Mandibular Lateral Displacement in Growing Patients: Etiopathogenesis, Prophylaxis, and Early Treatment—A Literature Review
Abstract
1. Introduction
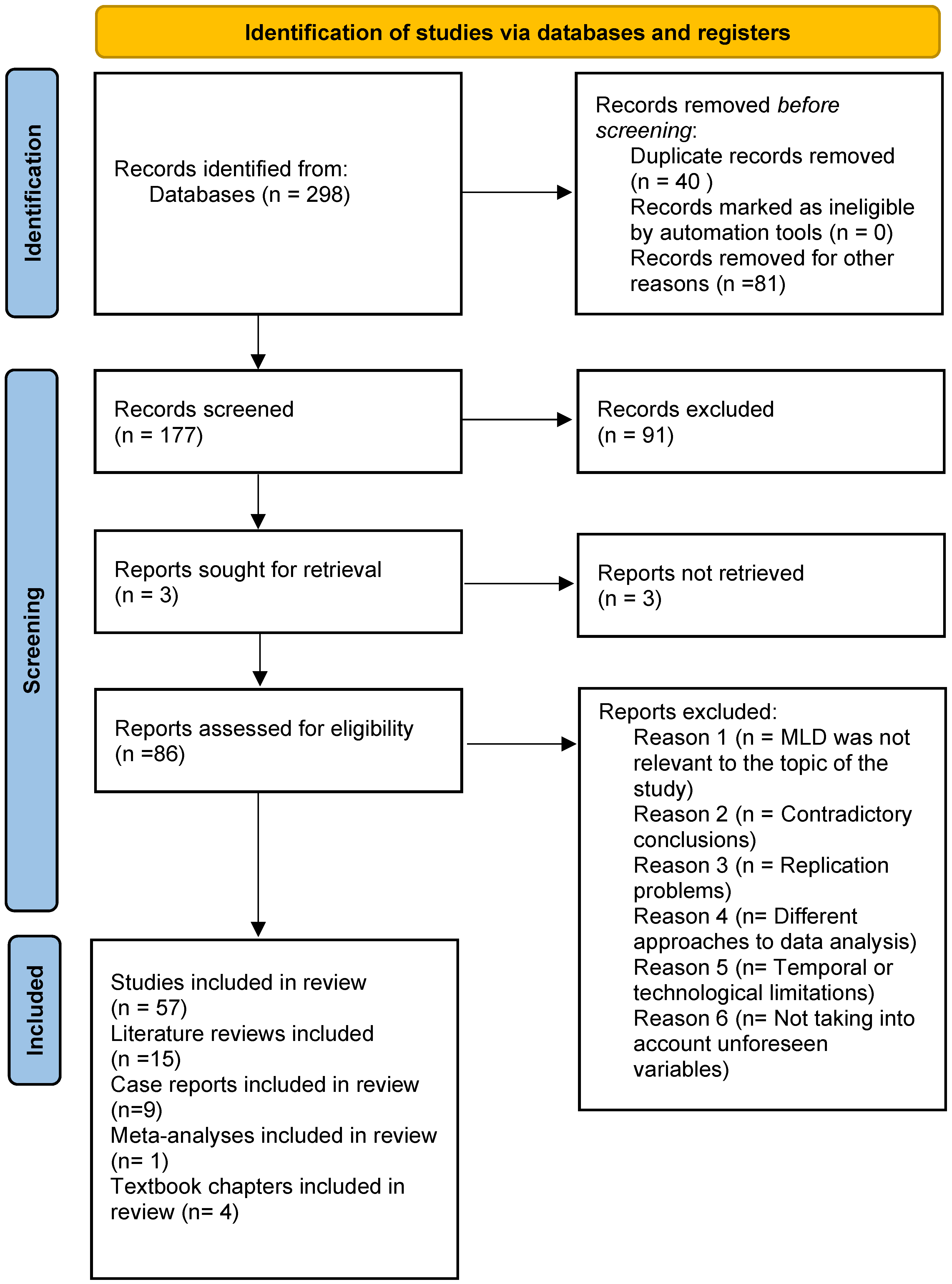
2. Materials and Methods
3. Results and Discussion
3.1. Morphological Characteristics Associated with Mandibular Lateral Deviation (MLD)
- upward inclination of the occlusal plane toward the side of mandibular displacement [28];
- a steeper posterior segment of the occlusal plane on the displacement side compared to the contralateral side [28];
- inclination of the occlusal plane resulting from three-dimensional mandibular displacement toward the side characterized by a smaller vertical dimension [30];
- increased mandibular body length on the side of displacement [29];
- increased effective mandibular length (Condylion–Pogonion) and ramus length (Condylion–Gonion) on the contralateral side relative to the mandibular displacement [29];
3.2. Functional Characteristics Associated with Mandibular Lateral Displacement (MLD)
- Neuromuscular imbalance and asymmetrical muscle function — reduced tone of the masseter muscle on the deviated side compared to the opposite side, accompanied by increased tone of the pterygoid muscles [34,35]. The particularly noteworthy study was conducted by Hao Guan et al. on growing rats with experimentally induced lateral functional mandibular displacement [36]. The induced displacement resulted in atrophy of the masseter and temporalis muscles on the deviated side and hypertrophy on the contralateral side. Moreover, asymmetric decomposition of muscle fiber types and cross-sectional area was observed. The overall body weight of the animals remained stable, indicating an unimpaired ability to feed. The researchers demonstrated that mechanical stimulation affected the expression of