Abstract
Objective: This study aims to investigate whether advanced age is an absolute contraindication for radical nephroureterectomy (RNU) in patients with upper tract urothelial carcinoma (UTUC) through a single-center case series and a systematic review with meta-analysis. Materials and methods: In the single-center case series, 588 UTUC patients who underwent RNU between May 2003 and June 2019 in West China Hospital were enrolled, and cancer-specific survival (CSS) was the primary outcome of interest. In the systematic review with meta-analysis, PubMed, Scopus, Embase, and Cochrane databases were systematically searched for related articles for further analysis. The endpoints for meta-analyses were overall survival (OS) and CSS. Results: The single-center case series included 57 (9.7%) octogenarians. The CSS of octogenarians after RNU was comparable to that of younger people. Advanced age (≥80) was not an independent risk factor for poor CSS (HR, 1.08; 95% CI, 0.48, 2.40). In a systematic review with meta-analysis, the cut-off value of advanced age is 70, and the results showed that advanced age was associated with inferior OS (pooled HR, 1.55; 95% CI, 1.29, 2.01) and CSS (pooled HR, 1.37; 95% CI, 1.08, 1.65). However, the subgroup analysis of countries found no positive correlation between advanced age and CSS (pooled HR, 1.33; 95% CI 0.92, 1.74) in Chinese. Conclusions: Advanced age may no longer be an absolute contraindication for RNU. RNU can be safely and effectively performed on UTUC patients of advanced age after a comprehensive presurgical evaluation.
1. Introduction
Urothelial carcinoma (UC) is the fourth most common malignancy in developed countries, and upper tract urothelial carcinoma (UTUC) only accounts for 5–10% of UC, with an estimated annual incidence of approximately 2 people per 100,000 [1,2]. Radical nephroureterectomy (RNU), with or without adjuvant therapy, serves as the gold standard treatment for high-risk organ-confined UTUC, providing durable local control and maximizing survival expectations [2]. Moreover, as upper tract urothelial carcinoma (UTUC) is most common in patients aged 70–90 years, the number of UTUC patients of advanced age worldwide is gradually increasing in the context of global aging.
Great advancements in anesthesia, surgical techniques (especially laparoscopy and robotics), and nursing during hospitalization have contributed to the theoretical and practical foundation of operations on elderly patients [3,4,5]. Recently, a growing number of studies have reported similar survival outcomes between younger and older patients after surgery [6,7]. However, whether RNU is a suitable and promising choice for patients of advanced age is heavily debated and remains unclear.
Therefore, the present study aims to investigate whether advanced age is an absolute contraindication for RNU by reporting the survival outcomes of UTUC patients with advanced age after RNU in Southwest China and placing our findings within the context of the literature by performing a systematic review and meta-analysis of studies on the topic of age and UTUC prognosis after RNU.
2. Methods and Materials
2.1. Single-Center Case Series
2.1.1. Patients and Data
Our study was approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (2021–1209), and the informed consent was allowed to be waived because of the retrospective nature, anonymous patients, and data. We retrospectively collected UTUC patients who had undergone RNU between May 2003 and June 2019 in the West China Hospital of Sichuan University. We excluded those with incomplete long-term prognostic information, those with non-urothelial carcinoma confirmed by RNU pathology, and we also excluded those who had a previous neoadjuvant therapy history. Ultimately, 588 patients were eligible for inclusion in further analysis (Figure 1a).
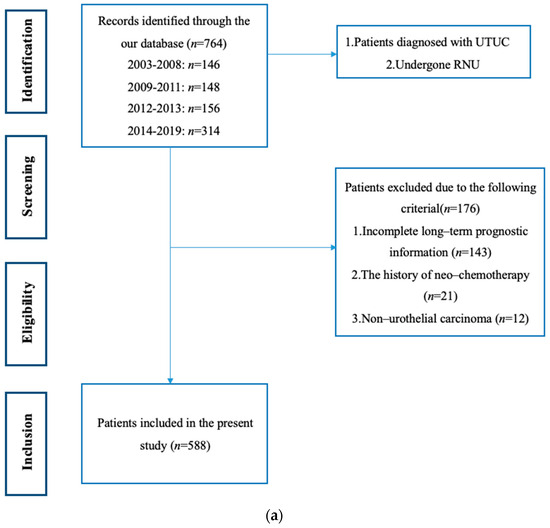
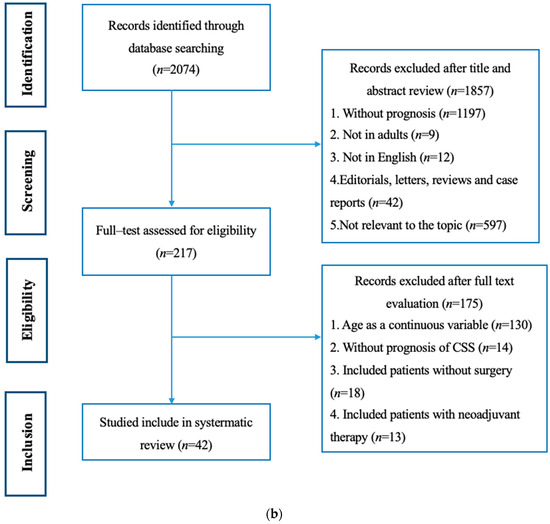
Figure 1.
(a) The specific screening flow chart of included patients. (b) The specific screening flow chart of included studies.
We collected clinical and pathological data from our hospital database. Clinical data included chronological age in the year of surgery, gender, body mass index (BMI), hemoglobin and albumin within 1 week before RNU, the American Society of Anesthesiologists (ASA) score, the history of adjuvant systemic chemotherapy, and surgical techniques. Pathological data included tumor location, tumor size, pathological tumor stage and grade, lymph node status, lymphovascular invasion (LVI), tumor architecture and multifocality, and surgical margin. The pathological tumor stage and grade were both derived by an independent review of RNU specimens by our professional urogenital pathologists, according to the American Joint Committee on Cancer (AJCC) tumor-node-metastasis (TNM) staging system and the WHO/ISUP recommendation grading system, respectively.
2.1.2. Follow-Up and Endpoints
Approximately 2 to 3 weeks after RNU is the rational time for first follow-up, at which time the pathological reports of the RNU specimen, including the general report and immunohistochemical report, have been completed. The main project was to analyze the nature of the primary tumor and make individual therapy plans. Generally, the protocol of subsequent follow-up was in accordance with the European Association of Urology guidelines. The patients were followed up every 3 months in the first year, every 6 months in the second year, and then once every 2 years if there were no recurrence or uncommon symptoms. The routine contents of follow-up included a physical examination, routine blood and urine tests, a contrast-enhanced computed tomography scan of the chest and abdomen, and cystoscopy.
Cancer-specific survival (CSS), defined as the time from RNU to death related to UTUC, and cancer-specific mortality were included in our study as the endpoints.
