Abstract
Disc displacement (DD) appears in the majority of temporomandibular disorder (TMD) patients. The correlation between craniofacial morphology and different disc positions has been underlined, while the craniofacial morphological differences based on sex and sagittal skeletal pattern stratification have been insufficiently studied. In this study, 304 patients with TMD complaints were included and classified into normal position, disc displacement with reduction (DDwR) and disc displacement without reduction (DDwoR) groups according to magnetic resonance imaging. A total of 24 cephalometric measurements, covering the cranial base, vertical relationship, sagittal relationship, mandible position and morphology, and dental relationship, were assessed using lateral cephalograms. A stratified analysis was performed based on the sex and sagittal skeletal pattern. Overall, DD patients had distinctive craniofacial morphological features. The posterior cranial base length and mandibular arc angle were statistically different only in females, while the Y-axis angle, occlusal plane angle and sella nasion point A angle (SNA) might be unique features in males. Skeletal class II had the most statistically different measurements compared to the others. Differences in the Frankfort mandibular incisor angle (FMIA) and saddle angle were especially displayed in skeletal class III patients. The sex and skeletal sagittal pattern could affect the morphological differences in TMD patients with different disc positions.
1. Introduction
Temporomandibular disorders (TMDs) refer to a series of heterogeneous musculoskeletal disorders with diverse manifestations and pathogenies [1]. Pain, noises, deviated jaw movement and decreased mouth opening are most commonly complained symptoms of TMD patients [2]. With a high prevalence of 27–38% in the general population [3], TMDs have become an unneglectable thorny issue in clinical treatment. Articular disc displacement composes an important subtype of TMDs and is reported to be diagnosed in nearly 70% of the TMD patients [4,5]. The articular disc is normally located between the mandibular condyle and the articular eminence of the temporal bone and functions as a cushion between the two bone surfaces during jaw movement [6,7]. The alteration of the disc position, frequently in the anterior direction, is described as disc displacement (DD) [8]. In the diagnosis of DD, magnetic resonance imaging (MRI) is considered the gold standard. Through analyzing MRIs taken in closed-mouth and open-mouth positions, DD can be further classified into that with reduction (DDwR) and without reduction (DDwoR).
The mechanisms of DD remain controversial. Some studies have underlined the potential correlations between craniofacial morphology and different disc positions in TMD patients [9,10]. A retrusion and clockwise rotation of the mandible, smaller ramus height and decreased posterior facial height have been reported as remarkable morphological features in DD patients [11]. However, insufficient attention has been paid to potential confounding factors, such as age, sex, ancestry or environment, which are possible risk factors for TMDs as well as significant determinants in the formation of different craniofacial morphologies [12]. A higher prevalence of TMDs in females than males has been reported [13], while the mechanisms of such sex-related difference remain arguable. The role of malocclusion in the pathogenesis of TMDs is debatable [14]. It has been reported by some studies that dental malocclusion and transverse discrepancies should not be predictors of TMDs, but the retro-positioned mandibles might be distinct in joint disorder patients [14,15]. However, few studies have subdivided TMD patients based on skeletal pattern, and insufficient evidence has been provided in verifying the differences in skeletal class I, class II and class III DD patients. Contemporarily, a tailored and comprehensive treatment strategy has been suggested for TMD treatment, which has also enhanced the need for exquisite assessment methods and the precise subcategorization of patients [16,17]. Therefore, a study with a stratified comparative analysis is required in order to discriminate the stratifying features in different subgroups.
The aim of the present study is to depict the morphological features in DD patients by analyzing MRI in closed-mouth and open-mouth positions as well as lateral cephalograms, so as to provide more evidence for the pathology of DD in different sexes and sagittal skeletal patterns.
2. Materials and Methods
2.1. Study Population
This retrospective study was conducted on Chinese Han patients who visited the orthodontic department of our hospital between 1 January 2021 and 30 December 2021. Written informed consent was obtained from all patients. MRI and X-ray cephalometry were examined only when the patients had TMD complaints or clinical symptoms to avoid excessive examinations. All the procedures were conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of West China Hospital of Stomatology, Sichuan University (No. WCH-SIRB-CT-2020-418, 31 December 2020). The inclusion criteria were as follows: (1) adult patients with permanent dentition, (2) with complaints of TMD symptoms, (3) with clear lateral cephalogram and MRI containing TMJ of both sides in closed-mouth and open-mouth positions. The exclusion criteria were as follows: (1) a history of tumor, maxillofacial deformity, trauma or craniofacial surgeries that might affect TMJ or craniofacial morphology; (2) a history of systemic diseases; (3) a history of orthodontic treatment or plastic surgery; (4) a history of TMD treatment.