regulatory proteins involved in the growth of the temporalis and masseter muscles, causing increased expression of GDF-8 (Growth Differentiation Factor-8) and decreased levels of IGF-1 (Insulin-Like Growth Factor-1) on the deviated side, with opposite effects in the contralateral muscles. After elimination of the mechanical disturbance, the muscles regained their original structure and function, identical to the pre-experimental state. According to the authors, this finding indicates that at the early stage, changes induced by functional mandibular lateral displacement are completely reversible. According to the authors, this finding indicates that at the early stage, changes induced by functional mandibular lateral displacement are completely reversible [36];
- Compensatory displacement of the mandibular condyles within the articular fossae, resulting from anterior translation or tilting of the condylar head on the ipsilateral side [37,38]. This phenomenon was demonstrated by Nerder et al. following the determination of the therapeutic mandibular position using a bite splint [37];
- Temporomandibular joint (TMJ) dysfunction, manifested as abnormalities during mandibular opening and closing. Mandibular displacement occurs not only at the terminal phase of the movement but also throughout its execution [37]. Research by Qi Chen et al. demonstrated the occurrence of acoustic TMJ symptoms (clicking sounds) in MLD patients during the initial and terminal phases of mandibular opening. This observation may suggest concurrent abnormalities in the articular disc [26].
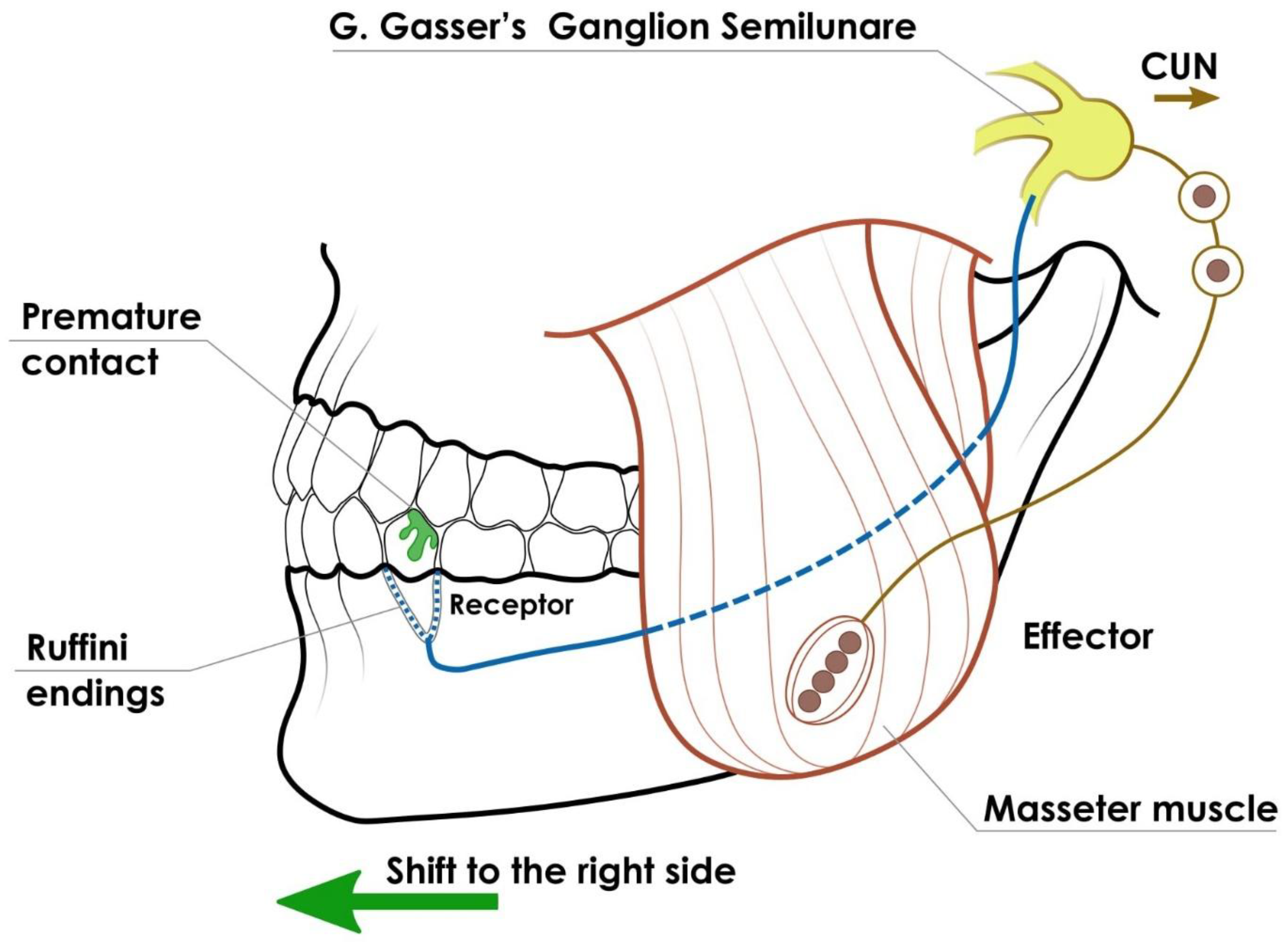
3.3. Etiology of Mandibular Lateral Displacement (MLD)
3.4. Pathogenesis of Mandibular Lateral Displacement (MLD)
3.5. Prevention and Early Treatment of Mandibular Lateral Displacement (MLD)
- 1.
