Abstract
Background: The COVID-19 pandemic has profoundly affected young adults’ lives globally, including those in Germany. This study investigated mental health and quality of life during the pandemic, with a particular focus on mood. Immune fitness, the body’s capacity to respond to health challenges (such as infections) by activating an appropriate immune response, was assessed as a physical health indicator. Methods: Data were collected from 317 participants, aged 18 to 35, via an online survey conducted between November 2021 and March 2022. Participants included 103 men (32.5%) and 214 women (67.5%), with a mean age of 25.5 years (SD = 4.1). Results: Compared to pre-pandemic levels, significant declines in mood, quality of life, immune fitness, and sleep quality were observed during the lockdown periods of the COVID-19 pandemic (p < 0.0125). The most pronounced effects were observed during the second lockdown, with declines extending into the second no-lockdown period for fatigue, depression, happiness, optimism, and immune fitness (p < 0.0125). Significant sex differences were found for the magnitude of mood effects (anxiety, depression, stress). No significant differences were found according to age or occupational status (student vs. work). Conclusions: The COVID-19 pandemic and associated lockdown periods had a significant negative effect on the mood, immune fitness, and well-being of young adults living in Germany.
1. Introduction
The COVID-19 pandemic was declared a global health emergency by the World Health Organization on 11 March 2020, leading to unprecedented public health measures worldwide. In Germany, the government quickly imposed restrictions to mitigate the spread of the virus, resulting in widespread closures of schools and businesses and strict limitations on social interactions [1]. Essential public facilities, including supermarkets, hospitals, and pharmacies, remained operational under stringent hygiene protocols, which mandated the use of face masks [1].
The progression of the pandemic in Germany was characterized by alternating periods of strict lockdowns and gradual easing of restrictions. Young adults faced significant challenges during these transitions, including the shift to remote work and online learning, which reduced opportunities for social interaction considerably. The psychological impact of isolation and social distancing measures was profound [2,3].
Germany’s economy experienced significant disruptions, with many businesses, especially in non-essential sectors, facing closures, decreased revenues, layoffs, and permanent shutdowns [4,5]. The ‘Kurzarbeit’ policy, which allowed companies to reduce employees’ working hours while the government compensated a portion of their lost wages, helped mitigate some negative effects and stabilized the job market. Despite this, unemployment rates peaked at 4.1% in 2020, and the consumer price index (CPI) saw a notable increase in November 2021, exacerbating financial stress [6,7,8,9]. These economic pressures particularly affected those with pre-existing low incomes and precarious working conditions [10,11]. Economic difficulties and job instability, which are known to lower quality of life and to be linked to increased mental health issues [1,12,13], likely contributed to the observed decline in quality of life during the pandemic.
Globally, studies have highlighted the pandemic’s adverse effects on mental well-being, with similar trends observed in Germany. Reports indicate increases in loneliness, stress, depression, and anxiety, particularly among younger individuals and women, who were more vulnerable to pandemic-related stressors [14,15,16,17,18,19,20,21]. Fear of COVID-19 further exacerbated mental health issues for some individuals [15].
Addressing mental health complaints is critical due to their impact on daily functioning and productivity [22]. Prolonged stress can dysregulate the body’s stress response system, leading to overactivation of the sympathetic nervous system and increased cortisol levels, which can impair immune function and increase susceptibility to diseases, including COVID-19 [23,24]. Additionally, anxiety and depression can disrupt sleep patterns, further compromising the immune system [25,26].
The current study aimed to assess mood, immune fitness, and quality of life among young adults in Germany before and during the COVID-19 pandemic. Specifically, it examined changes in mood and quality of life over different phases of the pandemic, as well as potential sex and age differences in these outcomes. Immune fitness is an important determinant of health and disease and refers to the body’s capacity to respond to health challenges (such as infections) by activating an appropriate immune response [27]. Therefore, in this study, immune fitness was assessed as a physical health indicator. Based on the results of previous studies conducted in the Netherlands, Argentina, and Türkiye [28,29] using the same study design [30,31], it was hypothesized that the negative effects on mood, immune fitness, and quality of life were more pronounced during lockdown periods than during no-lockdown periods (including the pre-pandemic period).
2. Methods
An online survey was conducted between mid-November 2021 and the end of March 2022. Potential participants were invited to participate in this study via university e-mail and printed flyers, mainly distributed in the city of Dresden. Eligible participants were those residing in Germany and aged between 18 and 35 years. There were no other inclusion or exclusion criteria.
This study was reviewed and approved by the Ethics Committee of the Medical Faculty of TU Dresden (approval code: SR-EK-8012020, date of approval: 27 September 2021). All participants provided electronic informed consent, and this study was conducted in accordance with the Declaration of Helsinki and its latest amendments. Participants could enter a prize draw with the chance to win one of four EUR 25 Amazon gift vouchers.
The survey was designed using LimeSurvey (open-source survey tool; Version 5.0.11+210727, Hamburg, Germany: LimeSurvey GmbH). Participants could complete the survey in German language or English (in case German was not their primary language). The survey, raw data, and detailed description of the study methodology have been published elsewhere [32].
Demographic data included age, sex (male or female), living situation (alone or with family or friends), and occupational status (student or employed). Mood was assessed with single-item rating scales ranging from 0 (absent) to 10 (extreme) and included stress, anxiety, depression, fatigue, loneliness, optimism, and happiness [33,34]. Quality of life [35], sleep quality [36], and immune fitness [27] were rated on scales, ranging from 0 (very poor) to 10 (excellent). Assessments were made for five periods: (1) ‘BP’ (the period before the COVID-19 pandemic), (2) ‘L1’ (the first lockdown period, March–May 2020), (3) ‘NL1’ (the first no-lockdown period, summer 2020), (4) ‘L2’ (the second lockdown, November 2020 to May 2021), and (5) ‘NL2’ (the second no-lockdown period, summer 2021).
Statistical analyses were conducted with SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 29.0. Armonk, NY, USA: IBM Corp.). Mean and standard deviation (SD) were computed for all variables. Since the data were not normally distributed, nonparametric tests were applied. Within-subject comparisons of the five time points were conducted with the Related-Sample Friedman Two-Way Analysis of Variance by Ranks test. A Bonferroni correction was applied, so that differences were considered significant if p < 0.0125. Between-group comparisons were conducted with the Independent Samples Mann–Whitney U Tests. Groups were formed according to sex (males versus females), age (18–24 years old versus 25–35 years old), occupation (student versus employed), and living situation (alone versus with family or friends).
