Abstract
Knee osteoarthritis (KOA) is a major cause of pain and disability worldwide, with no current treatment modality able to prevent the progressive destruction of articular cartilage. Mesenchymal stem cells (MSCs) have attracted interest in treating KOA and cartilage injury due to their self-renewal and multidirectional differentiation potential, as well as local bioactive factors with immunomodulatory and regenerative potential. This study aimed to evaluate the currently available studies using the intra-articular injection of Wharton’s jelly MSCs for KOA and cartilage injury. We analyzed all clinical trials published from inception to 31 December 2023. Six studies met the inclusion criteria, for a total of 97 patients and 134 knees. The follow-up period ranged from 3 to 48 months. There were no serious adverse effects noted. There was significant improvement in functional outcomes in the form of VAS, WOMAC, KOOS, and IKDC parameters, though radiological outcomes demonstrated mixed results. In conclusion, patients with KOA treated with intra-articular injections of Wharton’s jelly MSCs showed improvements in functional outcomes with no severe adverse effects. Multiple injections of Wharton’s jelly MSCs showed better outcomes compared to single-injection techniques. Wharton’s jelly MSCs may have potential as a cornerstone in the future treatment of KOA.
1. Introduction
Knee osteoarthritis (OA) is one of the most common joint disorders in the world, with an estimated 251 million people suffering from knee OA worldwide, according to the Global Burden of Disease 2010 Study. OA is also more prevalent in the aging population. The World Health Organization (WHO) estimated that 524 million people suffering from OA in 2010 were aged 65 or older, and this number is expected to triple, representing 16% of the world’s population by 2050. Knee OA is characterized by the progressive loss of articular cartilage, osteophytes, subchondral cysts, joint space narrowing, and intermittent inflammation of the joint tissues [1]. The exact pathogenesis of OA is still poorly understood, but it is thought to be a complex interplay among mechanical, biochemical, cellular, genetic, and immunologic phenomena [2]. The results of the progressive loss of joint cartilage may suggest there is an imbalance between the rate of cartilage loss and restoration, which may be due to the failure of the body to replenish the cartilage lost through normal use and aging, an inadequate response to injury or inflammation, or both [3]. On a related issue, articular cartilage injury of the knee may result from acute traumatic injury or subacute injury associated with other knee pathologies. Articular cartilage demonstrates limited regenerative potential in response to injury and, therefore, has been implicated as a potential risk factor in the development of early-onset OA [4].
According to the American Academy of Orthopaedic Surgeons (AAOS), the current treatment modalities for knee OA range from non-surgical methods, which include lifestyle modification, physiotherapy, multimodal analgesia, and intra-articular knee injection, to operative options, which include arthroscopic procedures, corrective osteotomies, and joint replacement surgeries [5]. The treatments for knee chondral injury range from symptomatic treatment with the usage of multimodal analgesia, intra-articular knee injections to surgical options, which include surgical debridement, cartilage reparative procedures including marrow stimulation techniques, cartilage replacement such as osteochondral transplantation, or regeneration for example autologous chondrocyte implantation.
While some of the treatment options may benefit patients through mainly symptomatic relief, none of them can prevent the affected articular cartilage from progressive destruction [6]. Interest in the use of biologic agents for regenerative medicine applications including in knee OA and chondral injury has increased in recent decades. The usage of mesenchymal stem cells (MSCs) in cartilage repair was pioneered by Wakitani et al. in 1998 [7]. The exact mechanism through which stem cell therapy may benefit knee OA is still not fully understood. Although native articular cartilage has a limited ability to regenerate, it is believed that injecting an adequate number of stem cells into the affected joint could alleviate symptoms or improve joint structure and function. This improvement may occur through cartilage restoration, stimulation of the body’s natural repair processes via growth factor secretion, support of other repair cells, or modulating the immune response [8].
