Abstract
Background: We aimed to study the presentation and in-hospital outcomes of obese patients hospitalized for cardiovascular diseases (CVDs) in a Middle Eastern country. Methods: This retrospective study included patients admitted to the Heart Hospital between 2015 and 2020. Patients were divided according to their body mass index (BMI): Group I (BMI 18.5–24.9), Group II (BMI 25–29.9), and Group III (BMI ≥ 30), by applying one-way ANOVAs and chi-square tests. The obese group (BMI ≥ 30) was graded and compared (Grade I (BMI 30–34.9), Grade II (BMI 35–39.9), and Grade III (BMI ≥ 40)). Results: There were 7284 patients admitted with CVDs (Group I (29%), Group II (37%), and Group III (34%)). The mean age was higher in Group III than Groups I and II (p < 0.001). Male sex was predominant in all groups except for morbid obesity (Grade III), in which females predominated. Diabetes mellitus (DM), hypertension, and dyslipidemia were more common in Group III. Chest pain was more common in Group II, while shortness of breath was more evident in Group III (p < 0.001). Group II had more ST-elevation myocardial infarction (STEMI), followed by Group I (p < 0.001). Atrial fibrillation (AF) was observed more frequently in Group III (p < 0.001). Congestive heart failure (CHF) was common in Group III (19%) (p < 0.001). In the subanalysis, (Grade I (62%), Grade II (22.5%), and Grade III (15.5%)), Grade I had more STEMI, whereas AF and CHF were higher in Grade III (p < 0.001). Percutaneous Coronary Intervention was performed less frequently in Grade III (p < 0.001). In-hospital mortality was higher in Grade III (17.1%), followed by Grades II (11.2%) and I (9.3%) (p < 0.001). Conclusions: In this study, one third of the hospitalized CVS patients were obese. AF and CHF with preserved EF were the most common cardiovascular presentations in obese patients. In patients with CVDs, obesity was associated with higher rates of comorbidities and in-hospital mortality. However, obesity measured by BMI alone was not an independent predictor of mortality in obese cardiac patients.
1. Introduction
Cardiovascular disease (CVD) is acknowledged as the primary global cause of mortality, responsible for 32% of all deaths or a total of 20.5 million deaths in 2021 [1]. Coronary artery disease (CAD) is influenced by obesity, an independent risk factor [2]. The prevalence of obesity continues to escalate, as evidenced by data from the National Health and Nutrition Examination Surveys (NHANES), indicating a rise in obesity prevalence among adults in the USA from 30.5% to 42.4%, with severe obesity nearly doubling from 4.7% to 9.2% [3]. In the Western world, the prevalence of obesity is 36.5% [4], while the Middle East reports prevalence rates of overweight and obese individuals ranging from 23.5% to 62.1% and 14.5% to 40.6%, respectively [5].
Recent statistics reveal that 43% and 24% of coronary revascularization procedures were performed in overweight and obese patients, respectively [6]. The mechanisms implicated in atherosclerosis development in obesity include abnormalities in lipid metabolism, insulin resistance, inflammation, endothelial dysfunction, and adipokine imbalance [7]. Obesity is also linked to type 2 diabetes, hypertension, heart disease, sleep apnea, and certain types of cancer [8]. Type 2 diabetes affects 18.5% of adults with obesity compared to 5.4% with normal weight, peaking at 23.2% in those with severe obesity [9].
A positive association between high body mass index (BMI) and coronary artery disease (CAD) risk is supported by findings that every 1 kg/m2 increase in body mass index leads to a 5–7% increase in CAD incidence across all BMI categories [10]. Obese patients exhibit a significantly higher risk of CAD even after accounting for age, sex, physical activity, and smoking [11].
Excess adiposity was found to be responsible for 23% of CHD in men and 15% in women, according to the Framingham study [12]. The duration of obesity correlates with an increased risk of cardiovascular disease mortality, with a clear dose-dependent pattern; for every two additional years with obesity, CVD mortality risk rises by 7% [13]. Compared to individuals with a normal BMI, obesity is associated with a significantly heightened risk of CVD morbidity and mortality [14]. Overweight and obese individuals have a greater incidence of CVD events compared to those with normal weight [15].
Interestingly, previous studies showed that obese patients display better survival rates than normal-weight and underweight individuals, a phenomenon known as the “obesity paradox” [16,17]. Overweight and obese patients with CHD also exhibit a lower risk of total and cardiovascular mortality compared to underweight and normal-weight CHD patients [18]. However, recent studies did not show this survival effect in patients with low ejection fraction heart failure or acute coronary syndrome when using alternative anthropometric measurements rather than weight or adjustment for other predictors [19,20].
A meta-analysis of patients with acute coronary syndrome demonstrated that overweight, obese, and severely obese patients have significantly lower mortality rates compared to those with a normal BMI [21]. Similarly, overweight and obese patients with congestive heart failure (CHF) experience reduced CVD mortality (19% and 40%, respectively) and all-cause mortality (16% and 33%, respectively) compared to CHF patients with normal BMI [22]. The low-BMI group, consisting of underweight or normal-weight individuals, demonstrated the highest rates of adverse events, mortality, and rehospitalizations, while the overweight group exhibited the lowest rates [23].
Given the high prevalence of obesity in the Middle East, there is a need to investigate the epidemiology and impact of obesity among hospitalized CVD patients. This study aimed to assess, in our region, the effect of obesity on the presentation, diagnosis, and in-hospital outcomes of CVDs. We hypothesized that obesity has particular CVS presentations and outcomes (length of hospital stay, cardiac complications, and mortality).