3. Results
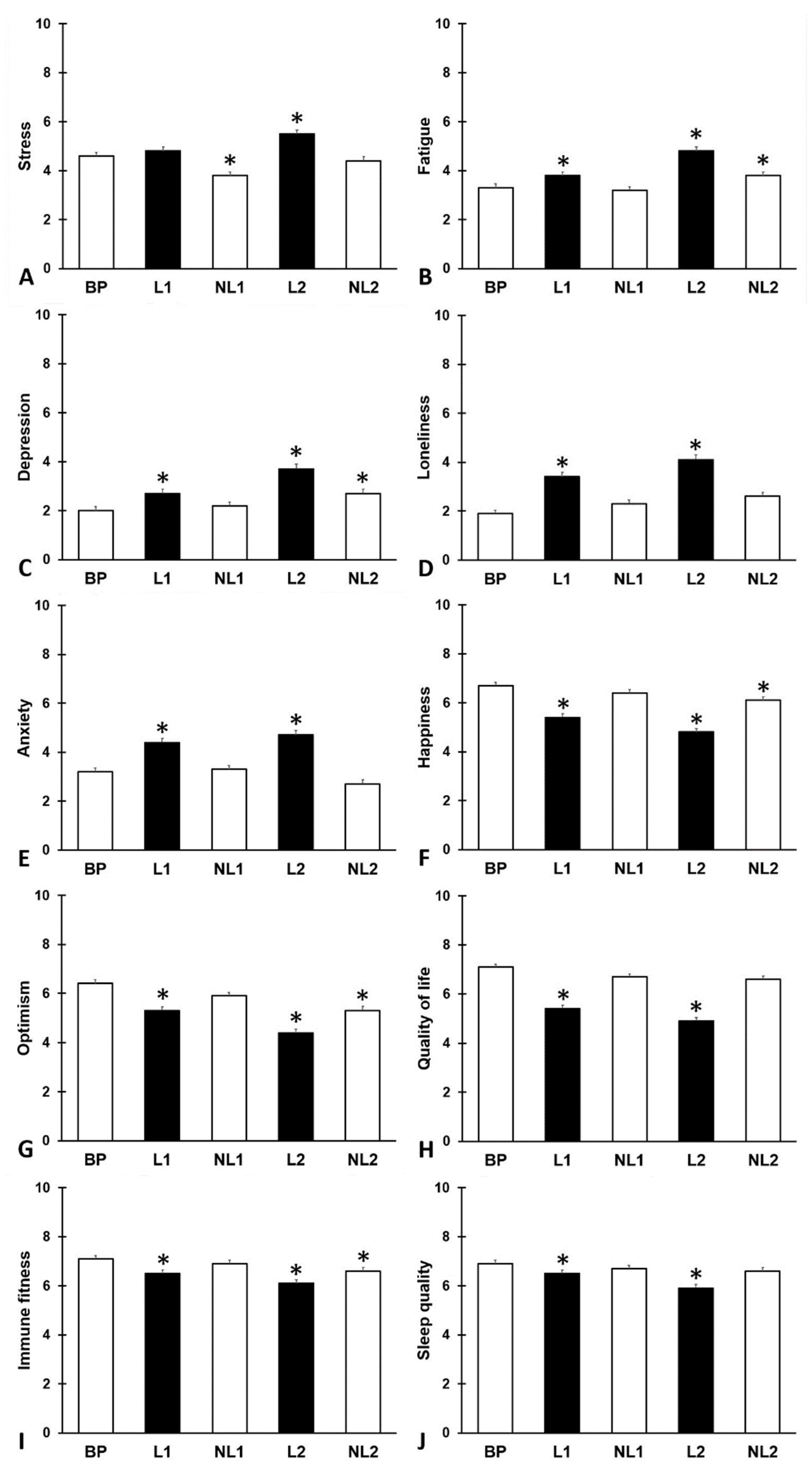
A total of N = 317 participants (103 men and 214 women) completed the survey. Their mean (SD) age was 25.5 (4.1) years old. Of the sample, N = 207 participants were students and N = 110 had a job during the COVID-19 pandemic. The study outcomes are summarized in Figure 1 and Table 1.
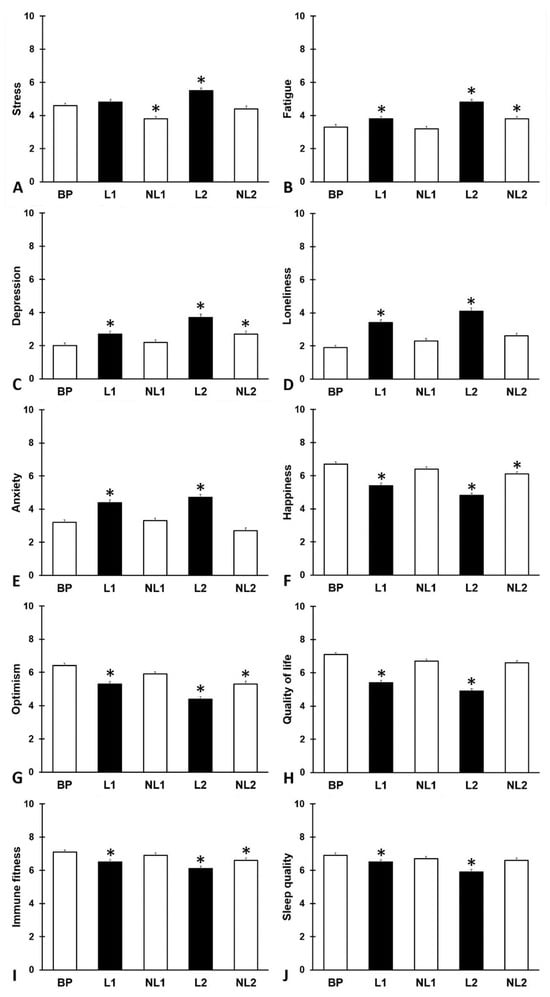
Figure 1.
Mood assessments. Mean and standard error are shown for (A) stress, (B) fatigue, (C) depression, (D) loneliness, (E) anxiety, (F) happiness, (G) optimism, (H) quality of life, (I) immune fitness, and (J) sleep quality. Abbreviations: BP = before the pandemic, L1 = lockdown 1, NL1 = no lockdown 1, L2 = lockdown 2, NL2 = no lockdown 2, COVID-19 = coronavirus disease 2019. Significant differences from ‘before the pandemic’ (p < 0.0125) are indicated by *.

Table 1.
Study outcomes.
Compared to BP, mood, quality of life, immune fitness, and sleep quality were significantly poorer during the two lockdown periods (L1 and L2). The effects were most pronounced during L2, with significant declines in fatigue, happiness, optimism, and immune fitness extending into NL2 compared to BP.
