Abstract
This research confronts the persistent challenge of data scarcity in medical machine learning by introducing a pioneering methodology that harnesses the capabilities of Generative Pre-trained Transformers (GPT). In response to the limitations posed by a dearth of labeled medical data, our approach involves the synthetic generation of comprehensive patient discharge messages, setting a new standard in the field with GPT autonomously generating 20 fields. Through a meticulous review of the existing literature, we systematically explore GPT’s aptitude for synthetic data generation and feature extraction, providing a robust foundation for subsequent phases of the research. The empirical demonstration showcases the transformative potential of our proposed solution, presenting over 70 patient discharge messages with synthetically generated fields, including severity and chances of hospital re-admission with justification. Moreover, the data had been deployed in a mobile solution where regression algorithms autonomously identified the correlated factors for ascertaining the severity of patients’ conditions. This study not only establishes a novel and comprehensive methodology but also contributes significantly to medical machine learning, presenting the most extensive patient discharge summaries reported in the literature. The results underscore the efficacy of GPT in overcoming data scarcity challenges and pave the way for future research to refine and expand the application of GPT in diverse medical contexts.
1. Introduction
The burgeoning field of medical machine learning confronts an ardent challenge—the paucity of comprehensive and clinically labeled training data [1,2]. The intricate nature of medical data, coupled with stringent privacy regulations, results in a scarcity that hampers the efficacy of machine learning models in healthcare applications. In particular, the insufficiency of labeled data exacerbates the predicament, impeding the ability to develop robust models capable of meaningful clinical insights [1,2].
This research endeavors to alleviate the constraints posed by the limited availability of labeled medical data by harnessing the unparalleled capabilities of Generative Pre-trained Transformers (GPT). In this study, we propose a novel approach that utilizes GPT to synthetically generate medical data, thereby circumventing the challenges associated with data scarcity. Moreover, GPT’s intrinsic ability to analyze and comprehend the synthetic data it generates opens avenues for the extraction of new features, offering a solution to the dearth of labeled data in the medical domain.
The first phase of our investigation involves a meticulous and systematic review of the existing literature, delving into the capabilities of GPT in synthetic data generation. By scrutinizing prior studies, we aim to provide a comprehensive understanding of GPT’s prowess in generating synthetic data for training machine learning models, thereby laying the groundwork for the subsequent phases of our research. Building upon the insights gleaned from the literature, our study proceeds to explore how GPT can not only generate synthetic data but also engage in the analysis of these datasets to extract novel features. Through a critical examination of existing methodologies, we seek to elucidate the potential of GPT in addressing the challenge of data scarcity from a holistic perspective.
As a practical demonstration of our proposed approach, we present a method for synthetically generating patient discharge messages using GPT, as conceptually represented in Figure 1. This pragmatic application serves as a testament to the feasibility and effectiveness of our proposed solution in tackling the limited availability of training data in the medical domain. Furthermore, we showcase how GPT can play a pivotal role in feature extraction from these synthetic patient discharge messages, illustrating its capability to mitigate the scarcity of labeled data (as shown in Figure 1). Through these empirical demonstrations, we aim to establish a robust foundation for the integration of GPT into the realm of medical machine learning, paving the way for enhanced model development in the face of data scarcity. Within the scope of this study, more than 70 patient discharge messages were automatically generated by the proposed GPT prompt. For all these discharge messages, seventeen fields were synthetically generated first, and then three more fields were generated for labeling these discharge message (e.g., severity, chances of hospital re-admission with justificaiton).
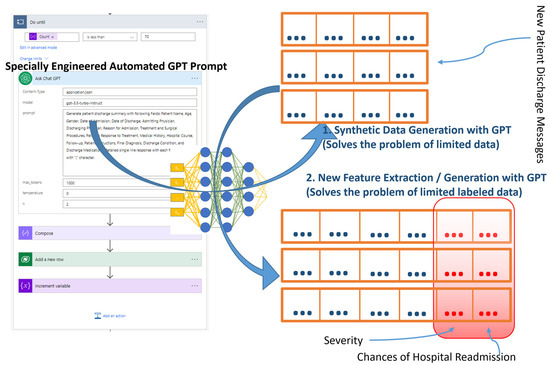
Figure 1.
Conceptual diagram of GPT-based training data generation, feature extraction, and labelling.
This study contributes to the current body of knowledge in the following ways:
- Conducted a comprehensive review of existing literature to explore the utilization of GPT in the medical domain. Among twenty identified works, this study highlighted seven distinct research endeavors that employed GPT to generate or enhance medically relevant data [3,4,5,6,7,8,9].
- Unlike previous studies that relied on manual utilization of GPT’s web interface (as shown in [3,4,5,6,7,8,9]), this research autonomously leveraged the GPT Application Programming Interface (API) alongside automation tools, enabling the efficient generation of a large volume of medically significant data.
- Employing innovative prompt engineering techniques, this study generated 70 synthetic patient discharge messages encompassing seventeen fields and autonomously labeled these messages using GPT technology, resulting in the addition of three augmented fields.
- The generated data underwent evaluation by medical professionals, yielding an impressive average precision, recall, and F1-score of 0.95, 0.97, and 0.96, respectively.
- Furthermore, the synthetically generated medical data were subjected to machine learning algorithms such as regression to uncover hidden correlations among various parameters.
In essence, this research seeks to contribute a novel and comprehensive methodology to the growing body of knowledge addressing the challenges posed by data scarcity in the medical domain [1,2,10]. According to the literature and to the best of our knowledge, this is the first study to generate higly accurate (with F1-score of up to 97%) patient dischage summaries using GPT technology.
2. Literature Review
A recent study in [11] reviews the use of ChatGPT in various aspects of medical research. It evaluates the evidence of ChatGPT’s application in areas including but not limited to treatment, diagnosis, medication provision, drug development, medical report improvement, literature review writing, research conduct, data analysis, and personalized medicine. The review follows the PRISMA guidelines and encompasses studies published between 2022 and 2023. The paper in [12] explores the use of ChatGPT in the systematic review and meta-analysis process in medical research. The paper discusses how ChatGPT can be used for tasks like Risk of Bias analysis and data extraction from randomized controlled trials, highlighting the tool’s ability to reduce the time and effort required for these tasks. It directly addresses the use of ChatGPT in streamlining the process of conducting systematic reviews and meta-analyses, which are integral components of evidence-based decision making in healthcare [12]. The paper illustrates how AI, specifically ChatGPT, can assist in various steps of the systematic review process, including evaluating methodologies and extracting data. The study in [13] focuses on the application of ChatGPT in streamlining the literature selection process for meta-analysis in medical research. It outlines a methodology for using ChatGPT to facilitate the screening of titles and abstracts during meta-analysis, aiming to reduce workload while maintaining recall efficiency. The study includes a glioma meta-analysis for validation and discusses the development of a pipeline called LARS (Literature Records Screener) to assess the performance of ChatGPT in this context [13]. It deals directly with improving the efficiency and effectiveness of literature selection and screening in the context of meta-analysis, a crucial step in systematic reviews and research synthesis [13]. The research work in [14] discusses the potential public health risks posed by large language models like ChatGPT, specifically focusing on the spread of misinformation (infodemic). It explores the evolution of these models, their impact on scientific literature production, and the need for policies to mitigate misinformation risks. It focuses on the broader public health impact and ethical considerations of AI technology in disseminating information [14]. The paper in [15] focuses on evaluating the use of large language models (LLMs) in healthcare. It addresses the need for a comprehensive evaluation framework that assesses LLMs not just for their natural language processing performance but also for their translational value in healthcare. The paper discusses various aspects of LLMs in healthcare, ethical concerns, and proposes a framework for evaluating their application in this field. It goes beyond just the technical aspects of LLMs and delves into the ethical, governance, and practical implications of their use in healthcare [15]. This paper emphasizes a comprehensive evaluation that includes translational value assessment and ethical considerations [15]. The publication in [16] examines the potential influence of large language models like ChatGPT on the field of nuclear medicine. It discusses the capabilities of these models in generating human-like text, their impact on academic publishing, and the potential risks associated with their use in the context of nuclear medicine. It highlights issues like academic integrity, misinformation, and the challenges posed by AI in producing reliable medical content [16]. The focus is on the broader implications of using AI tools like ChatGPT in nuclear medicine, particularly concerning the reliability of the content produced and the ethical considerations surrounding their use in academic and clinical settings [16]. The discussion includes the potential for AI-generated content to influence academic integrity and the spread of misinformation, which are key concerns in the context of public health and ethical use of AI in medicine [16].
The paper in [3] explores the potential of AI, particularly large language models (LLMs) like GPT-4, in generating original scientific research. It discusses the use of GPT-4 to write an original pharmaceutics manuscript, including formulating a research hypothesis, defining an experimental protocol, producing photo-realistic images, generating analytical data, and writing a publication-ready manuscript. This study also examines the limitations of LLMs in referencing literature and emphasizes the need for human input in interpretation and data validation [3]. It focuses on the innovative use of LLMs to generate and augment data, such as creating believable analytical data and images for pharmaceutical research [3]. The emphasis on the AI model’s ability to conceive and execute a research hypothesis and generate multimodal data aligns with the aspects of data generation and augmentation [3]. Research work in [17] explores the applications of ChatGPT and other large language models in various aspects of orthopedics, including education, surgery, and research [17]. The study discusses how these AI tools can assist orthopedic clinicians and surgeons in tasks like disease diagnosis, surgical planning, and educational support. The focus is on the practical applications of ChatGPT in providing assistance to medical professionals in orthopedics, including aiding in diagnosis, surgery, and medical education, which aligns with the aspects of decision support and medical inquiry assistance [17]. The study in [18] presents a systematic review of the applications, benefits, and limitations of ChatGPT in healthcare education, research, and practice. The review includes an analysis of the potential benefits of ChatGPT in scientific writing, healthcare research, and practice, along with concerns regarding ethical, copyright, transparency, and legal issues [18]. Recent work in [19] examines the potential of AI systems, specifically large language models, in generating health awareness messages. The study uses the Bloom model for generating messages about folic acid, comparing them to highly retweeted human-generated messages in terms of quality and clarity. It also involves human and computational evaluations to assess the effectiveness of AI-generated messages in health communication. It focuses on the empirical assessment of AI-generated health messages, analyzing their effectiveness and comparing them to human-generated content [19]. The emphasis on computational and human evaluations of the messages aligns with the aspects of data analysis in medical research [19]. The study in [4] focuses on using GPT-3.5 for data augmentation to address vaccine hesitancy classification in the Dutch language. The study leverages the language model for generating realistic examples of anti-vaccination tweets and evaluates the impact of this augmentation on various machine learning models [4]. It also examines the ability of the synthetic data to generalize to human data in classification tasks. It illustrates the use of GPT-3.5 for generating synthetic data to balance an imbalanced dataset in vaccine hesitancy monitoring, highlighting its capabilities in data augmentation and labeling [4].
Recent work in [5] focuses on enhancing medical question answering systems using GPT-2 for question augmentation and T5-Small for topic extraction. The paper details a model that employs BERT, GPT-2, and T5-Small to improve medical question answering performance, demonstrating the effectiveness of these techniques through experiments [5]. It highlights the use of AI models for augmenting medical question data, a crucial aspect in improving the quality and coverage of datasets used in medical question answering systems [5]. The study in [6] examines the use of GPT-3 in generating synthetic data for Human–Computer Interaction (HCI) research. It explores the ability of GPT-3 to produce believable accounts of HCI experiences and discusses the potential benefits and risks associated with using synthetic data generated by language models. It highlights the use of GPT-3 for generating synthetic user research data, focusing on the model’s ability to create realistic and believable responses in an HCI context [6]. The paper in [7] presents a study on using GPT-2 for data augmentation in the context of patient outcome prediction. The focus is on generating artificial clinical notes in Electronic Health Records (EHRs) to improve the training of machine learning models for predicting patient outcomes, such as readmission rates. The paper discusses a novel textual data augmentation method and evaluates its effectiveness in enhancing predictive performance of deep learning models in healthcare [7]. It explores the use of GPT-2 to augment medical datasets, specifically focusing on generating textual data that can be used to train models for predicting patient outcomes, aligning with data augmentation and labeling aspects [7]. The research work in [8] focuses on using GPT-2 to generate synthetic biological signals, specifically EEG (electroencephalography) and EMG (electromyography), to enhance data classification. The study demonstrates that models trained on synthetic data generated by GPT-2 can classify real EEG and EMG datasets with significant accuracy and that the inclusion of synthetic data during training improves classification performance [8]. It emphasizes the use of AI for generating synthetic biological signals, which augments the available data for training machine learning models in the field of biological signal processing [8]. The paper in [9] focuses on using Transformer-based models, particularly GPT-2, for generating synthetic medical text to augment datasets. The study experiments with these models for data augmentation in clinically relevant NLP tasks such as unplanned readmission prediction and phenotype classification. It evaluates the effectiveness of synthetic data in improving the performance of deep learning models in these healthcare contexts [9]. It highlights the application of AI models in creating synthetic medical text data, aiming to augment existing datasets for improved model training and performance in specific medical tasks [9]. Finally, the paper in [20] discusses the potential of ChatGPT in various medical applications. It examines ChatGPT’s ability to develop AI programs for medicine, its limitations and challenges, ethical concerns like biases and patient confidentiality, and compliance with healthcare regulations. The paper highlights ChatGPT’s potential in democratizing coding and developing AI in medicine, leading to breakthroughs in the medical AI sector [20]. The focus on ethical concerns, patient autonomy, and the responsible use of AI in medicine, along with the exploration of AI’s potential to revolutionize medical research and practice, aligns with this category [20]. These existing research works could be categorized into six distinct categores, as described in Figure 2.