2.2. Magnetic Resonance Imaging (MRI) Evaluation
The MRIs were performed with a 1.5T MRI scanner (Philips, Amsterdam, The Netherlands) with a TMJ surface coil. To identify the disc position, T2-weighted imaging (T2WI) generated by a fast spin echo (FSE) sequence was examined. Parameter settings were: 2300 ms for repetition time; 45 ms for echo time; 3 mm for slice thickness; 0 mm for slice gap; 2 for number of excitations; 288 × 256 pixels for image matrix. The scanning included nonorthogonal sagittal and nonorthogonal coronal sections in the closed-mouth position and nonorthogonal sagittal sections in the open-mouth position. Patients assumed a supine position with the center of the coil positioned at a 10 mm anterior to the tragus. For the closed-mouth position, patients were instructed to occlude in the intercuspal position and hold the lips in a relaxed status. For the open-mouth position, patients were instructed to slowly reach maximum unassisted mouth opening (MMO), and then rubber pads with different thicknesses were applied to maintain the posture. MRI data were stored in DICOM format and observed with RadiAnt DICOM Viewer (Medixant, Poznan, Poland). The diagnosis of the subjects was categorized into 3 groups [18,19,20] (Figure 1). Two operators (C.Y. and X.X.) conducted the MRI diagnosis. The intra-observer and inter-observer reliability was verified before the study with a kappa coefficient >0.85.
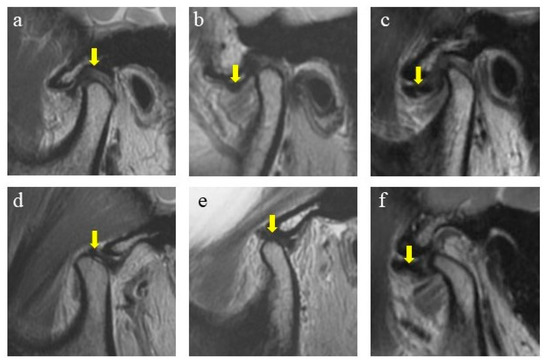
Figure 1.
Diagnosis of disc displacements in MRIs. (a) Normal, in closed-mouth position; (b) DDwR, in closed-mouth position; (c) DDwoR, in closed-mouth position; (d) normal, in open-mouth position; (e) DDwR, in open-mouth position; (f) DDwoR, in open-mouth position. Arrow shows the position of the articular disc.
2.2.1. Normal Position
In the closed-mouth position, the intermediate zone of the articular disc was located between the posterior slope of the articular eminence and the anterior slope of the condyle head (defined as from 11:30 to 12:30 o’clock to the condyle head). In the open-mouth position, the intermediate zone was located between the top of the condyle head and the articular eminence. Subjects with articular discs of both sides in the normal position were assigned to the normal group.
2.2.2. Disc Displacement with Reduction (DDwR)
In the closed-mouth position, the intermediate zone of the articular disc was anteriorly displaced relative to the anterior slope of the condyle head (defined as before 11:30 o’clock to the condyle head). In the open-mouth position, the intermediate zone was reduced to the top of the condyle head and articular eminence. Subjects diagnosed with bilateral DDwR or unilateral DDwR with the other in the normal position were assigned to the DDwR group.
2.2.3. Disc Displacement without Reduction (DDwoR)
In the closed-mouth position, the intermediate zone of the articular disc was anteriorly displaced relative to the anterior slope of the condyle head. In the open-mouth position, the intermediate zone was still anteriorly displaced, which indicated no reduction. Subjects diagnosed with bilateral DDwoR or unilateral DDwoR, with or without DDwR for the other side, were assigned to the DDwoR group.
2.3. Cephalometric Evaluation
The cephalograms were shot by using an X-ray scanner (Morita, Osaka, Japan) with the standardized technique. Each patient was instructed to assume a natural head position and occlude in ICP without swallowing or chewing. Digital cephalograms were anonymized and then traced using Uceph software (version 961, Chengdu, China). The Frankfort horizontal plane (FH plane) was considered as the reference plane. A total of 24 measurements (Figure 2 and Table 1) were performed to evaluate the cranial base, vertical relationship, sagittal relationship, mandible position and morphology, and dental relationship, respectively. Sagittal skeletal pattern categorization was based on the ANB angle as follows: (1) skeletal class I (ANB < 1°), (2) skeletal class II (1° ≤ ANB ≤ 5°) and (3) skeletal class III (ANB > 5°). Two operators (C.Y. and X.X.) conducted the cephalometric tracing. The intra-observer and inter-observer reliability was verified before the study with a kappa coefficient >0.80 for all the measurement items.
