Abstract
Recognition of risk factors for hospital-acquired infections (HAI) in patients with COVID-19 is warranted. We aimed to describe factors associated with the development of HAI in patients with severe COVID-19. We conducted a retrospective cohort study including all adult patients admitted with severe COVID-19 between March 2020 and November 2020. The primary outcome was HAI development. Bivariate and multiple logistic regression models were constructed. Among 1540 patients, HAI occurred in 221 (14%). A total of 299 episodes of HAI were registered. The most common HAI were hospital-acquired/ventilation-associated pneumonia (173 episodes) and primary bloodstream infection (66 episodes). Death occurred in 387 (35%) patients and was more frequent in patients with HAI (38% vs. 23%, p < 0.01). Early mechanical ventilation (aOR 18.78, 95% CI 12.56–28.07), chronic kidney disease (aOR 3.41, 95% CI 1.4–8.27), use of corticosteroids (aOR 2.95, 95% CI 1.92–4.53) and tocilizumab (aOR 2.68, 95% CI 1.38–5.22), age ≥ 60 years (aOR 1.91, 95% CI 1.27–2.88), male sex (aOR 1.52, 95% CI 1.03–2.24), and obesity (aOR 1.49, 95% CI 1.03–2.15) were associated with HAI. In patients with severe COVID-19, mechanical ventilation within the first 24 h upon admission, chronic kidney disease, use of corticosteroids, use of tocilizumab, age ≥ 60 years, male sex, and obesity were associated with a higher risk of HAI.
1. Introduction
Increased susceptibility to secondary bacterial and fungal infections has been described after respiratory viral infections [1]. Severe COVID-19 is associated with immune dysfunction characterized by persistent cytokine release, inflammatory activation, and immunosuppression [2]. Endothelial dysfunction, vascular leakage, impaired mucus clearance, biofilm formation, and microbiome changes, along with COVID-19-associated immune dysfunction, are implicated in the increased susceptibility to secondary infections [1]. The prevalence of secondary infections among hospitalized patients with COVID-19 ranges from 4% to 25%, but it may reach 50% in non-survivors [3,4,5,6]. Bloodstream infections (BSI), hospital-acquired/ventilator-associated pneumonia (HAP/VAP) due to Gram-negative bacteria, and COVID-19-associated aspergillosis (CAPA) are the leading causes of hospital-acquired infections (HAI), occurring in 25%, 36%, and 10–35% of cases, respectively [4,7,8]. Antibiotic overuse in hospitalized patients with COVID-19 may have affected the ecological and epidemiological trends of HAI [9]. Additionally, increasing frequencies of multidrug-resistant (MDR) isolates have been reported [10].
Although immunomodulatory treatments for COVID-19, such as dexamethasone and tocilizumab, have been associated with lower mortality [11,12], they could also lead to an increased risk of secondary infections. The use of methylprednisolone, hepatic failure, and diabetes have been associated with increased susceptibility to secondary infections [4]. Secondary bacterial infections lead to decreased survival rates and are a leading cause of death among severe COVID-19 patients [13]. Infections due to MDR pathogens have been associated with a mortality of 60% [14]. Recognition of risk factors for HAI in patients with COVID-19 is warranted. In this cohort study, we aimed to describe the risk factors associated with the development of HAI in hospitalized patients with severe and critical COVID-19.
2. Results
During the study period, 2017 patients were hospitalized with COVID-19, and 477 patients were excluded (Figure 1). We included 1540 patients who had a median age of 55 (IQR 45-65) years; 941/1540 (61.1%) were men. Obesity, hypertension, and type 2 diabetes mellitus (T2DM) were present in 681/1540 (44.2%), 528/1540 (34.3%), and 440/1540 (28.6%) subjects, respectively. The median time from symptom onset to admission was seven days (IQR 5-10). Empirical antibiotic therapy upon admission was used in 914/1540 (59.4%). Treatment with corticosteroids was prescribed in 688/1540 (44.6%) and tocilizumab in 97/1540 (6.3%). Among patients who developed HAI, male sex, obesity, lower oxygen saturation, lymphopenia, and higher concentrations of C-reactive protein (CRP), lactate dehydrogenase (LDH), and ferritin at hospital admission were present. Also, IMV and treatment with corticosteroids during the first 24 h of hospitalization were more frequent among patients with HAI. Enrolment in a COVID-19 clinical trial was more frequent in those without HAI (Table 1).
