Abstract
Early onset sepsis (EOS) is a potentially fatal condition in neonates, and its correct management is still challenging for neonatologists. Early antibiotic administration in the neonatal period may carry short- and long-term risks. Neonatal EOS calculator has been recently introduced as a new strategy to manage infants at risk of sepsis, and has shown promising results. Methods: In this single-center observational retrospective study, 1000 neonates ≥ 34 weeks’ gestation were enrolled with the aim to evaluate our standard protocol for the management of suspected EOS compared to the EOS calculator. Outcome measures included the following: (1) incidence of EOS and (2) proportion of infants in need of sepsis evaluations and antibiotics using our standard protocol versus theoretical application of EOS calculator. Results: A total of 223/1000 infants underwent blood investigations versus 35/1000 (3.5%) if EOS calculator had been applied (p < 0.0001; k = 0.18). Furthermore, 48/1000 infants received antibiotics with our protocol versus 35/1000 with EOS calculator (p = 0.12; k = 0.58). Three infants had a positive blood culture that EOS calculator would have missed. Conclusions: In our study, EOS calculator could have reduced investigations but not antibiotic therapy. EOS calculator is an effective and promising tool, but further studies are required to improve it.
1. Introduction
Neonatal sepsis is a systemic infection occurring in the first 28 days of life. Although the latest definition refers to early onset sepsis (EOS) as culture-proven sepsis within the first 72 h after birth [1], in the neonatal population a relevant proportion of sepsis is diagnosed based on clinical symptoms [2]. The incidence in high-income countries has significantly decreased over the past two decades, especially with the implementation of evidence-based intrapartum antimicrobial prophylaxis [1]. Currently, with the implementation of universal maternal antenatal screening and intrapartum antibiotic prophylaxis (IAP), the national incidence of group B streptococcus (GBS) EOS has declined from 1.8 cases per 1000 live births in 1990 to 0.23 cases per 1000 live births in 2015 [3].
Approximately 60% of term infants with EOS require intensive medical care, and mortality is around 2% to 3% [4,5,6].
Specific clinical risk factors have been described [7,8]. Moreover, the infant’s clinical condition at birth and the subsequent clinical course over the first 12 to 24 h after delivery are the strongest predictors of early-onset infections [7,9].
To date, diagnostic tests with the perfect ability to identify newborn infants likely to be infected are unavailable, and blood culture remains the gold diagnostic standard for EOS. Newborn infectious disease is manifested by clinical signs, but most are devious and difficult to distinguish from other conditions (e.g., transitional instability) [7,8,9,10,11,12,13]. Therefore, neonatal infectious disease remains a complex challenge for clinicians. In recent years, the so-called sepsis scores have been developed and validated, incorporating clinical and laboratory parameters [14]. Aiming to minimize antibiotic therapy and tailoring it to those who really need it, this new model estimates the probability of EOS using maternal risk factors associated with clinical signs in infants born at ≥34 weeks gestation [14]. This model is available as a Web-based Neonatal Early-Onset Sepsis Calculator (https://neonatalsepsiscalculator.kaiserpermanente.org, accessed on 23 April 2023) and includes recommended clinical actions at specific predicted risks. Figure 1 illustrates the three main approaches to identify neonates at risk for EOS. Although there is robust evidence that the sepsis calculator is able to reduce the use of antibiotics significantly [15], this strategy neither identifies with complete certainty all infants who will develop EOS nor completely avoids the treatment of infants who are not infected.
