Abstract
Klebsiella pneumoniae causes a variety of infections in both humans and animals. In this study, we characterised the genomes of human and animal isolates from two diagnostic laboratories on St. Kitts, a small Caribbean island inhabited by a large population of vervet monkeys. In view of the increased chances of direct or indirect contact with humans and other animal species, we used the One Health approach to assess transmission of K. pneumoniae across host species by sequencing 82 presumptive K. pneumoniae clinical isolates from humans (n = 51), vervets (n = 21), horses (n = 5), dogs (n = 4) and a cat (n = 1). Whole genome sequencing (WGS) was carried out using Illumina technology. De novo assembly was performed in CLC Genomics Workbench v.11.0. Single nucleotide polymorphisms were detected using NASP followed by phylogenetic analysis using IQ-TREE. Virulence and antimicrobial resistance gene contents were analysed using the Kleborate and CGE pipelines. WGS-based analysis showed that 72 isolates were K. pneumoniae sensu stricto and five K. quasipneumoniae and five K. variicola. K. pneumoniae isolates belonged to 35 sequence types (ST), three of which were occasionally shared between humans and animals: ST23, ST37 and ST307. The ST23 strains from vervets formed a separate cluster amongst publicly available sequenced ST23 strains, indicating the presence of a specific vervet sublineage. Animal strains harbored fewer resistance genes and displayed distinct virulence traits that appeared to be host-specific in vervet isolates. Our results show that K. pneumoniae infections on this Caribbean island are usually caused by host-specific lineages.
1. Introduction
Klebsiella pneumoniae is an important nosocomial pathogen that often displays multidrug resistance, including resistance to last choice antimicrobials such as carbapenems. While there are many publications describing the epidemiology, pathogenicity and antimicrobial resistance of this pathogen in humans [], little information is available on clinical isolates from animals [,,,]. K. pneumoniae has been associated with infections in horses [,,], cats and dogs [], monkeys [,] and cattle [,]. The types of infections seen in these animal species, except for mastitis in cattle, are similar to those observed in humans, mainly urinary tract infections (UTI) and septicemia []. Comparing the genomes of strains of different host origin can be used as one means of estimating the risk of across-host transfer, including zoonotic potential. Carbapenem resistance has been documented in clinical isolates from companion animals but also, in some cases, from livestock []. A growing number of reports on the occurrence of OXA-48 and other types of carbapemenases in bacteria isolated from companion animals have been published worldwide [,,]. However, few data are available on the genetic relatedness of animal and human isolates. Recent studies suggest that K. pneumoniae might be transmitted between dogs and owners within the same household [], and that human and canine strains causing UTI are genetically related [,,,].
In this study, we characterized the genomes of clinical K. pneumoniae isolates obtained at the diagnostic laboratories of a hospital and a veterinary school on the small Caribbean island of St. Kitts. The objective was to assess the risk of zoonotic transmission within this confined geographical area. The island is an ideal place to perform this type of study since it is a small island of about 174 km2 with an estimated population of approximately 57,000 people, and an even larger population of African green monkeys or vervets (Chlorocebus sabaeus) that were introduced during the 17th century on ships running the slave trade from Africa. Based on available data from the main hospital in the Federation of St. Kitts and Nevis, which deals with most of the patients in the country, the incidence of Klebsiella infections in humans is about 80 infections annually. Nevertheless, UTIs may also be treated by primary practitioners and, as such, the data may be an underestimation. Our study was conceived after two previous studies showed that vervets on the island suffer fatal infections caused by hypermucoid K. pneumoniae [] and are a reservoir of this pathogen, with carriage rates of approximately 40% and 20% in captive and wild-caught individuals, respectively []. The true level of infections in vervets cannot be estimated as most animals are living in the wild and no data are available. Available local isolates obtained from companion animals (dog, cat, and horse) were included in the study to study whether there could be another potential source of K. pneumoniae infections on the island, as these animals are in contact with both vervets and humans as well as each other.
2. Results
2.1. Species Identification
Among the 82 isolates identified as K. pneumoniae by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS), 72 were K. pneumoniae sensu stricto (50 human, 17 vervet, three equine, one canine and one feline), five Klebsiella quasipneumoniae subspecies quasipneumoniae (one human, two canine and two equine) and four Klebsiella variicola subspecies variicola (three vervet and one canine) based on Whole Genome Sequence (WGS) analysis. Multilocus sequence typing (MLST) of the 72 K. pneumoniae sensu stricto isolates led to identification of 35 STs, 27 of which were detected amongst human isolates. The two most prevalent lineages among human isolates were sequence type (ST) ST11 (10/50 human isolates) and ST39 (5/50) (Figure 1). Vervet isolates displayed a limited number of STs with ST60 (9/17) and ST23 (5/17) dominating (Figure 1). STs for the remaining K. pneumoniae isolates are displayed in Figure 1. MLST analysis of the five K. variicola subspecies variicola isolates showed that they were all different STs: ST697, ST1708-DLV (double locus variant), ST1791-SLV (single locus variant), ST209-SLV and ST549-SLV. Similarly, all five K. quasipneumoniae subspecies’ quasipneumoniae isolates belonged to distinct STs: ST1539, ST2638, ST1077-DLV, ST2637-SLV and ST338-SLV.
