Abstract
The reliability of health monitoring technologies has become increasingly critical as Ambient Intelligence (AmI) becomes integrated into healthcare. However, a significant gap remains in systematically evaluating reliability, particularly in resource-constrained environments. This study addresses this gap by introducing a comprehensive framework specifically designed to evaluate the reliability of AmI-based health monitoring systems. The proposed framework combines robust simulation-based techniques, including reliability block diagrams (RBDs) and Monte Carlo Markov Chain (MCMC), to evaluate system robustness, data integrity, and adaptability. Validation was performed using real-world continuous glucose monitoring (CGM) and heart rate monitoring (HRM) systems in elderly care. The results demonstrate that the framework successfully identifies critical vulnerabilities, such as rapid initial system degradation and notable connectivity disruptions, and effectively guides targeted interventions that significantly enhance overall system reliability and user trust. The findings contribute actionable insights for practitioners, developers, and policymakers, laying a robust foundation for further advancements in explainable AI, proactive reliability management, and broader applications of AmI technologies in healthcare.
1. Introduction
The rapid evolution of health monitoring technologies is reshaping healthcare by enabling proactive, continuous, and context-aware support across diverse populations [1,2,3]. Ambient Intelligence (AmI), with its seamless integration of sensing, reasoning, and actuation in everyday environments, has become a foundational paradigm for next-generation health monitoring and assistive technologies (ATs) [4,5]. These technologies promise to enhance patient outcomes, optimize resource allocation, and support aging-in-place strategies for elderly and vulnerable populations [6,7,8].
Despite these benefits, the reliability of AmI-based health monitoring systems remains a persistent concern [9,10]. Reliability in this context refers to a system’s consistent ability to deliver accurate, timely, and trustworthy monitoring under diverse operational conditions—including sensor degradation, data transmission errors, and unpredictable user contexts [9]. Failures in reliability can compromise patient safety, disrupt clinical workflows, and reduce user trust, particularly in remote or elderly care settings.
A notable gap in the literature is the absence of integrated frameworks that enable the systematic evaluation of reliability across heterogeneous, multi-layered AmI environments—especially those deployed in resource-constrained settings. While traditional reliability engineering methods such as reliability block diagrams (RBDs), Markov models, and Monte Carlo simulations (MCSs) have shown success in engineering domains [11,12], their direct application to AmI systems remains challenging. The inherent complexity of AmI—stemming from the diversity of sensors, contextual variability, and real-time operational requirements—demands evaluation frameworks that are both mathematically rigorous and contextually adaptive.
This paper addresses these challenges by proposing a comprehensive and modular framework for evaluating the reliability of AmI-based health monitoring systems. The framework integrates quantitative and qualitative reliability assessment approaches, incorporating probabilistic modeling, simulation, and human-centric evaluations. Its applicability is demonstrated through two real-world case studies: continuous glucose monitoring (CGM) and heart rate monitoring (HRM) in elderly care environments.
The specific contributions of this study are as follows:
- A structured review of reliability evaluation techniques relevant to AmI health monitoring systems.
- A modular framework that integrates RBD, Monte Carlo Markov Chain (MCMC) simulations, and human-contextual factors for comprehensive reliability assessment.
- Validation of the framework through empirical case studies in continuous glucose monitoring and heart rate monitoring for elderly care.
- Discussion of the framework’s practical implications, limitations, and directions for future research in explainable and trustworthy AmI systems.
The remainder of this paper is structured as follows: Section 2 reviews related work on reliability assessment methods in AmI-based health systems. Section 3 presents the mathematical foundations and case study setup. Section 4 details the proposed framework and its architecture. Section 5 discusses the experimental validation and findings. Section 6 offers a critical analysis of the framework’s performance and applicability. Finally, Section 7 concludes the paper and outlines future research directions.
2. Related Work
AmI integrates sensor networks, computational intelligence, and context-aware computing to support adaptive and personalized services in various domains, including healthcare [13,14,15]. Early foundational work by Acampora et al. [16] provided a comprehensive overview of the potential of AmI for healthcare and assisted living environments, highlighting its suitability for elderly care and chronic disease management. Since then, several studies have extended this vision to include real-time monitoring, context inference, and adaptive service delivery in health settings.
In the context of health monitoring, AmI-enabled assistive technologies (ATs) such as wearable devices, smart home sensors, and IoT-based applications are being increasingly employed to capture physiological and behavioral data [9]. These systems offer advantages in continuous monitoring and personalized care. However, ensuring the reliability of such systems in dynamic and resource-constrained environments remains a significant challenge [17]. The reliability of health monitoring systems refers not only to the accuracy and availability of individual sensors but also to the dependability of the entire system in capturing, processing, and delivering data without interruption or distortion [18].
Classical reliability evaluation approaches such as Fault Tree Analysis (FTA) and RBD have been used extensively in systems engineering [11,19]. These methods allow structured modeling of failure propagation paths and component-level dependencies. However, their applicability to complex, real-time AmI systems is limited by their static assumptions and lack of temporal dynamics.
To address this limitation, stochastic methods like Markov Chains and MCSs have been employed to model system behavior under uncertainty. For example, Liu et al. [20] proposed a semi-Markov process model for wearable devices, capturing failure transitions in health telemetry systems. Almaiah et al. [21] developed a novel context-aware probabilistic modeling scheme for smart medical environments using Bayesian networks. Nevertheless, these methods often require extensive historical data and computational overhead, which may not be feasible in real-world deployments.