There are multiple sources of MSCs, including bone marrow, adipose tissue, umbilical cord including Wharton’s jelly (WJ), amniotic fluid, blood, liver, and dental tissues. WJ is a mucoid connective tissue enclosing the three blood vessels of the umbilical cord, which is inherently rich with mesenchymal stem cells. WJ offers multiple distinct advantages, which include [9] (1) properties from both prenatal and postnatal MSCs; (2) no ethical issues regarding acquisition; (3) strong potential for proliferation and differentiation; (4) no risk of tumorigenicity; (5) stability of the karyotype; (6) elevated immunomodulatory activity; and (7) for patients in whom autologous MSCs have weaker stem cell capability.
Currently, the systematic reviews that concentrate on human umbilical cord (hUC) MSCs from WJ sources are limited. This systematic review was conducted to evaluate the current data regarding the safety and efficacy of hUC-MSCs from WJ sources for the treatment of knee OA and chondral injury.
2. Materials and Methods
2.1. Search Method
For a comprehensive search of health science journals, we used CINAHL (via EBSCOhost) and Medline (via PUBMED). The database was searched until 31 December 2023. The search strategy included all research trials using terms and keywords with Boolean operator strategies. The terms used were Wharton jelly, umbilical cord, mesenchymal stem cell, osteoarthritis, chondral, cartilage, knee, pain, function, QOL, quality of life, KOOS, IKDC, WOMAC, and Lysholm score, as listed below:
Keyword 1 “Wharton jelly” OR “umbilical cord” OR “mesenchymal stem cell” OR “osteoarthritis” OR “chondral” OR “cartilage” AND “knee”
AND
Keyword 2 “Pain” OR “function” OR “QOL” OR “quality of life” OR “KOOS” OR “IKDC” OR “WOMAC” OR “Lysholm”
Furthermore, the references of all retrieved articles were reviewed for relevant citations.
2.2. Inclusion Criteria
All human clinical trials that investigated the effect of hUC-MSCs from WJ sources in knee OA and cartilage injury were included from inception until 31 December 2023. Due to limited resources, only manuscripts written in English were included in this review.
2.3. Exclusion Criteria
Case reports, case series, animal studies, letters to the editor, posters, and review articles were excluded.
2.4. Screening of Article for Eligibility
We conducted this systematic review according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines. This systematic review was registered with the Open Science Framework Database (https://osf.io) on 25 August 2024 and possesses a registration DOI of https://doi.org/10.17605/OSF.IO/P5NHY.
The article screening process occurred in several phases. Initially, any article with a title that did not meet the inclusion criteria was excluded. Then, the abstracts of the remaining articles were evaluated, and those failing to meet the inclusion criteria were excluded. In the final phase, the full texts of the remaining articles were thoroughly assessed and included in our study if they met the inclusion and exclusion criteria. All authors participated in the selection and data extraction process, and any disagreements were resolved through consensus. A flowchart summarizing the article selection process and reasons for exclusion is presented in Figure 1.
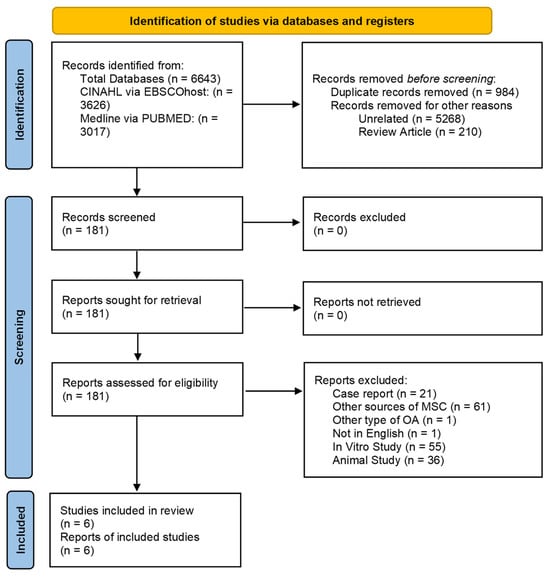
Figure 1.
Flow chart showing article selection process.
2.5. Data Extraction
The data from the relevant studies were individually extracted, detailing both the study design and outcomes. Key aspects of the study designs included the sample size, subject characteristics, methods of MSC collection and processing, and the duration of follow-up. The reported outcomes encompassed safety, clinical efficacy, and radiological assessments.