Figure 2.
Six distinct areas of research for “GPT in Medical Domain”.
- Literature Review and Meta-Analysis: Studies in [11,12,13,18] illustrate how AI, specifically ChatGPT, can streamline literature reviews and meta-analyses, aiding in efficient data extraction and evaluation methodologies.
- Data Analysis: As demonstrated in [21,22,23,24,25,26], GPT assists in analyzing research data and generating critical insights. Within the medical domain, research works in [11,19] demonstrate AI’s utility in analyzing complex datasets, including patient outcomes and health message effectiveness, enhancing predictive modeling and comprehension of medical data.
- Medical Question Answering and Decision Support Systems: Studies like [11,17,18] show the role of AI in assisting medical professionals with accurate information, aiding diagnosis, and providing decision support in clinical settings.
- Drug Discovery and Clinical Trial Analysis: While not directly covered in the reviewed articles, this category involves using AI to accelerate drug discovery processes and analyze clinical trial data, potentially enhancing the efficiency and efficacy of pharmaceutical development [11].
- Ethical and Public Health Implications of AI in Medicine: Several recent studies like [11,14,15,16,18,20] discuss the broader ethical implications and public health concerns of AI in medicine, including misinformation and academic integrity.
- Data Generation, Augmentation, and Labeling: To generate new features from data with limited fields, machine learning techniques like entity recognition, category classification, sentiment analysis, and others have traditionally been used [27,28,29,30,31,32,33,34]. After generating new features, the augmented data can be used to effectively train the machine learning models [27,28,29,30,31,32,33,34]. However, with the advent of GPT, new features could be generated either from synthetic data or from existing data, without using traditional feature extraction approaches, as shown in [35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70]. Even within the medical domain, synthetic data creation, data augmentation, and labelling have been proven to be crucial in recent times [3,4,5,6,7,8,9]. These papers illustrate the use of AI for creating and enhancing medical datasets, crucial for training robust machine learning models.
Finally, Table 1 clearly depicts how existing research works on using GPT in the medical domain could be categorized. As shown in Table 1, most of the existing liturature falls under the category of “Data Generation, Augmentation, and Labeling”. Within the next section, a practical scenario of how GPT could be used to generate synthetic medical data as well as how to generate labels for these synthetic data will be detailed.

Table 1.
Categorization of existing studies on the use of GPT in medical domain (X denotes “Topic of Interest”).
3. Methods
The GPT model is based on the Transformer architecture, which involves several key components, like Input Embedding and Positional Encoding, Transformer Blocks, Feed-Forward Neural Network, Normalization and Residual Connections, and Output layer [71].
3.1. Input Embedding and Positional Encoding
- Each input token (word or sub-word) is converted into a vector through an embedding layer.
- Positional encodings are added to these embeddings to provide information about the position of each token in the sequence.
- The combined embedding, E, is given by Equation (1).
3.2. Transformer Blocks
Each block consists of two main parts, the Multi-Head Self-Attention mechanism and the Feed-Forward Neural Network.
- Multi-Head Self-Attention:
- The attention mechanism can be described by Equation (2).
- In Equation (2), Q, K, V are the query, key, and value matrices, and dk is the dimension of the keys.
- In multi-head attention, this process is carried out in parallel multiple times with different, learned linear projections of the queries, keys, and values. The outputs are then concatenated and linearly transformed.
- Feed-Forward Neural Network:
- Each layer contains a fully connected feed-forward network, which is applied to each position separately and identically. This typically involves two linear transformations with a ReLU activation in between. It is represented with Equation (3).
3.3. Normalization and Residual Connections
- Each sub-layer (self-attention, feed-forward) in a transformer block has a residual connection around it, followed by layer normalization.
- The output of each sub-layer is , where is the function implemented by the sub-layer itself.
3.4. Output Layer
- The final layer is a linear transformation followed by a softmax function to predict the probability of the next token in the sequence.
- The output probabilities for a token are computed as , where W and b are the weights and biases of the output layer.
This mathematical framework enables GPT to capture complex patterns and relationships in sequential data [71] and is used in this study to generate synthetic patient discharge messages and even perform analysis on those discharge messages for assessing severity and chances of hospital readmission.
3.5. The Process of Automating Synthetic Medical Data Generation
In the conventional approach, users of GPT technology access the model through its web interface, initiating interactions via specific prompts to derive outputs from the system (as shown in Figure 3). This traditional approach has been demonstrated by research works [3,4,5,6,7,8,9]. Employing such a traditional methodology to produce synthetic medical data necessitates substantial user involvement, which can be time-consuming. To circumvent the need for manual intervention in querying the GPT interface, the current study integrates the GPT API with Microsoft Power Automate to fully automate the process of generating patient discharge summaries, as shown in Figure 3. Microsoft Power Automate orchestrates the interactions with the GPT through its API, facilitating a seamless automated workflow. Consequently, this novel automation strategy enhances the efficiency and effectiveness of generating synthetic patient discharge messages, thus streamlining the process significantly. As seen from Figure 3, the proposed approach of interacting with ChatGPT API is automated, fast, and efficient.
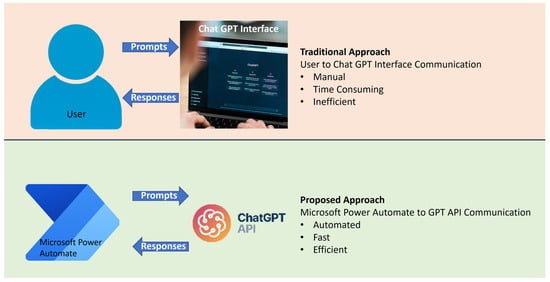
Figure 3.
Traditional approach of manual interaction with Chat GPT web interface vs. fully automated interaction via GPT API.
As seen in Figure 4, the orchestration of GPT API communication is performed using Microsoft Power Automate. The HTTP request component of Microsoft Power Automate can autonomously invoke multiple API calls. As shown in Figure 4, the first HTTP post call to GPT API generates 70 discharge messages. The second HTTP post call then critically evaluates these messages and labels them in terms of (1) severity, (2) chances of hospital readmission, and (3) reasoning. The details of both these calls are shown in Figure 5. It should be noted that Microsoft Power Automate allows the second prompt to investigate the previously generated synthetic message through the variable “Output”, as shown in Figure 5b. Thus, the contextual background of the previously generated messages could be efficiently analyzed in the second prompt, along with augmenting the previous messages with newer labels (i.e., severity, chances of hospital readmission, and reasoning). The reasoning information would be validated by expert doctors at a later stage.
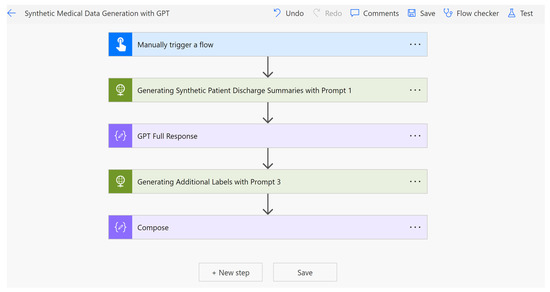
Figure 4.
Microsoft Power Automate invoking API calls to GPT API in an automated manner using HTTP requests.
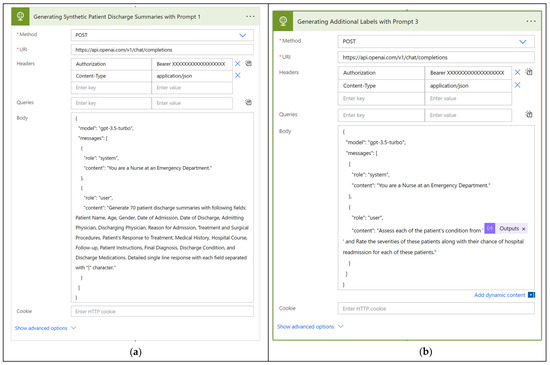
Figure 5.
The process of passing specially designed prompts through Microsoft Power Automate (HTTP post method). * preceding Method and URI denotes mandatory fields. (a) Generating 70 patient discharge messages. (b) Labelling each of the 70 messages with severity and chances of hospital readmission.
As shown in Figure 1 and Figure 5, a specially engineered GPT prompt can be used for generating patient discharge messages. Microsoft Power Automate with GPT API automatically generates patient discharge summaries with specifically guided headings, like Diagnosis, Treatment, Patient Instructions, Medications on Discharge, etc. The complete list can be seen from Appendix A using the prompt of Box 1. Many of these headings (presented in Appendix A) are required for assessment of severity and predicting the chances of hospital readmission, which would be performed in the next stage. As seen from Figure 6, Figure 7, Figure 8 and Figure 9, GPT generated the discharge summaries synthetically (i.e., not real patient information).
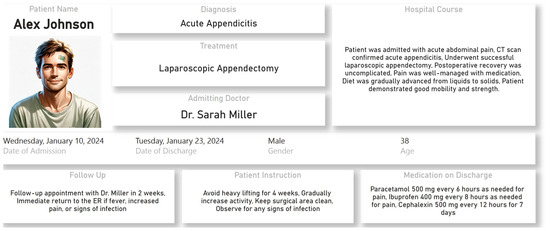
Figure 6.
Synthetic patient discharge summary generated for Alex Johnson using GPT prompt.
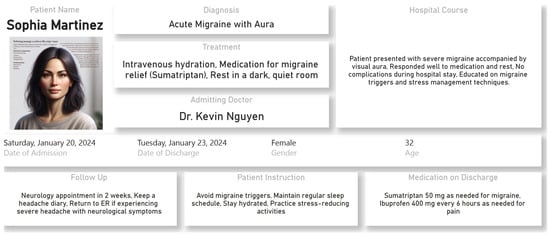
Figure 7.
Synthetic patient discharge summary generated for Sophia Martinez using GPT prompt.
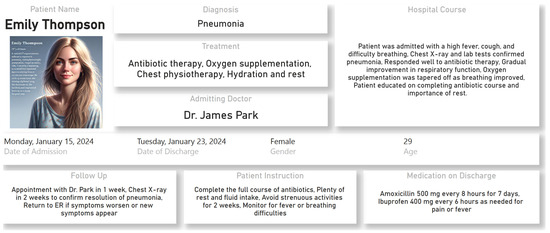
Figure 8.
Synthetic patient discharge summary generated for Emily Thompson using GPT prompt.
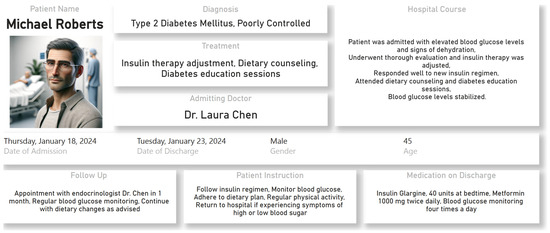
Figure 9.
Synthetic patient discharge summary generated for Michael Roberts using GPT prompt.
Box 1. Generating Synthetic Patient Discharge Summaries.