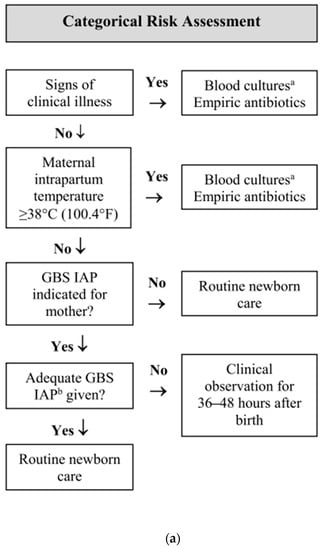
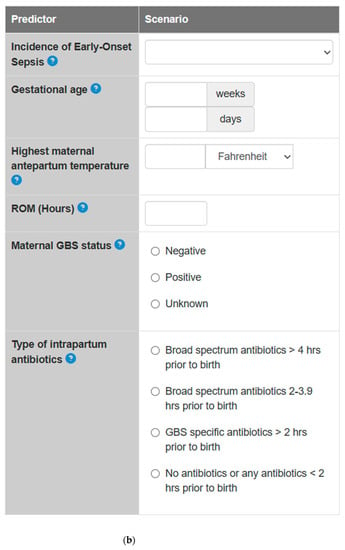
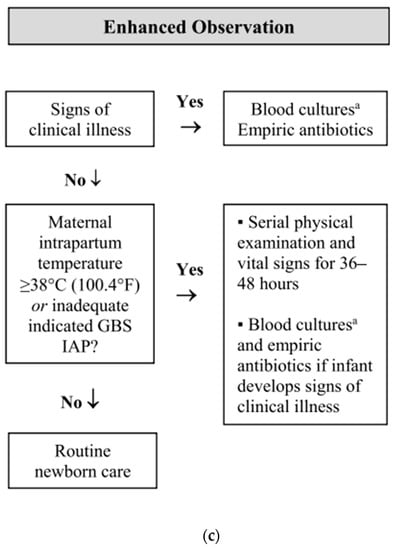
Figure 1.
Options for EOS risk assessment among infants born at ≥35 weeks’ gestation. (a) Categorical risk assessment. (b) Neonatal Early-Onset Sepsis Calculator. (c) Enhanced observation (Adapted from [16]). a consider lumbar puncture b adequate GBS IAP is defined as the administration of penicillin G, ampicillin, or cefazolin ≥ 4 hours before delivery.
Our study aimed to compare the management of newborn infants at risk of EOS according to our unit guidelines and the Neonatal Early-Onset Sepsis Calculator’s recommendations retrospectively applied.
2. Results
A total of 1000 neonates born at ≥34 weeks’ gestational age (GA) during the study period were enrolled.
Demographic characteristics and risk factors are shown in Table 1.

Table 1.
Demographic characteristics and risk factors for EOS among the study population.
According to our guidelines, 223/1000 (22.3%) newborns underwent blood investigations. On the contrary, following the EOS calculator’s recommendations, we would have performed blood tests just in 35/1000 newborns (3.5%) (p < 0.0001).
According to Cohen’s kappa coefficient, the agreement between the two protocols was 0.18 (CI 95%: 0.12–0.24). Also, following the EOS calculator’s recommendations, we would not have performed the blood tests in 193 newborns (86.5% of this population). On the contrary, the blood tests would have been indicated in five newborns according to the EOS calculator but were not performed as per our protocol (Figure 2).
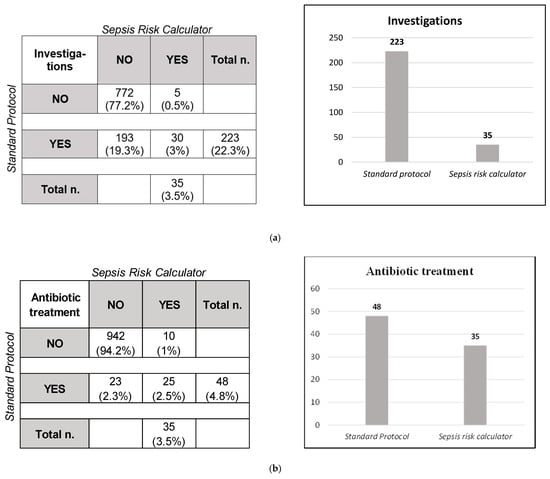
Figure 2.
Comparison between our local guidelines and EOS calculator. (a) Newborns who underwent investigations. (b) Newborns who received antibiotic treatment.
