Abstract
(1) Background: Upper body pain, particularly in the limbs and shoulders, is a common symptom among patients with spinal cord injury (SCI) and wheelchair users. Despite the focus on resistance muscle training as a suitable intervention for SCI individuals, findings across different populations and conditions have been inconsistent. (2) Methods: We conducted a systematic review to elucidate the correlations among exercise interventions, muscle strength enhancement, and pain reduction. A comprehensive literature search was performed using the keywords “spinal cord injury,” “pain,” “exercise,” “disability,” “paraplegia,” and “tetraplegia” across the DBpia, EMBASE, PubMed, and Science Direct databases. (3) Results: From 191 identified articles, 13 studies (1 from Korea and 12 from other countries) were selected for analysis. The results indicate that exercise interventions are effective in reducing pain in patients with SCI, with a particular emphasis on alleviating shoulder pain. (4) Conclusion: Exercise is essential for pain reduction in patients with SCI, especially those experiencing shoulder pain. However, there is a notable lack of experimental research focusing primarily on pain. The development of appropriate measurement instruments is crucial for the prevention and relief of pain in this patient population.
1. Introduction
Spinal Cord Injury (SCI) is a severe medical condition resulting from damage to the spinal cord that affects motor, sensory, and autonomic functions. This introductory section aims to delineate the epidemiology of SCI, define and classify the associated pain types, identify the causes of pain specific to SCI patients, and discuss relevant pain scoring systems. SCI primarily results from traumatic events such as vehicular accidents, falls, sports injuries, or violent acts. The global incidence of SCI varies, but it is estimated that there are approximately 54 cases per million people per year, which emphasizes this condition’s significant public health burden [1]. The epidemiological data highlight the need for targeted preventive measures and improved healthcare strategies to manage the long-term outcomes of SCI. Pain in SCI can be broadly classified into nociceptive and neuropathic pain. Nociceptive pain is caused by damage to non-neural tissue and is characterized by aching or throbbing in muscles or joints. In contrast, neuropathic pain occurs directly due to spinal cord damage and is often described as sharp, intense, or burning [1,2]. Understanding these distinctions is crucial for accurate diagnosis and treatment. Pain in SCI patients can stem from various sources. Neuropathic pain can arise from the injury site itself or from dysfunctional nerve fibers. Nociceptive pain may be related to overuse of certain muscle groups or joints due to altered mobility patterns [2]. Secondary complications such as infections, pressure sores, and urinary tract infections can also contribute to pain in SCI patients.
Upper limb and shoulder pain are some of the most common musculoskeletal pains experienced by patients with spinal cord injuries (SCI) [1]. Wheelchairs are used for mobility and activities of daily living among patients with SCI with complete or incomplete lower limb functional impairments, and more than 50% of wheelchair users suffer from injuries and pain due to the overuse of their upper limbs [2]. The upper limbs bear repetitive strain during everyday wheelchair use, leading to shoulder joint damage and various pains and diseases [3]. According to Dalyan et al. [4], 76 out of 130 patients with SCI (58.5%) suffered from upper extremity pain, with 71% reporting shoulder pain, 53% with wrist pain, 43% with hand pain, and 35% with elbow pain, and many patients experience pain in more than one location. Shoulder damage and pain are the most characteristic symptoms for patients with SCI using manual wheelchairs, and these lead to disorders such as mechanical impingement syndrome or rotator cuff injury [5,6], as well as excessive use of other upper extremity muscles, such as the wrists. The continued use of strong force to maneuver the wheelchair, even with decreased mobility in the elbow and wrist due to fatigue following a shoulder injury, has a detrimental effect on wrist muscle function, leading to wrist pain and potentially causing carpal tunnel syndrome [7].
Therefore, for patients with SCI to use manual wheelchairs requiring upper body strength effectively, they must be free of musculoskeletal disorders or pain in the upper body. Moreover, pain prevention and alleviation are crucial, as prolonged use of upper body strength, function, and endurance for mobility increases the risk of pain [8]. Various exercise interventions have been developed and studied for their efficacy in improving upper-body muscle strength and pain relief in patients with SCI. Resistance training, as highlighted in a prior study [9], improves skeletal muscle strength and overall physical function for individuals seeking enhanced physical capabilities and has been consistently chosen as the intervention method in numerous studies focusing on patients with pain and SCI. A statistical analysis of muscle strength changes following an eight-week intervention via resistance and stabilization exercises in male patients with chronic neck pain revealed significant improvements in maximum muscle strength and increased maximum extension strength at varying cervical flexion angles, as well as significant neck pain relief in the resistance exercise group [10]. According to Kim and Song [11], resistance exercises using elastic bands in patients with SCI significantly improved isokinetic muscle strength during right internal and external rotation of the shoulder joint and right extension of the elbow joint, compared with the control group. Hicks et al. [12] also reported that patients with SCI attained improved muscle strength and reduced depression, stress, and pain by regularly engaging in physical activities.
