Assessing the Impact of Risk Factors on Vaccination Uptake Policy Decisions Using a Bayesian Network (BN) Approach
Abstract
1. Introduction
1.1. Global Overview of Vaccine Hesitancy Factors That Influence COVID-19 Vaccine Uptake
1.2. Research Gaps
1.3. Decision-Making in the Context of Vaccination Uptake
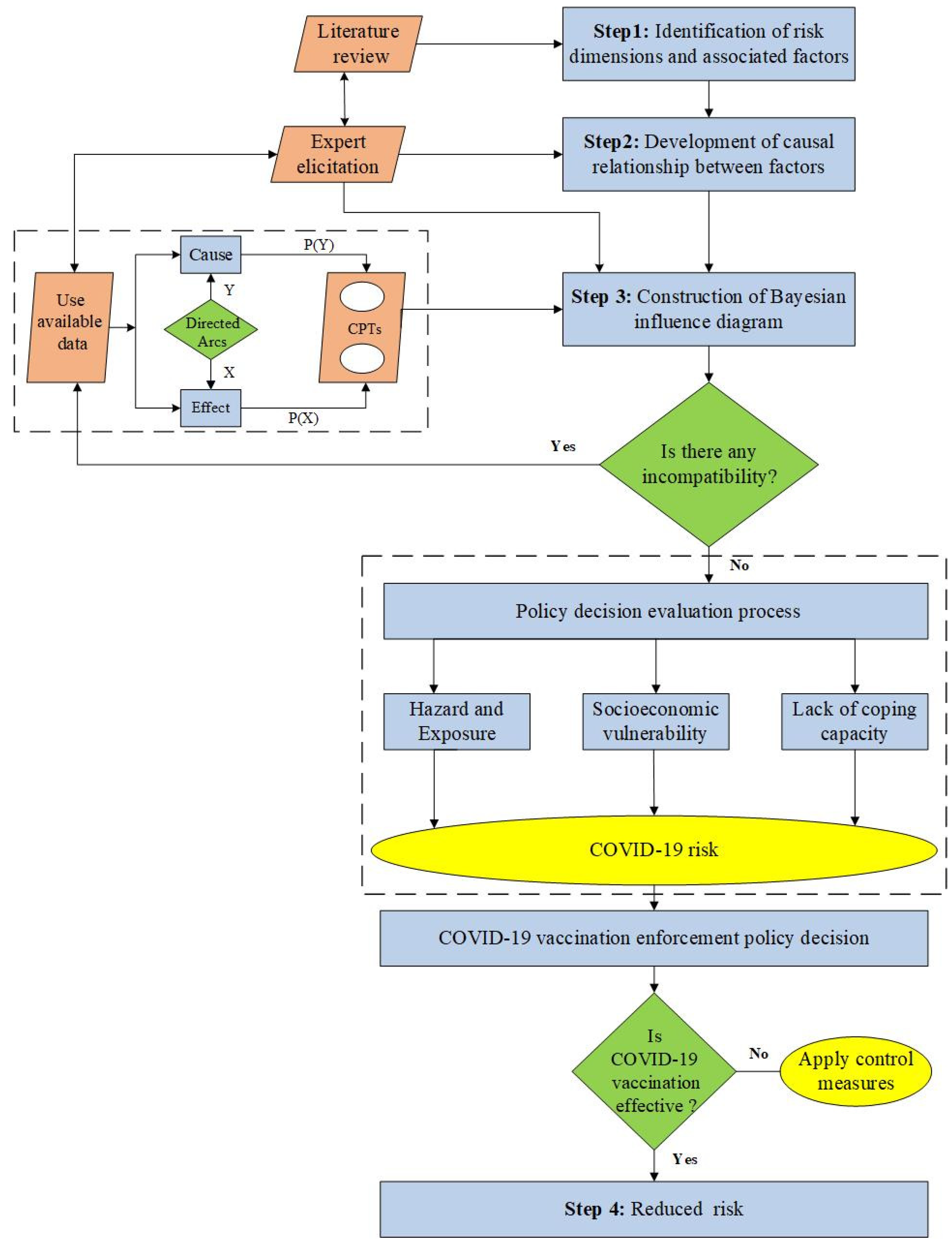
2. Materials and Methods
2.1. Study Area
2.2. Evaluation Strategy
3. Results
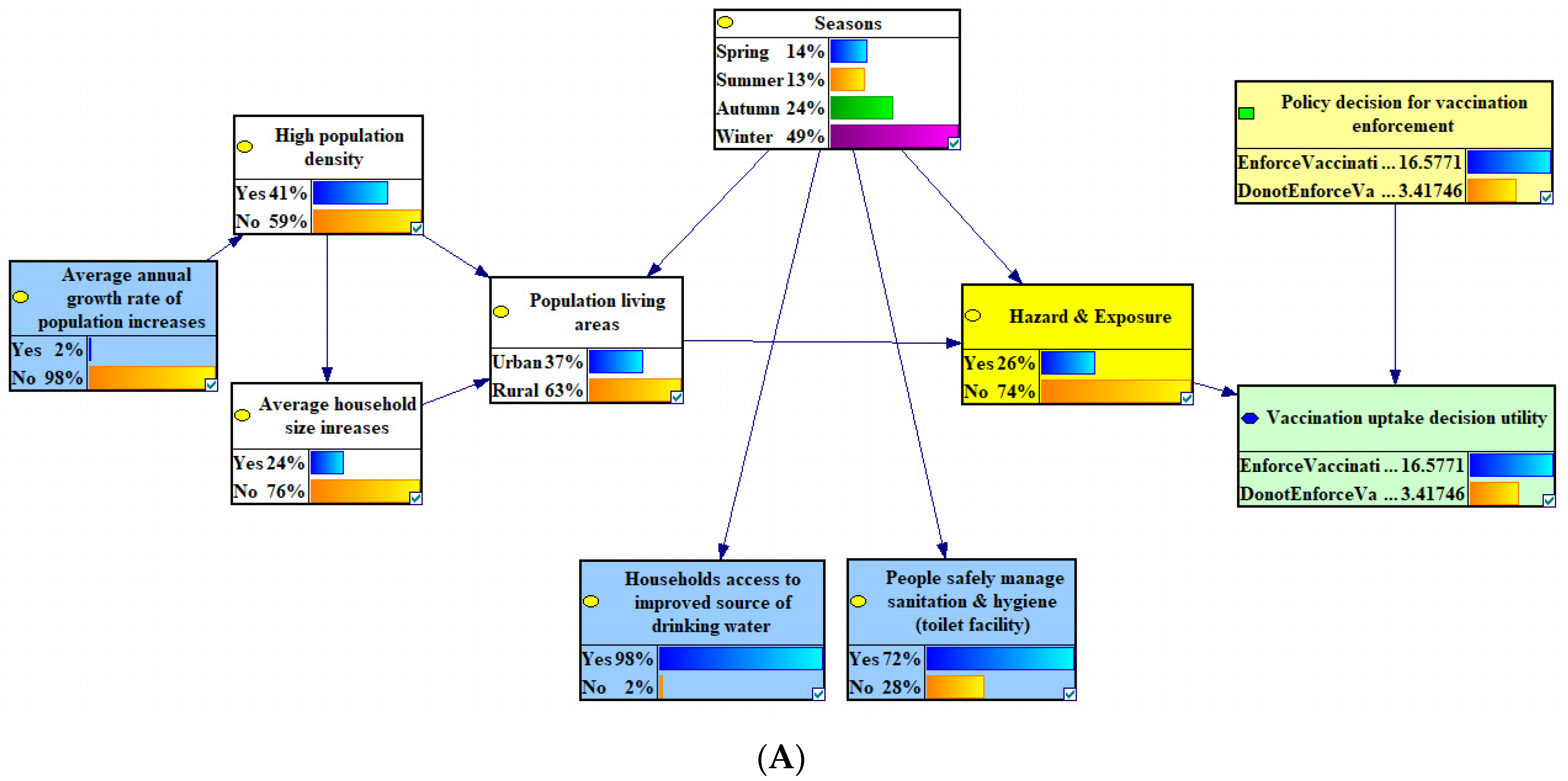
3.1. Hazard and Exposure Results
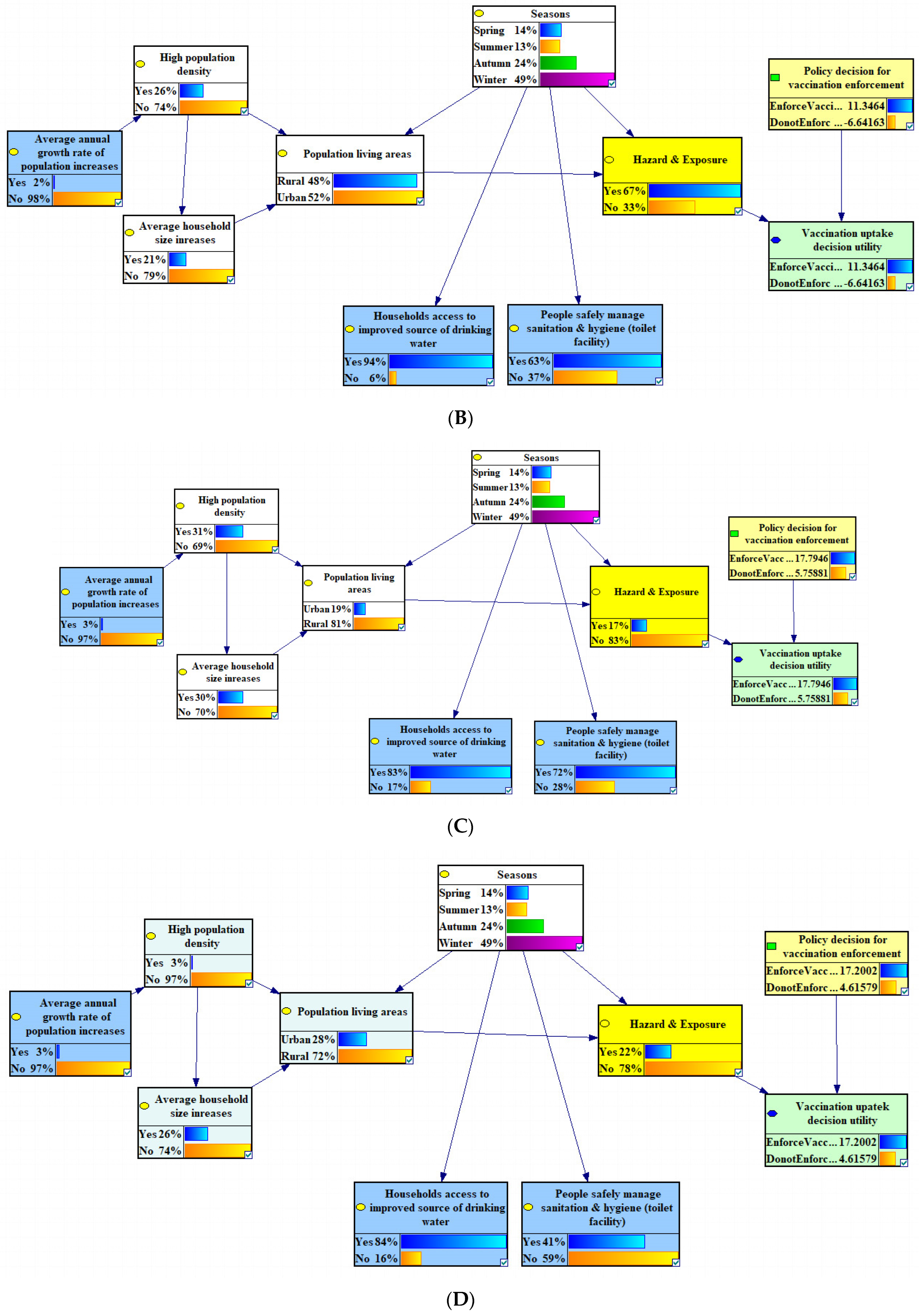
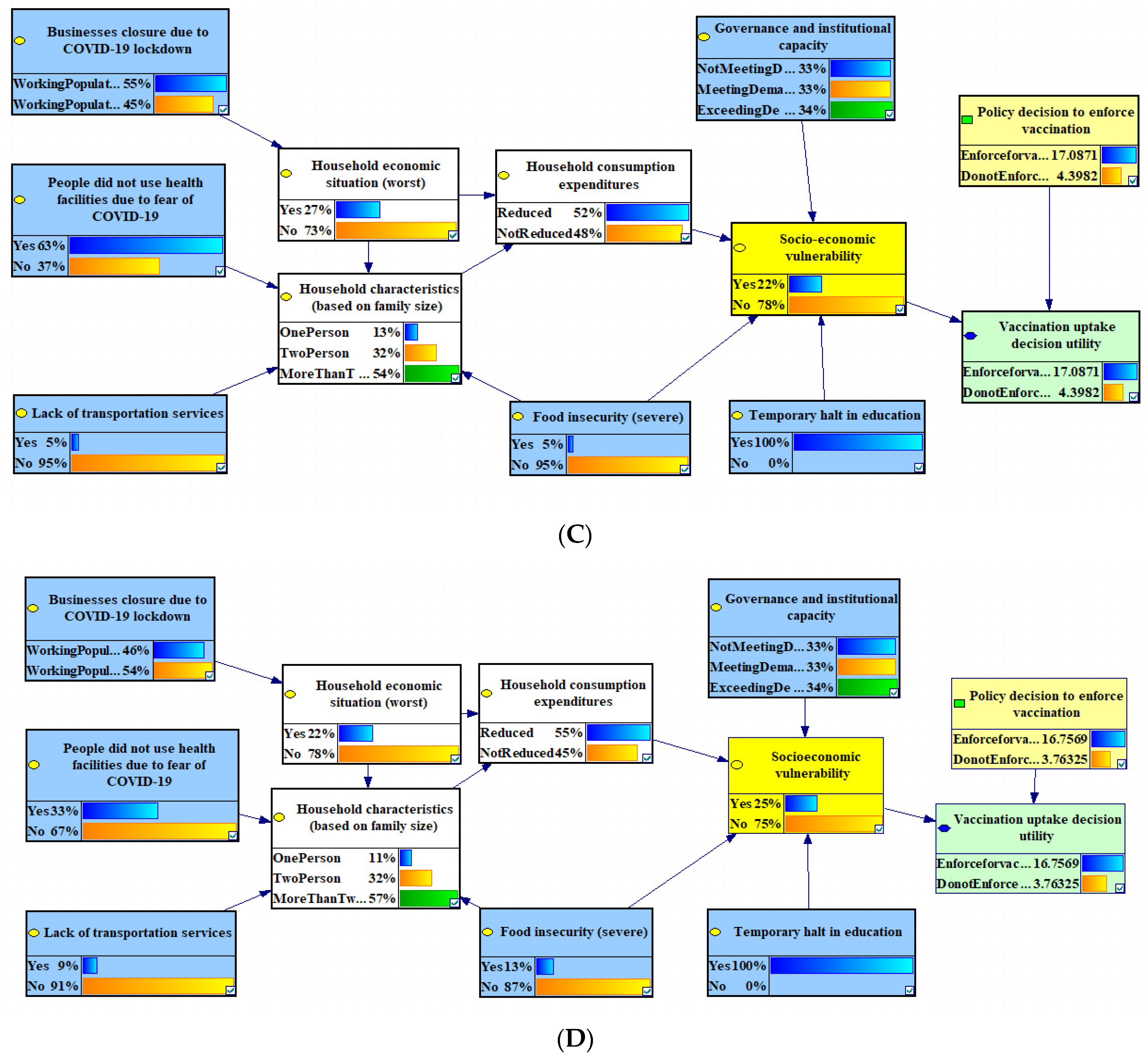
3.2. Socio-Economic Vulnerability
3.3. Lack of Coping Capacity
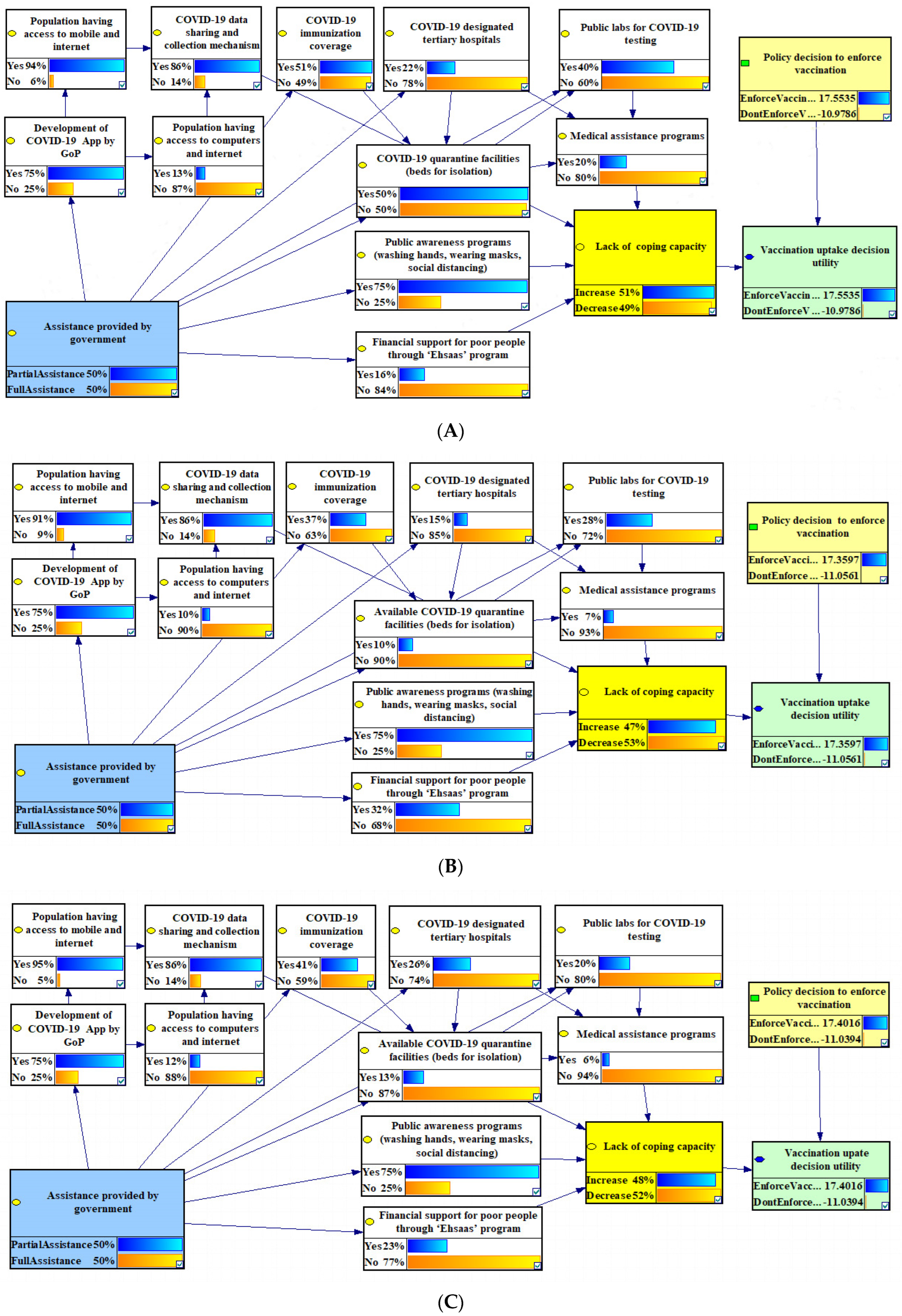
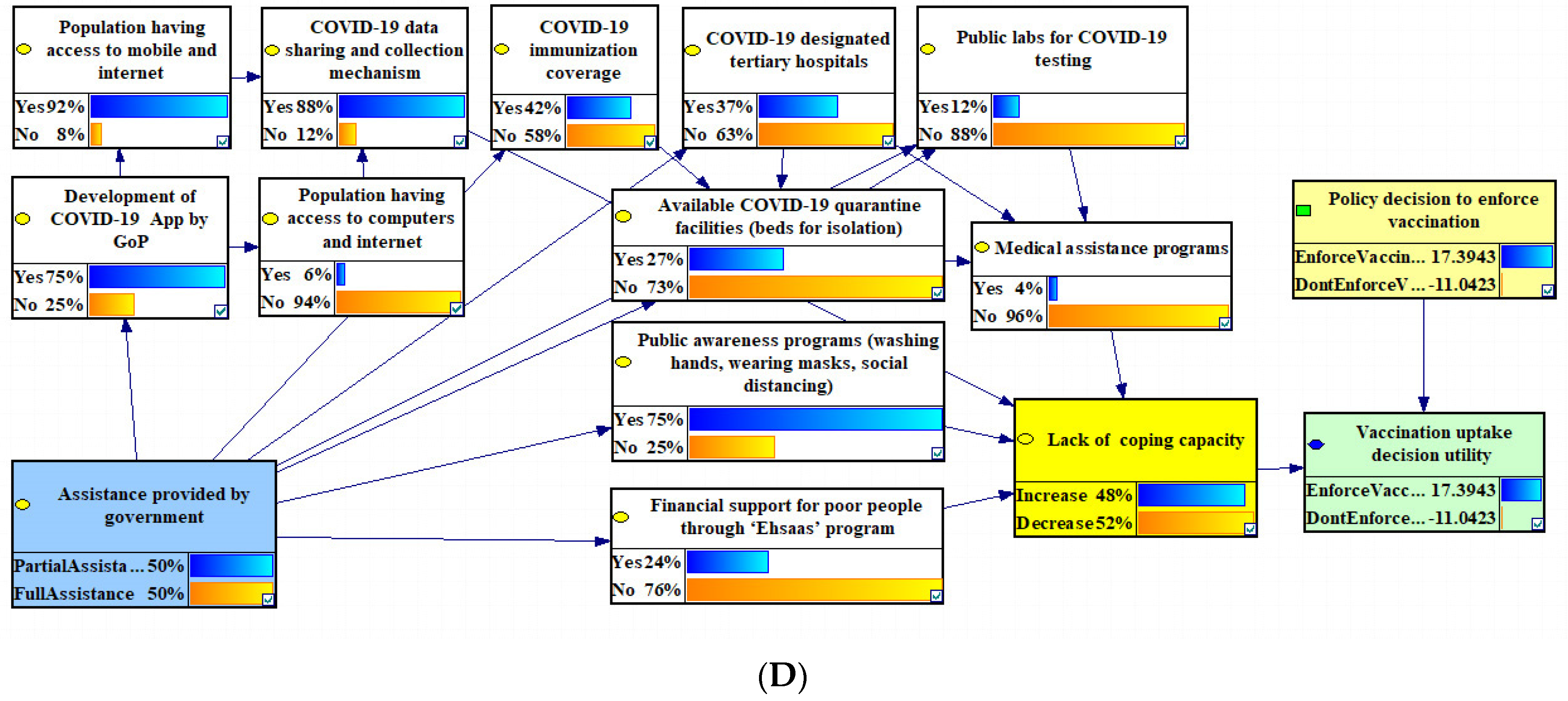
3.4. Total COVID-19 Risk
4. Discussion
4.1. Hazard and Exposure
4.2. Socio-Economic Vulnerability
4.3. Lack of Coping Capacity
4.4. Total COVID-19 Risk
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Agarwal, R.; Gopinath, G.; Farrar, J.; Hatchett, R.; Sands, P. A Global Strategy to Manage the Long-Term Risks of COVID-19; IMF Working Papers; IMF Publications: Washington, DC, USA, 2022. [Google Scholar]
- Sajid, Z. A dynamic risk assessment model to assess the impact of the coronavirus (COVID-19) on the sustainability of the biomass supply chain: A case study of a US biofuel industry. Renew. Sustain. Energy Rev. 2021, 151, 111574. [Google Scholar] [CrossRef] [PubMed]
- Al-Hasan, A.; Khuntia, J.; Yim, D. Does seeing what others do through social media influence vaccine uptake and help in herd immunity through vaccination? A cross-sectional analysis. Front. Public Health 2021, 9, 715931. [Google Scholar] [CrossRef] [PubMed]
- Andersson, P.A.; Tinghög, G.; Västfjäll, D. The effect of herd immunity thresholds on willingness to vaccinate. Humanit. Soc. Sci. Commun. 2022, 9, 243. [Google Scholar] [CrossRef] [PubMed]
- Forman, R.; Shah, S.; Jeurissen, P.; Jit, M.; Mossialos, E. COVID-19 vaccine challenges: What have we learned so far and what remains to be done? Health Policy 2021, 125, 553–567. [Google Scholar] [CrossRef] [PubMed]