2.1.3. Statistical Analysis
Analysis was performed using the software packages R 4.3.2 (http://www.R-project.org; accessed on 21 September 2023, The R Foundation, Boston, MA, USA) and EmpowerStats 4.0 (http://www.empowerstats.com; accessed on 21 September 2023 X and Y Solutions, Inc., Boston, MA, USA). Continuous variables were expressed as medians with interquartile ranges (IQRs), and categorical variables were expressed as numbers with percentages. Significant differences between groups were determined by the χ2 test and Mann–Whitney U test. CSS was calculated using Kaplan–Meier analysis, and the log-rank test was used for comparison. Cox proportional hazard models were used to investigate the associations of clinicopathological information with CSS by calculating HRs (95% CI). All statistical assessments were two-tailed and considered statistically significant at p < 0.05.
2.2. Systematic Review and Meta-Analysis
The conduct and reporting form of this meta-analysis were in accordance with the Meta-Analysis extension of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA-NMA) reporting guidelines [8]. The PRISMA checklist was provided in Supplementary Table S1.
2.2.1. Search Strategy and Selection Criteria
The PubMed, Scopus, Embase, and Cochrane databases were systematically searched for related articles. The predefined search terms are “UTUC,” “upper tract urothelial carcinoma,” “upper tract urinary carcinoma,” “urothelial carcinoma,” “renal pelvis and ureter tumor,” “radical nephroureterectomy” and “RNU”. Synonyms were combined by the Boolean operator (OR), and paratactic terms were combined by the Boolean operator (AND).
Population, intervention, comparison, outcomes, and study (PICOS) principles were used during the screening process [9], where PICOS stands for: population (P)—patients diagnosed with UTUC; intervention (I)—RNU surgery; comparison (C)—octogenarians and younger patients; outcomes (O)—cancer-specific mortality and CSS; and study designs (S)—retrospective comparative studies. The exclusion criteria were as follows: (a) age was regarded as a continuous variable; (b) not all patients had received RNU; (c) included patients with neoadjuvant therapy; and (d) there was no specific information on CSS. The specific screening flow chart is shown in Figure 1b.
2.2.2. Data Extraction and Quality Assessment
Two reviewers (JJY and QYW) independently extracted the following data, and disagreements were resolved through consensus: (1) first author’s name, (2) publication year, (3) country, (4) retrospective period, (5) number of patients, (6) median age, (7) cut-off value of age, (8) median follow-up time, (9) RNU surgical method, (10) use of neo-/adjuvant therapy, and (11) survival outcomes of overall survival (OS) and CSS.
The risk of bias was assessed independently by two investigators (JJY and XYL) using the Newcastle Ottawa Scale (NOS). The risk of bias was grouped into three categories, including “high quality” (points range: 7–9), “moderate quality” (points range: 4–6), and “low quality” (points range: 0–3). The disagreement was addressed by consulting with the co-authors.
2.2.3. Data Consolidation
We completed the complicated data synthesis process using StataMP 17 software. The HRs and 95% CIs of OS and CSS were obtained and pooled for analysis. The heterogeneity among studies was evaluated by the I2 value. If the I2 value was greater than 50%, the heterogeneity was considered to be significant, and a random effects model was used. Egger’s and Begg’s tests were utilized to evaluate the publication bias of our study. Subgroup analyses were performed on regions as well. The significant cut-off values of the p value were 0.05 for pooled results and 0.10 for publication bias.
3. Results
3.1. Single-Center Case Series
3.1.1. Baseline Characteristics of Total and Grouped Patients
A total of 588 patients were included in a single-center case series, with a male-to-female ratio of 322:266 and a median age of 68 (IQR: 60–75) years. A total of 292 (49.9%) patients were in high stage (T3/T4), and 435 (74.6%) patients were in high grade. The final pathological reports showed that lymph node metastasis (LNM), lymphovascular invasion, tumor necrosis, papillary architecture, and positive surgical margins occurred in 59 (9.6%), 92 (15.7%), 45 (7.7%), 319 (54.9%), and 49 (8.4%) cases, respectively.
There were 57 patients in the octogenarian group, with a median age of 83 (IQR: 81–85). There were 531 patients in the younger group, with a median age of 67 (IQR: 59–73). The octogenarian group had a significant association with lower BMI (p = 0.042), lower albumin (p = 0.019), a higher ASA score (p < 0.001), and an earlier tumor stage (p = 0.023). No significant differences were found for other characteristics (all p > 0.05).
Detailed clinicopathologic and laboratory characteristics are given in Table 1.

Table 1.
The clinical and pathological characteristics of patients.
3.1.2. Survival Outcomes and Cox Regression
The median follow-up time was 59 months (IQR: 32–83). During this period, 220 (37.4%) patients died from UTUC. The Kaplan–Meier plots showed that, compared with the younger group, the patients in the octogenarian group showed no significant difference in CSS (p = 0.37) (Figure 2a). Similar results were also found in the subgroup analysis of tumor stage (p = 0.63 for pT < 3; p = 0.64 for pT ≥ 3) (Figure 2b,c).
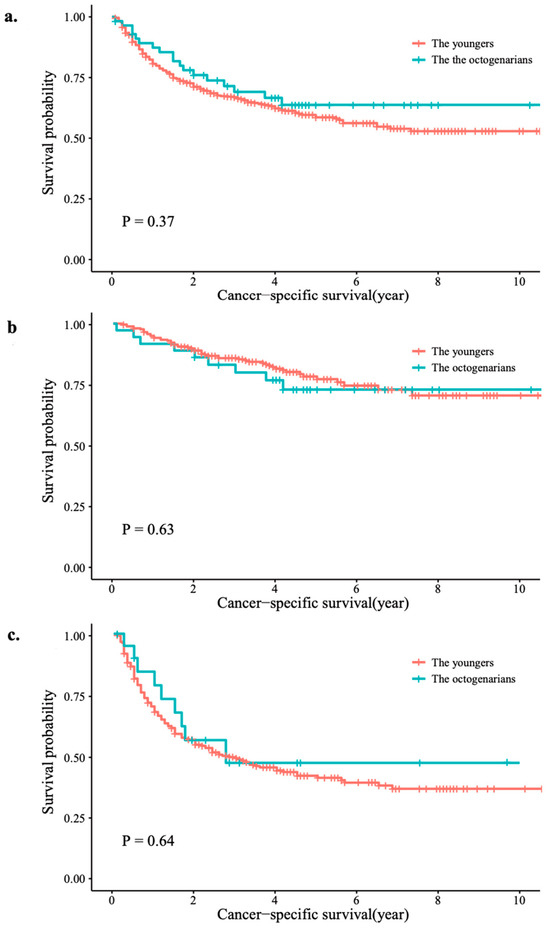
Figure 2.
Survival rates for the octogenarians and younger patients: (a) in the whole group; (b) tumor stage < T3; (c) tumor stage ≥ T3.