2. Materials and Methods
Study design and setting: This was a retrospective observational study of patients admitted to the Heart Hospital, Hamad Medical Corporation (HMC) between the 1 January 2015 and the 31 December 2019. Data were collected from the Coronary Care Unit (CCU) registry at the Heart Hospital from January 2015 to December 2019. The Heart Hospital at HMC is a tertiary hospital that caters for more than 95% of the cardiac inpatient and outpatient medical and surgical care needs of nationals and residents of Qatar. Data from each patient were collected by the patients’ physicians at the time of discharge on a predefined coded record form (CRF). Recorded data were checked and validated by a research coordinator in the department. Approximately 40% of Qatar’s population are Arabs, including Qatari nationals, and 60% are non-Arabs.
Study population and data: The study included all adult male and female patients admitted to the cardiology department with BMI documented on admission. Patients with incomplete cardiac or BMI data were excluded. Obesity was defined according to the World Health Organization criteria [24]. After fulfilling the inclusion criteria, patients were divided into three groups according to BMI: Group I, normal weight (18.5–24.9 kg/m2); Group II, overweight (25–29.9 kg/m2); and Group III, obese (≥30 kg/m2). The obese group was further divided into three grades: Grade 1 (30–34.9 kg/m2), Grade 2 (35–39.9 kg/m2), and Grade 3 (≥40 kg/m2) [24]. Subgroup analysis of the obese cohort (III) was performed to study obesity grades based on presentation, diagnosis, and in-hospital outcomes.
Research tools: The CRF included history, along with information regarding risk factors for CHD, indication for coronary angiography, and the angiographic findings of each patient. Selective coronary angiography was performed using Judkins catheters via the radial or femoral route as per the suitability assessed by the interventional cardiologist. Any artery with >70% luminal narrowing was stented with a drug-eluting stent.
The presence of diabetes mellitus was determined by the documentation in the patient’s previous or current medical record of a diagnosis of diabetes mellitus that had been treated with medication or insulin. The presence of hyperlipidemia was determined by a fasting cholesterol > 5.2 mmol/L in the patient’s medical record or any history of hyperlipidemia treatment by the patient’s physician. The presence of hypertension was determined by documentation in the medical record of hypertension, or if the patient was receiving treatment from their physician. Patients were divided into current cigarette smokers, past smokers with more than six months of abstinence from smoking, and those with no smoking history. The diagnosis of acute coronary syndrome was based on the final decision of the assigned consultants based on clinical, electrocardiographic, laboratory, and echocardiographic data.
Statistical analysis: Continuous variables were expressed as mean ± Standard Deviation (SD) or Interquartile Range (IQR), as appropriate, while categorical variables were expressed as frequencies and percentages. Risk factors, final diagnosis, laboratory parameters, Percutaneous Coronary Intervention (PCI) at the time of admission or prior to discharge, and complications during the hospital stay, including in-hospital mortality, were compared among Groups I–III by applying one-way analysis of variance (ANOVA) or Kruskal–Wallis (non-parametric) tests for continuous variables, and chi-square tests for categorical variables. Obese patients were reassessed by subanalysis according to their BMI (Grades I–III). Multivariate regression analysis was performed for in-hospital mortality in the overall cohort and then in each major cardiovascular presentation (AMI, CHF and AF), and also for obese patients (BMI ≥ 30); data were expressed as crude and adjusted odds ratios (ORs) and a 95% confidence interval. Data were adjusted for age, sex, diabetes mellitus and hypertension. p values were calculated and a two-tailed p value of less than or equal to 0.05 was considered statistically significant. Statistical analysis was performed using SPSS (version 22.0; SPSS, Inc.; Chicago, IL, USA) for Windows.
3. Results
There were 7284 patients admitted with CVD to the Heart Hospital who were eligible for enrollment in the study analysis (Figure 1).
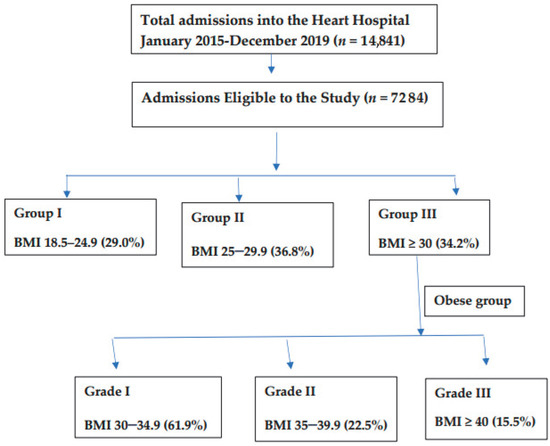
Figure 1.
Flowchart of the study design and body mass index (BMI) groups.
Table 1 shows the baseline characteristics of the study population. The mean age was significantly higher in Group III than in Groups I and II.

Table 1.
Baseline Characteristics of the study cohort.
Figure 2 shows the proportion of hospitalized male and female patients with CVD based on body mass index (BMI). Male sex was dominant in all BMI groups, except in the group with morbid obesity (≥40), where female sex predominated.

Figure 2.
Body mass index (BMI) in males and females.
Diabetes mellitus (DM) was more prevalent (61.6%) in Group III (p < 0.001). Similarly, hypertension was observed in 66.4% of patients in Group III, followed by 53.5% in Group II and 44.6% in Group I (p < 0.001). Dyslipidemia was noted in 56.9% of Group III, 40.9% of Group II, and 36.1% of Group I (p < 0.001). Chronic renal failure and peripheral arterial disease exhibited a similar distribution pattern to hypertension and dyslipidemia (p < 0.001). Smoking was observed more frequently in Group II than in Groups I and III (p < 0.001).