Recent research has explored the use of Artificial Intelligence techniques for reliability prediction. Deep learning models, such as Convolutional Neural Networks (CNNs) and Long Short-Term Memory (LSTM) networks, have demonstrated effectiveness in detecting anomalies and forecasting component failures from time-series sensor data [22,23,24]. Kibalya et al. [25] developed a reliability-aware deep reinforcement learning approach for intelligent health monitoring systems, showing improved responsiveness in uncertain contexts. However, these models are often black-box in nature, lacking interpretability, which poses a challenge in safety-critical healthcare environments.
Fuzzy logic and hybrid AI models have been introduced to address uncertainties in sensor readings and patient contexts [26]. For instance, Kumar and Dhulipala [27] developed a fuzzy reliability model for wearable devices operating in uncontrolled settings. Saranya and Fatima [28] combined fuzzy inference with IoT sensor fusion to increase context-awareness in ambient health monitoring. Such hybrid approaches offer flexibility but often suffer from scalability issues when applied to large-scale systems.
In parallel, the rise of Explainable AI (XAI) and Trustworthy AI frameworks has prompted the inclusion of interpretability and human-in-the-loop mechanisms in reliability modeling [29]. This is especially important in clinical environments where practitioners require not only predictions but also rationales behind system decisions. Additionally, the emergence of blockchain technologies has opened up new directions for reliability auditing, data provenance, and decentralized trust management in healthcare systems [30,31,32]. These technologies enable tamper-resistant logging and transparent validation of device behaviors, complementing traditional reliability assessment frameworks.
Despite these advances, a cohesive and adaptable framework that integrates classical, probabilistic, and intelligent reliability methods for AmI health monitoring remains lacking. Particularly in low-resource settings, existing models do not sufficiently account for constraints such as intermittent connectivity, energy limitations, and diverse user profiles. This paper aims to fill that gap by proposing a reliability evaluation framework that is both theoretically grounded and practically viable across heterogeneous ambient intelligence environments.
3. Materials and Methods
This section outlines the modeling techniques, mathematical formulations, datasets, and evaluation metrics used to assess the reliability of health monitoring technologies within AmI environments. The reliability modeling process integrates three key methodologies: RBDs, Continuous-Time Markov Chains (CTMCs), and MCSs. These techniques are applied to real-world case studies—CGM and HRM—used in elderly care.
3.1. Reliability Block Diagrams
RBDs provide a structured representation of system components and their functional dependencies. Each component is modeled as a block in a network, connected in series, parallel, or hybrid configurations [33]. For components in series, the system reliability is given by
where is the reliability function of component i at time t. Here, i indexes individual system components (e.g., sensors, processors, power units), and n denotes the total number of components represented in the RBD model. For components in parallel,
RBDs are used to structure subsystems such as power units, connectivity modules, and sensor arrays in both CGM and HRM devices.
3.2. Continuous-Time Markov Chains
CTMCs are employed to model the stochastic transitions between operational states of system components, such as normal, degraded, and failed [34,35]. A CTMC is characterized by a set of states S and a transition rate matrix Q. The probability of transitioning from state i to j at time t is governed by the Kolmogorov forward equation:
where is the transition rate from state k to state j. Transition rates were derived from empirical logs and device specifications.
3.3. Monte Carlo Simulation
MCSs are used to estimate system-level reliability under uncertainty [36]. For each of N simulation trials, component lifetimes were randomly sampled from exponential or Weibull distributions, and overall system reliability was estimated as
where if the system is operational in the k-th simulation at time t and 0 otherwise [36,37].
3.4. Case Study Descriptions
- Continuous glucose monitoring: The CGM system includes a subcutaneous glucose sensor, a Bluetooth low-energy (BLE) transmitter, and a mobile application interface. Reliability challenges included sensor drift, packet loss, and application crashes. Empirical data were drawn from pilot trials in elderly care facilities and device manufacturer specifications.
- Heart rate monitoring: The HRM system comprises wearable ECG sensors, signal preprocessing modules, and context-aware analytics. Failure risks include battery depletion, motion-induced artifacts, and connectivity interruptions. Failure rates were calibrated using benchmark datasets and pilot performance logs.
In practice, the reliability of CGM and HRM cannot be considered in isolation, as both systems often operate concurrently and share dependencies such as wireless connectivity, battery power, and user compliance. To account for this, the framework incorporates joint probability modeling and dependency assumptions that capture correlated failure behavior. For example, power depletion or network loss can simultaneously degrade both CGM and HRM performance, while user non-compliance (e.g., improper device placement) may introduce correlated error modes. These interdependencies are reflected in the layered RBD and Markov structure of the framework, ensuring system-level reliability is evaluated holistically rather than as the sum of independent subsystems.
3.5. Evaluation Metrics
The following quantitative metrics will be used to assess the reliability of AmI-based health monitoring systems within the proposed framework. These metrics provide formal mechanisms for quantifying operational performance and identifying failure trends under varying conditions.
- Reliability : This refers to the probability that a system performs its intended function without failure over the interval . It serves as the foundational metric in reliability analysis and is modeled as a function of time [38,39]:where T is the random variable representing time to failure.
- Mean time to failure (MTTF): This metric quantifies the expected operating time before a system experiences its first failure [40]. For non-repairable systems, it is computed as the integral of the reliability function:MTTF is particularly important in understanding how long the system can be relied upon without interruption [40].
- Failure rate : This represents the instantaneous failure rate at time t, indicating how quickly the system is likely to fail [38,41]. It is mathematically defined asA higher failure rate suggests greater unreliability, especially in systems with aging or degradation behaviors [38].