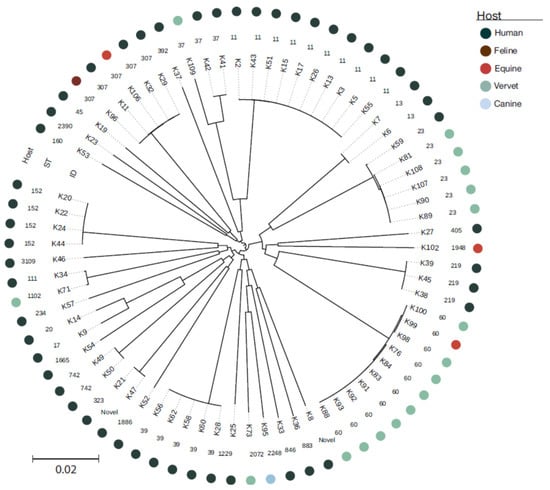
Figure 1.
Host origin, sequence type and SNP-based phylogenetic analysis of all isolates of the study. A figure including analysis of both core genome and accessory genome can be found in Supplementary File S2.
Potential exchange of K. pneumoniae between host species was limited to four STs: ST23 (five vervets and one human), ST307 (one horse, one cat and four humans), ST37 (one vervet and one human) and ST60 (one horse and nine vervets). However, significant differences were observed in the accessory genome of isolates from different hosts belonging to the same ST (Supplementary File S1). A more detailed investigation of the vervet ST23 isolates indicated that they formed a specific clade among the 80 available ST23 genomes in NCBI’s Reference Sequence Database (RefSeq) with data on host and geography (Figure 2).
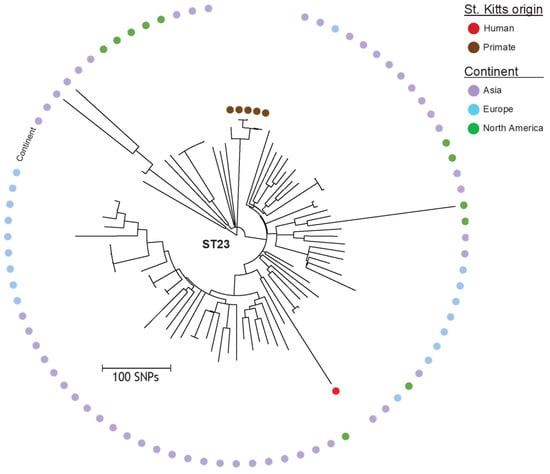
Figure 2.
Detailed SNP-based phylogeny of the five vervet and the single human ST23 K. pneumoniae isolates from this study as well as 80 internationally available human ST23 isolates from NCBI’s RefSeq database. Color labels for isolates of this study represent host (vervet or human), whereas color labels for other isolates represent continent of origin (Asia, Europe or North America).
2.2. Resistance Gene Content
Host-specific differences were also observed in resistance gene content. Human K. pneumoniae isolates generally carried a larger number of resistance genes compared to animal isolates (Supplementary File S1). Most (37/50) human isolates carried at least one acquired resistance gene, whereas the vast majority (19/22) of animal isolates did not carry any. The only three animal isolates harboring acquired resistance genes were two ST307 isolates from a horse and a cat, and one ST37 isolate from a vervet. The equine and feline ST307 isolates shared several resistance genes [blaCTX-M-15, blaOXA-1, aph(3′)-Id, aph(6), aac(3)-IIa, aac(6′)-Ib-cr, qnrB1, sul2, dfrA14 and catB3] and had mutations at gyrA and parC conferring fluoroquinolone resistance, but the equine isolate additionally carried tet(A) and blaTEM1b, whereas the feline isolate carried blaTEM-206. In contrast, none of the three human ST307 isolates carried blaOXA-1 and all of them contained tet(A). Similarly, the resistance gene profile of the ST37 isolate from vervet [blaTEM-1b, aph(3′)-Id, aph(6), aac(3)-IId, aadA2, sul2, dfrA12 and tet(B)] differed from that of the human ST37 isolate in many resistance genes [aadA2, sul1, sul2, dfrA15, catA2, cmlA1 and tet(D)] (Supplementary File S1).
Apart from these host-specific trends, WGS analysis revealed the presence of blaCTX-M-15 (n = 27) encoding extended-spectrum β-lactamase (ESBL); the other β-lactamases detected were blaTEM-1b (n = 24), blaTEM-206 (n = 1) and blaOXA-1 (n = 11), apart from the chromosomal SHV-, LEN- or OKP. Five fosfomycin resistance genes (all contained oqxA and oqxB as well as a fos variant: fosA (n = 77), fosA5 (n = 2) and fosA7 (n = 6)) belong to the core genome of Klebsiella and should not be regarded as acquired. Table N shows the resistance genes found in the K. pneumoniae isolates. Several aminoglycoside resistance genes were detected, as well as sulfonamides and trimethoprim resistance genes. Fluoroquinolone resistance was mediated by mutations, plasmid-mediated quinolone resistance genes and the bifunctional aac(6′)-Ib-cr gene. Detailed information can be found in Supplementary File S1.