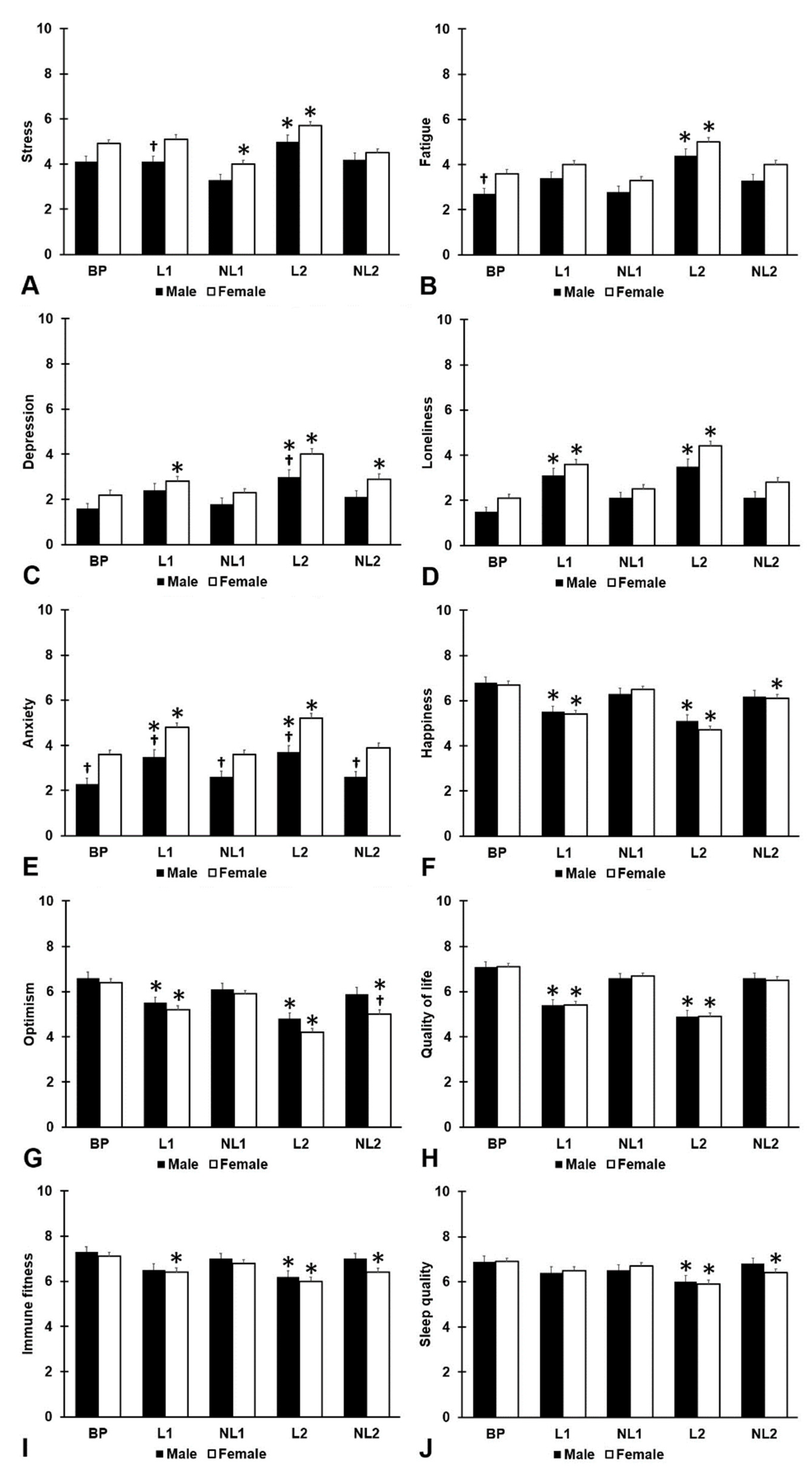
The study outcomes according to sex are summarized in Figure 2 and Table 2. Both males (N = 103, 32.5%) and females (N = 214, 67.5%) reported that compared to BP, mood, quality of life, immune fitness, and sleep quality were significantly poorer during the two lockdown periods (L1 and L2), with most pronounced effects observed during L2. Significant sex differences were found for stress, depression, anxiety, and optimism. During L1, the reported stress level of females was significantly higher than that of males (p = 0.003). Anxiety levels of females were significantly higher than those of males for all assessment periods, including BP (all p < 0.001). Depression levels of females during L2 were significantly higher compared to males (p = 0.010), and females were significantly less optimistic than males during NL2 (p = 0.011).
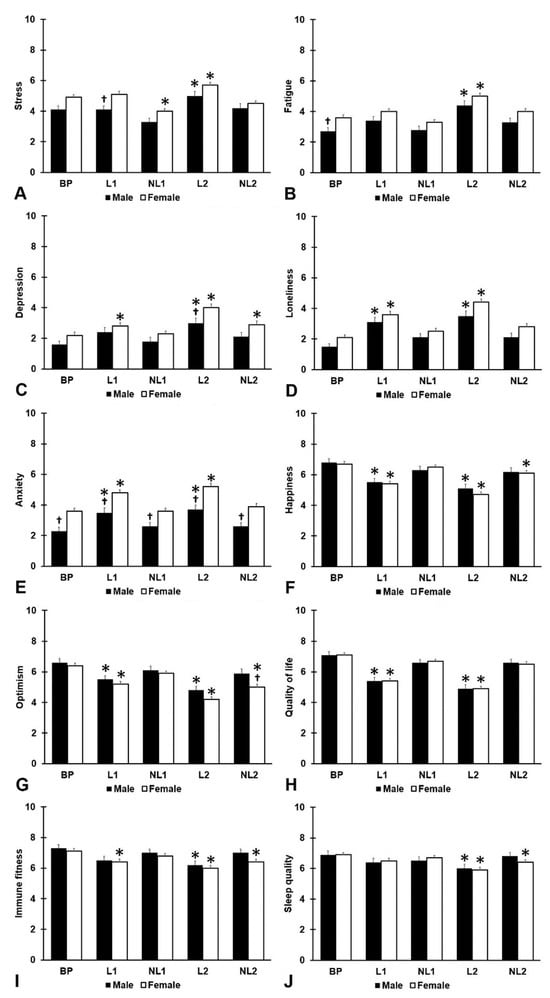
Figure 2.
Mood assessments according to sex. Mean and standard error are shown for (A) stress, (B) fatigue, (C) depression, (D) loneliness, (E) anxiety, (F) happiness, (G) optimism, (H) quality of life, (I) immune fitness, and (J) sleep quality. Abbreviations: BP = before the pandemic, L1 = lockdown 1, NL1 = no lockdown 1, L2 = lockdown 2, NL2 = no lockdown 2, COVID-19 = coronavirus disease 2019. Significant differences from ‘before the pandemic’ (p < 0.0125) are indicated by *. Significant differences between men and women (p < 0.010, after Bonferroni’s correction) are indicated by †.

Table 2.
Study outcomes according to sex.
No significant differences according to age were found (see Table 3). The 18–24-year-old group (N = 146, 46.1%) and the 25–35-year-old group (N = 171, 53.9%) reported similar patterns of poorer mood, immune fitness, and sleep quality during the lockdown periods.

Table 3.
Study outcomes according to age group.
Analyses according to occupation showed a similar outcome pattern (see Table 4). The only difference between students (N = 207, 65.3%) and those with a job (N = 110, 34.7%) was increased loneliness levels among students both before the pandemic (p = 0.013) and at L1 (p < 0.001), NL1 (p = 0.032), L2 (p = 0.001), and NL2 (p = 0.011). N = 98 (30.9%) participants were living alone, and N = 219 (69.1%) were living together with friends or family during the COVID-19 pandemic.

