Abstract
The presence of satisfactory bone volume is fundamental for the achievement of osseointegration. This systematic review aims to analyse the use of titanium meshes in guided bone regeneration in terms of bone gain, survival and success rates of implants, and percentages of exposure. An electronic search was conducted Articles were selected from databases in MEDLINE (PubMed), SCOPUS, Scielo, and Cochrane Library databases to identify studies in which bone regeneration was performed through particulate bone and the use of titanium meshes. Twenty-one studies were included in the review. In total, 382 patients, 416 titanium meshes, and 709 implants were evaluated. The average bone gain was 4.3 mm in horizontal width and 4.11 mm in vertical height. The mesh exposure was highly prevalent (28%). The survival rate of 145 simultaneous implants was 99.5%; the survival rate of 507 delayed implants was 99%. The success rate of 105 simultaneous implants was 97%; the success rate of 285 delayed implants was 95.1%. The clinical studies currently available in the literature have shown the predictability of this technique. It has a high risk of soft tissue dehiscence and membrane exposure although the optimal management of membrane exposition permits obtaining a sufficient bone regeneration volume and prevents compromising the final treatment outcome.
1. Introduction
Satisfactory bone volume is the first condition for obtaining a predictable long-term prognosis in oral implantology. However, some patients may present inadequate bone, which frequently makes difficult the successful outcome of the correct implant placement. Different techniques have been developed to increase bone volume, but at the present time, guided bone regeneration (GBR) represents the gold standard in bone regeneration for implant placement [1,2]. The biological bases of this technique focus on the “PASS” principles: primary closure, angiogenesis, space maintenance, and blood clot stability [3], in other words, this technique focus on the mechanical protection of the blood clot and the isolating of the bone defect, by using a barrier, to facilitate the migration and proliferation of bone-forming cells and to prevent soft tissue colonization inside the bone defect [1,4]. In the last two decades, several membrane designs have been studied. They can be divided into two categories: absorbable and non-resorbable, with different physical and biomaterial properties between them, but all types must have some properties such as biocompatibility, tissue integration, space-making, cell selectivity, tissue integration, and clinical manageability [5,6]. The physical and biomaterial properties of the membranes will influence the development of their function, as well as the result of the treatment, therefore, it will be of great importance to know the advantages and disadvantages of each of them [5,6].
The non-resorbable barriers are expanded and dense forms of titanium-reinforced polytetrafluoroethylene membranes (e-PTFE and d-PTFE), the titanium foils, and perforated titanium meshes (preshaped or customized) (Figure 1).
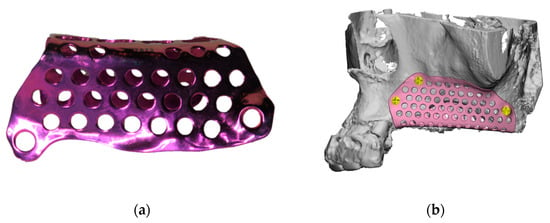
Figure 1.
(a) Custom-made titanium mesh (AVINENT®® Digital Health); (b) Use of Computer-Aided Design (CAD) and Computer-Aided manufacturing (CAM)to design custom-made devices for guided bone regeneration (GBR).
The biggest disadvantage of these types of membranes is they need to be removed with a second-stage surgical procedure. Despite this, they offer several advantages such as, maintaining the space for a sufficient period of time, providing an effective barrier function in terms of biocompatibility, they are simple to manage and present a reduced risk of long-term complications [7].
In cases where vertical augmentation is desired, or in the presence of severe bone atrophy, the use of more resistant and stable membranes is required. To satisfy these requirements, the e-PTFE membranes were subjected to modifications such as titanium reinforcement that favoured their properties and predictability, or the use of screws in its fixation to improve stability [8]. Thus, the titanium mesh appeared to intend to obtain a balance between the ideal malleability and enough rigidity to accomplish reconstructions of wide bone defects [9].
In the last 8 years, only three reviews about this subject have been conducted [10,11,12], therefore, the main objective was to assess the use of titanium meshes during guided bone regeneration, the quantity of augmented bone, survival and success rates of implants, complications, and predictability of this surgical technique.
2. Materials and Methods
The systematic review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) scale [13]).
2.1. Focused Questions
The following focused questions were formulated:
- Is the use of titanium mesh in combination with a particulate bone graft (autologous and/or heterologous) a successful technique regarding the quantity of augmented bone?
- What is the percentage of membrane exposures?