2.3. Plasmid Content
Twenty different plasmid replicon types were found, and several of them occurred in different animal species. The most prevalent replicons were ColRNAI (n = 72, found in human and primate isolates) and IncFIB(K) (n = 31, found in human, equine, primate, canine and feline isolates), followed by IncFII(K) (n = 14, found in human, equine, primate, and feline isolates), Col440I (n = 10, found in human isolates only) and IncHI1B (pNDM-Mar) (n = 7, found in human and primate isolates). The other plasmid replicons were carried by four or less isolates, mostly of human origin. Nine isolates did not carry any known plasmid replicons (Supplementary File S1).
2.4. Virulence Gene Content
Host-specific differences were also observed in the distribution of virulence genes. In general, the vervet isolates carried more virulence genes, and the virulence genes frequently differed from those present in human isolates (Supplementary File S1). The yersiniabactin gene was detected in 50% (25/50) of the human K. pneumoniae isolates, 70% (14/20) of the vervet isolates and two out of the three horse isolates (Supplementary File S1). Interestingly, the types of the yersiniabactin locus and the associated integrative conjugative element (ICEKp) differed between human and animal isolates. Host-specific differences in the yersiniabactin locus were observed in isolates belonging to ST23. Namely, the human isolate carried ybt1 on ICEkp10, while the five vervet isolates consistently harbored ybt9 on ICEKp3. All ST60 isolates from vervets (n = 9) and horse (n = 1) were associated with ybt2 on ICEKp1 (Supplementary File S1).
The aerobactin gene iuc1 was present in 13 isolates, including five vervet and one human ST23 isolate. In addition, the salmochelin gene was present in ST23 and ST60 isolates from humans and animals. The two genes associated with the hypermucoid phenotypes, rmpA and rmpA2, were found only in ST23 and ST60 isolates and, mainly in vervet ST23 isolates, only one single human ST23 strain carried the rmpA2_3 gene (Supplementary File S1).
2.5. Virulence and Resistance Scores
Kleborate scores provide a rough categorization of isolates based on their virulence and resistance content. Most isolates displayed a low virulence score of 0, meaning no acquired virulence loci (n = 41), or 1 (yersiniabactin only, n = 27). The 14 isolates with the highest virulence scores included a human ST234 strain with score 2 (yersiniabactin and colibactin, and aerobactin) and all 12 vervet ST23 and ST60 strains that had scores of 4. The only isolate with a score of 5 was the human ST23 strain. Surprisingly, no virulence genes were detected in 25 of the 50 clinical K. pneumoniae isolates from human patients, and 22 had a low virulence score of 1. Based on resistance gene content, 53 and 29 isolates were scored as level 0 (fewer resistance genes) and level 1 (ESBL-positive), respectively. No isolates belonged to levels 2 (carbapenemase-positive) and 3 (carbapenemase- and colistin-positive).
2.6. K. Variicola and K. Quasipneumoniae
No resistance genes were found in the four K. variicola isolates, and only four were detected in the five K. quasipneumoniae: blaTEM1b in the single human isolate, and aph(3”)-Ib, aph(6)-Id and sul1 in one of the two horse isolates. None of the K. quasipneumoniae isolates carried a known virulence gene and only one primate K. variicola isolate carried an iro-like gene, as determined by kleborate, however, its functionality is unknown. Plasmid replicons were only found in three K. quasipneumoniae (the two equine isolates carried IncFIB(K) and the human isolate additionally carried ColRNAI (pIGMS32), Col(pHAD28) and IncR) and two K. variicola isolates (IncFIB(K) in two primate isolates).
3. Discussion
This is one of the few studies investigating the genetic diversity of K. pneumoniae in the Caribbean region using a WGS-based approach, and the sole study including both human and animal isolates from this geographical region. Since the collapse of the sugar industry, the number of vervets has outgrown the human population (estimated in up to 60,000 units), and these monkeys have gradually made their way down from the mountain forests and into residential areas, increasing the probability of direct and indirect contact with humans and consequently the risk of zoonotic transmission of infectious diseases. Interestingly, these monkeys are a natural reservoir of K. pneumoniae [], which is a cause in these animals of opportunistic infections such as pneumonia, meningitis, peritonitis, cystitis and septicemia. A previous study on the island reported the occurrence of a small disease outbreak caused by K. pneumoniae, expressing the hypermucoviscosity phenotype and capsular serotype K2, in a vervet research colony []. All the affected monkeys displayed abscesses, mainly in the abdominal cavity, and less frequently in the lungs, cerebellum and skin.