- Availability : Availability extends the concept of reliability by accounting for both failure and repair cycles, making it especially relevant for health monitoring systems where devices can be reset, recalibrated, or replaced during operation. It is formally defined as the probability that the system is in a functioning state at a given time t. In steady-state analysis, availability is commonly expressed aswhere MTTR is the mean time to repair. Unlike , which declines monotonically with time, captures the balance between failure frequency and repair efficiency. For example, in CGM and HRM systems, even if sensors fail intermittently, rapid recalibration or battery replacement can restore operational status, leading to high availability despite lower reliability. This distinction ensures that the metric reflects practical system usability in real-world healthcare deployments [42].
Meanwhile, in this study all reliability models will be implemented using MATLAB R2025a and Python 3.11, specifically leveraging libraries such as NumPy and SciPy. Monte Carlo simulations will be run with iterations to ensure statistical robustness. Failure distributions and model parameters will be fitted using Maximum Likelihood Estimation (MLE) based on empirical or benchmark data where available.
4. Proposed Methodology
Building upon the foundational modeling approaches described in the previous section, this part of the study presents the proposed framework for context-aware reliability evaluation in AmI-based health monitoring systems. The methodology integrates structural system modeling, probabilistic reliability estimation, and dynamic user-context adaptation. It is designed to offer a unified and scalable mechanism for assessing and enhancing reliability in real-world healthcare deployments.
The proposed framework adopts a modular, layered architecture that combines classical reliability techniques—such as RBD and CTMC—with context-sensitive evaluation and user-centric adaptations. This integration facilitates both quantitative computation and real-time reliability adjustment, especially in dynamic and resource-constrained environments typical of AmI healthcare settings.
4.1. Framework Architecture
The architectural foundation of the proposed methodology is visualized in Figure 1. It outlines the core relationships between AmI-based assistive technologies (AmI-ATs), their use-case scenarios, and the underlying system components (hardware, software, power, connectivity, and human factor) that impact reliability dimensions such as integrity, dependability, and trustworthiness.
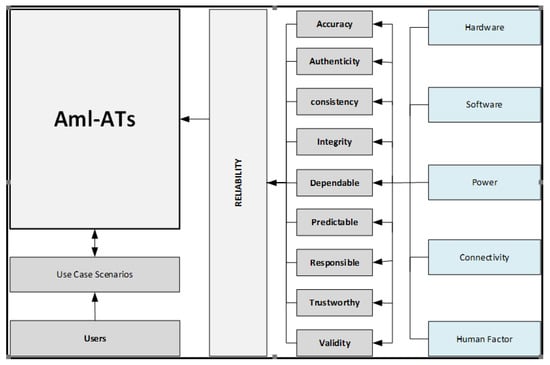
Figure 1.
High-level architecture of the proposed AmI-AT reliability framework. The diagram illustrates interdependencies between core subsystems—hardware, software, connectivity, and power—and their influence on key reliability attributes. User context and application-specific constraints also inform failure modeling.
The architecture is composed of four primary layers:
- Input layer: Captures modeling data from sensor sources, user behavior logs, and operational scenarios, forming the basis for tailored reliability evaluations.
- System components layer: Decomposes the system into its core technical elements—hardware, software, power supply, and connectivity—for individual subsystem modeling using RBD and CTMC techniques.
- Contextual layer: Adjusts reliability scores using environmental and human factors such as motion interference, ambient conditions, or user non-compliance.
- AmI-AT management layer: Combines advanced modeling tools and assessment criteria to compute system-level reliability:
- −
- Reliability estimation module: Implements MCMC simulations, RBD modeling, and quantitative metrics.
- −
- Assessment module: Integrates both quantitative (e.g., MTTF, availability) and qualitative dimensions (e.g., trust, explainability).
4.2. Implementation Process
The procedural implementation of the framework is shown in Figure 2. Each subsystem (connectivity, software, hardware, and power) is independently modeled to compute its reliability function. Human interaction data modifies these functions through context-aware weighting. The aggregated output is a global reliability function for the full AmI-AT system.
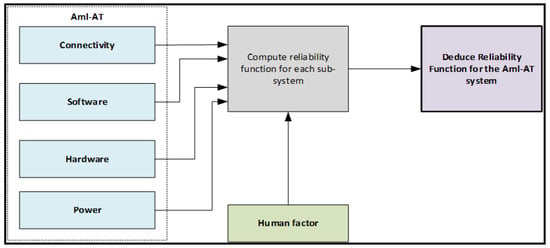
Figure 2.
Implementation workflow of the AmI-AT reliability framework. Each subsystem is modeled independently using empirical failure data and evaluated through RBD, CTMC, and MCMC techniques. The outputs are integrated to derive a global reliability score.
Reliability scores are computed based on observed or inferred failure rates and modeled using the techniques described in the Section 3. This modular workflow ensures that any subsystem (e.g., power module) can be re-evaluated independently without recalibrating the entire model.
4.3. Human Factor Modeling and Quantification
Human factors are explicitly modeled within the contextual layer because device misuse, non-compliance, and improper handling represent critical determinants of real-world reliability. These are incorporated through context-aware weighting of subsystem reliabilities, where baseline reliability functions are adjusted by compliance-derived factors. For example, missed sensor calibrations, delayed battery charging, or improper device placement reduce effective reliability by scaling downward.
Data for quantifying human factors are drawn from multiple sources, including compliance logs (e.g., calibration frequency, charging history), user behavior logs (e.g., device usage interruptions), and surveys or expert evaluations. These inputs enable dynamic adjustment of reliability estimates, allowing the framework to capture variability introduced by human behavior. Future integration with established Human Reliability Analysis (HRA) techniques and cognitive error databases will enhance precision by systematically classifying and quantifying user-driven errors.