- Grinding of deciduous tooth cusps. After examination with articulating paper, the procedure is performed with a water-cooled diamond bur. In MLD, the palatal cusps of the upper deciduous molars and the buccal cusps of the lower deciduous molars are most often ground on the affected side. Premature contacts should be assessed repeatedly before the procedure and ground gradually. A positive therapeutic effect after selective grinding of premature contacts is reported in 27–64% of cases [33,72,73,74].
- 2.
- Myotherapy. After eliminating premature dental contacts, patients with lateral functional displacement of the mandible are recommended to perform certain exercises. Some of them consist of maximum movements of the mandible in the opposite direction to the disorder and return to the starting position (independent or forced movement with the hand) [75]. In addition, exercises are introduced to prevent mandibular displacement during adduction by stabilizing it in place. The occurrence of dysfunctions related to, among other things, mandibular movements, chewing, and swallowing should be assessed individually. In the event of abnormalities, myofunctional therapy and re-education should be introduced to eliminate these dysfunctions. The exercises should lead to the mandible reaching a resting position in the correct relationship with the midline of the face [26,33,73,74].
- 3.
- Onlays. Several authors have described the use of composite onlays to treat crossbite accompanied by MLD. They are designed to unblock the mandible, inhibit forced lateral movement, and enable proper transverse development of the maxilla by raising the bite [54]. Neto et al. describe a method combining selective grinding of deciduous tooth cusps with the creation of composite occlusal planes to achieve centric occlusion, proper mandibular guidance, and optimal TMJ function. Their use was also intended to ensure bite plane alignment [76]. Tuomo Kantomaa conducted studies on children with crossbite during the deciduous dentition period. He performed composite guiding surfaces on the buccal surface of the upper canine and first or second deciduous molar on the side of the disorder, in combination with grinding premature contacts on deciduous teeth. In most patients, the crossbite was corrected after one month [77]. Unilateral crossbite caused by MLD should be treated during the deciduous dentition stage [78].
- 4.
- Maxillary expansion. In cases where corrective grinding is insufficient, maxillary expansion is often performed first using rapid maxillary expansion (RME) or slow maxillary expansion (SME) [11,79]. Zineb Safi-Eddine et al. describe the frequent need to expand the upper dental arch during MLD treatment [80]. For this purpose, David B. Kennedy et al. point to the possibility of using appliances such as the W-arch, Quad Helix, Expander, Haas, or hyrax screw appliance in the deciduous and early mixed dentition to expand the maxilla. In early permanent dentition, Haas-type palatal expansion appliances with a hyrax or Superscrew are used [11]. In addition, Biega et al. present the effectiveness of Invisalign First aligners in the treatment of MLD [81].
- 5.
- Functional appliances. In the early treatment of MLD, functional appliances are used to influence the teeth, soft tissues, TMJ, and bone tissue. These appliances are made in disocclusion and the most correct position of the mandible in relation to the maxilla, taking into account the sagittal and orbital planes, after obtaining a positive functional test result. Szpinda-Barczyńsa et al. describe the effects of MLD therapy accompanying other malocclusions [82]. Case studies present the effectiveness of MLD treatment using the Klammt functional appliance, which can be used to widen the dental arches [83,84]. The U-bugel activator is also mentioned, which consists of two acrylic plates with occlusal surfaces for the teeth in the lateral sections, cut along the occlusal plane. Its wire elements include two lip arches and loops connecting the upper and lower acrylic plates in the shape of the letter U, which are turned upwards with their convexities. Activation of these loops enables compensatory displacement of the mandible [85]. Removable single-jaw appliances with an acrylic plate are most often used to correct the transverse dimension of the arches, using one or more expansion screws [86].
