Treatment of Post-Traumatic Diaphyseal and Distal Tibial Bone Defects by Distraction Osteogenesis: A Monocentric Experience
Abstract
1. Introduction
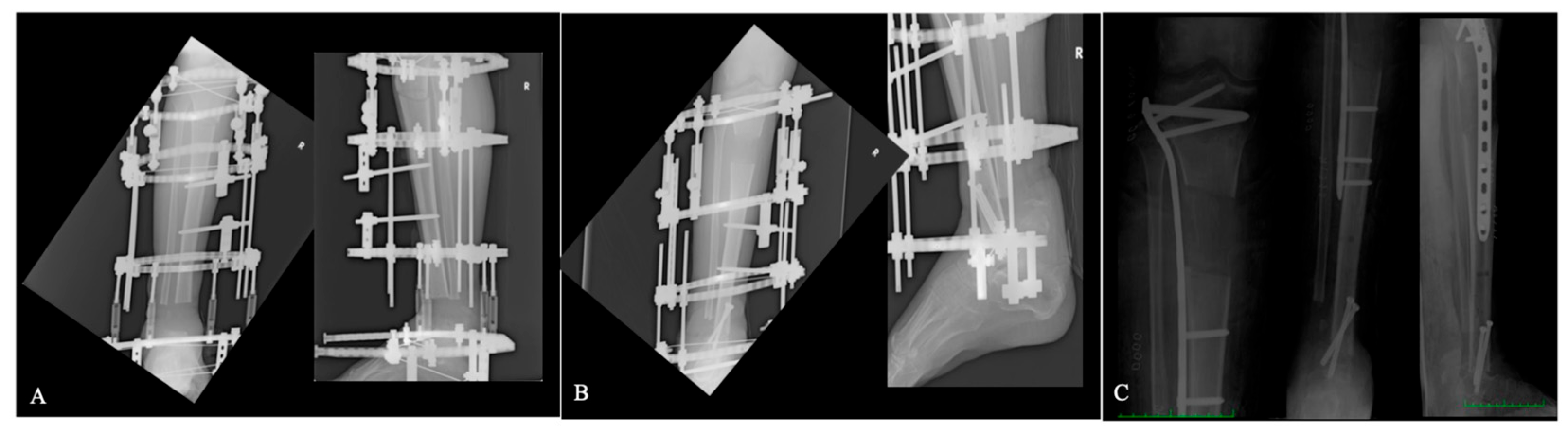
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lu, Y.; Wang, Q.; Ren, C.; Li, M.; Li, Z.; Zhang, K.; Huang, Q.; Ma, T. Proximal versus Distal Bone Transport for the Management of Large Segmental Tibial Defect: A Clinical Case Series. Sci. Rep. 2023, 13, 3883. [Google Scholar] [CrossRef]
- Melvin, S.J.; Dombroski, D.G.; Torbert, J.T.; Kovach, S.J.; Esterhai, J.L.; Mehta, S. Open Tibial Shaft Fractures: I. Evaluation and Initial Wound Management. Am. Acad. Orthop. Surg. 2010, 18, 10–19. [Google Scholar] [CrossRef]
- Liu, K.; Jia, Q.; Wang, X.; Bahesutihan, Y.; Ma, C.; Ren, P.; Liu, Y.; Yusufu, A. Complications Associated with Single-Level Bone Transport for the Treatment of Tibial Bone Defects Caused by Fracture-Related Infection. BMC Musculoskelet. Disord. 2023, 24, 514. [Google Scholar] [CrossRef]
- Mauffrey, C.; Barlow, B.T.; Smith, W. Management of Segmental Bone Defects. J. Am. Acad. Orthop. Surg. 2015, 23, 143–153. [Google Scholar] [CrossRef]
- Ilizarov, G.A. The Principles of the Ilizarov Method. Bull. Hosp. Jt. Dis. Orthop. Inst. 1988, 48, 1–11. [Google Scholar]
- Spiegelberg, B.; Parratt, T.; Dheerendra, S.; Khan, W.; Jennings, R.; Marsh, D. Ilizarov Principles of Deformity Correction. Ann. R. Coll. Surg. Engl. 2010, 92, 101–105. [Google Scholar] [CrossRef]
- Lasanianos, N.G.; Kanakaris, N.K.; Giannoudis, P.V. Current Management of Long Bone Large Segmental Defects. Orthop. Trauma 2010, 24, 149–163. [Google Scholar] [CrossRef]
- Rosslenbroich, S.; Oh, C.-W.; Kern, T.; Mukhopadhaya, J.; Raschke, M.; Kneser, U.; Krettek, C. Current Management of Diaphyseal Long Bone Defects—A Multidisciplinary and International Perspective. J. Clin. Med. 2023, 12, 6283. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, S.M.; Papakostidis, C.; Giannoudis, V.P.; Mandía-Martínez, A.; Giannoudis, P.V. Distraction Osteogenesis versus Induced Membrane Technique for Infected Tibial Non-Unions with Segmental Bone Loss: A Systematic Review of the Literature and Meta-Analysis of Available Studies. Eur. J. Trauma Emerg. Surg. 2024, 50, 705–721. [Google Scholar] [CrossRef]
- Noonan, K.J.; Leyes, M.; Forriol, F.; Cañadell, J. Distraction Osteogenesis of the Lower Extremity with Use of Monolateral External Fixation. A Study of Two Hundred and Sixty-One Femora and Tibiae*. J. Bone Jt. Surg. 1998, 80, 793–806. [Google Scholar] [CrossRef] [PubMed]