Conversely, studies have also shown that using manual wheelchairs improved the physical fitness of patients with SCI [13] and that patients with SCI using wheelchairs had stronger shoulder function than patients with SCI with incomplete ambulation [14]. Furthermore, a study analyzing the correlations between physical activity levels and physical fitness parameters among patients with SCI [15] revealed almost no correlation between physical activity levels, types of activity, and upper limb muscle strength, indicating a low association level. These inconsistencies in study findings across study populations and conditions necessitate a systematic review of previous studies to clarify the correlations among (1) exercise interventions, (2) improvement of muscle strength, and (3) pain relief.
This study aimed to conduct a systematic review of studies conducted in Korea and abroad that have used changes in pain after exercise intervention in patients with SCI as the dependent variable and to investigate whether exercise interventions effectively alleviate upper body pain in patients with SCI. Based on the findings, we hypothesized that recommendations can be made for future studies and implications for alleviating upper body pain in patients with SCI.
2. Materials and Methods
2.1. Study Planning
Our systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A statement was prepared in accordance with the PRISMA 2020 guidelines to ensure comprehensive reporting. The study procedure was as follows: (1) study planning, (2) literature search, (3) literature selection and categorization, (4) data analysis and results, and (5) discussion and conclusion. We employed the PICOS framework during the study planning phase to delineate the study objectives (Table 1). Specifically, P (Participants) comprised individuals with SCI experiencing upper body pain. I (Intervention) involved exercise, with C (Comparison) representing the control group in randomized controlled trials. O (Outcome) focused on changes in pain, and S (Study Design) indicated experimental studies. Notably, for P (Participants), individuals with lower back pain were intentionally excluded from the study. Using this PICOS strategy, we aimed to investigate improving musculoskeletal pain—the most common cause of upper body pain—through exercise, focusing on the cervical and lumbar regions [16].

Table 1.
Intervention protocol.
2.2. Literature Search
A literature search was conducted in DBpia for Korean articles and EMBASE, PubMed, and Science Direct for studies published abroad to identify academic articles (excluding degree dissertations). The search keywords were a combination of “spinal cord injury (SCI)”, “pain”, “exercise”, “disability”, “paraplegia”, and “tetraplegia”. In the Science Direct database, the search was conducted using the Advanced Search feature, including all keywords under “Find articles with these terms” and combining keywords in “Title, abstract or author-specified keywords”.
The search was conducted from 18–21 September 2023. There were no restrictions on the publication year for Korean and non-Korean literature, but the language for non-Korean articles was limited to English. Out of 191 articles found, 54 were Korean, and 137 were non-Korean. Additionally, five studies in the journal “Spinal Cord,” [17] published by the International Spinal Cord Society, were included as “Additional records identified through other sources” in the non-Korean literature search. The literature search was carried out independently by one researcher and then reviewed by a second researcher.
2.3. Literature Selection and Categorization
The selection and classification of literature were conducted according to the PRISMA 2020 flow diagram for new systematic reviews, which included searches of databases and registers only (Figure 1 and Table 2). In the identification step, 52 duplicate search results were excluded, and 139 studies remained. In the screening step, the titles and abstracts of the studies were reviewed to determine eligibility per the PICOS, and the full texts of the studies deemed eligible were reviewed. The exclusion criteria in the second screening step were as follows: (1) literature reviews and meta-analysis studies, (2) animal studies, (3) studies with full text unavailable, (4) non-experimental studies, (5) inappropriate or unclear pain criteria for participants, (6) interventions not involving exercise, and (7) no or unverifiable outcomes. No automation tools were used in the selection process. The classification was carried out independently by one researcher and then comprehensively reviewed by a second researcher for appropriateness and completeness. Through this process, 13 studies were selected, including 1 Korean and 12 non-Korean articles.
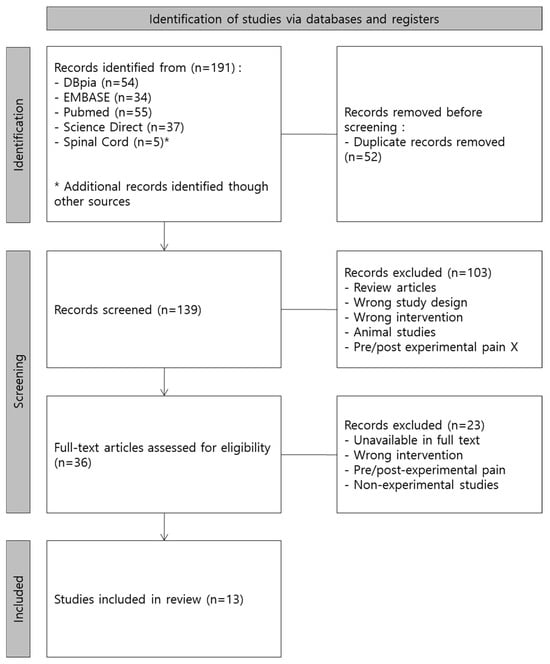
Figure 1.
