Abstract
In recent years, vibrational devices have been introduced in order to reduce patient discomfort in some situations such as orofacial pain, orthodontic therapy, and injection of local anaesthetics. This article aims to review the clinical experience given by the use of these devices in local anaesthesia. The literature search was carried out on the main scientific databases for articles up to November 2022. Eligibility criteria were established, and pertinent articles selected. The results were classified by author, year, type of study, sample size and characteristics, purpose of use, type of vibrational device used, protocol used, and outcomes. Nine relevant articles were found. These are split mouth randomized clinical trials which evaluate the reduction in pain perception with different devices and different protocols of use in children, during procedures which require local analgesia by injection, compared with traditional local anaesthesia with premedication based on anaesthetic gels. Different objective and subjective scales of pain and discomfort perception were used. Although results are promising, some data, such as those relating to vibrational intensity and frequency, are not clear. Evaluations on samples varying by age and context of use are necessary to fully define the indications for this type of aid during oral rehabilitation procedures.
1. Introduction
According to the International Association for the Study of Pain “Pain is an unpleasant sensory and emotional experience associated with defined or potential tissue damage or described in respect to such damage” [1]. The fear of dental procedures and treatments is one of the strongest fears in both paediatric and adult age groups [2,3,4]. This is particularly related to dental procedures in which needles are used, such as in local anaesthesia [5,6,7]. This happens mainly because patients often start dental sessions due to the presence of painful lesions (caries, periapical lesions, dental fractures, etc.), so are in a condition of stress and generalized fear [8,9,10]. The functional limitation due to temporomandibular dysfunction is often already accompanied by symptoms such as pain, and its therapeutic approach can itself stimulate the perception of pain and discomfort [11,12,13,14]. Even orthodontic therapy, regardless of the type of device used, is often perceived by patients as a painful and unpleasant [15,16,17,18,19]. For a long time, great attention has been paid to the possibility that alternative methods to the oral administration of analgesics, properly conveyed, can reduce the perception of various types of dental pain by promoting a state of well-being in the patient [20]. Transcutaneous electrical nerve stimulation (TENS), acupuncture, vibration, and conditioned pain modulation (CPM) are methods capable of controlling mechanisms underlying pain inhibition [20,21]. Much has been written on these topics and research continues to be carried out in this field [22,23]. In particular, the application of vibrational stimuli of low (30 Hz) or higher (up to 120 Hz) intensity would be able to reduce both the sensation of orthodontic dental pain, for a stimulation of local cellular metabolism that includes modulation of periodontal chemical mediators of inflammation (also involved in orthodontic movement due to an effect on bone remodelling), and orofacial and temporo-mandibular joint pain for a more extensive action that, similarly, improves blood and lymphatic circulation by relieving pain and improving functional recovery [24,25,26,27]. Local anaesthesia is one of the most frequently needed procedures to rehabilitate the patient, and is also the one often perceived as most painful and undesirable [6,7,8,28]. Many recent studies have documented the use of additional vibrational stimuli to relieve pain during the administration of local anaesthesia [29,30,31]. Yet, there are still no reviews of the literature on the subject. The main objective of this scoping review is to focus on the differences between any existing protocols (applied strength and frequency) and available devices to determine whether vibrations can significantly contribute to reducing pain in the administration of local anaesthesia during dental procedures.