3. Results
3.1. Study Design and Patient Demographics
Six studies met the inclusion and exclusion criteria, which included a total of 97 patients with 134 knees who received hUC-MSCs. Four studies were nonrandomized [10,11,12,13], while the other two were randomized [14,15]. For the Kellgren–Lawrence (KL) classification, all six studies included patients who suffered from knee OA KL classifications I to IV. Follow-up periods ranged from 3 to 48 months.
3.2. hUC-MSC Preparation
All studies explained the method of processing their hUC-MSCs, with MSC criteria in accordance with the International Society for Cellular Therapy (ISCT) guidelines [16].
3.3. Administration Method
In terms of number of injections, 3 studies used a single-injection technique to deliver the hUC-MSCs into the knee [11,12,15], while the other studies divided the hUC-MSCs into 2 injections, with 1 study administering the injection within 1 month apart [10], while another study administered the injections 6 months apart [14]. Another study divided the MSCs into four injections in 1-week intervals [13].
All 6 studies used a different dose for their studies, with the doses of hUC-MSCs ranging from 10 × 106 cells to 10 × 107 cells. One study used body weight as a guide for the dose of hUC-MSCs [10]. Other studies used a fixed dose, as mentioned in Table 1. In addition, another study also injected hyaluronic acid (HA) during the injection of hUC-MSCs, which was repeated on the 2nd and 3rd weeks [11].

Table 1.
Study design, subjects, procedure, and dose.
3.4. Adverse Effects
No serious adverse effects were observed in any of the studies. The most common adverse effect was knee effusion, which resolved spontaneously in all cases. Another common adverse effect seen was pain. One patient developed superficial vein phlebitis over the right short saphenous vein, which resolved spontaneously [10].
3.5. Functional Outcome
Among the 6 selected studies, there were multiple clinical parameters that were used to monitor clinical improvement, which included the visual analog scale (VAS) [11,12,13,14,15], the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [11,12,13,14], the Knee Injury and Osteoarthritis Outcome Score (KOOS) [10,15], the International Knee Documentation Committee (IKDC) [11], the SF-36 questionnaire [12,14], and the SF-12 questionnaire [13].
Out of 5 studies, 1 study reported VAS improvement with statistical significance [12]. In another study, a statistically significant result was also observed only in the repeated-injection group (MSC-2) compared to the single-injection group and control group [14], while VAS was statistically significant initially but was not sustained by 12th month [11]. While for the other study [15], there were some improvements; however, they were not statistically significant.
As for the WOMAC scores, 3 studies reported improvement with statistical significance [11,12,14]. Furthermore, there was a steady improvement in the WOMAC scores over the whole study period in MSC-2 (2 injections) as compared to MSC-1 (single-injection group) [14].
In two studies [10,15], there was a significant clinical improvement in the KOOS parameter. A significant improvement in the KOOS parameter was observed after 4 years of follow-up [10]. In another study, there was an improvement up to 8 weeks; however, these clinical improvements were not sustained [15].
In terms of the IKDC parameter, a statistically significant improvement was observed, with the mild OA group showing sustained improvement till study endpoint [11].
The author did not provide statistically relevant data in one of the studies [13]; however, there was generally a significant improvement in all parameters measured.
3.6. Radiological Outcome
There was no standardized timing or outcome measurements in any of the studies regarding radiological outcomes. Each clinical trial used different protocols and timing intervals to measure improvement, as mentioned in Table 2.

Table 2.
Safety, clinical, and radiological outcomes.
The severity of abnormal changes either disappeared or shifted to a milder form, which was statistically significant in one of the studies [10]. In another study, the measurement using MOAKS in 14 articular subregions showed a mixed result, with T2 values decreased in 9 of 14 regions; however, only 1 region was statistically significant, and an increase in cartilage thickness was observed in 10 of 14 regions, but only significant in 5 regions [12]. In other studies [11,14,15], the MRI outcomes were not statistically significant.