3.6. Authors’ Perspective
- In the author’s clinical practice, mandibular lateral displacement is a relatively frequent finding, particularly during early stages of craniofacial development. There are no current epidemiological data on its prevalence in the general Polish population or among orthodontic patients
- Early orthodontic intervention is recommended as soon as MLD is diagnosed. In patients with functional mandibular lateral displacement (MLD), the primary therapeutic objective is the elimination of occlusal interferences that prevent symmetrical positioning of the mandible. For this purpose, we use selective grinding of primary teeth, onlays, prosthetic restorations, as well as removable and fixed intraoral and extraoral appliances, taking into account individual indications.
- The treatment of mandibular lateral displacement (MLD) is conducted by an interdisciplinary team comprising an orthodontist, prosthodontist, physiotherapist, and speech therapist.
- In cases of severe morphological MLD, orthodontic treatment alone is often insufficient and requires orthognathic therapy.
4. Conclusions
- 1.
- During the deciduous and mixed dentition stages, early diagnosis of the occlusal asymmetry, identification of its etiology, and initiation of orthodontic intervention are essential.
- 2.
- The diagnosis and management of mandibular lateral displacement should adopt a multidisciplinary, team-based approach.
- 1.
- Standardization of Diagnostic Criteria—Development of clear, evidence-based criteria to differentiate functional from morphological mandibular lateral displacement, integrating clinical, radiological, and functional assessments.
- 2.
- Comparative Treatment Studies—Longitudinal studies comparing different early intervention strategies in children and adolescents to determine the most effective approaches for correcting MLD.
- 3.
- Reversibility and Timing—Assessment of the relationship between intervention timing and MLD reversibility.
- 4.
- Clinical Guidelines and Protocols—Establishment of evidence-based protocols for early detection, prevention, and treatment of MLD.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kochanowski, M.; Rogowska, K.; Dejak, B.D. Prosthetic treatment of temporomandibular disorders and lateral functional mandibular dislocation. Protet. Stomatol. 2021, 71, 343–354. [Google Scholar] [CrossRef]
- Sobieska, E.; Walerzak, M.; Molińska, M. Facial asymmetry–aetiology, classification and diagnostics based on the literature. In Forum Ortodontyczne/Orthodontic Forum; Termedia: Poznań, Poland, 2020; Volume 16, pp. 138–158. [Google Scholar]
- Laskin, D.M.; Greene, C.S.; Hylander, W.L. Temporomandibular Disorders: An Evidence-Based Approach to Diagnosis and Treatment; Quintessence Publishing: Batavia, IL, USA, 2006. [Google Scholar]
- Fuentes, M.A.; Opperman, L.A.; Buschang, P.; Bellinger, L.L.; Carlson, D.S.; Hinton, R.J. Lateral functional shift of the mandible: Part I. Effects on condylar cartilage thickness and proliferation. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Kutin, G.; Hawes, R.R. Posterior cross-bites in the deciduous and mixed dentitions. Am. J. Orthod. 1969, 56, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Severt, T.; Proffit, W. The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. Int. J. Adult Orthod. Orthognath. Surg. 1997, 12, 171–176. [Google Scholar]
- Posselt, U. Studies in the mobility of the human mandible. Acta Odontol. Scand. 1952, 10, 126–129. [Google Scholar]
- Ingervall, B. Retruded contact position of mandible, A comparison between children and adults. Odontol. Reby. 1964, 15, 130–149. [Google Scholar]
- Hodge, L.C., Jr.; Mahan, P.E. A study of mandibular movement from centric occlusion to maximum intercuspation. J. Prosthet. Dent. 1967, 18, 19–30. [Google Scholar] [CrossRef]
- Rieder, C.E. The prevalence and magnitude of mandibular displacement in a survey population. J. Prosthet. Dent. 1978, 39, 324–329. [Google Scholar] [CrossRef]
- Kennedy, D.B.; Osepchook, M. Unilateral posterior crossbite with mandibular shift: A review. J.-Can. Dent. Assoc. 2005, 71, 569. [Google Scholar]
- Thilander, B.; Wahlund, S.; Lennartsson, B. The effect of early interceptive treatment in children with posterior cross-bite. Eur. J. Orthod. 1984, 6, 25–34. [Google Scholar] [CrossRef]