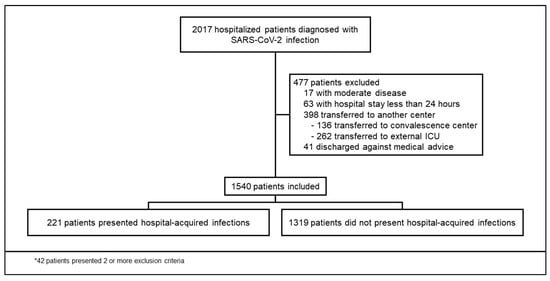
Figure 1.
Enrolment and inclusion.

Table 1.
Baseline demographic and clinical characteristics.
A total of 299 episodes of HAI occurred among 221 patients: 250/299 (83.6%) bacterial and 49/299 (16.3%) invasive fungal infections were registered. The most common HAI was HAP/VAP (173/299 episodes, 57.8%). The most frequently isolated organisms in respiratory samples were Enterobacter cloacae complex (49/173, 28.3%), Pseudomonas aeruginosa (35/173, 20.2%), and Staphylococcus aureus (32/173, 18.5%). A total of 66/299 (22.1%) episodes of primary bloodstream infections (BSI) were diagnosed; coagulase-negative Staphylococcus spp. (26/66, 39.4%) and Enterococcus spp. (12/66, 18.2%) were most frequently recovered. Additional bacterial infections included bone, joint, skin, and soft tissue infections (4/299 episodes, 1.3%), intraabdominal infections (3/299 episodes, 1.0%), urinary tract infections (2/299 episodes, 0.7%), and Clostridioides difficile infections (1/299 episode, 0.3%). A total of 26/299 episodes (8.7%) of probable/proven CAPA were documented, and Aspergillus fumigatus was the most common isolate (11/26, 42.3%). Additionally, 17/299 (5.7%) episodes of candidemia and 3/299 (1.0%) episodes of mucormycosis were diagnosed; Candida parapsilosis was the most common species isolated (12/17, 70.6%). A total of 19/221 (8.6%) and 9/221 (4.1%) patients were diagnosed with HAP/VAP and CAPA, HAP/VAP, and candidemia during their follow-up. Tables S1 and S2 in the supplementary material summarize bacterial and fungal pathogens recovered.
No carbapenem resistance was found among Enterobacter cloacae complex species (62 isolates), regardless of the site of infection. The second most frequent Gram-negative rod was Escherichia coli (46 isolates), and resistance to third-generation cephalosporins and carbapenems was observed in 23/46 (59.5%) and 4/46 (8.7%) isolates, respectively. Forty isolates of P. aeruginosa were recovered; piperacillin-tazobactam and carbapenem resistance was reported in 9/40 (22.5%) and 5/40 (12.5%) isolates, respectively. Among the Gram-positive cocci, the most common isolate was S. aureus (35 isolates); methicillin resistance was reported in 5/35 (14.3%) isolates. Among 23 Candida spp. isolates, 6/23 (26.1%) were azole-resistant (1 C. glabrata and 5 C. parapsilosis). Antimicrobial susceptibility patterns are summarized in Table S3.
A total of 387/1540 (25.1%) patients died. Death occurred in 84/221 (38.8%) patients with HAIs and in 303/1319 (23.0%) without HAIs (p < 0.01). The presence of HAI was associated with a greater risk of death (RR 1.65, 95% CI 1.36–2.01). Treatment with corticosteroids was associated with a lower probability of death (RR 0.57, 95% CI 0.47–0.69). When stratified by HAI, the protective factor of corticosteroids for death was modified (Figure 2). HAP/HAP due to Gram-negative bacilli was associated with in-hospital death (RR 1.54, 95% CI 1.22–1.94). The latter was not observed when Gram-positive cocci caused HAP/VAP (RR 1.38, 95% CI 0.86–2.19). Both Gram-positive cocci and Gram-negative bacilli-associated BSI were not associated with in-hospital death (RR 1.40, 95% CI 0.93–2.10, and 1.33, 95% CI 0.72–2.45, respectively). CAPA was associated with in-hospital death (RR 1.96, 95%CI, 1.33–2.88). Candidemia was not associated with in-hospital death (RR 0.96, 95% CI 0.40–2.21).