2. Materials and Methods
This scoping review project has been now (27 December 2022) registered as an Open-Ended Registration on OSF Registries (Open Science Framework, Center for Open Science©, 2011–2022). The search for sources for this scoping review of the literature began on 28 November 2022 and ended on 30 November 2022 by consulting four databases: PubMed, Scopus, Lilacs, and the Cochrane Library (Figure 1). Based on the acronym PCC (Population/Problem, Concept, Context), the research question that was set was the following: “Do dental patients under the effect of additional vibrational forces have a pain relief during dental local anaesthesia?” (Table 1). The search was conducted using the following MeSH terms and free terms in combination with the Boolean operators “AND” and “OR”: vibration, dentistry, paediatric dentistry, mouth, anaesthesia, pain. The two operators involved in the research of the sources carried out their activity independently, respecting specific inclusion criteria. The studies included in the review were of the randomized and non-randomized comparative clinical type. In vitro studies, finite element analysis studies, animal studies, case reports (and case series), and reviews were not eligible (Table 2). The bibliographic entries of each selected study and any previous reviews, when available, were consulted to avoid leaving out studies useful for this scoping review that may not have been among the search results. There were no restrictions on the year of publication. Only studies in English, for which abstract and full text were available, were ultimately considered. The results of the source search conducted by each operator were collected separately and then merged by Zotero software (Zotero 5.0 for Windows, Corporation for Digital Scholarship, Vienna, VA, USA) to eliminate any duplicates. In case of doubts about the contents of the abstracts of some studies, these were included for the full text reading and subsequent evaluation. Both review practitioners subsequently read the selected studies individually and confirmed or rejected inclusion in the scoping review. In the event of conflicting opinions, they consulted each other until they reached an unambiguous opinion. The two reviewers independently charted the data and discussed the results. Data related to each study characteristic included in the review were abstracted. In the results section, the studies will be grouped and summarized by study design, types of devices, and protocols used, only if appropriate.
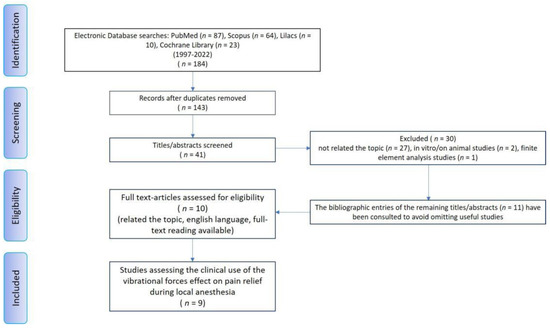
Figure 1.
Review flow diagram for the scoping review detailing the database searches, the number of abstract screened, and the full texts retrieved.

Table 1.
Research question based on the PCC (Population/Problem, Concept, Context) strategy.

Table 2.
Inclusion and Exclusion criteria.
3. Results
The database search initially yielded 184 results (PubMed 87, Lilacs 10, Cochrane Library 23, Scopus 64). Duplicates were removed with the help of the Zotero software. Following this phase, the remaining 41 results were checked for eligibility criteria by reading the abstracts. With this selection, 30 scientific articles were further discarded because they did not meet the eligibility criteria. Of the remaining 11 articles, useful for the review, the bibliographic entries were consulted to look for any further studies suitable for the review that had not emerged from the initial search. No other studies resulted from this supplemental research; so, only the original 10 articles were confirmed for the scoping review by full text reading. One study has been excluded because the full-text article was not available also after request to the authors, and another one was excluded because no outcome was reported. Therefore, only nine articles were included in the scoping review (Figure 1). The included studies were classified by author, year, type of study, sample size and its characteristics (sex, age), goal of the research, type of vibrational device used, protocol used, and pain relief as the outcome (Table 3).

Table 3.
Research articles included in the scoping review.