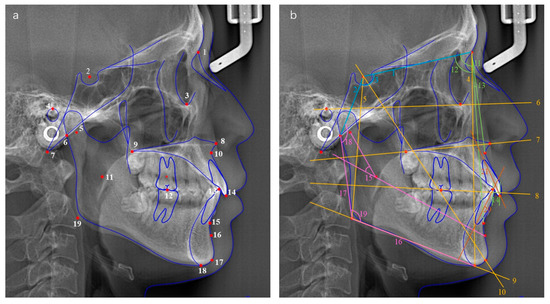
Figure 2.
(a) Cephalometric landmarks used in the study. (1) N, nasion; (2) S, sella; (3) Or, orbitale; (4) P, porion; (5) Dc point; (6) Ar, articulare; (7) Ba, basion; (8) ANS, anterior nasal spine; (9) PNS, posterior nasal spine; (10) A point; (11) Xi point; (12) first molar occlusal point; (13) lower incisor occlusal point; (14) upper incisor occlusal point; (15) B point; (16) Pm point; (17) Gn, gnathion; (18) Me, menton; (19) Go, gonion. (b) Planes and angles used in the study. Cranial base (blue): (1) anterior cranial base length, S–N; (2) posterior cranial base length, S–Ar; (3) saddle angle. Vertical relationship (yellow): (4) anterior facial height, N–Me; (5) posterior facial height, S–Go; (6) Frankfort plane; (7) palatal plane; (8) occlusal plane; (9) mandibular plane; (10) Y-axis. Sagittal relationship (green): (11) SNA; (12) SNB; (13) ANB; (14) Wits. Mandible position and morphology (pink): (15) mandibular arc angle, Dc–Xi–Pm; (16) mandibular body length; (17) ramus height; (18) articular angle; (19) gonial angle. Dental relationship (orange): (20) LI axis; (21) UI axis.

Table 1.
Cephalometric measurements and definitions.
2.4. Statistical Analysis
Statistical analyses were performed with Empowerstats (http://www.empowerstats.com, X&Y Solutions, Inc., Boston, MA, USA, assessed on 9 February 2022). Quantitative data are presented as mean ± standard deviation. Categorial data are presented as frequency and constituent ratio. The differences in quantitative data were evaluated through one-way analysis of variance (ANOVA). The differences in categorical variables were evaluated through R × C Chi-square test. Post-hoc comparisons were performed using the Student–Newman–Keuls (SNK) method. A stratified analysis was performed based on sex and sagittal skeletal pattern with the same statistical methods. An α error of 0.05 and a statistical power (1-β) of 80% was set for the statistical analysis. Based on a size effect estimated by posterior facial height, the required minimum sample size was set at 24 for each group.
3. Results
3.1. Demographic Information
The study enrolled 304 Chinese Han adults with TMDs (Figure 3), among whom 90 were categorized into the normal group, 99 into the DDwR group, and 115 into the DDwoR group (Table 2). The average age of the subjects was 30.8 ± 10.3 with no significant difference shown among the three groups (p = 0.131). Regarding sex, the DDwR and DDwoR groups showed higher proportions of females than the normal group (p < 0.001). The constituent ratio of different sagittal skeletal patterns in the three groups presented no significant difference (p = 0.126), while there was a slight rise in the proportion of class II in the DDwoR group.
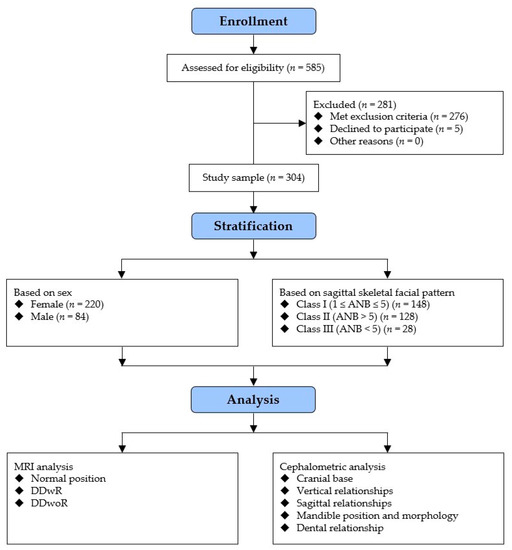
Figure 3.
Flow diagram of the study.

Table 2.
Demographic Information.
3.2. Overall Analysis
A total of 12 measurements showed statistical differences (Table 3 and Figure 4), including the posterior cranial base length (p = 0.013), posterior facial height (p < 0.001), facial height index (p < 0.001), Y-axis angle (p = 0.036), mandibular plane angle (p < 0.001), occlusal plane angle (p = 0.048), SNA (p = 0.006), SNB (p < 0.001), mandibular arc angle (p = 0.003), ramus height (p < 0.001), gonial angle (p = 0.034) and IMPA (p = 0.012).

Table 3.
Comparison of cephalometric measurements in normal, DDwR and DDwoR groups.