Chest pain was observed in 69.5% of patients in Group II, 66% in Group I, and 56.5% in Group III (p < 0.001). Shortness of breath and palpitations were most common in Group III, followed by Groups I and II (p < 0.001).
Table 2 and Figure 3 show the laboratory parameters of the study population. Troponin levels at the time of admission were higher in Group I, followed by Group II and Group III, p < 003. Peak troponins were also higher in Group II, followed by Group I and Group III, p < 0.001. BNP level was higher in Group I, followed by Group III and Group II, p < 0.001. Left ventricular ejection fraction (LVEF) of <30% was observed in more patients in Group I (14.7%), followed by Group III (11.5%) and Group II (11.1%). In contrast, LVEF of >50% was observed in more patients in Group III (46.7%), followed by Group II (46.1%) and Group I (40.6%) p < 0.001.

Table 2.
Laboratory and echocardiographic findings on admission.
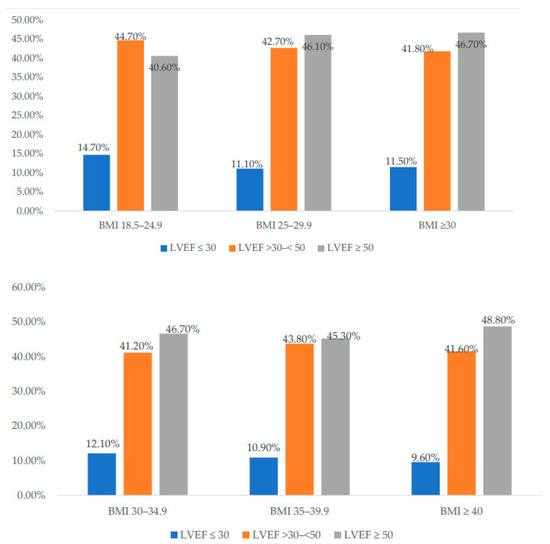
Figure 3.
Left ventricular ejection fraction (LVEF) based on body mass index (BMI) in the cohort (upper panel) and the obese groups (lower panel).
Table 3 shows the final diagnosis of the study populations. The majority of patients presented with ST-segment elevation myocardial infarction (STEMI). Among Group II patients, 58.3% had STEMI, followed by Group I (57.4%) and Group III (41.6%), p < 0.001. A similar trend was observed in non-ST-segment elevation myocardial infarction (NSTEMI) and unstable angina, with more patients in Group II having these final diagnoses with significant p values. Atrial fibrillation was observed in more patients in Group III (7.3%), followed by 3.8% in Group I and 3.5% in Group II, p < 0.001. Congestive heart failure was the final diagnosis in 475 subjects of Group III (19%), followed by Group I (13.3%) and Group II (11.4%), p < 0.001. Cardiomyopathy was the final diagnosis in 9.8% of Group I, 9.3% of Group III, and 7.3% of Group II, p < 0.004. The mean hospital stay was 4 days in Group I and Group III versus 3 days in Group II, p < 0.06.

Table 3.
Diagnosis of study population and procedure performed during hospital stay.
Table 3 also shows procedures performed during hospital stay. PCI at the time of admission was performed more in Group II (25.1%), followed by 24.1% in Group I and 15.4% in Group III, p < 0.001. Similarly, PCI before discharge was performed more in Group II (21.4%), followed by 18.8% in Group I and 17.7% in Group III, p < 0.003. Single vessel disease (VD) was observed more in Group II (20.2%), followed by 18.5% in Group I and 14.2% in Group III, p < 0.001. A similar pattern was observed in 2VD, with fewer patients (9.9%) in Group III compared to Groups II and I, p < 0.001. Three VD was observed more in Group I (17.7%), followed by Group II (17.1%) and Group III (13.1%), p < 0.001.
Atrial fibrillation (AF) during the hospital stay occurred more frequently in Group III (3.2%), followed by Group II (2.1%) and Group I (1.9%), p < 0.006. Ventricular fibrillation (VF) occurred more frequently in Group I than Groups II and III, p = 0.03. Ventricular tachycardia (VT) was also observed more frequently in Group I than in the other groups. Shock also occurred more frequently in Group I (1.9%), followed by Group II (1.8%) and Group III (1.0%), p < 0.02. More in-hospital mortality was observed in Group III (10.9%), followed by Group II (7.7%) and Group I (7.6%), p < 0.001 (Table 4).

Table 4.
Complications during hospital stay.
Subgroup Analysis of the obese group: The obese cohort (BMI ≥ 30) was graded according to their BMI (61.9% Grade I, 22.5% Grade II, and 15.5% Grade III). Table 5 shows the baseline characteristics of the obese population. The mean age was higher in Grade III than in Grades I and II (p < 0.001). DM was observed in 71.1%, 66.5%, and 57.3% of patients in Grades III, II, and I, respectively (p < 0.001). Similarly, hypertension was observed in 80.9%, 71.9%, and 60.8% of patients in Grades III, II, and I, respectively (p < 0.001). Dyslipidemia was noted in 65.5%, 63.3%, and 52.1% of patients in Grades II, III, and I, respectively (p < 0.001). Chronic renal failure exhibited a distribution pattern similar to that of DM and hypertension (p < 0.001). Smoking was observed more frequently in Grade I than in Grades II and III (p < 0.001). Chest pain was the most common symptom on admission, followed by shortness of breath and palpitations. Chest pain was observed in 60.9%, 53.2%, and 43.7% of patients in Grades I, II, and III, respectively (p < 0.001). Shortness of breath was the most common symptom in Grade III, followed by Grades II and I (p < 0.001).

Table 5.
Subgroup analysis of the obese cohort (Baseline Characteristics).