The present study was primarily conceived to assess whether K. pneumoniae isolates from vervets on St. Kitts are epidemiologically related to those causing infections in the local human and domestic animal populations. The results show that K. pneumoniae isolates from vervets are genetically unrelated to the vast majority of clinical isolates from humans and other animal species. Two genetic lineages, ST60 and ST23, appeared to be most prevalent in vervets. ST60 was isolated from nine vervets and one from abdominal fluid in a horse. Although it was not detected in any human case in this study, this lineage has been sporadically reported in human infections elsewhere [] and has been associated with suppurative peritonitis in captive monkeys belonging to another species, the gold-handed tamarin (Saguinus midas midas) []. ST23 was isolated from five vervets and one patient affected by urinary tract infection during the same period. However, the vervet isolates clustered separately from the human isolate in the phylogenetic analysis and differed with regard to the accessory genome. Namely, the human strain had a virulence score of 5, compared to 4 for the vervet strains. Furthermore, the Yersiniabactin gene was different and located on a different ICE. The aerobactin, Salmochelin and rmpA genes (causing hypermucoviscosity) were also different, and only these strains had a genotype that caused hypermucoviscosity, though the phenotypes were not assessed. The human strain had an additional colibactin gene that was not present in the vervet strains. The ST23 lineage is one of the best-known hypervirulent K. pneumoniae clones and is able to cause severe disease in apparently healthy individuals []. Multidrug-resistant hypervirulent variants of ST23 have been reported in China [,,], India [] and Korea []. Capsular serotype K1 isolates belonging to ST23 have been associated with liver abscesses mainly in Southeast Asia, but sporadic cases, often connected with travel or migration, have been reported from USA, Canada, Spain, France, Belgium, Sweden and Denmark []. A recent population study revealed a rapid global dissemination of hypervirulent clonal-group 23, which typically possess an integrative, conjugative element ICEKp encoding the siderophore yersiniabactin and genotoxin colibactin []. Our analyses show that the vervet ST23 isolates form a distinct monophyletic cluster in the ST23 population (Figure 2). Among the other three STs found in vervets, ST37 was also isolated from two cases of human infection: one urinary tract infection and one case of sepsis. ST37 is a common lineage in humans, frequently associated with ESBL-production, and has been previously found in animals [,,], but in our study they did not carry any genes encoding ESBL. However, vervet and human ST37 isolates from this study clustered separately in the phylogeny and harbored different antimicrobial resistance genes, though all lacked virulence genes (Figure 1). ST1102 and ST2072 were only detected in vervets, but the former ST has been previously reported in humans [].
Our results corroborate recent research indicating that host and ecological adaptations in K. pneumoniae may limit the spread of resistant or virulent clones across humans, animals and the environment []. The same study hypothesized sporadic transmission between humans and companion animals based on the occurrence of healthcare-associated clones such as ST307 and other highly virulent strains in these animals. ST307 is a common ST, globally colonizing and infecting both humans and animals [,,,]. Our study revealed the occurrence of this lineage in one horse, one cat and four human patients. A few host-specific differences were observed in the distribution of resistance, and none of them carried any virulence genes (Figure 1).
Antimicrobial resistance is an important feature of K. pneumoniae. The prevalence of resistance genes among human clinical isolates from St. Kitts was generally low compared to other regions of the world []. In particular, carbapenem and colistin resistance genes were not detected, which probably reflects the low usage of these antimicrobials at the local hospital (Andrea Williams, personal communication). The only ESBL-encoding gene was blaCTX-M-15, which was detected in 25 of the 50 human isolates among multiple lineages (ST307, ST11, St152, ST323, ST39, ST392, ST219 and ST26-1LV). blaCTX-M-15 also occurred in an equine and a feline strain belonging to ST307. K. pneumoniae isolates from vervets did not contain any ESBL-encoding gene and, except for a single ST37 strain, displayed susceptibility to all antimicrobials, which might reflect the absence of usage of antimicrobials in these animals.
Iron-capturing systems are important virulence factors in K. pneumoniae. Yersiniabactin, which allows bacterial growth in iron-deprived situations and protects against phagocyte defenses, is generally present in about one third of the clinical isolates and associated with invasive infections []. In our study, we found several variants of yersiniabactin in human and animal isolates. Interestingly, its prevalence was higher in the vervet isolates (70%) than in isolates from humans (51%) or other animal species, where only two out of ten isolates had a virulence gene. Apart from yersiniabactin, only few other iron-capturing systems were found. Four vervet isolates carried genes associated with the hypermucoid phenotype, which has been previously described as a prevalent phenotypic trait in strains infecting captive vervets on St. Kitts []. It appears that the isolates infecting vervets possess host-specific virulence traits, namely rmpA_1, located on KpVP-1, and rmpA-11, associated with the ICEKp1.