Using the standard protocol, 48/1000 infants received antibiotic therapy. Of these, two infants were equivocal, 25 presented with clinical illness (primarily respiratory distress), and 21 were asymptomatic. Moreover, 33.3% had a CRP between 15 and 30 mg/l, 29.2% had a CRP > 30 mg/L, and 18.8% had WBC > 25.000/mm3.
Based on the EOS calculator’s clinical features, 14 newborns were classified as “equivocal” and 35 as “clinical illness”. According to the EOS calculator, antibiotics were needed in those 35 infants with clinical illness.
The difference between the two protocols was not statistically significant (p = 0.12), indicating the same proportion of infants who underwent antibiotic therapy. The analysis showed that 25/48 infants were supposed to receive antibiotics according to both protocols, 23 according to our protocol and only ten according to the EOS calculator. These data were confirmed with a Cohen’s kappa coefficient of 0.58, proving moderate agreement (Figure 2).
Three newborns had a positive blood culture during the study period: one for Enterococcus faecalis and two for Streptococcus agalactiae B (GBS). All these infants never showed any clinical illness features reported in the EOS calculator and would not have needed antibiotic therapy according to the EOS calculator. The first case was a late preterm newborn who underwent blood investigations and culture without clinical signs and normal laboratory tests. The second case was a well-appearing newborn with bowel bleeding and a negative CRP; the third was an infant with max CRP of 33 mg/L without any clinical sign.
In a sub-population analysis of 18 newborns born to a mother with fever or Triple I suspected or confirmed, all newborns underwent blood investigations according to the standard protocol. In contrast, two would have undergone blood tests using the EOS calculator. Six of them (33%) received antibiotic therapy instead of two newborns with clinical illness that would have been treated according to the EOS calculator.
3. Materials and Methods
This was a single-centre observational retrospective study conducted at the Division of Neonatology at Filippo del Ponte Hospital in Varese, Italy.
The first 1000 consecutive neonates born at ≥34 weeks’ gestation between January 2021 and May 2021 were enrolled. Outborn infants and those with major congenital anomalies were excluded from the study. According to our unit guidelines, neonates born at ≥34 weeks’ GA were managed differently based on risk factors and GA, as shown in Figure 3 and Figure 4. Antibiotic therapy is started when clinical signs of sepsis are present and/or C-reactive protein (CRP) is over 15 mg/L.
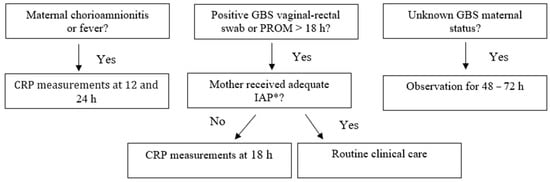
Figure 3.
Management of neonates born at ≥37 weeks’ gestation according to our local guidelines (“Standard protocol”). * adequate IAP is defined as the administration of penicillin G, ampicillin, or cefazolin ≥ 4 h before delivery.
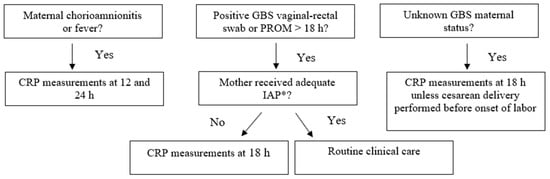
Figure 4.
Management of neonates born at ≥34 and ≤36 + 6 weeks gestation according to our local guidelines (“Standard protocol”). * adequate IAP is defined as the administration of penicillin G, ampicillin, or cefazolin ≥ 4 h before delivery.
The duration of the antibiotic therapy is five days in those cases with CRP exceeding the cut-off level and a well-appearing baby with negative blood culture, seven days if the baby has symptoms and ten days in case of positive blood culture. Discontinuing antibiotic therapy for neonates with negative blood culture at 48 h, negative CRP and no clinical signs of sepsis are promoted. The first-line antibiotic therapy is intravenous ampicillin plus amikacin.
All healthy infants, even those who underwent therapy, were managed at the Nursery (Level I). Only infants with clinical signs and symptoms were transferred to the NICU (Level III) for continued care.