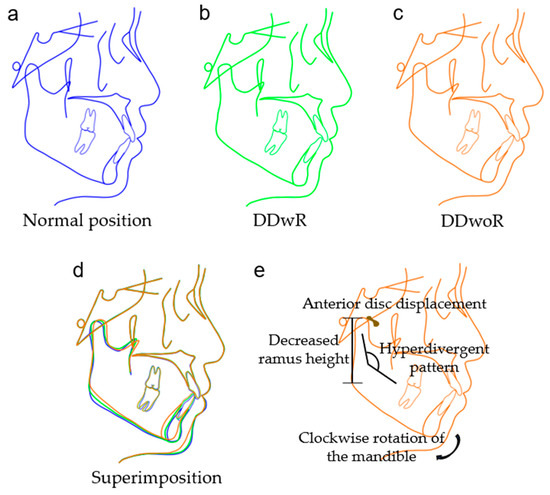
Figure 4.
Schematic figures showing morphological characteristics of TMD patients with different disc positions. (a) Normal group (blue); (b) DDwR group (green); (c) DDwoR group (orange); (d) superimposition of the three groups; (e) schematic illustration of the morphological changes in the DDwoR group compared with the normal group.
3.3. Stratified Analysis Based on Sex
Among the 220 female subjects studied, differences in posterior cranial base length (p = 0.013), posterior facial height (p < 0.001), facial height index (p < 0.001), mandibular plane angle (p = 0.013), SNB (p = 0.007), mandibular arc angle (p = 0.004) and ramus height (p = 0.001) were statistically different (Table 4 and Table S1). The results of the 84 male subjects were subtly different from the females. Measurements with statistical differences included posterior facial height (p = 0.047), facial height index (p = 0.034), Y-axis angle (p = 0.012), occlusal plane angle (p = 0.050), SNA (p = 0.003) and SNB (p = 0.005).

Table 4.
Stratified analysis based on sex.
3.4. Stratified Analysis Based on Sagittal Skeletal Pattern
Among the 148 class I subjects, measurements with statistical differences consisted of the posterior facial height (p = 0.009), facial height index (p = 0.012), ramus height (p = 0.011) and IMPA (p = 0.021) (Table 5 and Table S2). Among the 128 class II subjects, significant differences were observed in 10 measurements including the posterior cranial base length (p = 0.018), posterior facial height (p < 0.001), facial height index (p = 0.001), mandibular plane angle (p = 0.008), occlusal plane angle (p = 0.037), SNA (p = 0.020), SNB (p = 0.025), mandibular arc angle (p = 0.009), ramus height (p < 0.001), and IMPA (p = 0.012). Among the 28 class III subjects, significant differences were seen in the saddle angle (p = 0.042), SNA (p = 0.021), IMPA (p = 0.034) and FMIA (p = 0.033).

Table 5.
Stratified analysis based on sagittal skeletal pattern.
4. Discussion
The present study demonstrated that the differences in craniofacial morphology were associated with different disc positions. Only adult patients were included in order to avoid the influence of growth on the measurements. A total of 70.39% of the TMD patients included in the study were diagnosed with DD, which coincided with the proportions reported in the previous literature. A higher susceptibility to DD in females was suggested, with a significantly wider gap in the DDwR group and the DDwoR group. A slight increase in the proportion of skeletal class II patients with DDwoR could be observed, although the difference was not statistically significant.
Among the cranial base measurements, the posterior cranial base length was significantly smaller in the DD groups than in the normal group. This trend was common in all the stratified analyses, although in some subgroups no significant differences were present due to a limited sample volume. The posterior cranial base length, defined by measuring the sella to the articulare or basion, is closely related to skeletal pattern in terms of mandible position. The relationship between the cranial base and sagittal discrepancies has been widely discussed, but no consensus has yet been reached [21,22,23]. The smaller posterior cranial base possibly suggested a clockwise rotation of the mandible and a skeletal class II inclination, which was in line with the measurements for skeletal relationships in this study. The anterior cranial base length and saddle angle exhibited no significant difference among the three groups in the overall analysis. As for the stratified analysis, interestingly, a significant difference existed in the measurement for saddle angle in the class III subgroup.
Among the vertical relationship measurements, an insufficient posterior facial height and steeper mandibular plane angle were observed in the DD groups, in line with the previous literature [11]. The trend was more pronounced in the DDwoR group compared with the DDwR group. A clockwise rotation of the mandible, obtuse growth pattern of the mandible and suppressed ramus growth were possible causes of the unique manifestation. However, posterior facial height and mandibular plane angle were not significant indicators for DD in class III patients. A smaller Y-axis angle was shown in the DDwR group but not in the DDwoR group. Few studies have covered the Y-axis angle in measurements. Gidarakou et al. reported a larger Y-axis angle in symptomatic female patients with bilateral DDwoR in comparison with asymptomatic female volunteers [24]. Interestingly, the Y-axis angle was found to be statistically different in males but not in females, indicating that it might be a unique indicator for male TMD patients. A larger occlusal plane angle in the DDwoR group than in the DDwR group was found, especially in the male subgroup and the class II subgroup. Many previous studies focusing on female subjects reported no significance in the occlusal plane angle, which coincided with the findings in this study [25].
