Abstract
Background/Objectives: Reasons for long-term stays in intensive care units (ICUs) include various critical conditions, prolonged weaning with post-extubation dysphagia (PED), as well as the mere presence of a tracheal cannula. In an interprofessional QM project, medicine, nursing, physiotherapy, speech and language therapy (SLT), and occupational therapy work together to reduce the length of stay (LOS) in ICUs. SLT focuses on tracheal cannula management (TCM) and PED. The primary aim of SLT is fast and safe decannulation and thereby the reduction in LOS. Methods: Two SOPs for dealing with PED patients and for structured TCM were developed for this purpose and were both implemented in a postoperative ICU, together with a SLT staff increase. To compare the effects on the intervention group (IG, n = 54), a historical control (HC, n = 58) group was created through a retrospective data analysis. We screened all patients from ICU (n = 5605), including those with tracheostomy, and analyzed them during their ICU stay. Results: Clinically relevant results were observed for the mean time in days of tracheostomy in those who could be decannulated (HC = 43.43, IG = 23.8; d = 0.99) and, even more importantly, for LOS in days (HC = 33.41, IG = 23.8; d = 0.48). Conclusions: The integration of SLT in ICU care is feasible and helps to reduce the time to decannulation and LOS.
1. Introduction
Patients who remain in intensive care units (ICUs) for extended periods face a high disease burden and increased risks of illness and death. Factors contributing to extended ICU stays include multiple organ failure, unstable circulation, delirium, prolonged ventilator weaning with post-extubation dysphagia (PED), and the presence of a tracheal cannula (TC), which can complicate transfers to other wards or care facilities due to their limited capacity to manage such cases [1]. Tracheostomized ICU patients experience an even greater burden, with longer hospital and ICU stays, higher mortality rates, and a greater chance of being discharged to a care facility. These patients often have severe underlying conditions, and tracheostomy may prompt a reassessment of patient goals and advanced care planning [2]. Strong respiratory function, demonstrated by powerful cough reflexes and efficient secretion control, is reported as a fundamental predictive factor for successful decannulation [3]. Ideally, decannulation should occur during or at the conclusion of the patient’s stay in the ICU [4] to minimize the occurrence of further complications.
A recent national anesthesiology guideline recommends multiprofessional team efforts in order to improve the quality of treatment and shorten the LOS. However, the guideline focuses on the effects of mobilization and thereby on the physiotherapeutic role in the treatment process [5]. A national [6] and an international [7] guideline of intensive care societies both recommend broad staff education and strongly recommend to make speech and language therapy (SLT) available for ICU up to the point that “all patients with a tracheostomy must have communication and swallowing needs assessed by an SLT” [7]. Especially, SLT and there competencies in tracheostomy and dysphagia management [8] could provide additional input for intensive care treatment quality beyond their ancestral field of neurologic rehabilitation [9] and have already demonstrated positive effects on aspects such as pneumonia prevention and length of stay (LOS) in quality management (QM) projects [10,11]. Furthermore, there is evidence that the mere application of structured decannulation pathway is able reduce the total time to decannulation [12].
Therefore, in order to not only capture the best moment to discharge the patient, but also to facilitate the discharge process, we started an interprofessional QM project (IQ-ICU). This project integrates the work of medicine, nursing, physiotherapy, SLT, and occupational therapy to improve the quality of treatment, reduce morbidity, and reduce the length of stay (LOS) in the ICU, with each profession providing their respective [8]. SLT focuses primarily on the aspects of tracheal cannula management and dysphagia. In order to evaluate the effect of IQ-ICU, we retrospectively analyzed patient data one year prior to the implementation phase and compared this historic control group (HC) to an intervention group (IG) one year after the full start of the implemented QM project.
In this paper we will focus on the SLT part of the whole IQ project and its effect on endpoints associated with tracheostomy and dysphagia (IQ-ICU-SLT). The primary aim of the SLT was the fastest possible decannulation with maximum patient safety, and with that ideally a reduction in LOS on ICU.
2. Materials and Methods
Before the start of the IQ-ICU project, there were no specific SOPs dealing with dysphagia or tracheal cannula management for intensive care medicine. Decisions regarding oral feeding or decannulation were based on clinical experience mostly of the nurses and physicians. Only physiotherapy was part of the daily routine. SLT was only available upon specific requests of the ICU physicians in exceptional cases.
Therefore, we decided to implement a comprehensive concept with specific measurements for SLT treatment, focusing on cannula management and dysphagia, in a postoperative ICU of a German university hospital that operates with up to 43 beds.
2.1. Descrition of the Overall IQ-ICU Concept
No changes were made regarding the general intensive medical care approach of the physicians. Staffing levels in the therapy area were doubled so that therapy sessions could take place twice a day. An interprofessional Standard Operation Procedure (SOP) for the collaboration of physiotherapy, SLT, and occupational therapy was created. Furthermore, depending on the LOS, a daily interprofessional therapy conference and weekly goal meetings were introduced. The integration of family engagement was executed wherever feasible, and adequate supplies (for example, video endoscopes for flexible evaluation of swallowing and to detect readiness for decannulation) were procured (compare Figure 1 for the key points of the IQ-ICU project). Pharyngeal electrical stimulation (PES; Phagenesis Ltd., UK) was considered, but since the ICU patients do not necessarily meet the necessary etiologies for its application (in Europe, its neurogenic dysphagia), we decided against PES at the first stage of the IQ-ICU project, even though it showed superior results for faster decannulation [13].