PRISMA 2020 flow diagram for new systematic reviews, which included searches of databases and registers only.

Table 2.
Effectiveness of exercise programs for alleviation of upper body pain in patients with SCI.
2.4. Data Extraction
The full texts of the 13 selected studies were reviewed, and data were extracted per the PICOS strategy. The extracted data were organized according to first author (year), study design, study population, number of participants (N), intervention details, duration of intervention, assessment items and instruments, and outcomes. In evaluating the pain characteristics within the study populations, a thorough examination was conducted to ascertain whether the criteria included or excluded items specifically related to upper body pain. In cases where this information was absent or unclear, a meticulous review was undertaken to identify whether the study provided data on pain measured before the intervention. This analysis encompassed both the “study parameters (instrument)” and “results” sections. Two studies reported self-reported pain for only a subset of the participants.
In our systematic review, we extracted data using a standardized approach, focusing on the key aspects defined by the PICOS framework. Each selected study was analyzed for its methodological details, including study design, participant demographics, interventions, outcomes, and, crucially, the instruments used for measuring outcomes. Below, we summarize the commonly used research instruments in the included studies, emphasizing their purpose and significance in the context of spinal cord injury and pain assessment.
- -
- Wheelchair User Shoulder Pain Index (WUSPI): Used in seven studies, the WUSPI is a self-reported measure designed to assess shoulder pain severity and its impact on the daily activities of wheelchair users. This tool includes questions on pain intensity during various movements and is highly relevant for tracking the pain dynamics in individuals with SCI.
- -
- Performance-corrected WUSPI (PC-WUSPI): A variation of the original WUSPI, the PC-WUSPI adjusts for participants’ performance capability, providing a more tailored assessment of pain related to shoulder use. Four studies utilized it.
- -
- 36-Item Short Form Survey (SF-36): This broad health survey was used in three studies to measure aspects of quality of life related to physical and mental health. In the context of SCI, the SF-36 helps delineate how pain affects general well-being.
- -
- Visual Analog Scale (VAS): Used alongside WUSPI in two studies, the VAS is a straightforward measure in which participants rate their pain intensity on a scale, typically from ‘no pain’ to ‘worst imaginable pain.’ It is a widely accepted instrument for its simplicity and effectiveness in pain assessment.
3. Results
Our systematic review analyzed 13 articles that collectively studied a diverse population of spinal cord injury (SCI) patients. The most common type of study design among the included studies was a randomized controlled trial (six studies, 46%), followed by pre–post comparative experiments (five studies, 38%), a follow-up study for a randomized controlled trial [12] (one study, 8%), and a time-series design (one study, 8%).
The duration of SCI, spinal cord lesion site, complete/incomplete injury, and American Spinal Injury Association Impairment Scale grades varied depending on the inclusion criteria. Six studies (46%) had upper body pain-related criteria in the inclusion criteria, and two of these studies selected participants who had positive results on the functional shoulder impingement syndrome test. Functional shoulder impingement syndrome is one of the most common shoulder disorders among patients with SCI who use a wheelchair. It appears to have been employed as an inclusion criterion due to the persistent strain on the shoulder joint, leading to overuse of surrounding muscles and consequent muscle fatigue. This chronic strain exacerbates the condition, culminating in the development of shoulder impingement syndrome [29]. The pain-related criteria in the included studies were as follows:
- Positive results on shoulder impingement tests such as Neer’s impingement test, Hawkins–Kennedy test, and empty can test;
- Impact on one or more functional tasks due to unilateral or bilateral shoulder pain;
- Moderate shoulder or upper limb pain for a specified period.
The point of pain common in all three criteria was the “shoulder”; this may be attributed to the previous findings that more than half of the patients with SCI suffer from shoulder pain [2,4,30]. The type of pain was generally described as “shoulder pain”, and one study distinguished between neuropathic pain and nociceptive pain.
The duration of intervention ranged from 3 weeks to 9 months, and many studies generally used a relatively long-term intervention, with nine studies (69%) using an intervention lasting 10 weeks or longer. The most common intervention frequency was three times weekly (nine studies, 69%). The contents of the intervention were classified as follows: (1) ergometer, (2) strengthening exercise (bodyweight exercises, resistance exercises), and (3) hybrid exercise (upper limb + lower limb, ergometer + resistance training). Tools used during the experiments were an ergometer (six studies), Theraband (four studies), and hand weights (two studies). Hand weights were used in the same experiments as Theraband. One study used a treadmill, functional electrical stimulation leg cycle, and bodyweight exercise. In studies that did not directly mention the tool used, resistance training was used as the intervention; therefore, the tools used can be inferred based on the exercise motions. Eight studies used muscle training as the intervention, and six specified the exact targeted areas for exercise or motions. Table 3 shows the studies’ targeted areas and motions.