- What are the implant survival, success, and failure rate when performing this bone regeneration technique in simultaneous or delayed implant placement?
2.2. PICO Question
Bulleted lists look like this:
- P: Patients with partially o total edentulism candidates for GBR.
- I: Bone regeneration through autologous and/or heterologous bone graft and the use of titanium meshes.
- C: Different grafting materials and techniques.
- O: The success rate of this technique regarding the quantity of augmented bone, complications, and predictability of this surgical technique.
2.3. Eligibility Criteria
Inclusion criteria: (i) Studies in which a bone regeneration was performed using particulate bone graft (autologous and/or heterologous) and the use of titanium meshes; (ii) Clinical trials, cohort studies, and case series; (iii) Published in English or Spanish; (iv) Minimum 6 months follow-up period.
Exclusion criteria: (i) Studies performed in vitro or on animals; (ii) Systematic reviews, case reports, and expert opinions; (iii) Studies published before January 2000.
2.4. Information Sources
An electronic search was conducted in MEDLINE (PubMed), SCOPUS, Scielo, and Cochrane Library databases for articles published between 2000 and 2021. References of relevant studies selected were also searched to identify articles with potential inclusion. The last search was performed on 8th January 2021.
2.5. Search Strategy
The following search terms were used:
- (Titanium mesh [All Fields] AND bone graft [All Fields]).
- ((Titanium mesh [All Fields] AND (guided bone regeneration [All Fields] OR GBR [All Fields])).
- (Titanium mesh [All Fields] AND ridge augmentation [All Fields]).
2.6. Study Selection
All articles were reviewed initially by three experts (R.A.-A., E.R.-M., and B.G.-N.). In the event of any discrepancies, these were resolved by J.L.-L.
The first phase of the research consisted of the selection of titles, to eliminate those not concerning our research and eliminate the repeated ones. The second phase consisted of reading the abstract of each article to evaluate some parameters of inclusion. Finally, the full text of all studies selected was obtained.
2.7. Data Collection Process and Items
One reviewer R.A.-A., extracted the data from the selected studies, including characteristics of the study (authors, year of publication, country, and design), sample characteristics (number of patients, mean ages, and number of sites), surgery characteristics (the type of defect, type of surgery performed and materials used) and finally, the post-operatory details and outcomes (follow-up period, percentage of membrane exposures, horizontal/vertical bone regeneration obtained and implant survival, success, and failure rate) which were synthesized in Table 1 and Table 5. A second author (B.G.-N.) verified all the information collected.

Table 1.
Characteristics of the included studies.
The implant success rate was evaluated according to Albrektsson et al. criteria [14]: (i) Absence of subjective complaints such as pain, foreign body sensation, and/or dysesthesia; (ii) Absence of mobility; (iii) Absence of peri-implant radiolucency and infection with pus suppuration; (iv) Marginal bone resorption (MBR) not exceeding 1.5 mm after the first year of loading and up to 0.2 mm yearly thereafter.
2.8. Risk of Bias in Individual Studies
The methodology of the included randomized clinical trials (RCT) was evaluated using the Cochrane Collaboration’s risk of bias (RoB 2) tool [15]. The risk of bias for the non-randomized clinical trials (NRCT), was determined using the non-randomized clinical trials of Interventions (ROBINS-I) assessment tool [16]. The risk of bias was classified as “low risk”, “unclear risk”, and “high risk”.
3. Results
3.1. Study Selection
A total of 572 articles were identified in the first phase of the research. During the second phase, 94 articles were considered, and after full-text evaluation 16 studies were included in the review. Finally, five articles of interest were obtained through manual research obtaining a total of 21 articles were included in this review [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] (Figure 2).
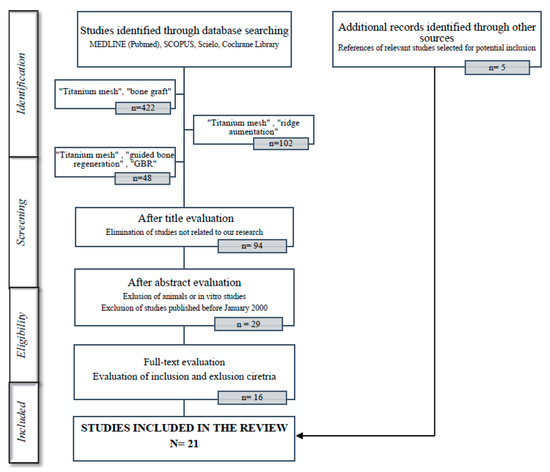
Figure 2.