The studies subject to the scoping review were published between 1997 and 2022. The total number of patients involved in studies on the use of supplementary vibrations during local anaesthesia in dental procedures should be equal to 611 subjects. Considering that only three studies specify the sex of the patients involved, we cannot state the distribution between the two sexes is homogeneous. Only three studies do not clarify the range of age of the patients [29,32,33]; overall, the patients involved are aged between 5 and 12 years, except for the two studies which do not clarify age range and classify their patients as adults [32,33]. Regarding the type of study, all the studies were split mouth randomized clinical trials. The experimental approach always included two sessions: one in which the traditional procedure is used in a dental hemiarch (premedication with anaesthetic gel and subsequent infiltration of the anaesthetic with syringe), and the other in which the vibrational device is applied before and during the injection. The experimental and control sides as well as which of the two interventions to perform in the first and second sessions are chosen randomly. On the control side, premedication with anaesthetic gels is carried out with 20% benzocaine [29,32,38], 8% lignocaine and 0.8% dibucaine [34], lignocaine hydrochloride 2% [31,33,36]. Injections infiltrate lidocaine with 1:100,000 epinephrine in all the studies except one where dental analgesia is obtained with Ubistesin-4% Articaine with epinephrine 1:200,000. Needles, when specified, are all around 24–27 gauges. Indications to dental anaesthesia in patients recruited in the research are not explained. Sites for injections, when the information is specified, are palatal [33] infraorbital [33], upper posterior buccal [32,33,37], inferior alveolar nerve block [33,36,37], and posterior palatal [37]. The vibrational devices used are a modified battery-powered shaver (Windmere Corp., Miami, FL) [32], DentalVibe® Injection Comfort system (BING Innovations, FL, USA) [29,33,34,36], Buzzy® (MMJ Labs, Atlanta GA, USA) [31,35], and Vibraject (Vibraject®MiltexInc LLC., York, PA, USA) [37]. One study shows the photo of the device used but does not give a trade name or provide information about its origin [30]. Except for one study, the others do not clarify what frequency or vibrational intensity the device is set to [32]. In all studies, the vibrational device is applied before, during, and after the injection of anaesthetic, but it is not always clear how long before and after the injection it is activated, and if there are any precautions to consider for better use. In the two studies where the Buzzy® device is used [31,35], a gel ice pack comprising water, sodium polyacrylate, and mixed isothiazolinones cooled to 5 °C for 30 s is applied to improve pain relief with vibrational stimulation. The response of the subjects involved in the trials is evaluated according to objective or subjective scales of measurement of stress, discomfort, and pain. In addition to heart rate and pO2 saturation [30,35,36], the most used scales were Iowa Cancer Pain Relief Initiative scale [32], VAS (visual analogue scale) [33,37], Wong–Baker score pain scale [35,36], FLACC (Faces, Legs, Activity, Cry, Consolability) score [30,31,35,37], RMS Pictorial Scale (RMS-PS) [31], and sound, eye, motor (SEM) scale [36]. Except for one study, according to which there are no differences compared to premedication with anaesthetic gel [36], all the others agree in stating that vibration (and where expected, also cold gel pack) reduces the perception of anxiety and pain related to the injection of the local anaesthetic, also aided by the noise of the vibrational device as a distracting element at the moment of injection.
4. Discussion
In this scoping review, we identified nine studies addressing vibrational stimuli as a method aimed at relieving pain during local dental anaesthesia, which were published between 1997 and 2022. Our results indicate a moderate focus of research, in particular, on the dissemination of knowledge and use in the context of the benefit given by local vibration at the time of infiltrative anaesthesia or nerve block. The biological mechanisms underlying this advantageous method in the field of local anaesthesia would be different from those underlying local vibrational stimulation in orthodontics, which are well documented and recognized [22,24,38,39]. From the first study reported in this review, which uses a device with another modified intended use to transfer the vibration at the injection site [32], to the most recent ones mentioned [29,30,31,33,34,35,36,37], in which dedicated devices are used, about twenty years have passed, and undoubtedly also the biological mechanisms to prove its effectiveness are better known. It would seem that “intermittent micro-sonic oscillations to the brain’s neurological pain sensors, closing the pain gate, blocking the pain of injections and is also more useful for paediatric patients and those who have a phobia of intraoral injection or pain as there is an audible distraction (70–75 db) provided” [34]. Stimulation such as vibration can reduce pain based on Ronald Melzack and Patric Wall’s gate control theory. Under this theory of controlling vibration-induced pain relief, painful sensations can be reduced through simultaneous activation of large-diameter nerve fibres that conduct non-harmful stimuli (touch and vibration) [36]. The brain cannot perceive more than one sensation at the same time [32,34,40]. Therefore, the feeling that reaches the brain first will be what the subject will actually feel. So, as a counter-stimulation, vibration reduces painful