In practical terms, this means that two devices with identical hardware and software reliability may diverge in effective reliability depending on how consistently they are used, calibrated, and maintained by patients or caregivers. By embedding this modeling, the framework ensures that technical reliability measures are realistically grounded in human interaction and operational context.
4.4. Layered Framework Integration
Figure 3 presents the full layered configuration of the AmI-AT reliability framework, reinforcing its adaptability and clarity. It visually delineates how inputs, components, and context interact to inform reliability modeling and system-level assessment.
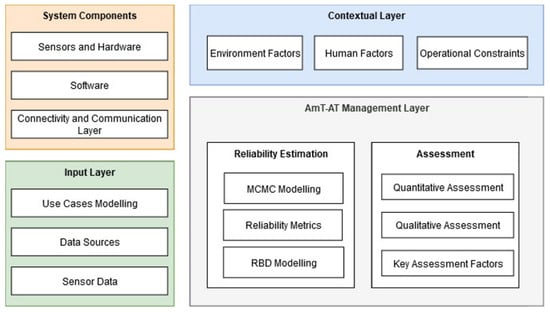
Figure 3.
Layered design of the full AmI-AT reliability framework. The input layer gathers real-time sensor data and contextual inputs; system component reliability is evaluated using classical techniques; contextual influences are modeled separately and aggregated; and the AmI-AT management layer combines outputs for reliability estimation and qualitative assessment.
The use of layering ensures clear separation of functions while maintaining interoperability across dimensions. For example, a change in environmental conditions (e.g., temperature or humidity) triggers adjustments in the contextual layer that cascade into the reliability estimation engine. This enables real-time or periodic adaptation of reliability scores.
It is important to clarify that the framework does not aim to directly predict or model disease prognosis, which requires clinical risk modeling. Instead, it evaluates the reliability of the technological ecosystem (sensors, connectivity, power, software, and human interaction). Disease-related interactions are indirectly reflected through contextual and human factor modules—for example, frequent calibration in diabetes management (CGM) increases the probability of user error, while irregular HRM usage during cardiac rehabilitation may amplify reliability risks.
4.5. System Adaptation and Feedback Mechanisms
A distinguishing feature of this methodology is its adaptability to operational change. As real-time inputs or updated failure data are ingested, the framework dynamically recalculates subsystem reliability. Combined with contextual awareness, this allows the system to respond to evolving user conditions, aging components, or infrastructure variability.
Overall, this layered and modular methodology offers significant improvements over traditional reliability models by integrating structural modeling, probabilistic dynamics, and behavioral context into a single, unified reliability evaluation framework for AmI-based health monitoring systems.
5. Experimental Results
To validate the applicability and effectiveness of the proposed AmI-based reliability framework, extensive experimental analyses were conducted using datasets from real-world CGM and HRM systems primarily used in elderly care settings. The analyses employed RBD, MCMC simulations, and advanced modeling techniques, outlined previously.
The state transition heatmap derived from empirical training data (Figure 4) highlights substantial stability within the normal operational state (99%), whereas both the degraded and failed states exhibit notable internal persistence (74%). In this context, the state transition probabilities were empirically estimated from annotated CGM and HRM device logs, where transitions denote the observed likelihood of moving between operational states (normal, degraded, failed, recovered). Persistence values (e.g., 99% in normal) correspond to self-transition probabilities, while cross-state values (e.g., 24% from degraded to recovered) represent recovery events documented in the dataset. These probabilities therefore reflect empirical likelihoods observed over the monitoring period rather than theoretical assumptions. For reproducibility, the CGM dataset spanned six months of elderly care monitoring across 45 subjects, while the HRM dataset included three months of wearable ECG monitoring across 30 subjects, amounting to approximately 1.2 million recorded device–state observations in total.
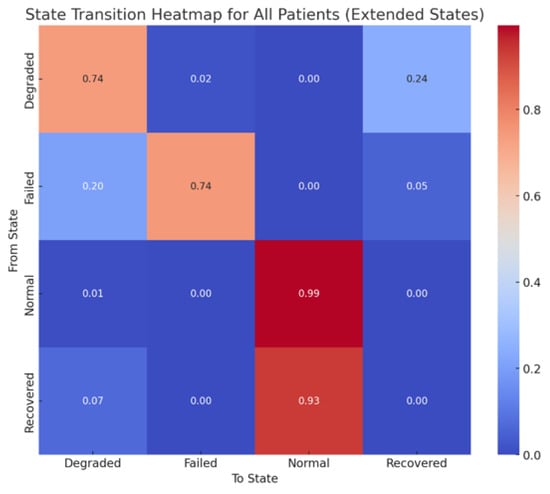
Figure 4.
State transition matrix generated from training data. Values represent empirically estimated transition probabilities between operational states of CGM and HRM systems, based on device logs collected in elderly care deployments.
Further investigation into cumulative system failures for CGM devices (Figure 5) demonstrates rapid degradation during early operational phases, with approximately 500 failures occurring within the initial week. These early failures primarily stem from calibration instability in CGM sensors, where sensor drift and packet loss during initial deployment often cause premature device errors. This rapid accumulation of failures underscores significant vulnerabilities early in system deployment, highlighting the critical need for preventive maintenance strategies and robust reliability enhancements at early stages.