Flow diagram of study inclusion.
3.2. Study Methods and Characteristics
Four studies were RCT [20,24,33,35], 2 were NRCT [21,28], 2 were prospective studies [22,32] and 13 were case series [17,18,19,23,25,26,27,29,30,31,34,36,37] and all of them were published between 2001 and 2021 (Table 1).
The studies were conducted in nine different countries, the total number of patients included was 382 (137 males, 193 females, and 52 non-specified) and a total of 416 titanium meshes.
There were four articles in which the gender was not specified [20,33,34,35]. The study with a higher number of patients was Miyamoto et al. (N = 41) [17] while the one with fewer patients was Ciocca et al. [29] with a total of nine patients. The mean age was 53.4 and four articles did not specify the mean age [24,27,34,35].
Regarding the characteristics of the surgeries performed, it was quantified the number of sites, and whether if it was in mandible or maxilla. In five studies, the number of sites was not specified [18,28,30,34,35], of which 164 sites belong to the maxilla and 129 to the mandible.
In 16 studies the graft material used was autologous bone; in six of them it was the only material used [17,18,20,21,23,28] (N = 120), and in the other 10 articles, autologous bone was associated with other graft materials such as inorganic bovine bone (ABB) [19,22,25,26,32,35,37] (N = 91), thermoplastic mouldable allograft paste (TMAP) [33] (N = 28), bovine porous bone protein (BPBM) [21] (N = 3), demineralized bovine bone mineral (DBBM) [27] (N = 13) or Hydroxyapatite [29] (N = 21). There were five studies in which autologous bone was not used and the regeneration was performed only with the use of ABB [24,30,34] (N = 67) or TMAP (36,31) (N = 39).
The removal of the mesh and the quantification of bone gains was performed during the second-stage surgery or also called in most studies as healing period, which was performed on average at 6.5 months.
3.3. Quality Assessment and Risk of Bias within Studies
The risk of bias of the RCT is presented in Table 2. Three RTCs were considered as having a low risk of bias even though there were some concerns about the blinding of participants and researchers [24,33,35] and Atef et al. did not report the blinding of outcome assessment and selective outcome reporting, potentially introducing selection bias [35]. One study was considered as having a high risk of bias since there were some concerns about the random sequence generation, the allocation concealment, and the blinding of participants and researchers [20].

Table 2.
Risk of Bias of included randomized clinical trials.
Two non-randomized clinical trials were included, and the risk of bias is represented in Table 3. These two articles were considered as having a low risk of bias but there were some concerns about potential bias in the classification of interventions [21,28] and also due to deviations from intended interventions [21].

Table 3.
Risk of Bias of included non-randomized clinical trials.
(The systematic review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) scale [13]) with 21 items.
3.4. Characteristics of the Mesh
Different types of meshes were used in the studies, all of them are summarized in Table 4.

Table 4.
Characteristics of the meshes used.
3.5. Bone Gain
The bone gains were quantified using cone-beam computed tomography (CBCT) images. In two studies, width bone gain was quantified [30,35], five studies quantified height bone gain [21,23,33,36,37], six studied both width and height bone gains [17,22,24,29,31,34] and finally 5 works did not quantify any bone gains after the surgery [18,22,26,27,29]. The average bone gains were 4.3 mm in horizontal width (range 3.1 mm performed with ABB to 8.6 mm performed with TMAP) and 4.11 mm in vertical height (range 2.56 mm performed with autologous and ABB 50:50 to 8.9 mm performed only with autologous).
One study performed GBR after tooth removal, to evaluate the prevention of alveolar collapse after tooth extraction, using titanium membrane [20].
Four studies evaluated the histologic and histomorphometric outcomes of GBR from biopsies of the newly regenerated bone [19,21,31,33]. According to Bassi et al. [31], the histological and histomorphometric analysis of the samples demonstrates the effectiveness of GBR employing titanium mesh, as a barrier membrane. Cucchi et al. [33] concluded that the regenerated bone differed from the native bone in terms of trabecular organization, as well as newly formed bone remained immature and very different from the native bone. Proussaefs et al. [19] demonstrated 36.47% of bone formation when the titanium mesh was used in combination with autogenous bone and ABB. Corinaldesi et al. [21] concluded that BPBM (30%) in combination with the autologous bone (70%) yielded similar bone formation patterns as autologous bone alone.