- Schröder, U.; Schröder, I. Early treatment of unilateral posterior crossbite in children with bilaterally contracted maxillae. Eur. J. Orthod. 1984, 6, 65–69. [Google Scholar] [CrossRef]
- Kecik, D.; Kocadereli, I.; Saatci, I. Evaluation of the treatment changes of functional posterior crossbite in the mixed dentition. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Giudice, A.L.; Polizzi, A.; Leonardi, R.; Isola, G. Clinical indications for the diagnosis and treatment of functional posterior crossbite in pediatric population: A narrative review with clinical description. J. Clin. Pediatr. Dent. 2024, 48, 12. [Google Scholar] [CrossRef] [PubMed]
- da Silva Filho, O.G.; Santamaria, M., Jr.; Filho, L.C. Epidemiology of posterior crossbite in the primary dentition. J. Clin. Pediatr. Dent. 2007, 32, 73–78. [Google Scholar] [CrossRef]
- Fushima, K.; Akimoto, S.; Takamot, K.; Kamei, T.; Sato, S.; Suzuki, Y. Incidence of temporomandibular joint disorders in patients with malocclusion. Nihon Ago Kansetsu Gakkai Zasshi 1989, 1, 40–50. [Google Scholar]
- Inui, M.; Fushima, K.; Sato, S. Facial asymmetry in temporomandibular joint disorders. J. Oral Rehabil. 1999, 26, 402–406. [Google Scholar] [CrossRef]
- Brin, I.; Ben-Bassat, Y.; Blustein, Y.; Ehrlich, J.; Hochman, N.; Marmary, Y.; Yaffe, A. Skeletal and functional effects of treatment for unilateral posterior crossbite. Am. J. Orthod. Dentofac. Orthop. 1996, 109, 173–179. [Google Scholar] [CrossRef]
- Hovhannisyan, A.; Kostrzewa-Janicka, J.; Zadurska, M.; Mierzwińska-Nastalska, E. Development and growth of the facial skeleton in individual skeletal classes in the human population. Literature review. In Forum Ortodontyczne/Orthodontic Forum; Termedia: Poznań, Poland, 2018; Volume 14, pp. 48–60. [Google Scholar]
- Wang, Y.C.; Ko, E.W.C.; Huang, C.S.; Chen, Y.R.; Takano-Yamamoto, T. Comparison of transverse dimensional changes in surgical skeletal Class III patients with and without presurgical orthodontics. J. Oral Maxillofac. Surg. 2010, 68, 1807–1812. [Google Scholar] [CrossRef]
- Biedziak, B.; Szarmach, I.; Zadurska, M. (Eds.) Współczesna Diagnostyka Ortodontyczna; Med Tour Press International: Warszawa, Poland, 2025. (In Polish) [Google Scholar]
- Akahane, Y.; Deguchi, T.; Hunt, N.P. Morphology of the temporomandibular joint in skeletal class iii symmetrical and asymmetrical cases: A study by cephalometric laminography. J. Orthod. 2001, 28, 119–128. [Google Scholar] [CrossRef]
- Rahman, M.; Kadir, A.K.M.S.; Akhtar, M. Frequency of Midline Shift, Nose Deviation, Chin Deviation, and Functional Deviation of Jaw in Orthodontic Patient. Rangpur Dent. Coll. J. 2019, 7, 26–29. [Google Scholar]
- Sudhakar, N.; Dinesh, S. Unilateral posterior crossbite-shoot it at sight. A review. J. Dent. Med. Sci. 2013, 12, 47–50. [Google Scholar] [CrossRef]
- Chen, Q.; Mai, Z.H.; Lu, H.F.; Chen, L.; Chen, Z.; Ai, H. Treatment of a mandibular functional shift in an adolescent boy with temporomandibular disorder and crossbites. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 660–673. [Google Scholar] [CrossRef] [PubMed]
- Adly, M.S.; Adly, A.S.; Adly, A.S. Assessment of early orthodontic treatment on functional shifts by telemonitoring mandibular movements using a smart phone. J. Telemed. Telecare 2020, 26, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Ishizaki, K.; Suzuki, K.; Mito, T.; Tanaka, E.M.; Sato, S. Morphologic, functional, and occlusal characterization of mandibular lateral displacement malocclusion. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 454.e1–454.e9. [Google Scholar] [CrossRef] [PubMed]
- Velásquez, R.L.; Coro, J.C.; Londoño, A.; McGorray, S.P.; Wheeler, T.T.; Sato, S. Three-dimensional morphological characterization of malocclusions with mandibular lateral displacement using cone-beam computed tomography. CRANIO® 2018, 36, 143–155. [Google Scholar] [CrossRef]
- Schudy, F.F. Cant of the occlusal plane and axial inclinations of teeth. Angle Orthod. 1963, 33, 69–82. [Google Scholar]
- Kawamoto, H.K.; Kim, S.S.; Jarrahy, R.; Bradley, J.P. Differential diagnosis of the idiopathic laterally deviated mandible. Plast. Reconstr. Surg. 2009, 124, 1599–1609. [Google Scholar] [CrossRef]
