catenin in the lung, which was accompanied by reduced pulmonary edema [], suggesting the therapeutic value of HDAC6 inhibition in ALI treatment.
The role of zinc-dependent HDACs in managing chronic lung diseases is more complex. Pathological cell type-specific imbalance of class I and II HDAC activities was observed in idiopathic pulmonary fibrosis (IPF). Positive outcomes have been predicted in managing IPF through HDAC1 and HDAC2 inhibition by Kim et al. []. This group recently reported HDAC1 as a signature marker in systemic sclerosis-associated interstitial lung disease []. However, the pan-HDAC inhibitor, SAHA, is not practical in the treatment of cystic fibrosis ex vivo []. Further, HDAC2 is essential for suppressing pro-inflammatory gene expression in chronic lung diseases like COPD and severe asthma [,].
Zinc-dependent HDACs (mainly HDAC3, HDAC4, and HDAC8) are suggested as potential therapeutic targets in managing hypertension []. It was also reported that specific HDAC6 inhibition with tubastatin A attenuated lung injury in a rat model of COPD [], thus offering a promising therapeutic strategy for COPD treatment. Further, there is a significant demand for the development of isoform-specific inhibitors for the treatment of lung injury as well as other diseases []. As a therapeutic remedy option, it is also essential to revisit and check the efficacy and selectivity of existing inhibitors. In addition, drug repurposing can be another therapeutic option to cure lung injury. For example, it was recently demonstrated that escitalopram, a selective serotonin reuptake inhibitor (SSRI), can be utilized as a treatment option for ALI. It inhibits the SIK2/HDAC4/NF-κB signaling pathway and overcomes the lung injury []. Combinational therapy, which includes HDAC inhibitors and DNA methylation modifiers, has been proven to be effective in murine models of LPS-induced inflammatory lung injury []. Further, developing dual-specificity inhibitors is another promising approach for treating lung injury and co-morbid pathologies. Thus, a recently designed dual inhibitor of HDACs and the PI3K/AKT pathway, CUDC-907, effectively treated bleomycin-TGFβ1-induced lung fibrosis as well as TGFβ1-induced tumor fibrosis [].
6. Conclusions
As detection methods for post-translational protein modifications improve, the repertoire of cellular acylated molecules continues to expand. This necessitates discovering and validating responsible enzymes involved in these processes, as well as the functions of different targeting sites. Our current understanding of these modifications is primarily based on studies of a limited number of lysine/histone acetyltransferases and lysine/histone deacetylases. Additionally, understanding the interplay between epigenetics, post-translational modifications, and metabolism in different cell types presents a significant challenge. However, with the advancement of genetic and biochemical tools, future research will focus on unraveling the molecular specificity of zinc-dependent HDACs. This review is primarily focused on the role of zinc-dependent HDACs in the regulation of EC-mediated lung function, emphasizing that the role of these enzymes can be isoform- and agonist-specific. However, additional studies are required to further elucidate the role of specific zinc-dependent HDAC subtypes and individual enzymes in the complex process of lung function regulation.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biom14020140/s1, Figure S1: Secondary and tertiary structures of zinc-dependent HDACs derived upon protein data bank and UniProt; Table S1: Molecular and structural characteristics of zinc-dependent HDACs.
Author Contributions
Conception and design: A.D.V.; writing—original draft and figure preparation: R.S.P.; participation in draft writing: M.E.M.; drafting the manuscript for important intellectual content: R.L., D.J.R.F., V.P., Z.B., A.K.-K., L.K., Y.S. and A.D.V. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported, in whole or in part, by NIH grants HL157440; HL158909; HL138410, AHA grant 23TPA1072536, and an Augusta University intramural grant IGPCT00035.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Mokrá, D. Acute lung injury—From pathophysiology to treatment. Physiol. Res. 2020, 69, S353–S366. [Google Scholar] [CrossRef] [PubMed]
- Long, M.E.; Mallampalli, R.K.; Horowitz, J.C. Pathogenesis of pneumonia and acute lung injury. Clin. Sci. 2022, 136, 747–769. [Google Scholar] [CrossRef] [PubMed]
- Rubenfeld, G.D.; Caldwell, E.; Peabody, E.; Weaver, J.; Martin, D.P.; Neff, M.; Stern, E.J.; Hudson, L.D. Incidence and outcomes of acute lung injury. N. Engl. J. Med. 2005, 353, 1685–1693. [Google Scholar] [CrossRef]
- Cusack, R.; Bos, L.D.; Povoa, P.; Martin-Loeches, I. Endothelial dysfunction triggers acute respiratory distress syndrome in patients with sepsis: A narrative review. Front. Med. 2023, 10, 1203827. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. ARDS Definition Task Force. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar]
- Steinberg, K.P.; Hudson, L.D.; Goodman, R.B.; Hough, C.L.; Lanken, P.N.; Hyzy, R.; Thompson, B.T.; Ancukiewicz, M.; National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N. Engl. J. Med. 2006, 354, 1671–1684. [Google Scholar]
- Wiedemann, H.P.; Wheeler, A.P.; Bernard, G.R.; Thompson, B.T.; Hayden, D.; deBoisblanc, B.; Connors, A.F., Jr.; Hite, R.D.; Harabin, A.L.; National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Comparison of two fluid-management strategies in acute lung injury. N. Engl. J. Med. 2006, 354, 2564–2575. [Google Scholar] [CrossRef]
- Arcaro, G.; Zenere, B.M.; Travia, D.; Zenti, M.G.; Covi, G.; Lechi, A.; Muggeo, M. Non-invasive detection of early endothelial dysfunction in hypercholesterolaemic subjects. Atherosclerosis 1995, 114, 247–254. [Google Scholar] [CrossRef]
- Maniatis, N.A.; Kotanidou, A.; Catravas, J.D.; Orfanos, S.E. Endothelial pathomechanisms in acute lung injury. Vasc. Pharmacol. 2008, 49, 119–133. [Google Scholar] [CrossRef]
- Vassiliou, A.G.; Kotanidou, A.; Dimopoulou, I.; Orfanos, S.E. Endothelial damage in acute respiratory distress syndrome. Int. J. Mol. Sci. 2020, 21, 8793. [Google Scholar] [CrossRef]
- Romero, M.J.; Yue, Q.; Singla, B.; Hamacher, J.; Sridhar, S.; Moseley, A.S.; Song, C.; Mraheil, M.A.; Fischer, B.; Zeitlinger, M.; et al. Direct endothelial ENaC activation mitigates vasculopathy induced by SARS-CoV2 spike protein. Front. Immunol. 2023, 14, 1241448. [Google Scholar] [CrossRef]
- Xu, S.W.; Ilyas, I.; Weng, J.P. Endothelial dysfunction in COVID-19: An overview of evidence, biomarkers, mechanisms and potential therapies. Acta Pharmacol. Sin. 2023, 44, 695–709. [Google Scholar] [CrossRef] [PubMed]
- Huertas, A.; Guignabert, C.; Barberà, J.A.; Bärtsch, P.; Bhattacharya, J.; Bhattacharya, S.; Bonsignore, M.R.; Dewachter, L.; Dinh-Xuan, A.T.; Dorfmüller, P.; et al. Pulmonary vascular endothelium: The orchestra conductor in respiratory diseases: Highlights from basic research to therapy. Eur. Respir. J. 2018, 51, 1700745. [Google Scholar] [CrossRef] [PubMed]
- Simmons, S.; Erfinanda, L.; Bartz, C.; Kuebler, W.M. Novel mechanisms regulating endothelial barrier function in the pulmonary microcirculation. J. Physiol. 2019, 597, 997–1021. [Google Scholar] [CrossRef]
- Borek, I.; Birnhuber, A.; Voelkel, N.F.; Marsh, L.M.; Kwapiszewska, G. The vascular perspective on acute and chronic lung disease. J. Clin. Investig. 2023, 133, e170502. [Google Scholar] [CrossRef] [PubMed]
- Mehta, D.; Malik, A.B. Signaling mechanisms regulating endothelial permeability. Physiol. Rev. 2006, 86, 279–367. [Google Scholar] [CrossRef]
- Dudek, S.M.; Garcia, J.G. Cytoskeletal regulation of pulmonary vascular permeability. J. Appl. Physiol. (1985) 2001, 91, 1487–1500. [Google Scholar] [CrossRef]
- Lampugnani, M.G.; Corada, M.; Caveda, L.; Breviario, F.; Ayalon, O.; Geiger, B.; Dejana, E. The molecular organization of endothelial cell to cell junctions: Differential association of plakoglobin, beta-catenin, and alpha-catenin with vascular endothelial cadherin (VE-cadherin). J. Cell Biol. 1995, 129, 203–217. [Google Scholar] [CrossRef]
- Dejana, E.; Orsenigo, F.; Lampugnani, M.G. The role of adherens junctions and VE-cadherin in the control of vascular permeability. J. Cell Sci. 2008, 121, 2115–2122. [Google Scholar] [CrossRef]
- Aslam, M.; Gündüz, D.; Troidl, C.; Heger, J.; Hamm, C.W.; Schulz, R. Purinergic Regulation of Endothelial Barrier Function. Int. J. Mol. Sci. 2021, 22, 1207. [Google Scholar] [CrossRef]
