Abstract
Background/Aims: Myosteatosis implies impaired muscle quality. The aim of the study was to investigate the association of myosteatosis with other muscle abnormalities and its role in the prognosis of liver cirrhosis (LC). Method: Skeletal muscle index (SMI) and myosteatosis were measured by computed tomography. Myosteatosis was defined as muscle radiodensity and evaluated according to dry body mass index (BMI). Median values and interquartile range were used for continuous and count (percentage) for categorical variables. Results: A total of 197 consecutive patients were included (age 61 (IQR 52–68); 67% male; MELD score 11 (interquartile range 7.5–16)). Myosteatosis was identified in 73.6% and sarcopenia in 44.6% of patients. Myosteatosis was positively associated with age (p = 0.024) and Child–Pugh (p = 0.017) and inversely associated with SMI (p = 0.026). Patients with myosteatosis exhibited lower 360-day survival (log-rank p = 0.001) compared to those without it. MELD (p < 0.001) and myosteatosis (p = 0.048) emerged as negative prognostic factors of survival in multivariate model. Individuals combining low muscle strength and impaired muscle quality and quantity displayed more advanced LC, impaired muscle performance, lower BMI (p < 0.001 each) and a three times higher mortality rate compared to those with low muscle quality alone. Conclusions: The presence of myosteatosis was associated with advanced age, low skeletal mass and more severe LC. Myosteatosis was associated with poor prognosis and may represent a prodromal phase of muscle degeneration before the development of sarcopenia.
1. Introduction
Myosteatosis is defined as increased fat infiltration or accumulation in skeletal muscle and implies compromised muscle quality. There are three potential phenotypes of adipose tissue distribution [1] in the muscles, i.e., inter-musculary, intra-musculary, and intra-myocellulary lipids. Myosteatosis is now considered a distinct entity from sarcopenia, but sarcopenia is also a component of its definition according to the updated European Working Group on Sarcopenia in Older People (EWGSOP-2) criteria [2]. Myosteatosis is associated with aging and mobility–disability consequences such as hip fractures, hospitalization, mortality and surgery in older adults [3,4]. It is also associated with high mortality rates in different clinical settings including critically ill patients with cancer, kidney or cardiovascular diseases [5,6,7,8]. In the cases of liver cirrhosis, myosteatosis is associated with minimal and overt hepatic encephalopathy and risk of falls [9,10,11] and has been incorporated into MELD as MELD–Sarco–Myo–HE score [12]. Moreover, myosteatosis has been implicated in the pre- and post-liver transplantation outcome [13,14,15]. Myosteatosis may be considered as a precursor of sarcopenia in the elderly [1] but its temporal correlation with muscle loss during the course of liver cirrhosis has not been documented.
Assessment of the cross-sectional surface area of axial and appendicular skeletal muscles by computed tomography (CT) at the level of the third lumbar vertebra (L3) is considered one of the most sensitive, widely used noninvasive approaches to evaluate muscle quantity and quality [16]. The evaluation of radiodensity in Hounsfield units (HU) is a measurement indicating the way X-rays pass through water. If density is lower than water, then there is evidence of fat. The lower the density, the higher the degree of myosteatosis. The correlation of HU evaluation with lipid content was confirmed by the direct evaluation of fat storage by muscle biopsy [17].
There is a debate in the literature whether myosteatosis is associated with severity of liver disease and whether there is an interaction between myosteatosis and low muscle mass or sarcopenia [18,19].
The aim of the present study was to investigate the interplay between muscle quality and quantity and the association of myosteatosis with the severity of liver cirrhosis, other muscle abnormalities such as low muscle mass and performance, and body adipose tissue composition. The role of myosteatosis in the prognosis of liver disease was also examined.
2. Materials and Methods
2.1. Study Population
This prospective study was conducted in a single tertiary center from May 2018 to December 2021. Patients with liver cirrhosis from the outpatient clinic and the wards of the Hippokration Hospital were included. The hospitalized patients were enrolled just before hospital discharge while they were in a stable condition without acute clinical events. Patients with alcoholic cirrhosis were included provided they had stopped consuming alcohol for at least one month before enrollment. The diagnosis of cirrhosis was based on liver histology and/or a combination of imaging, endoscopic and clinical findings. Cirrhosis was considered as decompensated in patients with history of ascites, variceal bleeding, hepatic encephalopathy and jaundice of non-obstructive cause (bilirubin >3 mg/dL for non-cholestatic and >10 mg/dL for cholestatic causes of cirrhosis). Patients with hepatocellular carcinoma or other extrahepatic malignancies, liver transplantation, immunosuppressive therapy other than corticosteroids human immunodeficiency virus infection and heart, kidney or respiratory failure were excluded from the study.