Generate patient discharge summary with following fields: Patient Name, Age, Gender, Date of Admission, Date of Discharge, Admitting Physician, Discharging Physician, Reason for Admission, Treatment and Surgical Procedures, Patient’s Response to Treatment, Medical History, Hospital Course, Follow-up, Patient Instructions, Final Diagnosis, Discharge Condition, and Discharge Medications. Detailed single line response with each field separated with “|” character.
Box 2. Generating the Images of the Patients Using the Information from Discharge Summaries.
Based on the description of the generated discharge summary, generate an image of that patient.
For Alex Johnson (Figure 6), the GPT response before generating the synthetic patient image is “Based on this summary, I will create an artistic representation of Alex Johnson, a 38-year-old male who has just recovered from an appendectomy. Let’s visualize Alex as having short brown hair, a medium build, and a friendly appearance, reflecting his recovery phase”.
As shown earlier in Figure 1 from the synthetically generated discharge summaries, GPT can effectively be used for generating new features. Figure 5b and Figure 10 illustrate this process further. As seen from Figure 10, critical information (e.g., nature of their medical conditions, treatments received, and the instructions provided upon discharge) are used for generating new features like severity of condition and change of hospital readmission. Box 3 shows the GPT prompt used for this feature augmentation process (as previously demonstrated in Figure 5b).
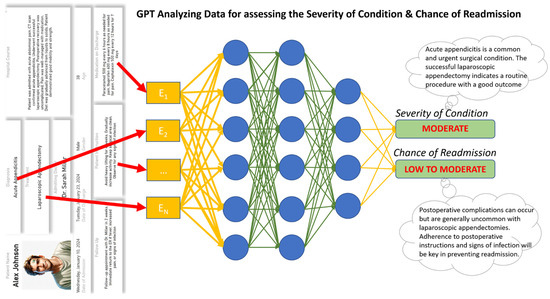
Figure 10.
Feature extraction process using GPT for labelling the discharge messages.
Box 3. Generating New Features for Labeling the Discharge Messages.
Rate the severities of these patients along with their chance of hospital readmission for each of these patients.
As seen from Figure 10, for Alex Johnson (i.e., discharge summary presented in Figure 6), GPT assessed the severity of his condition to be “Moderate” and the changes of hospital readmission to be “Low to Moderate”. This process can be effectively used to label the synthetic data as low, moderate, high, etc., and could be efficiently used to train machine learning models at a later stage. The same methodology could be used for generating synthetic electrocardiogram signals or other bio-signals as well as labelling these signals. Hence, GPT to solve GPT is presented as an effective solution towards solving data scarcity as well as fewer labels in the medical domain.
4. Results
Using the methodology detailed in the previous section, within this study, 70 patient discharge summaries were synthetically generated. As seen from Table 2, these patient discharge summaries had 20 fields comprising Patient Name, Age, Gender, Date of Admission, Date of Discharge, Admitting Physician, Discharging Physician, Reason for Admission, Treatment and Surgical Procedures, Patient’s Response to Treatment, Medical History, Hospital Course, Follow-up, Patient Instructions, Final Diagnosis, Discharge Condition, Discharge Medications, Severity Level, Probability of Hospital Re-admission, and Reasoning. As mentioned in the previous section, the first 17 fields were generated with GPT Prompt 1 and then labelling information (i.e., Severity Level, Probability of Hospital Re-admission, and Reasoning) was generated with Prompt 2. Appendix A shows the details of these 70 generated discharge summaries. Out of these 20 fields, only Age was numeric in nature, and as a result, Table 3 provides various statistics on this numeric field. The value of Age ranged between 23 and 89. There were two date fields, namely date of admission and date of discharge.

Table 2.
Seventy synthetically generated patient discharge summaries with 20 fields each.

Table 3.
Statistics on Age field.
Date of admission ranged from 12 January 2021 to 20 December 2021. Date of discharge ranged from 20 January 2021 to 30 December 2021. From these date fields, the duration of hospital stay could be calculated. Hospital stay ranged from 3 (for Sophie Duncan) to 334 days (Maria Johnson). Finally, Figure 11 shows the distributions of labeling data (i.e., Severity level and Chances of Hospital Re-admission). As seen from Figure 11, 12.86% of the discharge summaries were labeled with the severity level of high and 67.14% of the discharge summaries were labeled with severity level being low. In terms of hospital re-admission, 60% of cases were moderate, 24.29% of cases were low, and 15.71% of the cases were flagged as “moderate to high”.
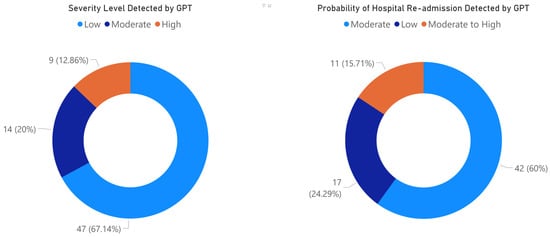
Figure 11.
Results of labeling patient discharge summaries with GPT.
The last three columns in Table 3, namely Severity Level, Probability of Hospital Re-admission, and Reasoning, were generated anew using Prompt 3. This additional information was autonomously generated by GPT, as demonstrated in Figure 5b. Given that GPT was instructed to act as a medical professional in generating these details, the augmented data underwent evaluation by two medical experts.
The evaluation results are depicted in Table 4, revealing an average precision, recall, and F1-score of 0.95, 0.97, and 0.96, respectively, across all three labeled tasks. This indicates GPT’s capability to automatically label medical data with a high level of accuracy. Notably, in Table 4, the F1-Score was highest, at 97% for reasoning, followed by severity and likelihood of hospital admission. This manual validation process underscores the potential for utilizing GPT and related technologies with confidence in generating and enhancing synthetic medical data.

Table 4.
Evaluation of the augmented data by GPT.
Other than manually evaluating the validity of generated information, machine learning algorithms could also be used on the generated synthetic data for obtaining AI-driven insights [72]. The next section will discuss how machine learning algorithms could be used on these synthetic data for obtaining AI-driven insights.
5. Discussion and Concluding Remarks
This research introduces a groundbreaking methodology to address the challenge of data scarcity in medical machine learning by leveraging the capabilities of GPT. The study proposes a comprehensive approach that utilizes GPT for synthetic data generation and subsequent feature extraction, offering a transformative solution to the limitations imposed by the scarcity of labeled medical data. The empirical demonstration involving the synthetic generation of patient discharge messages serves as a practical testament to the feasibility and effectiveness of the proposed methodology, showcasing its potential to revolutionize the integration of GPT into the realm of medical machine learning. Figure 12 shows the deployment of the GPT-based solution in the latest Samsung Galaxy S23 Ultra mobile phone using Microsoft Power BI’s deployed App. The application of this deployment process has been showcased in recent studies through the utilization of low-code platforms [27,30,31,32,34]. As this study exclusively solved the labeled data scarcity for training machine learning models within medical domain (as discussed in [1,2,10]), it needs to be demonstrated how the generated synthetic data could be used in machine leanirng. Figure 12 shows that automated regression identified “Hospital Stays” to be highly corelated with the severity of the patient. The AI-driven insight shown in Figure 12 (within Samsung Galaxy S23 Ultra Mobile) shows that out of the 19 fields, Patient’s Age, Chance of Hospital readmission, and Hospital stays are correlated with severity. This automated regression using “Key Influencer” visualization of Microsoft Power BI has been reported in [73]. The previous section evaluated the validity of the generated medical data using manual evaluation by an expert medical professional. Now, this section demonstrates the use of the automated machine learning algorithm (i.e., regression to obtain the correlated variables) on the synthetic data.
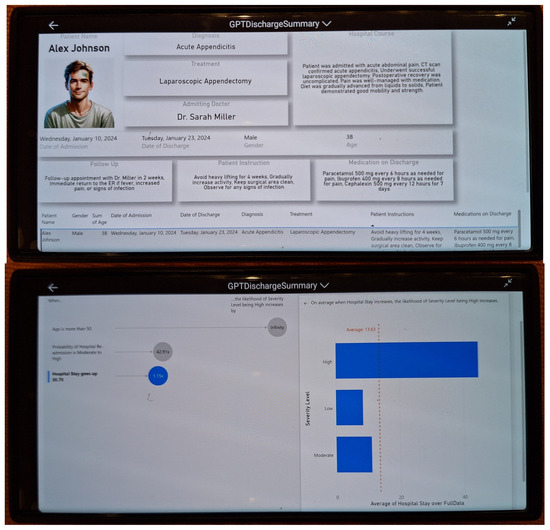
Figure 12.
GPT-based patient discharge summary viewed and analyzed with machine learning algorithms in Samsung Galaxy S23 Ultra.
In summary, this study presents a pioneering and thorough methodology designed to address the data scarcity issues faced by researchers and scientists in the medical field. Leveraging this approach, automation tools such as Microsoft Power Automate were employed alongside the ChatGPT API to not only generate synthetic medical data automatically but also to label these datasets autonomously. The labeling process conducted by GPT was manually assessed by medical experts, yielding an impressive F1-score of 97%. Additionally, machine learning techniques, including regression analysis, were applied to the synthetic data, affirming the validity of the generated information. The integration of ChatGPT API’s synthetic data generation and feature extraction capabilities not only facilitates the development of more robust machine learning models for healthcare applications but also sets the stage for future research endeavors. Future works should explore the application of GPT across diverse medical datasets, optimize its capabilities for specific contexts, and delve into the ethical implications of deploying synthetic data in medical research. This study lays the foundation for a trajectory of research that promises to redefine the landscape of medical machine learning, ultimately benefiting both researchers and clinicians in their pursuit of improved healthcare outcomes.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data attached within this paper.
Conflicts of Interest
The author declares no conflict of interest.
Appendix A

Table A1.
Seventy patient discharge summaries generated with GPT.
Table A1.
Seventy patient discharge summaries generated with GPT.