- Corte, C.C.D.; Silveira, B.L.d.; Marquezan, M. Influence of occlusal plane inclination and mandibular deviation on esthetics. Dent. Press J. Orthod. 2015, 20, 50–57. [Google Scholar] [CrossRef]
- Sharma, D.S.; Srivastava, S.; Tandon, S. Preventive orthodontic approach for functional mandibular shift in early mixed dentition: A case report. J. Oral Biol. Craniofacial Res. 2019, 9, 209–214. [Google Scholar] [CrossRef]
- Xia, K.; Sun, W.; Yu, L.; Huang, X.; Zhao, Z.; Liu, J. Treatment of the mandibular shift in an adult woman and the diagnostic value of joint space index: A case report. Eur. J. Med. Res. 2020, 25, 50. [Google Scholar] [CrossRef]
- Di Palma, E.; Tepedino, M.; Chimenti, C.; Tartaglia, G.M.; Sforza, C. Effects of the functional orthopaedic therapy on masticatory muscles activity. J. Clin. Exp. Dent. 2017, 9, e886. [Google Scholar] [CrossRef][Green Version]
- Guan, H.; Yonemitsu, I.; Ikeda, Y.; Ono, T. Reversible Effects of Functional Mandibular Lateral Shift on Masticatory Muscles in Growing Rats. Biomedicines 2023, 11, 2126. [Google Scholar] [CrossRef]
- Nerder, P.H.; Bekke, M.; Solow, B. The functional shift of the mandible in unilateral posterior crossbite and the adaptation of the temporomandibular joints: A pilot study. Eur. J. Orthod. 1999, 21, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Rabelo, K.A.; Melo, S.L.S.; Torres, M.G.G.; Peixoto, L.R.; Campos, P.S.F.; Rebello, I.M.C.R.; de Melo, D.P. Assessment of condyle position, fossa morphology, and disk displacement in symptomatic patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 124, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Thilander, B.; Rubio, G.; Pena, L.; de Mayorga, C. Prevalence of temporomandibular dysfunction and its association with malocclusion in children and adolescents: An epidemiologic study related to specified stages of dental development. Angle Orthod. 2002, 72, 146–154. [Google Scholar] [PubMed]
- Nakaminami, T.; Nishio, K.; Miyauchi, S.; Maruyama, T. The effect of posterior crossbite on stomatognathic function. J. Jpn. Soc. Stomatognath. Funct. 1988, 6, 87–96. [Google Scholar]
- Wojtaszek-Lis, J.; Regulski, P.; Laskowska, M.; Zadurska, M. Effects of premature loss of deciduous teeth on the morphology and functions of the masticatory organ. Literature review. In Forum Ortodontyczne/Orthodontic Forum; Termedia: Poznań, Poland, 2018; Volume 14, pp. 29–47. [Google Scholar]
- Tai, K.; Park, J.H.; Ikeda, K.; Nishiyama, A.; Sato, Y. Severe facial asymmetry and unilateral lingual crossbite treated with orthodontics and 2-jaw surgery: 5-year follow-up. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 509–523. [Google Scholar] [CrossRef]
- Chowdhury, M.S.H.; Sultana, N.; Naim, M.A.; Nashrin, T.; Nahar, L. Prevalence of cross bite among the orthodontic patients at a dental unit of Bangladesh. J. Natl. Inst. Neurosci. Bangladesh 2019, 5, 167–171. [Google Scholar] [CrossRef]
- Bishara, S.E.; Burkey, P.S.; Kharouf, J.G. Dental and facial asymmetries: A review. Angle Orthod. 1994, 64, 89–98. [Google Scholar]
- Chambers, D.W.; Zitterkopf, J.G. How people make decisions about whether or not to seek orthodontic care: Upstream in the treatment chain. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 826–831. [Google Scholar] [CrossRef]
- Cheng, J.C.; Au, W.Y. Infantile torticollis: A review of 624 cases. J. Pediatr. Orthop. 1994, 14 6, 802–808. [Google Scholar] [CrossRef]
- Kaur, S. Congenital torticollis and its physiotherapy management. Int. J. Health Sci. Res 2020, 10, 94–101. [Google Scholar]
- Jain, U.; Jain, P.; Patel, A.; Bharti, C.; Kausar, H. Functional Management of Rare Condition of Congenital Muscular Torticollis Precipitated Malocclusion. Saudi J. Dent. Oral Res. 2020, 5, 351–357. [Google Scholar] [CrossRef]
- Bittar, K.C.B. Photogrammetry protocol in babies with congenital torticollis: Part 1–inter-arch intraoral assessment. J. Complex. Health Sci. 2024, 7, 125–133. [Google Scholar] [CrossRef]
- Michalska, A.; Szmurło, M.; Pogorzelska, J.; Szczukocki, M.; Szwilling, Z. Congenital muscular torticollis–an over view of treatment methods. Child Neurol. Dziecięca 2017, 26, 69–74. [Google Scholar] [CrossRef]
- Amat, P. Occlusion, orthodontics and posture: Are there evidences? The example of scoliosis. Int. J. Stomatol. Occlusion Med. 2009, 2, 2–10. [Google Scholar] [CrossRef][Green Version]