perception. [41] The oral region is very sensitive because more than a third of the cells in the somatosensory cortex of the brain are dedicated to the sensory inputs of the mouth [32]. The physiological basis of pain relief by vibration is extensively described in one of the most recent studies published on this topic and included in this review. The range of stimulation used stimulates two mechanoreceptors: mainly the Pacinian corpuscle nerve endings, and possibly the Meissner’s corpuscle nerve endings. They are “primarily responsible for vibration detection and high discrimination touch, respectively. Both signals are transmitted via Aβ nerve fibres, which are relatively large-diameter nerve fibres. The pain of injection is transmitted via the small-diameter Aδ and C nerve fibres, primarily Aδ for the pricking pain of needle insertion” and “Vibration or scratching can alter the steady state of the Aβ fibres in a way that exceeds their adaptation potential, which leads to suppression of pain signals transmitting via smaller fibres” [29]. This could explain the efficacy of this method in dental anaesthesia. It would also seem true that the reduction in pain is greater if the source of vibration is applied not only within the area directly affected by the painful stimulus, but also when the application of vibration stimulates the underlying bone on the same side as the perceived pain. This should encourage the development of devices in which the vibratory stimulus is conveyed more and more in a site-specific way with the anaesthetic. The integrated and non-integrated vibration/injection systems currently available are used in comparative studies, always of split mouth type, in order to evaluate how this element is decisive in the effectiveness of the method. As we have seen from the results of this review, the studies reported almost all have a sample of paediatric patients. Although the reason for this choice is not always made clear by the various authors, the reason could lie not only in the fact that children are the most vulnerable category of patients but, as expressed in a study included in the review, the choice of the age range of the sample may be linked to the fact that it is “an age where cognitive development begins to manifest itself” [31]. A final feature that emerged and to consider is that the studies considered almost all refer to both objective and subjective measurements of anxiety and pain. In this review, the studies included made use of five pain measurement scales. The most used scale in the medical field for its simplicity is the VAS (visual analogue scale), especially to describe subjective emotions such as pain [42]. The Iowa Cancer Pain Relief Initiative scale is useful to rate behavioural changes related to pain. Thirty characteristics are assessed, and the participant is asked to rate both the extent to which the behaviour is present and degree of change from baseline [32]. The Wong–Baker FACES pain rating scale is often preferred by parents and patients for reporting pain severity. However, the “no hurt” and “hurts worst” anchor risk to confound pain measurement with non-nociceptive states [43]. The Face, Legs, Activity, Cry, and Consolability (FLACC) scale is one of the most commonly and widely used behavioural observation pain scales [44]. It is also the most frequently used scale used in the studies included in this review [30,31,35,37]. Although developed and validated to evaluate postoperative pain, this scale is currently applied to assess acute pain in multiple settings, including in the emergency department, and it is considered an appropriate observational tool in acute pain assessment in the paediatric population. The RMS Pictorial Scale (RMS-PS) used in one of the studies included in the review [31]. It is an innovative scale for the assessment of a child’s dental anxiety. Also, even if scarcely documented in literature, its application looks promising [45]. One study assessed pain perception using the sound, eye, motor (SEM) scale based on its rating of the patient’s reaction during injection [36]. This scale, such as the FLACC, is often used in combination with other scales to assess the patient’s subjective pain and stress perception, avoiding the use of an operator’s assessment scale [46].
5. Conclusions
The use of devices that convey vibrational stimuli to the tissues surrounding those that will be affected shortly thereafter by the injection of anaesthetic, in the different dental procedures with analgesia, can be valuable in terms of reducing the perception of the painful stimulus on the basis of the biological and receptor mechanisms already known. The paediatric indication is currently the most widely documented in literature, but expanding experiences on different age ranges can be important. The operational protocols and the objective and subjective assessment scales to interpret patient responses are still not uniform to provide a reference guide for clinicians who decide they want their patients to benefit from this comfortable operational support.
Author Contributions
Conceptualization, A.P. and S.Z.; methodology, E.M.; validation, S.Z., A.P. and E.M.; formal analysis, A.P.; investigation, M.R.A.; resources, A.P. and M.R.A.; data curation, A.P.; writing—original draft preparation, A.P.; writing—review and editing, S.Z.; visualization, E.M.; supervision, S.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data will be available on request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- International Association for the Study of Pain (IASP). IASP Taxonomy. Available online: https://www.iasppain.org/Education/Content.aspx?ItemNumber=1698#Pain. (accessed on 28 November 2022).