- Yahia, A.I.O.; Alshahrani, A.M.; Alsulmi, W.G.H.; Alqarni, M.M.M.; Abdulrahim, T.K.A.; Heba, W.F.H.; Alqarni, T.A.A.; Alharthi, K.A.Z.; Buhran, A.A.A. Determinants of COVID-19 vaccine acceptance and hesitancy: A cross-sectional study in Saudi Arabia. Hum. Vaccines Immunother. 2021, 17, 4015–4020. [Google Scholar] [CrossRef]
- Valckx, S.; Crèvecoeur, J.; Verelst, F.; Vranckx, M.; Hendrickx, G.; Hens, N.; Van Damme, P.; Pepermans, K.; Beutels, P.; Neyens, T. Individual factors influencing COVID-19 vaccine acceptance in between and during pandemic waves (July–December 2020). Vaccine 2022, 40, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Giannouchos, T.V.; Steletou, E.; Saridi, M.; Souliotis, K. Mandatory vaccination support and intentions to get vaccinated for COVID-19: Results from a nationally representative general population survey in October 2020 in Greece. J. Eval. Clin. Pract. 2021, 27, 996–1003. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 2020, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Hu, Y.; Xu, M.; Chen, Z.; Yang, W.; Jiang, Z.; Li, M.; Jin, H.; Cui, G.; Chen, P.; et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy adults aged 60 years and older: A randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 2021, 21, 803–812. [Google Scholar] [CrossRef]
- Amit, S.; Regev-Yochay, G.; Afek, A.; Kreiss, Y.; Leshem, E. Early rate reductions of SARS-CoV-2 infection and COVID-19 in BNT162b2 vaccine recipients. Lancet 2021, 397, 875–877. [Google Scholar] [CrossRef]
- Haas, E.J.; Angulo, F.J.; McLaughlin, J.M.; Anis, E.; Singer, S.R.; Khan, F.; Brooks, N.; Smaja, M.; Mircus, G.; Pan, K.; et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: An observational study using national surveillance data. Lancet 2021, 397, 1819–1829. [Google Scholar] [CrossRef]