- Stirling, A.J.; Howel, D.; Millner, P.A.; Sadiq, S.; Sharples, D.; Dickson, R.A. Late-onset idiopathic scoliosis in children six to fourteen years old. A cross-sectional prevalence study. J. Bone Jt. Surg. 1996, 78, 1330–1336. [Google Scholar] [CrossRef]
- Gault, I. Correlations between orthodontic treatment and posture. J. Dentofac. Anomalies Orthod. 2008, 11, 232–250. [Google Scholar] [CrossRef]
- Saccucci, M.; Tettamanti, L.; Mummolo, S.; Polimeni, A.; Festa, F.; Salini, V.; Tecco, S. Scoliosis and dental occlusion: A review of the literature. Scoliosis 2011, 6, 15. [Google Scholar] [CrossRef]
- Segatto, E.; Lippold, C.; Végh, A. Craniofacial features of children with spinal deformities. BMC Musculoskelet. Disord. 2008, 9, 169. [Google Scholar] [CrossRef]
- Krysiński, Z.; Sójka, A. Objawy dysfunkcji narządu żucia u młodocianych pacjentów z chorobami narządu ruchu–badania wstępne. Protet. Stomatol. 2005, 55, 267–272. [Google Scholar]
- Cabrera-Domínguez, M.E.; Domínguez-Reyes, A.; Pabón-Carrasco, M.; Pérez-Belloso, A.J.; Coheña-Jiménez, M.; Galán-González, A.F. Dental malocclusion and its relation to the podal system. Front. Pediatr. 2021, 9, 654229. [Google Scholar] [CrossRef]
- Nakashima, A.; Nakano, H.; Yamada, T.; Inoue, K.; Sugiyama, G.; Kumamaru, W.; Nakajima, Y.; Sumida, T.; Yokoyama, T.; Mishiama, K.; et al. The relationship between lateral displacement of the mandible and scoliosis. Oral Maxillofac. Surg. 2017, 21, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Laskowska, M.; Olczak-Kowalczyk, D.; Zadurska, M.; Czubak, J.; Czubak-Wrzosek, M.; Walerzak, M.; Tyrakowski, M. Evaluation of a relationship between malocclusion and idiopathic scoliosis in children and adolescents. J. Child. Orthop. 2019, 13, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Huggare, J.; Pirttiniemi, P.; Serlo, W. Head posture and dentofacial morphology in subjects treated for scoliosis. Proc. Finn. Dent. Society. Suom. Hammaslaakariseuran Toim. 1991, 87, 151–158. [Google Scholar]
- Janicki, J.A.; Alman, B. Scoliosis: Review of diagnosis and treatment. Paediatr. Child Health 2007, 12, 771–776. [Google Scholar] [CrossRef]
- Ikemitsu, H.; Zeze, R.; Yuasa, K.; Izumi, K. The relationship between jaw deformity and scoliosis. Oral Radiol. 2006, 22, 14–17. [Google Scholar] [CrossRef]
- Ciuraj, M.; Lipowicz, A.; Graja, K.; Zwolska, P.; Myśliwiec, A. Physiotherapeutic methods of treatment of mandibular distal occlusion and the progress of therapy: A case report. J. Bodyw. Mov. Ther. 2022, 29, 26–32. [Google Scholar] [CrossRef]
- Girard, M.; Leroux, C. Gestion des muscles et des fonctions par le kinésithérapeute dans les traitements orthodontiques et ortho-chirurgicaux. Rééducation oro-myofonctionnelle. L’Orthodontie Française 2015, 86, 95–111. [Google Scholar] [CrossRef]
- Bardellini, E.; Gulino, M.G.; Fontana, S.; Amadori, F.; Febbrari, M.; Majorana, A. Can the Treatment of Dental Malocclusions Affect the Posture in Children? J. Clin. Pediatr. Dent. 2022, 46, 241–248. [Google Scholar] [CrossRef]
- Głowacka, J.; Opydo-Szymaczek, J.; Mehr, K.; Pawlaczyk-Kamieńska, T.; Głowacki, J. Adolescent idiopathic scoliosis and malocclusion—A cross sectional study of female patients without previous orthodontic treatment. Anthropol. Anzeiger Ber. Uber Die Biol.-Anthropol. Lit. 2020, 77, 269–280. [Google Scholar] [CrossRef]
- Sasaki, J.; Hasegawa, S.; Yamamoto, S.; Watanabe, S.; Miyachi, H.; Nagao, T. Relationship between facial asymmetry and positional plagiocephaly analyzed by three-dimensional computed tomography. J. Cranio-Maxillofac. Surg. 2020, 48, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Losee, J.E.; Mason, A.C. Deformational plagiocephaly: Diagnosis, prevention, and treatment. Clin. Plast. Surg. 2005, 32, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Hong, M.; Park, H.S. Analysis of dental compensation in patients with facial asymmetry using cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 493–501. [Google Scholar] [CrossRef]
- Perry, H., Jr. The physiology of mandibular displacement. Angle Orthod. 1960, 30, 51–69. [Google Scholar]
- Boman, V.R. Roentgenographic study of the move ment of the mandible from physiological rest position to occlusion of teeth. Ph.D Thesis, Northwestern University, Evanston, IL, USA, 1948. [Google Scholar]
