Abstract
The quality of the enamel plays a critical role in the retention and performance of orthodontic brackets. This systematic review and meta-analysis aimed to evaluate the effect of resin infiltration pretreatment on the shear bond strength (SBS) of orthodontic brackets. An electronic search was conducted in October 2024 using PubMed, Web of Science (WoS), and Scopus databases, employing the keywords (resin infiltration AND bracket); (ICON AND bracket). The review adhered to PRISMA guidelines and utilized the PICO framework. Of the 143 articles initially identified, 63 underwent screening. Strict inclusion criteria were applied of which the most important were resin infiltration pretreatment, studies conducted on natural teeth and SBS evaluation. This left 19 studies for final analysis. The risk of bias was assessed using the checklist for quasi-experimental studies (Non-Randomized Experimental Studies) developed by the Joanna Briggs Institute (JBI). Among these, 13 studies used human teeth and 13 utilized Transbond XT as the adhesive. Metal brackets were predominantly examined (n = 17). The Adhesive Remnant Index (ARI) was assessed in 13 studies. Importantly, 11 studies concluded that resin infiltration significantly enhances SBS, 8 of which were conducted on human teeth. The meta-analysis revealed significantly higher SBS results when resin infiltrate was applied to healthy enamel. This finding underscores the dual benefits of resin infiltration: increased bond strength and the protection of enamel integrity during debonding procedures. The results suggest that resin infiltration not only improves the mechanical retention of orthodontic brackets but also serves as an enamel-preserving approach.
1. Introduction
Enamel morphogenesis is a complex process that begins with the secretion of enamel matrix protein, followed by mineralization and maturation [1]. Abnormalities in these processes lead to enamel developmental disorders (DDE). These include hypomineralization, hypomaturation, hypoplasia, and hyperplasia. Their causes may be systemic, genetic, or environmental, such as fluorosis, amelogenesis imperfecta, or vitamin D deficiency. Hypomineralization and hypomaturation are qualitative defects and occur due to disorders in the maturation phase of amelogenesis. [2]. Hypomineralization manifests itself as a soft, chalky, or cheese-like appearance of the enamel, while hypomaturation presents as opaque and discolored enamel that fractures easily [3]. There is usually a clear border with healthy tissue [4]. Hypoplasia is a quantitative defect caused by abnormal thickness of the enamel [5]. It manifests itself as pitting, fissuring, or absence of enamel. In most of these cases of DDE the bond with the adhesive material is disturbed. That makes tooth reconstruction and bonding of orthodontic brackets difficult. This is believed to be due to the shielding of the enamel mineral by acid-insoluble proteins [6]. Hyperplasia, on the other hand, is characterized by the presence of enamel rings protruding beyond the normal surface of the crown on all erupted teeth [7]. The incorrect shape of the vestibular surface of the teeth makes it difficult not only to bond, but also to position the orthodontic brackets correctly.
The need for treatment, preventing further damage and improving aesthetics, has led to the development of several noninvasive methods for treating noncavity carious lesions and DDE, including fluoride, casein phosphopeptide, and amorphous calcium phosphate [8]. A relatively new product that combines prevention with restoration is the resin infiltration agent [9]. It penetrates demineralized enamel lesions and closes intercrystalline spaces by creating a polymer skeleton. That micromechanically blocks remaining enamel prisms and hydrogen ions, preventing further demineralization and caries development while increasing microhardness [9,10,11]. Due to the low viscosity of the resin, the pores between the crystals are filled, creating a diffusion barrier within the entire lesion (Figure 1). It leads to hardening of the demineralized tissues and increasing their mechanical strength [10]. This type of treatment is often used in young patients who often need orthodontic care. Therefore, the question of how it will affect subsequent treatment with fixed orthodontic appliances, which is a challenge in patients with demineralization and DDE due to adhesion problems, is very important.
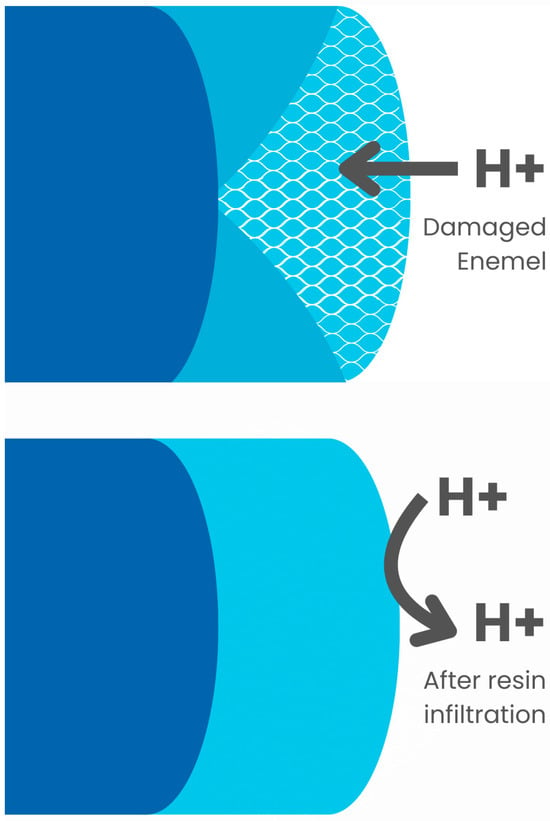
Figure 1.
Resin infiltration.
Accidental debonding of an orthodontic bracket during treatment with fixed appliances can lead to longer treatment times, higher treatment costs, frustration, and dissatisfaction for both the patient and the dentist, increase the risk of white spots appearing and, in some cases, even to uncontrolled tooth movement [12,13,14,15,16]. That is why it is so important that the brackets stay on the teeth throughout the entire treatment process. There are numerous scientific studies analyzing the factors that affect the detachment of brackets. Some authors divide them into factors dependent and independent of the patient [17,18,19]. Others, distinguish early and late factors [20]. As observations show, most accidental detachments of brackets occur immediately after their gluing. This is related to errors in the procedure of gluing the brackets and the duration of full polymerization of the composite, which can last from 30 min to 24 h [21,22,23,24]. Late failures are caused by mechanical damage to the device by the patient. They most often result from non-compliance with recommendations, especially dietary ones, aging of the composite material, and the formation of white spots around the orthodontic brackets, which weaken the bond of the adhesive material with the enamel [20,25]. Unfortunately, in some cases, orthodontic treatment must be continued or even started despite the presence of enamel demineralization.