Table 4.
Study outcomes according to occupation.
No significant differences were found according to living situation (see Table 5). For both groups, comparable patterns of poorer mood, immune fitness, and sleep quality were reported for the two lockdown periods relative to BP, with the most pronounced effects observed during L2.

Table 5.
Study outcomes according to living situation.
4. Discussion
This study examined the impact of the COVID-19 pandemic on the mental well-being of young adults in Germany. The findings show significant declines in mood, quality of life, immune fitness, and sleep quality during the two lockdown periods, L1 and L2, with the most pronounced effects noted during L2. These outcomes align with prior research and underscore the need for targeted mental health support during such crises [16,27,28,37,38,39,40,41].
The observed decline in mood may be partially attributable to disruptions to daily routines, which may have exacerbated feelings of isolation and loneliness, especially among university students. The shift to remote learning and the absence of on-campus activities led to a significant sense of loss and isolation [42,43,44]. The closure of social outlets confined many young adults to their homes, intensifying loneliness due to the lack of customary social interactions and support networks [45,46,47]. Additionally, the transition to remote work and online learning required swift adaptation, likely contributing to declines in mood [48]. This shift may have intensified feelings of isolation and loneliness, particularly for those relying heavily on social interactions for support [49].
Uncertainties about the crisis duration and severity, along with fear of infection, likely heightened stress and anxiety levels [16,20]. COVID-19-related fear also correlated with increased depression symptoms, deteriorating health status, distress, and generalized anxiety symptoms [15,50]. The data reveal a significant increase in loneliness during the lockdown periods, aligning with international reports [39,40,41]. While research on the prevalence of loneliness among young Germans is mixed [51,52], the findings presented here add to the literature on its impact during the lockdowns. Some individuals found virtual means to connect, partially mitigating isolation [53].
Financial concerns significantly contributed to the decline in mood among young adults in Germany during the pandemic. Despite governmental efforts, financial hardships persisted [8,54]. The shutdown of businesses, particularly in the service industry, led to job losses and financial uncertainty [8]. Economic instability and reduced career prospects further fueled financial anxiety, placing considerable stress on young adults and students [8,11,55]. Furthermore, financial worries can exacerbate pre-existing mental health issues potentially triggered by the pandemic [55,56,57], compounding the observed decline in mood. Germany’s strong social market economy, despite its robust welfare systems, was strained during the pandemic. Support mechanisms, though helpful, could not fully mitigate economic anxieties, especially among students and young adults in precarious unemployment [5,6,7]. The initial public support for lockdown measures in Germany, which declined over time, correlates with the increase in anxiety and depression among young adults [5].
The current study showed a decline in both mood and sleep quality, likely due to lifestyle changes following the onset of the COVID-19 pandemic. Jabakhanji et al. [58] attribute the reduction in sleep quality to changes in lifestyles and worse mental health, highlighting the close relationship between sleep quality and mood. Lower sleep quality, in turn, can decrease immune fitness and increase susceptibility to infection [59].
Furthermore, movement restrictions and the closure of recreational facilities significantly reduced physical activity levels, leading to a more sedentary lifestyle [60]. Reduced physical activity can negatively impact sleep quality, mood, and quality of life [61,62,63,64]. Physical activity has been shown to improve depressive and anxiety symptoms, and those less active are more likely to experience loneliness [61,63,65,66]. Herbolsheimer et al. [67] reported significant reductions in physical activity and increased sedentary time among German participants during the pandemic, with over a third failing to meet the WHO’s physical activity guidelines [68]. Additionally, depressive symptoms were associated with increased sedentary behavior, particularly among young adults, aligning with findings linking reduced physical activity to greater distress and anxiety symptoms [67,69].
The significant decreases in immune fitness may be influenced by various stressors prevalent during the pandemic. Increased stress and anxiety levels, declines in sleep quality, reduced physical activity, and social isolation can all negatively impact immune functioning [70]. Stress, characterized by the release of hormones such as cortisol, can significantly suppress immune functioning, thereby increasing susceptibility to infection. If stress becomes chronic, it can lead to glucocorticoid (receptor-) resistance, hindering the hypothalamic–pituitary–adrenal (HPA) axis’s ability to regulate pro-inflammatory cytokines effectively, resulting in heightened levels of inflammation [71]. Social isolation can exacerbate distress, further compromising immune function [72]. Additionally, declines in sleep quality and reduced physical activity are known to weaken immune function [73]. Poor sleep quality can disrupt circadian rhythms and suppress immune responses, while reduced physical activity can weaken immune defenses [74]. Regular exercise offers significant benefits for the immune systems in terms of susceptibility, progression, and outcome of infections like COVID-19 [75]. The combined effect of these factors can contribute to weakened immune functioning and a reduction in self-reported immune fitness. As shown previously, lower immune fitness makes individuals more vulnerable to illnesses [76], including the presence and severity of COVID-19 symptoms [77].
Several sex differences were observed. Women consistently reported higher anxiety levels across all time periods, aligning with existing research [78,79,80]. This observation may arise from sex differences in factors such as socialization, psychosocial traits, biological distinctions in brain structures, and hormonal fluctuations. Neurobiological studies have identified differences in amygdala volume and cerebral blood flow, as well as serotonin transporter gene expression, which may increase women’s susceptibility to anxiety [80,81,82,83]. Additionally, women may be more likely to seek help and disclose mental health concerns, while men might underreport symptoms due to societal masculinity norms [84].
The observed increase in depression levels among women during the second lockdown may be related to occupational representation, caregiving responsibilities, and the economic impact of the COVID-19 pandemic [85]. Women in Germany are overrepresented in sectors like healthcare, education, and retail, which were heavily affected by lockdown measures, leading to decreased work-related social interactions, economic instability, and stress [86,87,88]. Additionally, the closure of schools and childcare services increased caregiving responsibilities, adding stress as women balanced childcare, household duties, and work [85,89]. Many women reduced their working hours to manage increased caregiving responsibilities, as they were often the lower-earning parents, making it economically sensible for them to take on more caregiving responsibilities [14]. The cumulative effects of prolonged stress and reduced social interaction causing feelings of loneliness likely contributed to the observed increase in depression during the second lockdown [3,88,90,91,92].
This study has several limitations that should be considered when interpreting its findings. The recruitment strategy, which utilized university emails and printed flyers in Dresden, might lead to a sampling bias favoring more educated individuals from urban areas, thereby limiting the generalizability of the results to other age groups or populations. Additionally, this study relied on retrospective self-report measures to assess mood, quality of life, and immune fitness, which are vulnerable to recall bias and social desirability bias. The latter could have introduced inaccuracies in the provided answers to the survey. Important variables such as pre-existing mental health conditions, coping strategies, social support networks, and access to healthcare services, which could influence young adults’ well-being, were not assessed, limiting our ability to comprehensively understand the factors affecting their overall well-being. The cross-sectional study design also precludes the establishment of causal relationships between variables. Moreover, the survey’s availability solely in English and German may have introduced language and cultural biases, potentially excluding non-speakers. Future studies should address these limitations by exploring the long-term effects of the COVID-19 pandemic on mental health outcomes, evaluating intervention strategies, and examining how social factors contribute to mental health disparities to enhance our understanding of how crises impact mental well-being and inform effective responses.