3.6. Mesh Exposure
Except for Corinaldesi et al. [21] all the included studies evaluated the mesh exposure (N = 404), and it proved to be a highly prevalent complication, appearing in 115 cases out of 404 meshes (28%) (range 0% to 80%). Of these 115 exposed meshes, 25 were removed due to more severe complications, and 75 were stabilized and controlled through local hygiene measures.
According to the studies in which the implant was placed simultaneously [18,23,30,33,34] the mesh exposure rate was 14% (13 out of 87). In contrast, in the cases of guide bone regeneration (GBR) and delayed implant placement [17,19,21,22,23,24,25,27,29,31,32,37] the mean mesh exposure rate was 30% (58 out of 187).
3.7. Implant Placement
Apart from performing the alveolar ridge augmentation, there were 16 studies in which dental implants were placed [18,19,21,22,23,24,25,27,29,30,31,32,33,34,37] (Table 4). The other five studies focused on the bone regeneration process without involving implant placement. The outcomes were studied and summarized in Table 5.

Table 5.
Evaluation of characteristics of implant placement.
In total, 709 implants were placed and the total prevalence of implant failure in this review was 0.5% (4 implants were lost). The follow-up time after the implant placement was on average of 32 months (range 6 to 96).
In five studies, bone augmentation was performed simultaneously with implant placement (N = 145) [18,23,30,33,34], in the other studies, the implant placement was delayed after 7,1 months on average (N = 564) (range 3 to 10 months) [17,19,21,22,23,24,25,27,29,31,32,37].
The implant success rate was assessed considering at least 6 months from the prosthetic load. The survival rate of 145 simultaneous implants was 99.5%; the survival rate of 507 delayed implants was 99%. The success rate of 105 simultaneous implants was 97%; the success rate of 285 delayed implants was 95.1%. Proussaefs et al. [19] did not specify the survival and success rates and Corinaldesi et al. [21], Torres et al. [24], Zita et al. [30], and Ciocca et al. [32] did not specify the success rate.
The marginal bone resorption (MBR) was evaluated in 6 studies and it was on average of 0.75 mm [19,22,23,24,30,31,37] (N = 234). There were no statistically significant differences between de MBR observed in the simultaneous implants and delayed implants.
4. Discussion
From the analysis of the recent published articles, few studies concerning GBR using titanium mesh were published. The present systematic review aimed to evaluate the results reported in the literature evaluating the following aspects: (a) the success rate of this technique regarding the quantity of augmented bone; (b) the complications rate by means of exposure; (c) the implants survival and success rate. The topic was focused on the presence of the titanium meshes used as a physical barrier for ridge reconstruction in partial or total edentulism, preventing soft tissue colonization and allowing osteoprogenitor cells to reach the site and form new bone.
4.1. Bone Gain
The use of non-resorbable titanium meshes allows maintaining the shape between the barrier and the bone defect. Furthermore, the pores allow to maintain vascularization both to the soft tissue and to the bone during the regeneration process and facilitates tissue nutrition [12,38]. Generally, the literature showed that the use of non-resorbable titanium meshes in GBR represent a safe and predictable technique to gain vertical and/or horizontal bone augmentation, in the treatment of small and medium-sized defects around dental implants and prevention of alveolar ridge after tooth extraction [9,20,30,35]. The analysis of the studies included in the present systematic review corroborates this statement, although only six included studies quantified both width and height bone gains [17,19,22,24,31,34]. The histological and histomorphometric analysis also demonstrates the effectiveness of GBR using the titanium mesh, and good capacity of the method to increase bone volume in the distal mandibular atrophies [19,21,31,33]. On the other hand, other authors like Uehara et al. [29] appear more doubtful about the success of this technique. According to their success criteria, only 13 sites were judged as successful with a success rate of 56.6%, emphasizing that, the greatest success rate was obtained at the sites with a shorter span of augmentation.
When comparing the success of this technique with other GBR techniques such as the use of PTFE membranes, results of bone gain did not differ much. Cucchi et al. [39] found that the height bone gain was 4.2 (range 2.7 to 5.8) mm when using PTFE and 4.1 (range 2.6 to 6.3) mm when using a titanium mesh. Sagheb et al. [40], found a height bone gain higher (4.16 and 5.5 mm).

Table 6.
Incidence of membrane/barrier exposure in different techniques.
Table 6.