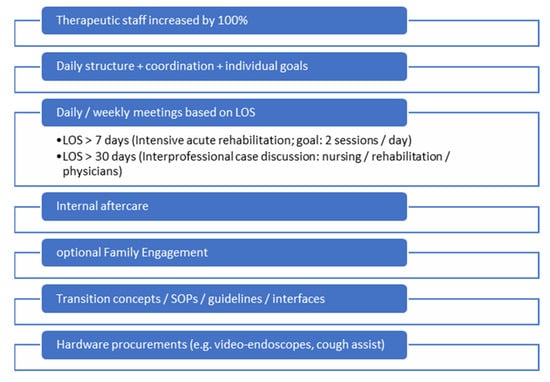
Figure 1.
Key points of the interprofessional quality management framework project.
2.2. Descrition of the SLT Concept
A relevant part of ICU patient care is the dysphagia and tracheostomy management, with essential contributions from the SLT team. The SLT team consisted of +- seven members across the whole intervention period. Two SOPs (the pathways of the SOPs are depicted in Figure 2 and Figure 3) for dealing with PED patients and for structured tracheal cannula management based on international expert recommendations (3) were developed for this purpose by the SLT team in preparation of the project implementation and were both implemented during in a 3-month period at the beginning of 2024. Every team member was trained for the concept. Additionally, all members are qualified for tracheal cannula management and FEES according to the respective curriculums [14,15] that are accepted by national and international expert societies (German Society for Swallowing Disorders and European Society for Swallowing Disorders). SLT diagnostics comprised either clinical dysphagia examinations and/or FEES. SLT treatment targeted airway and swallowing functions and was based on individualized cannula management (uncuffing, stepwise increase in time with a speaking valve, parameter-based and mutual assessment for decannulation readiness), dysphagia therapy, targeted rehabilitative interventions (e.g., muscle strength training, use of cuff assist), compensatory techniques, and diet adaptations. For a complete overview, see Figure 2 and Figure 3. Beyond the SLT treatment concept, precise criteria for decannulation with SLT-specific diagnostic elements were developed and applied as part of the implementation period between pre and post (see Figure 4). These criterial were used in order to assess readiness for decannulation. All of them had to be met before decannulation was performed. The decision to decannulate was made in an interprofessional case discussion. A further SLT treatment goal was to teach the patients self-care competence for their cannula (i.e., self suctioning). In order to put this into practice, there was a planned SLT staff increase from approximately 0.1 to 0.8 full-time employee equivalents. SLT was allocated to tracheal cannula management if the first assessment of general condition indicated readiness for treatment (see Figure 3).
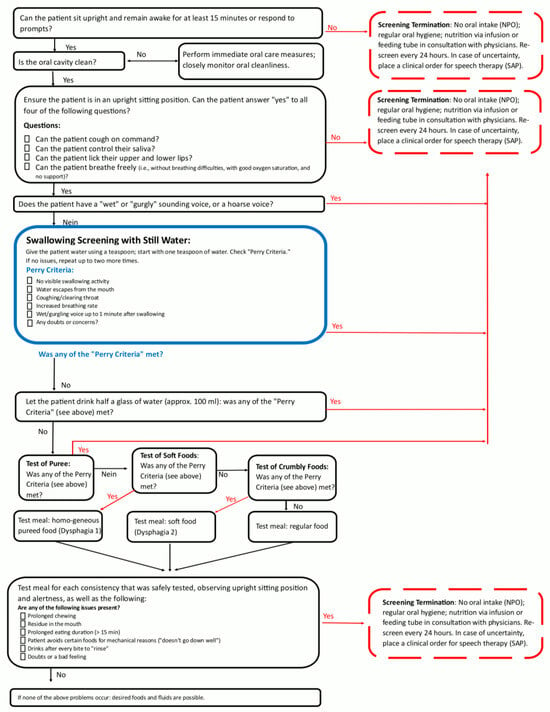
Figure 2.
Swallowing screening for the intensive care units and general wards. Pathway for oral intake or clinical examination by Speech and Language Therapist (part of a standard operation procedure for post-extubation dysphagia), derived from Perry et al. (2001) [16].
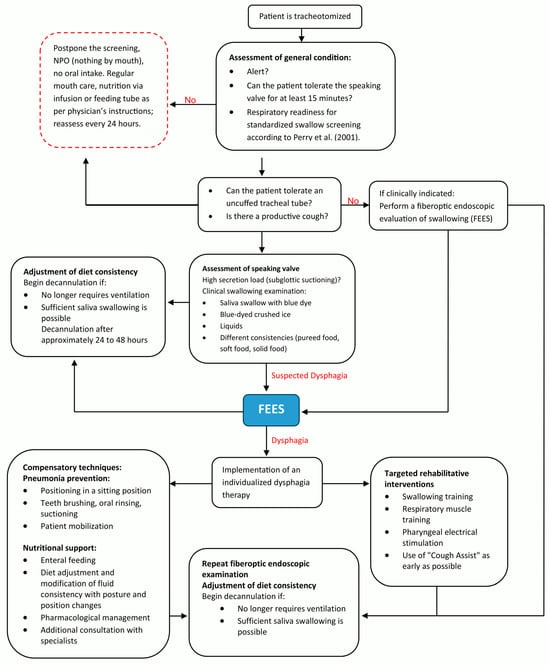
Figure 3.