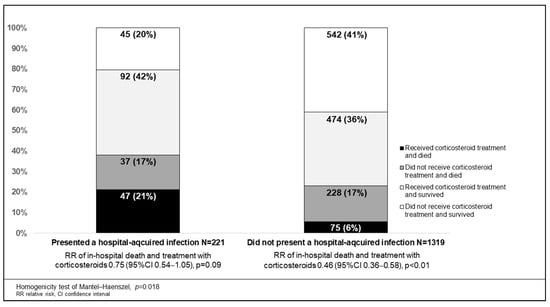
Figure 2.
Association of in-hospital death and treatment with corticosteroids according to presence or absence of hospital-acquired infections.
Median LOS in survivors was seven days (IQR 5−14). Surviving patients that developed a HAI had longer LOS (median of 27 days [IQR 20−42] versus 7 days [5,6,7,8,9,10,11], p < 0.01). IMV during follow-up occurred in 131 patients, of which 58/131 (44.2%) developed HAI, and 73/131 (55.7%) did not (p = 0.187).
On bivariate analysis, a higher risk of HAI was associated with male sex, obesity, lower lymphocyte count, CRP > 10 mg/dL, ferritin > 500 mg/dL, LDH > 246 IU/L, D-dimer > 500 mg/mL, use of IMV on the first 24 h upon admission, and treatment with corticosteroids and tocilizumab. Enrolment in a COVID-19 clinical trial was associated with a lower risk of HAI (Table S4). On multivariate analysis, use of IMV on the first 24 h upon admission (aOR 18.78, 95% CI 12.56–28.07), chronic kidney disease (aOR 3.41, 95% CI 1.4–8.27), treatment with corticosteroids (aOR 2.95, 95% CI 1.92–4.53) and treatment with tocilizumab (aOR 2.69, 95% CI 1.38–5.22), age greater than 60 years (aOR 1.91, 95% CI 1.27–2.88), male sex (aOR 1.52, 95% CI 1.03–2.24), and obesity (aOR 1.49, 95% CI 1.03–2.15) were independently associated with HAI (Table 2). Because of the strong association between the use of IMV in the first 24 h upon admission and the development of HAI, non-prespecified multivariate analysis using the previously selected variables was done to study the association between early IMV and HAP/VAP, BSI, candidemia, and CAPA. IMV in the first 24 h upon admission was independently associated with the development of HAP/VAP (aOR 15.86 95% CI 10.13–24.83), BSI (aOR 15.80 95% CI 7.94–31.42), CAPA (aOR 8.93 95% CI 3.56–22.40), and candidemia (aOR 7.27 95% CI 2.39–22.14) in separate models.

Table 2.
Risk factors associated with the development of hospital-acquired infections.
3. Discussion
In our study, IMV in the first 24 h, chronic kidney disease, treatment with corticosteroids, treatment with tocilizumab, older age, male sex, and obesity were independently associated with a higher risk of developing HAI in severe and critical COVID-19 hospitalized patients. Male sex has been associated with the development of secondary infections among COVID-19 patients in addition to a worse overall prognosis [15]. Up to 71% of patients that develop secondary infections are males [14], which may be related to sex-driven differences in immunological responses [16]. Similarly, age has been consistently associated with HAI and worse prognosis in COVID-19 [17]. The latter could be due to immunosenescence and increasing comorbidity burden, which have been described as risk factors for secondary infections in severe and critical COVID-19 [18]. Liver injury and T2DM were related to the development of BSI in an Italian cohort [4]. Similarly, T2DM, hypertension, and obesity were associated with an increased risk of secondary infection in COVID-19 patients [19]. Chronic kidney disease was associated with persistent immune dysfunction and a greater risk of HAI [20]. We did not observe an association between T2DM or hypertension and the development of HAI, which could be partly explained because of the high frequency of these comorbidities in our region [21] and, consequently, in our sample. Because of barrier disruption and ICU-related disease severity, IMV has been consistently described as one of the main risk factors for HAI [22]. In our study, early IMV may reflect increased severity or late presentation and, consequently, increased immune dysfunction on admission. Additionally, a longer time of airway exposure to biotrauma could have increased the risk of developing HAI. Treatment with corticosteroids and tocilizumab was associated with the development of HAI. The use of methylprednisolone has been previously associated with the development of secondary infections in COVID-19 patients [4]. Because of their immunomodulatory properties, corticosteroids and tocilizumab have been associated with the development of HAI [19]. Our results suggest that the beneficial effect of corticosteroid treatment on mortality could be mitigated by the presence of HAI. Secondary infections could disrupt the effects of corticosteroids and the immune response against SARS-CoV-2 [23].