Incidence of membrane/barrier exposure in different techniques.
| Author | Type of Barrier/Membrane | Exposure Rate (%) |
|---|---|---|
| Rasia dal Polo et al. [10] | Titanium mesh | 16 |
| Ricci et al. [11] | Titanium mesh | 22 |
| Briguglio et al. [12] | Titanium mesh | 52 |
| Wessing et al. [41] | Collagen membrane | 20 |
| Wessing et al. [41] | Cross-linked membrane | 28 |
| Ricci et al. [11] | d-PTFE | 17 |
| Roca-Millan et al. [42] | Titanium foils | 23 |
4.2. Mesh Exposure
From the analysis of the complications, the investigation was focused on mesh exposures which was the most usual complication when performing this technique. To prevent premature exposure of the augmented area, all the analysed studies highlighted the necessity to mobilize the flaps to obtain a primary wound closure without tensions. According to the results of this review, the mean rate of mesh exposure was 28%. Other reviews about membrane/mesh exposure were found in the literature (Table 6).
The prevalence of mesh exposure in the cases of GBR and delayed implant placement was higher than when simultaneous implant placement. The reason for this higher incidence might be correlated with “free-end” edentulism and severe vertical ridge resorption, as well as a low number of included cases in the simultaneous placement group.
Some authors propose that to reduce the rate of mesh exposure, consensus protocols are needed, but also more precise customized meshes. Also, the use of resorbable membranes and PRP to prevent the risk of early dehiscence [18,43,44].
Even though the most frequent complication associated with this device is its exposure, according to the results of this review, it is worth noting that this event does not necessarily compromise the final treatment outcome and further complications were avoided using topical application of chlorhexidine gel [19,25].
Comparing to other types of techniques, Garcia et al. [45] found that when GBR is associated with collagen membranes or e-PTFE, the exposure of the membrane may influence bone gain. The sites without exposure achieved 74% more horizontal bone gain than sites with membrane exposure. In all types of GBR, meticulous soft-tissue handling is mandatory to obtain flaps without tension over the membranes, in order that the regenerative tissue can be kept entirely covered. When a titanium mesh is exposed and the grafted bone had been sufficiently stabilized by newly formed bone, the integrity of the hole new bone regeneration can be mostly ensured and avoid superinfection. This is possible due to its pores since they play a crucial role in vascularization of the graft and allows its hygiene [19,23,25].
4.3. Characteristics of the Mesh
Regarding the thickness of the mesh most currently used is 0.2 mm (range 0.1–0.5 mm), since it provides sufficient rigidity to maintain space and protect the graft [34,37]. According to other authors, a titanium mesh should be sufficiently stiff to be able to resist the muscular tensions and the pressure of the surgical flap, but at the same quite manageable to be adapted to the bone defect [10,11,12,30,34,37].
The external form should be as round as possible to avoid damaging he flap and the surface as smooth as possible to avoid bacterial colonization or infection [10,12,37]. In most of the articles, the authors specify the devices were polished and rounded before placed, to avoid dehiscence and soft tissue ruptures.
4.4. Implant Success and Survival Rates
It has been reported that the survival rates of implants placed in regenerated bone were similar to those described for implants placed into native bone [44,45]. The implant survival rate of the included articles of this review was 99.25% and the implant success rate was 93.35%, similar to other works available in the literature [46,47].
4.5. Limitations
It must be taken into account the heterogeneity in design, data collection methods, and analyses performed across the included studies. Moreover, the lack of RTCs with a large sample is observed. Most of the included articles were case series, and some of them did not report the bone gain obtained.
Despite the differences regarding the surgical protocols (collagen membrane association, different timing of mesh removal, different graft materials) results were similar. Therefore, it was not easy to identify the most successful surgical technique when a titanium mesh is used.
Only four studies performed controlled randomization [20,24,33,35], and in one of them, the implant timing, the follow-up, and survival/success implant rates were not specified [20].
5. Conclusions
Based on the literature presented, it is possible to assess that the use of a titanium mesh in combination with autologous and/or heterologous particulate grafts represent a safe and predictable technique to increase vertical and/or horizontal bone volume in cases of defects in partially edentulous patients, in the treatment of small and medium-sized defects around dental implants and alveolar ridge preservation after tooth extraction.
However, the use of titanium meshes presented disadvantages related to the necessity of the second-stage surgical procedure, with increased patient morbidity and rehabilitation time. Furthermore, it has a high risk of soft tissue dehiscence and membrane exposure.
The membrane exposure rate of this technique reaches 28% of the cases. The optimal management of membrane exposition permits obtaining a sufficient bone regeneration volume and prevents compromising the final treatment outcome.
The implant survival and implant success values are similar to those described for implants placed into the native bone and when performing other GBR techniques. No significant differences were observed between the implant survival and implant success rates between simultaneous and delayed implant placement.