Pathway of the standard operation procedure for structured tracheal cannula management in ICU with special focus on patients with risk of dysphagia based on international expert recommendations of Likar et al. (2024) [17] and Perry et al. (2001) [16].
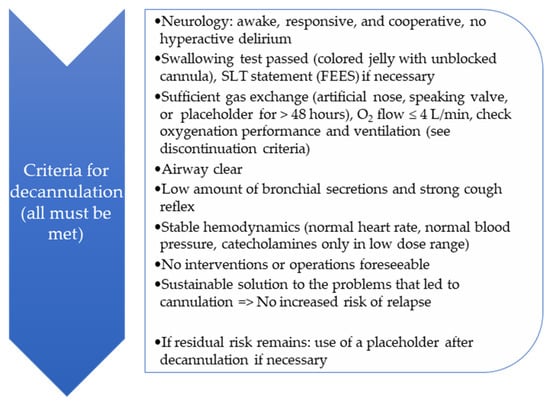
Figure 4.
Criteria for decannulation with SLT-specific diagnostic elements that were applied as part of the implementation period between pre and post. The decision to decannulate was made in an interprofessional case discussion.
2.3. Study Design, Patient Inclusion and Endpoints
As a basis for comparison of the effects on the intervention group (IG), a historical control (HC) group was created through a retrospective data analysis of the year 2023 (Ethics Committee of the Rhineland-Palatinate Chamber of Physicians: 2024-17433). The whole time period of the comparison was across 24 (+3) months in a non-randomized pre-/post study design (see Figure 5). The study is registered with the WHO Register for Clinical Trials (DRKS00036084).
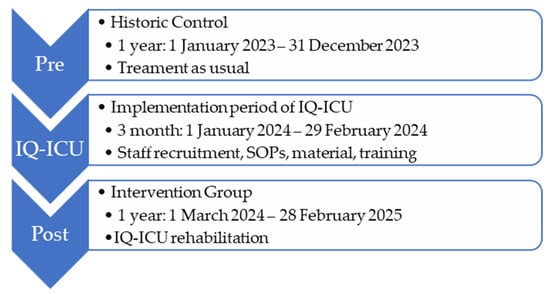
Figure 5.
Pre-post study design with project implementation period between pre and post.
We included all patients who underwent tracheostomy during intensive care stay or later during the hospital stay or who already entered the ICU tracheostomized. No additional exclusion criteria were applied. The primary endpoint of the framework project (IQ-ICU) is a composite endpoint, combining morbidity and the length of stay in ICU. Secondary outcomes were morbidity, amongst many others measured by the Sequential Organ Failure Assessment Score (SOFA, 0–24, organ dysfunction) [18], the Simplified Acute Physiology Score II (SAPS II, 0–163, risk of mortality) [19], the Clinical Frailty Scale (CFS, 0–9, frailty) [20], and functional dependence and independence (Early Rehabilitation Barthel-Index A (−325–0) and B, (0–100) [21], and mortality.
SLT-Specific Aspects of Study Design, Patient Inclusion, and Endpoints
As the SLT-specific primary outcome (P1), we considered the group differences in days with tracheal cannula during the ICU stay. Clinically more relevant, but not solely attributable to SLT, is the LOS in the ICU; hence, we considered it as a further primary, but not SLT-specific, outcome (P2). SLT-specific secondary outcomes were the number of possible safe decannulations during the ICU stay, given SLT in minutes, amount of performed clinical and endoscopic swallowing examinations, and competence of self-care for their cannula (i.e., self-suctioning).
This paper specifically analyzes the SLT-related outcomes. In further sub-analyses, the relationship between tracheal cannula management and its potential influence on the LOS will be investigated.
2.4. Data Acquisition, Aggregation, and Statistic Analyses
Data were collected from two online patient data management systems by two members of the study group (I.N. and L.M.). All patient data were entered into one pseudonymized Excel sheet table. After several mutual meetings and data curation, it resulted in a clear-to-analyze version. All further statistical calculations (either with Microsoft Excel 2016, Remont, WA, USA, or SPSS v.29, IBM, Armonk, NY, USA) are based on this final version of the raw data table. For inferential statistics of metric variables, we calculated two-sample t-tests (two-sided significance) and X2-tests for nominal variables. Additionally, for the most relevant outcomes, effect sizes according to Cohen’s D [22] were provided.
3. Results
After assessment of eligibility of n = 5605 patients (HC n = 2647; IG n = 2958), we enrolled 115 tracheostomized patients during the investigation period who came from a broad-spectrum, postoperative intensive care unit, allocated n = 112 (2%) to IQ-ICU-SLT (HC n = 54, IG n = 58), and analyzed these cases regarding the SLT-specific endpoints (see Figure 6 for details of enrollment).
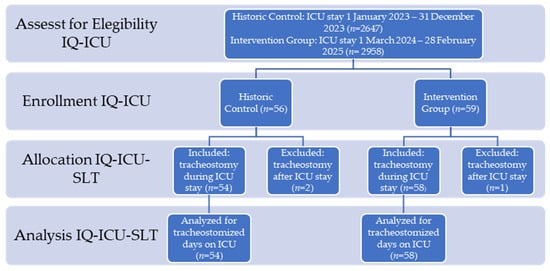
Figure 6.