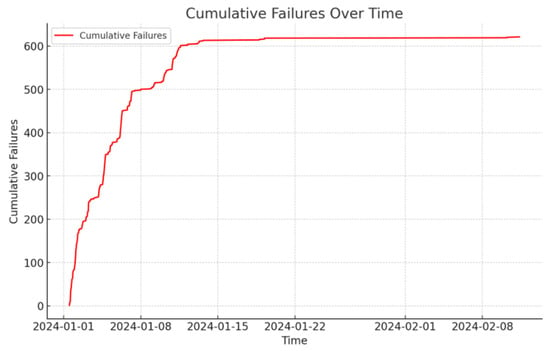
Figure 5.
Cumulative failures for CGM devices. Rapid failure accumulation within the first week reflects calibration instability and sensor drift during initial deployment.
Analysis of overall system reliability for HRM devices over time (Figure 6) reveals near-perfect initial performance, followed by a pronounced reliability drop around one month post-deployment. This decline is attributed to HRM device susceptibility to motion artifacts, battery depletion, and occasional connectivity interruptions in continuous ECG monitoring. This sudden decline emphasizes the importance of continuous monitoring and proactive maintenance measures, incorporating redundancy and predictive maintenance to sustain reliability and prevent sudden operational disruptions.
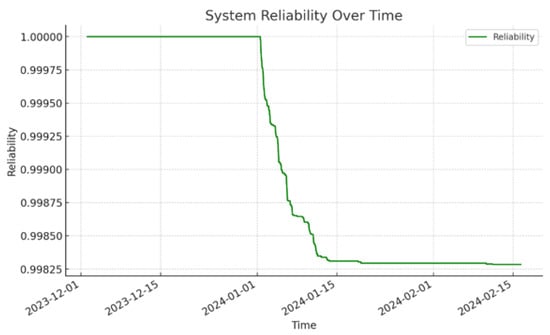
Figure 6.
System reliability for HRM devices. Reliability remains high during initial operation but declines sharply after one month due to motion artifacts, battery depletion, and connectivity instability.
A comparative analysis of improved versus degraded systems (Figure 7) illustrates the clear efficacy of reliability interventions. Systems incorporating redundancy and predictive maintenance strategies exhibit consistently higher reliability levels compared to degraded systems without such enhancements, underscoring the tangible benefits of systematic reliability improvements.
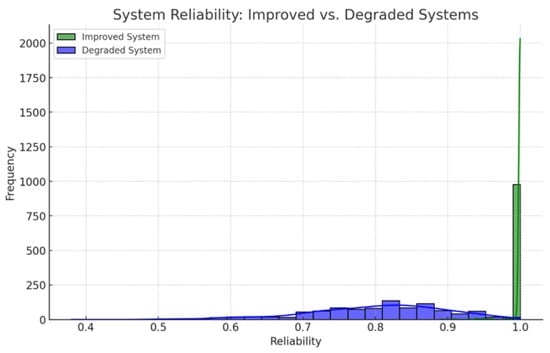
Figure 7.
System reliability: improved vs. degraded systems.
The Monte Carlo simulation results presented in Figure 8 display the distribution of anomalies detected across simulation trials, indicating that most scenarios exhibit a manageable number of anomalies (typically between zero to three). These outcomes affirm the framework’s capability to effectively predict and isolate high-risk operational scenarios, allowing for targeted management interventions.
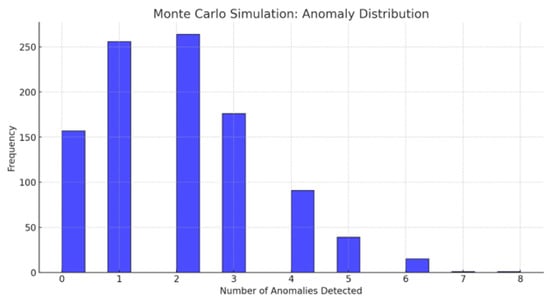
Figure 8.
Monte Carlo simulation: anomaly distribution.
Connectivity reliability analysis (Figure 9) shows intermittent yet regular connectivity disruptions, underscoring critical vulnerabilities within the communication infrastructure. These connectivity patterns emphasize the necessity of strategic enhancements in network infrastructure and redundant communication channels to ensure robust and continuous data transmission, which is critical for reliable health monitoring operations.
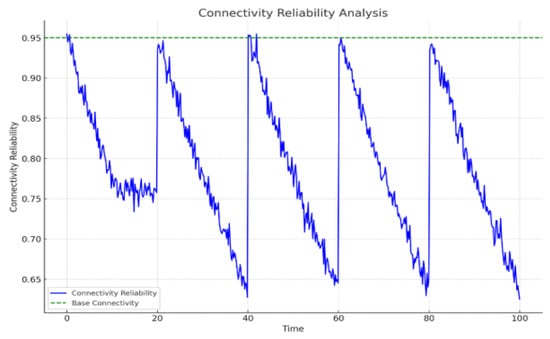
Figure 9.
Regular connectivity analysis.
Finally, reliability assessments at the sensor level (Figure 10) reveal distinct performance trajectories across different HRM sensors, highlighting accelerated reliability deterioration for sensors such as accelerometers and gyroscopes. These sensor-specific findings emphasize the importance of targeted component-level interventions and systematic implementation of sensor upgrades or redundancy strategies to maintain optimal overall system performance.
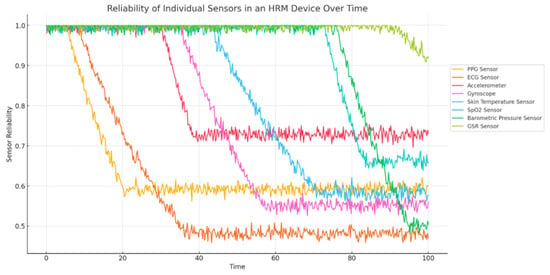
Figure 10.