- Hall, V.J.; Foulkes, S.; Charlett, A.; Atti, A.; Monk, E.J.; Simmons, R.; Wellington, E.; Cole, M.J.; Saei, A.; Oguti, B.; et al. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative healthcare workers in England: A large, multicentre, prospective cohort study (SIREN). Lancet 2021, 397, 1459–1469. [Google Scholar] [CrossRef]
- Khalife, J.; VanGennep, D. COVID-19 herd immunity in the absence of a vaccine: An irresponsible approach. Epidemiol. Health 2021, 43, e2021012. [Google Scholar] [CrossRef] [PubMed]
- Lacsa, J.E.M.; Cordero, D.A., Jr. We are here… so where’s the vaccine? Achieving ‘herd immunity in the midst of the COVID-19 pandemic. J. Public Health 2021, 43, e533–e534. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Costantino, V.; Trent, M. Modelling of COVID-19 vaccination strategies and herd immunity, in scenarios of limited and full vaccine supply in NSW, Australia. Vaccine 2022, 40, 2506–2513. [Google Scholar] [CrossRef]
- Peters, M.D. Addressing vaccine hesitancy and resistance for COVID-19 vaccines. Int. J. Nurs. Stud. 2022, 131, 104241. [Google Scholar] [CrossRef]
- Hotez, P.J.; Cooney, R.E.; Benjamin, R.M.; Brewer, N.T.; Buttenheim, A.M.; Callaghan, T.; Caplan, A.; Carpiano, R.M.; Clinton, C.; DiResta, R.; et al. Announcing the Lancet Commission on vaccine refusal, acceptance, and demand in the USA. Lancet 2021, 397, 1165–1167. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2022, 52, 3127–3141. [Google Scholar] [CrossRef]
- Geoghegan, S.; O’Callaghan, K.P.; Offit, P.A. Vaccine safety: Myths and misinformation. Front. Microbiol. 2020, 11, 372. [Google Scholar] [CrossRef]
- Shen, A. Finding a way to address a wicked problem: Vaccines, vaccination, and a shared understanding. Hum. Vaccines Immunother 2020, 16, 1030–1033. [Google Scholar] [CrossRef]
- Butter, S.; McGlinchey, E.; Berry, E.; Armour, C. Psychological, social, and situational factors associated with COVID-19 vaccination intentions: A study of UK key workers and non-key workers. Br. J. Health Psychol. 2022, 27, 13–29. [Google Scholar] [CrossRef]
- WHO. Report of the SAGE Working Group on Vaccine Hesitancy; World Health Organization: Geneva, Switzerland, 2014; p. 64.