The study protocol was approved by the Hippokration Hospital ethical committee. All patients signed a written informed consent form before their inclusion in the study.
2.2. Clinical Data
Demographic and clinical data (such as age, gender, cause of liver cirrhosis) as well as laboratory parameters (including biochemical and clotting profile) were prospectively recorded. Based on these data, MELD score was calculated.
Body weight (BW) was measured using an electronic scale and standing height using a stadiometer (Seca 769 digital scale and Seca 220 stadiometer, respectively, Seca Medical Systems, Hamburg, Germany). Dry weight was calculated by subtracting 5% of the measured BW for mild ascites, 10% for moderate ascites and 15% for tense ascites, with an additional 5% subtracted if bilateral pedal edema was present, as suggested by European Association for the study of the liver [20]. Dry body mass index (BMI) (kg/m2) was also calculated.
2.3. Muscle Strength Assessment
Muscle strength for all included patients and controls was measured using a calibrated hydraulic hand dynamometer (Jamar Hydraulic Dynamometer, model 5030j1, Jamar Co., Duluth, MN, USA). Three handgrip measurements from each hand were recorded for each participant [21] and maximum measurements were used for statistical analysis.
2.4. Muscle Mass Quantity and Quality Assessment
CT was performed within 7 days after enrollment. Muscle mass assessment was performed by measuring the muscle mass area at the level of L3, using appropriate software (SliceOmatic V4.3 software, Tomovision, Montreal, QC, Canada) as described by Georgiou A et al. [22]. Skeletal muscle was quantified using −29 to +150 Hounsfield Units (HU) range. The area was then adjusted to height in order to calculate skeletal mass index (SMI) (cm)2/height2 (in m2). Furthermore, an analysis of muscular, visceral and subcutaneous adipose tissue was also performed. Myosteatosis was defined as muscle radiodensity at L3 < 41 HU for patients with dry BMI < 24.9 kg/m2 and <33 HU for those with ≥25 kg/m2 [9,18]. The same software was utilized to calculate visceral adipose tissue index (VATI, cm2/m2) and subcutaneous adipose tissue index (SATI, cm2/m2).
2.5. Physical Performance Assessment
The short physical performance battery test (SPPB) was used to assess muscle performance. It includes the time the volunteer needs to perform five sits on a chair without using their hands, balance in three consecutive standing positions, and gait speed. Test scores range from 0 to 12 and SPPB score of ≤ 8 indicates decreased performance [23].
2.6. Sarcopenia Diagnosis
According to the updated EWGSOP-2 criteria [2], sarcopenia is diagnosed when low muscle strength and decreased muscle mass and/or quality (myosteatosis) are present. In the current study, low SMI cut-off values (<50 cm2/m2 for men and <39 cm2/m2 for women) set by Carey et al. [24] were used to identify patients with decreased muscle mass based on CT. If the patient had low muscle strength accompanied by decreased muscle mass and/or myosteatosis, they were classified as sarcopenic.
2.7. Follow-Up
The patients were prospectively followed-up during hospitalization and, if discharged, at the outpatient clinic, from electronic medical records and by telephone at 12 months.
2.8. Statistical Analysis
All data were analyzed using the statistical package SPSS (version 23.0; SPSS Inc., Chicago, IL, USA). Quantitative variables were expressed as median values and interquartile ranges (IQR) and categorical variables as count (percentage). Data were expressed as median and interquartile range (IQR) for continuous and count with percentage for categorical variables. Mann–Whitney U and Kruskal–Wallis tests were used for comparisons of continuous variables between groups and chi-squared test for categorical variables. A two-tailed p-value of less than 0.05 was considered statistically significant.
Factors associated with a p value of <0.05 in the univariate analysis as well as age and gender were entered in the multivariate model and non-significant factors were removed by a backward selection process.
Actuarial probabilities of death during follow-up were calculated by Kaplan–Meier method and compared between groups by log-rank test. Cox’s proportional hazards regression model was used to estimate risk factors that were associated with poor prognosis.
