Preoperative Health Status and Clinical Predictors of Health-Related Quality of Life Improvement After Lumbar Spinal Stenosis Surgery: A Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
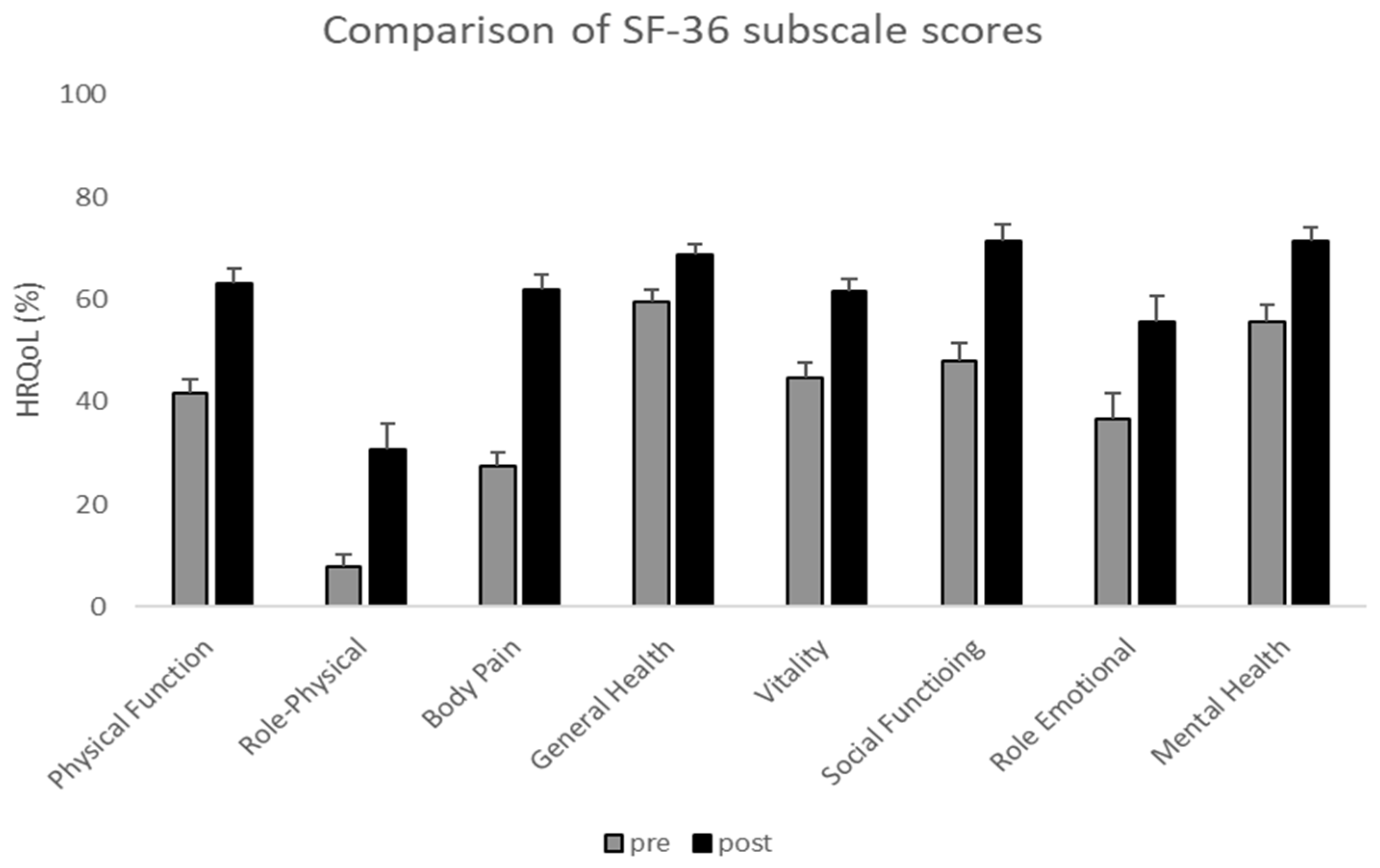
3. Results
4. Discussion
4.1. Clinical Implication
4.2. Limitations
4.3. Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HRQoL | Health-related quality of life |
| LSS | Lumbar spinal stenosis |
| SF-36 | Short Form Health Survey 36 |
| PCS | Physical components of SF-36 |
| MCS | Mental components of SF-36 |
| ODI | Oswestry Disability Index |
| RMDQ | Roland Morris Disability Questionnaire |
| QBPDS | Quebec Back Pain Disability Scale |
| VAS | Visual Analog Scale |
| SAS | Zung Self-Rating Anxiety Scale |
| SDS | Zung Self-Rating Depression Scale |
| BMI | Body mass index |
References
- Anderson, D.B.; Beard, D.J.; Rannou, F.; Hunter, D.J.; Suri, P.; Chen, L.; Van Gelder, J.M. Clinical assessment and management of lumbar spinal stenosis: Clinical dilemmas and considerations for surgical referral. Lancet Rheumatol. 2024, 6, e727–e732. [Google Scholar] [CrossRef] [PubMed]
- Igari, T.; Otani, K.; Sekiguchi, M.; Konno, S.I. Epidemiological Study of Lumbar Spinal Stenosis Symptoms: 10-Year Follow-Up in the Community. J. Clin. Med. 2022, 11, 5911. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, L.; Cole, R.; Kim, D.H.; Li, L.; Suri, P.; Guermazi, A.; Hunter, D.J. Spinal stenosis prevalence and association with symptoms: The Framingham Study. Spine J. 2009, 9, 545–550. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bagley, C.; MacAllister, M.; Dosselman, L.; Moreno, J.; Aoun, S.G.; El Ahmadieh, T.Y. Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Research 2019, 8, 137. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ferretti, F.; Coluccia, A.; Gusinu, R.; Gualtieri, G.; Muzii, V.F.; Pozza, A. Quality of life and objective functional impairment in lumbar spinal stenosis: A protocol for a systematic review and meta-analysis of moderators. BMJ Open 2019, 9, e032314. [Google Scholar] [CrossRef]