4. Discussion
The injection of hUC-MSCs is safe, as demonstrated by this and other systematic reviews, which included other types of MSCs, commonly bone marrow and adipose tissue [17,18,19,20]. The most common adverse effect of MSC knee injection was knee swelling or effusion, which spontaneously resolved without intervention. The adverse effects may be related to the dose of MSCs, which was demonstrated by another systematic review, where a higher dose of MSCs caused more adverse events [18]. Even though MSCs are generally regarded as having low immunogenicity, they can still trigger an immune reaction [21]. Another point of concern is about the neoplastic potential in the joint due to stem cells’ multidirectional growth potential. Up to this point in time, according to current data, no adverse effects in terms of joint deformity, tumor formation, or death have been reported [22]. Long-term follow-up studies showed that serum tumor markers did not increase from before to 3 years after MSCs therapy [23].
Based on the results of this systematic review, hUC-MSCs are effective for treating knee OA, from mild to severe forms of knee OA. HUC-MSC administration could improve functional outcomes, or VAS, WOMAC, KOOS, and IKDC scores, with a persistent improvement that may be archived even beyond 48 months, which may signify a functional disease-modifying therapy [10]. It is possible that the effects of hUC-MSCs are more significant in lower grades of knee OA [11], whereas the paracrine activity of MSCs would be more effective in milder knee OA [19].
Multiple injections of hUC-MSCs may be more effective compared to a single dose, as, in one study, the MSC-2 injection group showed more significant improvements compared to the single-injection group [14].
Radiological outcomes demonstrated mixed results. There was an improvement in cartilage thickness; however, this was generally not significant, which was also observed by another network meta-analysis of different sources of MSCs [22]. Clinical outcomes may not correlate with MRI findings, with hUC-MSCs still being useful for symptomatic treatment rather than restoration to normal knee articular cartilage and anatomy. The ‘unrelated’ outcome of clinical and radiological findings may be due to a misconception in the understanding of MSCs. MSCs were named after a group of cells that could be isolated and cultured while maintaining the potential to be induced into other types of mesoderm cells. Thus, unfortunately, the term is being used to infer that these cells differentiate into regenerating tissue-producing cells. The term “Medicinal Signaling Cells” has been recommended to better describe these cells’ ability to target sites of injury or disease and release bioactive factors that are both immunomodulatory and regenerative, functioning as therapeutic agents [24]. Upon activation by injury or other methods, MSCs secrete several bioactive molecules that create a regenerative microenvironment by establishing a powerful trophic field [21].
Comparing multiple sources of MSCs, hUC-MSCs were the most effective in improving function in one network meta-analysis [22].
5. Limitations
There are a few limitations to this systematic review. The sample sizes were small in all the clinical trials. The dose of hUC-MSCs varied among studies, with some studies adding other adjuncts to the knee injection. The clinical trials in these studies lacked uniformity in monitoring the clinical and radiological outcomes including the MRI parameter, resulting in interpretation and data analysis difficulties. The study periods were also relatively short and with variable intervals of monitoring. Most of the study periods in this systematic review were less than 1 year. A longer duration is needed to see any possible long-term adverse effects and clinical outcomes. All these differences may have led to differences in evaluating the therapeutic effects of hUC-MSCs in the treatment of knee OA. More clinical trials with a longer follow-up period and larger patient numbers are needed to prove the safety and efficacy of hUC-MSCs in treating knee OA.
6. Conclusions
The intra-articular injection of hUC-MSCs is safe and improves pain and functional outcomes in the treatment of knee OA. Multiple injections of hUC-MSCs show better results compared to the single-injection technique. The use of hUC-MSCs for the treatment of knee OA may be the mainstay of therapy in the future.
Author Contributions
Conceptualization, A.H.M.Y.B. and M.I.-S.; methodology, I.N.-M.; validation, S.F.A.W.; formal analysis, M.I.-S. and M.S.Z.; resources, A.H.M.Y.B.; data curation, M.I.-S., A.F.M.D., N.M. and M.K.R.R.; writing—original draft preparation, M.I.-S. and M.K.R.R.; writing—review and editing, M.I.-S., I.N.-M. and M.S.Z.; supervision, I.N.-M., S.F.A.W. and A.H.M.Y.B.; project administration, M.I.-S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data are provided within the article and are available from the corresponding author upon request.