As shown in Table 2, tumors with advanced stage and grade, tumor size greater than 3, papillary architecture, LNM, positive surgical margin, ureter location, as well as patients with anemia, lower albumin, and without adjuvant systemic chemotherapy history were associated with poor CSS in the univariate Cox analysis (all p < 0.05). Then, to include as many clinical indicators as possible, we included all variables whose p values were less than 0.10 in the multivariate Cox regression, and the results indicated that tumor stage, size, site, grade, and lymph node status were independently associated with CSS (all p < 0.05). However, age was not a significant risk factor in univariate or multivariate analysis (HR, 0.80, 95% CI, 0.50, 1.30, p = 0.376; and HR, 1.08, 95% CI, 0.48, 2.40, p = 0.853, respectively).

Table 2.
Univariate and multivariate analyses of cancer-specific survival.
3.2. Systematic Review and Meta-Analysis
3.2.1. Systematic Review
The systematic search yielded a total of 2074 studies, of which 42 were found to be eligible after full-text evaluation (Figure 1b). The main characteristics of the included studies are summarized in Table 3. Among the 42 studies, the sample sizes ranged from 24 to 3544 patients, and a total of 22,490 UTUC patients after RNU were included. These studies were published between 2006 and 2023, and the patient recruitment periods ranged from 1987 to 2021. The median age ranged from 61.0 to 74.5 years, and the median follow-up time was between 18.0 and 82.8 months.

Table 3.
The characteristics of the included studies.
Interestingly, nearly all of the included studies (35/42, 83.3%) were Asian studies; three studies were global. It is noteworthy that only five studies (5/42, 11.9%) focused on the influence of the specific cut-off value of age on survival outcomes, while in others, age was just a baseline characteristic and happened to be a categorical variable. Although the age variable was noncontinuous in all the included studies, there was still a large difference among studies that emphasized dichotomous or multicategorical variables and their cut-off values.
3.2.2. Quality Assessment
NOS was used to evaluate the quality of the included studies, and the results are shown in Supplementary Table S2. High quality was determined to be high in 39 studies, moderate in 3 studies, and no study was marked as low quality.
3.2.3. Meta-Analysis
Considering the aim of the present study and the number limitation of the included studies with the same age cut-off value, we finally chose 70 as a relatively appropriate value, and the corresponding studies were subjected to meta-analysis.
Data on the association between the age of 70 and OS and CSS were available from 5 and 10, respectively. For OS, one study conducted by Kuo et al. was excluded because of the similar publication year and institution, and the same region. In our center, age greater than 70 was not a significantly adverse factor for OS for UTUC patients after RNU (HR 1.04, 95% CI 0.80–1.36), which was also used for pooled analysis. High heterogeneity (p < 0.001, I2 = 91.9%) was observed among the five studies. Therefore, the pooled effect value of OS (pooled HR 1.55, 95% CI 1.29–2.01) was calculated using a random-effects model (Figure 3a).
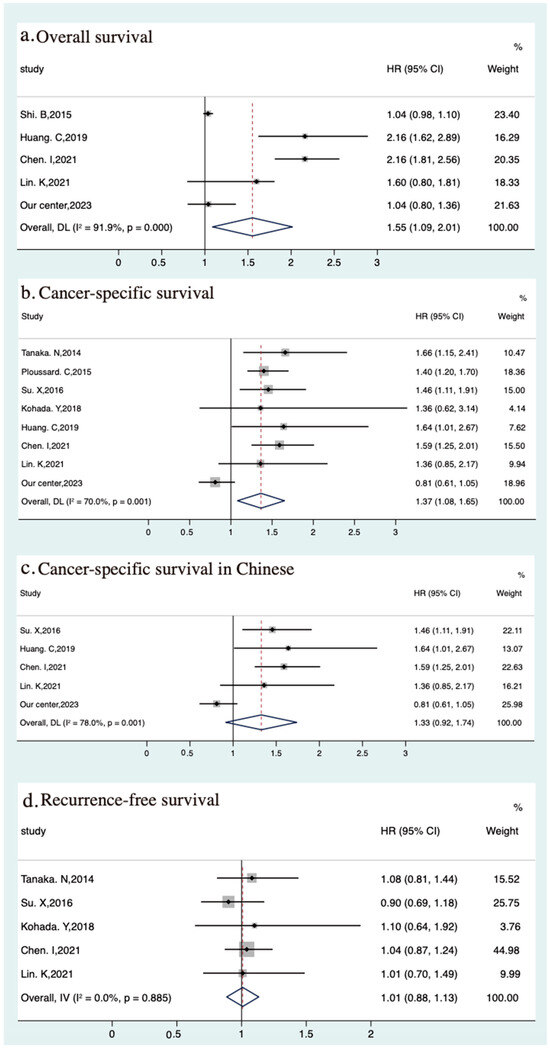
Figure 3.
Meta-analyses of oncological outcomes of the elders (>70) vs. youngers: (a) overall survival [24,38,44,45], (b) cancer-specific survival [20,21,31,36,38,44,45], (c) cancer-specific survival in Chinese [31,38,44,45], (d) recurrence-free survival [20,31,36,44,45].
Among the ten studies on CSS, two studies with similar regions and institutions and one study with information on cancer-specific mortality rather than CSS were excluded. Then, data from the remaining studies and data from our single-center case series (HR, 0.81, 95% CI 0.61–1.05) were used for meta-analysis, and the results indicated a significant association between age greater than 70 and poor CSS (pooled HR, 1.37, 95% CI 1.08–1.65). Significant heterogeneity was observed in the primary analysis (p = 0.001; I2 = 70.0%) (Figure 3b). Interestingly, to explore the influence of region on the association of age with CSS, we extracted five studies from China, and the pooled HR estimate for CSS was 1.33 (95% CI, 0.92–1.74), indicating no clear correlation between age and CSS; there was high heterogeneity among these studies (p = 0.001; I2 = 78.0%) (Figure 3c).
Due to the number restriction of the included studies, we utilized Egger regression to evaluate publication bias, and no obvious publication bias was observed in those studies (p = 0.193 for OS, p = 0.900 for CSS, p = 0.861 for sub-CSS).
4. Discussion
Population aging has posed a substantial challenge for the management of UTUC around the world. The increase in UTUC patients, characterized by localized lesions on first diagnosis, has been attributed to the strengthening of health awareness and widespread use of CT [1]. In addition, advances in minimally invasive therapies (especially in laparoscopic and robotic technology) have assuaged concerns about conventional surgery, offered advantages associated with less blood loss, decreased pain, and faster operation time, and created an opportunity to perform surgery on elderly patients [52,53]. However, the RNU for the aged UTUC patients is still controversial.