Despite the additional difficulty in maintaining the brackets on the teeth due to the reduced SBS to demineralized enamel, there is also an increased risk of enamel damage during debonding of the brackets [26]. It should be remembered that after the orthodontic treatment is completed, the brackets must be removed without damaging the enamel. Therefore, during bonding, the goal should not be to achieve maximum bond strength, but to proceed with great caution. According to research, the minimum shear bond strength (SBS) that allows the bracket to be held throughout the treatment process should be between 6 and 8 MPa [27]. Other authors report that even at a force of 10 MPa, there is a risk of damaging the enamel during debonding [28,29] (Figure 2).
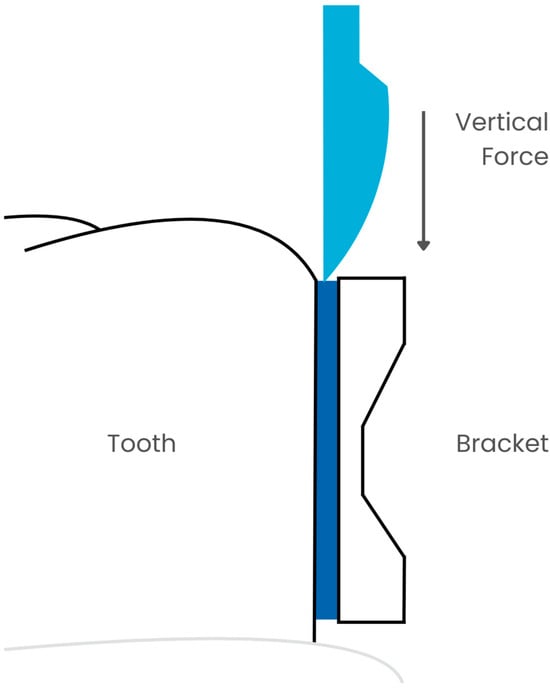
Figure 2.
SBS measurement.
Due to the constant increase in demand for orthodontic treatment, patients with DDE are increasingly appearing in offices. It is extremely important to be aware of how to provide them with the most comfortable treatment while minimizing the risk of enamel damage during removal of the appliance, which is much greater than in healthy patients. However, the authors of this systematic review did not identify any previous reviews assessing the impact of Resin Infiltrant Agents on the shear bond strength of orthodontic brackets. This study aims to address this gap.
2. Materials and Methods
2.1. Focused Question
The systematic review followed the PICO framework [30] as follows: In the case of orthodontic bracket bonding (population), will the use of resin infiltration (investigated condition) affect shear bond strength (outcome) compared to bonding without enamel pretreatment (comparison condition)?
2.2. Protocol
The selection process for articles included in the systematic review was carefully outlined following the PRISMA flow diagram [31] (see Figure 3). The systematic review was registered on the Open Science Framework under the following link: https://doi.org/10.17605/OSF.IO/CRK2W (accessed 5 October 2024).
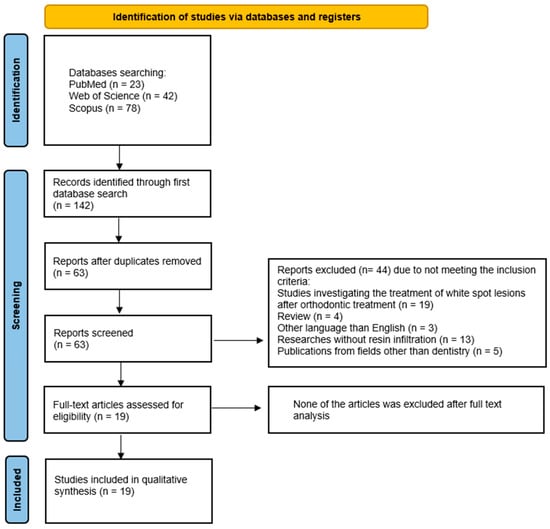
Figure 3.
The PRISMA 2020 flow diagram.
2.3. Eligibility Criteria
The researchers agreed to include only the articles that met the following criteria [32,33,34,35,36,37,38,39,40]:
- Resin infiltration pretreatment;
- Studies conducted on natural teeth;
- SBS evaluation studies;
- In vitro and in vivo studies;
- Use all kinds of orthodontic brackets;
- Studies in English;
- Full-text articles.
The exclusion criteria the reviewers agreed upon were as follows [32,33,34,35,36,37,38,39,40]:
- No resin infiltration pretreatment;
- No SBS evaluation;
- Non-English papers
- Systematic review articles;
- Review articles;
- No full-text accessible;
- Duplicated publications.
No restrictions were applied with regard to the year of publication.
2.4. Information Sources, Search Strategy, and Study Selection
In October 2024, the PubMed, Scopus, and Web of Science (WoS) databases were searched to find articles meeting the specified inclusion criteria. To find articles focusing on the influence of resin infiltration pretreatment on shear bond strength of orthodontic brackets, the search was narrowed to specific keywords: (resin infiltration AND bracket); (ICON AND bracket). In the Scopus and WoS database, the results were refined to titles, abstracts, and keywords, while in PubMed, they were narrowed down to titles and abstracts. All searches conformed to the predefined eligibility criteria, and only articles with accessible full-text versions were taken into consideration.
2.5. Data Collection and Data Items
Two reviewers (J.K. and S.K.) carefully selected the articles that met the inclusion criteria. The extracted data were then introduced into a standardized Excel file.
2.6. Assessing Risk of Bias in Individual Studies
In the preliminary phase of selecting studies, the authors independently examined the titles and abstracts of each study to reduce the possibility of reviewer bias. They evaluated the level of consensus among reviewers using Cohen’s κ test [41]. The authors resolved any disagreements about whether to include or exclude a study through discussions.
2.7. Quality Assessment
Two independent reviewers (J.M. and M.D.) assessed the procedural quality of each study included in the article using the Joanna Briggs Institute (JBI) checklist for quasi-experimental studies (nonrandomized experimental studies) [42]. The checklist consists of 9 questions:
- Is it clear in the study what is the ‘cause’ and what is the ‘effect’?
- Were the participants included in any similar comparisons?
- Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest? Was there a control group?
- Were there multiple measurements of the outcome both before and after the intervention/exposure?
- Was a follow up completed, and if not, were differences between groups in terms of their follow up adequately described and analyzed? Were the outcomes of participants included in any comparisons measured in the same way?
- Were the outcomes measured in a reliable way?
- Was an appropriate statistical analysis used?
The answer to these questions can be yes, no, unclear, not applicable. Any discrepancies in answering were resolved through discussion until a consensus was reached.
2.8. Meta-Analysis
Sheer bond strength was calculated in some of the reviewed studies and could be compared with the meta-analytic tools. The publications were divided depending on whether the resin infiltrates healthy or demineralized enamel. In order to compare the raw mean differences between the treated and control groups, the researchers applied forest plots. In order to detect potential publication bias, the researchers evaluated funnel plots, along with rank correlation tests and regression tests.