Several different mobile genetic elements (MGE), associated with the spread of antimicrobial resistance genes and virulence genes, were detected among the K. pneumoniae isolates. We could not associate resistance genes and virulence genes to them due to the fragmented nature of Illumina-based draft genomes. Several plasmid incompatibility groups were shared between human and animal isolates (Figure 1), especially IncF. Primate Klebsiella isolates carried several plasmids that were not associated with antimicrobial resistance. These plasmids may instead be involved in virulence.
While performing this study, a cross-Caribbean study based on the WGS of 270 human Klebsiella isolates was published [], further enlarging the knowledge of the population structure of this bacterial species in the Caribbean. Many of the most frequent STs observed in that study were also found in our study (ST11, ST23, ST152 and ST307). However, some of the prevalent STs in our study (ST39 and ST219) were not listed among the main STs in the cross-Caribbean study, indicating possible differences in clonal distribution between countries.
K. quasipneumoniae and K. variicola could only be identified by WGS analysis using Kleborate, as they were not included in our MALDI-TOF MS database. The significance of these species in disease is not yet clear, especially in animals. Antimicrobial resistance was rare and the prevalence of virulence genes was low in these species. A novel iro gene was present in a K. variicola isolate from a vervet. The significance of this finding remains unclear.
4. Materials and Methods
4.1. Bacterial Isolates
The strain collection comprised 82 presumptive K. pneumoniae isolates from humans (n = 51), vervets (n = 21), horses (n = 5), dogs (n = 4) and a cat (n = 1) on St. Kitts. Human isolates were isolated from consecutive clinical samples submitted to the clinical microbiology laboratory at Joseph N France General Hospital between March 2017 and January 2018, whereas animal isolates from clinical samples were collected by the diagnostic laboratory at Ross University School of Veterinary Medicine over the period of 2011–2018. After initial identification by classical biochemical tests, species identification was confirmed by MALDI-TOF MS (Vitek MS RUO, bioMérieux, Marcy-l’Étoile, France) using Saramis v.3.5 (bioMérieux) for spectra interpretation.
4.2. Whole Genome Sequence (WGS) Analysis
Overnight cultures were grown in tryptic soy broth at 37°C with 200 rpm shaking. Genomic DNA was extracted using the DNeasy Blood and Tissue kit (Qiagen). Library preparation was carried out using the Nextera XT kit and paired-end 2 × 250 bp sequencing on a MiSeq, all following standard Illumina protocols (Illumina, Inc., San Diego, California, USA). All raw reads have been deposited in ENA with BioProject ID PRJEB42526.
De novo assembly and MLST were performed in CLC Genomics Workbench v.11.0 using the tools within the Microbial Genomics Module. Various web-based tools, both at the Centre for Genomic Epidemiology (http://www.genomicepidemiology.org/ accessed on 21 September 2020) and Kleborate [], a pipeline specifically for the genetic characterization of Klebsiella whole genomes, were used for species identification, MLST and plasmid replicon typing, as well as to determine the presence and scores of acquired virulence and antimicrobial resistance markers. RAST was used for analysis of plasmid contigs.
To investigate the genetic relatedness of the isolates, a maximum likelihood tree was generated from core genome SNPs. Briefly, sequence reads were mapped against the reference genome of strain FDAARGOS_156 (GenBank accession CP014123) using NASP v.1.0.0 []. First, duplicated regions in the reference were removed using NUCmer followed by aligning of the reads using the Burrows–Wheeler Aligner (Li et al., 2009). All positions with < 10-fold coverage or if the variant was present in <90% of the base calls were excluded. The relatedness of the isolates was inferred using IQ-TREE v.2.1.1 to obtain a midpoint rooted phylogeny. Additionally, using NASP, a phylogeny based on the genomics data of different Klebsiella species (39) was generated for species identification, as well as a midpoint-rooted maximum likelihood SNP-based phylogeny using FastTree v.2.1.10 with all available K. pneumoniae ST23 genomes (n = 80, accessed 9 July 2020) in NCBI’s RefSeq, with available data on host and geography.
5. Conclusions
Human and animal K. pneumoniae infections on St. Kitts are usually caused by genetically distinct, host-specific lineages. Although some monkey isolates belong to ST23, which is often associated with hypervirulent epidemic clones in other parts of the world, WGS-based analysis showed these to cluster separately, have a distinct virulence gene profile and display lower abundance of antimicrobial resistance genes compared to human clinical isolates. These and other differences indicate that the risk of K. pneumoniae transmission between vervets, humans and other animal species appears to be limited by host and ecological barriers
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11010042/s1, Supplementary File S1: Phylogeny and accessory genes of K. pneumoniae, Supplementary File S2: strain information.
Author Contributions
Conceptualization, P.B., L.G. and M.S.; methodology, P.B., L.G. and M.S.; software, P.B., M.S. and A.M.; validation, all authors; formal analysis, P.B. and M.S.; investigation, all authors; resources, A.W. and I.H.-S.; data curation, P.B. and M.S.; writing—original draft preparation, P.B.; writing—review and editing, all authors; visualization, M.S.; supervision, P.B. and L.G.; project administration, P.B. and L.G.; funding acquisition, P.B. and L.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by an intramural grant of RUSVM, grant number 2017LG.