In the present study, we conducted a retrospective analysis to compare the survival outcomes (CSS) between octogenarians and younger patients and placed our findings in an international context by systematically reviewing the relevant literature. In our center, octogenarians with UTUC who underwent RNU showed a comparable outcome to younger UTUC patients. Further review of previous studies and meta-analyses indicated that advanced age (>70 years) tended to be related to poor OS and CSS. However, there was no significant association between advanced age and CSS in China.
Our results are in concordance with several single- and multi-institutional studies in which a negative association between the advanced age and prognosis of UTUC patients after RNU has been found [47,54]. In contrast, several previous studies have shown that age was an independent predictor of long-term survival for UTUC patients, and advanced age was found to be associated with worse outcomes [55,56]. However, few studies have been conducted on the topic of patient age, and our systematic review only found five studies on this topic. In 2009, a multicenter study of 1453 patients after RNU found that being older at the time of RNU was associated with inferior CSS, which was also observed by Stanley et al. in 2011 even after adjusting for tumor stage, grade, and treatment [12,56]. In contrast, the latest publication, studied by Koterazawa et al., retrospectively included 283 UTUC patients after laparoscopic RNU and demonstrated that no significant difference in the incidence of postoperative complications and 5-year OS, CSS, and RFS was observed between octogenarians and younger patients [51].
There might be several sources of the between-study heterogeneity observed herein. First, the majority of the previous studies only investigated chronological age, and few studies have considered anesthetic risk, biological age, comorbidities, and other potential factors. In 2018, biological age, evaluated by the categories of hemoglobin and white blood cells, was reported to show a stronger relationship with outcomes than chronological age in UTUC patients, especially elderly patients [57]. However, clinically, less aggressive, and nonstandard treatment regimens were recommended to patients based on their advancing age, and a patient’s chronological age alone may prevent them from receiving the best care for their disease. According to the American Society of Clinical Oncology guidelines, geriatric assessment (GA) should be used as intended to guide treatment decisions for elderly patients (≥65 years old) with cancer to identify vulnerabilities [58]. A recent study investigated the effects of age, ASA grading, and the Charlson Comorbidity Index (CCI) on UTUC outcomes and suggested that RNU should be a promising choice even among elderly patients who are eligible after GA [59]. However, Phaibulvatanapong et al. reported that CCI might not be suitable for assessing the comorbidity of cancer patients because cancer is one of the grading factors, which could result in patients with metastatic disease receiving an unjustified high score [60]. More future studies are needed to further explore and evaluate this in clinical practice.
In addition, the basic characteristics, such as race and region, may also cause selection bias. For UTUC, men in Europe and America typically have a 1.5–2.5 times higher risk than women, while in Asia, women have a 1.3 times higher risk than males [61,62,63]. Furthermore, being male was found to be associated with adverse outcomes in China rather than America, and the black race was found to be relevant to adverse outcomes in America [55,64]. This may partly explain the result of the pooled analysis that advanced age was significantly related to poor CSS, but the relationship disappeared when the region was restricted to China. However, in the above analysis, we failed to take gender and race into consideration. Sex in our center did not appear to be an independent predictor of CSS (HR 1.07; 95% CI 0.82, 1.40; p = 0.612), which was in line with most earlier studies. Interestingly, Kobayashi et al. evaluated the impact of gender-adjusted age on prognosis in upper tract urothelial carcinoma patients following RNU and demonstrated that older age was significantly associated with CSS independently of pathological features in male patients but not in female patients [28]. Moreover, in 2013, Liu et al. reviewed the data from 285 men and 136 women treated with RNU for UTUC, and the results showed that the impact of gender on UTUC outcomes is age-specific [65]. Females aged ≥59 years had worse outcomes than their male counterparts, while women <42 years and 42–58 years had better outcomes than men. Sex hormones and their receptors were thought to be the cause of gender differences in outcomes. Therefore, further research is needed to confirm whether sex- or age-specific sex has an effect on UTUC outcomes and to elucidate the molecular mechanism.
According to the EAU guidelines, the curative therapy for UTUC remains RNU, while nephron-sparing surgery or several novel technologies, such as ablation, are a choice for low-risk UTUC and patients with solitary kidney or severe renal impairment [2]. Older patients should not be denied potentially curative surgery based solely on their age; instead, we should make every effort to assess the overall condition of older patients. Recently, other studies have also demonstrated that indicators that reflect preoperative inflammation or nutritional status, such as the neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, and platelet-to-lymphocyte ratio, are associated with worse outcomes in patients with carcinoma [66,67]. Therefore, an authoritative evaluation system or nomogram aimed at identifying a special population of elderly patients who can benefit from RNU is urgently needed to guide clinical practice.
Notably, the strength of our study was that we provided a comprehensive reference about the relationship between the chronological age of UTUC patients at the time of RNU and survival outcomes and suggested that advanced age may not be an absolute contraindication for RNU by combining our single-center findings with a systematic review as well as a meta-analysis. Nonetheless, our study had some limitations. For our cases, the small size of octogenarians and the absence of specific comorbidities, due to the retrospective setting, are the most notable. Moreover, studies that focused on the influence of age were scarce, and age tended to be a continuous variable in most studies. The cut-off value for age in the pooled analysis was 70, which was limited by the number of included studies. However, it is relatively common for patients with newly diagnosed UTUC to be older than 70 years, whereas we were interested in the age of 80 years, which limits the external application of the conclusions of our study. Admittedly, in this single-center case series, we only chose the ASA score to reflect the general condition of patients from the perspective of tolerance to anesthesia. However, some novel indicators, which were determined by preoperative status and previously reported to influence the prognosis of UTUC patients, were not included in our analysis. These indicators included body composition based on computed tomography scans (e.g., iliopsoas muscle area, visceral fat density, intermuscular fat area, muscle attenuation, etc.), preoperative nutrition and inflammatory status (e.g., Naples prognostic score, controlling nutritional status score, prognostic nutritional index, etc.), and other indexes (e.g., CCI, modified frailty index, etc.). We are conducting a prospective, multicenter study with improved baseline balance and more complete basal characteristics to address these limitations.
5. Conclusions
Our single-center case series and the systematic review indicated that advanced age may not be an absolute contraindication for RNU in UTUC patients. RNU can be a safe and effective choice for UTUC patients of advanced age after a comprehensive presurgical evaluation.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12237273/s1. Table S1: The PRISMA checklist of the present study. Table S2: Newcastle-Ottawa Scale for assessing the quality of included studies. References [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,28,47,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] are cited in the Supplementary Materials.
Author Contributions
Conception and design: J.Y., Q.W. (Qiyou Wu), Q.W. (Qiang Wei) and Y.B. Administrative support: Y.B. and Q.W. (Qiang Wei). Provision of study materials or patients: X.L. and J.Y. Collection and assembly of data: X.L., L.Z. and J.Y. Data analysis and interpretation: Q.W. (Qiyou Wu) and J.Y. Manuscript writing: All authors. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (Grant number: 81500522) and the Science and Technology Department of Sichuan Province (Grant numbers: 2020YFS0090 and 2020YFS0046).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (2021–1209, date of approval 12 October 2021.).