3. Results
A total of 197 consecutive patients (median age 61 (IQR 52–68), 67% male, MELD 11 (7.5–16), 60.9% with decompensated cirrhosis, 43.1%, 23.4% and 33.5% with alcoholic, viral and other causes of liver disease, respectively) were included in the study. Non-alcoholic steatohepatitis (NASH) or cryptogenic cirrhosis were diagnosed in 8.6% and 3% of patients, respectively. Dry BMI ≤25 kg/m2, >25 kg/m2 but ≤30 kg/m2 and >30 kg/m2 was measured in 41.1%, 39.6% and 19.3% of patients, respectively. Myosteatosis was identified in 73.6% and sarcopenia in 44.6% of the participants. Myosteatosis was present in all but three patients with sarcopenia (only three patients had low SMI and low handgrip without myosteatosis). Therefore, myosteatosis was identified in 96.5% of patients with sarcopenia.
Patients with myosteatosis vs. those without were older (p = 0.004) and had more often alcoholic etiology (p = 0.028), decompensated cirrhosis (p < 0.001), and history of hepatic encephalopathy (p = 0.013) (Table 1). Moreover, patients with myosteatosis compared to those without displayed lower dry BMI (p = 0.001), lower skeletal muscle mass (p < 0.001) and decreased muscle performance (p < 0.001). Gender, VATI and SATI did not produce different effects between the two groups (Table 1). Myosteatosis was present in 89.5% of patients with low SMI.

Table 1.
Comparison of demographics, clinical characteristics between patients with and without myosteatosis (N = 197). Median values and interquartile range are used for continuous and count (percentage) for categorical variables.
In multivariate analysis, after adjusting for age, gender, dry BMI, Child–Pugh score, SMI, handgrip and SPPB, only advanced age (p = 0.024), low SMI (p = 0.026) and advanced Child–Pugh (p = 0.017) appeared to be associated with myosteatosis (multivariate 1). If cirrhosis status (dichotomized as decompensated or non-decompensated) replaced Child–Pugh score, then low SMI (p = 0.013) and decompensated cirrhosis (p = 0.009) were associated with the presence of myosteatosis (multivariate 2). MELD score was not associated with the presence of myosteatosis in multivariate analysis (multivariate 3) (Table 2).

Table 2.
Factors associated with presence of myosteatosis in univariate and multivariate analysis (3 models) in all 197 patients.
3.1. Survival
After assessing Kaplan–Meier survival curves at 360 days, patients with myosteatosis displayed increased mortality rate compared to those without (no patient died in those without myosteatosis) (log-rank p = 0.001) (Figure 1A). Cox’s univariate analysis showed that the variables exhibiting association with mortality were age (p = 0.002), presence of myosteatosis (p = 0.008), MELD score (p < 0.001), low SMI (p < 0.001) and low SATI (p = 0.030). In multivariate analysis (after adjustment for age, gender, dry BMI, MELD, low SMI and SATI), only MELD score (HR 4.911, 95% CI 2.390–10.094, p < 0.001) and the presence of myosteatosis (HR 7.778, 95% CI 1.022–59.206, p = 0.048) emerged as independent, prognostic factors of mortality (Table 3). All deaths were due to liver-related causes.
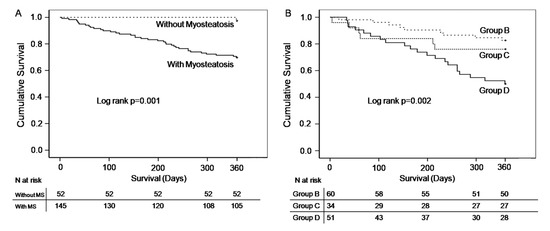
Figure 1.
Kaplan–Meier survival curves for patients with myosteatosis vs. those without (A); Kaplan–Meier survival curves for the 3 phenotypes according to the extent of muscle abnormalities (myosteatosis alone (group B); myosteatosis combined by low handgrip strength (group C *); myosteatosis combined by low handgrip strength and low skeletal mass index (group D *) (B). * Groups C and D had sarcopenia according to the updated EWGSOP-2 criteria [2].

Table 3.
Factors predicting 360-day mortality in univariate and multivariate analysis in 197 patients.
3.2. Study of Groups Composed According to the Extent of Muscle Abnormalities
Taking into consideration three parameters, i.e., presence of myosteatosis, low handgrip strength and low SMI, 194 patients were classified into four groups: neither myosteatosis nor sarcopenia in 25.3% (group A), myosteatosis alone (with normal handgrip and normal SMI) in 30.9% (group B), sarcopenia according to low handgrip strength and myosteatosis (but normal SMI) in 17.5% (group C) and sarcopenia according to low handgrip, myosteatosis and low SMI in 26.3% (group D). Only three cases exhibited low handgrip and low SMI (sarcopenia) without myosteatosis, so no group was composed from these three patients.