Table 6 and Figure 3 show the laboratory parameters of the study population. Troponin levels at the time of admission were higher in Grade I, followed by Grades II and III, p < 0.07. Peak troponins were also higher in Grade I, followed by Grades II and III, p < 0.007. LVEF was <30% in Grade I (12.1%), followed by Grades II (10.9%) and III (9.6%).

Table 6.
Laboratory and echocardiographic findings on admission for obese patients.
Table 7 shows the final diagnoses of the study population. Among Grade I patients, 47.2% had STEMI, followed by Grade II (37.2%) and Grade III (25.6%), p < 0.001. A similar trend was observed for NSTEMI and unstable angina, with more patients in Grade I presenting with NSTEMI or unstable angina than in the other grades. Atrial fibrillation was observed in 11.6%, 7.5%, and 6.1% of the patients in Grades III, II, and I, respectively (p < 0.001). Congestive heart failure was the more frequent diagnosis in Grade III (27.6%), followed by 16% and 12.5% in Grades I and II, respectively (p < 0.001).

Table 7.
Diagnosis of obese patients and procedures performed during hospital stay among obese patients.
Procedures performed during hospital stay are given in Table 7. PCI procedures were less performed in morbidly obese patients, Grade III, as PCI at the time of admission was performed more in Grade I (18.5%), followed by 13.5% in Grade II and 5.7% in Grade III, p < 0.001. Similarly, PCI before discharge was performed more in Grade I (20.5%), followed by 14.4% in Grade II and 11.4% in Grade III, p < 0.003. Single vessel disease was more prevalent in Grade I (16.2%), followed by 13.2% in Grade II and 7.8% in Grade III, p < 0.001. A similar pattern was observed with 2VD and 3VD, with fewer patients in Grade III as compared to Grades I and II, p < 0.001 and p < 0.007, respectively.
Ventricular tachycardia (VT) during the hospital stay occurred more frequently in Grade II (2.1%), followed by Grade I (1.7%), p = 0.02. More in-hospital mortality was observed in Grade III (17.1), followed by 11.2% in Grade II and 9.3% in Grade I (p < 0.001) (Table 8).

Table 8.
Complications during hospital stay among obese patients.
Multivariate regression analysis: The univariate analysis shows that obesity is a significant risk factor for in-hospital mortality. A multivariate analysis was performed to check whether it is also significant after adjusting for age and sex. To assess the predictive role of obesity in in-hospital mortality, the crude odds ratio (OR) of BMI ≥ 30 was 1.47 (95% CI 1.25–1.74), p = 0.001, in the overall cohort, 1.46 (95% CI 1.10–1.92), p = 0.008, among AMI patients, 0.92 (95% CI 0.69–1.23), p = 0.56, among CHF patients, and 0.67 (95% CI 0.38–1.17), p = 0.16, for AF patients. However, after adjustment for age and sex, the significant impact of BMI disappeared (OR 1.08, 95% CI 0.90–1.29), p = 0.39, for AMI patients. Table 9 shows the crude and adjusted OR for predictors of mortality among obese patients only. BMI ≥ 30 was a predictor for mortality; however, after adjustment for comorbidities, this effect on mortality was eliminated.

Table 9.
Multivariate regression analysis for predictors of mortality among obese patients unadjusted and adjusted for age, sex, and comorbidities.
4. Discussion
The present study describes the impact of obesity on the presentation and outcomes of patients hospitalized for CVDs in a Middle Eastern country. In Qatar, the rate of obesity is high (33%), with a predominance of female gender [25]. Among patients who were hospitalized at the HH, obesity was a predictor of mortality in the unadjusted model. Overweight and obese patients had a 3- or 5-fold increased risk of developing thromboembolic events [26]. Moreover, obese patients with thromboembolism had characteristic risk factors and better survival [25]. However, the mechanism of this paradox in survival remains unclear. It could be related to potential lead time bias that occurs when obese patients develop cardiovascular events earlier in their lifetime or are tested earlier for CVD than patients with normal weight, leading to earlier diagnosis and treatment and confounding differences in outcomes [27]. Moreover, the authors redefined the “obesity” paradox and replaced it with the “BMI” paradox, exploring several limitations of using BMI alone to reflect subject adiposity status [28]. Furthermore, the protective effect of obesity is no longer considered.
In this analysis, one-third of the hospitalized patients were obese, and the most common reason for admission was AF, followed by CHF, particularly with a preserved ejection fraction. The average age of patients in the obese group was higher than those of patients in the normal and overweight groups. Obese individuals were more likely to have comorbidities.
The overweight individuals had a higher proportion of STEMI among the study cohort. A 10 kg increase in body weight increases the risk of CAD by 12% and, simultaneously, the systolic blood pressure rises by 3 mmHg and the diastolic by 2.3 mmHg consequently [29]. Furthermore, NSTEMI affects more young people, and excess weight could be one of the most important risk factors ahead of smoking. The higher the BMI, the sooner NSTEMI develops [30]. The BMI paradox was also observed in STEMI [31]. Based on the available data, obesity is an independent risk factor for STEMI at a young age [32]. Our analysis showed that obesity is a significant predictor of mortality among AMI patients; however, when we considered age and sex, this effect on mortality was eliminated.
Park et al. [33] found a BMI paradox in patients referred for PCI in whom BMI > 30 kg/m2 was associated with lower mortality and risk of CV events after PCI. The investigators did not explain this paradox clearly but called for further studies. Others have suggested that in obese patients, larger vessels are treated with larger stent diameter, or this could be related to the cardio-protective effect of adipokines [33,34].
A recent meta-analysis of patients with CHD concluded that obesity is associated with a lower risk of mortality in the short term but has a higher risk after 5 years (J-shaped pattern) [35].