Table 3.
Targeted areas of exercise and motions.
Changes in pain were measured using the Wheelchair User Shoulder Pain Index (WUSPI) (seven studies), performance corrected-WUSPI (four studies), and 36-item short form survey (three studies), and a visual analog scale was used along with WUSPI in two studies [31,32]. The most frequently used parameter, along with pain, was quality of life (Health-Related Quality of Life). Eight types of instruments were used in eight studies, which was justifiable considering that findings suggested a negative correlation of WUSPI with physical and psychological health and overall quality of life and satisfaction, and viewed pain as a factor adversely affecting the quality of life in patients with SCI [33]. Other study parameters included physical markers during exercise (e.g., heart rate, peak oxygen uptake, %peak watts), muscle activity, strength, muscle endurance, upper extremity functionality, fatigue, self-efficacy, physical activity, level of participation, stress, depressive mood, pain interference, and body composition.
4. Discussion
This systematic review aimed to assess the effectiveness of exercise interventions in alleviating upper body pain among spinal cord injury (SCI) patients. The results from the review of 13 articles involving a diverse population of SCI patients provide substantial evidence supporting the efficacy of these interventions. Specifically, the studies demonstrated that moderate to high-intensity resistance exercises are particularly beneficial in reducing pain levels in the upper body, which includes critical areas such as the shoulders and upper limbs. The findings highlight the potential for structured exercise programs to be incorporated as a key component of pain management strategies for SCI patients. These interventions not only assist in pain reduction but also contribute to improving overall physical function and quality of life. The beneficial effects of exercise underscore its importance as a non-pharmacological treatment option that can be tailored to individual patient needs based on the severity and type of injury. The results of our systematic review following a certain set of criteria and processes show that exercise interventions effectively reduced pain in patients with SCI with upper body pain, and exercise was identified as essential for patients with SCI and shoulder pain. Most studies included strength training, supporting the effectiveness of incorporating it into exercise programs for patients with SCI, irrespective of injury location or severity. Moderate to high-intensity resistance exercises targeting specific muscle groups enhance muscle strength [34,35]. In some studies that followed pain in patients post-intervention, either no immediate or follow-up changes in pain or an increase in pain was observed during the follow-up period, and this appears to be associated with a decline in exercise participation after the intervention period [36], highlighting the importance of strategies to motivate continual exercise participation and habit formation.
Changes in pain were adopted and measured as secondary outcomes in most studies due to the subjective nature of pain, which presents challenges in quantitatively and objectively measuring it in experimental settings. Hence, researchers presumably aimed to demonstrate the relationship and validity by measuring and analyzing pain alongside outcomes that provide numerical values, such as muscle strength or activity. Most instruments used for pain assessment are self-reported scales, and assessment generally relies on the statements of study participants. Consequently, using pain as a primary outcome might lead to concerns about the accuracy and reliability of the results. Therefore, there is a need for the development of validated pain instruments that can measure changes in pain as a primary outcome, and experimental studies using pain as the primary outcome should be conducted to prevent and alleviate pain in patients with SCI.
Thus, we sought to examine musculoskeletal pain in the upper body in patients with SCI by analyzing existing studies. However, neuropathic pain and other pain types were included in our analysis due to the difficulty of determining whether shoulder pain in patients with SCI is musculoskeletal pain [16] and the abundance of studies that do not specify the type of pain. Musculoskeletal pain is the most common cause of joint pain, and the cause of chronic pain must be identified to provide appropriate treatment [37]. Thus, we recommend that future studies use the Leeds Assessment of Neuropathic Symptoms and Signs to enhance the reliability of experimental studies. The Leeds Assessment of Neuropathic Symptoms and Signs allows the researcher to distinguish between neuropathic pain and nociceptive pain [38], and it can be used to assess whether shoulder pain in patients with SCI is neuropathic pain or nociceptive musculoskeletal pain [39]. Using this instrument to accurately distinguish the cause of shoulder and upper body pain when enrolling study participants would enable researchers to produce more accurate results regarding the cause of pain.