- Fang, Z.; Wang, X.; Sun, X.; Hu, W.; Miao, Q.R. The role of histone protein acetylation in regulating endothelial function. Front. Cell Dev. Biol. 2021, 9, 672447. [Google Scholar] [CrossRef] [PubMed]
- Ingber, D.E.; Wang, N.; Stamenovic, D. Tensegrity, cellular biophysics, and the mechanics of living systems. Rep. Prog. Phys. 2014, 77, 046603. [Google Scholar] [CrossRef] [PubMed]
- Widdicombe, J. Functional morphology and physiology of pulmonary rapidly adapting receptors (RARs). Anat. Rec. A Discov. Mol. Cell Evol. Biol. 2003, 270, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.F.; Nelson, C.M.; Tan, J.L.; Chen, C.S. Cadherins, RhoA, and Rac1 are differentially required for stretch-mediated proliferation in endothelial versus smooth muscle cells. Circ. Res. 2007, 101, e44–e52. [Google Scholar] [CrossRef] [PubMed]
- Tzima, E.; Irani-Tehrani, M.; Kiosses, W.B.; Dejana, E.; Schultz, D.A.; Engelhardt, B.; Cao, G.; DeLisser, H.; Schwartz, M.A. A mechanosensory complex that mediates the endothelial cell response to fluid shear stress. Nature 2005, 437, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Wu, D.; Birukov, K.G. Mechanosensing and mechanoregulation of endothelial cell functions. Compr. Physiol. 2019, 9, 873–904. [Google Scholar]
- Kovacs, L.; Kovacs-Kasa, A.; Verin, A.D.; Fulton, D.; Lucas, R.; Su, Y. Histone deacetylases in vascular permeability and remodeling associated with acute lung injury. Vessel. Plus. 2018, 2, 15. [Google Scholar] [CrossRef]
- Lee, D.Y.; Chiu, J.J. Atherosclerosis and flow: Roles of epigenetic modulation in vascular endothelium. J. Biomed. Sci. 2019, 26, 56. [Google Scholar] [CrossRef]
- Luo, G.; Liu, B.; Fu, T.; Liu, Y.; Li, B.; Li, N.; Geng, Q. The role of histone deacetylases in acute lung injury-friend or foe. Int. J. Mol. Sci. 2023, 24, 7876. [Google Scholar] [CrossRef]
- Shen, Z.; Bei, Y.; Lin, H.; Wei, T.; Dai, Y.; Hu, Y.; Zhang, C.; Dai, H. The role of class IIa histone deacetylases in regulating endothelial function. Front. Physiol. 2023, 14, 1091794. [Google Scholar] [CrossRef]
- Zhang, H.N.; Dai, Y.; Zhang, C.H.; Omondi, A.M.; Ghosh, A.; Khanra, I.; Chakraborty, M.; Yu, X.B.; Liang, J. Sirtuins family as a target in endothelial cell dysfunction: Implications for vascular ageing. Biogerontology 2020, 21, 495–516. [Google Scholar] [CrossRef] [PubMed]
- Bahl, S.; Seto, E. Regulation of histone deacetylase activities and functions by phosphorylation and its physiological relevance. Cell Mol. Life Sci. 2021, 78, 427–445. [Google Scholar] [CrossRef]
- Eom, G.H.; Kook, H. Posttranslational modifications of histone deacetylases: Implications for cardiovascular diseases. Pharmacol. Ther. 2014, 143, 168–180. [Google Scholar] [CrossRef] [PubMed]
- Seidel, C.; Schnekenburger, M.; Dicato, M.; Diederich, M. Histone deacetylase 6 in health and disease. Epigenomics 2015, 7, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Iaconelli, J.; Xuan, L.; Karmacharya, R. HDAC6 modulates signaling pathways relevant to synaptic biology and neuronal differentiation in human stem-cell-derived neurons. Int. J. Mol. Sci. 2019, 20, 1605. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Kawaguchi, Y.; Lai, C.H.; Kovacs, J.J.; Higashimoto, Y.; Appella, E.; Yao, T.P. MDM2-HDAC1-mediated deacetylation of p53 is required for its degradation. EMBO J. 2002, 21, 6236–6245. [Google Scholar] [CrossRef]
- Banerjee, S.; Adhikari, N.; Amin, S.A.; Jha, T. Histone deacetylase 8 (HDAC8) and its inhibitors with selectivity to other isoforms: An overview. Eur. J. Med. Chem. 2019, 164, 214–240. [Google Scholar] [CrossRef]
- Kumar, S.; Attrish, D.; Srivastava, A.; Banerjee, J.; Tripathi, M.; Chandra, P.S.; Dixit, A.B. Non-histone substrates of histone deacetylases as potential therapeutic targets in epilepsy. Expert. Opin. Ther. Targets 2021, 25, 75–85. [Google Scholar] [CrossRef]
- Zheng, W. The Zinc-dependent HDACs: Non-histone substrates and catalytic deacylation beyond deacetylation. Mini Rev. Med. Chem. 2022, 22, 2478–2485. [Google Scholar] [CrossRef]
- Dunaway, L.S.; Pollock, J.S. HDAC1: An environmental sensor regulating endothelial function. Cardiovasc. Res. 2022, 118, 1885–1903. [Google Scholar] [CrossRef]
- Yao, H.; Rahman, I. Role of histone deacetylase 2 in epigenetics and cellular senescence: Implications in lung inflammaging and COPD. Am. J. Physiol. Lung Cell Mol. Physiol. 2012, 303, L557–L566. [Google Scholar] [CrossRef]
- Pandey, D.; Hori, D.; Kim, J.H.; Bergman, Y.; Berkowitz, D.E.; Romer, L.H. NEDDylation promotes endothelial dysfunction: A role for HDAC2. J. Mol. Cell Cardiol. 2015, 81, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Ziesché, E.; Kettner-Buhrow, D.; Weber, A.; Wittwer, T.; Jurida, L.; Soelch, J.; Müller, H.; Newel, D.; Kronich, P.; Schneider, H.; et al. The coactivator role of histone deacetylase 3 in IL-1-signaling involves deacetylation of p65 NF-κB. Nucleic Acids Res. 2013, 41, 90–109. [Google Scholar] [CrossRef] [PubMed]
- Zampetaki, A.; Zeng, L.; Margariti, A.; Xiao, Q.; Li, H.; Zhang, Z.; Pepe, A.E.; Wang, G.; Habi, O.; deFalco, E.; et al. Histone deacetylase 3 is critical in endothelial survival and atherosclerosis development in response to disturbed flow. Circulation 2010, 121, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Liu, Q.; Adrianto, I.; Wu, X.; Glassbrook, J.; Khalasawi, N.; Yin, C.; Yi, Q.; Dong, Z.; Geissmann, F.; et al. Histone deacetylase 3 controls lung alveolar macrophage development and homeostasis. Nat. Commun. 2020, 11, 3822. [Google Scholar] [CrossRef] [PubMed]
- Kee, H.J.; Ryu, Y.; Seok, Y.M.; Choi, S.Y.; Sun, S.; Kim, G.R.; Jeong, M.H. Selective inhibition of histone deacetylase 8 improves vascular hypertrophy, relaxation, and inflammation in angiotensin II hypertensive mice. Clin. Hypertens. 2019, 25, 13. [Google Scholar] [CrossRef] [PubMed]
- Hou, F.; Wei, W.; Qin, X.; Liang, J.; Han, S.; Han, A.; Kong, Q. The posttranslational modification of HDAC4 in cell biology: Mechanisms and potential targets. J. Cell Biochem. 2020, 121, 930–937. [Google Scholar] [CrossRef] [PubMed]
- Ding, Q.; Shao, C.; Rose, P.; Zhu, Y.Z. Epigenetics and vascular senescence-potential new therapeutic targets? Front. Pharmacol. 2020, 11, 535395. [Google Scholar] [CrossRef]
- Litke, C.; Bading, H.; Mauceri, D. Histone deacetylase 4 shapes neuronal morphology via a mechanism involving regulation of expression of vascular endothelial growth factor D. J. Biol. Chem. 2018, 293, 8196–8207. [Google Scholar] [CrossRef]
- Turpaev, K.T. Transcription factor KLF2 and its role in the regulation of inflammatory processes. Biochemistry 2020, 85, 54–67. [Google Scholar] [CrossRef]
- Margariti, A.; Zampetaki, A.; Xiao, Q.; Zhou, B.; Karamariti, E.; Martin, D.; Yin, X.; Mayr, M.; Li, H.; Zhang, Z.; et al. Histone deacetylase 7 controls endothelial cell growth through modulation of beta-catenin. Circ. Res. 2010, 106, 1202–1211. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Li, X.; Parra, M.; Verdin, E.; Bassel-Duby, R.; Olson, E.N. Control of endothelial cell proliferation and migration by VEGF signaling to histone deacetylase 7. Proc. Natl. Acad. Sci. USA 2008, 105, 7738–7743. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.; Young, B.D.; Li, S.; Qi, X.; Richardson, J.A.; Olson, E.N. Histone deacetylase 7 maintains vascular integrity by repressing matrix metalloproteinase 10. Cell 2006, 126, 321–334. [Google Scholar] [CrossRef] [PubMed]
- Gao, C.; Ho, C.C.; Reineke, E.; Lam, M.; Cheng, X.; Stanya, K.J.; Liu, Y.; Chakraborty, S.; Shih, H.M.; Kao, H.Y. Histone deacetylase 7 promotes PML sumoylation and is essential for PML nuclear body formation. Mol. Cell. Biol. 2008, 28, 5658–5667. [Google Scholar] [CrossRef] [PubMed]
- Turtoi, A.; Mottet, D.; Matheus, N.; Dumont, B.; Peixoto, P.; Hennequière, V.; Deroanne, C.; Colige, A.; De Pauw, E.; Bellahcène, A.; et al. The angiogenesis suppressor gene AKAP12 is under the epigenetic control of HDAC7 in endothelial cells. Angiogenesis 2012, 15, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Kasotakis, G.; Kintsurashvili, E.; Galvan, M.D.; Graham, C.; Purves, J.T.; Agarwal, S.; Corcoran, D.L.; Sullenger, B.A.; Palmer, S.M.; Remick, D.G. Histone deacetylase 7 inhibition in a murine model of gram-negative pneumonia-induced acute lung injury. Shock 2020, 53, 344–351. [Google Scholar] [CrossRef]
- Schiano, C.; Benincasa, G.; Franzese, M.; Della Mura, N.; Pane, K.; Salvatore, M.; Napoli, C. Epigenetic-sensitive pathways in personalized therapy of major cardiovascular diseases. Pharmacol. Ther. 2020, 210, 107514. [Google Scholar] [CrossRef]