Among the sagittal relationship measurements, both the SNA and SNB were significantly smaller in the DDwoR group than in the DDwR and normal groups, indicating a retrusion of both the maxillae and mandible. A decrease in the SNB has been the consensus in most of the previous studies, but results on the SNA have varied [25,26,27]. A longitudinal study with a follow-up time of over three years by Carlos Flores-Mir et al. pointed out that TMJ disc abnormality was associated with reduced forward growth of the maxillae and mandible, which supported the results in this study [28]. The results of the stratified analysis might provide an explanation for the controversy surrounding the SNA, as this trend especially existed in males and was therefore not shown in the studies with only females included. Notably, the SNA and SNB use the cranial base as the reference to appraise the positions of the jaws and therefore the relationship between DD and the cranial base might influence the SNA and SNB angle. Similarly, the measurements of Wits might as well be misinterpreted owing to the change in the occlusal plane. It was suggested that more references for assessments, such as the bisector of the palatal plane to the mandibular plane angle, should be applied in the sagittal relationship appraisal [29].
Among the mandible position and morphology measurements, differences were observed in the mandibular arc angle, ramus height and gonial angle. The findings in this study suggested the mandibular body length remained while the ramus height descended. One main theory for the ramus height decrease was that the ramus would undergo osseous changes and compromise its height under abnormal mechanical loading caused by DD, as abundant studies have revealed the effectiveness of mechanical forces in affecting bone growth and remodeling [30,31,32]. An obtuse mandibular growth pattern in the DDwoR group was exhibited by a smaller mandibular arc angle and larger gonial angle. The rotational change in the mandible caused by the shortening ramus height and obtuse mandibular growth pattern might explain the hyperdivergent facial profile of DD patients. Differences in mandible position and morphology were especially significant in female and class II subgroups.
Among the dental relationship measurements, only the IMPA was statistically different and the decreasing trend of the IMPA existed in all subgroups. The FMIA was similar in class I and II, which indicated that the difference in IMPA might be attributed to the distinction of the FMA. Interestingly, the FMIA was significantly larger in the skeletal class III group. Moon et al. reported a similar change in the FMIA in 66 women with an oversized mandible and TMJ internal disarrangement [25]. The decreased FMIA indicated that lingual-inclined lower incisors, as a compensatory change to combat the skeletal class III relationship, might be a unique feature in class III patients with DD.
TMDs are reported to appear remarkably more frequent and severe in females than in males [33]. The sex-related difference is an intriguing issue from a biopsychosocial view. Different muscle fiber compositions and strengths could influence the stabilization of the articular disc [34]. Estrogen metabolism might also greatly contribute to the osseous changes of the condyle and enhance pain sensibility [35,36]. As they are closely related to abnormal oral parafunctions such as grinding and clinching, or sleep disorders, some psychological and social indicators might be unneglectable topics in studying these differences [37]. In this study, sex-related morphological changes in DD were significant. Mandibular morphological measurements including mandibular arc angle and ramus height were highly specific in females, indicating the crucial effects on mandibular bone growth and remodeling. In males, the Y-axis angle, occlusal plane angle and SNA were specific, concerning the growth direction of the maxillae and mandible.
Several studies have presented a debated view on the susceptibility to TMDs in different skeletal malocclusions [38]. Studies by Abrahamsson et al. and Paunonen et al. both reported that orthognathic surgeries could have a positive effect on TMDs, reflecting the correlation between skeletal malocclusion and TMDs [39,40]. Skeletal facial patterns greatly influence the osseous and muscular transmission of occlusal force in the stomatognathic system, therefore influencing the adaptive remodeling of the temporomandibular joint [41]. The results of this study agreed with the viewpoint that sagittal skeletal patterns were related with DD, as DD patients of different sagittal skeletal patterns had different indicators of craniofacial morphology. Class II patients exhibited the most significant indicators. A clockwise rotation of the mandible, reflected by a larger mandibular plane angle, larger occlusal angle and smaller SNB, is the typical feature of class II DD patients. In class III patients, the saddle angle and FMIA are the unique indicators. The FMIA, which suggested compensatory lingual-inclined lower incisors, drew more attention to the occlusal interference in class III DD patients.