- Abulaiti, A.; Yilihamu, Y.; Yasheng, T.; Alike, Y.; Yusufu, A. The Psychological Impact of External Fixation Using the Ilizarov or Orthofix LRS Method to Treat Tibial Osteomyelitis with a Bone Defect. Injury 2017, 48, 2842–2846. [Google Scholar] [CrossRef]
- Sarangi, G.; Mishra, S.; Das, T.K.; Acharya, R.; Sharma, A. Assesment of Functional and Radiological Outcomes of Proximal Tibia Fractures Surgically Treated with Ilizarov Fixators. Cureus 2025, 17, e79464. [Google Scholar] [CrossRef]
- Qu, H.; Guo, W.; Yang, R.; Li, D.; Tang, S.; Yang, Y.; Dong, S.; Zang, J. Reconstruction of Segmental Bone Defect of Long Bones after Tumor Resection by Devitalized Tumor-Bearing Bone. World J. Surg. Oncol. 2015, 13, 282. [Google Scholar] [CrossRef]
- Papakostidis, C.; Bhandari, M.; Giannoudis, P.V. Distraction Osteogenesis in the Treatment of Long Bone Defects of the Lower Limbs. Bone Jt. J. 2013, 95-B, 1673–1680. [Google Scholar] [CrossRef] [PubMed]
- Barakat, A.H.; Sayani, J.; Guryel, E.; O\’Dowd-Booth, C. Lengthening Nails for Distraction Osteogenesis: A Review of Current Practice and Presentation of Extended Indications. Strateg. Trauma Limb Reconstr. 2020, 15, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Yao, L.; Mao, H.; Dong, W.; Wu, Z.; Liu, Q. Application of the Distraction Support in Intramedullary Nailing Treatment for Tibial Shaft Fracture. Chin. J. Traumatol. 2025, 28, 113–117. [Google Scholar] [CrossRef]
- Eward, W.C.; Kontogeorgakos, V.; Levin, L.S.; Brigman, B.E. Free Vascularized Fibular Graft Reconstruction of Large Skeletal Defects after Tumor Resection. Clin. Orthop. Relat. Res. 2010, 468, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Valtanen, R.S.; Yang, Y.P.; Gurtner, G.C.; Maloney, W.J.; Lowenberg, D.W. Synthetic and Bone Tissue Engineering Graft Substitutes: What Is the Future? Injury 2021, 52, S72–S77. [Google Scholar] [CrossRef]
- Schick, V.D.; Zampogna, B.; Marrara, G.; Siracusano, L.; Larizza, L.; Calaciura, S.; Sanzarello, I.; Marinozzi, A.; Leonetti, D. Custom-Made 3D-Printed Titanium Implants for Managing Segmental Distal Tibial Bone Defects: A Systematic Literature Review. J. Clin. Med. 2025, 14, 1796. [Google Scholar] [CrossRef]
- Khaled, A.; El-Gebaly, O.; El-Rosasy, M. Masquelet-Ilizarov Technique for the Management of Bone Loss Post Debridement of Infected Tibial Nonunion. Int. Orthop. 2022, 46, 1937–1944. [Google Scholar] [CrossRef]