- Gal, J.; Chen, J.; Na, D.Y.; Tichacek, L.; Barnett, K.R.; Zhu, H. The acetylation of Lysine-376 of G3BP1 regulates RNA binding and stress granule dynamics. Mol. Cell. Biol. 2019, 39, e00052-19. [Google Scholar] [CrossRef]
- Leucker, T.M.; Nomura, Y.; Kim, J.H.; Bhatta, A.; Wang, V.; Wecker, A.; Jandu, S.; Santhanam, L.; Berkowitz, D.; Romer, L.; et al. Cystathionine γ-lyase protects vascular endothelium: A role for inhibition of histone deacetylase 6. Am. J. Physiol. Heart Circ. Physiol. 2017, 312, H711–H720. [Google Scholar] [CrossRef]
- Kaluza, D.; Kroll, J.; Gesierich, S.; Yao, T.P.; Boon, R.A.; Hergenreider, E.; Tjwa, M.; Rössig, L.; Seto, E.; Augustin, H.G.; et al. Class IIb HDAC6 regulates endothelial cell migration and angiogenesis by deacetylation of cortactin. EMBO J. 2011, 30, 4142–4156. [Google Scholar] [CrossRef]
- Nomura, Y.; Nakano, M.; Woo Sung, H.; Han, M.; Pandey, D. Inhibition of HDAC6 Activity Protects against endothelial dysfunction and atherogenesis in vivo: A role for HDAC6 neddylation. Front. Physiol. 2021, 12, 675724. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Kim, S.H.; Choi, M.C.; Lee, J.; Oh, D.Y.; Im, S.A.; Bang, Y.J.; Kim, T.Y. Class II histone deacetylases play pivotal roles in heat shock protein 90-mediated proteasomal degradation of vascular endothelial growth factor receptors. Biochem. Biophys. Res. Commun. 2008, 368, 318–322. [Google Scholar] [CrossRef] [PubMed]
- Duan, B.; Ye, D.; Zhu, S.; Jia, W.; Lu, C.; Wang, G.; Guo, X.; Yu, Y.; Wu, C.; Kang, J. HDAC10 promotes angiogenesis in endothelial cells through the PTPN22/ERK axis. Oncotarget 2017, 8, 61338–61349. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Tan, R.; Sun, M.; Yuan, L.; Ruiz, M.; Dupuis, J.; Hu, Q.; Zhu, L. MiR-1249 on endothelial extracellular vesicles mediates cigarette smoke-induced pulmonary hypertension by inhibiting HDAC10 (Histone Deacetylase 10)-NFκB (Nuclear Factor κB)-CaSR (Calcium-Sensing Receptor) cascade. Hypertension 2022, 79, 2721–2732. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Ge, J. Proteinase-activated receptor-2 modulates Ve-Cadherin expression to affect human vascular endothelial barrier function. J. Cell. Biochem. 2017, 118, 4587–4593. [Google Scholar] [CrossRef] [PubMed]
- Yao, F.; Jin, Z.; Lv, X.; Zheng, Z.; Gao, H.; Deng, Y.; Liu, Y.; Chen, L.; Wang, W.; He, J.; et al. Hydroxytyrosol acetate inhibits vascular endothelial cell pyroptosis via the HDAC11 signaling pathway in atherosclerosis. Front. Pharmacol. 2021, 12, 656272. [Google Scholar] [CrossRef] [PubMed]
- Yao, F.; Jin, Z.; Zheng, Z.; Lv, X.; Ren, L.; Yang, J.; Chen, D.; Wang, B.; Yang, W.; Chen, L.; et al. HDAC11 promotes both NLRP3/caspase-1/GSDMD and caspase-3/GSDME pathways causing pyroptosis via ERG in vascular endothelial cells. Cell Death Discov. 2022, 8, 112. [Google Scholar] [CrossRef] [PubMed]
- Porter, N.J.; Christianson, D.W. Structure, mechanism, and inhibition of the zinc-dependent histone deacetylases. Curr. Opin. Struct. Biol. 2019, 59, 9–18. [Google Scholar] [CrossRef]
- Shvedunova, M.; Akhtar, A. Modulation of cellular processes by histone and non-histone protein acetylation. Nat. Rev. Mol. Cell Biol. 2022, 23, 329–349. [Google Scholar] [CrossRef]
- Schator, D.; Gomez-Valero, L.; Buchrieser, C.; Rolando, M. Patho-epigenetics: Histone deacetylases as targets of pathogens and therapeutics. microLife 2021, 2, uqab013. [Google Scholar] [CrossRef]
- Yoshida, M.; Kudo, N.; Kosono, S.; Ito, A. Chemical and structural biology of protein lysine deacetylases. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2017, 93, 297–321. [Google Scholar] [CrossRef]
- Zhao, T.C.; Wang, Z.; Zhao, T.Y. The important role of histone deacetylases in modulating vascular physiology and arteriosclerosis. Atherosclerosis 2020, 303, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Ito, M.; Elliott, W.M.; Cosio, B.; Caramori, G.; Kon, O.M.; Barczyk, A.; Hayashi, S.; Adcock, I.M.; Hogg, J.C.; et al. Decreased histone deacetylase activity in chronic obstructive pulmonary disease. N. Engl. J. Med. 2005, 352, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Caramori, G.; Lim, S.; Oates, T.; Chung, K.F.; Barnes, P.J.; Adcock, I.M. Expression and activity of histone deacetylases in human asthmatic airways. Am. J. Respir. Crit. Care Med. 2002, 166, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Kee, H.J.; Eom, G.H.; Joung, H.; Shin, S.; Kim, J.R.; Cho, Y.K.; Choe, N.; Sim, B.W.; Jo, D.; Jeong, M.H.; et al. Activation of histone deacetylase 2 by inducible heat shock protein 70 in cardiac hypertrophy. Circ. Res. 2008, 103, 1259–1269. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.Y.; Kee, H.J.; Jin, L.; Ryu, Y.; Sun, S.; Kim, G.R.; Jeong, M.H. Inhibition of class IIa histone deacetylase activity by gallic acid, sulforaphane, TMP269, and panobinostat. Biomed. Pharmacother. 2018, 101, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.; Eom, G.H. HDAC and HDAC inhibitor: From cancer to cardiovascular diseases. Chonnam Med. J. 2016, 52, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, A. Targeting the Zinc-dependent histone deacetylases (HDACs) for drug discovery. In Chemical Epigenetics; Springer: Cham, Switzerland, 2020; Volume 33, ISBN 978-3-030-42981-2. [Google Scholar]
- Neugebauer, R.C.; Sippl, W.; Jung, M. Inhibitors of NAD+ dependent histone deacetylases (sirtuins). Curr. Pharm. Des. 2008, 14, 562–573. [Google Scholar]
- Agarwal, R.; Pattarawat, P.; Duff, M.R.; Wang, H.R.; Baudry, J.; Smith, J.C. Structure-based discovery of selective histone deacetylase (HDAC) 3 and 4 inhibitors. bioRxiv 2022. [Google Scholar] [CrossRef]
- Milazzo, G.; Mercatelli, D.; Di Muzio, G.; Triboli, L.; De Rosa, P.; Perini, G.; Giorgi, F.M. Histone deacetylases (HDACs): Evolution, specificity, role in transcriptional complexes, and pharmacological actionability. Genes 2020, 11, 556. [Google Scholar] [CrossRef]
- Delcuve, G.P.; Khan, D.H.; Davie, J.R. Roles of histone deacetylases in epigenetic regulation: Emerging paradigms from studies with inhibitors. Clin. Epigenetics 2012, 4, 5. [Google Scholar] [CrossRef]
- Emiliani, S.; Fischle, W.; Van Lint, C.; Al-Abed, Y.; Verdin, E. Characterization of a human RPD3 ortholog, HDAC3. Proc. Natl. Acad. Sci. USA 1998, 95, 2795–2800. [Google Scholar] [CrossRef] [PubMed]
- Taunton, J.; Hassig, C.A.; Schreiber, S.L. A mammalian histone deacetylase related to the yeast transcriptional regulator Rpd3p. Science 1996, 272, 408–411. [Google Scholar] [CrossRef] [PubMed]
- de Ruijter, A.J.; van Gennip, A.H.; Caron, H.N.; Kemp, S.; van Kuilenburg, A.B. Histone deacetylases (HDACs): Characterization of the classical HDAC family. Biochem. J. 2003, 370, 737–749. [Google Scholar] [CrossRef] [PubMed]
- Bradley, E.W.; Carpio, L.R.; van Wijnen, A.J.; McGee-Lawrence, M.E.; Westendorf, J.J. Histone deacetylases in bone development and skeletal disorders. Physiol. Rev. 2015, 95, 1359–1381. [Google Scholar] [CrossRef] [PubMed]
- Moser, M.A.; Hagelkruys, A.; Seiser, C. Transcription and beyond: The role of mammalian class I lysine deacetylases. Chromosoma 2014, 123, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Kim, J.S. A short guide to histone deacetylases including recent progress on class II enzymes. Exp. Mol. Med. 2020, 52, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Bertos, N.R.; Wang, A.H.; Yang, X.J. Class II histone deacetylases: Structure, function, and regulation. Biochem. Cell Biol. 2001, 79, 243–252. [Google Scholar] [CrossRef]
- Verdin, E.; Dequiedt, F.; Kasler, H.G. Class II histone deacetylases: Versatile regulators. Trends Genet. 2003, 19, 286–293. [Google Scholar] [CrossRef]
- Grozinger, C.M.; Schreiber, S.L. Regulation of histone deacetylase 4 and 5 and transcriptional activity by 14-3-3-dependent cellular localization. Proc. Natl. Acad. Sci. USA 2000, 97, 7835–7840. [Google Scholar] [CrossRef]
- Di Giorgio, E.; Brancolini, C. Regulation of class IIa HDAC activities: It is not only matter of subcellular localization. Epigenomics 2016, 8, 251–269. [Google Scholar] [CrossRef] [PubMed]
- Lahm, A.; Paolini, C.; Pallaoro, M.; Nardi, M.C.; Jones, P.; Neddermann, P.; Sambucini, S.; Bottomley, M.J.; Lo Surdo, P.; Carfí, A.; et al. Unraveling the hidden catalytic activity of vertebrate class IIa histone deacetylases. Proc. Natl. Acad. Sci. USA 2007, 104, 17335–17340. [Google Scholar] [CrossRef] [PubMed]
- Parra, M. Class IIa HDACs—New insights into their functions in physiology and pathology. FEBS J. 2015, 282, 1736–1744. [Google Scholar] [CrossRef] [PubMed]