Transparent reporting of trial enrollment and analysis adopted from CONSORT.
3.1. Patient Characteristics After Enrollment
Amongst the most prominent etiologies were heart-vascular surgery and plastic operations on vessels, surgery of the gastrointestinal tract, and organ replacement therapy.
General patient characteristics across both groups such as the mean age in years (HC = 65.43, IG = 67.75) and BMI (HC = 27.0, IG = 28.06) appear to be comparable, although sex is unequally distributed, with fewer females in the HC (f = 29.6%). Regarding clinical characteristics, both group samples show typical values in ICU-related scores. The risk of morbidity (according to SOFA max) was higher in the HC but not unequally distributed for all other scores. In 20.4% of patients in the HC and in 10.3% of patients in the IG (15.18% across both groups), the complication of apoplexy emerged. Mortality across groups was not unequal. Regarding types of tracheostomies, there were more surgical (primary and secondary) tracheostomies in the IG. This difference also resulted in an earlier performed tracheostomy or first day with a TC in ICU (patients with prior tracheostomy) in the IG (mean of days: HC = 13.93, IG = 9.71) All the most relevant patient and clinical characteristics can be viewed in Table 1.

Table 1.
Patient characteristics (n = 112) with means, standard deviations (SDs), and frequencies during the ICU stay for both groups (historic control, HC, and intervention group, IG,) with analysis of potential differences in distribution.
3.2. Results for SLT-Specific Primary and Secondary Study Endpoints
Across all patients, there is a significant effect for the primary outcome of SLT, resulting in a reduction in the mean number of days with a cannula in the ICU by approximately eight days (HC = 18.85 → IG = 10.31), with a medium effect size (d = 0.54) (see Figure 7/Table 2).
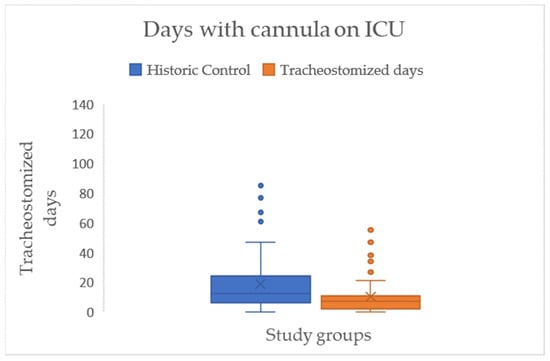
Figure 7.
Boxplots with median (-), mean (x), interquartile range (IQR box), whiskers (1.5 × IQR), and outliers (°) for tracheostomized period (days with cannula) during the ICU stay for both study groups.

Table 2.
Primary SLT-specific (P1) and general (P2) results, as well as secondary outcomes, between the historic control (HC) and intervention group (IG) with differences, statistical significance (* denotes p ≤ 0.05), and effect sizes (ESs) for the most relevant outcomes.
This is linked to the LOS in the ICU, which shows a comparable effect size (d = 0.48) and, on average, a significant reduction in mean days between the two groups by approximately twelve days (HC = 33.74 → IG = 21.94) (see Figure 8/Table 2).
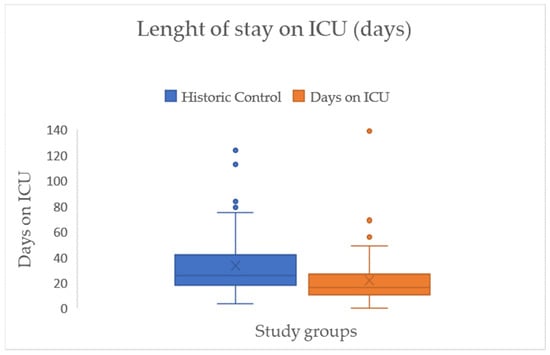
Figure 8.
Boxplots with median (-), mean (x), interquartile range (IQR box), whiskers (1.5 × IQR), and outliers (°) for length of stay in ICU in days across both study groups.
To demonstrate the interdependence of days with a cannula and LOS in the ICU, we calculated linear regression, with cannulated days in the ICU as the predictor variable for LOS in the ICU. The coefficient of determination showed that 77% (p < 0.001) of the variation in LOS can be explained by days with a cannula in the ICU, while the rest is explained by some other variables not included (Figure 9).
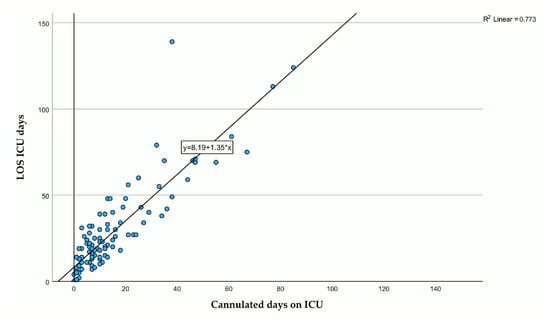
Figure 9.
Scatterplot of residence time in days of the tracheal cannula (x-axis, independent variable) and length of stay in the ICU in days (y-axis, dependent variable) with line of origin, regression line, regression model, and information about goodness of fit.