Retrospectively, the same babies were attributed EOS score to compare with our unit guidelines. Each newborn was classified as “well-appearing”, “equivocal” or “clinical illness” based on the characteristics reported in the EOS calculator website (https://neonatalsepsiscalculator.kaiserpermanente.org, accessed on 23 April 2023) [17]. Each patient’s EOS risk and subsequent management recommendation were determined using an EOS incidence rate of 0.5/1000 live births, in line with the data reported by the CDC [8,17].
Data collected included the following: neonatal data, mode of delivery and maternal and neonatal risk factors (GBS maternal status, amniotic membrane rupture ≥ 18 h, maternal fever > 38 °C and suspected or confirmed Triple I). We also described the presence and type of clinical signs of EOS, relevant laboratory results, blood culture and duration of antibiotic therapy.
Possible management recommendations were as follows: (1) no culture, no antibiotics, routine vitals; (2) no culture, no antibiotics, vitals every 4 h for 24 h; (3) blood culture, vitals every 4 h for 24 h; (4) strongly consider starting empiric antibiotics, vitals per NICU; and (5) empiric antibiotics, vitals per NICU.
Data were collected in a designated database, and a comparison between the different protocols was performed using McNemar’s test (statistical significance p < 0.05), and the Cohen’s kappa coefficient was used to assess the degree of agreement among.
4. Discussion
Avoiding unnecessary antibiotics remains one of the most critical challenges for neonatologists. However, early diagnosis and correct management of EOS remain crucial.
Early antibiotic exposure is associated with increased antibiotic resistance and intestinal microbiome impoverishment [18,19], and it has also been linked with late-onset sepsis, necrotizing enterocolitis, increased mortality and long-term health outcomes. Administration of antibiotics is also related to admission to the intensive care unit, invasive procedures and higher hospital costs. Of note, these aspects decrease the establishment of breastfeeding and rooming-in [20,21].
Two main approaches currently exist using risk factors to identify infants at increased risk of EOS: a categorical risk factor assessment and a multivariate risk assessment (Figure 1). The first is an algorithm for managing GBS-specific disease developed by the CDC that has been used as a general framework for preventing all EOS [8,22,23]. Limitations of this approach include a lack of clear definitions of newborn clinical illnesses, difficulties in identifying maternal chorioamnionitis, an inconsistent consideration of intrapartum antibiotics and a lack of neonatal cut-offs to define abnormal laboratory tests.
The second approach is a multivariate risk assessment based on the Kaiser Permanente EOS calculator developed to avoid overtreatment. The EOS calculator is based on a multivariate predictive risk model, intended to estimate a newborn’s individual risk of EOS by adding the perinatal and maternal risk factors and the infant’s clinical presentation [11,15,24]. This model overcomes some disadvantages of the CDC algorithm, such as the dichotomization of the continuous variables and the inclusion of maternal chorioamnionitis as an impactful risk factor for starting antibiotic therapy [25]. Several studies reported its efficacy in reducing antibiotic overtreatment, laboratory testing, painful procedures and NICU admissions [11,20,25].
Potential concern is the need for continuous monitoring to assess infants as clinically ill, equivocal or well appearing over the first 12–24 h after birth. Authors have also reported patients with culture-proven EOS who would not have received antibiotics based on the decision making of the EOS calculator [26,27,28].
Our local guidelines are based on the CDC algorithm with some amendments. First, we perform laboratory tests for all newborns born to mothers with inadequate IAP; second, we treat only newborns born to febrile mothers with clinical signs of sepsis or altered biomarkers such as CRP > 15 mg/L.