Acknowledgments
We would like to acknowledge the support of the professors, lecturers, administrative, and supporting staff of the Faculty of Medicine, University Kebangsaan Malaysia, in completing this systematic review.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Abramson, S.B.; Attur, M. Developments in the scientific understanding of osteoarthritis. Arthritis Res. Ther. 2009, 11, 227. [Google Scholar] [CrossRef]
- Creamer, P.; Hochberg, M.C. Osteoarthritis. Lancet 1997, 350, 503–508. [Google Scholar] [CrossRef]
- Martel-Pelletier, J.; Barr, A.J.; Cicuttini, F.M.; Conaghan, P.G.; Cooper, C.; Goldring, M.B.; Goldring, S.R.; Jones, G.; Teichtahl, A.J.; Pelletier, J.P. Osteoarthritis. Nat. Rev. Dis. Primers 2016, 2, 16072. [Google Scholar] [CrossRef]
- Roseti, L.; Desando, G.; Cavallo, C.; Petretta, M.; Grigolo, B. Articular Cartilage Regeneration in Osteoarthritis. Cells 2019, 8, 1305. [Google Scholar] [CrossRef]
- Brophy, R.H.; Fillingham, Y.A. AAOS Clinical Practice Guideline Summary: Management of Osteoarthritis of the Knee (Nonarthroplasty), Third Edition. J. Am. Acad. Orthop. Surg. 2022, 30, e721–e729. [Google Scholar] [CrossRef]
- Mora, J.C.; Przkora, R.; Cruz-Almeida, Y. Knee osteoarthritis: Pathophysiology and current treatment modalities. J. Pain Res. 2018, 11, 2189–2196. [Google Scholar] [CrossRef]
- Wakitani, S.; Imoto, K.; Yamamoto, T.; Saito, M.; Murata, N.; Yoneda, M. Human autologous culture expanded bone marrow mesenchymal cell transplantation for repair of cartilage defects in osteoarthritic knees. Osteoarthr. Cartil. 2002, 10, 199–206. [Google Scholar] [CrossRef]
- Whittle, S.L.; Johnston, R.V.; McDonald, S.; Worthley, D.; Campbell, T.M.; Buchbinder, R. Stem cell injections for osteoarthritis of the knee. Cochrane Database Syst. Rev. 2019, 2019, CD013342. [Google Scholar] [CrossRef]
- Arutyunyan, I.; Elchaninov, A.; Makarov, A.; Fatkhudinov, T. Umbilical Cord as Prospective Source for Mesenchymal Stem Cell-Based Therapy. Stem Cells Int. 2016, 2016, 6901286. [Google Scholar] [CrossRef]
- Samara, O.; Jafar, H.; Hamdan, M.; Al-Ta’mari, A.; Rahmeh, R.; Hourani, B.; Mandalawi, N.; Awidi, A. Ultrasound-guided intra-articular injection of expanded umbilical cord mesenchymal stem cells in knee osteoarthritis: A safety/efficacy study with MRI data. Regen. Med. 2022, 17, 299–312. [Google Scholar] [CrossRef] [PubMed]
- Dilogo, I.H.; Canintika, A.F.; Hanitya, A.L.; Pawitan, J.A.; Liem, I.K.; Pandelaki, J. Umbilical cord-derived mesenchymal stem cells for treating osteoarthritis of the knee: A single-arm, open-label study. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 799–807. [Google Scholar] [CrossRef]
- Günay, A.E.; Karaman, I.; Guney, A.; Karaman, Z.F.; Demirpolat, E.; Gonen, Z.B.; Dogan, S.; Yerer, M.B. Assessment of clinical, biochemical, and radiological outcomes following intra-articular injection of Wharton jelly-derived mesenchymal stromal cells in patients with knee osteoarthritis: A prospective clinical study. Medicine 2022, 101, e30628. [Google Scholar] [CrossRef]