5. Conclusions
This study of young adults in Germany during the COVID-19 pandemic highlights the profound negative impacts of the pandemic and associated lockdowns on mood, quality of life, immune fitness, and sleep quality. Our results reveal significant sex differences, with women consistently reporting higher levels of anxiety, more stress during the first lockdown, and higher depression scores during the second lockdown. The findings underscore the necessity for ongoing mental health support and the integration of these considerations into public health planning and response.
Author Contributions
Conceptualization, P.A.H., P.K., A.H.K., J.G., A.-K.S. and J.C.V.; methodology, P.A.H. and J.C.V.; data collection, A.H.K.; formal analysis, J.C.V.; writing—original draft preparation, P.A.H. and J.C.V.; writing—review and editing, P.A.H., P.K., A.H.K., J.G., A.-K.S. and J.C.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Ethics Committee of the Medical Faculty of the TU Dresden (approval code: SR-EK-8012020, date of approval: 27 September 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset is published open access in the MDPI journal Data and is available online as a supplement to Koyun et al. [32].
Conflicts of Interest
The authors declare no conflicts of interest in relation to this publication. Over the past 3 years, J.V. has received research grants from Inbiose and has acted as a consultant/advisor for Eisai, KNMP, Med Solutions, Mozand, Red Bull, Sen-Jam Pharmaceutical, and Toast!. J.G. is a part-time employee of Danone Nutricia Research and received research grants from the Nutricia research foundation, Top Institute Pharma, Top Institute Food and Nutrition, GSK, STW, NWO, Friesland Campina, CCC, Raak-Pro, and EU. P.K. is the CEO of PanGenix. The other authors have no potential conflicts of interest to disclose.
References
- Klein, S.; Fegert, J.M.; Geprägs, A.; Brähler, E.; Clemens, V. The impact of the COVID-19 pandemic on health, quality of life and intrafamilial relations—A Population-Based Survey in Germany. Front. Psychol. 2022, 13, 844057. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Benke, C.; Autenrieth, L.K.; Asselmann, E.; Pané-Farré, C.A. One year after the COVID-19 outbreak in Germany: Long-term changes in depression, anxiety, loneliness, distress and life satisfaction. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 273, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Fuchs-Schündeln, N.; Kuhn, M.; Tertilt, M. The Short-Run Macro Implications of School and Child-Care Closures. In IZA Discussion Paper Series (Report No. 13353); IZA Institute of Labor Economics: Bonn, Germany, 2020; Available online: https://docs.iza.org/dp13353.pdf (accessed on 5 October 2024).
- Naumann, E.; Möhring, K.; Reifenscheid, M.; Wenz, A.; Rettig, T.; Lehrer, R.; Krieger, U.; Juhl, S.; Friedel, S.; Fikel, M.; et al. COVID-19 policies in Germany and their social, political, and psychological consequences. Eur. Policy Anal. 2020, 6, 191–202. [Google Scholar] [CrossRef]
- Braband, C.; Consiglio, V.S.; Grabka, M.M.; Hainbach, N.; Königs, S. Disparities in Labour Market and Income Trends During the First Year of the COVID-19 Crisis. Evidence from Germany. OECD, 2022. Available online: https://www.oecd.org/en/publications/disparities-in-labour-market-and-income-trends-during-the-first-year-of-the-covid-19-crisis_e72b8b65-en.html (accessed on 1 October 2024).
- Herzog-Stein, A.; Nüß, P.; Peede, L.; Stein, U. Germany and the United States in coronavirus distress: Internal versus external labour market flexibility. J. Labour Mark. Res. 2022, 56, 11. [Google Scholar] [CrossRef]
- Gewalt, S.C.; Berger, S.; Krisam, R.; Krisam, J.; Breuer, M. University students’ economic situation during the COVID-19 pandemic: A cross-sectional study in Germany. PLoS ONE 2022, 17, e0275055. [Google Scholar] [CrossRef]
- Federal Statistical Office. Unemployed in Germany. Available online: https://www.destatis.de/EN/Themes/Economy/Short-Term-Indicators/Labour-Market/arb110.html#241576 (accessed on 16 May 2024).
- Hövermann, A. Soziale Lebenslagen, soziale Ungleichheit und Corona—Auswirkungen für Erwerbstätige. WSI Policy Brief 2020, 44, 1–24. [Google Scholar]
- Aucejo, E.M.; French, J.; Araya, M.P.U.; Zafar, B. The impact of COVID-19 on student experiences and expectations: Evidence from a survey. J. Public Econ. 2020, 191, 104271. [Google Scholar] [CrossRef]
- Gong, Y.; Liu, X.; Zheng, Y.; Mei, H.; Que, J.; Yuan, K.; Yan, W.; Shi, L.; Meng, S.; Bao, Y.; et al. COVID-19 induced economic slowdown and mental health issues. Front. Psychol. 2022, 13, 777350. [Google Scholar] [CrossRef]
- Cheng, G.H.; Chan, D.K. Who Suffers More from Job Insecurity? A Meta-Analytic Review. Appl. Psychol. 2007, 57, 272–303. [Google Scholar] [CrossRef]
- Kohlrausch, B.; Zucco, A. Die Corona-Krise trifft Frauen doppelt: Weniger Erwerbseinkommen und mehr Sorgearbeit. WSI Policy Brief 2020, 40, 1–14. [Google Scholar]
- Bäuerle, A.; Steinbach, J.; Schweda, A.; Beckord, J.; Hetkamp, M.; Weismüller, B.; Kohler, H.; Musche, V.; Dörrie, N.; Teufel, M.; et al. Mental health burden of the COVID-19 outbreak in Germany: Predictors of mental health impairment. J. Prim. Care Community Health 2020, 11, 215013272095368. [Google Scholar] [CrossRef] [PubMed]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef] [PubMed]
- Peters, A.; Rospleszcz, S.; Greiser, K.H.; Dallavalle, M.; Berger, K. The impact of the COVID-19 pandemic on self-reported health. Dtsch. Arztebl. Int. 2020, 117, 861–867. [Google Scholar] [CrossRef]
- Salanti, G.; Peter, N.; Tonia, T.; Holloway, A.; White, I.R.; Darwish, L.; Low, N.; Egger, M.; Haas, A.D.; Fazel, S.; et al. The Impact of the COVID-19 Pandemic and Associated Control Measures on the Mental Health of the General Population: A Systematic Review and Dose-Response Meta-analysis. Ann. Intern. Med. 2022, 175, 1560–1571. [Google Scholar] [CrossRef]
- Petzold, M.B.; Bendau, A.; Plag, J.; Pyrkosch, L.; Maricic, L.M.; Betzler, F.; Rogoll, J.; Große, J.; Ströhle, A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020, 10, e01745. [Google Scholar] [CrossRef]