In order to look at the effect on SLT and decannulation alone, we analyzed the subgroup of patients who were decannulated during their ICU stay. We therefore used the dates of successful attempts. Regarding the frequency of decannulation, we found no significant difference between the two groups. In the HC, there were seven (12.96%) successfully decannulations, and in the IG, there were five (8.62%) (see Figure 10/Table 2).
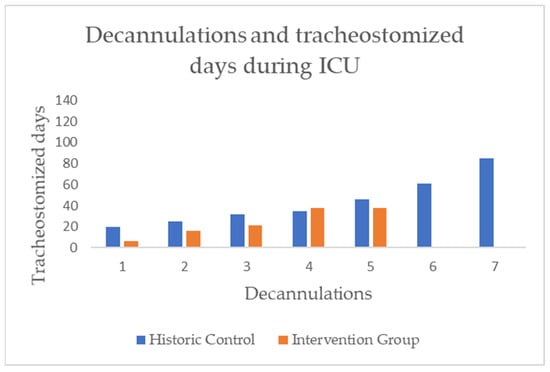
Figure 10.
Bar chart of individual tracheostomized days in ICU until decannulation took place, differentiated by group.
In the next step of the analysis, we focused on the residence time of cannulas in those who could be decannulated. A large effect size (d = 0.99), but no statistical significance, was demonstrated for the time difference in days with a cannula between the two groups (HC = 43.43, IG = 23.85) (see Figure 11/Table 2).
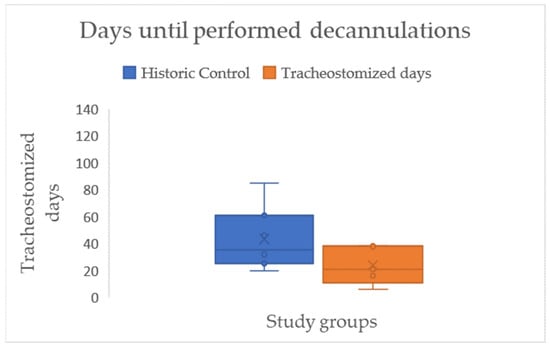
Figure 11.
Boxplots with median (-), mean (x), interquartile range (IQR box), whiskers (1.5 × IQR), and outliers (°) for the residence time of cannulas, in days, amongst those who were decannulated during the ICU stay, differentiated by study groups.
In order to evaluate the developed criteria for assessing readiness for decannulation, and as a safety measure, we counted the number of unsuccessful decannulation attempts and compared the two groups in this respect. In total, there were four unsuccessful decannulation attempts, two in each group. A slightly different distribution was found between the subgroups in which the unsuccessful attempts occurred. Within the IG, where there was a specific protocol to assess readiness for decannulation (see Figure 4), there were no unsuccessful attempts within the subgroup of patients who underwent a final successful decannulation. Unsuccessful attempts occurred only in the subgroup that could not be decannulated during their stay in the ICU. For a full overview, see Figure 12.
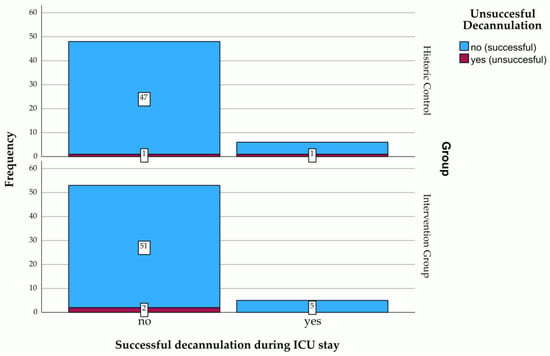
Figure 12.
Stacked bar chart of unsuccessful decannulation attempts in those who were either finally decannulated during their ICU stay or not, differentiated by study groups. Figures represent the frequency of each category.
The final part of the analysis is related to SLT, its integration into the ICU setting, and its qualitative impact on the project. SLT consisted of individualized cannula management and targeted rehabilitative interventions (see Figure 2 and Figure 3). The allocation of SLT to the dedicated patients was possible for about 65% in the IG, and this was significantly higher and more intensive (d = 0.739) than the only 9% of patients in the HC who received SLT during their ICU stay. This also impacted the diagnostic component of patient care and led to significantly more clinical dysphagia examinations (CDAs), as well as Flexible Endoscopic Evaluations of Swallowing. On the other hand, it did not lead to more patients who were fed by mouth (HC = 11.11% vs. IG = 13.79%) (see Table 2).
Regarding the competence of self-care for their cannula (i.e., self-suctioning), we unfortunately cannot report results, since it was not possible to gather reliable information from the electronic patient documentation systems on this topic.
4. Discussion
After implementation of the IQ-ICU project, we were able to demonstrate a mean reduction in days tracheostomized in the ICU by eight days and a reduction in LOS by twelve days for all patients. Concerning those who could be decannulated during their ICU stay, highly clinically relevant results with a large effect size (d = 0.99) could be demonstrated by a mean reduction in the residence time of the tracheal cannula by 20 days. Due to the small sample of performed decannulations (HC n = 7, IG n = 5), this did not reach statistical significance.
The mean reduction in the residence time of the tracheal cannula is in line with a comparable pre–post study investigating the effect of a tracheostomy pathway [12]. Also, for the direct group comparison of those who could be decannulated in the ICU, the observed difference of 20 days indicates that there are similar effects to those described after the introduction of early rehabilitation concepts (30 days) [23].