- Das Gupta, K.; Shakespear, M.R.; Curson, J.E.B.; Murthy, A.M.V.; Iyer, A.; Hodson, M.P.; Ramnath, D.; Tillu, V.A.; von Pein, J.B.; Reid, R.C.; et al. Class IIa Histone deacetylases drive toll-like receptor-inducible glycolysis and macrophage inflammatory responses via pyruvate kinase M2. Cell Rep. 2020, 30, 2712–2728.e8. [Google Scholar] [CrossRef] [PubMed]
- Fischer, D.D.; Cai, R.; Bhatia, U.; Asselbergs, F.A.; Song, C.; Terry, R.; Trogani, N.; Widmer, R.; Atadja, P.; Cohen, D. Isolation and characterization of a novel class II histone deacetylase, HDAC10. J. Biol. Chem. 2002, 277, 6656–6666. [Google Scholar] [CrossRef] [PubMed]
- Guardiola, A.R.; Yao, T.P. Molecular cloning and characterization of a novel histone deacetylase HDAC10. J. Biol. Chem. 2002, 277, 3350–3356. [Google Scholar] [CrossRef]
- Tong, J.J.; Liu, J.; Bertos, N.R.; Yang, X.J. Identification of HDAC10, a novel class II human histone deacetylase containing a leucine-rich domain. Nucleic Acids Res. 2002, 30, 1114–1123. [Google Scholar] [CrossRef]
- Núñez-Álvarez, Y.; Suelves, M. HDAC11: A multifaceted histone deacetylase with proficient fatty deacylase activity and its roles in physiological processes. FEBS J. 2022, 289, 2771–2792. [Google Scholar] [CrossRef]
- Cao, J.; Sun, L.; Aramsangtienchai, P.; Spiegelman, N.A.; Zhang, X.; Huang, W.; Seto, E.; Lin, H. HDAC11 regulates type I interferon signaling through defatty-acylation of SHMT2. Proc. Natl. Acad. Sci. USA 2019, 116, 5487–5492. [Google Scholar] [CrossRef]
- Kee, H.J.; Kook, H. Roles and targets of class I and IIa histone deacetylases in cardiac hypertrophy. J. Biomed. Biotechnol. 2011, 2011, 928326. [Google Scholar] [CrossRef]
- Dzreyan, V.A.; Demyanenko, S.V. The role of post-translational protein acetylation and deacetylation in the apoptosis of neurons of the peripheral nervous system. Biochem. Mosc. Suppl. Ser. A 2023, 17, 249–263. [Google Scholar] [CrossRef]
- Ali, I.; Conrad, R.J.; Verdin, E.; Ott, M. Lysine acetylation goes global: From epigenetics to metabolism and therapeutics. Chem. Rev. 2018, 118, 1216–1252. [Google Scholar] [CrossRef] [PubMed]
- Millán-Zambrano, G.; Burton, A.; Bannister, A.J.; Schneider, R. Histone post-translational modifications—Cause and consequence of genome function. Nat. Rev. Genet. 2022, 23, 563–580. [Google Scholar] [CrossRef]
- Chen, H.P.; Zhao, Y.T.; Zhao, T.C. Histone deacetylases and mechanisms of regulation of gene expression. Crit. Rev. Oncog. 2015, 20, 35–47. [Google Scholar] [CrossRef] [PubMed]
- King, J.; Patel, M.; Chandrasekaran, S. Metabolism, HDACs, and HDAC inhibitors: A systems biology perspective. Metabolites 2021, 11, 792. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; He, Y.; Fu, W.; Sahebkar, A.; Tan, Y.; Xu, S.; Li, H. Histone deacetylases (HDACs) and atherosclerosis: A mechanistic and pharmacological review. Front. Cell Dev. Biol. 2020, 8, 581015. [Google Scholar] [CrossRef]
- Cross, D.; Drury, R.; Hill, J.; Pollard, A.J. Epigenetics in Sepsis: Understanding its role in endothelial dysfunction, immunosuppression, and potential therapeutics. Front. Immunol. 2019, 10, 1363. [Google Scholar] [CrossRef]
- Zemskov, E.A.; Gross, C.M.; Aggarwal, S.; Zemskova, M.A.; Wu, X.; Gu, C.; Wang, T.; Tang, H.; Black, S.M. NF-κB-dependent repression of Sox18 transcription factor requires the epigenetic regulators histone deacetylases 1 and 2 in acute lung injury. Front. Physiol. 2022, 13, 947537. [Google Scholar] [CrossRef]
- Kashio, T.; Shirakura, K.; Kinoshita, M.; Morita, M.; Ishiba, R.; Muraoka, K.; Kanbara, T.; Tanaka, M.; Funatsu, R.; Hino, N.; et al. HDAC inhibitor, MS-275, increases vascular permeability by suppressing Robo4 expression in endothelial cells. Tissue Barriers 2021, 9, 1911195. [Google Scholar] [CrossRef]
- Rolando, M.; Stefani, C.; Doye, A.; Acosta, M.I.; Visvikis, O.; Yevick, H.G.; Buchrieser, C.; Mettouchi, A.; Bassereau, P.; Lemichez, E. Contractile actin cables induced by Bacillus anthracis lethal toxin depend on the histone acetylation machinery. Cytoskeleton 2015, 72, 542–556. [Google Scholar] [CrossRef]
- Pandey, D.; Sikka, G.; Bergman, Y.; Kim, J.H.; Ryoo, S.; Romer, L.; Berkowitz, D. Transcriptional regulation of endothelial arginase 2 by histone deacetylase 2. Arter. Thromb. Vasc. Biol. 2014, 34, 1556–1566. [Google Scholar] [CrossRef] [PubMed]
- Hori, D.; Nomura, Y.; Nakano, M.; Han, M.; Bhatta, A.; Chen, K.; Akiyoshi, K.; Pandey, D. Endothelial-specific overexpression of histone deacetylase 2 protects mice against endothelial dysfunction and atherosclerosis. Cell Physiol. Biochem. 2020, 54, 947–958. [Google Scholar]
- Hou, Q.; Hu, K.; Liu, X.; Quan, J.; Liu, Z. HADC regulates the diabetic vascular endothelial dysfunction by targetting MnSOD. Biosci. Rep. 2018, 38, BSR20181042. [Google Scholar] [CrossRef] [PubMed]
- Bedenbender, K.; Scheller, N.; Fischer, S.; Leiting, S.; Preissner, K.T.; Schmeck, B.T.; Vollmeister, E. Inflammation-mediated deacetylation of the ribonuclease 1 promoter via histone deacetylase 2 in endothelial cells. FASEB J. 2019, 33, 9017–9029. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.G.; Liu, F.; Verin, A.D.; Birukova, A.; Dechert, M.A.; Gerthoffer, W.T.; Bamberg, J.R.; English, D. Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. J. Clin. Investig. 2001, 108, 689–701. [Google Scholar] [CrossRef] [PubMed]
- Hait, N.C.; Allegood, J.; Maceyka, M.; Strub, G.M.; Harikumar, K.B.; Singh, S.K.; Luo, C.; Marmorstein, R.; Kordula, T.; Milstien, S.; et al. Regulation of histone acetylation in the nucleus by sphingosine-1-phosphate. Science 2009, 325, 1254–1257. [Google Scholar] [CrossRef] [PubMed]
- Joshi, A.D.; Barabutis, N.; Birmpas, C.; Dimitropoulou, C.; Thangjam, G.; Cherian-Shaw, M.; Dennison, J.; Catravas, J.D. Histone deacetylase inhibitors prevent pulmonary endothelial hyperpermeability and acute lung injury by regulating heat shock protein 90 function. Am. J. Physiol. Lung Cell Mol. Physiol. 2015, 309, L1410–L1419. [Google Scholar] [CrossRef]
- Zhao, Q.; Yu, Z.; Zhang, F.; Huang, L.; Xing, C.; Liu, N.; Xu, Y.; Wang, X. HDAC3 inhibition prevents oxygen glucose deprivation/reoxygenation-induced transendothelial permeability by elevating PPARγ activity in vitro. J. Neurochem. 2019, 149, 298–310. [Google Scholar] [CrossRef]
- Zhao, Q.; Zhang, F.; Yu, Z.; Guo, S.; Liu, N.; Jiang, Y.; Lo, E.H.; Xu, Y.; Wang, X. HDAC3 inhibition prevents blood-brain barrier permeability through Nrf2 activation in type 2 diabetes male mice. J. Neuroinflammation 2019, 16, 103. [Google Scholar] [CrossRef]
- Ma, Q. Role of nrf2 in oxidative stress and toxicity. Annu. Rev. Pharmacol. Toxicol. 2013, 53, 401–426. [Google Scholar] [CrossRef]
- Huang, S.; Chen, G.; Sun, J.; Chen, Y.; Wang, N.; Dong, Y.; Shen, E.; Hu, Z.; Gong, W.; Jin, L.; et al. Histone deacetylase 3 inhibition alleviates type 2 diabetes mellitus-induced endothelial dysfunction via Nrf2. Cell Commun. Signal. 2021, 19, 35. [Google Scholar] [CrossRef] [PubMed]
- Celermajer, D.S.; Sorensen, K.E.; Gooch, V.M.; Spiegelhalter, D.J.; Miller, O.I.; Sullivan, I.D.; Lloyd, J.K.; Deanfield, J.E. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992, 340, 1111–1115. [Google Scholar] [CrossRef]
- Chen, L.; Shang, C.; Wang, B.; Wang, G.; Jin, Z.; Yao, F.; Yue, Z.; Bai, L.; Wang, R.; Zhao, S.; et al. HDAC3 inhibitor suppresses endothelial-to-mesenchymal transition via modulating inflammatory response in atherosclerosis. Biochem. Pharmacol. 2021, 192, 114716. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.Y.; Lee, C.I.; Lin, T.E.; Lim, S.H.; Zhou, J.; Tseng, Y.C.; Chien, S.; Chiu, J.J. Role of histone deacetylases in transcription factor regulation and cell cycle modulation in endothelial cells in response to disturbed flow. Proc. Natl. Acad. Sci. USA 2012, 109, 1967–1972. [Google Scholar] [CrossRef] [PubMed]
- Waltregny, D.; Glénisson, W.; Tran, S.L.; North, B.J.; Verdin, E.; Colige, A.; Castronovo, V. Histone deacetylase HDAC8 associates with smooth muscle alpha-actin and is essential for smooth muscle cell contractility. FASEB J. 2005, 19, 966–968. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, S.; Cleary, R.A.; Wang, R.; Gannon, O.J.; Seto, E.; Tang, D.D. Histone deacetylase 8 regulates cortactin deacetylation and contraction in smooth muscle tissues. Am. J. Physiol. Cell Physiol. 2014, 307, C288–C295. [Google Scholar] [CrossRef] [PubMed]