- Marrara, G.; Zampogna, B.; Schick, V.D.; Larizza, L.; Rizzo, P.; Sanzarello, I.; Nanni, M.; Leonetti, D. Post-Traumatic Segmental Tibial Defects Management: A Systematic Review of the Literature. Appl. Sci. 2024, 15, 64. [Google Scholar] [CrossRef]
- Masquelet, A.C.; Begue, T. The Concept of Induced Membrane for Reconstruction of Long Bone Defects. Orthop. Clin. N. Am. 2010, 41, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Benulic, C.; Canton, G.; Gril, I. Management of Acute Bone Loss Following High Grade Open Tibia Fractures. Acta Biomed. 2020, 30, e2020012. [Google Scholar]
- Paley, D.; Maar, D.C. Ilizarov Bone Transport Treatment for Tibial Defects. J. Orthop. Trauma 2000, 14, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H. Operative Lengthening of the Femur. Clin. Orthop. Relat. Res. 1978, 136, 125–142. [Google Scholar] [CrossRef]
- Paley, D. Problems, Obstacles, and Complications of Limb Lengthening by the Ilizarov Technique. Clin. Orthop. Relat. Res. 1990, 250, 81–104. [Google Scholar] [CrossRef]
- Migliorini, F.; La Padula, G.; Torsiello, E.; Spiezia, F.; Oliva, F.; Maffulli, N. Strategies for Large Bone Defect Reconstruction after Trauma, Infections or Tumour Excision: A Comprehensive Review of the Literature. Eur. J. Med. Res. 2021, 26, 118. [Google Scholar] [CrossRef]
- Haase, L.; Moon, T.; Burcke, A.; Speybroeck, J.; Wetzel, R.; Sontich, J.; Ochenjele, G.; Napora, J. Comparison of Outcomes and Operative Course between Septic and Aseptic Nonunion in Long Bones. Eur. J. Orthop. Surg. Traumatol. 2022, 33, 1929–1935. [Google Scholar] [CrossRef]
- Feng, D.; Zhang, Y.; Jia, H.; Xu, G.; Wu, W.; Yang, F.; Ding, J.; Li, D.; Wang, K.; Luo, Y.; et al. Complications Analysis of Ilizarov Bone Transport Technique in the Treatment of Tibial Bone Defects–a Retrospective Study of 199 Cases. BMC Musculoskelet. Disord. 2023, 24, 864. [Google Scholar] [CrossRef]
- Tian, R.; Zheng, F.; Zhao, W.; Zhang, Y.; Yuan, J.; Zhang, B.; Li, L. Prevalence and Influencing Factors of Nonunion in Patients with Tibial Fracture: Systematic Review and Meta-Analysis. J. Orthop. Surg. Res. 2020, 15, 377. [Google Scholar] [CrossRef]
| n° (%) | Age (Years) | Weight (kg) | Height (m) | BMI (kg/m2) | Smoking | |
|---|---|---|---|---|---|---|
| Whole | 19 (100%) | 32.42 | 75.1 | 1.73 | 25.04 | 14 (73.7%) |
| Male | 14 (73.7%) | 34.28 | 78.1 | 1.76 | 26.3 | 12 (63.2%) |
| Female | 5 (26.3%) | 27.2 | 66.3 | 1.64 | 24.7 | 2 (10.5%) |