Reliability of individual sensors in HRM device over time.
In summary, the results from these experimental analyses provide robust evidence supporting the proposed AmI-AT reliability framework. They demonstrate its effectiveness in capturing critical system dynamics, identifying strategic intervention points, and highlighting areas of vulnerability. The analyses emphasize the necessity for proactive reliability management approaches, early intervention strategies, and robust communication infrastructure enhancements, collectively contributing to the sustained reliability and effectiveness of AmI-based health monitoring systems.
6. Discussion
The proposed AmI-AT reliability framework advances the evaluation of health monitoring systems, particularly in elderly care. Unlike models that focus narrowly on isolated components, this framework integrates structural, probabilistic, and contextual elements, reflecting how reliability is shaped by hardware, software, environment, and user behavior.
Its layered design supports subsystem-level evaluation while enabling system-wide synthesis. By incorporating user context, the framework ensures that reliability assessments are not only technical but also human-centered. The use of RBD and MCMC techniques provides a rigorous mathematical basis for uncertainty analysis, supporting both short-term interventions and long-term reliability planning.
The rapid accumulation of failures in early operation (Figure 5 and Figure 6) reflects the “infant mortality” phenomenon, driven by factors such as sensor initialization faults, calibration drift, software bugs, and transient network instability. Burn-in testing, scheduled recalibration, and proactive fault detection are effective strategies to mitigate these start-up vulnerabilities.
Periodic fluctuations in connectivity reliability (Figure 9) can be attributed to predictable operational events (e.g., charging cycles, scheduled reboots, firmware updates) and user-related behaviors (e.g., movement across coverage zones or device removal). Wireless interference may further accentuate these disruptions. Design strategies such as staggered charging, predictive handoff, and adaptive connectivity management can reduce the impact of such recurring events.
Limitations remain. The case studies focused on CGM and HRM, potentially limiting generalizability, and the framework assumes stationary transition probabilities and simplified sensor failure distributions. Addressing these gaps will require dynamic modeling, predictive analytics, and uncertainty-aware simulations to better capture the variability of real-world deployments.
7. Conclusions and Future Work
This paper presented a modular framework for evaluating the reliability of AmI-based health monitoring systems. Grounded in classical reliability engineering and modern probabilistic modeling, the framework supports systematic analysis across sensors, software, connectivity, and user interaction. Validation through CGM and HRM case studies demonstrated its effectiveness in identifying failure points, forecasting reliability trajectories, and supporting targeted improvements.
Several directions emerge for future work. These include extending validation to new domains such as mental health, pediatric care, and post-operative monitoring; enabling real-time reliability tracking and dynamic model reconfiguration; and integrating hybrid AI with adaptive learning for predictive accuracy. Explicitly linking reliability outputs with disease-specific prognosis models—such as connecting CGM traces to hypoglycemia risk or HRM readings to arrhythmia detection—would bridge technical reliability with clinical outcomes.
Future refinements should also address current modeling assumptions by (i) incorporating dynamic, non-stationary transition probabilities, (ii) using machine learning to capture evolving failure patterns, and (iii) employing robust simulation techniques under uncertainty (e.g., Latin Hypercube sampling or Bayesian Monte Carlo). These advances would improve the realism and predictive power of reliability assessment.
As Ambient Intelligence evolves, ensuring reliability will remain essential for patient safety, clinical efficacy, and user trust. The proposed framework lays a scalable foundation for advancing both research and practice in dependable digital health technologies.
Author Contributions
Conceptualization, M.S.S. and N.J.; methodology, M.S.S.; software, M.S.S.; validation, M.S.S., N.J. and K.S.; formal analysis, M.S.S.; investigation, M.S.S.; resources, M.S.S.; data curation, M.S.S.; writing—original draft preparation, M.S.S. and I.D.M.; writing—review and editing, I.D.M. and N.J.; visualization, M.S.S.; supervision, N.J. and K.S.; project administration, N.J. and K.S.; funding acquisition, N.J. and K.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original data presented in the study are openly available in Kaggle at https://www.kaggle.com/datasets/avibagul80/time-series-cgm-dataset and https://www.kaggle.com/datasets/ahmadsaeed1007/heart-rate-time-series-mitbih-database (accessed on 1 June 2025).