| Patient Name | Age | Gender | Date of Admission | Date of Discharge | Admitting Physician | Discharging Physician | Reason for Admission | Treatment and Surgical Procedures | Patient’s Response to Treatment | Medical History | Hospital Course | Follow-Up | Patient Instructions | Final Diagnosis | Discharge Condition | Discharge Medications | Severity Level | Probability of Hospital Re-Admission | Reasoning |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| John Doe | 34 | Male | 1/1/2021 | 2/2/2021 | Dr. Smith | Dr. Williams | Acute appendicitis | Appendectomy | Patient responded well to surgical intervention | No significant past medical history | Patient underwent successful appendectomy, recovered without complications | To review in outpatient clinic after 1 week | Light diet, rest and wound care | Final diagnosis of acute appendicitis | Stable at discharge | Prescribed antibiotics, painkillers, and laxatives | Moderate | Low | Severity based on condition ‘Acute appendicitis’. Readmission probability based on discharge condition ‘Stable at discharge’ and medical history. |
| Maria Johnson | 56 | Female | 1/12/2021 | 12/12/2021 | Dr. Johnson | Dr. Robinson | Stroke | IV Thrombolysis, Physical therapy | Significant improvement in mobility and speech | History of hypertension and heart disease | Patient received thrombolysis within time limit and underwent intense rehab | To review in stroke clinic after 4 weeks | Medication compliance, regular exercise, and healthy diet | Final diagnosis of ischemic stroke | Functional improvements, stable at discharge | Prescribed blood thinners, statins, and antihypertensives | High | Moderate to High | Severity based on condition ‘Stroke’. Readmission probability based on discharge condition ‘Functional improvements, stable at discharge’ and medical history. |
| Susan Harris | 38 | Female | 3/15/2021 | 3/20/2021 | Dr. Russo | Dr. Murray | Gallstones | Laparoscopic cholecystectomy | Patient responded well to surgery | No significant past medical history | Surgery was uncomplicated and patient recovered without issue | Follow up with primary care in 2 weeks | Maintain low-fat diet | Final diagnosis of cholelithiasis and cholecystitis | Stable, full recovery anticipated | Prescribed painkillers and antibiotics. | Moderate | Low | Severity based on condition ‘Gallstones’. Readmission probability based on discharge condition ‘Stable, full recovery anticipated’ and medical history. |
| James Thompson | 69 | Male | 2/1/2021 | 2/7/2021 | Dr. White | Dr. Black | Chest pain, confirmed as myocardial infarction | Angioplasty and stent placement | Patient showed remarkable improvement post-procedure | Has a history of diabetes and hypertension | Patient had a successful procedure and was monitored in ICU for a day. Released later to general ward | Cardiology follow-up in one month | Lifestyle modification, medication compliance | Acute anterior wall Myocardial Infarction | Stable at discharge | Medications including antiplatelets, beta-blockers, ACE inhibitors, statins and anti-diabetic regimen. | High | Moderate to High | Severity based on condition ‘Myocardial Infarction’. Readmission probability based on discharge condition ‘Stable at discharge’ and medical history of diabetes and hypertension. |
| Elizabeth Davis | 42 | Female | 4/10/2021 | 4/15/2021 | Dr. Turner | Dr. Walker | Pneumonia | Antibiotics treatment and respiratory therapy | Patient’s condition improved significantly | Previously healthy with no significant medical history | Treated with IV antibiotics and oxygen through nasal cannula | Pulmonary follow-up in 3 weeks | Completion of oral antibiotic course, rest, and hydration | Final diagnosis of community-acquired pneumonia | Improving at discharge | Oral antibiotics and bronchodilator inhaler. | Moderate | Low | Severity based on condition ‘Pneumonia’. Readmission probability based on discharge condition ‘Improving at discharge’ and previously healthy status. |
| David Wilson | 57 | Male | 10/21/2021 | 10/31/2021 | Dr. Morris | Dr. Wright | Liver failure | Supportive care, liver transplant assessment | Slow but steady improvement | History of alcoholism and Hepatitis C | Patient managed with diuretics and lactulose, assessed for transplant suitability | Follow-up with hepatology team in 1 week | Avoidance of alcohol, low salt diet | End-stage liver disease | Stable at discharge, with close outpatient monitoring | Prescribed diuretics, lactulose, and multivitamins. | High | Moderate to High | Severity based on condition ‘Liver failure’. Readmission probability based on discharge condition ‘Stable at discharge, with close outpatient monitoring’ and medical history of alcoholism and Hepatitis C. |
| Anna Taylor | 89 | Female | 5/9/2021 | 5/16/2021 | Dr. Simmons | Dr. Mitchell | Hip fracture after fall | Hip pinning surgery | Gradual improvement with physical therapy | Osteoporosis, past history of falls | Surgery was successful with no complications, physiotherapy started postoperatively | Ortho follow-up after 2 weeks | Physical therapy, fall precautions at home | Femoral neck fracture | Stable with improving mobility | Analgesics and Calcium and Vitamin D supplements. | Moderate | Low | Severity based on condition ‘Hip fracture’. Readmission probability based on discharge condition ‘Stable with improving mobility’ and medical history of osteoporosis. |
| Michael Anderson | 72 | Male | 6/19/2021 | 6/28/2021 | Dr. Young | Dr. Hernandez | Prostate cancer | Prostatectomy | Well tolerated procedure with good recovery | Past history of asthma | Surgery completed successfully and patient made steady progress in recovery | Urology follow-up after 1 month | Medication compliance, report any urinary difficulties | Prostate adenocarcinoma | Stable at discharge | Prescribed painkillers and inhaled corticosteroids. | High | Low | Severity based on condition ‘Prostate cancer’. Readmission probability based on discharge condition ‘Stable at discharge’ and past history of asthma. |
| Patricia Lee | 52 | Female | 8/1/2021 | 8/7/2021 | Dr. Morris | Dr. Hall | Breast Cancer | Lumpectomy and radiation | Good recovery with no post-op complications | First degree relative with breast cancer | Surgery completed with clear margins, initiated on post-op radiation | Oncology follow-up in 1 week | Healthy diet, regular exercise, follow recommended screening guidelines | Breast Cancer, stage IIa | Stable at discharge | Prescribe painkillers and anti-emetics. | High | Moderate to High | Severity based on condition ‘Breast Cancer’. Readmission probability based on discharge condition ‘Stable at discharge’ and family history of breast cancer. |
| Jacob Martinez | 30 | Male | 11/5/2021 | 11/9/2021 | Dr. King | Dr. Gonzalez | Acute pancreatitis | Fluid resuscitation and supportive care | Improved significantly with treatment | History of gallstones | Patient received IV fluids and pain management | GI follow up in 2 weeks | Low-fat diet, avoid alcohol, medication compliance | Acute pancreatitis | Improved, stable at discharge | Prescribed pain medication and proton pump inhibitors. | Low | Moderate to High | Severity based on condition ‘Acute pancreatitis’. Readmission probability based on discharge condition ‘Improved, stable at discharge’ and medical history of gallstones. |
| Melissa Martin | 65 | Female | 9/19/2021 | 10/1/2021 | Dr. Thompson | Dr. Moore | Type 2 Diabetes Complications | Insulin Therapy, Diabetic Education | Patient responded well to therapy | Long-standing history of Type 2 Diabetes | Patient was educated about the importance of regular blood sugar monitoring, diet and exercise | Endocrinology follow up in 1 month | Regular blood sugar monitoring, maintain balanced diet, regular exercise | Uncontrolled Type 2 Diabetes | Stable at discharge | Insulin and oral hypoglycemic agents. | High | Moderate to High | Severity based on condition ‘Type 2 Diabetes Complications’. Readmission probability based on discharge condition ‘Stable at discharge’ and medical history of Type 2 Diabetes. |
| Jason Jackson | 45 | Male | 5/22/2021 | 6/1/2021 | Dr. Roberts | Dr. Lopez | Traumatic Brain Injury | Debulking surgery, rehabilitation | Patient showed gradual improvement | No remarkable past medical history | Patient underwent surgery and was transferred to rehabilitation post-stabilization | Neurosurgery follow-up in 1 week | Ongoing rehabilitation, medication adherence | Traumatic Brain Injury | Fair condition at discharge | Prescribed anticonvulsants and analgesics. | Moderate | Moderate to High | Severity based on condition ‘Traumatic Brain Injury’. Readmission probability based on discharge condition ‘Fair condition at discharge’ and medical history. |
| Linda Ramos | 70 | Female | 12/10/2021 | 12/20/2021 | Dr. Reed | Dr. Jenkins | Chronic Obstructive Pulmonary Disease (COPD) exacerbation | Inhaler therapy, steroids, antibiotics | Patient’s breathing improved significantly | History of smoking and COPD | Managed with nebulizers, steroids and antibiotics | Pulmonary follow-up in 2 weeks | Smoking cessation, use inhalers as instructed | Chronic Obstructive Pulmonary Disease, acute exacerbation | Stable at discharge | Prescribed inhalers, steroids and antibiotics. | High | Moderate to High | Severity based on condition ‘COPD exacerbation’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of smoking and COPD. |
| Joshua White | 62 | Male | 7/7/2021 | 7/12/2021 | Dr. Foster | Dr. Simmons | Heart failure exacerbation | Diuretics, ACE inhibitors, lifestyle modification | Patient’s condition improved and stabilized | History of hypertension and heart disease | Managed with medications and patient education about lifestyle changes | Cardiology follow-up in 1 month | Regular exercise, low sodium diet, medication compliance | Congestive Heart Failure, acute exacerbation | Stable at discharge | Prescribed diuretics, ACE inhibitors and beta blockers. | High | Moderate to High | Severity based on condition ‘Heart failure exacerbation’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of hypertension and heart disease. |
| Emma Bailey | 88 | Female | 9/15/2021 | 10/1/2021 | Dr. Russell | Dr. Watson | Alzheimer’s disease, behavioral changes | Adjustment of medications, behavioral therapy | Gradual improvement in sleep pattern and agitation | Long-standing Alzheimer’s disease | Patient was managed with adjustment of Alzheimer’s medications and behavioral techniques | Neurology follow-up in 1 month | Routine, structured day, family support | Alzheimer’s disease with behavioral complications | Stable at discharge | Prescribed Donepezil, antipsychotics and sleep aids. | Moderate | Low | Severity based on condition ‘Alzheimer’s disease, behavioral changes’. Readmission probability based on discharge condition ‘Stable at discharge’ and long-standing Alzheimer’s disease. |
| Michael Cox | 77 | Male | 12/20/2021 | 12/30/2021 | Dr. Rogers | Dr. Bennett | Complications of Chronic Kidney Disease | Dialysis, nutritional counseling | Patient’s renal function improved significantly | History of Chronic Kidney Disease and Hypertension | Managed with dialysis and medications | Nephrology follow-up in 2 weeks | Low sodium, low potassium diet, medication compliance | Chronic Kidney Disease, stage V | Stable at discharge | Prescribed blood pressure medications, phosphate binders and erythropoietin. | High | Moderate to High | Severity based on condition ‘Complications of Chronic Kidney Disease’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of Chronic Kidney Disease and Hypertension. |
| Sarah Walker | 64 | Female | 7/25/2021 | 8/5/2021 | Dr. Richardson | Dr. Hughes | Gastritis | Antacid administration, dietary changes | Patient experienced reduction of symptoms | History of gastritis and GERD | Managed with antacids and dietary changes | Follow-up appointment with gastroenterologist in 3 weeks | Avoid spicy food, medication compliance | Acute gastritis | Stable at discharge | Prescribed Proton-pump inhibitors. | Low | Low | Severity based on condition ‘Gastritis’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of gastritis and GERD. |
| Christopher Cooper | 85 | Male | 8/1/2021 | 8/10/2021 | Dr. Ramirez | Dr. Hill | Rheumatoid Arthritis pain | Pain medication adjustment, physical therapy | Patient’s mobility improved and pain reduced | History of Rheumatoid Arthritis | Pain management approach adjusted, PT introduced | Follow-up with Rheumatologist in 2 weeks | Physical therapy exercises, medication compliance | Rheumatoid arthritis with acute flare | Stable at discharge | Prescribed NSAIDs, steroids, DMARDs. | Moderate | Low | Severity based on condition ‘Rheumatoid Arthritis pain’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of Rheumatoid Arthritis. |