There was a sequential ascending order across the groups A, B, C and D in age (56 (50–63.5), 57.5 (51.2–66), 62.5 (57–69.5) and 67 (59–72.5) years, respectively; p < 0.001) and severity of LC as it was documented by the increasing rate of decompensated cirrhosis (32.7%, 58.3%, 73.5% and 80.4%, respectively; p < 0.001) and Child–Pugh (5 (5–7), 7 (5–9), 7 (6–8) and 9 (7–10), respectively; p < 0.001). Similar but not so well-arranged results were demonstrated in MELD score (Table 4). In contrast, there was a sequential descending order across the groups in muscle performance (SPPB) (p < 0.001) values. Similar but not so well-arranged results were illustrated in dry BMI, handgrip force, SATI and SMI (p < 0.001 for all the above). No difference among groups was demonstrated in gender and VATI.

Table 4.
Comparison of demographics and clinical characteristics among 4 groups according to the extent of muscle abnormalities (194 patients).
Group D had significantly more advanced liver disease (according to MELD and Child–Pugh score), lower BMI, muscle performance and SATI compared to group C. Patients in group D were older, more often of alcoholic etiology, had significantly more advanced liver disease, lower BMI, functionality and SATI compared to groups B and A. Patients in Group C had similar parameters to group B but they had lower BMI and muscle performance compared to those of group B. Patients in group C were older, had significantly more advanced liver disease lower muscle functionality and SATI compared to those of group A. Group B had significantly more advanced liver disease, lower BMI and SATI compared to those of group A (Table S1).
Considering the Kaplan–Meier curve at 360 days, in groups exhibiting myosteatosis alone (group B) or with myosteatosis plus more extended muscle abnormalities (C and D) (no patient died in group A), patients of group D had a higher mortality rate compared to those of group B (log-rank p = 0.001) but not C (log-rank p = 0.068) (log-rank p = 0.002 in overall) (Figure 1B). According to the Cox’s regression analysis, after adjustment for age and gender, patients in group C had similar risk of death to those of group B (reference group) (p = 0.530). However, mortality was three times higher in those of group D compared to those of group B (HR 3.097 (1.338–7.169), p = 0.008) (Table 5).

Table 5.
Hazard ratios for death according to extent of muscle abnormalities. Crude and adjusted values by the use of Cox’s regression analysis.
4. Discussion
The presence of myosteatosis was associated with aging, more severe liver cirrhosis and history of hepatic encephalopathy, lower skeletal muscle mass, performance and BMI in this cohort of patients with cirrhosis of various etiologies, more than half decompensated. Patients with myosteatosis displayed poor outcome even after adjusting for significant covariates. When patients with myosteatosis were divided according to the severity level of muscle aberrations, individuals combining low muscle strength, impaired quality and quantity were older and displayed more often alcoholic etiology, advanced liver disease, lower BMI, more impaired muscle quality and performance and higher mortality rate compared to those with low muscle quality alone.
Myosteatosis was detected in 74% of our patients with cirrhosis even in the absence of sarcopenia. Concomitant presence of myosteatosis occurred in 96.5% patients with sarcopenia (defined by the most recent EWGSOP-2 criteria) [2] and in 89.5% of those with low muscle mass (SMI), displaying an interconnection between impaired muscle quality and quantity. It was also illustrated that myosteatosis was associated with the presence of hepatic encephalopathy, a finding that was previously reported in the literature [9,10,11]. It was suggested that hyperammonemia resulting in skeletal muscle ammonia uptake promoted skeletal muscle mitochondrial dysfunction, decreased lipid oxidation and finally led to lipid deposition in muscles [25]. In addition, systemic inflammation and oxidative stress usually accompany liver cirrhosis and are associated with metabolic dysfunction of skeletal muscle, impaired muscle protein synthesis, turnover and function [26,27]. Most patients with liver cirrhosis live a sedentary life with restricted daily physical activity. In addition, they may experience decreased appetite due to salt restriction and alcohol consumption, early satiety due to ascites, and impaired gastric and intestinal motility [28]. Measuring dietary intake is difficult in clinical practice and accurate assessments remain unclear in patients experiencing complications of cirrhosis. All the above along with aging may result in malnutrition, increased muscle catabolism, muscle atrophy and replacement of muscle by adipose tissue.