- Biswas, M.R.; Alzubaidi, M.S.; Shah, U.; Abd-Alrazaq, A.A.; Shah, Z. A scoping review to find out worldwide COVID-19 vaccine hesitancy and its underlying determinants. Vaccines 2021, 9, 1243. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Gagnon, D.; Nickels, E.; Jeram, S.; Schuster, M. Mapping vaccine hesitancy—Country-specific characteristics of a global phenomenon. Vaccine 2014, 32, 6649–6654. [Google Scholar] [CrossRef]
- Al-Amer, R.; Maneze, D.; Everett, B.; Montayre, J.; Villarosa, A.R.; Dwekat, E.; Salamonson, Y. COVID-19 vaccination intention in the first year of the pandemic: A systematic review. J. Clin. Nurs. 2022, 31, 62–86. [Google Scholar] [CrossRef] [PubMed]
- AlShurman, B.A.; Khan, A.F.; Mac, C.; Majeed, M.; Butt, Z.A. What demographic, social, and contextual factors influence the intention to use COVID-19 vaccines: A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 9342. [Google Scholar] [CrossRef] [PubMed]
- Al-Jayyousi, G.F.; Sherbash, M.A.M.; Ali, L.A.M.; El-Heneidy, A.; Alhussaini, N.W.Z.; Elhassan, M.E.A.; Nazzal, M.A. Factors influencing public attitudes towards COVID-19 vaccination: A scoping review informed by the socio-ecological model. Vaccines 2021, 9, 548. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Leigh, J.P.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 2022, 13, 3801. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Gudi, N.; Nambiar, D.; Dumka, N.; Ahmed, T.; Sonawane, I.R.; Kotwal, A. A rapid review of evidence on the determinants of and strategies for COVID-19 vaccine acceptance in low and middle-income countries. J. Glob. Health 2021, 11, 05027. [Google Scholar] [CrossRef] [PubMed]
- Solís Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef]
- Roy, D.N.; Biswas, M.; Islam, E.; Azam, S. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: A systematic review. PLoS ONE 2022, 17, e0265496. [Google Scholar] [CrossRef]