In our study, the laboratory tests could have been avoided in 86.5% of newborns according to the EOS calculator when compared to our local guidelines, resulting in a statistically significant difference in reducing unnecessary blood investigations with a relevant benefit in clinical practice. Potential advantages could have been less workload, more care for the newborns and less risk of incorrect or ambiguous evaluation. Our data are similar to those reported in a recent meta-analysis by Deshmukh et al. describing a reduction from 15.5% to 2.5% of laboratory tests using the EOS calculator [29]. In 2018, Dhudasia and Puopolo et al. confirmed a laboratory test reduction of 82% after introducing the EOS calculator [30]. Contrary to our unit’s protocol, only five newborns (0.6%) should have undergone blood investigations according to the EOS calculator. These babies needed transient respiratory support (high flow nasal-cannula or oxygen therapy) for mild respiratory distress that resolved in a few hours.
Another controversial aspect is the choice of biomarkers. According to our unit’s guidelines, the deciding factor to start antibiotics is CRP > 15 mg/L, as we know that CRP and PCT have a good negative predictive value but are neither sensitive nor specific to guide EOS care decisions in the absence of culture-confirmed infections. However, to date, serial evaluation of inflammatory markers is not recommended in well-appearing term newborns at risk of EOS [1,31].
In our study, the number of patients needing antibiotic therapy was substantially the same between the two approaches. However, the patients were not the same. According to the EOS calculator, just half of the newborns were eligible for antibiotic treatment, and ten more infants should have started therapy based on respiratory distress. Conversely, in our unit, infants with isolated respiratory distress with negative biomarkers undergo a close clinical observation and are not administered antibiotics immediately.
According to our experience, the EOS calculator seems at risk of overestimating respiratory symptoms that can overlap with other neonatal clinical manifestations, such as the transient tachypnea of newborns. In accordance with Laccetta and colleagues, careful consideration of the risk factors for EOS, anamnestic data and alternative diagnoses should further reduce unnecessary antibiotics administration. For equivocal patients (presenting with tachycardia, tachypnea, temperature instability or respiratory distress), other clinical indicators of EOS, such as skin discolouration and circulatory signs, altered behaviour or responsiveness, and feeding difficulties should be considered [32].
In our study, we found that the EOS calculator failed to detect three confirmed neonatal bloodstream infections. However, the correct interpretation of these cases is questionable, and all of them had no clinical signs suggesting a transient bacteremia or a benign course due to early therapy.
Currently, in high-income countries, the incidence of EOS in term and late preterm babies has reduced to around 0.5–1/1000 and does not differ from our hospital data in the last years. Thus, according to the EOS calculator, in a small population of 18 infants born to mothers with fever, blood tests and antibiotics would have been needed in two infants. However, according to our guidelines, they all underwent blood tests and six newborns were started on antibiotics. Although the local EOS incidence of 0.5/1000 live births was set up in the calculator, it is reasonable that a higher incidence was assumed in this sub-population, and the new definition of “Triple I” was incorporated [33].
An interesting approach is the risk assessment of newborn clinical conditions suggested by the GBS Prevention Working Group of Emilia-Romagna (Italy) using serial physical examination (SPE) performed at standardized time points for all newborns. This approach, however, requires experience and specific staff training [34,35].
A promising new approach has been recently published. It includes the combination of EOS calculator and SPE for all newborns with the possibility of evaluating the administration of antibiotic therapy in infants showing only mild respiratory symptoms with other systemic signs. Combined strategy seems to significantly reduce laboratory testing and antibiotic prescriptions [36].
Our study has some limitations. First, it was a retrospective study with a small sample size and the EOS calculator was applied retrospectively. Also, the overall incidence of presumed culture-proven EOS in the studied population (3/1000) is likely to be overestimated because of the limited study period.
5. Conclusions
Although the use of EOS has dramatically decreased the number of babies undergoing multiple blood examinations after birth, there is still room for further improvements in evaluating babies at risk of EOS to avoid missing asymptomatic bloodstream infections and to reduce antibiotic administration.
The missing cases of three bloodstream infections deserve careful consideration. This might lead to the implementation of clinical indicators to be considered in the calculator, such as altered behaviour or responsiveness, feeding difficulties, altered skin colour, body temperature, acidosis and glycemic instability.
Further randomized studies evaluating the safety and implementation of EOS calculator are urgently warranted.