- Bandela, M.; Belvitch, P.; Garcia, J.G.N.; Dudek, S.M. Cortactin in lung cell function and disease. Int. J. Mol. Sci. 2022, 23, 4606. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.; Kettmann, R.; Dequiedt, F. Class IIa histone deacetylases: Regulating the regulators. Oncogene 2007, 26, 5450–5467. [Google Scholar] [CrossRef]
- Martin, M.; Kettmann, R.; Dequiedt, F. Class IIa histone deacetylases: Conducting development and differentiation. Int. J. Dev. Biol. 2009, 53, 291–301. [Google Scholar] [CrossRef]
- Kovacs-Kasa, A.; Kovacs, L.; Cherian-Shaw, M.; Patel, V.; Meadows, M.L.; Fulton, D.J.; Su, Y.; Verin, A.D. Inhibition of Class IIa HDACs improves endothelial barrier function in endotoxin-induced acute lung injury. J. Cell Physiol. 2021, 236, 2893–2905. [Google Scholar] [CrossRef]
- Lobera, M.; Madauss, K.P.; Pohlhaus, D.T.; Wright, Q.G.; Trocha, M.; Schmidt, D.R.; Baloglu, E.; Trump, R.P.; Head, M.S.; Hofmann, G.A.; et al. Selective class IIa histone deacetylase inhibition via a non-chelating zinc-binding group. Nat. Chem. Biol. 2013, 9, 319–325. [Google Scholar] [CrossRef]
- Li, M.; Zheng, Y.; Yuan, H.; Liu, Y.; Wen, X. Effects of dynamic changes in histone acetylation and deacetylase activity on pulmonary fibrosis. Int. Immunopharmacol. 2017, 52, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Xiao, C.; Long, F.; Su, Z.; Jia, W.; Qin, M.; Huang, M.; Wu, W.; Suguro, R.; Liu, X.; et al. HDAC4 regulates vascular inflammation via activation of autophagy. Cardiovasc. Res. 2018, 114, 1016–1028. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Cheng, H.; Chen, X.; Gu, J.; Su, W.; Cai, G.; Yan, Y.; Wang, C.; Xia, X.; Zhang, K.; et al. The activation of histone deacetylases 4 prevented endothelial dysfunction: A crucial mechanism of HuangqiGuizhiWuwu Decoction in improving microcirculation dysfunction in diabetes. J. Ethnopharmacol. 2023, 307, 116240. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.M.; Wang, X.; Li, C.X.; Liu, X.Y.; Guo, X.J.; Li, Y.; Chen, Y.L.; Ye, H.X.; Chen, H.S. SP1 promotes HDAC4 expression and inhibits HMGB1 expression to reduce intestinal barrier dysfunction, oxidative stress, and inflammatory response after sepsis. J. Innate Immun. 2022, 14, 366–379. [Google Scholar] [CrossRef]
- Hu, K.; Huang, M.J.; Ling, S.; Li, Y.X.; Cao, X.Y.; Chen, Y.F.; Lei, J.M.; Fu, W.Z.; Tan, B.F. LncRNA CASC11 upregulation promotes HDAC4 to alleviate oxidized low-density lipoprotein-induced injury of cardiac microvascular endothelial cells. Kaohsiung J. Med. Sci. 2023, 39, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Carmeliet, P.; Jain, R.K. Molecular mechanisms and clinical applications of angiogenesis. Nature 2011, 473, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, N.; Gerber, H.P.; LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 2003, 9, 669–676. [Google Scholar] [CrossRef]
- Liu, J.; Zhou, X.; Li, Q.; Zhou, S.M.; Hu, B.; Hu, G.W.; Niu, X.; Guo, S.C.; Wang, Y.; Deng, Z.F. Role of phosphorylated HDAC4 in stroke-induced angiogenesis. Biomed. Res. Int. 2017, 2017, 2957538. [Google Scholar] [CrossRef]
- Schader, T.; Löwe, O.; Reschke, C.; Malacarne, P.; Hahner, F.; Müller, N.; Gajos-Draus, A.; Backs, J.; Schröder, K. Oxidation of HDAC4 by Nox4-derived H2O2 maintains tube formation by endothelial cells. Redox Biol. 2020, 36, 101669. [Google Scholar] [CrossRef]
- Hrgovic, I.; Doll, M.; Pinter, A.; Kaufmann, R.; Kippenberger, S.; Meissner, M. Histone deacetylase inhibitors interfere with angiogenesis by decreasing endothelial VEGFR-2 protein half-life in part via a VE-cadherin-dependent mechanism. Exp. Dermatol. 2017, 26, 194–201. [Google Scholar] [CrossRef]
- Zecchin, A.; Pattarini, L.; Gutierrez, M.I.; Mano, M.; Mai, A.; Valente, S.; Myers, M.P.; Pantano, S.; Giacca, M. Reversible acetylation regulates vascular endothelial growth factor receptor-2 activity. J. Mol. Cell Biol. 2014, 6, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Urbich, C.; Rössig, L.; Kaluza, D.; Potente, M.; Boeckel, J.N.; Knau, A.; Diehl, F.; Geng, J.G.; Hofmann, W.K.; Zeiher, A.M.; et al. HDAC5 is a repressor of angiogenesis and determines the angiogenic gene expression pattern of endothelial cells. Blood 2009, 113, 5669–5679. [Google Scholar] [CrossRef]
- Tsou, P.S.; Wren, J.D.; Amin, M.A.; Schiopu, E.; Fox, D.A.; Khanna, D.; Sawalha, A.H. Histone deacetylase 5 is overexpressed in scleroderma endothelial cells and impairs Angiogenesis via repression of proangiogenic factors. Arthritis Rheumatol. 2016, 68, 2975–2985. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Tan, J.; Yuan, Y.; Shen, J.; Chen, Y. Semaglutide ameliorates lipopolysaccharide-induced acute lung injury through inhibiting HDAC5-mediated activation of NF-κB signaling pathway. Hum. Exp. Toxicol. 2022, 41, 9603271221125931. [Google Scholar] [CrossRef]
- Wang, Y.; Abrol, R.; Mak, J.Y.W.; Das Gupta, K.; Ramnath, D.; Karunakaran, D.; Fairlie, D.P.; Sweet, M.J. Histone deacetylase 7: A signalling hub controlling development, inflammation, metabolism and disease. FEBS J. 2023, 290, 2805–2832. [Google Scholar] [CrossRef]
- Hsu, A.; Duan, Q.; McMahon, S.; Huang, Y.; Wood, S.A.; Gray, N.S.; Wang, B.; Bruneau, B.G.; Haldar, S.M. Salt-inducible kinase 1 maintains HDAC7 stability to promote pathologic cardiac remodeling. J. Clin. Investig. 2020, 130, 2966–2977. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.T.; Gao, C.; Liu, Y.; Guo, S.; Wang, A.; Wang, B.; Erdjument-Bromage, H.; Miyagi, M.; Tempst, P.; Kao, H.Y. Monoubiquitination of filamin B regulates vascular endothelial growth factor-mediated trafficking of histone deacetylase 7. Mol. Cell Biol. 2013, 33, 1546–1560. [Google Scholar] [CrossRef]
- Yang, J.; Moraga, A.; Xu, J.; Zhao, Y.; Luo, P.; Lao, K.H.; Margariti, A.; Zhao, Q.; Ding, W.; Wang, G.; et al. A histone deacetylase 7-derived peptide promotes vascular regeneration via facilitating 14-3-3γ phosphorylation. Stem Cells. 2020, 38, 556–573. [Google Scholar] [CrossRef]
- Martin, M.; Geudens, I.; Bruyr, J.; Potente, M.; Bleuart, A.; Lebrun, M.; Simonis, N.; Deroanne, C.; Twizere, J.C.; Soubeyran, P.; et al. PP2A regulatory subunit Bα controls endothelial contractility and vessel lumen integrity via regulation of HDAC7. EMBO J. 2013, 32, 2491–2503. [Google Scholar] [CrossRef]
- Parra, M.; Mahmoudi, T.; Verdin, E. Myosin phosphatase dephosphorylates HDAC7, controls its nucleocytoplasmic shuttling, and inhibits apoptosis in thymocytes. Genes Dev. 2007, 21, 638–643. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kovacs-Kasa, A.; Gorshkov, B.A.; Kim, K.M.; Kumar, S.; Black, S.M.; Fulton, D.J.; Dimitropoulou, C.; Catravas, J.D.; Verin, A.D. The protective role of MLCP-mediated ERM dephosphorylation in endotoxin-induced lung injury in vitro and in vivo. Sci. Rep. 2016, 6, 39018. [Google Scholar] [CrossRef]
- Kim, K.M.; Csortos, C.; Czikora, I.; Fulton, D.; Umapathy, N.S.; Olah, G.; Verin, A.D. Molecular characterization of myosin phosphatase in endothelium. J. Cell Physiol. 2012, 227, 1701–1708. [Google Scholar] [CrossRef] [PubMed]
- Guo, K.; Ma, Z.; Zhang, Y.; Han, L.; Shao, C.; Feng, Y.; Gao, F.; Di, S.; Zhang, Z.; Zhang, J.; et al. HDAC7 promotes NSCLC proliferation and metastasis via stabilization by deubiquitinase USP10 and activation of β-catenin-FGF18 pathway. J. Exp. Clin. Cancer Res. 2022, 41, 91. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Wei, X.; Wang, Z.; Han, H.; Fu, Y.; Liu, J.; Zhang, Y.; Guo, J.; Dong, C.; Zhou, D.; et al. HDAC9 exacerbates endothelial injury in cerebral ischaemia/reperfusion injury. J. Cell Mol. Med. 2016, 20, 1139–1149. [Google Scholar] [CrossRef]
- Lu, S.; Li, H.; Li, K.; Fan, X.D. HDAC9 promotes brain ischemic injury by provoking IκBα/NF-κB and MAPKs signaling pathways. Biochem. Biophys. Res. Commun. 2018, 503, 1322–1329. [Google Scholar] [CrossRef]
- Sun, J.; Zhang, L.; Cheng, Q.; Wu, Y. Aberrant expression and regulatory role of histone deacetylase 9 in vascular endothelial cell injury in intracranial aneurysm. Biomol. Biomed. 2023, 24, 61–72. [Google Scholar] [CrossRef]
- Brancolini, C.; Di Giorgio, E.; Formisano, L.; Gagliano, T. Quis custodiet ipsos custodes (who controls the controllers)? Two decades of studies on HDAC9. Life 2021, 11, 90. [Google Scholar] [CrossRef]
- Joo, E.E.; Yamada, K.M. Post-polymerization crosstalk between the actin cytoskeleton and microtubule network. Bioarchitecture 2016, 6, 53–59. [Google Scholar] [CrossRef]
- Valenzuela-Fernández, A.; Cabrero, J.R.; Serrador, J.M.; Sánchez-Madrid, F. HDAC6: A key regulator of cytoskeleton, cell migration and cell-cell interactions. Trends Cell Biol. 2008, 18, 291–297. [Google Scholar] [CrossRef]