- Garg, D.; Singh, D.; Vichare, S.; Saneja, R. Craniofacial Imaging and Diagnosis of Temporomandibular Disorders Based on the Vienna Concept. In Applications of Three-Dimensional Imaging for Craniofacial Region; Springer: Berlin/Heidelberg, Germany, 2024; pp. 201–222. [Google Scholar]
- Caroccia, F.; Moscagiuri, F.; Falconio, L.; Festa, F.; D’Attilio, M. Early orthodontic treatments of unilateral posterior crossbite: A systematic review. J. Clin. Med. 2020, 10, 33. [Google Scholar] [CrossRef]
- Lindner, A. Longitudinal study on the effect of early interceptive treatment in 4-year-old children with unilateral cross-bite. Eur. J. Oral Sci. 1989, 97, 432–438. [Google Scholar] [CrossRef]
- Karłowska, I. Współczesna Ortodoncja, 3rd ed.; PZWL Wydawnictwo Lekarskie: Warszawa, Poland, 2018. [Google Scholar]
- Neto, G.P.; Puppin-Rontani, R.M.; Garcia, R.C.R. Changes in the masticatory cycle after treatment of posterior crossbite in children aged 4 to 5 years. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 464–472. [Google Scholar] [CrossRef]
- Kantomaa, T. Correction of unilateral crossbite in the deciduous dentition. Eur. J. Orthod. 1986, 8, 80–83. [Google Scholar] [CrossRef]
- Malandris, M.; Mahoney, E. Aetiology, diagnosis and treatment of posterior cross-bites in the primary dentition. Int. J. Paediatr. Dent. 2004, 14, 155–166. [Google Scholar] [CrossRef]
- Rutili, V.; Mrakic, G.; Nieri, M.; Franceschi, D.; Pierleoni, F.; Giuntini, V.; Franchi, L. Dento-skeletal effects produced by rapid versus slow maxillary expansion using fixed jackscrew expanders: A systematic review and meta-analysis. Eur. J. Orthod. 2021, 43, 301–312. [Google Scholar] [CrossRef]
- Safi-Eddine, Z.; Ousehal, L. Treatment of Lateral Functional Shift of the Mandible: A Case Report. Open Access Libr. J. 2025, 12, 1–9. [Google Scholar] [CrossRef]
- Biega, E.; Becker, K.; Czaniecka, K. Unconventional usage of the Invisalign Fist system in treating a complete crossbite due to a lateral functional mandibular shift—A case report. In Forum Ortodontyczne/Orthodontic Forum; Termedia: Poznań, Poland, 2021; Volume 17, pp. 50–63. [Google Scholar]
- Szpinda-Barczyńska, A.; Perkowski, K. Interceptive treatment of class III malocclusions—A case report. In Forum Ortodontyczne/Orthodontic Forum; Termedia: Poznań, Poland, 2021; Volume 17, pp. 64–70. [Google Scholar]
- Laskowska, M.; Dąbkowska, M.; Szpinda-Barczyńska, A.; Witanowska, J.; Zadurska, M. Incontinentia pigmenti—A description of three cases. In Forum Ortodontyczne/Orthodontic Forum; Termedia: Poznań, Poland, 2018; Volume 14, pp. 321–332. [Google Scholar]
- Kobylińska, A.; Sobiech, P.; Kuśmierczyk, D.; Olczak-Kowalczyk, D. Improvement of psychosocial well-being in adolescent patient by frenuloplasty and orthodontic diastema closure: 12-years observation period. A case report. Nowa Stomatol. 2023, 28, 52–56. [Google Scholar]
- Karwetzky, R. Die Beseitigung der ein-und doppelseitigen Bukkookklusion. Fortschritte Der Kieferorthopädie 1975, 36, 135–141. [Google Scholar] [CrossRef]
- Binder, R.E. Correction of posterior crossbites: Diagnosis and treatment. Pediatr. Dent. 2004, 26, 266–272. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowalska, K.; Machorowska-Pieniążek, A. Mandibular Lateral Displacement in Growing Patients: Etiopathogenesis, Prophylaxis, and Early Treatment—A Literature Review. J. Clin. Med. 2025, 14, 8090. https://doi.org/10.3390/jcm14228090
Kowalska K, Machorowska-Pieniążek A. Mandibular Lateral Displacement in Growing Patients: Etiopathogenesis, Prophylaxis, and Early Treatment—A Literature Review. Journal of Clinical Medicine. 2025; 14(22):8090. https://doi.org/10.3390/jcm14228090
Chicago/Turabian StyleKowalska, Karolina, and Agnieszka Machorowska-Pieniążek. 2025. "Mandibular Lateral Displacement in Growing Patients: Etiopathogenesis, Prophylaxis, and Early Treatment—A Literature Review" Journal of Clinical Medicine 14, no. 22: 8090. https://doi.org/10.3390/jcm14228090
APA StyleKowalska, K., & Machorowska-Pieniążek, A. (2025). Mandibular Lateral Displacement in Growing Patients: Etiopathogenesis, Prophylaxis, and Early Treatment—A Literature Review. Journal of Clinical Medicine, 14(22), 8090. https://doi.org/10.3390/jcm14228090