The observed frequency of HAI is in accordance with previous reports [5,6,13,19]. An important difference must be established between co-infections, defined as those that occur in the first 72 h after hospital admission, and secondary infections, defined as those that occur after the first 48 h after hospital admission. Our focus was on secondary infections [3]. Higher mortality and LOS are expected in COVID-19 patients who develop HAI [14]. Our cohort is characterized by subjects with a high number of comorbidities, which are major problems in our region [21]. We also observed high proportions of empiric antibiotic therapy use, which has been previously described [24] and has not been associated with a lower risk of HAI [10]. Previous antibiotic exposure was not correlated with the antimicrobial susceptibility patterns of the infecting microorganisms.
HAP/VAP and primary BSI were the most frequently diagnosed HAIs. Enterobacter complex species, E. coli, P. aeruginosa, S. aureus, coagulase negative Staphylococcus species, and Klebsiella pneumoniae were the most commonly reported microorganisms, as previously described [10]. The main invasive fungal infection in our cohort was CAPA. The results of antimicrobial susceptibility testing are in accordance with previous COVID-19-related reports, where resistance to third-generation cephalosporins is a common problem and carbapenem resistance is an emerging threat [25]. Similarly, azole-resistant Candida infections are an emerging problem in hospital settings [26]. Antimicrobial overprescribing during the pandemic has increased dramatically. Inappropriate use of antimicrobials will likely play a role in the spread of antimicrobial resistance in the near future, yielding broad-spectrum antibiotics ineffective [27].
Our study presents limitations inherent to its retrospective nature that must be considered. We describe risk factors that predispose to a wide range of both bacterial and fungal infections, so the impact of individual risk factors may not reflect their association with a specific type of infection or individual microbial isolate. Even though our results suggest that early IMV is associated with HAI development, we cannot rule out that a longer time of exposure to IMV may have played a role in the development of infections. Of note, early IMV was independently associated with HAP/VAP, BSI, CAPA, and candidemia in exploratory analysis. Because our study was conducted before widespread vaccination was implemented in our region, the interpretation of our results must consider that a post-vaccination lower frequency of severe forms of COVID-19 could impact the development of HAIs. The importance of accurate imaging has been previously described [28], and although multilobe involvement was registered in most patients, we could not register additional radiological data. Additionally, the unicentric nature of the study must be taken into consideration. Finally, we cannot account for the learning curve during the study period, during which increasing knowledge and specific interventions (such as corticosteroid treatment) may have impacted our results. The large sample size, prespecified analysis plan, and systematic data collection are the main strengths of our study.
In this study, we describe risk factors associated with the development of various types of HAIs in patients hospitalized with severe forms of COVID-19. Although further research is warranted, recognizing such risk factors could allow active surveillance and continuous reinforcement of bundle prevention packages according to specific patient characteristics.