- Wu, L.; Buchanan, H.; van Wijk, A.J. Translation and Validation of the Short Form of the Fear of Dental Pain Questionnaire in China. Front. Psychol. 2021, 12, 721670. [Google Scholar] [CrossRef] [PubMed]
- Lima, D.S.M.; Barreto, K.A.; Rank, R.C.I.C.; Vilela, J.E.R.; Corrêa, M.S.N.P.; Colares, V. Does previous dental care experience make the child less anxious? An evaluation of anxiety and fear of pain. Eur. Arch. Paediatr. Dent. 2021, 22, 139–143. [Google Scholar] [CrossRef]
- Renton, T. Introduction to Pain. Prim. Dent. J. 2019, 7, 17–21. [Google Scholar] [CrossRef]
- Al Qutub, A.W. Pain Experience after Dental Implant Placement Compared to Tooth Extraction. Int. J. Dent. 2021, 2021, 4134932. [Google Scholar] [PubMed]
- Colares, V.; Franca, C.; Ferreira, A.; Amorim Filho, H.A.; Oliveira, M.C. Dental anxiety and dental pain in 5- to 12-year-old children in Recife, Brazil. Eur. J. Paediatr. Dent. 2013, 14, 15–19. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, G.; Alkhamis, N.; Mattarozzi, K.; Mazzetti, M.; Piana, G. Fear of dental pain in Italian children: Child personality traits and parental dental fear. J. Public Health Dent. 2016, 76, 179–183. [Google Scholar] [CrossRef]
- Jeddy, N.; Nithya, S.; Radhika, T.; Jeddy, N. Dental anxiety and influencing factors: A cross-sectional questionnaire-based survey. Indian J. Dent. Res. 2018, 29, 10–15. [Google Scholar]
- Rauch, A.; Hahnel, S.; Schierz, O. Pain, Dental Fear, and Oral Health-related Quality of Life-Patients Seeking Care in an Emergency Dental Service in Germany. J. Contemp Dent. Pract. 2019, 20, 3–7. [Google Scholar]
- Monteiro, J.; Tanday, A.; Ashley, P.F.; Parekh, S.; Alamri, H. Interventions for increasing acceptance of local anaesthetic in children and adolescents having dental treatment. Cochrane Database Syst. Rev. 2020, 2, CD011024. [Google Scholar] [CrossRef]
- Kroese, J.M.; Kopp, S.; Lobbezoo, F.; Alstergren, P. TMJ Pain and Crepitus Occur Early Whereas Dysfunction Develops Over Time in Rheumatoid Arthritis. J. Oral Facial Pain Headache 2020, 34, 398–405. [Google Scholar] [CrossRef]
- Lee, H.J.; Kim, S.T. A questionnaire-based study of sleep-wake patterns and sleep quality in a TMJ and orofacial pain clinic. Cranio 2020, 38, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Gazal, G. Overcoming temporomandibular joint clicking and pain. Cranio 2020, 38, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, I.M.; Brogårdh-Roth, S.; Månsson, J.; Ekberg, E. Temporomandibular pain in adolescents with a history of preterm birth. J. Oral Rehabil. 2019, 46, 589–596. [Google Scholar] [CrossRef]
- Cardoso, P.C.; Espinosa, D.G.; Mecenas, P.; Flores-Mir, C.; Normando, D. Pain level between clear aligners and fixed appliances: A systematic review. Prog. Orthod. 2020, 21, 3. [Google Scholar] [CrossRef]
- Lin, W.; Farella, M.; Antoun, J.S.; Topless, R.K.; Merriman, T.R.; Michelotti, A. Factors associated with orthodontic pain. J. Oral Rehabil. 2021, 48, 1135–1143. [Google Scholar] [CrossRef]
- Costa, E.O.D.; Blagitz, M.N.; Normando, D. Impact of catastrophizing on pain during orthodontic treatment. Dental Press J. Orthod. 2020, 25, 64–69. [Google Scholar] [CrossRef]