Author Contributions
Conceptualization, R.A.-A. and B.G.-N.; methodology, R.A.-A. and B.G.-N.; validation, R.A.-A., B.G.-N. and J.L.-L.; formal analysis, R.A.-A.; investigation, R.A.-A. and E.R.-M.; resources, J.L.-L.; data curation, R.A.-A., E.R.-M. and J.L.-L.; writing—original draft preparation, R.A.-A. and E.R.-M.; writing—review and editing, R.A.-A.; visualization, B.G.-N. and J.L.-L.; project administration, A.M.-R., E.V.-O. and J.L.-L.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Elgali, I.; Omar, O.; Dahlin, C.; Thomsen, P. Guided bone regeneration: Materials and biological mechanisms revisited. Eur. J. Oral Sci. 2017, 125, 315–337. [Google Scholar] [CrossRef]
- Chiapasco, M.; Casentini, P.; Zaniboni, M. Bone augmentation procedures in implant dentistry. Int. J. Oral Maxillofac. Implant. 2009, 24, 237–259. [Google Scholar]
- Wang, H.L.; Boyapati, L. “PASS” principles for predictable bone regeneration. Implant. Dent. 2006, 15, 8–17. [Google Scholar] [CrossRef]
- Dahlin, C.; Linde, A.; Gottlow, J.; Nyman, S. Healing of bone defects by guided tissue regeneration. Plast. Reconstr. Surg. 1988, 81, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Hämmerle, C.H.; Jung, R.E.; Feloutzis, A. A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. J. Clin. Periodontol. 2002, 29, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Scantlebury, T.V. 1982–1992: A decade of technology development for guided tissue regeneration. J. Periodontol. 1993, 1129–1137. [Google Scholar] [CrossRef]
- Zhang, J.; Xu, Q.; Huang, C.; Mo, A.; Li, J.; Zuo, Y. Biological properties of an anti-bacterial membrane for guided bone regeneration: An experimental study in rats. Clin. Oral Implant. Res. 2010, 21, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Hämmerle, C.H.; Jung, R.E. Bone augmentation by means of barrier membranes. Periodontology 2000 2003, 33, 36–53. [Google Scholar] [CrossRef]
- Rakhmatia, Y.D.; Ayukawa, Y.; Furuhashi, A.; Koyano, K. Current barrier membranes: Titanium mesh and other membranes for guided bone regeneration in dental applications. J. Prosthodont. Res. 2013, 57, 3–14. [Google Scholar] [CrossRef]
- Ricci, L.; Perrotti, V.; Ravera, L.; Scarano, A.; Piattelli, A.; Iezzi, G. Rehabilitation of deficient alveolar ridges using titanium grids before and simultaneously with implant placement: A systematic review. J. Periodontol. 2013, 84, 1234–1242. [Google Scholar] [CrossRef]
- Rasia-dal Polo, M.; Poli, P.P.; Rancitelli, D.; Beretta, M.; Maiorana, C. Alveolar ridge reconstruction with titanium meshes: A systematic review of the literature. Med. Oral Patol. Oral Cir. Buccal 2014, 19, e639–e646. [Google Scholar] [CrossRef] [PubMed]
- Briguglio, F.; Falcomatà, D.; Marconcini, S.; Fiorillo, L.; Briguglio, R.; Farronato, D. The Use of Titanium Mesh in Guided Bone Regeneration: A Systematic Review. Int. J. Dent. 2019, 2019, 9065423. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group. Preferred reporting ítems for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.-R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implant. 1986, 1, 11–25. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M. ROBINS-1: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Miyamoto, I.; Funaki, K.; Yamauchi, K.; Kodama, T.; Takahashi, T. Alveolar ridge reconstruction with titanium mesh and autogenous particulate bone graft: Computed tomography-based evaluations of augmented bone quality and quantity. Clin. Implant Dent. Relat. Res. 2012, 14, 304–311. [Google Scholar] [CrossRef]
- Degidi, M.; Scarano, A.; Piattelli, A. Regeneration of the alveolar crest using titanium micromesh with autologous bone and a resorbable membrane. J. Oral Implantol. 2003, 29, 86–90. [Google Scholar] [CrossRef]