- Liang, H.; Lu, S.; Jiang, D.; Fei, Q. Clinical outcomes of lumbar spinal surgery in patients 80 years or older with lumbar stenosis or spondylolisthesis: A systematic review and meta-analysis. Eur. Spine J. 2020, 29, 2129–2142. [Google Scholar] [CrossRef]
- Wei, F.L.; Zhou, C.P.; Liu, R.; Zhu, K.L.; Du, M.R.; Gao, H.R.; Wu, S.D.; Sun, L.L.; Yan, X.D.; Liu, Y.; et al. Management for lumbar spinal stenosis: A network meta-analysis and systematic review. Int. J. Surg. 2021, 85, 19–28. [Google Scholar] [CrossRef]
- McKillop, A.B.; Carroll, L.J.; Battié, M.C. Depression as a prognostic factor of lumbar spinal stenosis: A systematic review. Spine J. 2014, 14, 837–846. [Google Scholar] [CrossRef]
- McIlroy, S.; Walsh, E.; Sothinathan, C.; Stovold, E.; Norwitz, D.; Norton, S.; Weinman, J.; Bearne, L. Pre-operative prognostic factors for walking capacity after surgery for lumbar spinal stenosis: A systematic review. Age Ageing 2021, 50, 1529–1545. [Google Scholar] [CrossRef]
- Mao, Z.; Ahmed, S.; Graham, C.; Kind, P.; Sun, Y.N.; Yu, C.H. Similarities and Differences in Health-Related Quality-of-Life Concepts Between the East and the West: A Qualitative Analysis of the Content of Health-Related Quality-of-Life Measures. Value Health Reg. Issues 2021, 24, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Beyer, F.; Prasse, T.; Eysel, P.; Bredow, J. Quality of life in lumbar spinal stenosis: Does it correlate with magnetic resonance imaging and spinopelvic parameters? J. Orthop. 2023, 47, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Evans, J.D. Straightforward Statistics for the Behavioral Sciences; Thomson Brooks/Cole: Belmont, CA, USA, 1996. [Google Scholar]
- The Jamovi Project. Jamovi (Version 2.5) [Computer Software]. 2024. Available online: https://www.jamovi.org (accessed on 19 April 2025).