- Schelhorn, I.; Ecker, A.; Lüdtke, M.N.; Rehm, S.; Tran, T.; Bereznai, J.L.; Meyer, M.L.; Sütterlin, S.; Kinateder, M.; Lugo, R.G.; et al. Psychological burden during the COVID-19 pandemic in Germany. Front. Psychol. 2021, 12, 640518. [Google Scholar] [CrossRef]
- Bonnewyn, A.; Bruffaerts, R.; Van Oyen, H.; Demarest, S.; Demyttenaere, K. The impact of mental disorders on daily functioning in the Belgian community. Results of the study “European Study on Epidemiology of Mental Disorders” (ESemeD). Rev. Med. Liege. 2005, 60, 849–854. [Google Scholar]
- Dhabhar, F.S. Effects of stress on immune function: The good, the bad, and the beautiful. Immunol. Res. 2014, 58, 193–210. [Google Scholar] [CrossRef]
- Segerstrom, S.C.; Miller, G.E. Psychological stress and the human Immune System: A Meta-analytic study of 30 years of inquiry. Psychol. Bull. 2004, 130, 601–630. [Google Scholar] [CrossRef] [PubMed]
- De Almondes, K.M.; Marín Agudelo, H.A.; Jiménez-Correa, U. Impact of sleep deprivation on emotional regulation and the immune system of healthcare workers as a risk factor for COVID 19: Practical recommendations from a task force of the Latin American Association of Sleep Psychology. Front. Psychol. 2021, 12, 564227. [Google Scholar] [CrossRef] [PubMed]
- Lueke, N.A.; Assar, A. Poor sleep quality and reduced immune function among college students: Perceived stress and depression as mediators. J. Am. Coll. Health 2022, 72, 1112–1119. [Google Scholar] [CrossRef] [PubMed]
- Verster, J.C.; Kraneveld, A.D.; Garssen, J. The assessment of immune fitness. J. Clin. Med. 2022, 12, 22. [Google Scholar] [CrossRef]
- Hendriksen, P.A.; Garssen, J.; Bijlsma, E.Y.; Engels, F.; Bruce, G.; Verster, J.C. COVID-19 lockdown-related changes in mood, health and academic functioning. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 1440–1461. [Google Scholar] [CrossRef]
- Hendriksen, P.A.; Kiani, P.; Merlo, A.; Czerniczyniec, A.; Lores-Arnaiz, S.; Bruce, G.; Garssen, J.; Karadayian, A.; Verster, J.C. Mood and quality of life during the COVID-19 pandemic of Buenos Aires university students. Rev. Argent. Clin. Psicol. 2024, 33, 1–11. [Google Scholar]
- Hendriksen, P.A.; Merlo, A.; Garssen, J.; Bijlsma, E.Y.; Engels, F.; Bruce, G.; Verster, J.C. The impact of COVID-19 lockdown on academic functioning and mood: Data from Dutch pharmacy students, PhD candidates and post-docs. Data 2021, 6, 120. [Google Scholar] [CrossRef]
- Hendriksen, P.A.; Kiani, P.; Merlo, A.; Karadayian, A.; Czerniczyniec, A.; Lores-Arnaiz, S.; Bruce, G.; Verster, J.C. The COLIBAS study—COVID-19 lockdown effects on mood, academic functioning, alcohol consumption, and perceived immune fitness: Data from Buenos Aires university students. Data 2022, 7, 131. [Google Scholar] [CrossRef]
- Koyun, A.H.; Hendriksen, P.A.; Kiani, P.; Merlo, A.; Balikji, J.; Stock, A.-K.; Verster, J.C. COVID-19 lockdown effects on mood, alcohol consumption, academic functioning, and perceived immune fitness: Data from young adults in Germany. Data 2022, 7, 125. [Google Scholar] [CrossRef]
- Verster, J.C.; Sandalova, E.; Garssen, J.; Bruce, G. The use of single-item ratings versus traditional multiple-item questionnaires to assess mood and health. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 183–198. [Google Scholar] [CrossRef]
- Verster, J.C.; Mulder, K.E.; Verheul, M.C.; Van Oostrom, E.C.; Hendriksen, P.A.; Scholey, A.; Garssen, J. Test-retest reliability of single-item assessments of immune fitness, mood, and quality of life. Heliyon 2023, 9, e15280. [Google Scholar] [CrossRef]
- Verster, J.C.; Išerić, E.; Ulijn, G.A.; Oskam, S.M.P.; Garssen, J. Single-item assessment of Quality of Life: Scale validation and associations with mood and health outcomes. J. Clin. Med. 2024, 13, 5217. [Google Scholar] [CrossRef] [PubMed]
- Snyder, E.; Cai, B.; DeMuro, C.; Morrison, M.F.; Ball, W. A new single-item sleep quality scale: Results of psychometric evaluation in patients with chronic primary insomnia and depression. J. Clin. Sleep. Med. 2018, 14, 1849–1857. [Google Scholar] [CrossRef]
- Schwinger, M.; Trautner, M.; Kärchner, H.; Otterpohl, N. Psychological impact of corona lockdown in Germany: Changes in need satisfaction, well-being, anxiety, and depression. Int. J. Environ. Res. Public Health 2020, 17, 9083. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.; Kneer, J.; Krüger, T.H.C. Mental Health, Sense of Coherence, and Interpersonal Violence during the COVID-19 Pandemic Lockdown in Germany. J. Clin. Med. 2020, 9, 3708. [Google Scholar] [CrossRef] [PubMed]
- Dahlberg, L. Loneliness during the COVID-19 pandemic. Aging Mental Health 2021, 25, 1161–1164. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, R.; Burns, A.; Leavey, G.; Leroi, I.; Burholt, V.; Lubben, J.; Holt-Lunstad, J.; Victor, C.; Lawlor, B.; Vilar-Compte, M.; et al. Impact of the COVID-19 pandemic on loneliness and social isolation: A Multi-country study. Int. J. Environ. Res. Public Health 2021, 18, 9982. [Google Scholar] [CrossRef]
- Ernst, M.; Niederer, D.; Werner, A.M.; Czaja, S.J.; Mikton, C.; Ong, A.D.; Rosen, T.; Brähler, E.; Beutel, M.E. Loneliness before and during the COVID-19 pandemic: A systematic review with meta-analysis. Am. Psychol. 2022, 77, 660–677. [Google Scholar] [CrossRef]
- Sigurdardottir, M.S.; Torfason, M.T.; Jonsdottir, A.H. Social tie formation of COVID-19 students: Evidence from a two-cohort longitudinal study. Higher Educ. 2022, 86, 333–351. [Google Scholar] [CrossRef]
- Zhou, Y.; Xu, X.; Schönrock-Adema, J.; Brouwer, J.; Bos, N.A.; Diemers, A.D. Influence of online collaborative learning on social network and academic performance of medical students: Lessons learned from the COVID-19 pandemic. Front. Med. 2023, 10, 1242638. [Google Scholar] [CrossRef]
- Birmingham, W.C.; Wadsworth, L.L.; Lassetter, J.H.; Graff, T.C.; Lauren, E.; Hung, M. COVID-19 lockdown: Impact on college students’ lives. J. Am. Coll. Health 2021, 71, 879–893. [Google Scholar] [CrossRef] [PubMed]