- Proussaefs, P.; Lozada, J. Use of titanium mesh for staged localized alveolar ridge augmentation: Clinical and histologic-histomorphometric evaluation. J. Oral Implantol. 2006, 32, 237–247. [Google Scholar] [CrossRef]
- Pinho, M.N.; Roriz, V.L.; Novaes, A.B.; Taba, M.; Grisi, M.F.; de Souza, S.L.; Palioto, D.B. Titanium membranes in prevention of alveolar collapse after tooth extraction. Implant. Dent. 2006, 15, 53–61. [Google Scholar] [CrossRef]
- Corinaldesi, G.; Pieri, F.; Marchetti, C.; Fini, M.; Aldini, N.N.; Giardino, R. Histologic and histomorphometric evaluation of alveolar ridge augmentation using bone grafts and titanium micromesh in humans. J. Periodontol. 2007, 78, 1477–1484. [Google Scholar] [CrossRef] [PubMed]
- Pieri, F.; Corinaldesi, G.; Fini, M.; Aldini, N.N.; Giardino, R.; Marchetti, C. Alveolar ridge augmentation with titanium mesh and a combination of autogenous bone and anorganic bovine bone: A 2-year prospective study. J. Periodontol. 2008, 79, 2093–2103. [Google Scholar] [CrossRef] [PubMed]
- Corinaldesi, G.; Pieri, F.; Sapigni, L.; Marchetti, C. Evaluation of survival and success rates of dental implants placed at the time of or after alveolar ridge augmentation with an autogenous mandibular bone graft and titanium mesh: A 3- to 8-year retrospective study. Int. J. Oral Maxillofac. Implant. 2009, 24, 1119–1128. [Google Scholar]
- Torres, J.; Tamimi, F.; Alkhraisat, M.H.; Manchón, A.; Linares, R.; Prados-Frutos, J.C.; Hernández, G.; López Cabarcos, E. Platelet-rich plasma may prevent titanium-mesh exposure in alveolar ridge augmentation with anorganic bovine bone. J. Clin. Periodontol. 2010, 37, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Her, S.; Kang, T.; Fien, M.J. Titanium mesh as an alternative to a membrane for ridge augmentation. J. Oral Maxillofac. Surg. 2012, 70, 803–810. [Google Scholar] [CrossRef]
- Lizio, G.; Corinaldesi, G.; Marchetti, C. Alveolar ridge reconstruction with titanium mesh: A three-dimensional evaluation of factors affecting bone augmentation. Int. J. Oral Maxillofac. Implant. 2014, 1354–1363. [Google Scholar] [CrossRef]
- Poli, P.P.; Beretta, M.; Cicciù, M.; Maiorana, C. Alveolar ridge augmentation with titanium mesh. A retrospective clinical study. Open Dent. J. 2014, 8, 148–158. [Google Scholar] [CrossRef]
- Sumida, T.; Otawa, N.; Kamata, Y.U.; Kamakura, S.; Mtsushita, T.; Kitagaki, H.; Mori, S.; Sasaki, K.; Fujibayashi, S.; Takemoto, M.; et al. Custom-made titanium devices as membranes for bone augmentation in implant treatment: Clinical application and the comparison with conventional titanium mesh. J. Craniomaxillofac. Surg. 2015, 43, 2183–2188. [Google Scholar]
- Uehara, S.; Kurita, H.; Shimane, T.; Sakai, H.; Kamata, T.; Teramoto, Y.; Yamada, S. Predictability of staged localized alveolar ridge augmentation using a micro titanium mesh. Oral Maxillofac. Surg. 2015, 19, 411–416. [Google Scholar] [CrossRef]
- Zita Gomes, R.; Paraud Freixas, A.; Han, C.H.; Bechara, S.; Tawil, I. Alveolar Ridge Reconstruction with Titanium Meshes and Simultaneous Implant Placement: A Retrospective, Multicenter Clinical Study. Biomed. Res. Int. 2016, 2016, 5126838. [Google Scholar] [CrossRef]
- Andreasi Bassi, M.; Andrisani, C.; Lico, S.; Ormanier, Z.; Ottria, L.; Gargari, M. Guided bone regeneration via a preformed titanium foil: Clinical, histological and histomorphometric outcome of a case series. Oral Implantol. 2016, 16, 164–174. [Google Scholar]
- Ciocca, L.; Lizio, G.; Baldissara, P.; Sambuco, A.; Scotti, R.; Corinaldesi, G. Prosthetically CAD-CAM-Guided Bone Augmentation of Atrophic Jaws Using Customized Titanium Mesh: Preliminary Results of an Open Prospective Study. J. Oral Implantol. 2018, 44, 131–137. [Google Scholar] [CrossRef]
- Cucchi, A.; Sartori, M.; Parrilli, A.; Aldini, N.N.; Vignudelli, E.; Corinaldesi, G. Histological and histomorphometric analysis of bone tissue after guided bone regeneration with non-resorbable membranes vs. resorbable membranes and titanium mesh. Clin. Implant. Dent. Relat. Res. 2019, 21, 693–701. [Google Scholar] [CrossRef]