- Celebi, F.; Turk, T.; Bicakci, A.A. Effects of low-level laser therapy and mechanical vibration on orthodontic pain caused by initial archwire. Am. J. Orthod. Dentofacial Orthop. 2019, 156, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P.S.; Strydom, H.; Katsaros, C.; MacDonald, L.; Curatolo, M.; Fudalej, P.; Pandis, N. Non-pharmacological interventions for alleviating pain during orthodontic treatment. Cochrane Database Syst. Rev. 2016, 12, CD010263. [Google Scholar] [CrossRef]
- Fujii-Abe, K.; Umino, M.; Kawahara, H.; Terada, C.; Satomura, K.; Fukayama, H. New method for postoperative pain relief using a combination of noxious and non-noxious stimuli after impacted wisdom tooth extraction. J. Oral Sci. 2019, 61, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Çebi, A.T. Effects of transcutaneous electrical nerve stimulation on pain after impacted third molar surgery. Med. Oral Patol. Oral Cir. Bucal. 2019, 24, e404–e408. [Google Scholar] [CrossRef]
- Çelebi, F. Mechanical Vibration and Chewing Gum Methods in Orthodontic Pain Relief. Turk. J. Orthod. 2022, 35, 133–138. [Google Scholar] [CrossRef]
- Johnson, M.I.; Paley, C.A.; Wittkopf, P.G.; Mulvey, M.R.; Jones, G. Characterising the Features of 381 Clinical Studies Evaluating Transcutaneous Electrical Nerve Stimulation (TENS) for Pain Relief: A Secondary Analysis of the Meta-TENS Study to Improve Future Research. Medicina 2022, 58, 803. [Google Scholar] [CrossRef]
- Taha, K.; Conley, R.S.; Arany, P.; Warunek, S.; Al-Jewair, T. Effects of mechanical vibrations on maxillary canine retraction and perceived pain: A pilot, single-center, randomized-controlled clinical trial. Odontology 2020, 108, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Muir, B.; Brown, C.; Brown, T.; Tatlow, D.; Buhay, J. Immediate changes in temporomandibular joint opening and pain following vibration therapy: A feasibility pilot study. J. Can. Chiropr. Assoc. 2014, 58, 467–480. [Google Scholar]
- Pigg, M. Chronic intraoral pain--assessment of diagnostic methods and prognosis. Swed. Dent. J. Suppl. 2011, 220, 7–91. [Google Scholar]
- Hansson, P.; Ekblom, A.; Thomsson, M.; Fjellner, B. Influence of naloxone on relief of acute oro-facial pain by transcutaneous electrical nerve stimulation (TENS) or vibration. Pain 1986, 24, 323–329. [Google Scholar] [CrossRef]
- DiFelice, M.G.; Vandewalle, K.S.; Maller, S.C.; Hancock, R.H. Effects of a vibratory device on pain from anesthetic injections. Compend Contin. Educ. Dent. 2014, 35, 246, 248, 250–251. [Google Scholar]
- Salma, R.G.; Alsayeh, A.; Maneea, A.B.; Alrassan, F.; Almarshad, A. The effectiveness of electronic pulsed soft tissue vibration compared with topical anaesthesia in reducing the pain of injection of local anaesthetics in adults: A randomized controlled split-mouth clinical trial. Int. Oral Maxillofac. Surg. 2021, 50, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Hegde, K.M.; Srinivasan, I.; Melwani, A.; Radhakrishna, S. Effect of vibration during local anesthesia administration on pain, anxiety, and behavior of pediatric patients aged 6-11 years: A crossover split-mouth study. J. Dent. Anesth. Pain Med. 2019, 19, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.; Juneja, P.; Masih, U.; Bhushan, A.K.B.; Bhaduaria, U.S.; Badjatya, K. Efficacy of external cold and a vibrating device in reducing pain and anxiety during local anaesthesia. J. Family Med. Prim. Care 2021, 10, 4017–4022. [Google Scholar] [CrossRef]
- Hutchins, H.S., Jr.; Young, F.A.; Lackland, D.T.; Fishburne, C.P. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth. Prog. 1997, 44, 87–89. [Google Scholar] [PubMed]