Our result that the decannulation process can be sped up but that the number of patients who can be decannulated remains stable has also been shown by others [23]. No more decannulations are possible, which can mean that there might be some “iatrogenic” barrier for possible decannulations that cannot be “bypassed” by traditional means of tracheostomy management (see Section 4.2, Ideas for Future Research).
As demonstrated by the regression model, which exhibited an explained variance of 77%, the days with a cannula can be regarded as a robust predictor of length of stay (LOS). This is noteworthy despite the fact that it functions as a surrogate parameter for a variety of clinical conditions. Hence, it seems very likely that efforts to reduce the residence time of tracheal cannulas will directly translate into reduced LOS in the ICU. This perspective is distinctive in that research has either sought to predict decannulation success [24,25] or LOS [26].
The evaluation of the developed criteria for assessing readiness for decannulation revealed no significant group difference with respect to frequency of unsuccessful attempts to decannulate (HC: 3.7% vs. IG: 3.45%). However, a slightly different distribution was found between the subgroups in which these unsuccessful attempts occurred. Within the IG, there were no unsuccessful attempts in the subgroup of patients who underwent a final successful decannulation during their ICU stay. Due to the limited number of cases (two in each group), it seems inappropriate to interpret these results with respect to the chosen decannulation parameters. With regard to the consequences of this non-finding, please refer to the considerations set out in Section 4.2.
When focusing on the feasibility of integrating SLT in the ICU setting, we were able to allocate SLT to 65% of dedicated patients in the IG. This resulted in significantly more treatment (d = 0.739) and also impacted the diagnostic component of patient care. with significantly more clinical dysphagia examinations (CDAs), as well as Flexible Endoscopic Evaluations of Swallowing. Hence, we conclude that this is evidence for the practical applicability of respective guideline recommendations [6,7]. On the other hand, this did not lead to more patients who were fed by mouth (HC = 11.11% vs. IG = 13.79%), although this cannot be considered a primary goal for ICUs and can always be addressed in subsequent normal wards.
4.1. Limitations
First of all, limitations arise from the pre–post study design. A randomized controlled trial would have been a more desirable study design, but it was not feasible to implement two different projects in the same ICU ward with the same staff simultaneously. Also the retrospective data analysis for the HC bears risks of bias. For instance, a strong source of bias would have been data from the COVID-19 period. Consequently, the retrospective analysis was constrained to the post-COVID-19 period, with sufficient temporal distance.
The fact that no more decannulations were possible in the IG than in the HC, as we had expected, could have been influenced by the differences in the tracheostomy types between the two groups. There were significantly more surgical tracheostomies in the IG (12) than in the HC, contributing to more efforts for decannulation (e.g., the necessary surgical closure of the stoma) [27]. A potential source of bias, contributing to a shorter LOS in the IG, and hence a reverse effect to the one previously discussed, could be the mean difference in time of tracheostomy (first day with a TC in the ICU) of four days between the two groups (HC = 13.93 → IG = 9.7). This is because there is relevant evidence that found early tracheostomy to result in fewer ICU days [28]. However, given that both groups can be classified as “early tracheostomies” and that we identified both an inhibiting and a promoting potential bias within the same group (i.e., our IG), it is anticipated that these biases will offset each other.
4.2. Considerations and Ideas for Future Research
For a better understanding of the effect of SLT on the reduction in time until decannulation in the IG, we will perform a detailed case study of these patients as a next step.
In order to keep up with state-of-the-art research, we want to implement the Standardized Endoscopic Swallowing Evaluation for Tracheostomy Decannulation (SESETD) protocol [29] in the IQ-ICU-SLT SOP.
As explained, due to uncertainty regarding whether ICU patients would meet the necessary etiologies for PES application (i.e., neurogenic dysphagia in Europe), we decided against PES at the first stage of the IQ-ICU project. Nevertheless, its proven usefulness in speeding up the decannulation process [13] makes it an interesting tool. Since across both of our groups, the complication of apoplexy emerged in 15.18%, with an associated high risk of neurogenic and post-extubation dysphagia [30], we consider PES a potential future means of PED prevention. Hence, PES could be integrated into the weaning from ventilation process during the early intubation phase in order to reduce PED and extubation failure/or necessary tracheostomies, with the potential to further shorten the LOS in the ICU. Therefore, includable etiologies (e.g., stroke, brain tumor, traumatic brain injury) or clinical symptoms indicating neurogenic dysphagia (e.g., tolerance of endotracheal tubes, saliva pooling) that potentially would benefit from PES application in general ICU wards have to be identified. By this, the PED could be reduced, and this might result in either a lower necessity for tracheostomy overall or more decannulations that can be immediately performed in the ICU and not later in course of rehabilitation.
The demonstrated feasibility of implementing SLT in tracheostomy management in an ICU and the accompanying positive results of IQ-ICU-SLT should be acknowledged by professional societies and associations and lead to clear recommendations for the inclusion of SLT in ICUs, as already demonstrated in one guideline [7].
5. Conclusions
This project demonstrated that interprofessional teamwork between medicine, nursing, physiotherapy, SLT, and occupational therapy in a general ICU is feasible and can improve the quality of treatment and reduce morbidity, as well as LOS in the ICU. Integrating SLT and its expertise into intensive care will likely lead to benefits such as shorter times to decannulation and safer decannulation processes, since necessary diagnostics like FEES can be performed more often and by specially trained staff. This also enhances patients’ quality of life.