- Xu, Y.; Liu, Y.; Ding, D.; Ru, B.; Wan, Q.; Ji, Z.; Liu, W.; Guo, R.; Hu, J.; Zhang, N.; et al. Clinical efficacy of unilateral laminotomy for bilateral decompression in the treatment of adjacent segment disease after lumbar fusion. Front. Surg. 2024, 11, 1449838. [Google Scholar]
- Gornet, M.F.; Copay, A.G.; Sorensen, K.M.; Schranck, F.W. Assessment of health-related quality of life in spine treatment: Conversion from SF-36 to VR-12. Spine J. 2018, 18, 1292–1297. [Google Scholar] [CrossRef]
- Graebsch, C.; Buser, Z.; Leroy, S.; Wang, J.C.; Yoon, T.; Bone, S.; Meisel, H.J.; Schenk, P. AO Spine Knowledge Forum Degenerative. Pain and functional outcome after microsurgical decompression of lumbar spinal stenosis: Very short-and long-term postoperative analysis. Glob. Spine J. 2025. ahead of print. [Google Scholar] [CrossRef]
- Tovian, S.M. Psychological assessment of surgical candidates: Evidence-based procedures and practices. J. Pers. Assess. 2023, 106, 558–560. [Google Scholar] [CrossRef]
- Michaelsson, K.; Sanden, B. Obesity is associated with inferior results after surgery for lumbar spinal stenosis: A study of 2633 patients from the Swedish spine register. Spine 2013, 38, 435–441. [Google Scholar]
- Mauro, D.; Nasi, D.; Paracino, R.; Capece, M.; Carrassi, E.; Aiudi, D.; Mancini, F.; Lattanzi, S.; Colasanti, R.; Iacoangeli, M. The relationship between preoperative predictive factors for clinical outcome in patients operated for lumbar spinal stenosis by decompressive laminectomy. Surg. Neurol. Int. 2020, 11, 27. [Google Scholar] [CrossRef]
- Wong, J.J.; Tricco, A.C.; Côté, P.; Liang, C.Y.; Lewis, J.A.; Bouck, Z.; Rosella, L.C. Association between depressive symptoms or depression and health outcomes for low back pain: A systematic review and meta-analysis. J. Gen. Intern. Med. 2022, 37, 1233–1246. [Google Scholar] [CrossRef]
- Mok, L.C.; Lee, I.F. Anxiety, depression and pain intensity in patients with low back pain who are admitted to acute care hospitals. J. Clin. Nurs. 2008, 17, 1471–1480. [Google Scholar] [CrossRef] [PubMed]
- Aalto, T.J.; Malmivaara, A.; Kovacs, F.; Herno, A.; Alen, M.; Salmi, L.; Kröger, H.; Andrade, J.; Jiménez, R.; Tapaninaho, A.; et al. Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: Systematic review. Spine 2006, 31, E648–E663. [Google Scholar] [CrossRef] [PubMed]
- Uysal, E.; Çine, H.Ş.; Azizoğlu, S.İ.; Çakaloğlu, H.C.; Yavuz, A.Y.; Yaşar, A.H.; Aydın, M.V. Psychological burdens in lumbar spinal stenosis: The underrated influence of preoperative depression and anxiety on surgical outcomes and quality of life. J. Turk. Spinal Surg. 2025, 36, 1–9. [Google Scholar] [CrossRef]
- Djurasovic, M.; Owens, R.K.; Carreon, L.Y.; Gum, J.L.; Bisson, E.F.; Bydon, M.; Glassman, S.D. The impact of smoking on patient-reported outcomes following lumbar decompression: An analysis of the Quality Outcomes Database. J. Neurosurg. Spine 2024, 42, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Rajesh, N.; Moudgil-Joshi, J.; Kaliaperumal, C. Smoking and degenerative spinal disease: A systematic review. Brain Spine 2022, 2, 100916. [Google Scholar] [CrossRef]
- Knutsson, B.; Mukka, S.; Wahlström, J.; Järvholm, B.; Sayed-Noor, A.S. The association between tobacco smoking and surgical intervention for lumbar spinal stenosis: Cohort study of 331,941 workers. Spine J. 2018, 18, 1313–1317. [Google Scholar] [CrossRef]