Author Contributions
Conceptualization, S.P. and M.C.B.; method ology, S.P. and M.C.B.; validation, M.A. and A.B.; investigation, M.C.B.; data curation, S.P. and M.C.B.; writing—review and editing, all co-authors; supervision, I.B., L.F. and L.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This research is based on a retrospective clinical data collection of a populations routinely treated with the local protocol for prevention of EOS approved by the Hospital Committee (ISPG.5-AOP.1.3.1-PCI.0).
Informed Consent Statement
All parents of infants involved have signed consent for routine care data collection at birth.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Puopolo, K.; Benitz, W.E.; Zaoutis, T.E.; Cummings, J.; Juul, S.; Hand, I.; Eichenwald, E.; Poindexter, B.; Stewart, D.L.; Aucott, S.W.; et al. Management of Neonates Born at ≥35 0/7 Weeks’ Gestation With Suspected or Proven Early-Onset Bacterial Sepsis. Pediatrics 2018, 142, e20182894. [Google Scholar] [CrossRef] [PubMed]
- Hornik, C.P.; Fort, P.; Clark, R.H.; Watt, K.; Benjamin, D.K., Jr.; Smith, P.B.; Manzoni, P.; Jacqz-Aigrain, E.; Kaguelidou, F.; Cohen-Wolkowiez, M. Early and late onset sepsis in very-low-birth-weight infants from a large group of neonatal intensive care units. Early Hum. Dev. 2012, 88 (Suppl. S2), S69–S74. [Google Scholar] [CrossRef] [PubMed]
- Nanduri, S.A.; Petit, S.; Smelser, C.; Apostol, M.; Alden, N.B.; Harrison, L.H.; Lynfield, R.; Vagnone, P.S.; Burzlaff, K.; Spina, N.L.; et al. Epidemiology of invasive early-onset and late-onset group B streptococcal disease in the United States, 2006 to 2015: Multistate laboratory and population-based surveillance. JAMA Pediatr. 2019, 173, 224–233. [Google Scholar] [CrossRef]
- Schrag, S.J.; Farley, M.M.; Petit, S.; Reingold, A.; Weston, E.J.; Pondo, T.; Hudson Jain, J.; Lynfield, R. Epidemiology of invasive early onset neonatal sepsis, 2005 to 2014. Pediatrics 2016, 138, e20162013. [Google Scholar] [CrossRef]
- Weston, E.J.; Pondo, T.; Lewis, M.M.; Martell-Cleary, P.M.; Morin, C.; Jewell, B.; Daily, P.; Apostol, M.; Petit, S.; Farley, M.; et al. The burden of invasive early-onset neonatal sepsis in the United States, 2005–2008. Pediatr. Infect. Dis. J. 2011, 30, 937–941. [Google Scholar] [CrossRef]
- Stoll, B.J.; Hansen, N.I.; Sánchez, P.J.; Faix, R.G.; Poindexter, B.B.; Van Meurs, K.P.; Bizzarro, M.J.; Goldberg, R.N.; Frantz, I.D., III; Hale, E.C.; et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Early onset neonatal sepsis: The burden of group B Streptococcal and E. coli disease continues. Pediatrics 2011, 127, 817–826. [Google Scholar] [CrossRef]
- Escobar, G.J.; Li, D.K.; Armstrong, M.A.; Gardner, M.N.; Folck, B.F.; Verdi, J.E.; Xiong, B.; Bergen, R.; Neonatal Infection Study Group. Neonatal sepsis workups in infants ≥2000 g at birth: A population based study. Pediatrics 2000, 106 Pt 1, 256–263. [Google Scholar] [CrossRef]
- Verani, J.R.; McGee, L.; Schrag, S.J. Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC). Prevention of perinatal group B streptococcal disease—Revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010, 59, 1–36. [Google Scholar]