Surely, the demonstrated positive effects on the reduction in LOS cannot be solely attributed to SLT input on treatment. However, the demonstrated reduction in days until possible and safe decannulation can be considered an indicator of the effective integration of SLT into this process in general ICUs.
Author Contributions
Conceptualization, M.B., J.K., U.B. and H.M.; methodology, M.B., J.K., U.B. and H.M.; validation, M.B., I.N., J.K., L.M., U.B. and R.K.; formal analysis, J.K., M.B., R.K., L.M. and I.N.; investigation, I.N., L.M. and M.B.; resources, M.B. and U.B.; data curation, I.N., L.M., J.K. and M.B.; writing—original draft preparation, J.K. and M.B.; writing—review and editing, J.K., M.B., R.K. and U.B.; visualization, J.K.; supervision, M.B., U.B., H.M. and J.K.; project administration, M.B., J.K., U.B. and H.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the State Chamber of Physicians of Rhineland-Palatinate (No.: 2024-17433; 21 February 2024), and is registered with the WHO register for Clinical Trials (DRKS00036084).
Informed Consent Statement
The approval of the ethics committee covers the data analysis for the historical control group and the intervention group as they were gathered as a part of the daily clinical routine. Hence, no individual patient consent was obtained. Publication of these anonymized data is accepted, especially when part of aggregated data.
Data Availability Statement
The data are not publicly available due to restrictions on the use of clinical patient data. Furthermore, a public accessibility is not covered by the given ethics vote. In this, data sharing is limited to inner institutional research partners.
Acknowledgments
All clinical colleagues are acknowledged for their daily work in the clinical routine!
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Yu, W.; Dan, L.; Cai, J.; Wang, Y.; Wang, Q.; Zhang, Y.; Wang, X. Incidence of post-extubation dysphagia among critical care patients undergoing orotracheal intubation: A systematic review and meta-analysis. Eur. J. Med. Res. 2024, 29, 444. [Google Scholar] [CrossRef]
- Vargas, M.; Battaglini, D.; Antonelli, M.; Corso, R.; Frova, G.; Merli, G.; Petrini, F.; Ranieri, M.V.; Sorbello, M.; Di Giacinto, I.; et al. Follow-up short and long-term mortalities of tracheostomized critically ill patients in an Italian multi-center observational study. Sci. Rep. 2024, 14, 2319. [Google Scholar] [CrossRef]
- Calderone, A.; Filoni, S.; De Luca, R.; Corallo, F.; Calapai, R.; Mirabile, A.; Caminiti, F.; Conti-Nibali, V.; Quartarone, A.; Calabrò, R.S.; et al. Predictive Factors of Successful Decannulation in Tracheostomy Patients: A Scoping Review. J. Clin. Med. 2025, 14, 3798. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Saran, S.; Baronia, A.K. The practice of tracheostomy decannulation—A systematic review. J. Intensive Care 2017, 5, 38. [Google Scholar] [CrossRef] [PubMed]
- Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin e.V. (DGAI). Lagerungstherapie und Mobilisation von Kritisch Erkrankten auf Intensivstationen. 2024. Available online: https://register.awmf.org/de/leitlinien/detail/001-015 (accessed on 24 September 2025).
- Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI). Empfehlung zur Struktur und Ausstattung von Intensivstationen 2022 (Erwachsene). Available online: https://www.divi.de/publikationen/intensivstationen (accessed on 15 October 2025).
- The Short-Life Standards and Guidelines Working Party of the UK National Tracheostomy Safety Project. Guidance for: Tracheostomy Care. 2023. Available online: https://www.ficm.ac.uk/sites/ficm/files/documents/2021-11/2020-08%20Tracheostomy_care_guidance_Final.pdf (accessed on 3 October 2025).