- Karki, P.; Birukova, A.A. Microtubules as major regulators of endothelial function: Implication for lung injury. Front. Physiol. 2021, 12, 758313. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Ma, M.; Ma, Z.; Fu, J. HDAC6 inhibition prevents TNF-α-induced caspase 3 activation in lung endothelial cell and maintains cell-cell junctions. Oncotarget 2016, 7, 54714–54722. [Google Scholar] [CrossRef] [PubMed]
- Smith, Q.; Macklin, B.; Chan, X.Y.; Jones, H.; Trempel, M.; Yoder, M.C.; Gerecht, S. Differential HDAC6 activity modulates ciliogenesis and subsequent mechanosensing of endothelial cells derived from pluripotent stem cells. Cell Rep. 2018, 24, 895–908.e6. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.S.; Hubbert, C.C.; Lu, J.; Lee, Y.S.; Lee, J.Y.; Yao, T.P. Histone deacetylase 6 regulates growth factor-induced actin remodeling and endocytosis. Mol. Cell Biol. 2007, 27, 8637–8647. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yuan, Z.; Zhang, Y.; Yong, S.; Salas-Burgos, A.; Koomen, J.; Olashaw, N.; Koomen, J.; Olashaw, N.; Parsons, J.T.; et al. HDAC6 modulates cell motility by altering the acetylation level of cortactin. Mol. Cell. 2007, 27, 197–213. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, N.; Caron, C.; Matthias, G.; Hess, D.; Khochbin, S.; Matthias, P. HDAC-6 interacts with and deacetylates tubulin and microtubules in vivo. EMBO J. 2003, 22, 1168–1179. [Google Scholar] [CrossRef]
- Yu, J.; Ma, Z.; Shetty, S.; Ma, M.; Fu, J. Selective HDAC6 inhibition prevents TNF-α-induced lung endothelial cell barrier disruption and endotoxin-induced pulmonary edema. Am. J. Physiol. Lung Cell Mol. Physiol. 2016, 311, L39–L47. [Google Scholar] [CrossRef] [PubMed]
- Zilberman, Y.; Ballestrem, C.; Carramusa, L.; Mazitschek, R.; Khochbin, S.; Bershadsky, A. Regulation of microtubule dynamics by inhibition of the tubulin deacetylase HDAC6. J. Cell Sci. 2009, 122, 3531–3541. [Google Scholar] [CrossRef]
- Li, D.; Xie, S.; Ren, Y.; Huo, L.; Gao, J.; Cui, D.; Liu, M.; Zhou, J. Microtubule-associated deacetylase HDAC6 promotes angiogenesis by regulating cell migration in an EB1-dependent manner. Protein Cell. 2011, 2, 150–160. [Google Scholar] [CrossRef]
- Zhang, Q.Q.; Zhang, W.J.; Chang, S. HDAC6 inhibition: A significant potential regulator and therapeutic option to translate into clinical practice in renal transplantation. Front. Immunol. 2023, 14, 1168848. [Google Scholar] [CrossRef]
- Saito, S.; Lasky, J.A.; Guo, W.; Nguyen, H.; Mai, A.; Danchuk, S.; Sullivan, D.E.; Shan, B. Pharmacological inhibition of HDAC6 attenuates endothelial barrier dysfunction induced by thrombin. Biochem. Biophys. Res. Commun. 2011, 408, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Gorshkov, B.A.; Zemskova, M.A.; Verin, A.D.; Bogatcheva, N.V. Taxol alleviates 2-methoxyestradiol-induced endothelial permeability. Vasc. Pharmacol. 2012, 56, 56–63. [Google Scholar] [CrossRef]
- Borgas, D.; Chambers, E.; Newton, J.; Ko, J.; Rivera, S.; Rounds, S.; Lu, Q. Cigarette smoke disrupted lung endothelial barrier integrity and increased susceptibility to acute lung injury via histone deacetylase 6. Am. J. Respir. Cell Mol. Biol. 2016, 54, 683–696. [Google Scholar] [CrossRef] [PubMed]
- Karki, P.; Ke, Y.; Tian, Y.; Ohmura, T.; Sitikov, A.; Sarich, N.; Montgomery, C.P.; Birukova, A.A. Staphylococcus aureus-induced endothelial permeability and inflammation are mediated by microtubule destabilization. J. Biol. Chem. 2019, 294, 3369–3384. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmann, N.; Wroblowski, S.; Knyphausen, P.; de Boor, S.; Brenig, J.; Zienert, A.Y.; Meyer-Teschendorf, K.; Praefcke, G.J.K.; Nolte, H.; Krüger, M.; et al. Structural and mechanistic insights into the regulation of the fundamental rho regulator RhoGDIα by lysine acetylation. J. Biol. Chem. 2016, 291, 5484–5499. [Google Scholar] [CrossRef]
- Menden, H.; Xia, S.; Mabry, S.M.; Noel-MacDonnell, J.; Rajasingh, J.; Ye, S.Q.; Sampath, V. Histone deacetylase 6 regulates endothelial MyD88-dependent canonical TLR signaling, lung inflammation, and alveolar remodeling in the developing lung. Am. J. Physiol. Lung Cell Mol. Physiol. 2019, 317, L332–L346. [Google Scholar] [CrossRef]
- Zhang, H.P.; Wang, L.; Fu, J.J.; Fan, T.; Wang, Z.L.; Wang, G. Association between histone hyperacetylation status in memory T lymphocytes and allergen-induced eosinophilic airway inflammation. Respirology 2016, 21, 850–857. [Google Scholar] [CrossRef]
- Liao, W.; Sun, J.; Liu, W.; Li, W.; Jia, J.; Ou, F.; Su, K.; Zheng, Y.; Zhang, Z.; Sun, Y. HDAC10 upregulation contributes to interleukin 1β-mediated inflammatory activation of synovium-derived mesenchymal stem cells in temporomandibular joint. J. Cell Physiol. 2019, 234, 12646–12662. [Google Scholar] [CrossRef]
- Wang, L.; Zheng, S.; Zhang, L.; Xiao, H.; Gan, H.; Chen, H.; Zhai, X.; Liang, P.; Zhao, J.; Li, Y. Histone deacetylation 10 alleviates inflammation after intracerebral hemorrhage via the PTPN22/NLRP3 pathway in rats. Neuroscience 2020, 432, 247–259. [Google Scholar] [CrossRef]
- Tian, Y.; Shi, H.; Zhang, D.; Wang, C.; Zhao, F.; Li, L.; Xu, Z.; Jiang, J.; Li, J. Nebulized inhalation of LPAE-HDAC10 inhibits acetylation-mediated ROS/NF-κB pathway for silicosis treatment. J. Control. Release 2023, 364, 618–631. [Google Scholar] [CrossRef]
- Gao, L.; Cueto, M.A.; Asselbergs, F.; Atadja, P. Cloning and functional characterization of HDAC11, a novel member of the human histone deacetylase family. J. Biol. Chem. 2002, 277, 25748–25755. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Ma, Z.; Huang, D.; Zhang, J.; Li, J.; Zhi, P.; Zhang, L.; Feng, Y.; Ge, X.; Zhai, J.; et al. Clinicopathological characteristics and prognostic significance of HDAC11 protein expression in non-small cell lung cancer: A retrospective study. Transl. Lung Cancer Res. 2022, 11, 1119–1131. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Xie, C.; Chen, Q.; Zhuang, S. HDAC11, an emerging therapeutic target for metabolic disorders. Front. Endocrinol. 2022, 13, 989305. [Google Scholar] [CrossRef] [PubMed]
- Bala, S.; Csak, T.; Kodys, K.; Catalano, D.; Ambade, A.; Furi, I.; Lowe, P.; Cho, Y.; Iracheta-Vellve, A.; Szabo, G. Alcohol-induced miR-155 and HDAC11 inhibit negative regulators of the TLR4 pathway and lead to increased LPS responsiveness of Kupffer cells in alcoholic liver disease. J. Leukoc. Biol. 2017, 102, 487–498. [Google Scholar] [CrossRef]
- Zheng, C.; Zhong, M.; Qi, Z.; Shen, F.; Zhao, Q.; Wu, L.; Huang, Y.; Tsang, S.Y.; Yao, X. Histone deacetylase inhibitors relax mouse aorta partly through their inhibitory action on L-type Ca2+ channels. J. Pharmacol. Exp. Ther. 2017, 363, 211–220. [Google Scholar] [CrossRef] [PubMed]
- He, R.; Liu, B.; Geng, B.; Li, N.; Geng, Q. The role of HDAC3 and its inhibitors in regulation of oxidative stress and chronic diseases. Cell Death Discov. 2023, 9, 131. [Google Scholar] [CrossRef] [PubMed]
- Reichert, N.; Choukrallah, M.A.; Matthias, P. Multiple roles of class I HDACs in proliferation, differentiation, and development. Cell Mol. Life Sci. 2012, 69, 2173–2187. [Google Scholar] [CrossRef] [PubMed]
- Telles, E.; Seto, E. Modulation of cell cycle regulators by HDACs. Front. Biosci. (Sch. Ed.) 2012, 4, 831–839. [Google Scholar]
- Ramaiah, M.J.; Tangutur, A.D.; Manyam, R.R. Epigenetic modulation and understanding of HDAC inhibitors in cancer therapy. Life Sci. 2021, 277, 119504. [Google Scholar] [CrossRef]
- Peng, Z.; Shu, B.; Zhang, Y.; Wang, M. Endothelial response to pathophysiological stress. Arter. Thromb. Vasc. Biol. 2019, 39, e233–e243. [Google Scholar] [CrossRef]
- Dzobo, K.E.; Hanford, K.M.L.; Kroon, J. Vascular metabolism as driver of Atherosclerosis: Linking endothelial metabolism to inflammation. Immunometabolism 2021, 3, e210020. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.T.; Hung, W.C. Inhibition of proliferation, sprouting, tube formation and Tie2 signaling of lymphatic endothelial cells by the histone deacetylase inhibitor SAHA. Oncol. Rep. 2013, 30, 961–967. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Sun, M.; Ramchandran, R.; Raj, J.U. IGF-1 signaling in neonatal hypoxia-induced pulmonary hypertension: Role of epigenetic regulation. Vasc. Pharmacol. 2015, 73, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Zhou, Y.; Loberg, A.; Tahara, S.M.; Malik, P.; Kalra, V.K. Activated transcription factor 3 in association with histone deacetylase 6 negatively regulates microRNA 199a2 transcription by chromatin remodeling and reduces endothelin-1 expression. Mol. Cell Biol. 2016, 36, 2838–2854. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Li, G.; Su, F.; Cai, Y.; Shi, L.; Meng, Y.; Liu, Z.; Sun, J.; Wang, M.; Qian, M.; et al. HDAC8 cooperates with SMAD3/4 complex to suppress SIRT7 and promote cell survival and migration. Nucleic Acids Res. 2020, 48, 2912–2923. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.F.; Lu, J.Y.; Zhang, Y.J.; Zhang, L.X.; Lu, G.D.; Xie, Z.J.; Cheng, M.B.; Shen, Y.F.; Zhang, Y. C/EBPα negatively regulates SIRT7 expression via recruiting HDAC3 to the upstream-promoter of hepatocellular carcinoma cells. Biochim. Biophys. Acta 2016, 1859, 348–354. [Google Scholar] [CrossRef]