- Nasehi, A.; Bhardwaj, S.; Kamath, A.T.; Gadicherla, S.; Pentapati, K.C. Clinical pain evaluation with intraoral vibration device during local anesthetic injections. J. Clin. Exp. Dent. 2015, 7, e23–e27. [Google Scholar] [CrossRef]
- Shilpapriya, M.; Jayanthi, M.; Reddy, V.N.; Sakthivel, R.; Selvaraju, G.; Vijayakumar, P. Effectiveness of new vibration delivery system on pain associated with injection of local anesthesia in children. J. Indian Soc. Pedod. Prev. Dent. 2015, 33, 173–176. [Google Scholar]
- Alanazi, K.J.; Pani, S.; AlGhanim, N. Efficacy of external cold and a vibrating device in reducing discomfort of dental injections in children: A split mouth randomised crossover study. Eur. Arch. Paediatr. Dent. 2019, 20, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Menni, A.C.; Radhakrishna, A.N.; Prasad, M.G. DentalVibe® versus lignocaine hydrochloride 2% gel in pain reduction during inferior alveolar nerve block in children. J. Dent. Anesth. Pain Med. 2020, 20, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Albouni, M.A.; Kouchaji, C.; Al-Akkad, M.; Voborna, I.; Mounajjed, R. Evaluation of the Injection Pain with the Use of Vibraject during Local Anesthesia Injection for Children: A Randomized Clinical Trial. J. Contemp. Dent. Pract. 2022, 23, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Telatar, B.C.; Gungor, A.Y. Effectiveness of vibrational forces on orthodontic treatment: A randomized, controlled clinical trial. J. Orofac. Orthop. 2021, 82, 288–294. [Google Scholar] [CrossRef]
- Reiss, S.; Chouinard, M.C.; Frias Landa, D.; Nanda, R.; Chandhoke, T.; Sobue, T.; Allareddy, V.; Kuo, C.L.; Mu, J.; Uribe, F. Biomarkers of orthodontic tooth movement with fixed appliances and vibration appliance therapy: A pilot study. Eur. J. Orthod. 2020, 42, 378–386. [Google Scholar] [CrossRef]
- Dalton, J.A.; McNaull, F. A call for standardizing the clinical rating of pain intensity using a 0 to 10 rating scale. Cancer Nurs. 1998, 21, 46–49. [Google Scholar] [CrossRef]
- Aminabadi, N.A.; Farahani, R.M.; Balayi Gajan, E. The efficacyof distraction and counterstimulation in the reduction of pain reaction to intraoral injection by pediatric patients. J. Contemp. Dent. Pract. 2008, 9, 33–40. [Google Scholar] [CrossRef]
- Chiarotto, A.; Maxwell, L.J.; Ostelo, R.W.; Boers, M.; Tugwell, P.; Terwee, C.B. Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: A systematic review. J. Pain 2019, 20, 245–263. [Google Scholar] [CrossRef] [PubMed]
- Garra, G.; Singer, A.J.; Domingo, A.; Thode, H.C., Jr. The Wong-Baker pain FACES scale measures pain, not fear. Pediatr. Emerg. Care 2013, 29, 17–20. [Google Scholar] [CrossRef]
- Crellin, D.J.; Harrison, D.; Santamaria, N.; Huque, H.; Babl, F.E. The Psychometric Properties of the FLACC Scale Used to Assess Procedural Pain. J. Pain 2018, 19, 862–872. [Google Scholar] [CrossRef] [PubMed]
- Shetty, R.M.; Khandelwal, M.; Rath, S. RMS Pictorial Scale (RMS-PS): An innovative scale for the assessment of child’s dental anxiety. J. Indian Soc. Pedod. Prev. Dent. 2015, 33, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Guner Onur, S.; Tonguc Altin, K.; Demetgul Yurtseven, B.; Haznedaroglu, E.; Sandalli, N. Children’s drawing as a measurement of dental anxiety in paediatric dentistry. Int. J. Paediatr. Dent. 2020, 30, 666–675. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).