In the present study, myosteatosis was independently associated with higher Child–Pugh score or decompensated cirrhosis status but not with MELD score. Child–Pugh score includes two clinical components, i.e., ascites and hepatic encephalopathy, which are not included in MELD score. It is therefore reasonable that patients with clinical characteristics of decompensated cirrhosis (ascites, hepatic encephalopathy) have reduced physical activity and diminished food intake, which along with hyperammonemia decrease body weight and deteriorate muscle robustness.
There is a correlation between myosteatosis and obesity or total body fat percentage in patients with non-alcoholic fatty liver disease without cirrhosis [29,30]. In addition, in patients with morbid obesity and NASH, muscle fat content was reported high, but no low muscle mass was observed [31]. The population investigated in the above studies was totally different from that in current study. It concerned individuals with NASH usually without cirrhosis [29,30,31]. In the present study, only patients with cirrhosis were included and the vast majority of them had alcoholic or viral etiology. Only a small part had NASH or cryptogenic cirrhosis. Moreover, we did not demonstrate any correlation of myosteatosis with increased visceral fat deposition or elevated body weight. On the contrary, we detected a link between the presence of myosteatosis and reduced dry body weight implying that mechanisms other than insulin resistance or fat accumulation might explain the high rate of myosteatosis in end-stage liver disease. There is evidence of increasing global burden of NASH-relating cirrhosis with established “pre-existing” obesity-related myosteatosis and alterations in muscle and adipose tissue. Hence, it remains to be seen whether the above-mentioned relationships between myosteatosis and liver-related outcomes are upheld in these patient populations.
We used CT imaging to assess myosteatosis and we selected the muscle attenuation cut-offs proposed by previous investigators [9,32]. CT is a widely available method; it can be acquired as part of clinical routine in patient care and was reported as the best option for estimating myosteatosis [18,27,32,33]. However, CT cannot directly measure the location of fat deposition or lipid droplets in the muscle and cannot differentiate among potential phenotypes of fat distribution [1,34]. Therefore, the type and location of muscle fat infiltration occurring in different settings of liver disease need to be further examined.
We also demonstrated that muscle changes were increasing in accordance with liver disease severity. Four main phenotypes according to the extent of muscle changes were exhibited: neither MS nor sarcopenia, myosteatosis alone, myosteatosis combined by decreased muscle force (sarcopenia according to EWGSOP-2) [2] and myosteatosis coexisting with decreased muscle strength and muscle wasting (sarcopenia according to EWGSOP-2) [2]. The magnitude of muscle abnormalities aligned with the severity of liver cirrhosis, increasing age, and waning in muscle force and functionality. Muscle attenuation level (degree of myosteatosis) was better in the myosteatosis alone phenotype but worsened further in phenotype where myosteatosis coexisted with decreased muscle strength and mass loss. Only three persons had low handgrip strength and muscle mass (sarcopenia) without myosteatosis, showing that myosteatosis usually precedes subsequent muscle abnormalities in this clinical setting. The presence of myosteatosis alone in earlier stages as opposed to additive muscle defects in late stages of liver cirrhosis may imply that myosteatosis antedated muscle force decline and sarcopenia during the natural course of liver cirrhosis. On the other hand, myosteatosis acted synergistically with muscle mass loss and impaired performance in late stages of liver cirrhosis.
Previous investigators have reported that the presence of myosteatosis is a poor prognostic factor for liver cirrhosis outcome [12,13,35]. In the present study, no patient died during one year-follow-up in non-myosteatosis group. In addition, we demonstrated that myosteatosis is associated with high risk of death after adjusting for multiple covariates. When we divided patients into groups according to the extent of muscle changes, we discovered that mortality risk was increasing as the muscle quantity, quality and performance worsened. More specifically, patients with all three changes (myosteatosis, low muscle force and muscle mass loss) had more than three times higher risk of death than those with myosteatosis alone.
Our study acknowledges particular strengths. The sample is large and well studied, dry body weight has been used, the methods of measuring muscle mass, quality and body composition of adipose tissue are sophisticated, and those of diagnosing sarcopenia are based on the most recently updated criteria.
The limitations of the study include the lack of muscle biopsies for the location of fat deposition and the absence of longitudinal data to better investigate the evolution of myosteatosis during the course of liver cirrhosis from compensated to decompensated.