Informed Consent Statement
The informed consent was allowed to be waived because of the retrospective nature, anonymous patients, and data.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, upon reasonable request.
Acknowledgments
This manuscript has been read and approved by all authors, and each author believes that the manuscript represents an honest work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Rouprêt, M.; Seisen, T.; Birtle, A.J.; Capoun, O.; Compérat, E.M.; Dominguez-Escrig, J.L.; Andersson, I.G.; Liedberg, F.; Mariappan, P.; Mostafid, A.H.; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2023 Update. Eur. Urol. 2023, 84, 49–64. [Google Scholar] [CrossRef]
- Olotu, C. Anesthesia for the elderly: A narrative review. Minerva Anestesiol. 2021, 87, 1128–1138. [Google Scholar] [CrossRef]
- Wang, Y.-Y.; Yue, J.-R.; Xie, D.-M.; Carter, P.; Li, Q.-L.; Gartaganis, S.L.; Chen, J.; Inouye, S.K. Effect of the Tailored, Family-Involved Hospital Elder Life Program on Postoperative Delirium and Function in Older Adults. JAMA Intern. Med. 2020, 180, 17–25. [Google Scholar] [CrossRef]
- Aceto, P.; Incalzi, R.A.; Bettelli, G.; Carron, M.; Chiumiento, F.; Corcione, A.; Crucitti, A.; Maggi, S.; Montorsi, M.; Pace, M.C.; et al. Perioperative Management of Elderly patients (PriME): Recommendations from an Italian intersociety consensus. Aging Clin. Exp. Res. 2020, 32, 1647–1673. [Google Scholar] [CrossRef]
- Kim, J.-K.; Hwang, K.-T.; Soh, H.-S.; Shon, O.-J.; Park, K.-C. Comparison of tibial plateau fracture surgical outcomes between young and elderly patients: Are outcomes really poorer in the elderly? Arch. Orthop. Trauma Surg. 2022, 142, 2419–2427. [Google Scholar] [CrossRef]
- Menna, G.; Rapisarda, A.; Izzo, A.; D’ercole, M.; D’alessandris, Q.G.; Olivi, A.; Montano, N. Surgical and Clinical Outcomes of Microvascular Decompression: A Comparative Study between Young and Elderly Patients. Brain Sci. 2022, 12, 1216. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D. Evaluations of the uptake and impact of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Statement and extensions: A scoping review. Syst. Rev. 2017, 6, 263. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef]
- Ataus, S.; Onal, B.; Tunc, B.; Erozenci, A.; Cekmen, A.; Kural, A.R.; Oner, A. Factors Affecting the Survival of Patients Treated by Standard Nephroureterectomy for Transitional Cell Carcinoma of the Upper Urinary Tract. Int. Urol. Nephrol. 2006, 38, 9–13. [Google Scholar] [CrossRef]
- Li, C.-C.; Chang, T.-H.; Wu, W.-J.; Ke, H.-L.; Huang, S.-P.; Tsai, P.-C.; Chang, S.-J.; Shen, J.-T.; Chou, Y.-H.; Huang, C.-H. Significant Predictive Factors for Prognosis of Primary Upper Urinary Tract Cancer after Radical Nephroureterectomy in Taiwanese Patients. Eur. Urol. 2008, 54, 1127–1135. [Google Scholar] [CrossRef]
- Shariat, S.F.; Godoy, G.; Lotan, Y.; Droller, M.; Karakiewicz, P.I.; Raman, J.D.; Isbarn, H.; Weizer, A.; Remzi, M.; Roscigno, M.; et al. Advanced patient age is associated with inferior cancer-specific survival after radical nephroureterectomy. BJU Int. 2010, 105, 1672–1677. [Google Scholar] [CrossRef]
- Chromecki, T.F.; Ehdaie, B.; Novara, G.; Pummer, K.; Zigeuner, R.; Seitz, C.; Pycha, A.; Lee, R.K.; Cha, E.K.; Karakiewicz, P.I.; et al. Chronological age is not an independent predictor of clinical outcomes after radical nephroureterectomy. World J. Urol. 2011, 29, 473–480. [Google Scholar] [CrossRef]
- Milojevic, B.; Djokic, M.; Sipetic-Grujicic, S.; Milenkovic-Petronic, D.; Vuksanovic, A.; Bumbasirevic, U.; Vukovic, I.; Dragicevic, D.; Tulic, C. Upper urinary tract transitional cell carcinoma: Location is not correlated with prognosis. BJU Int. 2012, 109, 1037–1042. [Google Scholar] [CrossRef]
- Metcalfe, M.; Kassouf, W.; Rendon, R.; Bell, D.; Izawa, J.; Chin, J.; Kapoor, A.; Matsumoto, E.; Lattouf, J.-B.; Saad, F.; et al. Regional differences in practice patterns and associated outcomes for upper tract urothelial carcinoma in Canada. Can. Urol. Assoc. J. 2012, 6, 455–462. [Google Scholar] [CrossRef][Green Version]
- Lim, S.K.; Shin, T.-Y.; Kim, K.H.; Chung, B.H.; Hong, S.J.; Choi, Y.D.; Rha, K.H. Intermediate-Term Outcomes of Robot-Assisted Laparoscopic Nephroureterectomy in Upper Urinary Tract Urothelial Carcinoma. Clin. Genitourin. Cancer 2013, 11, 515–521. [Google Scholar] [CrossRef]
- Li, W.-M.; Wu, W.-J.; Li, C.-C.; Ke, H.-L.; Wei, Y.-C.; Yeh, H.-C.; Chou, Y.-H.; Huang, C.-H. The effect of tumor location on prognosis in patients with primary ureteral urothelial carcinoma. Urol. Oncol. Semin. Orig. Investig. 2013, 31, 1670–1675. [Google Scholar] [CrossRef]
- Obata, J.; Kikuchi, E.; Tanaka, N.; Matsumoto, K.; Hayakawa, N.; Ide, H.; Miyajima, A.; Nakagawa, K.; Oya, M. C-reactive protein: A biomarker of survival in patients with localized upper tract urothelial carcinoma treated with radical nephroureterectomy. Urol. Oncol. Semin. Orig. Investig. 2013, 31, 1725–1730. [Google Scholar] [CrossRef]
- Luo, H.-L.; Chen, Y.-T.; Chuang, Y.-C.; Cheng, Y.-T.; Lee, W.-C.; Kang, C.-H.; Chiang, P.-H. Subclassification of upper urinary tract urothelial carcinoma by the neutrophil-to-lymphocyte ratio (NLR) improves prediction of oncological outcome. BJU Int. 2014, 113, E144–E149. [Google Scholar] [CrossRef]