- Stienen, M.N.; Joswig, H.; Smoll, N.R.; Tessitore, E.; Schaller, K.; Hildebrandt, G.; Gautschi, O.P. Short- and long-term effects of smoking on pain and health-related quality of life after non-instrumented lumbar spine surgery. Clin. Neurol. Neurosurg. 2016, 142, 87–92. [Google Scholar] [CrossRef]
- Kajino, M.; Tsushima, E. Effects of physical activity on quality of life and physical function in postoperative patients with gastrointestinal cancer. Phys. Ther. Res. 2020, 24, 43–51. [Google Scholar] [CrossRef]
- Eubanks, J.E.; Cupler, Z.A.; Gliedt, J.A.; Bejarano, G.; Skolasky, R.L.; Smeets, R.J.E.M.; Schneider, M.J. Preoperative spinal education for lumbar spinal stenosis: A feasibility study. PMR 2024, 16, 992–1000. [Google Scholar] [CrossRef]
- Janse, R.J.; Hoekstra, T.; Jager, K.J.; Zoccali, C.; Tripepi, G.; Dekker, F.W.; van Diepen, M. Conducting correlation analysis: Important limitations and pitfalls. Clin. Kidney J. 2021, 14, 2332–2337. [Google Scholar] [CrossRef]
- Morone, G.; De Angelis, L.; Martino Cinnera, A.; Carbonetti, R.; Bisirri, A.; Ciancarelli, I.; Iosa, M.; Negrini, S.; Kiekens, C.; Negrini, F.; et al. Artificial intelligence in clinical medicine: A state-of-the-art overview of systematic reviews with methodological recommendations for improved reporting. Front. Digit. Health 2025, 7, 1550731. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Jung, J.Y.; Mahatthanatrakul, A.; Kim, J.S. Artificial intelligence in spinal imaging and patient care: A review of recent advances. Neurospine 2024, 21, 474–486. [Google Scholar] [CrossRef] [PubMed]
- Wilson, B.; Gaonkar, B.; Yoo, B.; Salehi, B.; Attiah, M.; Villaroman, D.; Ahn, C.; Edwards, M.; Laiwalla, A.; Ratnaparkhi, A.; et al. Predicting spinal surgery candidacy from imaging data using machine learning. Neurosurgery 2021, 89, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Broida, S.E.; Schrum, M.L.; Yoon, E.; Sweeney, A.P.; Dhruv, N.N.; Gombolay, M.C.; Yoon, S.T. Improving surgical triage in spine clinic: Predicting likelihood of surgery using machine learning. World Neurosurg. 2022, 163, e192–e198. [Google Scholar] [CrossRef]
- Khan, O.; Badhiwala, J.H.; Witiw, C.D.; Wilson, J.R.; Fehlings, M.G. Machine learning algorithms for prediction of health-related quality-of-life after surgery for mild degenerative cervical myelopathy. Spine J. 2021, 21, 1659–1669. [Google Scholar] [CrossRef]
| Demographic variables | Age (years) | 72.21 ± 8.8 |
| Sex (F; M) | 19 (31.1%); 42 (68.9%) | |
| Weight (Kg) | 81.18 ± 14.8 | |
| Height (cm) | 170.16 ± 10.6 | |
| BMI | 27.45 ± 4 | |
| Living alone (no; yes) | 49 (80.3%); 12 (19.7%) | |
| Instruction level (≤5 years; >5–≤8 years; >8–≤13 years; >13 years) | 11 (18.0%); 20 (32.8%); 21 (34.4%); 9 (14.7%) | |
| Health status information | Physically demanding work (no; yes) | 26 (42.6%); 35 (57.4%) |
| Smoking habits (no; ex-smokers; yes) | 18 (29.5%); 11 (18.0%); 32 (52.5%) | |
| Pain onset (months) | 56.66 ± 110.4 | |
| Complex drug therapy (no; yes) | 36 (59%); 25 (41.0%) | |
| Sport activity (no; yes) | 31 (50.8%); 30 (49.2%) | |
| History of back pain (no; yes) | 11 (18.0%); 50 (82.0%) | |
| Physiological distress (no; yes) | 42 (68.8%); 19 (31.2%) | |
| Diabetes (no; yes) | 49 (80.3%); 12 (19.7%) | |