The degree of heterogeneity (tau2) was estimated using restricted maximum likelihood [43]. In addition to the tau2 estimate, the Q-test for heterogeneity and the I2 statistic were also used. Analyses were performed separately for studies made on sound and demineralized enamel.
Statistical analysis was performed with Jamovi 2.3.28 [44], supported by the R statistical environment [45] with the MAJOR package [43].
In order to compare the raw SBS values between studies conducted on demineralized and sound teeth, the weighted mean was compared using Welch’s t-test.
3. Results
3.1. Study Selection
A search of the electronic databases PubMed, Scopus, and WoS yielded 143 records. Of these, 80 were duplicates and were thus removed. The remaining 63 articles were subjected to abstract screening, which resulted in the exclusion of 44 articles that did not meet the inclusion criteria: 19 studies were investigating the treatment of white spot lesions after orthodontic treatment, 4 studies were review, 3 studies were written in other languages than English, in 13 studies the resin infiltrant was not in use, and 5 studies were from other fields than dentistry. A thorough analysis of the 19 confirmed that all of them met the inclusion criteria. Therefore, the final number of articles included in this review was 19.
3.2. General Characteristics of the Included Studies
The studies included in the systematic review present research focused on the shear bond strength of orthodontic brackets bonded to the enamel pretreated with resin infiltrants. The general characteristics of the studies are presented in Table 1. Thirteen researchers decided to conduct the experiment on human teeth [46,47,48,49,50,51,52,53,54,55,56,57,58], while the rest used bovine teeth [59,60,61,62,63,64]. In 13 studies, Transbond XT was used as the only adhesive material [46,48,52,53,54,55,56,57,58,60,61,63,64]. Four authors conducted tests on several adhesive materials and compared them with each other [47,49,50,59], and two did not provide the name of the agent used [51,62]. Seventeen authors examined metal brackets [46,47,48,49,50,51,52,53,55,57,58,59,60,61,62,63,64], while the remaining two did not provide information about the material of the brackets used [54,56].

Table 1.
General characteristic of the included studies.
The largest number of authors, 10, decided to compare SBS after covering the enamel with various preparations inhibiting demineralization [46,48,52,53,54,56,57,60,61,62]. Three of them conducted studies on bovine teeth [60,61,62]. Triwardhani et al. observed the highest SBS values on resin-infiltrated teeth, but at the same time he received the highest ARI value [62]. Despite this, he recommends infiltration. On the other hand, the results of Attin et al. [60] and Vianna et al. [61] suggest that infiltration does not affect SBS. From a clinical point of view, more important are studies conducted on human teeth. Among them, only Gulec et al. concluded that resin infiltration reduces the SBS value, but they additionally checked the content of mineral substances in the tooth tissues and after infiltration it was increased [46]. Costenoble et al. decided to bond the brackets immediately after infiltration and a month later [56]. Their results show that in the case of waiting a month, the SBS value becomes significantly lower, which does not happen when the procedures are performed immediately after each other. The remaining authors agree that infiltration increases the SBS, and its value is similar to that obtained on healthy enamel or even higher [48,52,53,54,57]. Ekizer et al. [54] and Baka et al. [48] showed that a similar effect can be obtained using CPP-ACP, which was not confirmed by Nimbalkar et al. [57].
Naidu et al. [59] and Mews et al. [63] used resin infiltration not only on demineralized enamel but also on healthy enamel and came to the same conclusions that even on healthy enamel there is an increase in bond strength and, in addition, despite the increase in ARI, there are fewer enamel defects after debonding.
Montasser and Taha [55] and Al-Mayali [50] studied the effect of different bonding agents on SBS after resin infiltration. Their results are completely different. While Montasser and Taha [55] obtained the lowest SBS values with ICON and self-etching primer, Al-Mayali [50] obtained the highest bond strength with this combination. However, both studies have one thing in common—resin infiltration causes more adhesive to remain on the enamel. Yetkiner et al., in addition to using different bonds, also checked the effect of H3PO4 and HCl etching, but found no significant differences with SBS [64].
Insee et al. [47] and Anicic et al. [49] investigated whether the adhesive used to bond brackets affects SBS when infiltration is used. It turned out to be not insignificant. However, their results were contradictory. Insee et al. [47] obtained a decrease in SBS with Assure Plus, while Anicic et al. [49] obtained the highest bond strength with this adhesive. However, both obtained results similar to the control group with Transbond XT.
Interesting and original studies were conducted by Al-Mayali et al. [51] and Hammad et al. [58]. They investigated how diet affects the SBS of brackets after resin infiltration. Al-Mayali et al. [51] used the storage of teeth in ethanol and corn oil and concluded that despite the significant negative impact of these substances, especially alcohol, on SBS, infiltration causes an increase in bond strength regardless of the conditions. Hammad et al. [58], examining in vivo the effect of Coca-Cola and Sprite beverages on teeth intended for extraction, reached identical conclusions.
3.3. Main Study Outcomes
The detailed characterization of selected studies is presented in Table 2. Publications varied with each other in terms of the assessed parameters. Thirteen authors evaluated the composite remaining on the teeth using ARI [46,47,48,49,50,53,54,55,56,59,62,63,64], and for the purpose of this review, the arithmetic mean was calculated to compare the results. It turned out that in three works it was over 1 [46,53,54], and in another three over 2 [47,55,63]. SEM analysis was performed for six studies [48,52,56,58,62,64], and only in one of them damage to the enamel surface was observed, and this study used bovine teeth [62]. Only in three works was the SBS value below 10 MPa [46,47,62]. Eleven researchers concluded that resin infiltration significantly increases SBS value [48,49,50,51,52,54,57,58,59,62,63]; eight of these studies were conducted on human teeth [48,49,50,51,52,54,57,58].

Table 2.
Detailed characteristics of studies.
3.4. Quality Assessment
For all of the 9 questions, 14 papers received a positive answer to 8 of them [46,47,48,49,50,51,52,53,54,55,56,57,60,61], 4 papers received a positive answer to 7 [58,62,63,64], and 1 remaining paper received a positive answer to 6 of them [59] (see Table 3).

Table 3.
Quality assessment—JBI checklist for quasi-experimental studies (nonrandomized experimental studies) [42].
3.5. Meta-Analysis
The raw data used for the meta-analysis, along with the division into groups, are presented in Table 4.

Table 4.
Numerical data with division into groups used for meta-analysis.