- Tanaka, N.; Kikuchi, E.; Kanao, K.; Matsumoto, K.; Shirotake, S.; Miyazaki, Y.; Kobayashi, H.; Kaneko, G.; Hagiwara, M.; Ide, H.; et al. A Multi-Institutional Validation of the Prognostic Value of the Neutrophil-to-Lymphocyte Ratio for Upper Tract Urothelial Carcinoma Treated with Radical Nephroureterectomy. Ann. Surg. Oncol. 2014, 21, 4041–4048. [Google Scholar] [CrossRef]
- Ploussard, G.; Xylinas, E.; Lotan, Y.; Novara, G.; Margulis, V.; Rouprêt, M.; Matsumoto, K.; Karakiewicz, P.I.; Montorsi, F.; Remzi, M.; et al. Conditional Survival after Radical Nephroureterectomy for Upper Tract Carcinoma. Eur. Urol. 2015, 67, 803–812. [Google Scholar] [CrossRef]
- Lee, H.-Y.; Li, C.-C.; Huang, C.-N.; Ke, H.-L.; Li, W.-M.; Liang, P.-I.; Yang, S.-F.; Tu, H.-P.; Wu, W.-J.; Yeh, H.-C. Prognostic Significance of Lymphovascular Invasion in Upper Urinary Tract Urothelial Carcinoma is Influenced by Tumor Location. Ann. Surg. Oncol. 2015, 22, 1392–1400. [Google Scholar] [CrossRef]
- Morizane, S.; Yumioka, T.; Yamaguchi, N.; Masago, T.; Honda, M.; Sejima, T.; Takenaka, A. Risk stratification model, including preoperative serum C-reactive protein and estimated glomerular filtration rate levels, in patients with upper urinary tract urothelial carcinoma undergoing radical nephroureterectomy. Int. Urol. Nephrol. 2015, 47, 1335–1341. [Google Scholar] [CrossRef]
- Shi, B.; Su, B.; Fang, D.; Tang, Y.; Xiong, G.; Guo, Z.; He, Q.; Yang, X.; Zhao, W.; Guo, Y.; et al. High expression of KPNA2 defines poor prognosis in patients with upper tract urothelial carcinoma treated with radical nephroureterectomy. BMC Cancer 2015, 15, 380. [Google Scholar] [CrossRef]
- Tanaka, N.; Kikuchi, E.; Kanao, K.; Matsumoto, K.; Shirotake, S.; Miyazaki, Y.; Kobayashi, H.; Kaneko, G.; Hagiwara, M.; Ide, H.; et al. Impact of Combined Use of Blood-based Inflammatory Markers on Patients with Upper Tract Urothelial Carcinoma Following Radical Nephroureterectomy: Proposal of a Cumulative Marker Score as a Novel Predictive Tool for Prognosis. Eur. Urol. Focus 2015, 1, 54–63. [Google Scholar] [CrossRef]
- Zhang, X.-K.; Zhang, Z.-L.; Yang, P.; Cai, M.-Y.; Hu, W.-M.; Yun, J.-P.; Zhou, F.-J.; Qian, C.-N.; Cao, Y. Tumor necrosis predicts poor clinical outcomes in patients with node-negative upper urinary tract urothelial carcinoma. Jpn. J. Clin. Oncol. 2015, 45, 1069–1075. [Google Scholar] [CrossRef][Green Version]
- Cheng, Y.-C.; Huang, C.-N.; Wu, W.-J.; Li, C.-C.; Ke, H.-L.; Li, W.-M.; Tu, H.-P.; Li, C.-F.; Chang, L.-L.; Yeh, H.-C. The Prognostic Significance of Inflammation-Associated Blood Cell Markers in Patients with Upper Tract Urothelial Carcinoma. Ann. Surg. Oncol. 2016, 23, 343–351. [Google Scholar] [CrossRef]
- Kobayashi, H.; Kikuchi, E.; Tanaka, N.; Shirotake, S.; Miyazaki, Y.; Ide, H.; Obata, J.; Hoshino, K.; Matsumoto, K.; Kaneko, G.; et al. Patient age was an independent predictor of cancer-specific survival in male patients with upper tract urothelial carcinoma treated by radical nephroureterectomy. Jpn. J. Clin. Oncol. 2016, 46, 554–559. [Google Scholar] [CrossRef][Green Version]
- Liang, C.; Chi, R.; Huang, L.; Wang, J.; Liu, H.; Xu, D.; Qian, S.; Qian, X.; Qi, J. Upper Tract Urothelial Carcinomas Accompanied by Previous or Synchronous Nonmuscle-Invasive Bladder Cancer and Preoperative Hydronephrosis Might Have Worse Oncologic Outcomes After Radical Nephroureterectomy. Clin. Genitourin. Cancer 2016, 14, e469–e477. [Google Scholar] [CrossRef]
- Shibing, Y.; Liangren, L.; Qiang, W.; Hong, L.; Turun, S.; Junhao, L.; Lu, Y.; Zhengyong, Y.; Yonghao, J.; Guangqing, F.; et al. Impact of tumour size on prognosis of upper urinary tract urothelial carcinoma after radical nephroureterectomy: A multi-institutional analysis of 795 cases. BJU Int. 2016, 118, 902–910. [Google Scholar] [CrossRef]
- Su, X.; Fang, D.; Li, X.; Xiong, G.; Zhang, L.; Hao, H.; Gong, Y.; Zhang, Z.; Zhou, L. The Influence of Tumor Size on Oncologic Outcomes for Patients with Upper Tract Urothelial Carcinoma after Radical Nephroureterectomy. BioMed Res. Int. 2016, 2016, 4368943. [Google Scholar] [CrossRef]
- Cao, Z.-P.; Guan, B.; Zhao, G.-Z.; Fang, D.; Xiong, G.-Y.; Li, X.-S.; Zhou, L.-Q. Validation of the Pretreatment Neutrophil-to-Lymphocyte Ratio as a Prognostic Factor in a Large Cohort of Chinese Patients with Upper Tract Urothelial Carcinoma. Chin. Med. J. 2017, 130, 2063–2068. [Google Scholar] [CrossRef]
- Daimon, T.; Kosaka, T.; Kikuchi, E.; Mikami, S.; Miyazaki, Y.; Hashimoto, A.; Hashimoto, S.; Mizuno, R.; Miyajima, A.; Okada, Y.; et al. Prognostic significance of erythrocyte protein band 4.1-like5 expression in upper urinary tract urothelial carcinoma. Urol. Oncol. Semin. Orig. Investig. 2017, 35, 543.e17–543.e24. [Google Scholar] [CrossRef]
- Huang, J.; Yuan, Y.; Wang, Y.; Zhang, J.; Kong, W.; Chen, H.; Chen, Y.; Huang, Y. Prognostic value of preoperative plasma fibrinogen level and platelet-to-lymphocyte ratio (F-PLR) in patients with localized upper tract urothelial carcinoma. Oncotarget 2017, 8, 36761–36771. [Google Scholar] [CrossRef]