| N° | Mechanism of Injury | Injury Side | Location of Bone Defect | Bone Defect Size (cm) | Previous Surgeries (n°) | Time from Trauma to DO (Month) | Bacterial Culture |
|---|---|---|---|---|---|---|---|
| 1 | Fall from height | Left | Diaphyseal | 4.7 | 3 | 14 | EF |
| 2 | Road accident | Right | Diaphyseal | 4 | 1 | 1 | / |
| 3 | Fall from height | Right | Diaphyseal | 5.2 | 4 | 12 | SE + ECC |
| 4 | Road accident | Right | Distal | 4.6 | 2 | 2 | / |
| 5 | Workplace injury | Left | Diaphyseal | 5.2 | 2 | 2 | / |
| 6 | Road accident | Left | Diaphyseal | 3.2 | 1 | 1 | / |
| 7 | Fall from height | Left | Distal | 4.7 | 2 | 3 | PA |
| 8 | Road accident | Left | Distal | 5.1 | 2 | 7 | SA |
| 9 | Road accident | Right | Distal | 3.4 | 1 | 1 | / |
| 10 | Fall from height | Right | Distal | 6.3 | 3 | 36 | EF + SA |
| 11 | Road accident | Right | Distal | 4.1 | 2 | 4 | SE + CF |
| 12 | Road accident | Right | Diaphyseal | 3.2 | 3 | 6 | SA |
| 13 | Road accident | Left | Diaphyseal | 4.2 | 4 | 2 | / |
| 14 | Fall from height | Left | Diaphyseal | 7.2 | 3 | 10 | SA |
| 15 | Road accident | Right | Diaphyseal | 8.1 | 5 | 3 | MRSA |
| 16 | Workplace injury | Right | Distal | 3.4 | 1 | 2 | / |
| 17 | Road accident | Left | Distal | 4.1 | 1 | 2 | / |
| 18 | Fall from height | Right | Diaphyseal | 5.8 | 3 | 6 | SA |
| 19 | Road accident | Right | Diaphyseal | 4.8 | 3 | 2 | / |
| Average | 4.8 ± 1.32 | 2.47 | 6.1 ± 8.1 |
| N° | Surgery | EFT (Weeks) | Time to Bone Union (Weeks) | Surgical Complications | Post-Surgery Complications | FU (Weeks) | LLD (cm) |
|---|---|---|---|---|---|---|---|
| 1 | Ilizarov | 28 | N/A | / | AKA | 147 | N/A |
| 2 | Hybrid (Ilizarov + nailing) | 17 | 25 | / | Pin tract infection | 180 | 1 |
| 3 | Hybrid (Ilizarov + nailing) | 25 | 31 | / | / | 130 | 2.3 |
| 4 | Hybrid (Ilizarov + nailing) | 20 | 26 | / | / | 222 | 0.2 |
| 5 | Ilizarov | 26 | 33 | / | / | 243 | 0.3 |
| 6 | Hybrid (Ilizarov + plating) | 15 | 20 | / | / | 135 | 0.3 |
| 7 | Hybrid (Ilizarov + nailing) | 17 | 26 | / | / | 205 | 1.2 |
| 8 | Hybrid (Ilizarov + nailing) | 21 | 28 | / | / | 152 | 1 |
| 9 | Hybrid (Ilizarov + nailing) | 19 | 25 | / | / | 170 | 1.1 |
| 10 | Ilizarov + Arthrodesis at the Docking site | 28 | 36 | / | / | 203 | 0.2 |
| 11 | Ilizarov + Arthrodesis at the Docking site | 17 | 21 | / | K wires breakage | 203 | 1.4 |
| 12 | Hybrid (Ilizarov + nailing) | 13 | 19 | / | / | 78 | 1.7 |
| 13 | Hybrid (Ilizarov + nailing) | 16 | 21 | / | / | 270 | 1.2 |