Meta-analysis showed that when resin infiltration of healthy enamel was used, SBS values were significantly higher in the control groups. Eight studies conducted on sound enamel were included in the analysis (Figure 4). Mean differences ranged from −3.0000 to 5.2000, with 62% of the estimates being positive. The estimated mean difference based on the random effects model was \hat{\mu} = 2.8643 (95% CI: 2.6249 to 3.1037). The mean score was significantly different from zero (z = 23.4512, p < 0.0001). According to the Q test, the true scores appeared to be heterogeneous (Q(7) = 15.9369, p = 0.0257, tau2 = 0.0000, I2 = 0.0006%). The 95% prediction interval for the true scores is given by 2.6249 to 3.1037. Hence, the true results of the studies are in the same direction as the estimated mean result, even though some heterogeneity may exist. Two groups (Hammad et al. (2013)-Transbond XT-human-sound.1; Hammad et al. (2013)-Transbond XT-human-sound.2 [58]) had relatively large weights compared to the rest of the studies (i.e., \mbox{weight} \ge 3/k, so a weight at least 3 times as large as having equal weights across studies). An examination of the studentized residuals revealed that one study (Montasser and Taha (2014)-Transbond XT-human-sound.2 [55]) had a value larger than ±2.7344 and may be a potential outlier in the context of this model. According to the Cook’s distances, none of the studies could be considered to be overly influential.
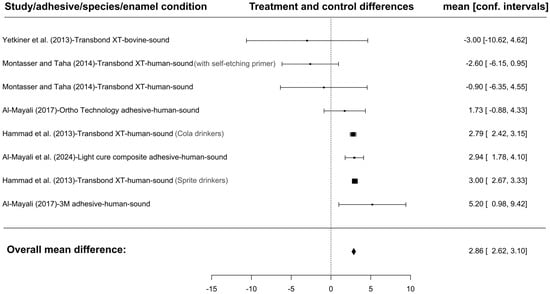
Figure 4.
The forest plot for SBS is shown below. A total of eight groups were assessed because five of the studies included multiple groups relevant to the current analysis, which were presented separately. For each study, the absolute differences between the means for the treated and untreated groups (represented by the black rectangles), and their confidence intervals are displayed. The size of the rectangle corresponds to the number of evaluated teeth. The dashed line in the middle represents the ‘point of no effect’. The results on the left side of the plot show studies in which the treated group had a lower SBS value compared to the control group, while those on the right side indicate higher values [50,51,55,58,64]. The figure was created with Jamovi 2.3.28 (Jamovi, Australia) software.
The meta-analysis showed that in the case of resin infiltration of demineralized enamel there were no significant differences in the SBS level between the study and control groups. A total of 18 groups presenting results conducted on demineralized enamel were included in the analysis (Figure 5). The observed mean differences ranged from −13.8000 to 8.9500, with the majority of estimates being negative (56%). The estimated average mean difference, based on the random-effects model, was μ^ = −0.7533\hat{\mu} = −0.7533 (95% CI: −3.3999 to 1.8933). Therefore, the average outcome did not differ significantly from zero (z = −0.5579, p = 0.5769). According to the Q-test, the true outcomes appeared to be heterogeneous (Q(17) = 308.9387, p < 0.0001, tau2 = 30.8538, I2 = 97.1450%). A 95% prediction interval for the true outcomes ranged from −11.9573 to 10.4506. Hence, although the average outcome is estimated to be negative, in some studies the true outcome may, in fact, be positive. No study had a value greater than ±2.9913 in the examination of the studentized residuals, indicating the absence of outliers in the context of this model. No study was considered overly influential according to Cook’s distances. Neither the regression test nor the rank correlation showed any asymmetry in the funnel plot (p = 0.6540 and p = 0.7099, respectively).
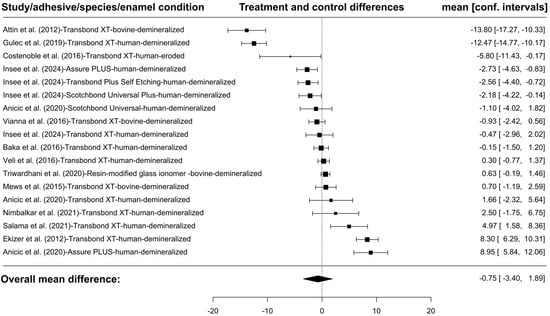
Figure 5.
The forest plot on SBS is shown below. The final number of groups assessed was 18 because some of the 13 studies assessed included multiple groups relevant to the current analysis and were presented separately. For each study, the absolute differences between the mean for the treated and untreated groups (black rectangle) and the confidence intervals are shown. The size of the rectangle refers to the number of evaluated teeth. The dashed line in the middle shows the ‘point of no effect’. The results on the left-hand side of the table illustrate studies in which the treated group exhibited a lower SBS value in comparison to the control group, while those on the right-hand side demonstrate higher values [46,47,48,49,52,53,54,56,57,60,61,62,63]. The figure was created with Jamovi 2.3.28 (Jamovi, Australia) software.
A comparison of SBS values between healthy and demineralized enamel showed that significantly higher values occurred in the case of healthy enamel. (See Figure 6).
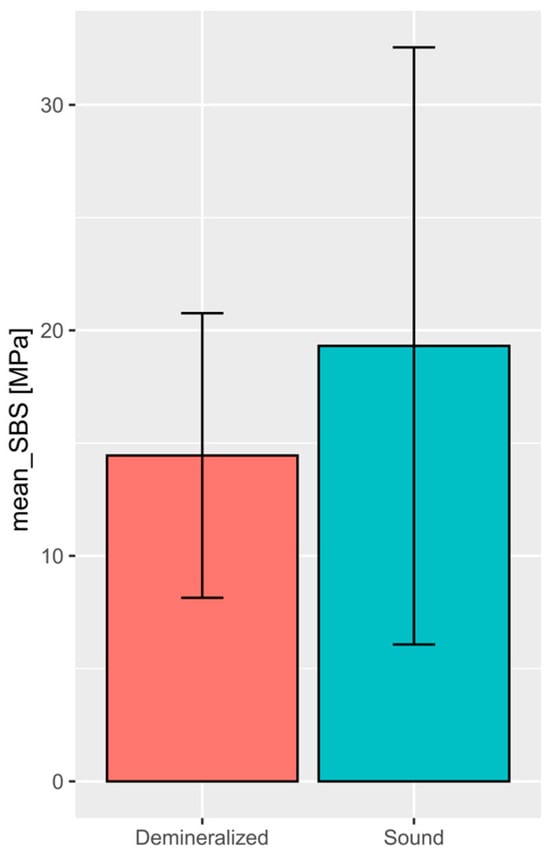
Figure 6.
The following plot provides a comparison of the raw values of SBS among studies on demineralized and sound teeth. The plot shows weighted means and standard deviations, which reflect the different size of populations included in the studies. The difference presented is statistically significant (Welch’s t-test p-value = 0.0002) [65]. The figure was created with Jamovi 2.3.28 (Jamovi, Australia) software.