Furthermore, while we limited the point of pain to the upper body, the site of pain was limited to the shoulder due to the participant inclusion criteria that reflected that shoulder pain is the most common pain experienced by patients with SCI [1,4]. The shoulder muscles were also the primary targets for muscle-strengthening exercises. However, given that upper body pain experienced by patients with SCI may occur in various places, including the shoulders, wrist, hands, and elbows, and injury in one area influences other areas [7], increasing overall upper body strength and preventing pain is essential. Future experimental studies should be conducted to evaluate and strengthen the muscles of the entire upper body, including the back, abdomen, and chest, of patients with SCI, and appropriate exercise interventions should be applied. Nevertheless, the increased load due to propelling wheelchairs in environments with high speeds and steep inclines leads to an increase in the range of motion and muscle activity of the trunk flexion and extension rather than the range of motion of the upper limb joints, and core muscles need to be mobilized to prevent injury [7,31,40], which is consistent with previous findings that emphasize the need to strengthen the abdominal muscles and spinal extensors for this purpose [41].
The WUSPI designed by Lee et al. [42] is used to assess shoulder pain in wheelchair users and was the most frequently used instrument in the included studies. Curtis et al. [43] adapted the WUSPI into Korean, using terminology that reflects Korea’s cultural characteristics while maintaining the original’s integrity, and validated the instrument for measuring shoulder pain in wheelchair users in Korea. Both the original WUSPI and the Korean version consist of 15 items, categorized into mobility-related items such as “moving from bed to wheelchair” and “pushing a wheelchair for more than 10 min” and daily activity-related items such as “putting on pants” and “washing the back”. According to Park and Cho [44], 570,462 people with physical disabilities, including those with SCI, are economically active (48.0%), with an employment rate of 46.2%. Despite the active participation of almost half of these individuals in social and economic activities, the WUSPI only contains one item for this: “activities at work/school”; this indicates a gap in identifying and measuring the pain wheelchair users might experience in social and economic contexts. Furthermore, living standards have changed significantly since the time of development of the WUSPI, as the penetration rate of cellphones/smartphones among people with physical disabilities has reached 95.2% [45], calling for new items that reflect such shifts. Therefore, new items should be developed, or existing items should be modified in this context.
According to Lee and Shin [14], patients with SCI who use a wheelchair have significantly stronger shoulder muscles, especially shoulder external rotation, and right internal and external rotation, compared to those capable of incomplete ambulation. These results are inconsistent with previous findings that the use of a wheelchair induces continuous stress on the shoulder and relevant disorders and adversely affects the surrounding muscles. The reason was attributed to the fact that the study population consisted of patients with SCI without shoulder injury or pain. That is, the use of a wheelchair by users without a history of shoulder injury seems to have had positive effects on shoulder rotation and strength. Conversely, inappropriate use of manual wheelchairs may induce pain, and it is important to choose a manual wheelchair suitable for the user’s body shape and conditions.
A user survey was conducted on the perceived need and satisfaction with manual wheelchairs among three patients with varying degrees of SCI who are representative of the SCI population [43]. In addition, a study in Korea proposed that the standard wheelchair design is ergonomically appropriate for the body figures of Koreans by measuring the specifications of wheelchairs marketed in Korea and comparing them with anthropometric measurements [44]. However, these were standard specifications obtained from patients with temporary disabilities and may be inappropriate for patients with SCI who must use wheelchairs for prolonged periods and durations. Lee and Yoo [45] recommend the use of lightweight, ergonomically suitable manual wheelchairs to prevent injuries and disorders in individuals with SCI who are at risk of shoulder pain, as well as power assist devices designed to avoid deformities in the upper limbs and enhance mobility. Therefore, it is essential to develop guidelines that enable individuals with SCI to self-assess their physical condition, presence and degree of shoulder pain, and muscle strength. Additionally, it is essential to establish an environment where they can choose manual wheelchairs with ergonomic structures and specifications suited to their assessment results. In particular, there is a call for developing new manual wheelchairs equipped with features that can prevent and alleviate shoulder pain. Such advancements in assistive technology are crucial for improving the quality of life for SCI patients, emphasizing the practical implications of our findings.
While the study is significant for examining correlations among exercise interventions, muscle strength improvements, and pain relief, it is important to acknowledge that researchers’ subjective biases in the selection and extraction of study data could not be completely eliminated. This acknowledgment underscores the need for cautious interpretation of the results.
5. Conclusions
Our study underscores the significant impact of exercise interventions in alleviating upper body and shoulder pain among spinal cord injury (SCI) patients. Exercise interventions, particularly moderate- to high-intensity resistance exercises, play a crucial role in managing pain for individuals with spinal cord injuries. However, the sustained effectiveness of these interventions is often compromised by a decline in exercise adherence after the conclusion of structured programs. This underscores the necessity of developing innovative strategies that maintain exercise engagement and promote the formation of long-term habits for ongoing pain management.