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI | Artificial Intelligence |
| AIoT | Artificial Intelligence of Things |
| AmI | Ambient Intelligence |
| AT | Assistive Technology |
| BLE | Bluetooth Low Energy |
| CGM | Continuous Glucose Monitoring |
| CTMC | Continuous-Time Markov Chain |
| ECG | Electrocardiogram |
| FTA | Fault Tree Analysis |
| HRM | Heart Rate Monitoring |
| IoT | Internet of Things |
| MCMC | Monte Carlo Markov Chain |
| MCS | Monte Carlo Simulation |
| RBD | Reliability Block Diagram |
| XAI | Explainable Artificial Intelligence |
References
- Bollineni, C.; Sharma, M.; Hazra, A.; Kumari, P.; Manipriya, S.; Tomar, A. IoT for Next-Generation Smart Healthcare: A Comprehensive Survey. IEEE Internet Things J. 2025, 12, 32616–32639. [Google Scholar] [CrossRef]
- Geetha, S.; Karthikeyan, P.; Yughesh, N.; Prasanth, D.; Vishva, V. Context-Aware Remote Patient Monitoring System with IoT and Digital Security. In Proceedings of the 2024 International Conference on System, Computation, Automation and Networking (ICSCAN), Puducherry, India, 27–28 December 2024; pp. 1–6. [Google Scholar]
- Ianculescu, M.; Constantin, V.Ș.; Gușatu, A.M.; Petrache, M.C.; Mihăescu, A.G.; Bica, O.; Alexandru, A. Enhancing Connected Health Ecosystems Through IoT-Enabled Monitoring Technologies: A Case Study of the Monit4Healthy System. Sensors 2025, 25, 2292. [Google Scholar] [CrossRef] [PubMed]
- Attallah, O.; Al-Kabbany, A.; Zaghlool, S.B.; Kholief, M. Immersive technology and ambient intelligence for assistive living, medical, and healthcare solutions. Front. Hum. Neurosci. 2024, 18, 1376959. [Google Scholar] [CrossRef]
- Samanta, S.; Mitra, A.; Mishra, S.; Parvathaneni, N.S. Ambient Healthcare: A New Paradigm in Medical Zone. In Enabling Person-Centric Healthcare Using Ambient Assistive Technology: Personalized and Patient-Centric Healthcare Services in AAT; Springer: Cham, Switzerland, 2023; pp. 247–267. [Google Scholar]
- Hu, M.; Han, S.; Ghorbany, S.; Zhang, K. Healthy Aging in Place with the Aid of Smart Technologies: A Systematic Review. Encyclopedia 2024, 4, 1918–1932. [Google Scholar] [CrossRef]
- Jamshidi, S.; Hashemi, S. The Scientific Landscape of the Aging-in-Place Literature: A Bibliometric Analysis. J. Ageing Longev. 2024, 4, 417–432. [Google Scholar] [CrossRef]
- Vrančić, A.; Zadravec, H.; Orehovački, T. The role of smart homes in providing care for older adults: A systematic literature review from 2010 to 2023. Smart Cities 2024, 7, 1502–1550. [Google Scholar] [CrossRef]
- Sarkar, M.; Lee, T.H.; Sahoo, P.K. Smart healthcare: Exploring the internet of medical things with ambient intelligence. Electronics 2024, 13, 2309. [Google Scholar] [CrossRef]
- Jaber, A.S.; Idrees, A.K. Wireless body sensor networks: Applications, challenges, patient monitoring, Decision making, and machine learning in medical applications. In AI and IoT for Sustainable Development in Emerging Countries: Challenges and Opportunities; Springer: Cham, Switzerland, 2022; pp. 417–437. [Google Scholar]
- Jakkula, B.; Mandela, G.R.; Ch SN, M. Reliability block diagram (RBD) and fault tree analysis (FTA) approaches for estimation of system reliability and availability—A case study. Int. J. Qual. Reliab. Manag. 2021, 38, 682–703. [Google Scholar] [CrossRef]
- Lazarova-Molnar, S.; Friederich, J.; Niloofar, P. Reliability modeling and simulation: Advancements with data-driven techniques and expert knowledge integration. Simulation 2024, 101, 845–862. [Google Scholar] [CrossRef]
- Magade, K.; Sharma, A. Significant role of IoT in Cyber-Physical Systems, Context Awareness, and Ambient Intelligence. In The Next Generation Innovation in IoT and Cloud Computing with Applications; CRC Press: Boca Raton, FL, USA, 2025; pp. 16–34. [Google Scholar]
- Chen, T.C.T. Ambient intelligence (AmI). In Explainable Ambient Intelligence (XAmI) Explainable Artificial Intelligence Applications in Smart Life; Springer: Cham, Switzerland, 2024; pp. 1–21. [Google Scholar]
- Ghosh, U.B.; Kesharwani, A.; Khatri, T. Deep Dive into Cognitive Assisted Ambient Intelligent System for Quality Healthcare. In Healthcare Analytics and Advanced Computational Intelligence; CRC Press: Boca Raton, FL, USA, 2024; pp. 13–29. [Google Scholar]
- Acampora, G.; Cook, D.J.; Rashidi, P.; Vasilakos, A.V. A survey on ambient intelligence in healthcare. Proc. IEEE 2013, 101, 2470–2494. [Google Scholar] [CrossRef]
- Queirós, A.; Dias, A.; Silva, A.G.; Rocha, N.P. Ambient assisted living and health-related outcomes—A systematic literature review. Informatics 2017, 4, 19. [Google Scholar] [CrossRef]
- Qayyum, T.; Trabelsi, Z.; Waqar Malik, A.; Hayawi, K. Mobility-aware hierarchical fog computing framework for Industrial Internet of Things (IIoT). J. Cloud Comput. 2022, 11, 72. [Google Scholar] [CrossRef]
- Liu, C.; Zhou, C.; Tan, L.; Cui, J.; Xiao, W.; Liu, J.; Wang, H.; Wang, T. Reliability analysis of subsea manifold system using FMECA and FFTA. Sci. Rep. 2024, 14, 22873. [Google Scholar] [CrossRef]
- Liu, Q.; Dong, M.; Peng, Y. A novel method for online health prognosis of equipment based on hidden semi-Markov model using sequential Monte Carlo methods. Mech. Syst. Signal Process. 2012, 32, 331–348. [Google Scholar] [CrossRef]