| Amanda Bell | 59 | Female | 11/15/2021 | 11/25/2021 | Dr. Graham | Dr. Meyer | Depression | Cognitive Behavioral Therapy, medication adjustment | Patient’s mood improved with treatment | History of Major Depressive Disorder | Treatment included medication adjustment and therapy | Psychiatry follow-up in 1 week | Maintenance of therapy schedule, medication compliance | Major Depressive Disorder, recurrent, moderate | Stable at discharge | Prescribed SSRIs and benzodiazepines. | Moderate | Moderate to High | Severity based on condition ‘Depression’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of Major Depressive Disorder. |
| Anthony Reyes | 73 | Male | 9/20/2021 | 10/1/2021 | Dr. Jenkins | Dr. Gordon | Severe Hypertension | Increase in antihypertensives, lifestyle modifications | Patient’s blood pressure reduced and stabilized | Long-standing history of Hypertension | Managed with an increase in hypertension medication and lifestyle modifications | Cardiology follow-up in 2 weeks | Regular exercise, weight loss, low sodium diet, medication compliance | Extremely high blood pressure | Stable at discharge | Prescribed ACE inhibitors, Diuretics. | Moderate | Low | Severity based on condition ‘Severe Hypertension’. Readmission probability based on discharge condition ‘Stable at discharge’ and long-standing history of Hypertension. |
| Olivia Ward | 32 | Female | 10/21/2021 | 10/30/2021 | Dr. Cole | Dr. Cook | Pregnancy with hypertension | Bed rest, blood pressure medications | Blood pressure controlled with no distress to fetus | No significant past medical history | Managed with bed rest and blood pressure medications, and regular monitoring of fetus | Obstetrics follow-up in 1 week | Bed rest, medication compliance, regular antenatal checks | Gestational Hypertension | Stable at discharge | Prescribed labetalol. | Moderate | Low | Severity based on condition ‘Pregnancy with hypertension’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant past medical history. |
| William Howard | 56 | Male | 6/12/2021 | 6/23/2021 | Dr. Baylor | Dr. Black | Pneumonia | Antibiotics, respiratory therapy | Patient’s condition improved significantly | History of COPD | Treated with IV antibiotics and oxygen therapy | Pulmonary follow-up in 1 month | Complete antibiotic course, smoking cessation advice | Final diagnosis of community-acquired pneumonia | Stable at discharge | Prescribed oral antibiotics and inhalers. | Moderate | Moderate | Severity based on condition ‘Pneumonia’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of COPD. |
| Ava Davis | 43 | Female | 8/5/2021 | 8/15/2021 | Dr. Craig | Dr. Houston | Asthma exacerbation | Bronchodilators, steroids, inhaler technique review | Improvement in asthma control | Long-standing asthma | Treated with bronchodilators and steroids, inhaler technique revised | Pulmonary follow-up in 2 weeks | Avoid triggers, use inhaler as instructed | Asthma exacerbation | Stable at discharge | Prescribed inhalers and oral steroids. | Low | Moderate | Severity based on condition ‘Asthma exacerbation’. Readmission probability based on discharge condition ‘Stable at discharge’ and long-standing asthma. |
| Benjamin Turner | 66 | Male | 7/14/2021 | 7/24/2021 | Dr. Foster | Dr. Reed | Diabetic foot ulcer | Wound care, blood sugar control, antibiotics | Slow healing but progress with wound | History of type 2 diabetes, peripheral neuropathy | Managed with wound care, foot off-loading, and blood sugar control | Endocrinology follow-up in 1 month | Foot care, blood sugar control, follow up check | Diabetic foot ulcer | Stable at discharge | Prescribed insulin, oral hypoglycemic, topical and oral antibiotics. | Low | Moderate | Severity based on condition ‘Diabetic foot ulcer’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of type 2 diabetes, peripheral neuropathy. |
| Charlotte Simmons | 31 | Female | 3/22/2021 | 4/1/2021 | Dr. Thompson | Dr. Johnson | Ectopic Pregnancy | Laparoscopic surgery | Safe recovery post-surgery | Prior ectopic pregnancy | Ectopic pregnancy removal via laparoscopic approach | Ob-Gyn follow-up in 2 weeks | Rest, avoid lifting heavy weights, medication compliance | Final diagnosis of ectopic pregnancy | Rapid recovery at discharge | Prescribed painkillers and oral contraceptives. | Low | Moderate | Severity based on condition ‘Ectopic Pregnancy’. Readmission probability based on discharge condition ‘Rapid recovery at discharge’ and prior ectopic pregnancy. |
| Daniel Rodriguez | 58 | Male | 6/15/2021 | 6/26/2021 | Dr. Brooks | Dr. Davis | Coronary artery disease | Angioplasty and stent placement | Significant improvement post-procedure | History of smoking and hypertension | Procedure successful with no complications, smoking cessation advice given | Cardiology follow-up in 1 month | Smoking cessation, regular exercise, medication compliance | Final diagnosis of coronary artery disease | Stable at discharge | Prescribed antiplatelets, beta-blockers, ACE inhibitors, statins. | Low | Moderate | Severity based on condition ‘Coronary artery disease’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of smoking and hypertension. |
| Lily Morris | 76 | Female | 7/30/2021 | 8/9/2021 | Dr. Carter | Dr. Collins | Urinary tract infection | Antibiotics and hydration | Resolved with treatment | History of recurring UTIs | Treated with antibiotics, urinary culture guided treatment | Urology follow-up in 3 weeks | Hydration, wipe front to back, medication compliance | Final diagnosis of urinary tract infection | Resolved at discharge | Prescribed oral antibiotics. | Low | Moderate | Severity based on condition ‘Urinary tract infection’. Readmission probability based on discharge condition ‘Resolved at discharge’ and history of recurring UTIs. |
| Noah Taylor | 69 | Male | 6/23/2021 | 7/1/2021 | Dr. Howard | Dr. Bennett | Pulmonary embolism | Anticoagulation therapy | Symptoms improved with treatment | Past history of deep vein thrombosis | IV anticoagulation followed by oral therapy to maintain INR | Hematology follow-up in 1 week | Avoid activities that can lead to falls, medication compliance | Final diagnosis of pulmonary embolism | Stable at discharge | Prescribed oral anticoagulants. | Low | Moderate | Severity based on condition ‘Pulmonary embolism’. Readmission probability based on discharge condition ‘Stable at discharge’ and past history of deep vein thrombosis. |
| Zoe Parker | 54 | Female | 8/24/2021 | 8/31/2021 | Dr. Martin | Dr. Martinez | Crohn’s disease flare | Steroids, infliximab infusions | Response to treatment with symptom resolution | Established Crohn’s disease | Managed with IV corticosteroids and infliximab infusions | Gastroenterology follow-up in 2 weeks | Avoid triggers, medication compliance, hydrated | Crohn’s disease acute flare | Stable at discharge | Prescribed oral steroids, infliximab infusion appointments. | Low | Moderate | Severity based on condition ‘Crohn’s disease flare’. Readmission probability based on discharge condition ‘Stable at discharge’ and established Crohn’s disease. |
| Ethan Miller | 61 | Male | 12/8/2021 | 12/18/2021 | Dr. Adams | Dr. Barnes | Lung Cancer | Chemotherapy | Tolerating chemotherapy with manageable side effects | No significant past medical history | Patient initiated on chemotherapy regimen | Oncology follow-up in 1 week | Adequate hydration, medication compliance | Final diagnosis of lung cancer | Stable at discharge | Prescribed anti-emetics and pain management regimen. | Low | Low | Severity based on condition ‘Lung Cancer’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant past medical history. |
| Emily Roberts | 67 | Female | 11/26/2021 | 12/10/2021 | Dr. Jackson | Dr. Thompson | Acute renal failure | Dialysis | Renal function improved with dialysis, kidney function partially restored | Past history of hypertension and diabetes | Treated with intermittent hemodialysis and managed blood pressure and glucose | Nephrology follow-up in 1 week | Low sodium and potassium diet, medication compliance | Final diagnosis of acute renal failure | Improved at discharge | Prescribed antihypertensives, insulin, and dialysis prescription. | Low | Moderate | Severity based on condition ‘Acute renal failure’. Readmission probability based on discharge condition ‘Improved at discharge’ and past history of hypertension and diabetes. |
| Joseph Garcia | 80 | Male | 10/5/2021 | 10/15/2021 | Dr. Phillips | Dr. Campbell | Chronic heart failure exacerbation | Diuretics, ACE inhibitors, Beta-blockers | Symptoms improved with medication adjustment | Long-standing heart failure, prior myocardial infarction | Managed with increase in diuretic dose, blood pressure control | Cardiology follow-up in 1 week | Low sodium diet, daily weight monitoring, medication compliance | Chronic heart failure exacerbation | Stable at discharge | Prescribed diuretics, ACE inhibitors, beta-blockers. | Low | Moderate | Severity based on condition ‘Chronic heart failure exacerbation’. Readmission probability based on discharge condition ‘Stable at discharge’ and long-standing heart failure, prior myocardial infarction. |
| Mia Wong | 28 | Female | 7/22/2021 | 7/31/2021 | Dr. Evans | Dr. Rogers | Thyroiditis | Thyroid hormone replacement therapy | Thyroid hormone levels returned to normal | No significant medical history | Managed with thyroid hormone replacement therapy | Endocrinology follow-up in 1 month | Medication compliance | Final diagnosis of subacute thyroiditis | Stable at discharge | Levothyroxine. | Low | Moderate | Severity based on condition ‘Thyroiditis’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant medical history. |
| Isaac Perry | 46 | Male | 9/25/2021 | 10/1/2021 | Dr. Ross | Dr. Griffin | Cellulitis | IV antibiotics followed by oral antibiotics | Infection resolved with treatment | No significant medical history | Patient treated with IV then oral antibiotics | Follow-up with primary care in 1 week | Complete antibiotic course, local wound care | Final diagnosis of cellulitis | Resolved at discharge | Oral antibiotics. | Low | Moderate | Severity based on condition ‘Cellulitis’. Readmission probability based on discharge condition ‘Resolved at discharge’ and no significant medical history. |
| Sophia Lewis | 75 | Female | 8/2/2021 | 8/11/2021 | Dr. Kennedy | Dr. Dunn | Congestive heart failure exacerbation | Diuretics, dietary adjustments | Symptoms improved with treatment | History of coronary artery disease | Managed with medication optimization and dietary advice | Cardiology follow-up in 2 weeks | Low sodium diet, medication adherence | Congestive Heart Failure Exacerbation | Stable at discharge | Prescribed loop diuretics, ACE inhibitors, and beta blockers. | Low | Moderate | Severity based on condition ‘Congestive heart failure exacerbation’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of coronary artery disease. |
| Grace Foster | 61 | Female | 4/23/2021 | 4/30/2021 | Dr. Reed | Dr. Kline | Chronic Kidney Disease | Dialysis | Stable under dialysis treatment | History of diabetes and hypertension | Underwent dialysis and optimized blood pressure control | Nephrology follow-up in 1 week | Low sodium diet, medication compliance | Chronic Kidney Disease Stage 5 | Stable at discharge | Prescribed antihypertensive, erythropoiesis-stimulating agents. | Low | Moderate | Severity based on condition ‘Chronic Kidney Disease’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of diabetes and hypertension. |
| Noah Butler | 65 | Male | 10/1/2021 | 10/12/2021 | Dr. Wells | Dr. Perez | COPD Exacerbation | Corticosteroids, bronchodilators | Breathing improved noticeably | Long-standing COPD, ex-smoker | Managed with nebulized bronchodilators and systemic corticosteroids | Pulmonary follow-up in 1 month | Smoking cessation, use inhalers as instructed | Acute COPD exacerbation | Stable at discharge | Prescribed inhalers and a short course of oral steroids. | Low | Moderate | Severity based on condition ‘COPD Exacerbation’. Readmission probability based on discharge condition ‘Stable at discharge’ and long-standing COPD, ex-smoker. |
| Eleanor Barnes | 50 | Female | 9/10/2021 | 9/16/2021 | Dr. Stevens | Dr. Rivera | Rheumatoid Arthritis Flare | Steroids and NSAIDs | Pain and swelling reduced significantly | Long-standing Rheumatoid Arthritis | Managed with increase in steroids and NSAIDs | Rheumatology follow-up in 2 weeks | Gentle exercise, joint care, medication compliance | Acute Rheumatoid Arthritis flare | Stable at discharge | Prescribed steroids and NSAIDs. | Low | Moderate | Severity based on condition ‘Rheumatoid Arthritis Flare’. Readmission probability based on discharge condition ‘Stable at discharge’ and long-standing Rheumatoid Arthritis. |