- Ao, Y.; Duan, J.; Xiong, N.; Qian, N.; Zhang, R.; Yang, L.; Yu, S.; Wang, F. Repeated intra-articular injections of umbilical cord-derived mesenchymal stem cells for knee osteoarthritis: A phase I, single-arm study. BMC Musculoskelet. Disord. 2023, 24, 488. [Google Scholar] [CrossRef]
- Matas, J.; Orrego, M.; Amenabar, D.; Infante, C.; Tapia-Limonchi, R.; Cadiz, M.I.; Alcayaga-Miranda, F.; González, P.L.; Muse, E.; Khoury, M.; et al. Umbilical Cord-Derived Mesenchymal Stromal Cells (MSCs) for Knee Osteoarthritis: Repeated MSC Dosing Is Superior to a Single MSC Dose and to Hyaluronic Acid in a Controlled Randomized Phase I/II Trial. Stem Cells Transl. Med. 2019, 8, 215–224. [Google Scholar] [CrossRef]
- Khalifeh Soltani, S.; Forogh, B.; Ahmadbeigi, N.; Hadizadeh Kharazi, H.; Fallahzadeh, K.; Kashani, L.; Karami, M.; Kheyrollah, Y.; Vasei, M. Safety and efficacy of allogenic placental mesenchymal stem cells for treating knee osteoarthritis: A pilot study. Cytotherapy 2019, 21, 54–63. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.; Horwitz, E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef] [PubMed]
- Jiang, P.; Mao, L.; Qiao, L.; Lei, X.; Zheng, Q.; Li, D. Efficacy and safety of mesenchymal stem cell injections for patients with osteoarthritis: A meta-analysis and review of RCTs. Arch. Orthop. Trauma Surg. 2021, 141, 1241–1251. [Google Scholar] [CrossRef] [PubMed]
- Jeyaraman, M.; Muthu, S.; Ganie, P.A. Does the Source of Mesenchymal Stem Cell Have an Effect in the Management of Osteoarthritis of the Knee? Meta-Analysis of Randomized Controlled Trials. Cartilage 2021, 13 (Suppl. 1), 1532S–1547S. [Google Scholar] [CrossRef]
- de Windt, T.S.; Vonk, L.A.; Slaper-Cortenbach, I.C.; van den Broek, M.P.; Nizak, R.; van Rijen, M.H.; de Weger, R.A.; Dhert, W.J.; Saris, D.B. Allogeneic Mesenchymal Stem Cells Stimulate Cartilage Regeneration and Are Safe for Single-Stage Cartilage Repair in Humans upon Mixture with Recycled Autologous Chondrons. Stem Cells 2017, 35, 256–264. [Google Scholar] [CrossRef]
- Qu, H.; Sun, S. Efficacy of mesenchymal stromal cells for the treatment of knee osteoarthritis: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2021, 16, 11. [Google Scholar] [CrossRef]
- Lopa, S.; Colombini, A.; Moretti, M.; de Girolamo, L. Injective mesenchymal stem cell-based treatments for knee osteoarthritis: From mechanisms of action to current clinical evidences. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2003–2020. [Google Scholar] [CrossRef]
- Wei, Z.J.; Wang, Q.Q.; Cui, Z.G.; Inadera, H.; Jiang, X.; Wu, C.A. Which is the most effective one in knee osteoarthritis treatment from mesenchymal stem cells obtained from different sources?—A systematic review with conventional and network meta-analyses of randomized controlled trials. Ann. Transl. Med. 2021, 9, 452. [Google Scholar] [CrossRef]
- Margiana, R.; Markov, A.; Zekiy, A.O.; Hamza, M.U.; Al-Dabbagh, K.A.; Al-Zubaidi, S.H.; Hameed, N.M.; Ahmad, I.; Sivaraman, R.; Kzar, H.H.; et al. Clinical application of mesenchymal stem cell in regenerative medicine: A narrative review. Stem Cell Res. Ther. 2022, 13, 366. [Google Scholar] [CrossRef]
- Caplan, A.I. Mesenchymal Stem Cells: Time to Change the Name! Stem Cells Transl. Med. 2017, 6, 1445–1451. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).