Institutional Review Board Statement
The Interim Ethics Review Committee (IERC) of the Federation of Saint Christopher and Nevis reviewed and approved the study protocol. The IERC approval code is 2017-11-007.
Data Availability Statement
ENA BioProject ID PRJEB42526.
Acknowledgments
We thank Telbert Pyke for his helpi with installing Kleborate and other pipelines on the RUSVM server.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Wang, G.; Zhao, G.; Chao, X.; Xie, L.; Wang, H. The Characteristic of Virulence, Biofilm and Antibiotic Resistance of Klebsiella pneumoniae. Int. J. Environ. Res. Public Health 2020, 17, 6278. [Google Scholar] [CrossRef] [PubMed]
- Heinz, E.; Brindle, R.; Morgan-McCalla, A.; Peters, K.; Thomson, N.R. Caribbean multi-centre study of Klebsiella pneumoniae: Whole-genome sequencing, antimicrobial resistance and virulence factors. Microb. Genomics 2019, 5, e000266. [Google Scholar] [CrossRef]
- Forde, C.; Stierman, B.; Ramon-Pardo, P.; Dos Santos, T.; Singh, N. Carbapenem-resistant Klebsiella pneumoniae in Barbados: Driving change in practice at the national level. PLoS ONE 2017, 12, e0176779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheddie, P.; Dziva, F.; Akpaka, P.E. Detection of a CTX-M group 2 beta-lactamase gene in a Klebsiella pneumoniae isolate from a tertiary care hospital, Trinidad and Tobago. Ann. Clin. Microbiol. Antimicrob. 2017, 16, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melot, B.; Brisse, S.; Breurec, S.; Passet, V.; Malpote, E.; Lamaury, I.; Thiery, G.; Hoen, B. Community-acquired meningitis caused by a CG86 hypervirulent Klebsiella pneumoniae strain: First case report in the Caribbean. BMC Infect. Dis. 2016, 16, 736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmiedel, J.; Falgenhauer, L.; Domann, E.; Bauerfeind, R.; Prenger-Berninghoff, E.; Imirzalioglu, C.; Chakraborty, T. Multiresistant extended-spectrum β-lactamase-producing Enterobacteriaceae from humans, companion animals and horses in central Hesse, Germany. BMC Microbiol. 2014, 14, 187. [Google Scholar] [CrossRef] [Green Version]
- Loncaric, I.; Cabal Rosel, A.; Szostak, M.P.; Licka, T.; Allerberger, F.; Ruppitsch, W.; Spergser, J. Broad-Spectrum Cephalosporin-Resistant Klebsiella spp. Isolated from Diseased Horses in Austria. Animals 2020, 10, 332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanchard, T.L.; Kenney, R.M.; Timoney, P.J. Venereal disease. Vet. Clin. N. Am. Equine Pract. 1992, 8, 191–203. [Google Scholar] [CrossRef]
- Zogg, A.L.; Simmen, S.; Zurfluh, K.; Stephan, R.; Schmitt, S.N.; Nüesch-Inderbinen, M. High Prevalence of Extended-Spectrum β-Lactamase Producing Enterobacteriaceae Among Clinical Isolates From Cats and Dogs Admitted to a Veterinary Hospital in Switzerland. Front. Vet. Sci. 2018, 5, 62. [Google Scholar] [CrossRef] [Green Version]
- Guerra, M.F.; Teixeira, R.H.; Ribeiro, V.L.; Cunha, M.P.; Oliveira, M.G.; Davies, Y.M.; Silva, K.C.; Silva, A.P.; Lincopan, N.; Moreno, A.M.; et al. Suppurative peritonitis by Klebsiella pneumoniae in captive gold-handed tamarin (Saguinus midas midas). J. Med. Primatol. 2016, 45, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Whitehouse, C.A.; Keirstead, N.; Taylor, J.; Reinhardt, J.L.; Beierschmitt, A. Prevalence of hypermucoid Klebsiella pneumoniae among wild-caught and captive vervet monkeys (Chlorocebus aethiops sabaeus) on the island of St. Kitts. J. Wildl. Dis. 2010, 46, 971–976. [Google Scholar] [CrossRef]
- Klaas, I.C.; Zadoks, R.N. An update on environmental mastitis: Challenging perceptions. Transbound. Emerg. Dis. 2018, 65, 166–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schukken, Y.; Chuff, M.; Moroni, P.; Gurjar, A.; Santisteban, C.; Welcome, F.; Zadoks, R. The “other” gram-negative bacteria in mastitis: Klebsiella, Serratia, and more. Vet. Clin. N. Am. Food Anim. Pract. 2012, 28, 239–256. [Google Scholar] [CrossRef] [PubMed]