- Wessels, M.; Utegaliyev, N.; Bernhard, C.; Welsch, R.; Oberfeld, D.; Thönes, S.; Von Castell, C. Adapting to the pandemic: Longitudinal effects of social restrictions on time perception and boredom during the COVID-19 pandemic in Germany. Sci. Rep. 2022, 12, 1863. [Google Scholar] [CrossRef] [PubMed]
- Breetzke, J.; Wild, E. Social connections at work and mental health during the first wave of the COVID-19 pandemic: Evidence from employees in Germany. PLoS ONE 2022, 17, e0264602. [Google Scholar] [CrossRef] [PubMed]
- Geirdal, A.Ø.; Ruffolo, M.; Leung, J.; Thygesen, H.; Price, D.; Bonsaksen, T.; Schoultz, M. Mental health, quality of life, well-being, loneliness and use of social media in a time of social distancing during the COVID-19 outbreak. A cross-country comparative study. J. Ment. Health 2021, 30, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Kornilaki, E.N. The psychological effect of COVID-19 quarantine on Greek young adults: Risk factors and the protective role of daily routine and altruism. Int. J. Psychol. 2021, 57, 33–42. [Google Scholar] [CrossRef]
- Hoss, T.; Ancina, A.; Kaspar, K. Forced remote learning during the COVID-19 pandemic in Germany: A mixed-methods study on students’ positive and negative expectations. Front. Psychol. 2021, 12, 642616. [Google Scholar] [CrossRef]
- Jacob, L.; Smith, L.; Koyanagi, A.; Oh, H.Y.; Tanislav, C.; Shin, J.I.; Konrad, M.; Kostev, K. Impact of the coronavirus 2019 (COVID-19) pandemic on anxiety diagnosis in general practices in Germany. J. Psychiatr. Res. 2021, 143, 528–533. [Google Scholar] [CrossRef]
- Berger, K.; Riedel-Heller, S.; Pabst, A.; Rietschel, M.; Richter, D.; NAKO-Konsortium. Einsamkeit während der ersten Welle der SARS-CoV-2-Pandemie—Ergebnisse der NAKO-Gesundheitsstudie [Loneliness during the first wave of the SARS-CoV-2 pandemic-results of the German National Cohort (NAKO)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2021, 64, 1157–1164. [Google Scholar] [CrossRef]
- Ahrens, K.F.; Neumann, R.J.; Kollmann, B.; Brokelmann, J.; Von Werthern, N.M.; Malyshau, A.; Weichert, D.; Lutz, B.; Fiebach, C.J.; Wessa, M.; et al. Impact of COVID-19 lockdown on mental health in Germany: Longitudinal observation of different mental health trajectories and protective factors. Transl. Psychiatry 2021, 11, 392. [Google Scholar] [CrossRef]
- Hopp, M.D.S.; Händel, M.; Bedenlier, S.; Glaeser-Zikuda, M.; Kammerl, R.; Kopp, B.; Ziegler, A. The structure of social networks and its link to higher education students’ Socio-Emotional loneliness during COVID-19. Front. Psychol. 2022, 12, 733867. [Google Scholar] [CrossRef]
- Plenty, S.; Bracegirdle, C.; Dollmann, J.; Spiegler, O. Changes in young adults’ mental well-being before and during the early stage of the COVID-19 pandemic: Disparities between ethnic groups in Germany. Child Adolesc. Psychiatry Ment. Health 2021, 15, 69. [Google Scholar] [CrossRef] [PubMed]
- Sujan, M.H.; Tasnim, R.; Islam, M.S.; Ferdous, M.; Haghighathoseini, A.; Koly, K.N.; Pardhan, S. Financial hardship and mental health conditions in people with underlying health conditions during the COVID-19 pandemic in Bangladesh. Heliyon 2022, 8, e10499. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.; Fan, L. The relationship between financial worries and psychological distress among U.S. adults. J. Fam. Econ. Issues 2022, 44, 16–33. [Google Scholar] [CrossRef] [PubMed]
- Kiely, K.M.; Leach, L.S.; Olesen, S.C.; Butterworth, P. How financial hardship is associated with the onset of mental health problems over time. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 909–918. [Google Scholar] [CrossRef] [PubMed]
- Jabakhanji, S.B.; Lepinteur, A.; Menta, G.; Piper, A.; Vögele, C. Sleep quality and the evolution of the COVID-19 pandemic in five European countries. PLoS ONE 2022, 17, e0278971. [Google Scholar] [CrossRef]
- Cohen, S.; Doyle, W.J.; Alper, C.M.; Janicki-Deverts, D.; Turner, R.B. Sleep habits and susceptibility to the common cold. Arch. Intern. Med. 2009, 169, 62–67. [Google Scholar] [CrossRef]
- Wunsch, K.; Kienberger, K.; Niessner, C. Changes in physical activity patterns due to the COVID-19 pandemic: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2022, 19, 2250. [Google Scholar] [CrossRef]
- Alnawwar, M.A.; Alraddadi, M.I.; Algethmi, R.A.; Salem, G.A.; Salem, M.A.; Alharbi, A.A. The effect of physical activity on sleep quality and sleep disorder: A systematic review. Cureus 2023, 15, e43595. [Google Scholar] [CrossRef]
- Dolezal, B.A.; Neufeld, E.V.; Boland, D.M.; Martin, J.L.; Cooper, C.B. Interrelationship between sleep and exercise: A systematic review. Adv. Prev. Med. 2017, 2017, 1364387. [Google Scholar]
- Mahindru, A.; Patil, P.; Agrawal, V. Role of physical activity on mental health and well-being: A review. Cureus 2023, 15, e33475. [Google Scholar] [CrossRef]
- Mata, J.; Wenz, A.; Rettig, T.; Reifenscheid, M.; Möhring, K.; Krieger, U.; Friedel, S.; Fikel, M.; Cornesse, C.; Blom, A.G.; et al. Health behaviors and mental health during the COVID-19 pandemic: A longitudinal population-based survey in Germany. Soc. Sci. Med. 2021, 287, 114333. [Google Scholar] [CrossRef] [PubMed]
- Basso, J.C.; Suzuki, W.A. The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: A review. Brain Plasticity 2017, 2, 127–152. [Google Scholar] [CrossRef]
- Wenig, V.; Heumann, E.; Stock, C.; Busse, H.; Negash, S.; Pischke, C.R.; Heinrichs, K. Associations of loneliness with mental health and with social and physical activity among university students in Germany: Results of the COVID-19 German student well-being study (C19 GSWS). Front. Public Health 2023, 11, 1284460. [Google Scholar] [CrossRef] [PubMed]
- Herbolsheimer, F.; Peters, A.; Wagner, S.; Willich, S.N.; Krist, L.; Pischon, T.; Nimptsch, K.; Gastell, S.; Brandes, M.; Brandes, B.; et al. Changes in physical activity and sedentary behavior during the first COVID-19 pandemic- restrictions in Germany: A nationwide survey: Running head: Physical activity during the COVID-19 restrictions. BMC Public Health 2024, 24, 433. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 5 October 2022).