- Almaiah, M.A.; Yelisetti, S.; Arya, L.; Babu Christopher, N.K.; Kaliappan, K.; Vellaisamy, P.; Hajjej, F.; Alkdour, T. A novel approach for improving the security of IoT–medical data systems using an enhanced dynamic Bayesian network. Electronics 2023, 12, 4316. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhou, Z.; Fan, H.; Han, X.; Wang, J.; Chen, M. A Health State Prediction Model Based on Belief Rule Base and LSTM for Complex Systems. Intell. Autom. Soft Comput. 2024, 39, 73. [Google Scholar] [CrossRef]
- Said, N.; Mansouri, M.; Al Hmouz, R.; Khedher, A. Deep Learning Techniques for Fault Diagnosis in Interconnected Systems: A Comprehensive Review and Future Directions. Appl. Sci. 2025, 15, 6263. [Google Scholar] [CrossRef]
- Iswarya, P.; Manikandan, K. Algorithms for fault detection and diagnosis in wireless sensor networks using deep learning and machine learning-an overview. In Proceedings of the 2024 10th International Conference on Communication and Signal Processing (ICCSP), Melmaruvathur, India, 12–14 April 2024; pp. 1404–1409. [Google Scholar]
- Kibalya, G.; Serrat, J.; Gorricho, J.L.; Okello, D.; Zhang, P. A deep reinforcement learning-based algorithm for reliability-aware multi-domain service deployment in smart ecosystems. Neural Comput. Appl. 2023, 35, 23795–23817. [Google Scholar] [CrossRef]
- Abdalla, A.Y.; Abdalla, T.Y.; Chyaid, A.M. Internet of Things Based Fuzzy Systems for Medical Applications: A Review. IEEE Access 2024, 12, 163883–163902. [Google Scholar] [CrossRef]
- Kumar, M.S.; Dhulipala, V.S. Fuzzy allocation model for health care data management on IoT assisted wearable sensor platform. Measurement 2020, 166, 108249. [Google Scholar] [CrossRef]
- Saranya, S.; Fatima, N.S. IoT-based patient health data using improved context-aware data fusion and enhanced recursive feature elimination model. IEEE Access 2022, 10, 128318–128335. [Google Scholar] [CrossRef]
- Chamola, V.; Hassija, V.; Sulthana, A.R.; Ghosh, D.; Dhingra, D.; Sikdar, B. A review of trustworthy and explainable artificial intelligence (xai). IEEE Access 2023, 11, 78994–79015. [Google Scholar] [CrossRef]
- Yaqoob, I.; Salah, K.; Jayaraman, R.; Al-Hammadi, Y. Blockchain for healthcare data management: Opportunities, challenges, and future recommendations. Neural Comput. Appl. 2022, 34, 11475–11490. [Google Scholar] [CrossRef]
- Liu, Q.; Liu, Y.; Luo, M.; He, D.; Wang, H.; Choo, K.K.R. The security of blockchain-based medical systems: Research challenges and opportunities. IEEE Syst. J. 2022, 16, 5741–5752. [Google Scholar] [CrossRef]
- Pelekoudas-Oikonomou, F.; Zachos, G.; Papaioannou, M.; De Ree, M.; Ribeiro, J.C.; Mantas, G.; Rodriguez, J. Blockchain-based security mechanisms for IoMT Edge networks in IoMT-based healthcare monitoring systems. Sensors 2022, 22, 2449. [Google Scholar] [CrossRef]
- Catelani, M.; Ciani, L.; Venzi, M. RBD model-based approach for reliability assessment in complex systems. IEEE Syst. J. 2018, 13, 2089–2097. [Google Scholar] [CrossRef]
- El Moumen, H.; El Akchioui, N.; Toukmati, A. Continuous-Time Markov Processes for Reliability Analysis: A Comprehensive Study. In Proceedings of the 2024 4th International Conference on Innovative Research in Applied Science, Engineering and Technology (IRASET), Fez, Morocco, 16–17 May 2024; pp. 1–8. [Google Scholar]
- Cardelli, L.; Grosu, R.; Larsen, K.G.; Tribastone, M.; Tschaikowski, M.; Vandin, A. Algorithmic minimization of uncertain continuous-time Markov chains. IEEE Trans. Autom. Control 2023, 68, 6557–6572. [Google Scholar] [CrossRef]
- Ahmadi, M.; Shekhar, A.; Bauer, P. Reliability assessment for Modular Multilevel Converters using Monte Carlo Simulations. Int. J. Electr. Power Energy Syst. 2025, 165, 110482. [Google Scholar] [CrossRef]
- Faza, A. Estimation of System-Level Reliability Functions for the Power Grid using Probabilistic Modeling and Monte Carlo Simulation. IEEE Access 2025, 13, 71388–71407. [Google Scholar] [CrossRef]
- Zeng, Z.; Barros, A.; Coit, D. Dependent failure behavior modeling for risk and reliability: A systematic and critical literature review. Reliab. Eng. Syst. Saf. 2023, 239, 109515. [Google Scholar] [CrossRef]
- Bracke, S. Reliability Engineering; Springer: Singapore, 2024. [Google Scholar]
- Brito, É.S.; Tomazella, V.L.; Ferreira, P.H. Statistical modeling and reliability analysis of multiple repairable systems with dependent failure times under perfect repair. Reliab. Eng. Syst. Saf. 2022, 222, 108375. [Google Scholar] [CrossRef]
- Li, Z.; Han, C.; Coit, D.W. System reliability models with dependent degradation processes. In Advances in Reliability and Maintainability Methods and Engineering Applications: Essays in Honor of Professor Hong-Zhong Huang on His 60th Birthday; Springer: Cham, Switzerland, 2023; pp. 475–497. [Google Scholar]
- Karaani, S.; Zolghadri, M.; Besbes, M.; Baron, C.; Barkallah, M.; Haddar, M. Systematic analysis of the links between Obsolescence-Shortage and Reliability-Maintainability-Availability. IEEE Access 2025, 13, 88371–88389. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).