| Lucas Peterson | 78 | Male | 3/26/2021 | 4/1/2021 | Dr. McDonald | Dr. Baker | Gouty Arthritis | Colchicine, Allopurinol | Gout attack settled, and uric acid lowered | History of recurrent Gout attacks | Managed with acute gout treatment and urate-lowering therapy | Follow-up with Rheumatologist in 2 weeks | Low purine diet, avoid alcohol, medication compliance | Final diagnosis of Gouty Arthritis | Stable at discharge | Prescribed colchicine and allopurinol. | Low | Moderate | Severity based on condition ‘Gouty Arthritis’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of recurrent Gout attacks. |
| Sophie Duncan | 23 | Female | 5/30/2021 | 6/2/2021 | Dr. Bryant | Dr. Coleman | Acute appendicitis | Laparoscopic appendectomy | Excellent recovery with no complications | Previously healthy | Successfully underwent laparoscopic appendectomy | General Surgery follow-up in 2 weeks | Care of operative site, resume regular activity as tolerated | Acute appendicitis | Stable at discharge | Analgesics, wound care recommendations. | Low | Moderate | Severity based on condition ‘Acute appendicitis’. Readmission probability based on discharge condition ‘Stable at discharge’ and being previously healthy. |
| Samuel Larson | 71 | Male | 12/15/2021 | 12/22/2021 | Dr. Foster | Dr. Craig | Pneumonia | Antibiotics, respiratory support | Response to antibiotics with improved breathing | History of COPD | Received IV antibiotics and supplemental oxygen | Follow-up with Pulmonologist in 4 weeks | Take medications as prescribed, rest and adequate nutrition | Pneumonia | Stable at discharge | Oral antibiotics for completing course. | Moderate | Moderate | Severity based on condition ‘Pneumonia’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of COPD. |
| Sarah Woods | 58 | Female | 11/11/2021 | 11/17/2021 | Dr. Romero | Dr. Jacobs | Breast Cancer | Lumpectomy and sentinal lymph node biopsy | No complications with satisfactory recovery | No significant history | Procedure went without any complications, pathological report awaited | Follow-up with Oncologist in 1 week | Incision care, avoid physical exertion | Breast Cancer | Stable at discharge | Pain management medications. | Low | Moderate | Severity based on condition ‘Breast Cancer’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant past medical history. |
| Jack Hudson | 46 | Male | 10/24/2021 | 10/31/2021 | Dr. Paul | Dr. Baker | Gastric ulcers | Proton pump inhibitors, dietary modifications | Symptoms improved significantly with treatment | History of NSAID use | Managed with PPI therapy and dietary advice | Gastroenterology follow-up in 1 month | Avoid spicy food, alcohol, smoking, medication adherence | Gastric ulcer | Stable at discharge | Omeprazole, Sucralfate. | Low | Moderate | Severity based on condition ‘Gastric ulcers’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of NSAID use. |
| Ivy Johnson | 80 | Female | 9/3/2021 | 9/15/2021 | Dr. Jackson | Dr. Riley | Stroke rehabilitation | Physical and occupational therapy | Gradual improvement with still residual weakness | Past history of hypertension and diabetes | Underwent intensive rehabilitation therapy | Follow-up with Outpatient Rehab and Neurologist in 4 weeks | Physiotherapy, medication compliance | Stroke with right hemiparesis | Stable at discharge | Antihypertensives, oral antidiabetics, aspirin. | Low | Moderate | Severity based on condition ‘Stroke rehabilitation’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of hypertension and diabetes. |
| Elijah Myers | 55 | Male | 11/3/2021 | 11/10/2021 | Dr. Ayers | Dr. Harlow | Pancreatitis | IV fluids, pain management, and dietary adjustments | Symptoms improved significantly | History of alcohol abuse | Managed with IV fluids, pain management, and alcohol detox | Gastroenterology and Addiction specialist follow-up in 1 week | Total abstinence from alcohol, low-fat diet, medication compliance | Alcohol-induced pancreatitis | Improved at discharge | Prescribed pain killers, pancreatic enzymes, and detox medications. | Low | Moderate | Severity based on condition ‘Pancreatitis’. Readmission probability based on discharge condition ‘Improved at discharge’ and history of alcohol abuse. |
| Hannah Peters | 36 | Female | 10/11/2021 | 10/20/2021 | Dr. Madison | Dr. Turner | Uncontrolled Type 1 Diabetes | Insulin regulation, diet and lifestyle changes | Blood sugar levels returned to normal | Long-standing diabetes | Management involved adjustment of insulin dose and dietary advice | Endocrinology follow-up in 1 week | Regular monitoring, maintain balanced diet, regular exercise | Uncontrolled Type 1 Diabetes | Stable at discharge | Insulin as per optimized prescription. | Moderate | Moderate | Severity based on condition ‘Uncontrolled Type 1 Diabetes’. Readmission probability based on discharge condition ‘Stable at discharge’ and long-standing diabetes. |
| William Riley | 72 | Male | 7/22/2021 | 7/29/2021 | Dr. Howard | Dr. Jenkins | Chronic Obstructive Pulmonary disease exacerbation | Oxygen therapy, steroids, and antibiotics | Breathing normalized, chest clearing | History of smoking and COPD | Managed with nebulizers, steroids, and antibiotics | Pulmonary follow-up in 2 weeks | Smoking cessation, use inhalers as instructed | COPD exacerbation | Stable at discharge | Inhalers, steroids, and antibiotics. | Low | Moderate | Severity based on condition ‘Chronic Obstructive Pulmonary disease exacerbation’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of smoking and COPD. |
| Lucy Foster | 46 | Female | 9/15/2021 | 9/30/2021 | Dr. Reese | Dr. Castillo | Breast Cancer | Chemotherapy | Moderate side effects managed | No significant family history | Commencement of chemotherapy regimen | Oncology follow-up in 1 week | Healthy diet, gentle exercise, medication compliance | Breast Cancer, stage IIb | Stable at discharge | Prescribed antiemetic and analgesic. | Low | Moderate | Severity based on condition ‘Breast Cancer’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant family history. |
| Oliver Shaw | 35 | Male | 4/27/2021 | 5/2/2021 | Dr. Piper | Dr. Shaw | Fracture tibia | Open reduction and internal fixation | Recovery as expected, mobilizing with support | No significant medical history | Smooth surgery, recovery in ward until independent mobilization achieved | Orthopedic follow-up in 1 week | Weight-bearing as per advice, rest, elevate limb | Tibia fracture | Stable at discharge | Analgesics, anticoagulant. | Low | Moderate | Severity based on condition ‘Fracture tibia’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant medical history. |
| Stella Rogers | 55 | Female | 8/21/2021 | 8/31/2021 | Dr. Sparks | Dr. Kennedy | Vasculitis | Steroids and immunosuppressants | Symptoms improved significantly | No significant medical history | Managed with steroids and immunosuppressants | Rheumatology follow-up in 2 weeks | Medication compliance, regular follow ups, report any new symptoms | Vasculitis | Stable at discharge | Corticosteroids, immunosuppressants. | Low | Moderate | Severity based on condition ‘Vasculitis’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant medical history. |
| Liam Griffin | 81 | Male | 7/25/2021 | 8/8/2021 | Dr. Patterson | Dr. Phillips | Pneumonia | Antibiotics and supportive care | Condition improved significantly | History of diabetes, hypertension | Treated with IV antibiotics and oxygen therapy | Pulmonology follow-up in 3 weeks | Medication compliance, smoking cessation | Pneumonia | Stable at discharge | Oral antibiotics to complete course. | Moderate | Moderate | Severity based on condition ‘Pneumonia’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of diabetes, hypertension. |
| Hazel Ortiz | 45 | Female | 11/10/2021 | 11/18/2021 | Dr. Snyder | Dr. Hamilton | Severe Anemia | Blood transfusion, iron supplements | Blood levels normalized | History of heavy menstrual bleeding | Fluid resuscitation and blood transfusions were given | Gynecology follow-up in 1 week | Oral iron supplements, balanced diet | Severe Iron Deficiency Anemia | Stable at discharge | Iron supplement, analgesic. | Low | Moderate | Severity based on condition ‘Severe Anemia’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of heavy menstrual bleeding. |
| Levi Cooper | 63 | Male | 1/15/2021 | 1/20/2021 | Dr. Bowman | Dr. Francis | Gastrointestinal bleeding | Endoscopy, Clipping of bleeding ulcer | Bleeding stopped, stable condition | History of chronic NSAID use | Endoscopic intervention was successful without complications | Gastroenterology follow-up in 1 week | Avoid NSAIDs and alcohol, medication compliance | Peptic Ulcer Disease with bleeding | Stable at discharge | Proton pump inhibitors. | Low | Moderate | Severity based on condition ‘Gastrointestinal bleeding’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of chronic NSAID use. |
| Lily Rogers | 78 | Female | 6/8/2021 | 6/15/2021 | Dr. Dean | Dr. Foster | Chronic Kidney Disease progression | Dialysis initiation | Stable after starting dialysis | History of diabetes, Chronic Kidney Disease | Initiated on dialysis | Nephrology follow-up in 1 week | Medication compliance, appropriate diet | End-Stage Renal Disease | Stable at discharge | Antihypertensives, erythropoiesis-stimulating agents, phosphate binders. | Low | Moderate | Severity based on condition ‘Chronic Kidney Disease progression’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of diabetes, Chronic Kidney Disease. |
| Noah Barnes | 48 | Male | 8/1/2021 | 8/8/2021 | Dr. Ramirez | Dr. Hughes | Bell’s Palsy | Corticosteroids, Physical therapy | Slow return of facial movement | No significant medical history | Managed with corticosteroids and physical therapy | Neurology follow-up in 1 month | Facial muscle exercises, medication compliance | Bell’s Palsy | Improving at discharge | Prescribed corticosteroids, antivirals. | Low | Moderate | Severity based on condition ‘Bell’s Palsy’. Readmission probability based on discharge condition ‘Improving at discharge’ and no significant medical history. |
| Emily Foster | 34 | Female | 1/22/2021 | 1/27/2021 | Dr. Adams | Dr. Barnes | Appendicitis | Appendectomy | Excellent recovery post-surgery | No significant medical history | Underwent routine open appendectomy | Follow-up with surgeon in 2 weeks | Wound care, report any fever or wound discharge | Acute appendicitis | Stable at discharge | Prescribed painkillers and absorption. | Low | Moderate | Severity based on condition ‘Appendicitis’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant medical history. |
| Ethan Johnson | 45 | Male | 3/21/2021 | 4/5/2021 | Dr. Roberts | Dr. Edwards | Colon cancer | Resection of colon cancer, start of adjuvant chemotherapy | Disease under control, tolerated chemo well | No significant past medical history | Complete tumor resection achieved with histology confirming margins | Oncologist follow-up in 2 weeks | Healthy diet, regular exercise, medication compliance | Colon cancer stage III | Stable at discharge | Prescribed chemotherapeutics, antiemetics. | Low | Low | Severity based on condition ‘Colon cancer’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant past medical history. |
| Sophia James | 24 | Female | 11/5/2021 | 11/15/2021 | Dr. Jacobs | Dr. Willis | Severe Asthma Attack | Intravenous corticosteroids, nebulizer treatments | Breathing eased, symptoms improved | Lifetime Asthma | Hospitalized for acute asthma management | Pulmonary follow-up in 1 week | Avoid asthma triggers, regular use of control medication | Acute severe asthma attack, Asthma | Stable at discharge | Inhalers, oral corticosteroids for a short course. | Low | Moderate | Severity based on condition ‘Severe Asthma Attack’. Readmission probability based on discharge condition ‘Stable at discharge’ and lifetime asthma. |
| Jacob Owens | 58 | Male | 10/7/2021 | 10/14/2021 | Dr. Griffin | Dr. Patterson | Peptic ulcer disease | Proton pump inhibitors, H. pylori eradication | Symptoms improved significantly | No significant past medical history | Received treatment for H. pylori and proton pump inhibitors | Gastroenterology follow-up in 1 month | Avoid NSAIDs, alcohol, spicy foods; take medications with meals | Peptic ulcer disease | Stable at discharge | Prescribed proton-pump inhibitors. | Low | Low | Severity based on condition ‘Peptic ulcer disease’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant past medical history. |