| 14 | Hybrid (Ilizarov + nailing) | 29 | 35 | / | / | 97 | 1.4 |
| 15 | Hybrid (Ilizarov + plating) | 27 | 36 | / | / | 182 | 0.3 |
| 16 | Hybrid (Ilizarov + plating) | 16 | 22 | / | / | 68 | 0.2 |
| 17 | Hybrid (Ilizarov + nailing) | 21 | 25 | / | / | 95 | 0.7 |
| 18 | Ilizarov | 26 | 33 | / | Pin tract infection | 174 | 0.5 |
| 19 | Ilizarov | 24 | 30 | / | / | 197 | 0.8 |
| Average | 21.31 ± 5.13 | 25.89 ± 8.34 | 160.1 ± 57.1 | 0.83 ± 0.61 |
| N° | Bone Results ASAMI | Functional Results ASAMI |
|---|---|---|
| 1 | POOR | FAILURE |
| 2 | FAIR | FAIR |
| 3 | FAIR | FAIR |
| 4 | EXCELLENT | EXCELLENT |
| 5 | EXCELLENT | EXCELLENT |
| 6 | GOOD | EXCELLENT |
| 7 | GOOD | GOOD |
| 8 | EXCELLENT | EXCELLENT |
| 9 | EXCELLENT | EXCELLENT |
| 10 | EXCELLENT | EXCELLENT |
| 11 | GOOD | GOOD |
| 12 | EXCELLENT | GOOD |
| 13 | EXCELLENT | GOOD |
| 14 | GOOD | EXCELLENT |
| 15 | GOOD | EXCELLENT |
| 16 | EXCELLENT | GOOD |
| 17 | GOOD | GOOD |
| 18 | EXCELLENT | GOOD |
| 19 | EXCELLENT | GOOD |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leonetti, D.; Siracusano, L.; Schick, V.D.; Marrara, G.; Larizza, L.; Brigandì, M.; Alibrandi, A.; Sanzarello, I.; Nanni, M.; Zampogna, B. Treatment of Post-Traumatic Diaphyseal and Distal Tibial Bone Defects by Distraction Osteogenesis: A Monocentric Experience. J. Clin. Med. 2025, 14, 7933. https://doi.org/10.3390/jcm14227933
Leonetti D, Siracusano L, Schick VD, Marrara G, Larizza L, Brigandì M, Alibrandi A, Sanzarello I, Nanni M, Zampogna B. Treatment of Post-Traumatic Diaphyseal and Distal Tibial Bone Defects by Distraction Osteogenesis: A Monocentric Experience. Journal of Clinical Medicine. 2025; 14(22):7933. https://doi.org/10.3390/jcm14227933
Chicago/Turabian StyleLeonetti, Danilo, Lorenza Siracusano, Viktor Dietrich Schick, Giovanni Marrara, Leone Larizza, Massimo Brigandì, Angela Alibrandi, Ilaria Sanzarello, Matteo Nanni, and Biagio Zampogna. 2025. "Treatment of Post-Traumatic Diaphyseal and Distal Tibial Bone Defects by Distraction Osteogenesis: A Monocentric Experience" Journal of Clinical Medicine 14, no. 22: 7933. https://doi.org/10.3390/jcm14227933
APA StyleLeonetti, D., Siracusano, L., Schick, V. D., Marrara, G., Larizza, L., Brigandì, M., Alibrandi, A., Sanzarello, I., Nanni, M., & Zampogna, B. (2025). Treatment of Post-Traumatic Diaphyseal and Distal Tibial Bone Defects by Distraction Osteogenesis: A Monocentric Experience. Journal of Clinical Medicine, 14(22), 7933. https://doi.org/10.3390/jcm14227933