- Kim, J.K.; Moon, K.C.; Jeong, C.W.; Kwak, C.; Kim, H.H.; Ku, J.H. Variant histology as a significant predictor of survival after radical nephroureterectomy in patients with upper urinary tract urothelial carcinoma. Urol. Oncol. Semin. Orig. Investig. 2017, 35, 458.e9–458.e15. [Google Scholar] [CrossRef]
- Kohada, Y.; Hayashi, T.; Goto, K.; Kobatake, K.; Abdi, H.; Honda, Y.; Sentani, K.; Inoue, S.; Teishima, J.; Awai, K.; et al. Preoperative risk classification using neutrophil–lymphocyte ratio and hydronephrosis for upper tract urothelial carcinoma. Jpn. J. Clin. Oncol. 2018, 48, 841–850. [Google Scholar] [CrossRef]
- Zeng, S.; Dai, L.; Yang, J.; Gao, X.; Yu, X.; Ren, Q.; Wang, K.; Xu, J.; Yang, Z.; Yang, B.; et al. Development and external validation of a nomogram predicting prognosis of upper tract urothelial carcinoma after radical nephroureterectomy. Urol. Oncol. Semin. Orig. Investig. 2019, 37, 290.e17–290.e24. [Google Scholar] [CrossRef]
- Huang, C.-C.; Su, Y.-L.; Luo, H.-L.; Chen, Y.-T.; Sio, T.T.; Hsu, H.-C.; Lai, C.-H. Gender Is a Significant Prognostic Factor for Upper Tract Urothelial Carcinoma: A Large Hospital-Based Cancer Registry Study in an Endemic Area. Front. Oncol. 2019, 9, 157. [Google Scholar] [CrossRef]
- Chung, H.S.; Hwang, E.C.; Kim, M.S.; Yu, S.H.; Jung, S.I.; Kang, T.W.; Choi, C.; Choi, S.H.; Kwon, T.G.; Noh, J.H.; et al. Effects of Variant Histology on the Oncologic Outcomes of Patients with Upper Urinary Tract Carcinoma after Radical Nephroureterectomy: A Propensity Score–Matched Analysis. Clin. Genitourin. Cancer 2019, 17, e394–e407. [Google Scholar] [CrossRef]
- Kuroda, K.; Asakuma, J.; Horiguchi, A.; Kawaguchi, M.; Shinchi, M.; Masunaga, A.; Tasaki, S.; Sato, A.; Ito, K. Chronic kidney disease and positive surgical margins as prognosticators for upper urinary tract urothelial carcinoma patients undergoing radical nephroureterectomy. Mol. Clin. Oncol. 2019, 10, 547–554. [Google Scholar] [CrossRef]
- Chen, X.; Ji, H.; Wang, J.; Zhao, G.; Zheng, B.; Niu, Z.; He, W. Prognostic Value of the Preoperative Plasma D-Dimer Levels in Patients with Upper Tract Urothelial Carcinoma in a Retrospective Cohort Study. OncoTargets Ther. 2020, 13, 5047–5055. [Google Scholar] [CrossRef]
- Liu, W.; Wang, Z.; Liu, S.; Yao, Y.; Liu, Y.; Zhang, G. Preoperative positive voided urine cytology predicts poor clinical outcomes in patients with upper tract urothelial carcinoma undergoing nephroureterectomy. BMC Cancer 2020, 20, 1113. [Google Scholar] [CrossRef]
- Azawi, N.H.; Næraa, S.H.; Subhi, Y.; Vásquez, J.L.; Norus, T.; Dahl, C.; Thind, P.; Jensen, J.B. Oncological outcomes of radical nephroureterectomy for upper urinary tract urothelial neoplasia in Denmark. Scand. J. Urol. 2020, 54, 58–64. [Google Scholar] [CrossRef]
- Chen, I.-H.A.; Chang, C.-H.; Huang, C.-P.; Wu, W.-J.; Li, C.-C.; Chen, C.-H.; Huang, C.-Y.; Lo, C.-W.; Yu, C.-C.; Tsai, C.-Y.; et al. Factors Predicting Oncological Outcomes of Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma in Taiwan. Front. Oncol. 2021, 11, 766576. [Google Scholar] [CrossRef]
- Lin, K.-C.; Jan, H.-C.; Hu, C.-Y.; Ou, Y.-C.; Kao, Y.-L.; Yang, W.-H.; Ou, C.-H. Tumor Necrosis with Adjunction of Preoperative Monocyte-to-Lymphocyte Ratio as a New Risk Stratification Marker Can Independently Predict Poor Outcomes in Upper Tract Urothelial Carcinoma. J. Clin. Med. 2021, 10, 2983. [Google Scholar] [CrossRef]
- Milojevic, B.; Bumbasirevic, U.; Santric, V.; Kajmakovic, B.; Dragicevic, D.; Radisavcevic, D.; Sretenovic, M.; Grujicic, S.S. Prognostic significance of tumor multifocality on outcomes in patients with upper tract urothelial carcinoma after radical nephroureterectomy: A cohort study. Curr. Probl. Cancer 2021, 45, 100747. [Google Scholar] [CrossRef]
- Yamada, Y.; Ikeda, M.; Hirayama, T.; Murakami, Y.; Koguchi, D.; Matsuda, D.; Okuno, N.; Taoka, Y.; Utsunomiya, T.; Irie, A.; et al. Noninferior oncological outcomes in adults aged 80 years or older compared with younger patients who underwent radical nephroureterectomy for upper tract urothelial carcinoma. Asia-Pac. J. Clin. Oncol. 2022, 19, 305–311. [Google Scholar] [CrossRef]
- Kuo, C.-C.; Chen, G.-H.; Chang, C.-H.; Huang, C.-Y.; Chen, C.-H.; Li, C.-C.; Wu, W.-J.; Yu, C.-C.; Lo, C.-W.; Chen, Y.-T.; et al. Surgical outcome predictor analysis following hand-assisted or pure laparoscopic transperitoneal nephroureterectomy using the Taiwan upper urinary tract urothelial carcinoma database. Front. Surg. 2022, 9, 934355. [Google Scholar] [CrossRef]
- Gao, J.; Liu, J.; Liu, J.; Lin, S.; Ding, D. Survival and risk factors among upper tract urothelial carcinoma patients after radical nephroureterectomy in Northeast China. Front. Oncol. 2022, 12, 1012292. [Google Scholar] [CrossRef]
- Ke, H.-L.; Li, C.-C.; Lee, H.-Y.; Tu, H.-P.; Wei, Y.-C.; Yeh, H.-C.; Wu, W.-J.; Li, W.-M. Prognostic Value of Comorbidity for Patients with Upper Tract Urothelial Carcinoma after Radical Nephroureterectomy. Cancers 2022, 14, 1466. [Google Scholar] [CrossRef]