- Singh, T.; Kaur, P.; Singh, P.; Singh, S.; Munshi, A. Differential molecular mechanistic behavior of HDACs in cancer progression. Med. Oncol. 2022, 39, 171. [Google Scholar] [CrossRef]
- Lee, Y.; Gustafsson, A.B. Role of apoptosis in cardiovascular disease. Apoptosis 2009, 14, 536–548. [Google Scholar] [CrossRef]
- Tricot, O.; Mallat, Z.; Heymes, C.; Belmin, J.; Lesèche, G.; Tedgui, A. Relation between endothelial cell apoptosis and blood flow direction in human atherosclerotic plaques. Circulation 2000, 101, 2450–2453. [Google Scholar] [CrossRef]
- Bombeli, T.; Schwartz, B.R.; Harlan, J.M. Endothelial cells undergoing apoptosis become proadhesive for nonactivated platelets. Blood 1999, 93, 3831–3838. [Google Scholar] [CrossRef]
- Cancel, L.M.; Tarbell, J.M. The role of apoptosis in LDL transport through cultured endothelial cell monolayers. Atherosclerosis 2010, 208, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Tajadura, V.; Hansen, M.H.; Smith, J.; Charles, H.; Rickman, M.; Farrell-Dillon, K.; Claro, V.; Warboys, C.; Ferro, A. β-catenin promotes endothelial survival by regulating eNOS activity and flow-dependent anti-apoptotic gene expression. Cell Death Dis. 2020, 11, 493. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Peng, K.; Wu, Q.; Wang, Y.; Fan, X.; Zhang, D.M.; Passerini, A.G.; Sun, C. HDAC1 and 2 regulate endothelial VCAM-1 expression and atherogenesis by suppressing methylation of the GATA6 promoter. Theranostics 2021, 11, 5605–5619. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Cheng, N.; Du, J.; Zhang, H.; Zhang, C. MicroRNA-200b-3p promotes endothelial cell apoptosis by targeting HDAC4 in atherosclerosis. BMC Cardiovasc. Disord. 2021, 21, 172. [Google Scholar] [CrossRef] [PubMed]
- Shakespear, M.R.; Halili, M.A.; Irvine, K.M.; Fairlie, D.P.; Sweet, M.J. Histone deacetylases as regulators of inflammation and immunity. Trends Immunol. 2011, 32, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Wei, T.; Shen, Z.; Bei, Y.; Lin, H.; Dai, H. Classical HDACs in the regulation of neuroinflammation. Neurochem. Int. 2021, 150, 105182. [Google Scholar] [CrossRef] [PubMed]
- Rajendrasozhan, S.; Yang, S.R.; Edirisinghe, I.; Yao, H.; Adenuga, D.; Rahman, I. Deacetylases and NF-kappaB in redox regulation of cigarette smoke-induced lung inflammation: Epigenetics in pathogenesis of COPD. Antioxid. Redox Signal. 2008, 10, 799–811. [Google Scholar] [CrossRef]
- Hu, Y.; Suliman, B.A. Roles of HDACs in the responses of innate immune cells and as targets in inflammatory diseases. Adv. Exp. Med. Biol. 2017, 1024, 91–110. [Google Scholar]
- Gatla, H.R.; Muniraj, N.; Thevkar, P.; Yavvari, S.; Sukhavasi, S.; Makena, M.R. Regulation of chemokines and cytokines by histone deacetylases and an update on histone decetylase inhibitors in human diseases. Int. J. Mol. Sci. 2019, 20, 1110. [Google Scholar] [CrossRef]
- Luan, Y.; Liu, H.; Luan, Y.; Yang, Y.; Yang, J.; Ren, K.D. New insight in HDACs: Potential therapeutic targets for the treatment of Atherosclerosis. Front. Pharmacol. 2022, 13, 863677. [Google Scholar] [CrossRef]
- Kulthinee, S.; Yano, N.; Zhuang, S.; Wang, L.; Zhao, T.C. Critical functions of histone deacetylases (HDACs) in modulating inflammation associated with cardiovascular diseases. Pathophysiology 2022, 29, 471–485. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.; Verin, A.D.; Black, S.M.; Catravas, J.D. Regulators of endothelial and epithelial barrier integrity and function in acute lung injury. Biochem. Pharmacol. 2009, 77, 1763–1772. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Zhang, B.; Wei, X.; Wang, Z.; Fan, B.; Du, P.; Zhang, Y.; Jian, W.; Chen, L.; Wang, L.; et al. HDAC4/5-HMGB1 signalling mediated by NADPH oxidase activity contributes to cerebral ischaemia/reperfusion injury. J. Cell Mol. Med. 2013, 17, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Wang, Z.; Liu, J. Role of HDACs in normal and malignant hematopoiesis. Mol. Cancer 2020, 19, 5, Erratum in Mol. Cancer 2020, 19, 55. [Google Scholar] [CrossRef] [PubMed]
- Roche, J.; Bertrand, P. Inside HDACs with more selective HDAC inhibitors. Eur. J. Med. Chem. 2016, 121, 451–483. [Google Scholar] [CrossRef] [PubMed]
- Bieliauskas, A.V.; Pflum, M.K. Isoform-selective histone deacetylase inhibitors. Chem. Soc. Rev. 2008, 37, 1402–1413. [Google Scholar] [CrossRef]
- Li, Y.; Wang, F.; Chen, X.; Wang, J.; Zhao, Y.; Li, Y.; He, B. Zinc-dependent deacetylase (HDAC) inhibitors with different zinc binding groups. Curr. Top. Med. Chem. 2019, 19, 223–241. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lin, S.; Gu, Z.; Chen, L.; He, B. Zinc-dependent deacetylases (HDACs) as potential targets for treating Alzheimer’s disease. Bioorg. Med. Chem. Lett. 2022, 76, 129015. [Google Scholar] [CrossRef]
- Jin, G.; Wang, K.; Zhao, Y.; Yuan, S.; He, Z.; Zhang, J. Targeting histone deacetylases for heart diseases. Bioorg. Chem. 2023, 138, 106601. [Google Scholar] [CrossRef]
- von Knethen, A.; Brüne, B. Histone deacetylation inhibitors as therapy concept in sepsis. Int. J. Mol. Sci. 2019, 20, 346. [Google Scholar] [CrossRef]
- Shanmugam, G.; Rakshit, S.; Sarkar, K. HDAC inhibitors: Targets for tumor therapy, immune modulation and lung diseases. Transl. Oncol. 2022, 16, 101312. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.Y.; Tang, S.E.; Ko, F.C.; Wu, G.C.; Huang, K.L.; Chu, S.J. Valproic acid attenuates acute lung injury induced by ischemia-reperfusion in rats. Anesthesiology 2015, 122, 1327–1337. [Google Scholar] [CrossRef] [PubMed]
- Kasotakis, G.; Galvan, M.D.; Osathanugrah, P.; Dharia, N.; Bufe, L.; Breed, Z.; Mizgerd, J.P.; Remick, D.G. Timing of valproic acid in acute lung injury: Prevention is the best therapy? J. Surg. Res. 2017, 220, 206–212. [Google Scholar] [CrossRef]
- Kasotakis, G.; Galvan, M.; King, E.; Sarkar, B.; Stucchi, A.; Mizgerd, J.P.; Burke, P.A.; Remick, D. Valproic acid mitigates the inflammatory response and prevents acute respiratory distress syndrome in a murine model of Escherichia coli pneumonia at the expense of bacterial clearance. J. Trauma Acute Care Surg. 2017, 82, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Cheng, B.; Yang, L.; Li, G.; Yuan, Y.; Luo, G.; Shu, Z.; Jiang, H. LncRNA ZEB1-AS1 knockdown alleviates oxidative low-density lipoprotein-induced endothelial cell injury via the miR-590-5p/HDAC9 axis. Cent. Eur. J. Immunol. 2021, 46, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Larsson, P.; Ulfhammer, E.; Magnusson, M.; Bergh, N.; Lunke, S.; El-Osta, A.; Medcalf, R.L.; Svensson, P.A.; Karlsson, L.; Jern, S. Role of histone acetylation in the stimulatory effect of valproic acid on vascular endothelial tissue-type plasminogen activator expression. PLoS ONE. 2012, 7, e31573. [Google Scholar] [CrossRef] [PubMed]
- Usui, T.; Okada, M.; Mizuno, W.; Oda, M.; Ide, N.; Morita, T.; Hara, Y.; Yamawaki, H. HDAC4 mediates development of hypertension via vascular inflammation in spontaneous hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2012, 302, H1894–H1904. [Google Scholar] [CrossRef]
- Granger, A.; Abdullah, I.; Huebner, F.; Stout, A.; Wang, T.; Huebner, T.; Epstein, J.A.; Gruber, P.J. Histone deacetylase inhibition reduces myocardial ischemia-reperfusion injury in mice. FASEB J. 2008, 22, 3549–3560. [Google Scholar] [CrossRef]
- Thangavel, J.; Malik, A.B.; Elias, H.K.; Rajasingh, S.; Simpson, A.D.; Sundivakkam, P.K.; Vogel, S.M.; Xuan, Y.T.; Dawn, B.; Rajasingh, J. Combinatorial therapy with acetylation and methylation modifiers attenuates lung vascular hyperpermeability in endotoxemia-induced mouse inflammatory lung injury. Am. J. Pathol. 2014, 184, 2237–2249. [Google Scholar] [CrossRef]
- Thangavel, J.; Samanta, S.; Rajasingh, S.; Barani, B.; Xuan, Y.T.; Dawn, B.; Rajasingh, J. Epigenetic modifiers reduce inflammation and modulate macrophage phenotype during endotoxemia-induced acute lung injury. J. Cell Sci. 2015, 128, 3094–3105. [Google Scholar] [CrossRef]