The inherent challenges in pain measurement, owing to its subjective nature, call for the development of validated instruments capable of quantitatively assessing pain as a primary outcome. This advancement is crucial for refining research focused on the effective prevention and management of pain in SCI populations. Moreover, our findings reveal the necessity of distinguishing between neuropathic and nociceptive musculoskeletal pain to tailor treatment approaches more precisely.
Given the prevalence of shoulder pain in SCI patients, it is essential to adopt a comprehensive approach that considers the entire upper body. Such an approach could potentially offer more holistic pain management solutions, addressing the multifaceted nature of musculoskeletal pain. However, while the review underscores the importance of ergonomic considerations in manual wheelchair design, improving these designs, although beneficial, was not a primary focus of this review. Thus, the suggestion of enhancing wheelchair ergonomics, while valid, does not stem directly from the findings of this review but rather is a recognized need in the field.
Furthermore, the review highlights certain limitations in current pain assessment tools used in SCI research. Addressing these limitations could contribute to better clinical practices and research outcomes. However, it is important to clarify that enhancing these tools alone is unlikely to directly improve the overall quality of life for SCI individuals, as suggested earlier. Such improvements must be part of broader, multi-faceted interventions that include but are not limited to better pain management strategies.
Lastly, the review did not conclusively differentiate between neuropathic and nociceptive musculoskeletal pain, although it does suggest that understanding these differences could be crucial for tailoring pain management strategies. It is crucial to reiterate that the primary conclusion of this review focuses on the effectiveness of exercise interventions in managing pain, rather than on the distinctions between types of pain.
Author Contributions
Conceptualization, J.P., J.K., S.-D.E. and D.K.; methodology, J.P. and J.K.; formal analysis, J.P. and J.K.; investigation, J.P. and J.K.; resources, J.P., J.K. and D.K.; data curation, J.P. and J.K.; writing—original draft preparation, J.P. and J.K.; writing—review and editing, J.P. and D.K.; visualization, J.P. and J.K.; project administration, J.P., S.-D.E. and D.K.; funding acquisition, S.-D.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Korea National Rehabilitation Research Institute (Seoul, Republic of Korea), grant number 23-E-02.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author (D.K.) upon reasonable request.
Acknowledgments
We express our gratitude to the research teams involved in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Sie, I.H.; Waters, R.L.; Adkins, R.H.; Gellman, H. Upper extremity pain in the post rehabilitation spinal cord injured patient. Arch. Phys. Med. Rehabil. 1992, 73, 44–48. [Google Scholar] [PubMed]
- Finley, M.A.; Rasch, E.K.; Keyser, R.E.; Rodgers, M.M. The biomechanics of wheelchair propulsion in individuals with and without upper-limb impairment. J. Rehabil. Res. Dev. 2004, 41, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Cratsenberg, K.A.; Deitrick, C.E.; Harrington, T.K.; Kopecky, N.R.; Matthews, B.D.; Ott, L.M.; Coeytaux, R.R. Effectiveness of exercise programs for management of shoulder pain in manual wheelchair users with spinal cord injury. J. Neurol. Phys. Ther. 2015, 39, 197–203. [Google Scholar] [CrossRef]
- Dalyan, M.; Cardenas, D.D.; Gerard, B. Upper extremity pain after spinal cord injury. Spinal Cord 1999, 37, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Pentland, W.E.; Twomey, L.T. Upper limb function in persons with long term paraplegia and implications for independence: Part I. Spinal Cord 1994, 32, 211–218. [Google Scholar] [CrossRef]
- Van Drongelen, S.; van der Woude, L.H.; Janssen, T.W.; Angenot, E.L.; Chadwick, E.K.; Veeger, D.H. Mechanical load on the upper extremity during wheelchair activities. Arch. Phys. Med. Rehabil. 2005, 86, 1214–1220. [Google Scholar] [CrossRef] [PubMed]
- Boninger, M.L.; Impink, B.G.; Cooper, R.A.; Koontz, A.M. Relation between median and ulnar nerve function and wrist kinematics during wheelchair propulsion. Arch. Phys. Med. Rehabil. 2004, 85, 1141–1145. [Google Scholar] [CrossRef]