- Zhang, T.; Zhang, T.; Cai, X. The application of a newly designed L-shaped titanium mesh for GBR with simultaneous implant placement in the esthetic zone: A retrospective case series study. Clin. Implant. Dent. Relat. Res. 2019, 21, 862–872. [Google Scholar] [CrossRef] [PubMed]
- Atef, M.; Tarek, A.; Shaheen, M.; Alarawi, R.M.; Askar, N. Horizontal ridge augmentation using native collagen membrane vs. titanium mesh in atrophic maxillary ridges: Randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2020, 22, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Malik, R.; Gupta, A.; Bansal, P.; Sharma, R.; Sharma, S. Evaluation of Alveolar Ridge Height Gained by Vertical Ridge Augmentation Using Titanium Mesh and Novabone Putty in Posterior Mandible. J. Maxillofac. Oral Surg. 2020, 19, 32–39. [Google Scholar] [CrossRef]
- Cucchi, A.; Bianchi, A.; Calamai, P.; Rinaldi, L.; Mangano, F.; Vignudelli, E.; Corinaldesi, G. Clinical and volumetric outcomes after vertical ridge augmentation using computer-aided-design/computer-aided manufacturing (CAD/CAM) customized titanium meshes: A pilot study. BMC Oral Health 2020, 20, 219. [Google Scholar] [CrossRef] [PubMed]
- Celletti, R.; Davarpanah, M.; Etienne, D.; Pecora, G.; Tecucianu, J.F.; Djukanovic, D.; Donath, K. Guided tissue regeneration around dental implants in immediate extraction sockets: Comparison of e-PTFE and a new titanium membrane. Int. J. Periodontics Restor. Dent. 1994, 14, 242–253. [Google Scholar]
- Cucchi, A.; Vignudelli, E.; Napolitano, A.; Marchetti, C.; Corinaldesi, G. Evaluation of complication rates and vertical bone gain after guided bone regeneration with non-resorbable membranes versus titanium meshes and resorbable membranes. A randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2017, 19, 821–832. [Google Scholar] [CrossRef] [PubMed]
- Sagheb, K.; Schiegnitz, E.; Moergel, M.; Walter, C.; Al-Nawas, B.; Wagner, W. Clinical outcome of alveolar ridge augmentation with individualized CAD-CAM-produced titanium mesh. Int. J. Implant. Dent. 2017, 3, 36. [Google Scholar] [CrossRef] [PubMed]
- Wessing, B.; Lettner, S.; Zechner, W. Guided Bone Regeneration with Collagen Membranes and Particulate Graft Materials: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 87–100. [Google Scholar] [CrossRef]
- Roca-Millan, E.; Jané-Salas, E.; Estrugo-Devesa, A.; López-López, J. Evaluation of Bone Gain and Complication Rates after Guided Bone Regeneration with Titanium Foils: A Systematic Review. Materials 2020, 13, 5346. [Google Scholar] [CrossRef]
- Lim, G.; Lin, G.H.; Monje, A.; Chan, H.L.; Wang, H.L. Wound Healing Complications Following Guided Bone Regeneration for Ridge Augmentation: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Stenport, V.F.; Örtorp, A.; Thor, A. Onlay and inlay bone grafts with platelet-rich plasma: Histologic evaluations from human biopsies. J. Oral Maxillofac. Surg. 2011, 69, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.; Dodge, A.; Luepke, P.; Wang, H.L.; Kapila, Y.; Lin, G.H. Effect of membrane exposure on guided bone regeneration: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Benic, G.I.; Bernasconi, M.; Jung, R.E.; Hämmerle, C.H. Clinical and radiographic intra-subject comparison of implants placed with or without guided bone regeneration: 15-year results. J. Clin. Periodontol. 2017, 44, 315–325. [Google Scholar] [CrossRef]
- Clementini, M.; Morlupi, A.; Canullo, L.; Agrestini, C.; Barlattani, A. Success rate of dental implants inserted in horizontal and vertical guided bone regenerated areas: A systematic review. Int. J. Oral Maxillofac. Surg. 2012, 41, 847–855. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).