4. Discussion
The aim of this systematic review was to determine the effect of resin infiltration on the bond strength of orthodontic brackets. Eleven researchers found that resin infiltration significantly increased the SBS value [48,49,50,51,52,54,57,58,59,62,63]; eight of these studies were conducted on human teeth [48,49,50,51,52,54,57,58]. The analysis showed that the use of infiltration has no significant effect on the SBS of demineralized enamel; what is more, in the control groups the SBS was higher than after pretreatment of healthy enamel. Thirteen authors evaluated the composite remaining on the teeth using ARI [46,47,48,49,50,53,54,55,56,59,62,63,64]. Of these, six obtained a medium result below 1 [48,49,50,56,59,64]. No correlation was found between SBS and ARI values. SEM analysis was performed for six studies [48,52,56,58,62,64], and only in one of them damage to the enamel surface was observed. Additionally, it was a study using bovine teeth [62].
A few authors in their publication stated that at SBS above 10 MPa during debonding of orthodontic brackets, damage to the enamel may occur due to detachment of its prisms [28,29]. It is therefore alarming that after infiltration only three authors obtained SBS below 10 MPa [46,47,62]. In seven studies this result was within the range of 10–15 MPa [47,48,49,50,51,58,61], and in the remaining ones it was even higher [49,50,52,53,54,55,56,57,63,64]. Articles in which different adhesive materials were used show that the material used has a large effect on SBS. Al-Mayali, who studied adhesives from Ortho Technology and 3M, obtained a difference in bond strength of 7.78 MPa [50]. Insee et al. obtained the highest SBS values for Transbond XT material [47], similarly in the case of the study conducted by Demirsoy et al. without the use of infiltration, they obtained an average SBS value for Transbond XT of 15.03 MPa [66]. In contrast, in the study of Anicic et al. the bond strength for Transbond XT was 7.29 MPa lower than for Assure Plus [49]. This only proves the need for further research. However, according to the results of the meta-analysis, even after resin infiltration, the SBS value of demineralized enamel is significantly lower than that of healthy enamel.
Four researchers conducting experiments on bovine teeth determined the ARI [59,62,63,64]. Their mean results ranged from 0 [64] to 2.4 [63], which is significantly better than the values obtained in studies without the use of ICON, where the mean obtained by da Rocha et al. was 2.73 [67], while Henkin et al., using metal brackets from different companies, obtained mean results from 0.47 to 2.4, depending on the brackets used [68]. In the case of human teeth, ARI was measured in nine studies [46,47,48,49,50,53,54,55,56]. The lowest mean score of 0.5 was obtained by Costenoble et al. and Baka et al. [48,56], while the highest was 2.7 by Montasser and Taha [55]. In studies without resin infiltration, the results were lower. Mean values from 0.92 to 1.67, depending on the brackets used, were declared by Cervantes-Ganoza et al. [69], and Nawrocka et al. obtained mean scores from 1.9 to 2 [70]. Lower ARI scores are more beneficial in orthodontics because the need to remove remaining adhesive is an additional risk factor for damage to the enamel surface [71].
Assessment of the enamel surface using Scanning Electron Microscope (SEM) after the debonding of brackets allows for the determination of whether one of the important goals of research on shear bond strength has been achieved, namely minimizing enamel damage [72]. According to the research of Lishna et al., after debonding of metal brackets, in 25% of cases a rough surface, numerous thick scratches, and fine grooves are visible in SEM [73]. Among the works qualified for review, the SEM assessment was only descriptive without providing the Enamel Demage Index (EDI), which makes a reliable assessment difficult. Triwardhani et al. noticed damage in the form of irregular enamel porosity and damaged honeycombs, but there were fewer of them than in the control group [62]. However, Yetkiner et al. and Hammad et al. did not notice any enamel damage in the SEM image [58,64].
The need for research on ceramic brackets is immediately apparent, especially since Bakhadher in his review indicated ceramic brackets as a factor for increasing shear bond strength, and at the same time increasing the risk of enamel damage during debonding [74]. It may also be important to examine SBS during debonding using a different force direction. All of the researchers tested the force parallel to the enamel surface, and the studies by Klocke and Kahl-Nieke show that the force direction significantly affects SBS [75]. It would be worthwhile to examine the enamel surface after debonding using SEM with EDI to enable a reliable comparison of results. Additionally, it cannot be ignored that individual researchers who decided to conduct tests on various adhesive materials proved that SBS is dependent on them. However, there are too few studies to draw reliable conclusions.
Our study has several limitations that should be acknowledged. A meta-analysis for Adhesive Remnant Index (ARI) could not be conducted due to its ordinal nature and the lack of uniformity in the scales used across studies, with some employing a 0–3 scale and others a 1–4 scale. Although we standardized these scales to enable comparisons by presenting results as percentages, this approach may not fully capture the nuances of ordinal data or allow for advanced statistical analyses. Additionally, the interpretation of Scanning Electron Microscope (SEM) results posed a challenge, as only a limited number of studies provided SEM data, and several relied on the reader’s interpretation of the images without detailed descriptions. These inconsistencies limited the depth of analysis and comparability of the results. Furthermore, the division of studies into those conducted on healthy and demineralized enamel, while necessary for meaningful comparisons, introduced methodological heterogeneity. Lastly, the reliance on percentage representation for ARI and the variability in study designs underscore the need for more standardized methodologies in future research to enhance data comparability and the robustness of meta-analyses.
5. Conclusions
The presented studies allow us to clearly state that the use of ICON has a positive effect on orthodontic treatment by increasing shear bond strength while protecting the enamel from damage during debonding. There is no correlation between SBS and ARI values. The obtained results indicate that the use of resin infiltration of enamel before orthodontic treatment with fixed appliances can have significant clinical benefits. First of all, it reduces the risk of enamel damage during debonding in patients with DDE. Additionally, it can be used in patients who have difficulties in following dietary recommendations and, therefore, often experience accidental debonding of brackets, which often results in a significant extension of treatment time.