In the current study, PCI at the index admission was higher in the overweight group than in the obese group. Single or 2VD was more frequently observed in this group, whereas 3VD was less evident in the obese group. Notably, the number of obstructed vessels decreased with increasing BMI in the obese cohort.
Some studies showed that higher BMI is strongly associated with the risk of HF with preserved EF rather than HF with reduced EF [36]. Moreover, a few studies reported that parameters of excess adiposity (using the waist in the measures) are independently associated with HF risk; however, they concluded that these parameters generally do not add substantive risk information for HF beyond BMI [27,37,38]. Shortness of breath and palpitations were common in the obese patients; however, LVEF < 30% was more frequent in the overweight group than the obese group. In contrast, LVEF > 50% was observed more in obese patients presenting with HF symptoms (HF with preserved EF). Other studies on patients with acutely decompensated HF demonstrated an obesity paradox with CHF. This paradox was largely confined to older patients and those with reduced LV function [39]. Additionally, a report from the Cleveland Clinic found that although the obesity paradox was evident, this largely disappeared after adjustment for confounders and then was confined mainly to women in the overweight BMI range [40]. Furthermore, the risk of CHF associated with obesity was noted as independent of other risk factors, including gender as well as cardiorespiratory fitness levels [41,42,43,44].
In the present study, AF was observed more frequently in obese patients than in normal-weight and overweight patients. A meta-analysis of 16 studies demonstrated that obese individuals have a nearly 50% increased risk of AF compared with non-obese individuals [45]. Importantly, a large prospective study demonstrated an approximately 4% increase in AF risk per 1-unit increase in BMI in men and women [46]. Additionally, evidence suggests that obesity may also be a risk factor for the progression of paroxysmal AF to persistent AF, which carries a higher morbidity and mortality [47].
However, as in patients with hypertension, CHD, and CHF, overweight and obese patients with AF demonstrate an obesity paradox, with a nearly 50% reduction in CV and all-cause mortality compared with AF patients with normal BMI [48,49].
In the present study, a higher in-hospital mortality was observed in the obese group, followed by the overweight and normal-weight groups. In Grade III obese patients, mortality was higher than in Grades II and I. These results are in contrast with those of previous studies, as most have suggested that overweight and obese patients have a better prognosis. A BMI of more than 25 among AMI patients was an independent predictor of lower mortality and shorter length of stay in the USA [50]. A meta-analysis reported that overweight/mildly obese patients with CHD have a lower risk of total and CVD mortality than underweight and normal-weight CHD patients [18]. The authors attributed this paradox to the lack of discriminatory power of BMI to distinguish body fat and lean mass. A positive relationship between CVD mortality and BMI has been shown in many large-scale studies [51]. The production of adipocytokines, oxidative stress, and prothrombotic state in obese people may contribute to CAD risk in a more significant way than what has been explained with other CV risk factors [52,53,54]. On the other hand, some authors consider the “lean paradox”, in which low body fat percentage and low BMI could be a predictor of worse CVD outcomes [27,55].
Our data showed that obesity (using BMI) was not an independent predictor of mortality in AF and CHF patients. On the contrary, it was a predictor of mortality among AMI patients in an unadjusted model (crude OR 1.46).
The risk of selection bias limits the retrospective design of this study. Many subjects were admitted to the Heart Hospital without having their BMI or waist circumference recorded on admission, which led to an underestimation of the prevalence of obesity in each study group. Moreover, being a single-center study limits the generalizability of the findings. There are many limitations to using BMI alone as a predictor of outcome because it does not correctly reflect subject adiposity and its distribution, but it also varies according to gender and ethnicity, and it does not account for fitness related to the proportion of lean mass to adiposity (i.e., it cannot distinguish adipose tissue from lean body mass) [22,28,56].
The patients’ follow-up was not recorded, which is a limiting factor in addressing long-term mortality and rehospitalization. The occurrence of coronary spasm, insulin resistance, and micro-vessel CAD in young obese subjects is also an interesting area for research [57,58].
5. Conclusions
In this study, one-third of the hospitalized CVS patients were obese. AF and CHF with preserved EF were the most common cardiovascular presentations in obese patients. In patients with CVDs, obesity was associated with higher rates of comorbidities and in-hospital mortality. However, obesity measured by BMI alone was not an independent predictor of mortality in cardiac obese patients.
Author Contributions
Conceptualization, A.R.A. and A.E.-M.; methodology, A.A., A.E.-M., R.S., M.G., S.H., A.S.A., N.A., A.A., H.A.-T., H.A. and J.A.S.; formal analysis, R.S.; data curation, R.S., M.G., S.H. and A.S.A.; writing—original draft preparation, A.R.A. and A.E.-M.; writing—review and editing, R.S., S.H. and A.E.-M.; supervision, H.A., N.A., A.A., H.A.-T. and J.A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. All the authors of this manuscript are employed by the Hamad Medical Corporation, which is a governmental non-for-profit medical institution. All the authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Institutional Review Board Statement
Data were extracted retrospectively and anonymously from the coronary care unit (CCU) data registry, which was approved by the Institutional Review Board (IRB) of the MRC at HMC (MRC#11355/11), Doha, Qatar.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are given in the manuscript, tables, and figures.