The main purpose of this study was the stratified analysis design based on sex and sagittal skeletal pattern, rendering the discovery of statistically different parameters in different subgroups. Relatively more cephalometric measurements than previous studies were covered in this study in order to give clinicians and researchers a comprehensive view on the craniofacial morphology of DD patients. A limitation of this study is the relatively small sample size of class III subjects owing to imbalanced proportions of visiting patients. Owing to the study design, which is a monocentric cross-sectional study, the generalizability of the findings might be impaired and causal relationships between DD and morphological differences remain unreached. Multicentric and longitudinal study design is anticipated for the verification of the conclusions. Some factors including local or systemic comorbidities, medication and socio-demographic characteristics might represent a confounding source that influences disc positions, where further stratification analysis would be interesting. As the lateral cephalograms were unable to exhibit craniofacial asymmetry, the current study did not distinguish lateral from bilateral lesions. The development of three-dimensional cephalometric methods might help discover asymmetric morphological features in lateral lesions.
5. Conclusions
TMD patients with different disc positions had distinctive craniofacial morphology. All of the five aspects studied in this study showed significant differences, namely the cranial base, vertical relationship, sagittal relationship, mandible position and morphology, and dental relationship. The sex and skeletal sagittal pattern could influence the pattern of difference. Mandibular morphological measurements were highly remarkable in females, while the growth direction of the maxillae and mandible was especially concerned in males. Clockwise rotation is a notable feature in class II patients. In class III patients, incisal interference owing to the compensatory change might be especially cautioned. These measurements provided evidence for the sex-related and sagittal-skeletal-pattern-related differences in DD mechanism and might assist in the detection and discrimination of potential DD patients in clinical settings.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12020652/s1, Table S1: Stratified analysis based on sex; Table S2: Stratified analysis based on sagittal skeletal pattern.
Author Contributions
Conceptualization, C.Y. and X.X.; methodology, C.Y. and X.X.; software, C.Y. and P.F.; validation, C.Y., J.Z. and Q.C.; formal analysis, C.Y. and P.F.; investigation, C.Y. and J.Z.; resources, J.W. and X.X.; data curation, C.Y. and P.F.; writing—original draft preparation, C.Y.; writing—review and editing, J.W. and X.X.; visualization, X.X.; supervision, J.W. and X.X.; project administration, J.W.; funding acquisition, J.W. and X.X. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Technology Innovation Project of Science and Technology Bureau of Chengdu (Grant No. 2022-YF05-01691-SN), National Natural Science Foundation of China (Grant No. 82271019, 81970967), Sichuan Health Commission Medical Science and Technology Program (Grant No. 21ZD003), Research and Develop Program, West China Hospital of Stomatology Sichuan University (Grant No. RD-03-202101) and Major Special Science and Technology Project of Sichuan Province (Grant No. 2022ZDZX0031).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of West China Hospital of Stomatology, Sichuan University (No. WCHSIRB-CT-2020-418, 31 December 2020).
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author upon reasonable request.
Acknowledgments
The authors acknowledged the team of Uceph software (Uceph, Chengdu, China) for the software assistance in cephalometric evaluation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ohrbach, R.; Dworkin, S.F. The Evolution of TMD Diagnosis: Past, Present, Future. J. Dent. Res. 2016, 95, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Scrivani, S.J.; Keith, D.A.; Kaban, L.B. Temporomandibular disorders. N. Engl. J. Med. 2008, 359, 2693–2705. [Google Scholar] [CrossRef] [PubMed]