- Köck, R.; Daniels-Haardt, I.; Becker, K.; Mellmann, A.; Friedrich, A.W.; Mevius, D.; Schwarz, S.; Jurke, A. Carbapenem-resistant Enterobacteriaceae in wildlife, food-producing, and companion animals: A systematic review. Clin. Microbiol. Infect. 2018, 24, 1241–1250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pulss, S.; Stolle, I.; Stamm, I.; Leidner, U.; Heydel, C.; Semmler, T.; Prenger-Berninghoff, E.; Ewers, C. Multispecies and Clonal Dissemination of OXA-48 Carbapenemase in Enterobacteriaceae from Companion Animals in Germany, 2009–2016. Front. Microbiol. 2018, 9, 1265. [Google Scholar] [CrossRef]
- Guerra, B.; Fischer, J.; Helmuth, R. An emerging public health problem: Acquired carbapenemase-producing microorganisms are present in food-producing animals, their environment, companion animals and wild birds. Vet. Microbiol. 2014, 171, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Harada, K.; Usui, M.; Tsuyuki, Y.; Shiraishi, T.; Tamura, Y.; Yokota, S.I. Tigecycline susceptibility of Klebsiella pneumoniae complex and Escherichia coli isolates from companion animals: The prevalence of tigecycline-nonsusceptible K. pneumoniae complex, including internationally expanding human pathogenic lineages. Microb. Drug Resist. 2017, 24, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.M.; Fernandes, M.R.; Sellera, F.P.; Cerdeira, L.; Medeiros, L.K.G.; Garino, F.; Azevedo, S.S.; Lincopan, N. Multidrug-resistant CTX-M-15-producing Klebsiella pneumoniae ST231 associated with infection and persistent colonization of dog. Diagn. Microbiol. Infect. Dis. 2018, 92, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Ovejero, C.M.; Escudero, J.A.; Thomas-Lopez, D.; Hoefer, A.; Moyano, G.; Montero, N.; Martin-Espada, C.; Gonzalez-Zorn, B. Highly Tigecycline-Resistant Klebsiella pneumoniae Sequence Type 11 (ST11) and ST147 Isolates from Companion Animals. Antimicrob. Agents Chemother. 2017, 61, e02640-16. [Google Scholar] [CrossRef] [Green Version]
- Soto, E.; Dennis, M.M.; Beierschmitt, A.; Francis, S.; Sithole, F.; Halliday-Simmons, I.; Palmour, R. Biofilm formation of hypermucoviscous and non-hypermucoviscous Klebsiella pneumoniae recovered from clinically affected African green monkey (Chlorocebus aethiops sabaeus). Microb. Pathog. 2017, 107, 198–201. [Google Scholar] [CrossRef]
- Twenhafel, N.A.; Whitehouse, C.A.; Stevens, E.L.; Hottel, H.E.; Foster, C.D.; Gamble, S.; Abbott, S.; Janda, J.M.; Kreiselmeier, N.; Steele, K.E. Multisystemic abscesses in African green monkeys (Chlorocebus aethiops) with invasive Klebsiella pneumoniae--identification of the hypermucoviscosity phenotype. Vet. Pathol. 2008, 45, 226–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ito, R.; Shindo, Y.; Kobayashi, D.; Ando, M.; Jin, W.; Wachino, J.; Yamada, K.; Kimura, K.; Yagi, T.; Hasegawa, Y.; et al. Molecular epidemiological characteristics of Klebsiella pneumoniae associated with bacteremia among patients with pneumonia. J. Clin. Microbiol. 2015, 53, 879–886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Struve, C.; Roe, C.C.; Stegger, M.; Stahlhut, S.G.; Hansen, D.S.; Engelthaler, D.M.; Andersen, P.S.; Driebe, E.M.; Keim, P.; Krogfelt, K.A. Mapping the Evolution of Hypervirulent Klebsiella pneumoniae. mBio 2015, 6, e00630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, D.; Ma, G.; Li, C.; Jia, X.; Qin, C.; Yang, T.; Wang, L.; Jiang, X.; Ding, N.; Zhang, X.; et al. Emergence of a Multidrug-Resistant Hypervirulent Klebsiella pneumoniae Sequence Type 23 Strain with a Rare bla (CTX-M-24)-Harboring Virulence Plasmid. Antimicrob. Agents Chemother. 2019, 63, e02273-18. [Google Scholar] [CrossRef] [Green Version]
- Liu, B.T.; Su, W.Q. Whole genome sequencing of NDM-1-producing serotype K1 ST23 hypervirulent Klebsiella pneumoniae in China. J. Med. Microbiol. 2019, 68, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhang, X.; Torres, V.V.L.; Liu, H.; Rocker, A.; Zhang, Y.; Wang, J.; Chen, L.; Bi, W.; Lin, J.; et al. An Outbreak of Carbapenem-Resistant and Hypervirulent Klebsiella pneumoniae in an Intensive Care Unit of a Major Teaching Hospital in Wenzhou, China. Front. Public Health 2019, 7, 229. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Naha, S.; Bhadury, P.; Saha, B.; Dutta, M.; Dutta, S.; Basu, S. Emergence of OXA-232-producing hypervirulent Klebsiella pneumoniae ST23 causing neonatal sepsis. J. Antimicrob. Chemother. 2020, 75, 2004–2006. [Google Scholar] [CrossRef] [PubMed]