- Rivelsrud, M.C.; Hartelius, L.; Speyer, R.; Løvstad, M. Qualifications, professional roles and service practices of nurses, occupational therapists and speech-language pathologists in the management of adults with oropharyngeal dysphagia: A Nordic survey. Logop. Phoniatr. Vocol. 2024, 49, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Langton-Frost, N.; Brodsky, M.B. Speech-language pathology approaches to neurorehabilitation in acute care during COVID-19: Capitalizing on neuroplasticity. PM&R 2022, 14, 217–226. [Google Scholar] [CrossRef]
- Burek, A.; Büßelberg, N.; Stanschus, S. Qualitätssicherungs-Projekt zur Prävention von Aspirationspneumonien in der Akutversorgung von Schlaganfallpatienten mit Dysphagie. Forum Logopädie 2008, 22, 8–25. [Google Scholar]
- Martino, R.; Foley, N.; Bhogal, S.; Diamant, N.; Speechley, M.; Teasell, R. Dysphagia after stroke: Incidence, diagnosis, and pulmonary complications. Stroke 2005, 36, 2756–2763. [Google Scholar] [CrossRef]
- Smith, K.A.; Matthews, T.W.; Dubé, M.; Spence, G.; Dort, J.C. Changing practice and improving care using a low-risk tracheotomy clinical pathway. JAMA Otolaryngol.–Head Neck Surg. 2014, 140, 630–634. [Google Scholar] [CrossRef]
- Dziewas, R.; Stellato, R.; van der Tweel, I.; Walther, E.; Werner, C.J.; Braun, T.; Citerio, G.; Jandl, M.; Friedrichs, M.; Notzel, K.; et al. Pharyngeal electrical stimulation for early decannulation in tracheotomised patients with neurogenic dysphagia after stroke (PHAST-TRAC): A prospective, single-blinded, randomised trial. Lancet Neurol. 2018, 17, 849–859. [Google Scholar] [CrossRef]
- Ledl, C.; Frank, U.; Dziewas, R.; Arnold, B.; Bähre, N.; Betz, C.S.; Braune, S.; Deitmer, T.; Diesener, P.; Fischer, A.S.; et al. Curriculum “Trachealkanülenmanagement in der Dysphagietherapie”. Der Nervenarzt 2024, 95, 342–352. [Google Scholar] [CrossRef] [PubMed]
- Dziewas, R.; Glahn, J.; Helfer, C.; Ickenstein, G.; Keller, J.; Lapa, S.; Ledl, C.; Lindner-Pfleghar, B.; Nabavi, D.; Prosiegel, M.; et al. FEES für neurogene Dysphagien. Der Nervenarzt 2014, 85, 1006–1015. [Google Scholar] [CrossRef] [PubMed]
- Perry, L. Screening swallowing function of patients with acute stroke. Part two: Detailed evaluation of the tool used by nurses. J. Clin. Nurs. 2001, 10, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Likar, R.; Aroyo, I.; Bangert, K.; Degen, B.; Dziewas, R.; Galvan, O.; Grundschober, M.T.; Köstenberger, M.; Muhle, P.; Schefold, J.C.; et al. Management of swallowing disorders in ICU patients—A multinational expert opinion. J. Crit. Care 2024, 79, 154447. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure: On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Le Gall, J.R.; Lemeshow, S.; Saulnier, F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993, 270, 2957–2963. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. Can. Med. Assoc. J. 2005, 173, 489–495. [Google Scholar] [CrossRef]
- Schönle, P.W. The Early Rehabilitation Barthel Index—An early rehabilitation-oriented extension of the Barthel Index. Die Rehabil. 1995, 34, 69–73. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences, 2nd ed.; Lawrence Erlbaum: Hillsdale, MI, USA, 1988. [Google Scholar]
- Zivi, I.; Valsecchi, R.; Maestri, R.; Maffia, S.; Zarucchi, A.; Molatore, K.; Vellati, E.; Saltuari, L.; Frazzitta, G. Early Rehabilitation Reduces Time to Decannulation in Patients With Severe Acquired Brain Injury: A Retrospective Study. Front. Neurol. 2018, 9, 559. [Google Scholar] [CrossRef]
- Zaga, C.J.; Milliren, C.E.; McGrath, B.A.; Yang, C.J.; Schiff, B.A.; Warrillow, S.J.; Henningfeld, J.K.; Gregson, P.A.; Bedwell, J.R.; Beaudet, K.M.; et al. Predictors of Decannulation Success in Tracheostomy: A 10-Year Analysis of the Global Tracheostomy Collaborative Database. Otolaryngol.–Head Neck Surg. 2025, 173, 1138–1148. [Google Scholar] [CrossRef]
- Añón, J.M. Can we predict the duration of the decannulation process? Med. Intensiv. (Engl. Ed.) 2012, 36, 529–530. [Google Scholar] [CrossRef] [PubMed]
- Stieger, A.; Schober, P.; Venetz, P.; Andereggen, L.; Bello, C.; Filipovic, M.G.; Luedi, M.M.; Huber, M. Predicting admission to and length of stay in intensive care units after general anesthesia: Time-dependent role of pre- and intraoperative data for clinical decision-making. J. Clin. Anesth. 2025, 103, 111810. [Google Scholar] [CrossRef] [PubMed]
- Pandit, A.; Swami, G.; Kumar, K.D. Comparative Study of Percutaneous Dilatational Tracheostomy and Conventional Surgical Tracheostomy in Critically Ill Adult Patients. Indian J. Otolaryngol. Head Neck Surg. 2023, 75, 1568–1572. [Google Scholar] [CrossRef]
- Chorath, K.; Hoang, A.; Rajasekaran, K.; Moreira, A. Association of Early vs Late Tracheostomy Placement With Pneumonia and Ventilator Days in Critically Ill Patients: A Meta-analysis. JAMA Otolaryngol.—Head Neck Surg. 2021, 147, 450–459. [Google Scholar] [CrossRef]
- Dziewas, R.; Warnecke, T.; Labeit, B.; Schulte, V.; Claus, I.; Muhle, P.; Brake, A.; Hollah, L.; Jung, A.; von Itter, J.; et al. Decannulation ahead: A comprehensive diagnostic and therapeutic framework for tracheotomized neurological patients. Neurol. Res. Pract. 2025, 7, 18. [Google Scholar] [CrossRef]
- Bertschi, D.; Rotondo, F.; Waskowski, J.; Venetz, P.; Pfortmueller, C.A.; Schefold, J.C. Post-extubation dysphagia in the ICU−a narrative review: Epidemiology, mechanisms and clinical management (Update 2025). Crit. Care 2025, 29, 244. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.