In conclusion, the presence of myosteatosis was positively associated with age and severity of liver cirrhosis and it was inversely associated with skeletal muscle mass, performance, and BMI. The magnitude of muscle abnormalities in liver cirrhosis is proportional to age and severity of liver disease. Myosteatosis alone is present in earlier stage of the disease and younger age and may indicate a prodromal phase of muscle degeneration before the development of sarcopenia. Myosteatosis is a poor prognostic factor of outcome after adjusting for multiple covariates. The combination of multiple muscle abnormalities has an unfavorable effect on survival.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12093332/s1, Table S1: Comparison of demographics and clinical characteristics among 4 groups according to the extent of muscle abnormalities (patients 194).
Author Contributions
Conceptualization, E.G., M.D.K. and A.A.; Methodology, E.G., M.D.K., L.V., I.M., R.T., V.S., I.V. and A.A.; Software, T.A. and L.V.; Validation, E.G., T.A., M.D.K., L.V., I.M., R.T. and I.V.; Formal analysis, E.G., T.A. and V.S.; Investigation, E.G., M.D.K., I.M., R.T. and I.V.; Data curation, E.G.; Writing—original draft, E.G. and A.A.; Writing—review & editing, T.A., M.D.K., L.V., I.M., R.T., V.S., I.V. and A.A.; Visualization, T.A. and L.V.; Supervision, A.A.; Project administration, A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by Ethics Committee of the Hippokration Hospital, Athens, Greece, Approval number 14881.
Informed Consent Statement
All individuals signed an informed consent statement.
Data Availability Statement
Data are available on request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Correa-De-Araujo, R.; Addison, O.; Miljkovic, I.; Goodpaster, B.H.; Bergman, B.C.; Clark, R.V.; Elena, J.W.; Esser, K.A.; Ferrucci, L.; Harris-Love, M.O.; et al. Myosteatosis in the Context of Skeletal Muscle Function Deficit: An interdisciplinary workshop at the national institute on aging. Front. Physiol. 2020, 11, 963. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Aging 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Lang, T.; Cauley, J.A.; Tylavsky, F.; Bauer, D.; Cummings, S.; Harris, T.B. Computed tomographic measurements of thigh muscle cross-sectional area and attenuation coefficient predict hip fracture: The health, aging, and body composition study. J. Bone Miner Res. 2010, 25, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Frank-Wilson, A.W.; Chalhoub, D.; Figueiredo, P.; Jónsson, P.V.; Siggeirsdóttir, K.; Sigurdsson, S.; Eiriksdottir, G.; Guðnason, V.; Launer, L.; Harris, T.B.; et al. Associations of quadriceps torque properties with muscle size, attenuation, and intramuscular adipose tissue in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Loosen, S.H.; Schulze-Hagen, M.; Püngel, T.; Bündgens, L.; Wirtz, T.; Kather, J.N.; Vucur, M.; Paffenholz, P.; Demir, M.; Bruners, P.; et al. Skeletal muscle composition predicts outcome in critically ill patients. Crit. Care Explor. 2020, 2, e0171. [Google Scholar] [CrossRef]
- Fang, T.; Gong, Y.; Wang, Y. Prognostic values of myosteatosis for overall survival in patients with gastric cancers: A meta-analysis with trial sequential analysis. Nutrition 2023, 105, 111866. [Google Scholar] [CrossRef]
- Avesani, C.M.; de Abreu, A.M.; Ribeiro, H.S.; Brismar, T.B.; Stenvinkel, P.; Sabatino, A.; Lindholm, B. Muscle fat infiltration in chronic kidney disease: A marker related to muscle quality, muscle strength and sarcopenia. J. Nephrol. 2023, 36, 895–910. [Google Scholar] [CrossRef] [PubMed]
- Miljkovic, I.; Kuipers, A.; Cauley, J.A.; Prasad, T.; Lee, C.G.; Ensrud, K.; Cawthon, P.M.; Hoffman, A.R.; Dam, T.-T.; Gordon, C.L.; et al. Osteoporotic Fractures in Men Study Group. Greater skeletal muscle fat infiltration is associated with higher all-cause and cardiovascular mortality in older men. J. Gerontol. A Biol. Sci. Med. Sci. 2015, 70, 1133–1140. [Google Scholar] [CrossRef]