Acknowledgments
We thank the Medical Research Center (MRC) at Hamad Medical Corporation (HMC) and the Qatar National Library for their support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Di Cesare, M.; Bixby, H.; Gaziano, T.; Hadeed, L.; Kabudula, C.; McGhie, D.V.; Mwangi, J.; Pervan, B.; Perel, P.; Piñeiro, D.; et al. World Heart Report 2023: Confronting the World’s Number One Killer; World Heart Federation: Geneva, Switzerland, 2023. [Google Scholar]
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006, 113, 898–918. [Google Scholar] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief 2020, 360, 1–8. [Google Scholar]
- Berghöfer, A.; Pischon, T.; Reinhold, T.; Apovian, C.M.; Sharma, A.M.; Willich, S.N. Obesity prevalence from a European perspective: A systematic review. BMC Public Health 2008, 8, 200. [Google Scholar] [CrossRef] [PubMed]
- Okati-Aliabad, H.; Ansari-Moghaddam, A.; Kargar, S.; Jabbari, N. Prevalence of Obesity and Overweight among Adults in the Middle East Countries from 2000 to 2020: A Systematic Review and Meta-Analysis. J. Obes. 2022, 2022, 8074837. [Google Scholar] [CrossRef] [PubMed]
- Minutello, R.M.; Chou, E.T.; Hong, M.K.; Bergman, G.; Parikh, M.; Iacovone, F.; Wong, S.C. Impact of body mass index on in-hospital outcomes following percutaneous coronary intervention (report from the New York State Angioplasty Registry). Am. J. Cardiol. 2004, 93, 1229–1232. [Google Scholar] [CrossRef]
- Lovren, F.; Teoh, H.; Verma, S. Obesity and atherosclerosis: Mechanistic insights. Can. J. Cardiol. 2015, 31, 177–183. [Google Scholar] [CrossRef]
- Berenson, G.S.; Srinivasan, S.R.; Bao, W.; Newman, W.P.I.I.I.; Tracy, R.E.; Wattigney, W.A. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N. Engl. J. Med. 1998, 338, 1650–1656. [Google Scholar] [CrossRef]
- Saydah, S.; Bullard, K.M.; Cheng, Y.; Ali, M.K.; Gregg, E.W.; Geiss, L.; Imperatore, G. Trends in cardiovascular disease risk factors by obesity level in adults in the United States, NHANES 1999–2010. Obesity 2014, 22, 1888–1895. [Google Scholar] [CrossRef]
- Cho, E.; Manson, J.E.; Stampfer, M.J.; Solomon, C.G.; Colditz, G.A.; Speizer, F.E.; Willett, W.C.; Hu, F.B. A prospective study of obesity and risk of coronary heart disease among diabetic women. Diabetes Care 2002, 25, 1142–1148. [Google Scholar] [CrossRef]
- Bogers, R.P.; Bemelmans, W.J.E.; Hoogenveen, R.T.; Boshuizen, H.C.; Woodward, M.; Knekt, P.; van Dam, R.M.; Hu, F.B.; Visscher, T.L.S.; Menotti, A.; et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: A meta-analysis of 21 cohort studies including more than 300 000 persons. Arch. Intern. Med. 2007, 167, 1720–1728. [Google Scholar] [CrossRef]
- Wilson, P.W.F.; D’Agostino, R.B.; Sullivan, L.; Parise, H.; Kannel, W.B. Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch. Intern. Med. 2002, 162, 1867–1872. [Google Scholar] [CrossRef]
- Abdullah, A.; Wolfe, R.; Stoelwinder, J.U.; De Courten, M.; Stevenson, C.; Walls, H.L.; Peeters, A. The number of years lived with obesity and the risk of all-cause and cause-specific mortality. Int. J. Epidemiol. 2011, 40, 985–996. [Google Scholar] [CrossRef]
- Khan, S.S.; Ning, H.; Wilkins, J.T.; Allen, N.; Carnethon, M.; Berry, J.D.; Sweis, R.N.; Lloyd-Jones, D.M. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018, 3, 280–287. [Google Scholar] [CrossRef]
- Lavie, C.J.; Sharma, A.; Alpert, M.A.; De Schutter, A.; Lopez-Jimenez, F.; Milani, R.V.; Ventura, H.O. Update on obesity and obesity paradox in heart failure. Prog. Cardiovasc. Dis. 2016, 58, 393–400. [Google Scholar] [CrossRef]
- Sierra-Johnson, J.; Romero-Corral, A.; Somers, V.K.; Lopez-Jimenez, F.; Thomas, R.J.; Squires, R.W.; Allison, T.G. Prognostic importance of weight loss in patients with coronary heart disease regardless of initial body mass index. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 336–340. [Google Scholar] [CrossRef]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O. Obesity and cardiovascular disease. Risk factor, paradox, and impact of weight loss. J. Am. Coll. Cardiol. 2009, 53, 1925–1932. [Google Scholar] [CrossRef]
- Romero-Corral, A.; Montori, V.M.; Somers, V.K.; Korinek, J.; Thomas, R.J.; Allison, T.G.; Mookadam, F.; Lopez-Jimenez, F. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. Lancet 2006, 368, 666–678. [Google Scholar] [CrossRef]
- Butt, J.H.; Petrie, M.C.; Jhund, P.S.; Sattar, N.; Desai, A.S.; Køber, L.; Rouleau, J.L.; Swedberg, K.; Zile, M.R.; Solomon, S.D.; et al. Anthropometric measures and adverse outcomes in heart failure with reduced ejection fraction: Revisiting the obesity paradox. Eur. Heart J. 2023, 44, 1136–1153. [Google Scholar] [CrossRef]
- Kwaśny, A.; Łokieć, K.; Uchmanowicz, B.; Młynarska, A.; Smereka, J.; Czapla, M. Sex-related differences in the impact of nutritional status on in-hospital mortality in acute coronary syndrome: A retrospective cohort study. Nutr. Metab. Cardiovasc. Dis. 2023, 33, 2242–2250. [Google Scholar] [CrossRef]
- Niedziela, J.; Hudzik, B.; Niedziela, N.; Gąsior, M.; Gierlotka, M.; Wasilewski, J.; Myrda, K.; Lekston, A.; Poloński, L.; Rozentryt, P. The obesity paradox in acute coronary syndrome: A meta-analysis. Eur. J. Epidemiol. 2014, 29, 801–812. [Google Scholar] [CrossRef] [PubMed]
- Purnell, J.Q. Definitions, Classification, and Epidemiology of Obesity [Updated 4 May 2023]. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK279167/ (accessed on 25 August 2023).