- Koterazawa, S.; Kanno, T.; Kobori, G.; Ito, K.; Nakagawa, H.; Takahashi, T.; Takaoka, N.; Somiya, S.; Nagahama, K.; Ito, M.; et al. Clinical outcomes following laparoscopic radical nephroureterectomy in octogenarians. Int. J. Clin. Oncol. 2023, 28, 155–162. [Google Scholar] [CrossRef]
- Falagario, U.; Veccia, A.; Weprin, S.; Albuquerque, E.V.; Nahas, W.C.; Carrieri, G.; Pansadoro, V.; Hampton, L.J.; Porpiglia, F.; Autorino, R. Robotic-assisted surgery for the treatment of urologic cancers: Recent advances. Expert Rev. Med. Devices 2020, 17, 579–590. [Google Scholar] [CrossRef]
- Fan, G.; Li, K.; Wang, Y.; Zhao, Y.; Wang, Z. Efficacy and safety of robot-assisted laparoscopic, laparoscopic and open surgery in ureteral reimplantation: A network meta-analysis and systematic review. Updat. Surg. 2022, 74, 1491–1499. [Google Scholar] [CrossRef]
- Novara, G.; De Marco, V.; Gottardo, F.; Dalpiaz, O.; Bouygues, V.; Galfano, A.; Martignoni, G.; Patard, J.J.; Artibani, W.; Ficarra, V. Independent predictors of cancer-specific survival in transitional cell carcinoma of the upper urinary tract. Cancer 2007, 110, 1715–1722. [Google Scholar] [CrossRef]
- Zhou, Z.; Shi, H.J.; Jin, L.; Liu, X.; Zhai, T.S.; Zhang, J.X.; Ye, L. Prognostic significance of age, sex, race, and socioeconomic status in patients with stage III–IV upper tract urothelial carcinoma. Actas Urol. Esp. 2022, 46, 413–422. [Google Scholar] [CrossRef]
- Yap, S.A.; Schupp, C.W.; Chamie, K.; Evans, C.P.; Koppie, T.M. Effect of Age on Transitional Cell Carcinoma of the Upper Urinary Tract: Presentation, Treatment, and Outcomes. Urology 2011, 78, 87–92. [Google Scholar] [CrossRef]
- Inamoto, T.; Matsuyama, H.; Ibuki, N.; Komura, K.; Fujimoto, K.; Shiina, H.; Sakano, S.; Nagao, K.; Miyake, M.; Yasumoto, H.; et al. Risk stratification by means of biological age-related factors better predicts cancer-specific survival than chronological age in patients with upper tract urothelial carcinoma: A multi-institutional database study. Ther. Adv. Urol. 2018, 10, 403–410. [Google Scholar] [CrossRef]
- Schnipper, L.E.; Davidson, N.E.; Wollins, D.S.; Tyne, C.; Blayney, D.W.; Blum, D.; Dicker, A.P.; Ganz, P.A.; Hoverman, J.R.; Langdon, R.; et al. American Society of Clinical Oncology Statement: A Conceptual Framework to Assess the Value of Cancer Treatment Options. J. Clin. Oncol. 2015, 33, 2563–2577. [Google Scholar] [CrossRef]
- Teoh, J.Y.-C.; Ng, C.-F.; Eto, M.; Chiruvella, M.; Capitanio, U.; Esen, T.; Zeng, G.; Lechevallier, E.; Andonian, S.; de la Rosette, J. Radical nephroureterectomy for UTUC conferred survival benefits irrespective of age and comorbidities. World J. Urol. 2022, 40, 2657–2665. [Google Scholar] [CrossRef]
- Phaibulvatanapong, E.; Srinonprasert, V.; Ithimakin, S. Risk Factors for Chemotherapy-Related Toxicity and Adverse Events in Elderly Thai Cancer Patients: A Prospective Study. Oncology 2018, 94, 149–160. [Google Scholar] [CrossRef]
- Audenet, F.; Colin, P.; Yates, D.R.; Ouzzane, A.; Pignot, G.; Long, J.; Soulie, M.; Phé, V.; Bensadoun, H.; Guy, L.; et al. A proportion of hereditary upper urinary tract urothelial carcinomas are misclassified as sporadic according to a multi-institutional database analysis: Proposal of patient-specific risk identification tool. BJU Int. 2012, 110 Pt B, E583–E589. [Google Scholar] [CrossRef]
- Fang, D.; Xiong, G.; Li, X.; Kang, Y.; Zhang, L.; Zhao, G.; Chen, X.; Yao, L.; Zhang, X.; Yu, W.; et al. Incidence, characteristics, treatment strategies, and oncologic outcomes of synchronous bilateral upper tract urothelial carcinoma in the Chinese population. Urol. Oncol. Semin. Orig. Investig. 2015, 33, 66.e1–66.e11. [Google Scholar] [CrossRef]
- Luo, H.L.; Kang, C.H.; Chen, Y.T.; Chuang, Y.C.; Lee, W.C.; Cheng, Y.T.; Chiang, P.H. Diagnostic Ureteroscopy Independently Correlates with Intravesical Recurrence after Nephroureterectomy for Upper Urinary Tract Urothelial Carcinoma. Ann. Surg. Oncol. 2013, 20, 3121–3126. [Google Scholar] [CrossRef]
- Singla, N.; Fang, D.; Su, X.; Bao, Z.; Cao, Z.; Jafri, S.M.; Xiong, G.; Zhang, L.; Hutchinson, R.; Sagalowsky, A.; et al. A Multi-Institutional Comparison of Clinicopathological Characteristics and Oncologic Outcomes of Upper Tract Urothelial Carcinoma in China and the United States. J. Urol. 2017, 197, 1208–1213. [Google Scholar] [CrossRef]
- Liu, J.-Y.; Li, Y.-H.; Zhang, Z.-L.; Ye, Y.-L.; Liu, Z.-W.; Yao, K.; Dong, P.; Guo, S.-J.; Jiang, L.-J.; Zhong, M.-Z.; et al. Age-specific effect of gender on upper tract urothelial carcinoma outcomes. Med. Oncol. 2013, 30, 640. [Google Scholar] [CrossRef]
- Liu, J.; Wu, P.; Lai, S.; Song, X.; Fu, C.; Wang, X.; Liu, S.; Hou, H.; Liu, M.; Wang, J. Preoperative Monocyte-to-lymphocyte Ratio Predicts for Intravesical Recurrence in Patients with Urothelial Carcinoma of the Upper Urinary Tract after Radical Nephroureterectomy without a History of Bladder Cancer. Clin. Genitourin. Cancer 2021, 19, e156–e165. [Google Scholar] [CrossRef]
- Li, B.; Zhou, P.; Liu, Y.; Wei, H.; Yang, X.; Chen, T.; Xiao, J. Platelet-to-lymphocyte ratio in advanced Cancer: Review and meta-analysis. Clin. Chim. Acta 2018, 483, 48–56. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).