- Escobar, G.J.; Puopolo, K.M.; Wi, S.; Turk, B.J.; Kuzniewicz, M.W.; Walsh, E.M.; Newman, T.B.; Zupancic, J.; Lieberman, E.; Draper, D. Stratification of risk of early-onset sepsis in newborns >/=34 weeks’ gestation. Pediatrics 2014, 133, 30–36. [Google Scholar] [CrossRef]
- Newman, T.B.; Puopolo, K.M.; Wi, S.; Draper, D.; Escobar, G.J. Interpreting complete blood counts soon after birth in newborns at risk for sepsis. Pediatrics 2010, 126, 903–909. [Google Scholar] [CrossRef]
- Benitz, W.E. Adjunct laboratory tests in the diagnosis of early-onset neonatal sepsis. Clin Perinatol. 2010, 37, 421–438. [Google Scholar] [CrossRef] [PubMed]
- Shane, A.L.; Sanchez, P.J.; Stoll, B. Neonatal Sepsis. Lancet 2017, 390, 1770–1780. [Google Scholar] [CrossRef] [PubMed]
- Puopolo, K.M.; Draper, D.; Wi, S.; Newman, T.B.; Zupancic, J.; Lieberman, E.; Smith, M.; Escobar, G.J. Estimating the probability of neonatal early-onset infection on the basis of maternal risk factors. Pediatrics 2011, 128, e1155–e1163. [Google Scholar] [CrossRef] [PubMed]
- Kaiser Permanente Division of Research. Probability of Neonatal Early-Onset Infection Based on Maternal Risk Factors and the Infant’s Clinical Presentation. 2015. Available online: http://newbornsepsiscalculator.org/calculator (accessed on 23 April 2023).
- Kuzniewicz, M.W.; Puopolo, K.M.; Fischer, A.; Walsh, E.M.; Li, S.; Newman, T.B.; Kipnis, P.; Escobar, G.J. A quantitative, risk-based approach to the management of neonatal early-onset sepsis. JAMA Pediatr. 2017, 171, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Puopolo, K.M.; Lynfield, R.; Cummings, J.J.; Committee on Fetus and newborn; Committee on Infectious Diseases. Management of Infants at Risk of Group B Streptococcal Disease. Pediatrics 2019, 144, e20191881. [Google Scholar] [CrossRef]
- Joshi, N.S.; Huynh, K.; Lu, T.; Lee, H.C.; Frymoyer, A. Epidemiology and trends in neonatal early onset sepsis in California, 2010–2017. J. Perinatol. 2022, 42, 940–946. [Google Scholar] [CrossRef]
- Lista, G.; Meneghin, F.; Bresesti, I.; Castoldi, F. Functional nutrients in infants born by vaginal delivery or Cesarean section. Pediatr. Med. Chir. 2017, 39, 184. [Google Scholar] [CrossRef][Green Version]
- Morreale, C.; Giaroni, C.; Baj, A.; Folgori, L.; Barcellini, L.; Dhami, A.; Agosti, M.; Bresesti, I. Effects of Perinatal Antibiotic Exposure and Neonatal Gut Microbiota. Antibiotics 2023, 12, 258. [Google Scholar] [CrossRef]
- Benaim, E.H.; Upadhyay, K.; Talati, A.J. Comparison of institutional guidelines with established early onset sepsis risk calculator in reducing antibiotic use in an inner-city NICU in US. J. Glob. Antimicrob. Resist. 2020, 21, 124–129. [Google Scholar] [CrossRef]
- Cotton, M.C. Adverse consequences of neonatal antibiotic exposure. Curr. Opin. Pediatr. 2016, 28, 141–149. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Prevention of perinatal group B streptococcal disease: A public health perspective. MMWR Recomm. Rep. 1996, 45, 1–24. [Google Scholar]
- Schrag, S.; Gorwitz, R.; Fultz-Butts, K.; Schuchat, A. Prevention of perinatal group B streptococcal disease. revised guidelines from CDC. MMWR Recomm. Rep. 2002, 51, 1–22. [Google Scholar]