- Bhanji, R.A.; Moctezuma-Velazquez, C.; Duarte-Rojo, A.; Ebadi, M.; Ghosh, S.; Rose, C.; Montano-Loza, A.J. Myosteatosis and sarcopenia are associated with hepatic encephalopathy in patients with cirrhosis. Hepatol. Int. 2018, 12, 377–386. [Google Scholar] [CrossRef]
- Nardelli, S.; Lattanzi, B.; Merli, M.; Farcomeni, A.; Gioia, S.; Ridola, L.; Riggio, O. Muscle alterations are associated with minimal and overt hepatic encephalopathy in patients with liver cirrhosis. Hepatology 2019, 70, 1704–1713. [Google Scholar] [CrossRef]
- Nardelli, S.; Gioia, S.; Ridola, L.; Carlin, M.; Cioffi, A.D.; Merli, M.; Spagnoli, A.; Riggio, O. Risk of falls in patients with cirrhosis evaluated by timed up and go test: Does muscle or brain matter more? Dig. Liver Dis. 2022, 54, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Lattanzi, B.; Nardelli, S.; Pigliacelli, A.; Di Cola, S.; Farcomeni, A.; D’ambrosio, D.; Gioia, S.; Corradini, S.G.; Lucidi, C.; Mennini, G.; et al. The additive value of sarcopenia, myosteatosis and hepatic encephalopathy in the predictivity of model for end-stage liver disease. Dig. Liver Dis. 2019, 51, 1508–1512. [Google Scholar] [CrossRef] [PubMed]
- Ebadi, M.; Tsien, C.; Bhanji, R.A.; Dunichand-Hoedl, A.R.; Rider, E.; Motamedrad, M.; Mazurak, V.C.; Baracos, V.; Montano-Loza, A.J. Skeletal muscle pathological fat infiltration (myosteatosis) is associated with higher mortality in patients with cirrhosis. Cells 2022, 11, 1345. [Google Scholar] [CrossRef] [PubMed]
- Meister, F.A.; Bednarsch, J.; Amygdalos, I.; Boecker, J.; Strnad, P.; Bruners, P.; Lang, S.A.; Ulmer, T.F.; Heij, L.; Santana, D.A.M.; et al. Various myosteatosis selection criteria and their value in the assessment of short- and long-term outcomes following liver transplantation. Sci. Rep. 2021, 11, 13368. [Google Scholar] [CrossRef]
- Czigany, Z.; Kramp, W.; Lurje, I.; Miller, H.; Bednarsch, J.; Lang, S.A.; Ulmer, T.F.; Bruners, P.; Strnad, P.; Trautwein, C.; et al. The role of recipient myosteatosis in graft and patient survival after deceased donor liver transplantation. J. Cachexia Sarcopenia Muscle 2021, 12, 358–367. [Google Scholar] [CrossRef]
- Mourtzakis, M.; Prado, C.M.; Lieffers, J.R.; Reiman, T.; McCargar, L.J.; Baracos, V.E. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl. Physiol. Nutr. Metab. 2008, 33, 997–1006. [Google Scholar] [CrossRef]
- Larson-Meyer, D.E.; Smith, S.R.; Heilbronn, L.K.; Kelley, D.E.; Ravussin, E.; Newcomer, B.R. Look AHEAD Adipose Research Group. Muscle-associated triglyceride measured by computed tomography and magnetic resonance spectroscopy. Obesity 2006, 14, 73–87. [Google Scholar] [CrossRef]
- Ebadi, M.; Bhanji, R.A.; Tandon, P.; Mazurak, V.; Baracos, V.E.; Montano-Loza, A.J. Review article: Prognostic significance of body composition abnormalities in patients with cirrhosis. Aliment. Pharmacol. Ther. 2020, 52, 600–618. [Google Scholar] [CrossRef] [PubMed]
- Tachi, Y.; Kozuka, A.; Hirai, T.; Ishizu, Y.; Honda, T.; Kuzuya, T.; Hayashi, K.; Ishigami, M.; Goto, H. Impact of myosteatosis on skeletal muscle volume loss in patients with chronic liver disease. J. Gastroenterol. Hepatol. 2018, 33, 1659–1666. [Google Scholar] [CrossRef] [PubMed]
- Merli, M.; Berzigotti, A.; Zelber-Sagi, S.; Dasarathy, S.; Montagnese, S.; Genton, L.; Plauth, M.; Parés, A. EASL clinical practice guidelines on nutrition in chronic liver disease. J. Hepatol. 2019, 70, 172–193. [Google Scholar] [CrossRef]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardized approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef]