- Oreopoulos, A.; Padwal, R.; Kalantar-Zadeh, K.; Fonarow, G.C.; Norris, C.M.; McAlister, F.A. Body mass index and mortality in heart failure: A meta-analysis. Am. Heart J. 2008, 156, 13–22. [Google Scholar] [CrossRef]
- Sharma, A.; Lavie, C.J.; Borer, J.S.; Vallakati, A.; Goel, S.; Lopez-Jimenez, F.; Arbab-Zadeh, A.; Mukherjee, D.; Lazar, J.M. Meta-analysis of the relation of body mass index to all-cause and cardiovascular mortality and hospitalization in patients with chronic heart failure. Am. J. Cardiol. 2015, 115, 1428–1434. [Google Scholar] [CrossRef] [PubMed]
- El-Menyar, A.; Asim, M.; Al-Thani, H. Obesity Paradox in Patients with Deep Venous Thrombosis. Clin. Appl. Thromb./Hemost. 2018, 24, 986–992. [Google Scholar] [CrossRef] [PubMed]
- García-Raso, A.; Llamas Sillero, P. Elevated body fat is a risk factor for venous thromboembolism and thrombotic complications. Epidemiol. Rep. 2014, 2, 3. [Google Scholar] [CrossRef][Green Version]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Pinto, A.; Giusti, A.M.; Lenzi, A.; Poggiogalle, E. Obesity or BMI Paradox? Beneath the Tip of the Iceberg. Front. Nutr. 2020, 7, 53. [Google Scholar] [CrossRef]
- Din-Dzietham, R.; Liu, Y.; Bielo, M.V.; Shamsa, F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation 2007, 116, 1488–1496. [Google Scholar] [CrossRef]
- Madala, M.C.; Franklin, B.A.; Chen, A.Y.; Berman, A.D.; Roe, M.T.; Peterson, E.D.; Ohman, E.M.; Smith, S.C.; Gibler, W.B.; McCullough, P.A.; et al. Obesity and age of first non-ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 2008, 52, 979–985. [Google Scholar] [CrossRef]
- Das, S.R.; Alexander, K.P.; Chen, A.Y.; Powell-Wiley, T.M.; Diercks, D.B.; Peterson, E.D.; Roe, M.T.; de Lemos, J.A. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry). J. Am. Coll. Cardiol. 2011, 58, 2642–2650. [Google Scholar] [CrossRef]
- Jamil, G.; Jamil, M.; Alkhazraji, H.; Haque, A.; Chedid, F.; Balasubramanian, M.; Khairallah, B.; Qureshi, A. Risk factor assessment of young patients with acute myocardial infarction. Am. J. Cardiovasc. Dis. 2013, 3, 170–174. [Google Scholar]
- Park, D.-W.; Kim, Y.-H.; Yun, S.-C.; Ahn, J.-M.; Lee, J.-Y.; Kim, W.-J.; Kang, S.-J.; Lee, S.-W.; Lee, C.W.; Park, S.-W.; et al. Association of body mass index with major cardiovascular events and with mortality after percutaneous coronary intervention. Circ. Cardiovasc. Interv. 2013, 6, 146–153. [Google Scholar] [CrossRef]
- Momin, A.U.; Melikian, N.; Shah, A.M.; Grieve, D.J.; Wheatcroft, S.B.; John, L.; El Gamel, A.; Desai, J.B.; Nelson, T.; Driver, C.; et al. Leptin is an endothelial-independent vasodilator in humans with coronary artery disease: Evidence for tissue specificity of leptin resistance. Eur. Heart J. 2006, 27, 2294–2299. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.J.; Zhou, Y.J.; Galper, B.Z.; Gao, F.; Yeh, R.W.; Mauri, L. Association of body mass index with mortality and cardiovascular events for patients with coronary artery disease: A systematic review and meta-analysis. Heart 2015, 101, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; Patel, K.V.; Vaduganathan, M.; Sarma, S.; Haykowsky, M.J.; Berry, J.D.; Lavie, C.J. Physical activity, fitness, and obesity in heart failure with preserved ejection fraction. JACC Heart Fail. 2018, 6, 975–982. [Google Scholar] [CrossRef] [PubMed]
- Loehr, L.R.; Rosamond, W.D.; Poole, C.; McNeill, A.M.; Chang, P.P.; Folsom, A.R.; Chambless, L.E.; Heiss, G. Association of multiple anthropometrics of overweight and obesity with incident heart failure: The Atherosclerosis Risk in Communities Study. Circ. Heart Fail. 2009, 2, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Levitan, E.B.; Yang, A.Z.; Wolk, A.; Mittleman, M.A. Adiposity and incidence of heart failure hospitalization and mortality: A population-based prospective study. Circ. Heart Fail. 2009, 2, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Gayat, E.; Januzzi, J.L.; Sato, N.; Cohen-Solal, A.; diSomma, S.; Fairman, E.; Harjola, V.-P.; Ishihara, S.; Lassus, J.; et al. Body mass index and mortality in acutely decompensated heart failure across the world: A global obesity paradox. J. Am. Coll. Cardiol. 2014, 63, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Vest, A.R.; Wu, Y.; Hachamovitch, R.; Young, J.B.; Cho, L.S. The heart failure overweight/obesity survival paradox: The missing sex link. JACC Heart Fail. 2015, 3, 917–926. [Google Scholar] [CrossRef]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O. Adipose composition and heart failure prognosis: Paradox or not? J. Am. Coll. Cardiol. 2017, 70, 2750–2751. [Google Scholar] [CrossRef]