- Cheong, H.S.; Chung, D.R.; Park, M.; Kim, S.H.; Ko, K.S.; Ha, Y.E.; Kang, C.I.; Peck, K.R.; Song, J.H. Emergence of an extended-spectrum β-lactamase-producing serotype K1 Klebsiella pneumoniae ST23 strain from Asian countries. Epidemiol. Infect. 2017, 145, 990–994. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gundestrup, S.; Struve, C.; Stahlhut, S.G.; Hansen, D.S. First Case of Liver Abscess in Scandinavia Due to the International Hypervirulent Klebsiella pneumoniae Clone ST23. Open Microbiol. J. 2014, 8, 22–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lam, M.M.C.; Wyres, K.L.; Duchêne, S.; Wick, R.R.; Judd, L.M.; Gan, Y.H.; Hoh, C.H.; Archuleta, S.; Molton, J.S.; Kalimuddin, S.; et al. Population genomics of hypervirulent Klebsiella pneumoniae clonal-group 23 reveals early emergence and rapid global dissemination. Nat. Commun. 2018, 9, 2703. [Google Scholar] [CrossRef] [Green Version]
- Hansen, S.K.; Kaya, H.; Roer, L.; Hansen, F.; Skovgaard, S.; Justesen, U.S.; Hansen, D.S.; Andersen, L.P.; Knudsen, J.D.; Røder, B.L.; et al. Molecular characterization of Danish ESBL/AmpC-producing Klebsiella pneumoniae from bloodstream infections, 2018. J. Glob. Antimicrob. Resist. 2020, 22, 562–567. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Li, J.; Wang, Y.; Shen, J.; Shen, Z.; Wang, S. Presence of NDM in non-E. coli Enterobacteriaceae in the poultry production environment. J. Antimicrob. Chemother. 2019, 74, 2209–2213. [Google Scholar] [CrossRef] [Green Version]
- Zhong, X.S.; Li, Y.Z.; Ge, J.; Xiao, G.; Mo, Y.; Wen, Y.Q.; Liu, J.P.; Xiong, Y.Q.; Qiu, M.; Huo, S.T.; et al. Comparisons of microbiological characteristics and antibiotic resistance of Klebsiella pneumoniae isolates from urban rodents, shrews, and healthy people. BMC Microbiol. 2020, 20, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorpe, H.; Booton, R.; Kallonen, T.; Gibbon, M.J.; Couto, N.; Passet, V.; Lopez Fernandez, J.S.; Rodrigues, C.; Matthews, L.; Mitchell, S.; et al. One Health or Three? Transmission modelling of Klebsiella isolates reveals ecological barriers to transmission between humans, animals and the environment. bioRxiv 2021, 8, 455249. [Google Scholar] [CrossRef]
- Carvalho, I.; Alonso, C.A.; Silva, V.; Pimenta, P.; Cunha, R.; Martins, C.; Igrejas, G.; Torres, C.; Poeta, P. Extended-Spectrum Beta-Lactamase-Producing Klebsiella pneumoniae Isolated from Healthy and Sick Dogs in Portugal. Microb. Drug Resist. 2020, 26, 709–715. [Google Scholar] [CrossRef]
- Harada, K.; Shimizu, T.; Mukai, Y.; Kuwajima, K.; Sato, T.; Usui, M.; Tamura, Y.; Kimura, Y.; Miyamoto, T.; Tsuyuki, Y.; et al. Phenotypic and Molecular Characterization of Antimicrobial Resistance in Klebsiella spp. Isolates from Companion Animals in Japan: Clonal Dissemination of Multidrug-Resistant Extended-Spectrum β-Lactamase-Producing Klebsiella pneumoniae. Front. Microbiol. 2016, 7, 1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wyres, K.L.; Hawkey, J.; Hetland, M.A.K.; Fostervold, A.; Wick, R.R.; Judd, L.M.; Hamidian, M.; Howden, B.P.; Löhr, I.H.; Holt, K.E. Emergence and rapid global dissemination of CTX-M-15-associated Klebsiella pneumoniae strain ST307. J. Antimicrob. Chemother. 2019, 74, 577–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lam, M.M.C.; Wick, R.R.; Watts, S.C.; Cerdeira, L.T.; Wyres, K.L.; Holt, K.E. A genomic surveillance framework and genotyping tool for Klebsiella pneumoniae and its related species complex. Nat. Commun. 2021, 12, 4188. [Google Scholar] [CrossRef]
- Sahl, J.W.; Lemmer, D.; Travis, J.; Schupp, J.M.; Gillece, J.D.; Aziz, M.; Driebe, E.M.; Drees, K.P.; Hicks, N.D.; Williamson, C.H.D.; et al. NASP: An accurate, rapid method for the identification of SNPs in WGS datasets that supports flexible input and output formats. Microb. Genomics 2016, 2, e000074. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).