- Fajar, J.K.; Sallam, M.; Soegiarto, G.; Sugiri, Y.J.; Anshory, M.; Wulandari, L.; Kosasih, S.A.P.; Ilmawan, M.; Kusnaeni, K.; Fikri, M.; et al. Global Prevalence and Potential Influencing Factors of COVID-19 Vaccination Hesitancy: A Meta-Analysis. Vaccines 2022, 10, 1356. [Google Scholar] [CrossRef] [PubMed]
- Poljansek, K.; Vernaccini, L.; Dalla Valle, D.; Orenaike, O.; Galimberti, L. INFORM Covid-19 Warning Tool: Concept and Methodology; Publications Office of the European Union: Kirchberg, Luxembourg, 2021. [Google Scholar]
- Peleg, K.; Bodas, M.; Hertelendy, A.J.; Kirsch, T.D. The COVID-19 pandemic challenge to the All-Hazards Approach for disaster planning. Int. J. Disaster Risk Reduct. 2021, 55, 102103. [Google Scholar] [CrossRef]
- Petroni, M.; Hill, D.; Younes, L.; Barkman, L.; Howard, S.; Howell, I.B.; Mirowsky, J.; Collins, M.B. Hazardous air pollutant exposure as a contributing factor to COVID-19 mortality in the United States. Environ. Res. Lett. 2020, 15, 0940a9. [Google Scholar] [CrossRef]
- Chaudhary, M.T.; Piracha, A. Natural disasters—Origins, impacts, management. Encyclopedia 2021, 1, 1101–1131. [Google Scholar] [CrossRef]
- Duvat, V.K.; Volto, N.; Stahl, L.; Moatty, A.; Defossez, S.; Desarthe, J.; Grancher, D.; Pillet, V. Understanding interlinkages between long-term trajectory of exposure and vulnerability, path dependency and cascading impacts of disasters in Saint-Martin (Caribbean). Glob. Environ. Chang. 2021, 67, 102236. [Google Scholar] [CrossRef]
- Sam, P. Redefining vulnerability in the era of COVID-19. Lancet 2020, 395, 1089. [Google Scholar]
- Chen, Y.; Klein, S.L.; Garibaldi, B.T.; Li, H.; Wu, C.; Osevala, N.M.; Li, T.; Margolick, J.B.; Pawelec, G.; Leng, S.X. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res. Rev. 2021, 65, 101205. [Google Scholar] [CrossRef]
- Tavares, F.F.; Betti, G. The pandemic of poverty, vulnerability, and COVID-19: Evidence from a fuzzy multidimensional analysis of deprivations in Brazil. World Dev. 2021, 139, 105307. [Google Scholar] [CrossRef]