4. Materials and Methods
We conducted a retrospective cohort study in a COVID-19 reference center in Mexico City. Our center specializes in caring for adults with complex medical and/or surgical problems. On 16 March 2020, our center was converted into a dedicated COVID-19 facility. We registered demographic, clinical, and laboratory data of all consecutive adult patients admitted with a PCR-confirmed case of severe or critical COVID-19 between 18 March 2020 and 17 November 2020. We excluded patients who were transferred to other facilities before discharge, had a length of stay <24 h, or were discharged against medical advice. During the study period, routine SARS-CoV-2 real-time polymerase chain reaction (RT-PCR) testing on nasopharyngeal swab samples was performed upon admittance. Nucleic acid extraction was performed using the NucliSens easyMAG system (bioMérieux, Boxtel, The Netherlands), and RT-PCR was processed on an Applied Biosystems 7500 thermocycler (version 1.4, Foster City, CA, USA) according to specifications described elsewhere [29]. Data were registered using the electronic medical record. A severe case was considered when SpO2 was <93%, PaO2/FiO2 ratio < 300, respiratory rate ≥ 30 breaths per minute, or ≥50% lung involvement was observed in chest CT, whereas a critical case was considered when either shock, urgent need for invasive mechanical ventilation (IMV), or multi-organ failure were observed [30]. Immunosuppression was considered when the prescription of immunosuppressive medications or comorbidities (e.g., solid malignant tumors, hematologic malignancy, solid organ transplant, human immunodeficiency virus infection, and connective tissue disorders) were present. Each patient was followed up from admission to death or discharge. The primary outcome was the development of a culture-proven HAI. A HAI was considered if diagnosed 48 h after admission and if accepted criteria were met [31,32,33,34]. All cases were reviewed by an infectious disease specialist. During the study period, cultures and serum markers (e.g., procalcitonin and galactomannan) were only obtained if ordered by an infectious disease specialist. All samples were cultured for bacterial and fungal pathogens. Secondary outcomes were in-hospital death, length of stay (LOS), and IMV during follow-up. All patients received the standard of care according to available evidence at admission. In our center, the use of corticosteroids as standard treatment was implemented on 17 June 2020. During the study period, neither tocilizumab nor baricitinib was routinely administered. Written informed consent was waived due to the retrospective nature of the study. The study was approved by the Institutional Review Board (Ref. number 3333).
Considering a primary outcome probability of 50% [4], a mean absolute percentage error of 5%, and the identification of up to 10 potential predictors, we calculated a required sample size of at least 588 patients [35]. Mean, standard deviation (SD), median and interquartile range (IQR) were used to describe data according to the Shapiro–Wilk normality test. Comparisons between patients who presented the primary outcome were made using Chi-squared, Fisher’s exact test, independent samples t-test, and two-sample rank sum tests. To determine factors associated with the development of HAIs, bivariate analysis to calculate relative risk (RR) and 95% confidence interval (CI) were performed. A multiple logistic regression model that included variables of biological importance was constructed to identify factors independently associated with the development of HAI. Variables with interactions (e.g., liver cirrhosis, human immunodeficiency virus infection, and Charlson comorbidity index) assessed by the Mantel–Haenszel Chi test were not included. Laboratory values were not included in the multivariable analysis because of incomplete data and non-systematic determinations. For the multivariable analysis, adjusted odds ratios (aOR) were calculated. An exploratory analysis was done to describe the association between in-hospital death and the development of HAI. HAI-stratified associations between in-hospital death and treatment with corticosteroids were also studied in exploratory analysis. Missing data were not replaced. Two-sided p values < 0.05 were considered statistically significant. STATA version 15.1 (College Station, TX, USA) was used.
5. Conclusions
In our study, IMV within the first 24 h upon admission, chronic kidney disease, treatment with corticosteroids, treatment with tocilizumab, age greater than 60 years, male sex, and obesity were independently associated with a higher risk of presenting HAI in hospitalized patients with severe forms of COVID-19.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics12071108/s1, Table S1: Bacterial isolates, Table S2: Fungal isolates, Table S3: Antimicrobial susceptibility, Table S4: Risk factors associated with the development of hospital-acquired infections according to bivariate analysis.
Author Contributions
Conceptualization, F.S.-H., B.A.M.-G., A.P.-d.-L., M.F.G.-L. and J.S.-O.; methodology, F.S.-H., B.A.M.-G., C.M.R.-M., K.M.T.-T. and S.R.-L.; software B.A.M.-G.; validation, B.A.M.-G., N.O.-C., N.I.L.-G., G.Y.V.-Z., A.R.-C., J.S.-C., L.F.X.-S. and S.M.-R.; formal analysis, F.S.-H. and B.A.M.-G.; investigation, F.S.-H., B.A.M.-G., C.M.R.-M., K.M.T.-T., S.R.-L., N.O.-C., N.I.L.-G., G.Y.V.-Z., A.R.-C., J.S.-C., L.F.X.-S., S.M.-R., E.O.-H., A.G.-F., A.P.-d.-L., M.F.G.-L. and J.S.-O.; resources, A.P.-d.-L., M.F.G.-L. and J.S.-O.; data curation, F.S.-H. and B.A.M.-G.; writing—original draft preparation, F.S.-H., B.A.M.-G., E.O.-H., A.P.-d.-L., M.F.G.-L. and J.S.-O.; writing—review and editing, F.S.-H., B.A.M.-G., C.M.R.-M., K.M.T.-T., S.R.-L., N.O.-C., N.I.L.-G., G.Y.V.-Z., A.R.-C., J.S.-C., L.F.X.-S., S.M.-R., E.O.-H., A.G.-F., A.P.-d.-L., M.F.G.-L. and J.S.-O.; visualization, F.S.-H., B.A.M.-G., A.P.-d.-L., M.F.G.-L. and J.S.-O.; supervision, A.P.-d.-L., M.F.G.-L. and J.S.-O.; project administration, A.P.-d.-L., M.F.G.-L. and J.S.-O.; funding acquisition, J.S.-O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted following the Declaration of Helsinki and approved by the Institutional Review Board of Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (protocol code 3333, approved on 26 March 2020).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study.