| Layla Tyler | 63 | Female | 8/16/2021 | 8/28/2021 | Dr. Ellis | Dr. Foster | Congestive Heart Failure | Diuretics, vasodilators, beta-blockers | Symptoms improved with stabilization | Hypertension | Adjusted medication regimen; patient education about fluid intake and weight monitoring | Cardiology follow-up in 4 weeks | Medication compliance, daily weight, low sodium diet | Congestive Heart Failure | Stable at discharge | Prescribed diuretics, vasodilators, beta-blockers. | Low | Moderate | Severity based on condition ‘Congestive Heart Failure’. Readmission probability based on discharge condition ‘Stable at discharge’ and hypertension. |
| Max Peters | 46 | Male | 3/12/2021 | 3/18/2021 | Dr. King | Dr. Howard | Pneumothorax | Chest tube insertion | Chest re-expanded successfully | No significant past medical history | Underwent chest tube insertion for pneumothorax | Pulmonary follow-up in 2 weeks | Avoid heavy lifting, short flights for 2 weeks | Spontaneous Pneumothorax | Stable at discharge | Analgesics, follow up as directed. | Low | Low | Severity based on condition ‘Pneumothorax’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant past medical history. |
| Harper Davis | 71 | Female | 5/30/2021 | 6/6/2021 | Dr. Ross | Dr. Holland | COPD Exacerbation | Bronchodilators, steroids | Breathing improved noticeably | COPD, ex-smoker | Managed with nebulized bronchodilators and oral steroids | Pulmonary follow-up in 2 weeks | Smoking cessation, use inhalers as instructed | COPD exacerbation | Stable at discharge | Inhalers, oral steroid taper. | Low | Moderate | Severity based on condition ‘COPD Exacerbation’. Readmission probability based on discharge condition ‘Stable at discharge’ and COPD, ex-smoker history. |
| Thomas Mitchell | 79 | Male | 5/10/2021 | 5/21/2021 | Dr. Barrett | Dr. Osborne | Heart failure | Diuretics, beta-blockers, ACE inhibitors | Condition improved significantly with management | History of ischemic heart disease, hypertension | Managed with heart failure medications, fluid restriction | Cardiology follow-up in 2 weeks | Low salt diet, fluid restriction, medication compliance | Congestive heart failure | Stable at discharge | Furosemide, lisinopril, carvedilol. | Low | Moderate | Severity based on condition ‘Heart failure’. Readmission probability based on discharge condition ‘Stable at discharge’ and history of ischemic heart disease, hypertension. |
| Emily Ross | 43 | Female | 2/14/2021 | 2/21/2021 | Dr. Hamilton | Dr. Jenkins | Cholecystitis | Cholecystectomy | Recovery without complications | No significant past medical history | Underwent laparoscopic cholecystectomy | Surgery follow-up in 2 weeks | Gradual increase in diet, wound care | Cholecystitis | Stable at discharge | Analgesics, wound care recommendations. | Low | Low | Severity based on condition ‘Cholecystitis’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant past medical history. |
| Oliver Hall | 27 | Male | 7/18/2021 | 7/22/2021 | Dr. Washington | Dr. Murray | Meningitis | Antibiotics, steroids | Symptoms resolved notably | No significant past medical history | Managed with IV antibiotics and supportive care | Neurology follow-up in 2 weeks | Rest, hydration, antibiotic compliance | Meningitis | Stable at discharge | Continuation of oral antibiotics and analgesics. | Low | Low | Severity based on condition ‘Meningitis’. Readmission probability based on discharge condition ‘Stable at discharge’ and no significant past medical history. |
| Abigail Jackson | 65 | Female | 12/1/2021 | 12/10/2021 | Dr. Jenkins | Dr. Thompson | Stroke | Thrombolytic therapy, rehabilitation | Partial resolution of deficits | Hypertension, diabetes | Underwent IV thrombolysis and rehabilitation | Neurology and rehabilitation follow-up in 1 month | Physiotherapy, medication compliance, lifestyle modifications | Ischemic stroke | Moderate impairment at discharge | Antihypertensives, antidiabetics, anticoagulation. | Low | Moderate | Severity based on condition ‘Stroke’. Readmission probability based on moderate impairment at discharge and history of hypertension, diabetes. |
| Jackson Perez | 54 | Male | 6/30/2021 | 7/6/2021 | Dr. Adams | Dr. Collins | Peptic Ulcer Disease | Proton pump inhibitors, H. pylori eradication | Symptoms markedly improved | Past history of smoking, alcohol use | Managed with proton pump inhibitors and H. pylori eradication therapy | Gastroenterology follow-up in 4 weeks | Medication compliance, lifestyle modification, stop alcohol and smoking | Peptic Ulcer Disease | Stable at discharge | Antibiotics for H.pylori, PPIs. | Low | Moderate | Severity based on condition ‘Peptic Ulcer Disease’. Readmission probability based on stable condition at discharge and past history of smoking, alcohol use. |
| Sophia Kline | 31 | Female | 2/2/2021 | 2/7/2021 | Dr. Bailey | Dr. Bell | Pyelonephritis | IV antibiotics followed by oral antibiotics therapy | Symptoms resolved significantly | No significant past medical history | Managed with IV antibiotics followed by switch to oral | Primary care follow-up in 2 weeks | Hydration, avoid delaying urination, antibiotic compliance | Pyelonephritis | Stable at discharge | Oral antibiotics to complete 14 days course. | Low | Low | Severity based on condition ‘Pyelonephritis’. Readmission probability based on stable condition at discharge and no significant past medical history. |
| Grayson Walker | 32 | Male | 3/18/2021 | 3/25/2021 | Dr. Rodriguez | Dr. Webb | Appendicitis | Appendectomy | Excellent recovery with no complications | No significant medical history | Underwent appendectomy without complications | Surgery follow-up in 2 weeks | Resume normal diet gradually, wound care, report any fever | Appendicitis | Stable at discharge | Analgesics. | Low | Moderate | Severity based on condition ‘Appendicitis’. Readmission probability based on stable condition at discharge and no significant medical history. |
| Aria Harper | 73 | Female | 11/12/2021 | 11/30/2021 | Dr. Snyder | Dr. Walsh | Heart failure | Diuretics, lifestyle modification | Symptoms improved notably | History of Hypertension, Diabetes | Managed with diuretics and lifestyle modification advice | Cardiology follow-up in 1 month | Weight monitoring, low salt diet, exercise, medication compliance | Congestive Heart Failure | Stable at discharge | Prescribed diuretics, ACE inhibitors, and beta-blockers | Low | Moderate | Severity based on condition ‘Heart failure’. Readmission probability based on stable condition at discharge and history of Hypertension, Diabetes. |
References
- Gilbert, A.; Marciniak, M.; Rodero, C.; Lamata, P.; Samset, E.; Mcleod, K. Generating Synthetic Labeled Data from Existing Anatomical Models: An Example with Echocardiography Segmentation. IEEE Trans. Med. Imaging 2021, 40, 2783–2794. [Google Scholar] [CrossRef] [PubMed]
- Aouedi, O.; Sacco, A.; Piamrat, K.; Marchetto, G. Handling Privacy-Sensitive Medical Data With Federated Learning: Challenges and Future Directions. IEEE J. Biomed. Health Inform. 2022, 27, 790–803. [Google Scholar] [CrossRef]
- Elbadawi, M.; Li, H.; Basit, A.W.; Gaisford, S. The role of artificial intelligence in generating original scientific research. Int. J. Pharm. 2024, 652, 123741. [Google Scholar] [CrossRef] [PubMed]
- Van Nooten, J.; Daelemans, W. Improving Dutch Vaccine Hesitancy Monitoring via Multi-Label Data Augmentation with GPT-3.5. In Proceedings of the 13th Workshop on Computational Approaches to Subjectivity, Sentiment, & Social Media Analysis, Toronto, ON, Canada, 14 July 2023; Available online: https://openai.com/blog/chatgpt (accessed on 21 April 2024).
- Zhou, S.; Zhang, Y. DATLMedQA: A data augmentation and transfer learning based solution for medical question answering. Appl. Sci. 2021, 11, 11251. [Google Scholar] [CrossRef]
- Hämäläinen, P.; Tavast, M.; Kunnari, A. Evaluating Large Language Models in Generating Synthetic HCI Research Data: A Case Study. In Proceedings of the Conference on Human Factors in Computing Systems, Hamburg, Germany, 23–28 April 2023; Association for Computing Machinery: New York, NY, USA, 2023. [Google Scholar] [CrossRef]
- Lu, Q.; Dou, D.; Nguyen, T.H. Textual Data Augmentation for Patient Outcomes Prediction. In Proceedings of the 2021 IEEE international conference on bioinformatics and biomedicine (BIBM), Houston, TX, USA, 9–12 December 2021. [Google Scholar] [CrossRef]
- Bird, J.J.; Pritchard, M.G.; Fratini, A.; Ekart, A.; Faria, D.R. Synthetic Biological Signals Machine-Generated by GPT-2 Improve the Classification of EEG and EMG through Data Augmentation. IEEE Robot. Autom. Lett. 2021, 6, 3498–3504. [Google Scholar] [CrossRef]
- Amin-Nejad, A.; Ive, J.; Velupillai, S. Exploring Transformer Text Generation for Medical Dataset Augmentation. In Proceedings of the Twelfth Language Resources and Evaluation Conference, Marseille, France, 11–16 May 2020; Available online: https://github.com/tensorflow/tensor2tensor (accessed on 21 April 2024).
- Thamsen, B.; Yevtushenko, P.; Gundelwein, L.; Setio, A.A.A.; Lamecker, H.; Kelm, M.; Schafstedde, M.; Heimann, T.; Kuehne, T.; Goubergrits, L. Synthetic Database of Aortic Morphometry and Hemodynamics: Overcoming Medical Imaging Data Availability. IEEE Trans. Med. Imaging 2021, 40, 1438–1449. [Google Scholar] [CrossRef] [PubMed]
- Ruksakulpiwat, S.; Kumar, A.; Ajibade, A. Using ChatGPT in Medical Research: Current Status and Future Directions. J. Multidiscip. Health 2023, 16, 1513–1520. [Google Scholar] [CrossRef]
- Mahuli, S.A.; Rai, A.; Mahuli, A.V.; Kumar, A. Application ChatGPT in conducting systematic reviews and meta-analyses. Br. Dent. J. 2023, 235, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Geng, Y.; Du, Y.; Westerman, B.; Wang, D.; Ma, C.; Vallejo, J.J.G. Utilizing ChatGPT to select literature for meta-analysis shows workload reduction while maintaining a similar recall level as manual curation. medRxiv 2023. [Google Scholar] [CrossRef]
- De Angelis, L.; Baglivo, F.; Arzilli, G.; Privitera, G.P.; Ferragina, P.; Tozzi, A.E.; Rizzo, C. ChatGPT and the rise of large language models: The new AI-driven infodemic threat in public health. Front. Public Health 2023, 11, 1166120. [Google Scholar] [CrossRef]
- Reddy, S. Evaluating large language models for use in healthcare: A framework for translational value assessment. Inform. Med. Unlocked 2023, 41, 101304. [Google Scholar] [CrossRef]
- Alberts, I.L.; Mercolli, L.; Pyka, T.; Prenosil, G.; Shi, K.; Rominger, A.; Afshar-Oromieh, A. Large language models (LLM) and ChatGPT: What will the impact on nuclear medicine be? Eur. J. Nucl. Med. 2023, 50, 1549–1552. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Bhattacharya, M.; Pal, S.; Lee, S.; Chakraborty, C. ChatGPT and large language models in orthopedics: From education and surgery to research. J. Exp. Orthop. 2023, 10, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. ChatGPT Utility in Healthcare Education, Research, and Practice: Systematic Review on the Promising Perspectives and Valid Concerns. Healthcare 2023, 11, 887. [Google Scholar] [CrossRef]
- Lim, S.; Schmälzle, R. Artificial intelligence for health message generation: An empirical study using a large language model (LLM) and prompt engineering. Front. Commun. 2023, 8, 1129082. [Google Scholar] [CrossRef]
- Waisberg, E.; Ong, J.; Kamran, S.A.; Masalkhi, M.; Zaman, N.; Sarker, P.; Lee, A.G.; Tavakkoli, A. Bridging artificial intelligence in medicine with generative pre-trained transformer (GPT) technology. J. Med. Artif. Intell. 2023, 6, 13. [Google Scholar] [CrossRef]
- Maddigan, P.; Susnjak, T. Chat2VIS: Generating Data Visualizations via Natural Language Using ChatGPT, Codex and GPT-3 Large Language Models. IEEE Access 2023, 11, 45181–45193. [Google Scholar] [CrossRef]
- Lengerich, B.J.; Bordt, S.; Nori, H.; Nunnally, M.E.; Aphinyanaphongs, Y.; Kellis, M.; Caruana, R. LLMs Understand Glass-Box Models, Discover Surprises, and Suggest Repairs. arXiv 2023, arXiv:2308.01157. [Google Scholar]
- Sharma, A.; Devalia, D.; Almeida, W.; Patil, H.; Mishra, A. Statistical Data Analysis using GPT3: An Overview. In Proceedings of the 2022 IEEE Bombay Section Signature Conference (IBSSC), Mumbai, India, 8–10 December 2022; IEEE: Piscataway, NJ, USA, 2022. [Google Scholar]
- Espejel, J.L.; Ettifouri, E.H.; Alassan, M.S.Y.; Chouham, E.M.; Dahhane, W. GPT-3.5, GPT-4, or BARD? Evaluating LLMs reasoning ability in zero-shot setting and performance boosting through prompts. Nat. Lang. Process. J. 2023, 5, 100032. [Google Scholar] [CrossRef]
- de Kok, T. Generative LLMs and Textual Analysis in Accounting: (Chat)GPT as Research Assistant? 2023. Available online: https://ssrn.com/abstract=4429658 (accessed on 21 April 2024).