| Rheumatic disease (no; yes) | 59 (96.7%); 2 (2.3%) | |
| Comorbidity (more than 4) (no; yes) | 41 (67.2%); 20 (32.8%) |
| ODI Pre | ODI Post | RMDQ Pre | RMDQ Post | QBPDS Pre | QBPDS Post | VAS Pre | VAS Post | SAS Pre | SAS Post | SDS Pre | SDS Post | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± DS | 45.1 ± 18.8 | 24.2 ± 17.8 | 15.8 ± 4.86 | 10.6 ± 5.13 | 45.2 ± 18.2 | 28.5 ± 18.1 | 6.62 ± 2.58 | 3.05 ± 2.49 | 36.8 ± 8.5 | 30.7 ± 7.65 | 37.8 ± 10.5 | 32.8 ± 9.31 |
| Minimal value | 0 | 0 | 4 | 1 | 1 | 1 | 0 | 0 | 21 | 21 | 22 | 20 |
| Maximal value | 88 | 76 | 23 | 22 | 96 | 78 | 10 | 10 | 62 | 56 | 66 | 57 |
| Shapiro–Wilk W | 0.989 | 0.95 | 0.959 | 0.975 | 0.987 | 0.943 | 0.916 | 0.919 | 0.97 | 0.892 | 0.957 | 0.938 |
| Shapiro–Wilk p | 0.867 | 0.015 | 0.039 | 0.242 | 0.746 | 0.007 | <0.001 | < 0.001 | 0.136 | <0.001 | 0.033 | 0.004 |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| η2p | 0.56 | 0.49 | 0.46 | 0.6 | 0.34 | 0.27 |
| ΔScore SF-36 Components | ΔScore Clinical Scales | r | p | Interpretation |
|---|---|---|---|---|
| PCS | ODI | 0.354 | 0.005 | Weak |
| MCS | ODI | 0.535 | <0.001 | Moderate |
| PCS | RMDQ | 0.298 | 0.02 | Weak |
| MCS | RMDQ | 0.474 | <0.001 | Moderate |
| PCS | QBPDS | 0.256 | 0.04 | Weak |
| MCS | QBPDS | 0.499 | <0.001 | Moderate |
| PCS | VAS | 0.415 | <0.001 | Moderate |
| MCS | VAS | 0.293 | 0.02 | Weak |
| PCS | SAS | 0.546 | <0.001 | Moderate |
| MCS | SDS | 0.402 | 0.001 | Moderate |
| ΔScore SF-36 Subscales | Preoperative Variable | r | p |
|---|---|---|---|
| Physical function | Sport activity | 0.38 | 0.003 |
| Physical function | Comorbidity | −0.259 | 0.04 |
| Role physical | BMI | −0.368 | 0.004 |
| Role physical | Weight | −0.283 | 0.03 |
| Social function | Sport activity | 0.331 | 0.009 |
| Role emotional | BMI | −0.302 | 0.02 |
| Role emotional | Weight | −0.286 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciancarelli, I.; Martino Cinnera, A.; Ricci, A.; Iosa, M.; Cerasa, A.; Calabrò, R.S.; Morone, G. Preoperative Health Status and Clinical Predictors of Health-Related Quality of Life Improvement After Lumbar Spinal Stenosis Surgery: A Longitudinal Study. J. Clin. Med. 2025, 14, 4391. https://doi.org/10.3390/jcm14134391
Ciancarelli I, Martino Cinnera A, Ricci A, Iosa M, Cerasa A, Calabrò RS, Morone G. Preoperative Health Status and Clinical Predictors of Health-Related Quality of Life Improvement After Lumbar Spinal Stenosis Surgery: A Longitudinal Study. Journal of Clinical Medicine. 2025; 14(13):4391. https://doi.org/10.3390/jcm14134391
Chicago/Turabian StyleCiancarelli, Irene, Alex Martino Cinnera, Alessandro Ricci, Marco Iosa, Antonio Cerasa, Rocco Salvatore Calabrò, and Giovanni Morone. 2025. "Preoperative Health Status and Clinical Predictors of Health-Related Quality of Life Improvement After Lumbar Spinal Stenosis Surgery: A Longitudinal Study" Journal of Clinical Medicine 14, no. 13: 4391. https://doi.org/10.3390/jcm14134391
APA StyleCiancarelli, I., Martino Cinnera, A., Ricci, A., Iosa, M., Cerasa, A., Calabrò, R. S., & Morone, G. (2025). Preoperative Health Status and Clinical Predictors of Health-Related Quality of Life Improvement After Lumbar Spinal Stenosis Surgery: A Longitudinal Study. Journal of Clinical Medicine, 14(13), 4391. https://doi.org/10.3390/jcm14134391