- Lee, B.S. Wheelchair Perfectly Suited to Me: Wheelchair User Manual; Ministry of Health and Welfare National Rehabilitation Center: Seoul, Republic of Korea, 2018. [Google Scholar]
- Evans, W.J. Exercise training guidelines for the elderly. Med. Sci. Sports Exerc. 1999, 31, 12–17. [Google Scholar] [CrossRef]
- Lee, K.; Han, G. The effects of cervical resistance exercise and stabilization exercise on cervical extension strength and VAS in male patients with chronic neck pain. Korean J. Sports Sci. 2020, 29, 1325–1334. [Google Scholar] [CrossRef]
- Kim, K.G.; Song, N.H. Effect of elastic band exercise on the isokinetic muscular strength of spinal cord injury patients’ upper limbs. J. Wellness 2013, 8, 191–202. [Google Scholar]
- Hicks, A.L.; Martin, K.A.; Ditor, D.S.; Latimer, A.E.; Craven, C.; Bugaresti, J.; McCartney, N. Long-term exercise training in persons with spinal cord injury: Effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003, 41, 34–43. [Google Scholar] [CrossRef]
- McCormick, Z.L.; Lynch, M.; Liem, B.; Jacobs, G.; Hwang, P.; Hornby, T.G.; Rydberg, L.; Roth, E. Feasibility for developing cardiovascular exercise recommendations for persons with motor-complete paraplegia based on manual wheelchair propulsion; a protocol and preliminary data. J. Spinal Cord Med. 2016, 39, 45–49. [Google Scholar] [CrossRef]
- Lee, G.H.; Shin, Y.A. The influence of wheelchair use of individuals with spinal cord injury on upper extremity muscular function and cross-sectional area. Korean J. Sports Med. 2018, 36, 24–33. [Google Scholar] [CrossRef]
- Janssen, T.W.J.; Dallmeijer, A.J.; Veeger, D.J.; van der Woude, L.H. Normative values and determinants of physical capacity in individuals with spinal cord injury. J. Rehabil. Res. Dev. 2002, 39, 29–39. [Google Scholar]
- Putzke, J.D.; Richards, S.J.; Hicken, B.L.; DeVivo, M.J. Interference due to pain following spinal cord injury: Important predictors and impact on quality of life. Pain 2002, 100, 231–242. [Google Scholar] [CrossRef]
- Requejo, P.S.; Mulroy, S.J.; Haubert, L.L.; Newsam, C.J.; Gronley, J.K.; Perry, J. Evidence-based strategies to preserve shoulder function in manual wheelchair users with spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2008, 13, 86–119. [Google Scholar] [CrossRef]
- Kim, S.C.; Lee, Y.M.; Shin, K.H. The Effects of Trapezius and Serratus Anterior Strengthening Exercise on Pain and Muscle Activation in Spinal Cord Injury Patients with Functional Shoulder Impingement Syndrome. PNF Mov. 2018, 16, 33–42. [Google Scholar]
- Nightingale, T.E.; Rouse, P.C.; Walhin, J.P.; Thompson, D.; Bilzon, J.L. Home-based exercise enhances health-related quality of life in persons with spinal cord injury: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2018, 99, 1998–2006. [Google Scholar] [CrossRef] [PubMed]
- Gee, C.M.; Sinden, A.R.; Krassioukov, A.V.; Martin Ginis, K.A. The effects of active upper-limb versus passive lower-limb exercise on quality of life among individuals with motor-complete spinal cord injury. Spinal Cord. 2022, 60, 805–811. [Google Scholar] [CrossRef]
- Van Straaten, M.G.; Cloud, B.A.; Morrow, M.M.; Ludewig, P.M.; Zhao, K.D. Effectiveness of home exercise on pain, function, and strength of manual wheelchair users with spinal cord injury: A high-dose shoulder program with telerehabilitation. Arch. Phys. Med. Rehabil. 2014, 95, 1810–1817. [Google Scholar] [CrossRef]
- Mulroy, S.J.; Thompson, L.; Kemp, B.; Hatchett, P.P.; Newsam, C.J.; Lupold, D.G.; Haubert, L.L.; Eberly, V.; Ge, T.-T.; Azen, S.P.; et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury: A randomized controlled trial. Phys. Ther. 2011, 91, 305–324. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, M.; Jensen, K.; Juul-Kristensen, B. Hybrid high-intensity interval training using functional electrical stimulation leg cycling and arm ski ergometer for people with spinal cord injuries: A feasibility study. Pilot Feasibility Stud. 2022, 8, 43. [Google Scholar] [CrossRef] [PubMed]