- Pandey, A.; LaMonte, M.; Klein, L.; Ayers, C.; Psaty, B.M.; Eaton, C.B.; Allen, N.B.; de Lemos, J.A.; Carnethon, M.; Greenland, P.; et al. Relationship between physical activity, body mass index, and risk of heart failure. J. Am. Coll. Cardiol. 2017, 69, 1129–1142. [Google Scholar] [CrossRef]
- Pandey, A.; Cornwell, W.K.; Willis, B.; Neeland, I.J.; Gao, A.; Leonard, D.; DeFina, L.; Berry, J.D. Body mass index and cardiorespiratory fitness in mid-life and risk of heart failure hospitalization in older age: Findings from the cooper center longitudinal study. JACC Heart Fail. 2017, 5, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Kwaśny, A.; Uchmanowicz, I.; Juárez-Vela, R.; Młynarska, A.; Łokieć, K.; Czapla, M. Sex-Related Differences in the Impact of Nutritional Status on In-Hospital Mortality in Heart Failure: A Retrospective Cohort Study. Eur. J. Cardiovasc. Nurs. 2023, zvad050. [Google Scholar] [CrossRef]
- Wanahita, N.; Messerli, F.H.; Bangalore, S.; Gami, A.S.; Somers, V.K.; Steinberg, J.S. Atrial fibrillation and obesity: Results of a meta-analysis. Am. Heart J. 2008, 155, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.J.; Parise, H.; Levy, D.; D’Agostino, R.B.; Wolf, P.A.; Vasan, R.S.; Benjamin, E.J. Obesity and the risk of new-onset atrial fibrillation. JAMA 2004, 292, 2471–2477. [Google Scholar] [CrossRef] [PubMed]
- Tsang, T.S.; Barnes, M.E.; Miyasaka, Y.; Cha, S.S.; Bailey, K.R.; Verzosa, G.C.; Seward, J.B.; Gersh, B.J. Obesity as a risk factor for the progression of paroxysmal to permanent atrial fibrillation: A longitudinal cohort study of 21 years. Eur. Heart J. 2008, 29, 2227–2233. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; McAuley, P.A.; Church, T.S.; Milani, R.V.; Blair, S.N. Obesity and cardiovascular diseases: Implications regarding fitness, fatness, and severity in the obesity paradox. J. Am. Coll. Cardiol. 2014, 63, 1345–1354. [Google Scholar] [CrossRef] [PubMed]
- Tutor, A.W.; Lavie, C.J.; Kachur, S.; Milani, R.V.; Ventura, H.O. Updates on obesity and the obesity paradox in cardiovascular diseases. Prog. Cardiovasc. Dis. 2023, 78, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Elbaz-Greener, G.; Rozen, G.; Carasso, S.; Kusniec, F.; Marai, I.; Sud, M.; Strauss, B.; Smart, F.W.; Planer, D.; Amir, O. The Relationship between Body Mass Index and In-Hospital Mortality in the Contemporary Era of an Acute Myocardial Infarction Management. Vasc. Health Risk Manag. 2021, 17, 551–559. [Google Scholar] [CrossRef]
- Valavanis, I.K.; Mougiakakou, S.G.; Grimaldi, K.A.; Nikita, K.S. A multifactorial analysis of obesity as CVD risk factor: Use of neural network based methods in a nutrigenetics context. BMC Bioinform. 2010, 11, 453. [Google Scholar] [CrossRef]
- Grundy, S.M. Metabolic syndrome update. Trends Cardiovasc. Med. 2016, 26, 364–373. [Google Scholar] [CrossRef]
- El-Menyar, A.; Rizk, N.; Al Nabti, A.D.; Hassira, S.A.; Singh, R.; Abdel Rahman, M.O.; Suwaidi, J.A. Total and high molecular weight adiponectin in patients with coronary artery disease. J. Cardiovasc. Med. 2009, 10, 310–315. [Google Scholar] [CrossRef]
- Rizk, N.M.; El-Menyar, A.; Marei, I.; Sameer, M.; Musad, T.; Younis, D.; Farag, F.; Basem, N.; Al-Ali, K.; Al Suwaidi, J. Association of adiponectin gene polymorphism (+T45G) with acute coronary syndrome and circulating adiponectin levels. Angiology 2013, 64, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Elagizi, A.; Kachur, S.; Lavie, C.J.; Carbone, S.; Pandey, A.; Ortega, F.B.; Milani, R.V. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog. Cardiovasc. Dis. 2018, 61, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Razak, F.; Anand, S.S.; Shannon, H.; Vuksan, V.; Davis, B.; Jacobs, R.; Teo, K.K.; McQueen, M.; Yusuf, S.; The SHARE Investigators. Defining obesity cut points in a multiethnic population. Circulation 2007, 115, 2111–2118. [Google Scholar] [CrossRef] [PubMed]
- El-Menyar, A.A.; Gomaa, M.M.; Arafa, S.E. Obesity: A risk factor for acute myocardial infarction with angiographically patent epicardial coronary vessels in an adolescent. Med. Princ. Pract. 2006, 15, 449–452. [Google Scholar] [CrossRef]
- Frisbee, J.C. Vascular dysfunction in obesity and insulin resistance. Microcirculation 2007, 14, 269–271. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).