Author Contributions
Conceptualization, S.K. and J.K.; methodology, S.K.; software, S.K.; validation, J.K. and S.K.; formal analysis, S.K. and J.K.; investigation, S.K. and J.K.; resources, S.K. and J.K.; data curation, S.K. and J.K.; writing—original draft preparation, S.K. and J.K.; writing—review and editing, S.K. and J.M.; visualization, S.K. and J.K.; supervision, M.D.; project administration, S.K and J.K.; funding acquisition, J.M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financed by a subsidy from Wroclaw Medical University, number SUBZ.B180.24.058.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Olczak-Kowalczyk, D.; Krämer, N.; Gozdowski, D.; Turska-Szybka, A. Developmental Enamel Defects and Their Relationship with Caries in Adolescents Aged 18 Years. Sci. Rep. 2023, 13, 4932. [Google Scholar] [CrossRef] [PubMed]
- Robinson, C. Enamel Maturation: A Brief Background with Implications for Some Enamel Dysplasias. Front. Physiol. 2014, 5, 388. [Google Scholar] [CrossRef] [PubMed]
- Seow, W.K. Developmental Defects of Enamel and Dentine: Challenges for Basic Science Research and Clinical Management. Aust. Dent. J. 2014, 59, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Weerheijm, K.L. Molar Incisor Hypomineralization (MIH): Clinical Presentation, Aetiology and Management. Dent. Update 2004, 31, 9–12. [Google Scholar] [CrossRef]
- Bartlett, J.D. Dental Enamel Development: Proteinases and Their Enamel Matrix Substrates. ISRN Dent. 2013, 2013, 684607. [Google Scholar] [CrossRef]
- Nathwani, N.S.; Kelleher, M. Minimally Destructive Management of Amelogenesis Imperfecta and Hypodontia with Bleaching and Bonding. Dent. Update 2010, 37, 170–179. [Google Scholar] [CrossRef]
- Sedano, H.O.; Gorlin, R.J. Ringed Enamel Hyperplasia. Oral Surg. Oral Med. Oral Pathol. 1975, 39, 456–457. [Google Scholar] [CrossRef]
- Innes, N.P.T.; Frencken, J.E.; Bjørndal, L.; Maltz, M.; Manton, D.J.; Ricketts, D.; Van Landuyt, K.; Banerjee, A.; Campus, G.; Doméjean, S.; et al. Managing Carious Lesions: Consensus Recommendations on Terminology. Adv. Dent. Res. 2016, 28, 49–57. [Google Scholar] [CrossRef]
- Allen, D.N.; Fine, C.M.; Newton, M.N.; Kabani, F.; Muzzin, K.B.; Reed, K.M. Resin Infiltration Therapy: A Micro-Invasive Treatment Approach for White Spot Lesions. J. Dent. Hyg. 2021, 95, 31–35. [Google Scholar]
- Zakizade, M.; Davoudi, A.; Akhavan, A.; Shirban, F. Effect of Resin Infiltration Technique on Improving Surface Hardness of Enamel Lesions: A Systematic Review and Meta-Analysis. J. Evid.-Based Dent. Pract. 2020, 20, 101405. [Google Scholar] [CrossRef]
- Perdigão, J. Resin Infiltration of Enamel White Spot Lesions: An Ultramorphological Analysis. J. Esthet. Restor. Dent. 2020, 32, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Kiyamehr, Z.; Razeghinejad, M.H.; Rahbar, M.; Oskouei, S.G.; Vafaei, A. Factors Affecting the Duration of Fixed Orthodontic Treatment in Patients Treated in a University Department between 2016 and 2020. Maedica 2022, 17, 380–386. [Google Scholar] [CrossRef]
- Skidmore, K.J.; Brook, K.J.; Thomson, W.M.; Harding, W.J. Factors Influencing Treatment Time in Orthodontic Patients. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.D.; Campbell, P.M.; Schneiderman, E.D.; Buschang, P.H. A Practice-Based Evaluation of the Prevalence and Predisposing Etiology of White Spot Lesions. Angle Orthod. 2016, 86, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, K. Factors Affecting the Formation, Severity and Location of White Spot Lesions during Orthodontic Treatment with Fixed Appliances. J. Oral Maxillofac Res. 2014, 5, e4. [Google Scholar] [CrossRef]
- Stasinopoulos, D.; Papageorgiou, S.N.; Kirsch, F.; Daratsianos, N.; Jäger, A.; Bourauel, C. Failure Patterns of Different Bracket Systems and Their Influence on Treatment Duration: A Retrospective Cohort Study. Angle Orthod. 2018, 88, 338–347. [Google Scholar] [CrossRef]
- Aikins, E.; Ututu, C. An Audit of Bonding Failure among Orthodontic Patients in a Tertiary Hospital in South-South Nigeria. Int. J. Orthod. Rehabil. 2017, 8, 91. [Google Scholar] [CrossRef]
- Romano, F.L.; Correr, A.B.; Correr-Sobrinho, L.; Magnani, M.B.; Ruellas, A.C. Clinical Evaluation of the Failure Rates of Metallic Brackets. J. Appl. Oral Sci. 2012, 20, 228–234. [Google Scholar] [CrossRef]
- Khan, H.; Mheissen, S.; Iqbal, A.; Jafri, A.R.; Alam, M.K. Bracket Failure in Orthodontic Patients: The Incidence and the Influence of Different Factors. Biomed. Res. Int. 2022, 2022, 5128870. [Google Scholar] [CrossRef]
- Oesterle, L.J.; Shellhart, W.C. Effect of Aging on the Shear Bond Strength of Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 716–720. [Google Scholar] [CrossRef]
- Yamamoto, T.; Hanabusa, M.; Momoi, Y.; Sakaguchi, R.L. Polymerization Stress of Dental Resin Composite Continues to Develop 12 Hours after Irradiation. J. Esthet. Restor. Dent. 2015, 27, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, L.J.; Shellhart, W.C.; Belanger, G.K. Effect of Tacking Time on Bond Strength of Light-Cured Adhesives. J. Clin. Orthod. 1997, 31, 449–453. [Google Scholar] [PubMed]
- Oesterle, L.J.; Newman, S.M.; Shellhart, W.C. Comparative Bond Strength of Brackets Cured Using a Pulsed Xenon Curing Light with 2 Different Light-Guide Sizes. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, L.J.; Craig Shellhart, W.; Fisher, A. Effect of Primer Precuring on the Shear Bond Strength of Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 699–702. [Google Scholar] [CrossRef]
- Eliades, T.; Bourauel, C. Intraoral Aging of Orthodontic Materials: The Picture We Miss and Its Clinical Relevance. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 403–412. [Google Scholar] [CrossRef]