Data Availability Statement
The data presented in this study are available upon reasonable request to the corresponding authors.
Acknowledgments
The authors wish to thank the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán’s personnel, who have tirelessly cared for COVID-19 patients. We would also like to thank all patients who have been cared for in our center.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Behal, M.; Barlow, B.; Mefford, B.; Thompson Bastin, M.L.; Donaldson, J.C.; Laine, M.; Bissell, B.D. Pharmacotherapy in Coronavirus Disease 2019 and Risk of Secondary Infections: A Single-Center Case Series and Narrative Review. Crit. Care Explor. 2021, 3, e0492. [Google Scholar] [CrossRef] [PubMed]
- Osuchowski, M.F.; Winkler, M.S.; Skirecki, T.; Cajander, S.; Shankar-Hari, M.; Lachmann, G.; Monneret, G.; Venet, F.; Bauer, M.; Brunkhorst, F.M.; et al. The COVID-19 Puzzle: Deciphering Pathophysiology and Phenotypes of a New Disease Entity. Lancet Respir. Med. 2021, 9, 622–642. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Vidal, C.; Sanjuan, G.; Moreno-García, E.; Puerta-Alcalde, P.; Garcia-Pouton, N.; Chumbita, M.; Fernandez-Pittol, M.; Pitart, C.; Inciarte, A.; Bodro, M.; et al. Incidence of Co-Infections and Superinfections in Hospitalized Patients with COVID-19: A Retrospective Cohort Study. Clin. Microbiol. Infect. 2021, 27, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Giacobbe, D.R.; Battaglini, D.; Ball, L.; Brunetti, I.; Bruzzone, B.; Codda, G.; Crea, F.; de Maria, A.; Dentone, C.; di Biagio, A.; et al. Bloodstream Infections in Critically Ill Patients with COVID-19. Eur. J. Clin. Investig. 2020, 50, e13319. [Google Scholar] [CrossRef]
- Grasselli, G.; Scaravilli, V.; Mangioni, D.; Scudeller, L.; Alagna, L.; Bartoletti, M.; Bellani, G.; Biagioni, E.; Bonfanti, P.; Bottino, N.; et al. Hospital-Acquired Infections in Critically Ill Patients With COVID-19. Chest 2021, 160, 454–465. [Google Scholar] [CrossRef]
- Ramos, R.; de la Villa, S.; García-Ramos, S.; Padilla, B.; García-Olivares, P.; Piñero, P.; Garrido, A.; Hortal, J.; Muñoz, P.; Caamaño, E.; et al. COVID-19 Associated Infections in the ICU Setting: A Retrospective Analysis in a Tertiary-Care Hospital. Enferm. Infecc. Microbiol. Clin. 2023, 41, 278–283. [Google Scholar] [CrossRef]
- Rouzé, A.; Nseir, S. Hospital-Acquired Pneumonia/Ventilator-Associated Pneumonia and Ventilator-Associated Tracheobronchitis in COVID-19. Semin. Respir. Crit. Care Med. 2022, 43, 243–247. [Google Scholar] [CrossRef]
- Maslove, D.M.; Sibley, S.; Boyd, J.G.; Goligher, E.C.; Munshi, L.; Bogoch, I.I.; Rochwerg, B. Complications of Critical COVID-19. Chest 2022, 161, 989–998. [Google Scholar] [CrossRef]
- Zuglian, G.; Ripamonti, D.; Tebaldi, A.; Cuntrò, M.; Riva, I.; Farina, C.; Rizzi, M. The Changing Pattern of Bacterial and Fungal Respiratory Isolates in Patients with and without COVID-19 Admitted to Intensive Care Unit. BMC Infect. Dis. 2022, 22, 185. [Google Scholar] [CrossRef]
- Chan, X.H.S.; O’Connor, C.J.; Martyn, E.; Clegg, A.J.; Choy, B.J.K.; Soares, A.L.; Shulman, R.; Stone, N.R.H.; De, S.; Bitmead, J.; et al. Reducing Broad-Spectrum Antibiotic Use in Intensive Care Unit between First and Second Waves of COVID-19 Did Not Adversely Affect Mortality. J. Hosp. Infect. 2022, 124, 37–46. [Google Scholar] [CrossRef]