- Luo, Z.F.; Jiang, X.H.; Liu, H.; He, L.Y.; Luo, X.; Chen, F.C.; Tan, Y.L. miR-23b attenuates LPS-induced inflammatory responses in acute lung injury via inhibition of HDAC2. Biochem. Genet. 2021, 59, 604–616. [Google Scholar] [CrossRef] [PubMed]
- Asare, Y.; Campbell-James, T.A.; Bokov, Y.; Yu, L.L.; Prestel, M.; El Bounkari, O.; Roth, S.; El Bounkari, O.; Roth, S.; Megens, R.T.A.; et al. Histone deacetylase 9 activates IKK to regulate atherosclerotic plaque vulnerability. Circ. Res. 2020, 127, 811–823. [Google Scholar] [CrossRef] [PubMed]
- Illi, B.; Dello Russo, C.; Colussi, C.; Rosati, J.; Pallaoro, M.; Spallotta, F.; Rotili, D.; Spallotta, F.; Rotili, D.; Valente, S.; et al. Nitric oxide modulates chromatin folding in human endothelial cells via protein phosphatase 2A activation and class II histone deacetylases nuclear shuttling. Circ. Res. 2008, 102, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, J.T.; Antony, L.; Dalrymple, S.L.; Brennen, W.N.; Gerber, S.; Hammers, H.; Wissing, M.; Kachhap, S.; Luo, J.; Xing, L.; et al. Tasquinimod is an allosteric modulator of HDAC4 survival signaling within the compromised cancer microenvironment. Cancer Res. 2013, 73, 1386–1399. [Google Scholar] [CrossRef] [PubMed]
- Shen, F.; Hou, X.; Li, T.; Yu, J.; Chen, H.; Liu, N.; Qiu, A.; Zhuang, S. Pharmacological and genetic inhibition of HDAC4 alleviates renal injury and fibrosis in mice. Front. Pharmacol. 2022, 13, 929334. [Google Scholar] [CrossRef]
- Liu, L.; Zhou, X.; Shetty, S.; Hou, G.; Wang, Q.; Fu, J. HDAC6 inhibition blocks inflammatory signaling and caspase-1 activation in LPS-induced acute lung injury. Toxicol. Appl. Pharmacol. 2019, 370, 178–183. [Google Scholar] [CrossRef]
- Chi, Z.; Byeon, H.E.; Seo, E.; Nguyen, Q.T.; Lee, W.; Jeong, Y.; Choi, J.; Pandey, D.; Berkowitz, D.E.; Kim, J.H.; et al. Histone deacetylase 6 inhibitor tubastatin A attenuates angiotensin II-induced hypertension by preventing cystathionine γ-lyase protein degradation. Pharmacol. Res. 2019, 146, 104281. [Google Scholar] [CrossRef]
- Zhou, B.; Zeng, S.; Li, N.; Yu, L.; Yang, G.; Yang, Y.; Zhang, X.; Fang, M.; Xia, J.; Xu, Y. Angiogenic factor with G patch and FHA domains 1 is a novel regulator of vascular injury. Arter. Thromb. Vasc. Biol. 2017, 37, 675–684. [Google Scholar] [CrossRef]
- dos Santos, C.C.; Han, B.; Andrade, C.F.; Bai, X.; Uhlig, S.; Hubmayr, R.; Tsang, M.; Lodyga, M.; Keshavjee, S.; Slutsky, A.S.; et al. DNA microarray analysis of gene expression in alveolar epithelial cells in response to TNF-alpha, LPS, and cyclic stretch. Physiol. Genom. 2004, 19, 331–342. [Google Scholar] [CrossRef]
- dos Santos, C.C.; Okutani, D.; Hu, P.; Han, B.; Crimi, E.; He, X.; Keshavjee, S.; Greenwood, C.; Slutsky, A.S.; Zhang, H.; et al. Differential gene profiling in acute lung injury identifies injury-specific gene expression. Crit. Care Med. 2008, 36, 855–865. [Google Scholar] [CrossRef]
- Lynn, H.; Sun, X.; Casanova, N.; Gonzales-Garay, M.; Bime, C.; Garcia, J.G.N. Genomic and genetic approaches to deciphering acute respiratory distress syndrome risk and mortality. Antioxid. Redox Signal. 2019, 31, 1027–1052. [Google Scholar] [CrossRef] [PubMed]
- Göttlicher, M.; Minucci, S.; Zhu, P.; Krämer, O.H.; Schimpf, A.; Giavara, S.; Sleeman, J.P.; Lo Coco, F.; Nervi, C.; Pelicci, P.G.; et al. Valproic acid defines a novel class of HDAC inhibitors inducing differentiation of transformed cells. EMBO J. 2001, 20, 6969–6978. [Google Scholar] [CrossRef] [PubMed]
- Sztajnkrycer, M.D. Valproic acid toxicity: Overview and management. J. Toxicol. Clin. Toxicol. 2002, 40, 789–801. [Google Scholar] [CrossRef] [PubMed]
- Verin, A.D. Letter to the Editor: “Histone deacetylase 7 inhibition in a murine model of Gram-negative Pneumonia-induced acute lung injury”. Shock 2020, 53, 375. [Google Scholar] [CrossRef]
- Li, L.F.; Lee, C.S.; Lin, C.W.; Chen, N.H.; Chuang, L.P.; Hung, C.Y.; Liu, Y.Y. Trichostatin A attenuates ventilation-augmented epithelial-mesenchymal transition in mice with bleomycin-induced acute lung injury by suppressing the Akt pathway. PLoS ONE 2017, 12, e0172571. [Google Scholar] [CrossRef]
- Chen, H.Y.; Li, L.; Fu, Z.J. Histone deacetylase inhibitors trichostatin A and suberoylanilide hydroxamic acid attenuate ventilator-induced lung injury. Pharmazie 2014, 69, 55–59. [Google Scholar]
- Ni, Y.F.; Wang, J.; Yan, X.L.; Tian, F.; Zhao, J.B.; Wang, Y.J.; Jiang, T. Histone deacetylase inhibitor, butyrate, attenuates lipopolysaccharide-induced acute lung injury in mice. Respir. Res. 2010, 11, 33. [Google Scholar] [CrossRef]
- Zhang, L.; Jin, S.; Wang, C.; Jiang, R.; Wan, J. Histone deacetylase inhibitors attenuate acute lung injury during cecal ligation and puncture-induced polymicrobial sepsis. World J. Surg. 2010, 34, 1676–1683. [Google Scholar] [CrossRef]
- Pooladanda, V.; Thatikonda, S.; Bale, S.; Pattnaik, B.; Sigalapalli, D.K.; Bathini, N.B.; Singh, S.B.; Godugu, C. Nimbolide protects against endotoxin-induced acute respiratory distress syndrome by inhibiting TNF-α mediated NF-κB and HDAC-3 nuclear translocation. Cell Death Dis. 2019, 10, 81. [Google Scholar] [CrossRef]
- Leus, N.G.; van der Wouden, P.E.; van den Bosch, T.; Hooghiemstra, W.T.R.; Ourailidou, M.E.; Kistemaker, L.E.; Bischoff, R.; Gosens, R.; Haisma, H.J.; Dekker, F.J. HDAC 3-selective inhibitor RGFP966 demonstrates anti-inflammatory properties in RAW 264.7 macrophages and mouse precision-cut lung slices by attenuating NF-κB p65 transcriptional activity. Biochem. Pharmacol. 2016, 108, 58–74. [Google Scholar] [CrossRef]
- Nguyen, H.C.B.; Adlanmerini, M.; Hauck, A.K.; Lazar, M.A. Dichotomous engagement of HDAC3 activity governs inflammatory responses. Nature 2020, 584, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Ning, L.; Rui, X.; Bo, W.; Qing, G. The critical roles of histone deacetylase 3 in the pathogenesis of solid organ injury. Cell Death Dis. 2021, 12, 734. [Google Scholar] [CrossRef] [PubMed]
- Lauffer, B.E.; Mintzer, R.; Fong, R.; Mukund, S.; Tam, C.; Zilberleyb, I.; Flicke, B.; Ritscher, A.; Fedorowicz, G.; Vallero, R.; et al. Histone deacetylase (HDAC) inhibitor kinetic rate constants correlate with cellular histone acetylation but not transcription and cell viability. J. Biol. Chem. 2013, 288, 26926–26943. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K.; Jung, S.M.; Park, K.S.; Kim, K.J. Integrative analysis of lung molecular signatures reveals key drivers of idiopathic pulmonary fibrosis. BMC Pulm. Med. 2021, 21, 404. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.M.; Park, K.S.; Kim, K.J. Integrative analysis of lung molecular signatures reveals key drivers of systemic sclerosis-associated interstitial lung disease. Ann. Rheum. Dis. 2022, 81, 108–116. [Google Scholar] [CrossRef]
- Bergougnoux, A.; Petit, A.; Knabe, L.; Bribes, E.; Chiron, R.; De Sario, A.; Claustres, M.; Molinari, N.; Vachier, I.; Taulan-Cadars, M.; et al. The HDAC inhibitor SAHA does not rescue CFTR membrane expression in Cystic Fibrosis. Int. J. Biochem. Cell Biol. 2017, 88, 124–132. [Google Scholar] [CrossRef]
- Barnes, P.J. Histone deacetylase-2 and airway disease. Ther. Adv. Respir. Dis. 2009, 3, 235–243. [Google Scholar] [CrossRef]
- Barnes, P.J. Role of HDAC2 in the pathophysiology of COPD. Annu. Rev. Physiol. 2009, 71, 451–464. [Google Scholar] [CrossRef]
- Kee, H.J.; Kim, I.; Jeong, M.H. Zinc-dependent histone deacetylases: Potential therapeutic targets for arterial hypertension. Biochem. Pharmacol. 2022, 202, 115111. [Google Scholar] [CrossRef]
- Su, Y.; Han, W.; Kovacs-Kasa, A.; Verin, A.D.; Kovacs, L. HDAC6 Activates ERK in airway and pulmonary vascular remodeling of chronic obstructive pulmonary disease. Am. J. Respir. Cell Mol. Biol. 2021, 65, 603–614. [Google Scholar] [CrossRef]
- Wang, Y.; Wallach, J.; Duane, S.; Wang, Y.; Wu, J.; Wang, J.; Adejare, A.; Ma, H. Developing selective histone deacetylases (HDACs) inhibitors through ebselen and analogs. Drug Des. Dev. Ther. 2017, 11, 1369–1382. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Zheng, R.; Sun, S. Drug Repurposing: Escitalopram attenuates acute lung injury by inhibiting the SIK2/ HDAC4/ NF-κB signaling cascade. Biochem. Biophys. Res. Commun. 2022, 599, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Zhang, Y.; Tu, T.; Schmull, S.; Han, Y.; Wang, W.; Li, H. Dual inhibition of HDAC and tyrosine kinase signaling pathways with CUDC-907 attenuates TGFβ1 induced lung and tumor fibrosis. Cell Death Dis. 2020, 11, 765. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).