- Capano, G.; Howlett, M.; Jarvis, D.S.; Ramesh, M.; Goyal, N. Mobilizing policy (in) capacity to fight COVID-19: Understanding variations in state responses. Policy Soc. 2020, 39, 285–308. [Google Scholar] [CrossRef] [PubMed]
- Baniamin, H.M.; Rahman, M.; Hasan, M.T. The COVID-19 pandemic: Why are some countries coping more successfully than others? Asia Pac. J. Public Adm. 2020, 42, 153–169. [Google Scholar] [CrossRef]
- Serikbayeva, B.; Abdulla, K.; Oskenbayev, Y. State capacity in responding to COVID-19. Int. J. Public Adm. 2021, 44, 920–930. [Google Scholar] [CrossRef]
- Ferguson, N. Capturing human behaviour. Nature 2007, 446, 733. [Google Scholar] [CrossRef] [PubMed]
- Tomassen, F.; de Koeijer, A.; Mourits, M.; Dekker, A.; Bouma, A.; Huirne, R. A decision-tree to optimise control measures during the early stage of a foot-and-mouth disease epidemic. Prev. Vet. Med. 2002, 54, 301–324. [Google Scholar] [CrossRef] [PubMed]
- Sok, J.; Hogeveen, H.; Elbers, A.; Velthuis, A.; Lansink, A.O. Expected utility of voluntary vaccination in the middle of an emergent Bluetongue virus serotype 8 epidemic: A decision analysis parameterized for Dutch circumstances. Prev. Vet. Med. 2014, 115, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Karnon, J. A Simple Decision Analysis of a Mandatory Lockdown Response to the COVID-19 Pandemic; Springer: Berlin/Heidelberg, Germany, 2020; pp. 329–331. [Google Scholar]
- Tharwani, Z.H.; Kumar, P.; Marfani, W.B.; Shaeen, S.K.; Adnan, A.; Mohanan, P.; Islam, Z.; Essar, M.Y. What has been learned about COVID-19 vaccine hesitancy in Pakistan: Insights from a narrative review. Health Sci. Rep. 2022, 5, e940. [Google Scholar] [CrossRef]
- Butt, M.; Mohammed, R.; Butt, E.; Butt, S.; Xiang, J. Why have immunization efforts in Pakistan failed to achieve global standards of vaccination uptake and infectious disease control? Risk Manag. Healthc. Policy 2020, 13, 111. [Google Scholar] [CrossRef] [PubMed]
- Jamal, D.; Zaidi, S.; Husain, S.; Orr, D.W.; Riaz, A.; Farrukhi, A.A.; Najmi, R. Low vaccination in rural Sindh, Pakistan: A case of refusal, ignorance or access? Vaccine 2020, 38, 4747–4754. [Google Scholar] [CrossRef] [PubMed]