- Yenduri, G.; Srivastava, G.; Maddikunta, P.K.R.; Jhaveri, R.H.; Wang, W.; Vasilakos, A.V.; Gadekallu, T.R. Generative Pre-trained Transformer: A Comprehensive Review on Enabling Technologies, Potential Applications, Emerging Challenges, and Future Directions. arXiv 2023, arXiv:2305.10435. [Google Scholar] [CrossRef]
- Sufi, F.K.; Alsulami, M.; Gutub, A. Automating Global Threat-Maps Generation via Advancements of News Sensors and AI. Arab. J. Sci. Eng. 2022, 48, 2455–2472. [Google Scholar] [CrossRef]
- Sufi, F. Social Media Analytics on Russia–Ukraine Cyber War with Natural Language Processing: Perspectives and Challenges. Information 2023, 14, 485. [Google Scholar] [CrossRef]
- Sufi, F.K.; Razzak, I.; Khalil, I. Tracking Anti-Vax Social Movement Using AI-Based Social Media Monitoring. IEEE Trans. Technol. Soc. 2022, 3, 290–299. [Google Scholar] [CrossRef]
- Sufi, F.K.; Khalil, I. Automated Disaster Monitoring From Social Media Posts Using AI-Based Location Intelligence and Sentiment Analysis. IEEE Trans. Comput. Soc. Syst. 2022. [Google Scholar] [CrossRef]
- Sufi, F.K. AI-SocialDisaster: An AI-based software for identifying and analyzing natural disasters from social media. Softw. Impacts 2022, 13, 100319. [Google Scholar] [CrossRef]
- Sufi, F.K. A decision support system for extracting artificial intelligence-driven insights from live twitter feeds on natural disasters. Decis. Anal. J. 2022, 5, 100130. [Google Scholar] [CrossRef]
- Sufi, F.K.; Alsulami, M. Automated Multidimensional Analysis of Global Events with Entity Detection, Sentiment Analysis and Anomaly Detection. IEEE Access 2021, 9, 152449–152460. [Google Scholar] [CrossRef]
- Sufi, F. Algorithms in Low-Code-No-Code for Research Applications: A Practical Review. Algorithms 2023, 16, 108. [Google Scholar] [CrossRef]
- Balaji, S.; Magar, R.; Jadhav, Y.; Farimani, A.B. GPT-MolBERTa: GPT Molecular Features Language Model for molecular property prediction. arXiv 2023, arXiv:2310.03030. [Google Scholar]
- Hu, Y.; Mai, G.; Cundy, C.; Choi, K.; Lao, N.; Liu, W.; Lakhanpal, G.; Zhou, R.Z.; Joseph, K. Geo-knowledge-guided GPT models improve the extraction of location descriptions from disaster-related social media messages. Int. J. Geogr. Inf. Sci. 2023, 37, 2289–2318. [Google Scholar] [CrossRef]
- Maimaiti, M.; Liu, Y.; Luan, H.; Sun, M. Data augmentation for low-resource languages NMT guided by constrained sampling. Int. J. Intell. Syst. 2021, 37, 30–51. [Google Scholar] [CrossRef]
- Suhaeni, C.; Yong, H.-S. Mitigating Class Imbalance in Sentiment Analysis through GPT-3-Generated Synthetic Sentences. Appl. Sci. 2023, 13, 9766. [Google Scholar] [CrossRef]
- Romero-Sandoval, M.; Calderón-Ramírez, S.; Solís, M. Using GPT-3 as a Text Data Augmentator for a Complex Text Detector. In Proceedings of the 2023 IEEE 5th International Conference on BioInspired Processing (BIP), San Carlos, Alajuela, Costa Rica, 28–30 November 2023; IEEE: Piscataway, NJ, USA, 2023; pp. 1–6. [Google Scholar] [CrossRef]
- Cohen, S.; Presil, D.; Katz, O.; Arbili, O.; Messica, S.; Rokach, L. Enhancing social network hate detection using back translation and GPT-3 augmentations during training and test-time. Inf. Fusion 2023, 99, 101887. [Google Scholar] [CrossRef]
- Rebboud, Y.; Lisena, P.; Troncy, R. Prompt-based Data Augmentation for Semantically-Precise Event Relation Classification. In Proceedings of the 2023 IEEE 5th International Conference on BioInspired Processing (BIP), San Carlos, Alajuela, Costa Rica, 28–30 November 2023; Available online: http://ceur-ws.org (accessed on 21 April 2024).
- Grasler, I.; Preus, D.; Brandt, L.; Mohr, M. Efficient Extraction of Technical Requirements Applying Data Augmentation. In Proceedings of the ISSE 2022–2022 8th IEEE International Symposium on Systems Engineering, Vienna, Austria, 24–26 October 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022. [Google Scholar] [CrossRef]
- Singh, C.; Askari, A.; Caruana, R.; Gao, J. Augmenting interpretable models with large language models during training. Nat. Commun. 2023, 14, 7913. [Google Scholar] [CrossRef]
- Modzelewski, A.; Sosnowski, W.; Wilczynska, M.; Wierzbicki, A. DSHacker at SemEval-2023 Task 3: Genres and Persuasion Techniques Detection with Multilingual Data Augmentation through Machine Translation and Text Generation. In Proceedings of the 17th International Workshop on Semantic Evaluation (SemEval-2023), Toronto, ON, Canada, 13–14 July 2023; Available online: https://semeval.github.io/SemEval2023/ (accessed on 21 April 2024).
- Hong, X.-S.; Wu, S.-H.; Tian, M.; Jiang, J. CYUT at the NTCIR-16 FinNum-3 Task: Data Resampling and Data Augmentation by Generation. In Proceedings of the 16th NTCIR Conference on Evaluation of Information Access Technologies, Tokyo, Japan, 14–17 June 2022; Available online: https://huggingface.co/docs/transformers/main (accessed on 21 April 2024).
- Khatri, S.; Iqbal, M.; Ubakanma, G.; van der Vliet-Firth, S. SkillBot: Towards Data Augmentation using Transformer language model and linguistic evaluation. In Proceedings of the 2022 International Conference on Human-Centered Cognitive Systems, HCCS 2022, Shanghai, China, 17–18 December 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022. [Google Scholar] [CrossRef]
- Vogel, L.; Flek, L. Investigating Paraphrasing-Based Data Augmentation for Task-Oriented Dialogue Systems. In Lecture Notes in Computer Science (including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2022; pp. 476–488. [Google Scholar] [CrossRef]
- Casula, C.; Tonelli, S.; Kessler, F.B. Generation-Based Data Augmentation for Offensive Language Detection: Is It Worth It? In Proceedings of the 17th Conference of the European Chapter of the Association for Computational Linguistics, Dubrovnik, Croatia, 2–6 May 2023; Available online: https://github.com/dhfbk/annotators-agreement-dataset (accessed on 21 April 2024).
- Pouran, A.; Veyseh, B.; Dernoncourt, F.; Min, B.; Nguyen, T.H. Generating Complement Data for Aspect Term Extraction with GPT-2. In Proceedings of the Third Workshop on Deep Learning for Low-Resource Natural Language Processing, Virtual, 14 July 2022. [Google Scholar]
- D’Sa, A.G.; Illina, I.; Fohr, D.; Klakow, D.; Ruiter, D. Exploring Conditional Language Model Based Data Augmentation Approaches for Hate Speech Classification. In Lecture Notes in Computer Science (including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2021; pp. 135–146. [Google Scholar] [CrossRef]
- Meyer, S.; Elsweiler, D.; Ludwig, B.; Fernandez-Pichel, M.; Losada, D.E. Do We Still Need Human Assessors’ Prompt-Based GPT-3 User Simulation in Conversational AI. In Proceedings of the 4th Conference on Conversational User Interfaces, Glasgow, UK, 26–28 July 2022; ACM International Conference Proceeding Series; Association for Computing Machinery: New York, NY, USA, 2022. [Google Scholar] [CrossRef]
- Queiroz Abonizio, H.; Barbon Junior, S. Pre-trained Data Augmentation for Text Classification. In Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2020; pp. 551–565. [Google Scholar] [CrossRef]
- Tapia-Téllez, J.M.; Escalante, H.J. Data Augmentation with Transformers for Text Classification. In Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2020; pp. 247–259. [Google Scholar] [CrossRef]
- Hassani, H.; Silva, E.S. The Role of ChatGPT in Data Science: How AI-Assisted Conversational Interfaces Are Revolutionizing the Field. Big Data Cogn. Comput. 2023, 7, 62. [Google Scholar] [CrossRef]
- Nouri, N. Data Augmentation with Dual Training for Offensive Span Detection. In Proceedings of the 2022 Conference of the North American Chapter of the Association for Computational Linguistics: Human Language Technologies, Seattle, DC, USA, July 2022. [Google Scholar]
- Bayer, M.; Kaufhold, M.-A.; Buchhold, B.; Keller, M.; Dallmeyer, J.; Reuter, C. Data augmentation in natural language processing: A novel text generation approach for long and short text classifiers. Int. J. Mach. Learn. Cybern. 2022, 14, 135–150. [Google Scholar] [CrossRef] [PubMed]
- Anaby-Tavor, A.; Carmeli, B.; Goldbraich, E.; Kantor, A.; Kour, G.; Shlomov, S.; Tepper, N.; Zwerdling, N. Do Not Have Enough Data? Deep Learning to the Rescue! Proc. AAAI Conf. Artif. Intell. 2020, 34, 7383–7390. [Google Scholar] [CrossRef]
- Quteineh, H.; Samothrakis, S.; Sutcliffe, R. Textual Data Augmentation for Efficient Active Learning on Tiny Datasets. In Proceedings of the 2020 Conference on Empirical Methods in Natural Language Processing (EMNLP), Online, 16–20 November 2020; Available online: https://www.snorkel.org/ (accessed on 21 April 2024).
- Veyseh, A.P.B.; Van Nguyen, M.; Min, B.; Nguyen, T.H. Augmenting Open-Domain Event Detection with Synthetic Data from GPT-2. In Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2021; pp. 644–660. [Google Scholar] [CrossRef]
- Sawai, R.; Paik, I.; Kuwana, A. Sentence augmentation for language translation using gpt-2. Electronics 2021, 10, 3082. [Google Scholar] [CrossRef]
- Pellicer, L.F.A.O.; Ferreira, T.M.; Costa, A.H.R. Data augmentation techniques in natural language processing. Appl. Soft Comput. 2023, 132, 109803. [Google Scholar] [CrossRef]
- Chang, Y.; Zhang, R.; Pu, J. I-WAS: A Data Augmentation Method with GPT-2 for Simile Detection. In Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2023; pp. 265–279. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, W.; Cheng, L.; Ye, H. Diverse and High-Quality Data Augmentation Using GPT for Named Entity Recognition. In Communications in Computer and Information Science; Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2023; pp. 272–283. [Google Scholar] [CrossRef]
- Nakamoto, R.; Flanagan, B.; Yamauchi, T.; Dai, Y.; Takami, K.; Ogata, H. Enhancing Automated Scoring of Math Self-Explanation Quality Using LLM-Generated Datasets: A Semi-Supervised Approach. Computers 2023, 12, 217. [Google Scholar] [CrossRef]
- Jansen, B.J.; Jung, S.-G.; Salminen, J. Employing large language models in survey research. Nat. Lang. Process. J. 2023, 4, 100020. [Google Scholar] [CrossRef]
- Joon, J.; Chung, Y.; Kamar, E.; Amershi, S. Increasing Diversity While Maintaining Accuracy: Text Data Generation with Large Language Models and Human Interventions. arXiv 2023, arXiv:2306.04140. [Google Scholar]
- Borisov, V.; Leemann, T.; Seßler, K.; Haug, J.; Pawelczyk, M.; Kasneci, G. Deep Neural Networks and Tabular Data: A Survey. IEEE Trans. Neural Networks Learn. Syst. 2022, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Acharya, A.; Singh, B.; Onoe, N. LLM Based Generation of Item-Description for Recommendation System. In Proceedings of the 17th ACM Conference on Recommender Systems, RecSys 2023, Singapore, 18–22 September 2023; Association for Computing Machinery, Inc.: New York, NY, USA, 2023; pp. 1204–1207. [Google Scholar] [CrossRef]
- Narayan, A.; Chami, I.; Orr, L.; Ré, C. Can Foundation Models Wrangle Your Data? Proc. Vldb Endow. 2022, 16, 738–746. [Google Scholar] [CrossRef]
- Borisov, V.; Seßler, K.; Leemann, T.; Pawelczyk, M.; Kasneci, G. Language Models are Realistic Tabular Data Generators. arXiv 2022, arXiv:2210.06280. [Google Scholar]
- Lee, M. A Mathematical Interpretation of Autoregressive Generative Pre-Trained Transformer and Self-Supervised Learning. Mathematics 2023, 11, 2451. [Google Scholar] [CrossRef]
- Alahmar, A.; Mohammed, E.; Benlamri, R. Application of data mining techniques to predict the length of stay of hospitalized patients with diabetes. In Proceedings of the 2018 International Conference on Big Data Innovations and Applications, Barcelona, Spain, 6–8 August 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 38–43. [Google Scholar] [CrossRef]
- Sufi, F.K. AI-GlobalEvents: A Software for analyzing, identifying and explaining global events with Artificial Intelligence. Softw. Impacts 2022, 11, 100218. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).