- Iijima, M.; Muguruma, T.; Brantley, W.A.; Ito, S.; Yuasa, T.; Saito, T.; Mizoguchi, I. Effect of Bracket Bonding on Nanomechanical Properties of Enamel. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 735–740. [Google Scholar] [CrossRef]
- Cozza, P.; Martucci, L.; De Toffol, L.; Pencoc, S.I. Shear Bond Strength of Metal Brackets on Enamel. Angle Orthod. 2006, 76, 851–856. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J.; Zmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Brugnera, A.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM, and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef]
- Kiryk, J.; Matys, J.; Nikodem, A.; Burzyńska, K.; Grzech-Leśniak, K.; Dominiak, M.; Dobrzyński, M. The Effect of Er:Yag Laser on a Shear Bond Strength Value of Orthodontic Brackets to Enamel—A Preliminary Study. Materials 2021, 14, 2093. [Google Scholar] [CrossRef]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a Knowledge Representation for Clinical Questions. AMIA Annu. Symp. Proc. 2006, 2006, 359–363. [Google Scholar]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Struzik, N.; Wiśniewska, K.; Piszko, P.J.; Piszko, A.; Kiryk, J.; Matys, J.; Dobrzyński, M. SEM Studies Assessing the Efficacy of Laser Treatment for Primary Teeth: A Systematic Review. Appl. Sci. 2024, 14, 1107. [Google Scholar] [CrossRef]
- Kiryk, J.; Kiryk, S.; Kensy, J.; Świenc, W.; Palka, B.; Zimoląg-Dydak, M.; Dobrzyński, W.; Matys, J.; Dobrzyński, M. Effectiveness of Laser-Assisted Teeth Bleaching: A Systematic Review. Appl. Sci. 2024, 14, 9219. [Google Scholar] [CrossRef]
- Piszko, P.J.; Piszko, A.; Kiryk, J.; Lubojański, A.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. The Influence of Fluoride Gels on the Physicochemical Properties of Tooth Tissues and Dental Materials—A Systematic Review. Gels 2024, 10, 98. [Google Scholar] [CrossRef] [PubMed]
- Struzik, N.; Kensy, J.; Piszko, P.J.; Kiryk, J.; Wiśniewska, K.; Kiryk, S.; Korjat, Ł.; Horodniczy, T.; Sobierajska, P.; Matys, J.; et al. Contamination in Bone Substitute Materials: A Systematic Review. Appl. Sci. 2024, 14, 8266. [Google Scholar] [CrossRef]
- Smołka, P.; Nelke, K.; Struzik, N.; Wiśniewska, K.; Kiryk, S.; Kensy, J.; Dobrzyński, W.; Kiryk, J.; Matys, J.; Dobrzyński, M. Discrepancies in Cephalometric Analysis Results between Orthodontists and Radiologists and Artificial Intelligence: A Systematic Review. Appl. Sci. 2024, 14, 4972. [Google Scholar] [CrossRef]
- Piszko, P.J.; Piszko, A.; Kiryk, S.; Kiryk, J.; Horodniczy, T.; Struzik, N.; Wiśniewska, K.; Matys, J.; Dobrzyński, M. Bone Regeneration Capabilities of Scaffolds Containing Chitosan and Nanometric Hydroxyapatite—Systematic Review Based on In Vivo Examinations. Biomimetics 2024, 9, 503. [Google Scholar] [CrossRef]
- Rygas, J.; Matys, J.; Wawrzyńska, M.; Szymonowicz, M.; Dobrzyński, M. The Use of Graphene Oxide in Orthodontics—A Systematic Review. J. Funct. Biomater. 2023, 14, 500. [Google Scholar] [CrossRef]
- Kowalski, J.; Rygas, J.; Homa, K.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. Antibacterial Activity of Endodontic Gutta-Percha—A Systematic Review. Appl. Sci. 2024, 14, 388. [Google Scholar] [CrossRef]
- Kensy, J.; Dobrzyński, M.; Wiench, R.; Grzech-Leśniak, K.; Matys, J. Fibroblasts Adhesion to Laser-Modified Titanium Surfaces—A Systematic Review. Materials 2021, 14, 7305. [Google Scholar] [CrossRef]
- Watson, P.F.; Petrie, A. Method Agreement Analysis: A Review of Correct Methodology. Theriogenology 2010, 73, 1167–1179. [Google Scholar] [CrossRef] [PubMed]
- Chapter 3: Systematic Reviews of Effectiveness. In JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2020.
- Viechtbauer, W. Conducting Meta-Analyses in R with the Metafor Package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- The Jamovi Project (2022). Jamovi. (Version 2.3) [Computer Software]. Available online: https://www.jamovi.org (accessed on 6 January 2025).
- R Core Team (2021). R: A Language and Environment for Statistical Computing. (Version 4.1) [Computer Software]. R Packages Retrieved from MRAN Snapshot 2022-01-01. Available online: https://cran.r-project.org (accessed on 6 January 2025).
- Gulec, A.; Goymen, M. Assessment of the Resin Infiltration and CPP-ACP Applications before Orthodontic Brackets Bonding. Dent. Mater. J. 2019, 38, 854–860. [Google Scholar] [CrossRef] [PubMed]
- Insee, K.; Boonyanitchayakul, N.; Temprasert, C.; Klaisiri, A. Shear Bond Strength of Orthodontic Brackets to Resin-Infiltrated Enamel. Eur. J. Gen. Dent. 2024. [Google Scholar] [CrossRef]
- Baka, Z.M.; Akin, M.; Ileri, Z.; Basciftci, F.A. Effects of Remineralization Procedures on Shear Bond Strengths of Brackets Bonded to Demineralized Enamel Surfaces with Self-Etch Systems. Angle Orthod. 2016, 86, 661–667. [Google Scholar] [CrossRef] [PubMed]
- Anicic, M.S.; Goracci, C.; Juloski, J.; Miletic, I.; Mestrovic, S. The Influence of Resin Infiltration Pretreatment on Orthodontic Bonding to Demineralized Human Enamel. Appl. Sci. 2020, 10, 3619. [Google Scholar] [CrossRef]
- Yousif AL-Mayali, A.M. Effect of Icon and Bond Type on Shear Bond Strength: An In Vitro Study. Int. J. Med. Res. Health Sci. 2017, 6, 58–66. [Google Scholar]
- Muhsin, A.; Al-Mayali, Y.; Nahidh, M.; Kadhim, H.A.; Fahad, A.H. Impact of Food Simulants Material on Orthodontic Bond Strength after Application of Caries Infiltrant Resin (In Vitro Study). Med.-Leg. Update 2020, 20, 979–984. [Google Scholar]
- Salama, R.I.; Fansa, H.A.; Taju, W.G. Comparing the Effect of Two Different Remineralizing Agents on Shear Bond Strength of Orthodontics Brackets. Int. J. Dent. Oral Sci. 2021, 8, 2134–2139. [Google Scholar] [CrossRef]