- Anastassaki Köhler, A.; Hugoson, A.; Magnusson, T. Prevalence of symptoms indicative of temporomandibular disorders in adults: Cross-sectional epidemiological investigations covering two decades. Acta Odontol. Scand. 2012, 70, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Tanaka, E.; Tanaka, M.; Watanabe, M.; Del Pozo, R.; Tanne, K. Influences of occlusal and skeletal discrepancies on biomechanical environment in the TMJ during maximum clenching: An analytic approach with the finite element method. J. Oral Rehabil. 2001, 28, 888–894. [Google Scholar] [CrossRef]
- Ingawalé, S.; Goswami, T. Temporomandibular joint: Disorders, treatments, and biomechanics. Ann. Biomed. Eng. 2009, 37, 976–996. [Google Scholar] [CrossRef]
- Coombs, M.C.; Petersen, J.M.; Wright, G.J.; Lu, S.H.; Damon, B.J.; Yao, H. Structure-Function Relationships of Temporomandibular Retrodiscal Tissue. J. Dent. Res. 2017, 96, 647–653. [Google Scholar] [CrossRef]
- Naeije, M.; Te Veldhuis, A.H.; Te Veldhuis, E.C.; Visscher, C.M.; Lobbezoo, F. Disc displacement within the human temporomandibular joint: A systematic review of a ‘noisy annoyance’. J. Oral Rehabil. 2013, 40, 139–158. [Google Scholar] [CrossRef]
- Bósio, J.A.; Burch, J.G.; Tallents, R.H.; Wade, D.B.; Beck, F.M. Lateral cephalometric analysis of asymptomatic volunteers and symptomatic patients with and without bilateral temporomandibular joint disk displacement. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 248–255. [Google Scholar] [CrossRef]
- Brand, J.W.; Nielson, K.J.; Tallents, R.H.; Nanda, R.S.; Currier, G.F.; Owen, W.L. Lateral cephalometric analysis of skeletal patterns in patients with and without internal derangement of the temporomandibular joint. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 121–128. [Google Scholar] [CrossRef]
- Shu, C.; Xiong, X.; Huang, L.; Liu, Y. The relation of cephalometric features to internal derangements of the temporomandibular joint: A systematic review and meta-analysis of observational studies. Orthod. Craniofac. Res. 2021, 24, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Roosenboom, J.; Hens, G.; Mattern, B.C.; Shriver, M.D.; Claes, P. Exploring the Underlying Genetics of Craniofacial Morphology through Various Sources of Knowledge. BioMed Res. Int. 2016, 2016, 3054578. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.-B.; Wan, Y.-D.; Xiao, C.-Q.; Li, Y.-Q.; Zhang, Y.-Y.; An, Y.; Xiong, X. Craniofacial Morphology of Orthodontic Patients with and without Temporomandibular Disorders: A Cross-Sectional Study. Pain Res. Manag. 2022, 2022, 9344028. [Google Scholar] [CrossRef] [PubMed]
- Aboalnaga, A.A.; Amer, N.M.; Elnahas, M.O.; Salah Fayed, M.M.; Soliman, S.A.; ElDakroury, A.E.; Labib, A.H.; Fahim, F.H. Malocclusion and Temporomandibular Disorders: Verification of the Controversy. J. Oral Facial Pain Headache 2019, 33, 440–450. [Google Scholar] [CrossRef]
- Amer, N.M.; Aboalnaga, A.A.; Salah Fayed, M.M.; Labib, A.H. Transverse Malocclusion and Temporomandibular Disorders: Verification of the Controversy. J. Oral Facial Pain Headache 2019, 33, 355–361. [Google Scholar] [CrossRef]
- Roccuzzo, A.; Molinero-Mourelle, P.; Ferrillo, M.; Cobo-Vazquez, C.; Sanchez-Labrador, L.; Ammendolia, A.; Migliario, M.; de Sire, A. Type I Collagen-Based Devices to Treat Nerve Injuries after Oral Surgery Procedures. A Systematic Review. Appl. Sci. 2021, 11, 3927. [Google Scholar] [CrossRef]
- Ferrillo, M.; Marotta, N.; Giudice, A.; Calafiore, D.; Curci, C.; Fortunato, L.; Ammendolia, A.; de Sire, A. Effects of Occlusal Splints on Spinal Posture in Patients with Temporomandibular Disorders: A Systematic Review. Healthcare 2022, 10, 739. [Google Scholar] [CrossRef]
- Xiong, X.; Ye, Z.; Tang, H.; Wei, Y.; Nie, L.; Wei, X.; Liu, Y.; Song, B. MRI of Temporomandibular Joint Disorders: Recent Advances and Future Directions. J. Magn. Reson. Imaging 2021, 54, 1039–1052. [Google Scholar] [CrossRef]
- Fan, P.-d.; Xiong, X.; Cheng, Q.-Y.; Xiang, J.; Zhou, X.-M.; Yi, Y.-T.; Wang, J. Risk estimation of degenerative joint disease in temporomandibular disorder patients with different types of sagittal and coronal disc displacements: MRI and CBCT analysis. J. Oral Rehabil. 2023, 50, 12–23. [Google Scholar] [CrossRef]
- Bag, A.K.; Gaddikeri, S.; Singhal, A.; Hardin, S.; Tran, B.D.; Medina, J.A.; Curé, J.K. Imaging of the temporomandibular joint: An update. World J. Radiol. 2014, 6, 567–582. [Google Scholar] [CrossRef]
- Dhopatkar, A.; Bhatia, S.; Rock, P. An investigation into the relationship between the cranial base angle and malocclusion. Angle Orthod. 2002, 72, 456–463. [Google Scholar] [CrossRef]
- Chin, A.; Perry, S.; Liao, C.; Yang, Y. The relationship between the cranial base and jaw base in a Chinese population. Head Face Med. 2014, 10, 31. [Google Scholar] [CrossRef] [PubMed]