- RECOVERY Collaborative Group. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [CrossRef] [PubMed]
- Salama, C.; Han, J.; Yau, L.; Reiss, W.G.; Kramer, B.; Neidhart, J.D.; Criner, G.J.; Kaplan-Lewis, E.; Baden, R.; Pandit, L.; et al. Tocilizumab in Patients Hospitalized with COVID-19 Pneumonia. N. Engl. J. Med. 2021, 384, 20–30. [Google Scholar] [CrossRef]
- Shafran, N.; Shafran, I.; Ben-Zvi, H.; Sofer, S.; Sheena, L.; Krause, I.; Shlomai, A.; Goldberg, E.; Sklan, E.H. Secondary Bacterial Infection in COVID-19 Patients Is a Stronger Predictor for Death Compared to Influenza Patients. Sci. Rep. 2021, 11, 12703. [Google Scholar] [CrossRef] [PubMed]
- Vijay, S.; Bansal, N.; Rao, B.K.; Veeraraghavan, B.; Rodrigues, C.; Wattal, C.; Goyal, J.P.; Tadepalli, K.; Mathur, P.; Venkateswaran, R.; et al. Secondary Infections in Hospitalized COVID-19 Patients: Indian Experience. Infect. Drug. Resist. 2021, 14, 1893–1903. [Google Scholar] [CrossRef]
- Feng, Y.; Ling, Y.; Bai, T.; Xie, Y.; Huang, J.; Li, J.; Xiong, W.; Yang, D.; Chen, R.; Lu, F.; et al. COVID-19 with Different Severities: A Multicenter Study of Clinical Features. Am. J. Respir. Crit. Care Med. 2020, 201, 1380–1388. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Flanagan, K.L. Sex Differences in Immune Responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef]
- Dessie, Z.G.; Zewotir, T. Mortality-Related Risk Factors of COVID-19: A Systematic Review and Meta-Analysis of 42 Studies and 423,117 Patients. BMC Infect. Dis. 2021, 21, 855. [Google Scholar] [CrossRef]
- Cairns, S.; Reilly, J.; Stewart, S.; Tolson, D.; Godwin, J.; Knight, P. The Prevalence of Health Care–Associated Infection in Older People in Acute Care Hospitals. Infect. Control. Hosp. Epidemiol. 2011, 32, 763–767. [Google Scholar] [CrossRef]
- de Bruyn, A.; Verellen, S.; Bruckers, L.; Geebelen, L.; Callebaut, I.; de Pauw, I.; Stessel, B.; Dubois, J. Secondary Infection in COVID-19 Critically Ill Patients: A Retrospective Single-Center Evaluation. BMC Infect. Dis. 2022, 22, 207. [Google Scholar] [CrossRef]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.-M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-Related Mechanisms in Chronic Kidney Disease Prediction, Progression, and Outcome. J. Immunol. Res. 2018, 2018, 2180373. [Google Scholar] [CrossRef]
- Arredondo, A.; Orozco, E.; Alcalde-Rabanal, J.; Navarro, J.; Azar, A. Retos Sobre La Carga Epidemiológica y Económica Para Diabetes e Hipertensión En México. Rev. Saude Publica 2018, 52, 23. [Google Scholar] [CrossRef] [PubMed]
- Curley, G.F.; Laffey, J.G.; Zhang, H.; Slutsky, A.S. Biotrauma and Ventilator-Induced Lung Injury: Clinical Implications. Chest 2016, 150, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Moser, D.; Feuerecker, M.; Biere, K.; Han, B.; Hoerl, M.; Schelling, G.; Kaufmann, I.; Choukér, A.; Woehrle, T. SARS-CoV-2 Pneumonia and Bacterial Pneumonia Patients Differ in a Second Hit Immune Response Model. Sci. Rep. 2022, 12, 15485. [Google Scholar] [CrossRef]