- Ditor, D.S.; Latimer, A.E.; Ginis, K.A.M.; Arbour, K.P.; McCartney, N.; Hicks, A.L. Maintenance of exercise participation in individuals with spinal cord injury: Effects on quality of life, stress and pain. Spinal Cord 2003, 41, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Cardenas, D.D.; Felix, E.R.; Cowan, R.; Orell, M.F.; Irwin, R. Effects of home exercises on shoulder pain and pathology in chronic spinal cord injury: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2020, 99, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Nash, M.S.; van de Ven, I.; van Elk, N.; Johnson, B.M. Effects of circuit resistance training on fitness attributes and upper-extremity pain in middle-aged men with paraplegia. Arch. Phys. Med. Rehabil. 2007, 88, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Norrbrink, C.; Lindberg, T.; Wahman, K.; Bjerkefors, A. Effects of an exercise programme on musculoskeletal and neuropathic pain after spinal cord injury—Results from a seated double-poling ergometer study. Spinal Cord. 2012, 50, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Serra-Añó, P.; Pellicer-Chenoll, M.; García-Massó, X.; Morales, J.; Giner-Pascual, M.; González, L.M. Effects of resistance training on strength, pain and shoulder functionality in paraplegics. Spinal Cord. 2012, 50, 827–831. [Google Scholar] [CrossRef] [PubMed]
- Ballinger, D.A.; Rintala, D.H.; Hart, K.A. The relation of shoulder pain and range-of-motion problems to functional limitations, disability, and perceived health of men with spinal cord injury: A multifaceted longitudinal study. Arch. Phys. Med. Rehabil. 2000, 81, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.B.; Higgins, L.D.; Katz, J.N.; Garshick, E. Association of shoulder pain with the use of mobility devices in persons with chronic spinal cord injury. PM&R 2010, 2, 896–900. [Google Scholar] [CrossRef]
- Jacobs, P.L.; Nash, M.S. Exercise recommendations for individuals with spinal cord injury. Sports Med. 2004, 34, 727–751. [Google Scholar] [CrossRef]
- Lee, J.K.; Kang, M.Y.; Jeon, E.M. The effect of shoulder pain on the quality of life of manual wheelchair users with spinal cord injuries. Ther. Sci. Rehabil. 2023, 12, 33–44. [Google Scholar]
- Lee, S.; Choi, S.; Kim, Y.S.; Lee, S.M.; Jang, Y.S.; Jin, J.Y. A systematic review: Rehabilitative exercise programs for improving daily functions of individuals with a spinal cord injury. Korean J. Meas. Eval. Phys. Educ. Sports Sci. 2022, 24, 33–52. [Google Scholar]
- Martin Ginis, K.A.; van der Scheer, J.W.; Latimer-Cheung, A.E.; Barrow, A.; Bourne, C.; Carruthers, P.; Bernardi, M.; Ditor, D.S.; Gaudet, S.; de Groot, S.; et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: An update and a new guideline. Spinal Cord 2018, 56, 308–321. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.K. Evaluation and management of chronic pain. Korean J. Family Med. 2003, 24, 103–111. [Google Scholar]
- Bennett, M.I.; Smith, B.H.; Torrance, N.; Potter, J. The S-LANSS score for identifying pain of predominantly neuropathic origin: Validation for use in clinical and postal research. J. Pain 2005, 6, 149–158. [Google Scholar] [CrossRef]
- Bernard, P.L.; Codine, P.; Minier, J. Isokinetic shoulder rotator muscles in wheelchair athletes. Spinal Cord 2004, 42, 222–229. [Google Scholar] [CrossRef]
- Petrofsky, J.S.; Johnson, E.G.; Hanson, A.; Cuneo, M.; Dial, R.; Somers, R.; De La Torre, G.; Martinez, A.; McKenzie, M.; Forrester, B. Abdominal and lower back training for people with disabilities using a 6-second abs machine: Effect on core muscle stability. J. Appl. Res. Clin. Exp. Ther. 2005, 5, 345. [Google Scholar]
- Lee, K.; Hong, S.M.; Shin, Y.A. Physical fitness and exercise strategy according to general characteristics of spinal cord injured person. Exerc. Sci. 2019, 28, 110–121. [Google Scholar] [CrossRef]
- Curtis, K.A.; Roach, K.E.; Applegate, E.B.; Amar, T.; Benbow, C.S.; Genecco, T.D.; Gualano, J. Development of the wheelchair user’s shoulder pain index (WUSPI). Spinal Cord 1995, 33, 290–293. [Google Scholar] [CrossRef]
- Park, J.Y.; Cho, S.H. The reliability and validity of Korean version of the wheelchair user’s shoulder pain index in wheelchair users. J. Korean Soc. Phys. Med. 2013, 8, 573–582. [Google Scholar] [CrossRef]
- Korea Employment Agency for Persons with Disabilities. Survey of Economic Activities among Persons with Disabilities. 2022. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=383&tblId=DT_38304_2013_N004&conn_path=I2 (accessed on 10 May 2024).
- Ministry of Health and Welfare. National Survey on Persons with Disabilities: Rate of ICT Device Usage. 2020. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_11732S0115&conn_path=I2 (accessed on 11 November 2022).
- Kim, J.H.; Kwon, O.S.; Chung, D.H. A case study on user research for manual wheelchair use of people with spinal cord injuries. J. Korean Des. Cult. Soc. 2018, 24, 181–192. [Google Scholar] [CrossRef]
- Lee, S.-D.; Yoo, B.C. Ergonomic design of standard wheelchair for Korean adults. J. Korean Soc. Saf. 1993, 8, 94–98. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).