- Perveen, S.; Akram, M.; Nasar, A.; Arshad-Ayaz, A.; Naseem, A. Vaccination-hesitancy and vaccination-inequality challenges in Pakistan’s COVID-19 response. J. Community Psychol. 2022, 50, 666–683. [Google Scholar] [CrossRef]
- Sajid, Z.; Khan, F.; Zhang, Y. Integration of interpretive structural modelling with Bayesian network for biodiesel performance analysis. Renew. Energy 2017, 107, 194–203. [Google Scholar] [CrossRef]
- Dao, U.; Sajid, Z.; Khan, F.; Zhang, Y. Safety analysis of blended hydrogen pipelines using dynamic object-oriented bayesian network. Int. J. Hydrog. Energy 2024, 52, 841–856. [Google Scholar] [CrossRef]
- PBS. Pakistan Social And Living Standards Measurement Survey; Government of Pakistan: Islamabad, Pakistan, 2021. [Google Scholar]
- PBS. Special Survey for Evaluating Socio-Economic Impact of COVID-19 on Wellbeing of People 2020; Pakistan Bureau of Statistics: Islamabad, Pakistan, 2020. [Google Scholar]
- PBS. Salient Features—6th Population & Housing Census 2017; Government of Pakistan: Islamabad, Pakistan, 2017. [Google Scholar]
- PBS. Pakistan Demographic Survey (PDS); Government of Pakistan: Islamabad, Pakistan, 2006. [Google Scholar]
- NCOC. Current Laboratory Testing Capacity for COVID-19 In Pakistan; Government of Pakistan: Islamabad, Pakistan, 2021. [Google Scholar]
- NCOC. List of Province-Wise Quarantine Facilities in Pakistan; Government of Pakistan: Islamabad, Pakistan, 2021. [Google Scholar]
- NCOC. PAK COVID-19 Vaccination Pass App; Government of Pakistan: Islamabad, Pakistan, 2021. [Google Scholar]
- NCOC. National Immunization Management System; Government of Pakistan: Islamabad, Pakistan, 2021. [Google Scholar]
- Hemming, V.; Burgman, M.A.; Hanea, A.M.; McBride, M.F.; Wintle, B.C. A practical guide to structured expert elicitation using the IDEA protocol. Methods Ecol. Evol. 2018, 9, 169–180. [Google Scholar] [CrossRef]