- Czenczek-Lewandowska, E.; Leszczak, J.; Wyszyńska, J.; Baran, J.; Weres, A.; Lewandowski, B. The role of physical activity in the reduction of generalised anxiety disorder in young adults in the context of COVID-19 pandemic. Int. J. Environ. Res. Public Health 2022, 19, 11086. [Google Scholar] [CrossRef]
- Hekmatnia, Y.; Rahmani, F.; Feili, Z.; Ebrahimzadeh, F. A review of the effect of COVID-19 on immune responses of the body. J. Fam. Med. Primary Care 2022, 11, 1624–1632. [Google Scholar] [CrossRef]
- Russell, G.; Lightman, S. The human stress response. Nat. Rev. Endocrinol. 2019, 15, 525–534. [Google Scholar] [CrossRef]
- Pourriyahi, H.; Yazdanpanah, N.; Saghazadeh, A.; Rezaei, N. Loneliness: An immunometabolic syndrome. Int. J. Environ. Res. Public Health 2021, 18, 12162. [Google Scholar] [CrossRef]
- Besedovsky, L.; Lange, T.; Born, J. Sleep and immune function. Pflugers Arch. 2012, 463, 121–137. [Google Scholar] [CrossRef]
- Nieman, D.C.; Wentz, L.M. The compelling link between physical activity and the body’s defense system. J. Sport Health Sci. 2019, 8, 201–217. [Google Scholar] [CrossRef]
- Da Silveira, M.P.; Da Silva Fagundes, K.K.; Bizuti, M.R.; Starck, É.; Rossi, R.C.; De Resende ESilva, D.T. Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature. Clin. Exp. Med. 2020, 21, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Kiani, P.; Balikji, J.; Kraneveld, A.D.; Garssen, J.; Bruce, G.; Verster, J.C. Pandemic preparedness: The importance of adequate immune fitness. J. Clin. Med. 2022, 11, 2442. [Google Scholar] [CrossRef] [PubMed]
- Verster, J.C.; Išerić, E.; Garssen, J. The concept and assessment of immune fitness. Explor. Immunol. 2023, 3, 500–505. [Google Scholar] [CrossRef]
- Abdel-Khalek, A.M.; Maltby, J. Differences in Anxiety Scores of College Students from Germany, Spain, the United Kingdom, and the USA. Psychol. Rep. 2009, 104, 624–626. [Google Scholar] [CrossRef] [PubMed]
- Otten, D.; Tibubos, A.N.; Schomerus, G.; Brähler, E.; Binder, H.; Kruse, J.; Ladwig, K.; Wild, P.S.; Grabe, H.J.; Beutel, M.E. Similarities and differences of mental health in women and men: A systematic review of findings in three large German cohorts. Front. Public Health 2021, 9, 553071. [Google Scholar] [CrossRef] [PubMed]
- Cerasa, A.; Quattrone, A.; Piras, F.; Mangone, G.; Magariello, A.; Fagioli, S.; Girardi, P.; Muglia, M.; Caltagirone, C.; Spalletta, G. 5-HTTLPR, anxiety and gender interaction moderates right amygdala volume in healthy subjects. Soc. Cogn. Affect. Neurosci. 2013, 9, 1537–1545. [Google Scholar] [CrossRef]
- Wüst, S.; Kumsta, R.; Treutlein, J.; Frank, J.; Entringer, S.; Schulze, T.G.; Rietschel, M. Sex-specific association between the 5-HTT gene-linked polymorphic region and basal cortisol secretion. Psychoneuroendocrinol. 2009, 34, 972–982. [Google Scholar] [CrossRef]
- Kaczkurkin, A.N.; Moore, T.M.; Ruparel, K.; Ciric, R.; Calkins, M.E.; Shinohara, R.T.; Elliott, M.A.; Hopson, R.; Roalf, D.R.; Vandekar, S.N.; et al. Elevated amygdala perfusion mediates developmental sex differences in trait anxiety. Biol. Psychiatry 2016, 80, 775–785. [Google Scholar] [CrossRef]
- Kaczkurkin, A.N.; Raznahan, A.; Satterthwaite, T.D. Sex differences in the developing brain: Insights from multimodal neuroimaging. Neuropsychopharmacol. 2018, 44, 71–85. [Google Scholar] [CrossRef]
- Fisher, K.; Seidler, Z.E.; King, K.; Oliffe, J.L.; Rice, S.M. Men’s anxiety: A systematic review. J. Affect. Disord. 2021, 295, 688–702. [Google Scholar] [CrossRef]
- Huebener, M.; Waights, S.; Spiess, C.K.; Siegel, N.A.; Wagner, G.G. Parental well-being in times of COVID-19 in Germany. Rev. Econ. Household 2021, 19, 91–122. [Google Scholar] [CrossRef] [PubMed]
- Eurostat. Jobs with the Highest Share of Women in Q3 2021. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20220304-1 (accessed on 4 March 2022).
- Statista. Share of Women and Men in Different Professions in Germany 2023. Available online: https://www.statista.com/statistics/1407416/share-women-different-professions-germany/ (accessed on 19 February 2024).
- Liu, S.; Yang, L.; Zhang, C.; Xu, Y.; Cai, L.; Ma, S.; Wang, Y.; Cai, Z.; Du, H.; Li, R.; et al. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J. Psychiatr. Res. 2021, 137, 393–400. [Google Scholar] [CrossRef]
- Parmar, J.; L’Heureux, T.; Lobchuk, M.; Penner, J.; Charles, L.; St Amant, O.; Ward-Griffin, C.; Anderson, S. Double-duty caregivers enduring COVID-19 pandemic to endemic: “It’s just wearing me down”. PLoS ONE 2024, 19, e0298584. [Google Scholar] [CrossRef] [PubMed]
- Beutel, M.E.; Klein, E.M.; Brähler, E.; Reiner, I.; Jünger, C.; Michal, M.; Wiltink, J.; Wild, P.S.; Münzel, T.; Lackner, K.J.; et al. Loneliness in the general population: Prevalence, determinants and relations to mental health. BMC Psychiatry 2017, 17, 97. [Google Scholar] [CrossRef] [PubMed]
- Erzen, E.; Çikrikci, Ö. The effect of loneliness on depression: A meta-analysis. Int. J. Soc. Psychiatry 2018, 64, 427–435. [Google Scholar] [CrossRef]
- Tafet, G.E.; Nemeroff, C.B. The links between stress and depression: Psychoneuroendocrinological, genetic, and environmental interactions. J. Neuropsychiatry Clin. Neurosci. 2016, 28, 77–88. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).