- Veli, I.; Akin, M.; Baka, Z.M.; Uysal, T. Effects of Different Pre-Treatment Methods on the Shear Bond Strength of Orthodontic Brackets to Demineralized Enamel. Acta Odontol. Scand. 2016, 74, 7–13. [Google Scholar] [CrossRef]
- Ekizer, A.; Zorba, Y.O.; Uysal, T.; Ayrikcil, S. Effects of Demineralizaton-Inhibition Procedures on the Bond Strength of Brackets Bonded to Demineralized Enamel Surface. Korean J. Orthod. 2012, 42, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Montasser, M.A.; Taha, M. Effect of Enamel Protective Agents on Shear Bond Strength of Orthodontic Brackets. Prog. Orthod. 2014, 15, 34. [Google Scholar] [CrossRef]
- Costenoble, A.; Vennat, E.; Attal, J.P.; Dursun, E. Bond Strength and Interfacial Morphology of Orthodontic Brackets Bonded to Eroded Enamel Treated with Calcium Silicate-Sodium Phosphate Salts or Resin Infiltration. Angle Orthod. 2016, 86, 909–916. [Google Scholar] [CrossRef]
- Nimbalkar, S.; Lim, L.H.; Lee, Z.T.; Lim, K.H.; Sia, S.Y. Efficacy of Three Enamel Protecting Agents on Shear Bond Strength of Orthodontic Brackets Bonded to Demineralised Enamel with Conventional Adhesive. J. Clin. Diagn. Res. 2021, 15, 18. [Google Scholar] [CrossRef]
- Hammad, S.M.; Enan, E.T. In Vivo Effects of Two Acidic Soft Drinks on Shear Bond Strength of Metal Orthodontic Brackets with and without Resin Infiltration Treatment. Angle Orthod. 2013, 83, 648–652. [Google Scholar] [CrossRef]
- Naidu, E.; Stawarczyk, B.; Tawakoli, P.N.; Attin, R.; Attin, T.; Wiegand, A. Shear Bond Strength of Orthodontic Resins after Caries Infiltrant Preconditioning. Angle Orthod. 2013, 83, 306–312. [Google Scholar] [CrossRef]
- Attin, R.; Stawarczyk, B.; Keçik, D.; Knösel, M.; Wiechmann, D.; Attin, T. Shear Bond Strength of Brackets to Demineralize Enamel after Different Pretreatment Methods. Angle Orthod. 2012, 82, 56–61. [Google Scholar] [CrossRef]
- Vianna, J.S.; Marquezan, M.; Lau, T.C.L.; Anna, E.F.S. Bonding Brackets on White Spot Lesions Pretreated by Means of Two Methods. Dent. Press J. Orthod. 2016, 21, 39–44. [Google Scholar] [CrossRef]
- Triwardhani, A.; Budipramana, M.; Sjamsudin, J. Effect of Different White-Spot Lesion Treatment on Orthodontic Shear Strength and Enamel Morphology: In Vitro Study. J. Int. Oral Health 2020, 12, 120–128. [Google Scholar] [CrossRef]
- Mews, L.; Kern, M.; Ciesielski, R.; Fischer-Brandies, H.; Koos, B. Shear Bond Strength of Orthodontic Brackets to Enamel after Application of a Caries Infiltrant. Angle Orthod. 2015, 85, 645–650. [Google Scholar] [CrossRef]
- Yetkiner, E.; Özcan, M.; Wegehaupt, F.J. Effect of a Low-Viscosity Adhesive Resin on the Adhesion of Metal Brackets to Enamel Etched with Hydrochloric or Phosphoric Acid Combined with Conventional Adhesives. Artic. J. Adhes. Dent. 2013, 15, 575–581. [Google Scholar] [CrossRef]
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2016; Volume 35. [Google Scholar]
- Demirsoy, K.K.; Buyuk, S.K.; Abay, F.; Simsek, H.; Ozcelik, E. A Comparison of Bond Strength and Adhesive Remnant Index of 3D-Printed and Metal Orthodontic Brackets Attached Using Different Adhesives. Australas. Orthod. J. 2023, 39, 32–39. [Google Scholar] [CrossRef]
- da Rocha, J.M.; Gravina, M.A.; Campos, M.J.; Quintão, C.C.A.; Elias, C.N.; Vitral, R.W.F. Shear Bond Resistance and Enamel Surface Comparison after the Bonding and Debonding of Ceramic and Metallic Brackets. Dent. Press J. Orthod. 2014, 19, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Henkin, F. de S.; de Macêdo, É. de O.D.; Santos, K. da S.; Schwarzbach, M.; Samuel, S.M.W.; Mundstock, K.S. In Vitro Analysis of Shear Bond Strength and Adhesive Remnant Index of Different Metal Brackets. Dent. Press J. Orthod. 2016, 21, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Cervantes-Ganoza, L.; Castro-Ramirez, L.; Aroste-Andía, R.; Huamani-Echaccaya, J.; Ladera-Castañeda, M.; Cayo-Rojas, C. Comparison of the Adhesive Remnant Index and Shear Bond Strength of Different Metal Bracket Bases on Artificially Aged Human Teeth: An In Vitro Study. J. Int. Soc. Prev. Community Dent. 2024, 14, 396–404. [Google Scholar] [CrossRef]
- Nawrocka, A.; Nowak, J.; Sauro, S.; Hardan, L.; Bourgi, R.; Lukomska-Szymanska, M. Shear Bond Strength of Metal and Ceramic Brackets Depending on Etching Protocol in Direct Bonding Technique. Materials 2023, 16, 6697. [Google Scholar] [CrossRef]
- Pont, H.B.; Özcan, M.; Bagis, B.; Ren, Y. Loss of Surface Enamel after Bracket Debonding: An in-Vivo and Ex-Vivo Evaluation. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 387.e1–387.e9. [Google Scholar] [CrossRef]
- Kiryk, J.; Matys, J.; Grzech-Leśniak, K.; Dominiak, M.; Małecka, M.; Kuropka, P.; Wiglusz, R.J.; Dobrzyński, M. Sem Evaluation of Tooth Surface after a Composite Filling Removal Using Er:Yag Laser, Drills with and without Curettes, and Optional Edta or Naocl Conditioning. Materials 2021, 14, 4469. [Google Scholar] [CrossRef]
- Lishna, K.T.; Shaloob, M.; Antony, V.; Roshan, G.; Parayaruthottam, P.; Mohammed, N.V.P.; Raheesh, M. Assessment of Enamel Surface Using Scanning Electron Microscope After Debonding Conventional and Self-Ligating Metal and Ceramic Brackets: An In Vitro Study. J. Int. Oral Health 2024, 16, 214–222. [Google Scholar] [CrossRef]
- Bakhadher, W.; Halawany, H.; Talic, N.; Abraham, N.; Jacob, V. Factors Affecting the Shear Bond Strength of Orthodontic Brackets—A Review of In Vitro Studies. Acta Medica (Hradec Králové)/Univ. Carol. Fac. Medica Hradec Králové 2015, 58, 43–48. [Google Scholar] [CrossRef]
- Klocke, A.; Kahl-Nieke, B. Effect of Debonding Force Direction on Orthodontic Shear Bond Strength. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 261–265. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).