- Schmidt, O.; Gambhir, A.; Staffell, I.; Hawkes, A.; Nelson, J.; Few, S. Future cost and performance of water electrolysis: An expert elicitation study. Int. J. Hydrog. Energy 2017, 42, 30470–30492. [Google Scholar] [CrossRef]
- Jensen, F.V.; Nielsen, T.D. Bayesian Networks, and Decision Graphs; Springer: Berlin/Heidelberg, Germany, 2007; Volume 2. [Google Scholar]
- Zhang, L.W.; Guo, H.P. Introduction to Bayesian Networks; China Science Publishing & Media Ltd. (CSPM): Beijing, China, 2006. [Google Scholar]
- Arlot, S.; Celisse, A. A survey of cross-validation procedures for model selection. Stat. Surv. 2010, 4, 40–79. [Google Scholar] [CrossRef]
- Marcot, B.G.; Hanea, A.M. What is an optimal value of k in k-fold cross-validation in discrete Bayesian network analysis? Comput. Stat. 2021, 36, 2009–2031. [Google Scholar] [CrossRef]
- Durr-e-Nayab, N.U.H. PIDE COVID-19 E-Book; Pakistan Institute of Development Economics (PIDE): Islamabad, Pakistan, 2020. [Google Scholar]
- NCOC. List of COVID-19 Designated Tertiary Hospitals in Pakistan; Government of Pakistan: Islamabad, Pakistan, 2021. [Google Scholar]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abbas, H.W.; Sajid, Z.; Dao, U. Assessing the Impact of Risk Factors on Vaccination Uptake Policy Decisions Using a Bayesian Network (BN) Approach. Systems 2024, 12, 167. https://doi.org/10.3390/systems12050167
Abbas HW, Sajid Z, Dao U. Assessing the Impact of Risk Factors on Vaccination Uptake Policy Decisions Using a Bayesian Network (BN) Approach. Systems. 2024; 12(5):167. https://doi.org/10.3390/systems12050167
Chicago/Turabian StyleAbbas, Hafiz Waqar, Zaman Sajid, and Uyen Dao. 2024. "Assessing the Impact of Risk Factors on Vaccination Uptake Policy Decisions Using a Bayesian Network (BN) Approach" Systems 12, no. 5: 167. https://doi.org/10.3390/systems12050167
APA StyleAbbas, H. W., Sajid, Z., & Dao, U. (2024). Assessing the Impact of Risk Factors on Vaccination Uptake Policy Decisions Using a Bayesian Network (BN) Approach. Systems, 12(5), 167. https://doi.org/10.3390/systems12050167