- Gong, A.; Li, J.; Wang, Z.; Li, Y.; Hu, F.; Li, Q.; Miao, D.; Wang, L. Cranial base characteristics in anteroposterior malocclusions: A meta-analysis. Angle Orthod. 2016, 86, 668–680. [Google Scholar] [CrossRef]
- Gidarakou, I.K.; Tallents, R.H.; Kyrkanides, S.; Stein, S.; Moss, M.E. Comparison of skeletal and dental morphology in asymptomatic volunteers and symptomatic patients with bilateral disk displacement without reduction. Angle Orthod. 2004, 74, 684–690. [Google Scholar] [CrossRef] [PubMed]
- Moon, B.-S.; Yang, I.-H.; Ahn, S.-J. Dentofacial characteristics of women with oversized mandible and temporomandibular joint internal derangement. Angle Orthod. 2011, 81, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Jeon, D.-M.; Jung, W.-S.; Mah, S.-J.; Kim, T.-W.; Ahn, S.-J. The effects of TMJ symptoms on skeletal morphology in orthodontic patients with TMJ disc displacement. Acta Odontol. Scand. 2014, 72, 776–782. [Google Scholar] [CrossRef]
- Ahn, S.-J.; Baek, S.-H.; Kim, T.-W.; Nahm, D.-S. Discrimination of internal derangement of temporomandibular joint by lateral cephalometric analysis. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 331–339. [Google Scholar] [CrossRef]
- Flores-Mir, C.; Nebbe, B.; Heo, G.; Major, P.W. Longitudinal study of temporomandibular joint disc status and craniofacial growth. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 324–330. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Miani, A.; Tartaglia, G.M. The use of linear and angular measurements of maxillo-mandibular anteroposterior discrepancies. Clin. Orthod. Res. 1999, 2, 34–41. [Google Scholar] [CrossRef]
- Yuan, W.; Wu, Y.; Zhou, X.; Zheng, Y.; Wang, J.; Liu, J. Comparison and applicability of three induction methods of temporomandibular joint osteoarthritis in murine models. J. Oral Rehabil. 2021, 49, 430–441. [Google Scholar] [CrossRef]
- Bryndahl, F.; Eriksson, L.; Legrell, P.E.; Isberg, A. Bilateral TMJ disk displacement induces mandibular retrognathia. J. Dent. Res. 2006, 85, 1118–1123. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Wu, N.; Wang, J.; Wang, Y.; Wu, M.; Wang, H. Role of HIF-2α/NF-κB pathway in mechanical stress-induced temporomandibular joint osteoarthritis. Oral Dis. 2021, 28, 2239–2247. [Google Scholar] [CrossRef]
- Bueno, C.H.; Pereira, D.D.; Pattussi, M.P.; Grossi, P.K.; Grossi, M.L. Gender differences in temporomandibular disorders in adult populational studies: A systematic review and meta-analysis. J. Oral Rehabil. 2018, 45, 720–729. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-H.; Lee, K.M.; Auh, Q.S. MRI-Based Assessment of Masticatory Muscle Changes in TMD Patients after Whiplash Injury. J. Clin. Med. 2021, 10, 1404. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro-Dasilva, M.C.; Fillingim, R.B.; Wallet, S.M. Estrogen-Induced Monocytic Response Correlates with TMD Pain: A Case Control Study. J. Dent. Res. 2017, 96, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chao, Y.; Wan, Q.; Zhu, Z. The possible role of estrogen in the incidence of temporomandibular disorders. Med. Hypotheses 2008, 71, 564–567. [Google Scholar] [CrossRef]
- Ye, C.; Xiong, X.; Zhang, Y.; Pu, D.; Zhang, J.; Du, S.; Wang, J. Psychological Profiles and Their Relevance with Temporomandibular Disorder Symptoms in Preorthodontic Patients. Pain Res. Manag. 2022, 2022, 1039393. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.C.; Yap, A.U.; Türp, J.C. Prevalence of temporomandibular disorders in patients seeking orthodontic treatment: A systematic review. J. Oral Rehabil. 2020, 47, 270–280. [Google Scholar] [CrossRef]
- Abrahamsson, C.; Henrikson, T.; Nilner, M.; Sunzel, B.; Bondemark, L.; Ekberg, E.C. TMD before and after correction of dentofacial deformities by orthodontic and orthognathic treatment. Int. J. Oral Maxillofac. Surg. 2013, 42, 752–758. [Google Scholar] [CrossRef]
- Paunonen, J.; Helminen, M.; Sipilä, K.; Peltomäki, T. Temporomandibular disorders in Class II malocclusion patients after surgical mandibular advancement treatment as compared to non-treated patients. J. Oral Rehabil. 2019, 46, 605–610. [Google Scholar] [CrossRef]
- Rowlerson, A.; Raoul, G.; Daniel, Y.; Close, J.; Maurage, C.-A.; Ferri, J.; Sciote, J.J. Fiber-type differences in masseter muscle associated with different facial morphologies. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 37–46. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).