- Georgiou, A.; Papatheodoridis, G.V.; Alexopoulou, A.; Deutsch, M.; Vlachogiannakos, I.; Ioannidou, P.; Papageorgiou, M.V.; Papadopoulos, N.; Yannakoulia, M.; Kontogianni, M.D. Validation of cutoffs for skeletal muscle mass index based on computed tomography analysis against dual energy X-ray absorptiometry in patients with cirrhosis: The KIRRHOS study. Ann. Gastrenterol. 2020, 33, 80–86. [Google Scholar] [CrossRef]
- Freire, A.N.; Guerra, R.O.; Alvarado, B.; Guralnik, J.M.; Zunzunegui, M.V. Validity and reliability of the short physical performance battery in two diverse older adult populations in Quebec and Brazil. J. Aging Health 2012, 24, 863–878. [Google Scholar] [CrossRef]
- Carey, E.; Lai, J.; Wang, C.; Dasarathy, S.; Lobach, I.; Montano-Loza, A.J.; Dunn, M.A. A multicenter study to define sarcopenia in patients with end-stage liver disease. Liver Transpl. 2017, 23, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Davuluri, G.; Allawy, A.; Thapaliya, S.; Rennison, J.H.; Singh, D.; Kumar, A.; Sandlers, Y.; Van Wagoner, D.R.; Flask, C.A.; Hoppel, C.; et al. Hyperammonaemia-induced skeletal muscle mitochondrial dysfunction results in cataplerosis and oxidative stress. J. Physiol. 2016, 594, 7341–7360. [Google Scholar] [CrossRef] [PubMed]
- Albillos, A.; Lario, M.; Álvarez-Mon, M. Cirrhosis-associated immune dysfunction: Distinctive features and clinical relevance. J. Hepatol. 2014, 61, 1385–1396. [Google Scholar] [CrossRef] [PubMed]
- Ebadi, M.; Tsien, C.; Bhanji, R.A.; Dunichand-Hoedl, A.R.; Rider, E.; Motamedrad, M.; Mazurak, V.C.; Baracos, V.; Montano-Loza, A.J. Myosteatosis in cirrhosis: A review of diagnosis, pathophysiological mechanisms and potential interventions. Cells 2022, 11, 1216. [Google Scholar] [CrossRef]
- Purnak, T.; Yilmaz, Y. Liver disease and malnutrition. Best Pract. Res. Clin. Gastroenterol. 2013, 27, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Okada, H.; Hashimoto, Y.; Kumagai, M.; Nishimura, H.; Oda, Y.; Fukui, M. Relationship between nonalcoholic fatty liver disease and muscle quality as well as quantity evaluated by computed tomography. Liver Int. 2020, 40, 120–130. [Google Scholar] [CrossRef] [PubMed]
- De Munck, T.J.; Verhaegh, P.; Lodewick, T.; Bakers, F.; Jonkers, D.; Masclee, A.A.; Verbeek, J.; Koek, G.H. Myosteatosis in nonalcoholic fatty liver disease: An exploratory study. Clin. Res. Hepatol. Gastroenterol. 2021, 45, 101500. [Google Scholar] [CrossRef]
- Nachit, M.; Kwanten, W.J.; Thissen, J.-P.; De Beeck, B.O.; Van Gaal, L.; Vonghia, L.; Verrijken, A.; Driessen, A.; Horsmans, Y.; Francque, S.; et al. Muscle fat content is strongly associated with NASH: A longitudinal study in patients with morbid obesity. J. Hepatol. 2021, 75, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Montano-Loza, A.J.; Angulo, P.; Meza-Junco, J.; Prado, C.M.M.; Sawyer, M.B.; Beaumont, C.; Esfandiari, N.; Ma, M.; Baracos, V.E. Sarcopenic obesity and myosteatosis are associated with higher mortality in patients with cirrhosis. J. Cachexia Sarcopenia Muscle 2016, 7, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.; Kim, D.W.; Ko, Y.; Ha, J.; Bin Shin, Y.; Lee, J.; Sung, Y.S.; Kim, K.W. Updated systematic review and meta-analysis on diagnostic issues and the prognostic impact of myosteatosis: A new paradigm beyond sarcopenia. Ageing Res. Rev. 2021, 70, 101398. [Google Scholar] [CrossRef]
- Henin, G.; Lanthier, N.; Dahlqvist, G. Pathophysiological changes of the liver-muscle axis in end-stage liver disease: What is the right target? Acta Gastroenterol. Belg. 2022, 85, 611–624. [Google Scholar] [CrossRef] [PubMed]
- Bot, D.; Droop, A.; Lucassen, C.J.; van Veen, M.E.; van Vugt, J.L.A.; Feshtali, S.S.; Leistra, E.; Tushuizen, M.E.; van Hoek, B. Both muscle quantity and quality are predictors of waiting list mortality in patients with end-stage liver disease. Clin. Nutr. ESPEN 2021, 42, 272–279. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).