- Kuzniewicz, M.W.; Walsh, E.M.; Li, S.; Fischer, A.; Escobar, G.J. Development and implementation of an early-onset sepsis calculator to guide antibiotic management in late preterm and term neonates. Jt. Comm. J. Qual. Patient. Saf. 2016, 42, 232–239. [Google Scholar] [CrossRef]
- Van der Weijden, B.M.; Achten, N.B.; Bekhof, J.; Evers, E.E.; van Dongen, O.; Rijpert, M.; Kamps, A.W.A.; Ten Tusscher, G.W.; van Houten, M.A.; Plötz, F.B. Neonatal early onset sepsis calculator recommended significantly less empiric antibiotic treatment than national guidelines. Acta Paediatr. 2020, 109, 2549–2551. [Google Scholar] [CrossRef]
- Rajbhandari, S.; La Gamma, E.F. Early-onset sepsis calculator-risk of delaying treatment. JAMA Pediatr. 2017, 171, 1015. [Google Scholar] [CrossRef] [PubMed]
- Sloane, A.J.; Coleman, C.; Carola, D.L.; Lafferty, M.A.; Edwards, C.; Greenspan, J.; Aghai, Z.H. Use of a modified early-onset sepsis risk calculator for neonates exposed to chorioamnionitis. J. Pediatr. 2019, 213, 52–57. [Google Scholar] [CrossRef]
- Pettinger, K.J.; Mayers, K.; McKechnie, L.; Phillips, B. Sensitivity of the Kaiser Permanente early-onset sepsis calculator: A systematic review and meta-analysis. E Clin. Med. 2019, 19, 100227. [Google Scholar]
- Deshmukh, M.; Mehta, S.; Patole, S. Sepsis calculator for neonatal early onset sepsis–a systematic review and meta-analysis. J. Matern.-Fetal Neonatal Med. 2021, 34, 1832–1840. [Google Scholar] [CrossRef]
- Dhudasia, M.B.; Mukhopadhyay, S.; Puopolo, K.M. Implementation of the Sepsis Risk Calculator at an Academic Birth Hospital. Hosp. Pediatr. 2018, 8, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, V. Effective biomarkers for diagnosis of neonatal sepsis. J. Pediatr. Infect. Dis. Soc. 2014, 3, 234–245. [Google Scholar] [CrossRef]
- Laccetta, G.; Ciantelli, M.; Tuoni, C.; Sigali, E.; Miccoli, M.; Cuttano, A. Early-onset sepsis risk calculator: A review of its effectiveness and comparative study with our evidence-based local guidelines. Ital. J. Pediatr. 2021, 47, 73. [Google Scholar] [CrossRef] [PubMed]
- Higgins, R.D.; Saade, G.; Polin, R.A.; Grobman, W.A.; Buhimschi, I.A.; Watterberg, K.; Silver, R.M.; Raju, T.N. Chorioamnionitis Workshop Participants. Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: Summary of a workshop. Obs. Gynecol. 2016, 127, 426–436. [Google Scholar] [CrossRef] [PubMed]
- Berardi, A.; Fornaciari, S.; Rossi, C.; Patianna, V.; Reggiani, M.L.B.; Ferrari, F.; Neri, I.; Ferrari, F. Safety of physical examination alone for managing well-appearing neonates ≥35 weeks’ gestation at risk for early-onset sepsis. J. Matern. Neonatal Med. 2014, 28, 1123–1127. [Google Scholar] [CrossRef]
- Berardi, A.; Bedetti, L.; Spada, C.; Lucaccioni, L.; Frymoyer, A. Serial clinical observation for management of newborns at risk of early-onset sepsis. Curr. Opin. Pediatr. 2020, 32, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Cavigioli, F.; Viaroli, F.; Daniele, I.; Paroli, M.; Guglielmetti, L.; Esposito, E.; Cerritelli, F.; Zuccotti, G.; Lista, G. Neonatal Early Onset Sepsis (EOS) Calculator plus Universal Serial Physical Examination (SPE): A Prospective Two-Step Implementation of a Neonatal EOS Prevention Protocol for Reduction of Sepsis Workup and Antibiotic Treatment. Antibiotics 2022, 11, 1089. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).