- Martinez-Guerra, B.A.; Gonzalez-Lara, M.F.; De-Leon-Cividanes, N.A.; Tamez-Torres, K.M.; Roman-Montes, C.M.; Rajme-Lopez, S.; Villalobos-Zapata, G.I.; Lopez-Garcia, N.I.; Martínez-Gamboa, A.; Sifuentes-Osornio, J.; et al. Antimicrobial Resistance Patterns and Antibiotic Use during Hospital Conversion in the COVID-19 Pandemic. Antibiotics 2021, 10, 182. [Google Scholar] [CrossRef] [PubMed]
- Ayoub Moubareck, C.; Hammoudi Halat, D. The Collateral Effects of COVID-19 Pandemic on the Status of Carbapenemase-Producing Pathogens. Front. Cell. Infect. Microbiol. 2022, 12, 823626. [Google Scholar] [CrossRef] [PubMed]
- Habibzadeh, A.; Lankarani, K.B.; Farjam, M.; Akbari, M.; Kashani, S.M.A.; Karimimoghadam, Z.; Wang, K.; Imanieh, M.H.; Tabrizi, R.; Ahmadizar, F. Prevalence of Fungal Drug Resistance in COVID-19 Infection: A Global Meta-Analysis. Curr. Fungal Infect. Rep. 2022, 16, 154–164. [Google Scholar] [CrossRef]
- Peghin, M.; Vena, A.; Graziano, E.; Giacobbe, D.R.; Tascini, C.; Bassetti, M. Improving Management and Antimicrobial Stewardship for Bacterial and Fungal Infections in Hospitalized Patients with COVID-19. Ther. Adv. Infect. Dis. 2022, 9, 20499361221095732. [Google Scholar] [CrossRef]
- Brandi, N.; Ciccarese, F.; Rimondi, M.R.; Balacchi, C.; Modolon, C.; Sportoletti, C.; Renzulli, M.; Coppola, F.; Golfieri, R. An Imaging Overview of COVID-19 ARDS in ICU Patients and Its Complications: A Pictorial Review. Diagnostics 2022, 12, 846. [Google Scholar] [CrossRef]
- Corman, V.M.; Landt, O.; Kaiser, M.; Molenkamp, R.; Meijer, A.; Chu, D.K.; Bleicker, T.; Brünink, S.; Schneider, J.; Schmidt, M.L.; et al. Detection of 2019 Novel Coronavirus (2019-NCoV) by Real-Time RT-PCR. Eurosurveillance 2020, 25, 2000045. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M.; Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; et al. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. JAMA J. Am. Med. Assoc. 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Koehler, P.; Bassetti, M.; Chakrabarti, A.; Chen, S.C.A.; Colombo, A.L.; Hoenigl, M.; Klimko, N.; Lass-Flörl, C.; Oladele, R.O.; Vinh, D.C.; et al. Defining and Managing COVID-19-Associated Pulmonary Aspergillosis: The 2020 ECMM/ISHAM Consensus Criteria for Research and Clinical Guidance. Lancet Infect. Dis. 2021, 21, e149–e162. [Google Scholar] [CrossRef]
- Mermel, L.A.; Allon, M.; Bouza, E.; Craven, D.E.; Flynn, P.; O’Grady, N.P.; Raad, I.I.; Rijnders, B.J.A.; Sherertz, R.J.; Warren, D.K. Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infection: 2009 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 49, 1–45. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Niederman, M.S.; Chastre, J.; Ewig, S.; Fernandez-Vandellos, P.; Hanberger, H.; Kollef, M.; Li Bassi, G.; Luna, C.M.; Martin-Loeches, I.; et al. International ERS/ESICM/ESCMID/ALAT Guidelines for the Management of Hospital-Acquired Pneumonia and Ventilator-Associated Pneumonia. Eur. Respir. J. 2017, 50, 1700582. [Google Scholar] [CrossRef]
- Riley, R.D.; Ensor, J.; Snell, K.I.E.; Harrell, F.E.; Martin, G.P.; Reitsma, J.B.; Moons, K.G.M.; Collins, G.; van Smeden, M. Calculating the Sample Size Required for Developing a Clinical Prediction Model. BMJ 2020, 368, m441. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).