Abstract
Background: Obesity has been associated with increased incidence and severity of various cardiovascular risk factors and increased risk for stroke. However, the evidence of its effect on outcomes in stroke victims have been equivocal. We aimed to investigate the distribution of BMI in a nation-wide cohort of individuals, admitted for a stroke, and the relationship between BMI and in-hospital mortality. Methods: Data from the U.S. National Inpatient Sample (NIS) was collected, to identify hospitalizations for stroke, between October 2015 and December 2016. The patients were sub-divided into six groups based on their BMI: underweight, normal weight, overweight, obese I, obese II and extremely obese groups. Various sociodemographic and clinical parameters were gathered, and incidence of mortality and the length of hospital stay were analyzed. Multivariable analysis was performed to identify independent predictors of in-hospital mortality. Results: A weighted total of 84,185 hospitalizations for stroke were included in the analysis. The approximate mean patients aged was 65.5 ± 31 years, the majority being female (55.3%) and white (63.1%). The overall in-hospital mortality during the study period was 3.6%. A reverse J-shaped relationship between the body mass index and in-hospital mortality was documented, while patients with elevated BMI showed significantly lower in-hospital mortality compared to the underweight and normal weight study participants, 2.8% vs. 7.4%, respectively, p < 0.001. Age and several comorbidities, as well as the Deyo Comorbidity Index, were found to predict mortality in a multivariable analysis. Conclusion: A reverse J-shaped relationship between body mass index and in-hospital mortality was documented in patients admitted for a stroke in the U.S. during the study period. The above findings support the existence of an “obesity paradox” in patients hospitalized following a stroke, similar to that described in other cardiovascular conditions.
1. Introduction
Constantly growing number of people are affected by obesity worldwide. According to a recent report by the World Health Organization, the rate of obesity has tripled since the 70s, and by 2016 over 1.9 billion adults (31%) were overweight, of them 650 million (13%) were obese [1]. The prevalence of obesity in the U.S. has increased significantly in the last few decades, leading to significant social, clinical and economic implications [2,3,4,5,6].
Obesity and stroke, both reaching epidemic proportions, are clearly associated. Based on recent data, up to 25% of adults over the age of 25 are expected to experience a stroke during their lifetime [7]. Worldwide, stroke is a leading cause of long-term disability [8] and is responsible for 5.8 million death cases yearly [9]. Obesity is also a well-established risk factor for cerebrovascular disease, and the body-mass-index (BMI) has a nearly linear association with the risk for ischemic stroke [10,11,12,13,14].
Numerous studies linked obesity with higher incidence and increased severity of several cardiovascular risk factors, including increased risk for stroke. However, studies looking into the effect of obesity on outcomes in stroke victims have produced conflicting results. Several studies showed favorable outcomes, in terms of mortality, in overweight and obese stroke patients [15,16,17,18,19], including in those who suffered from a hemorrhagic stroke [20,21,22], supporting the theory of an “obesity paradox” in these patients. However, other studies have shown a detrimental effect of obesity on post-stroke longevity [23], and identified age as a modifying factor with higher mortality risk in younger obese stroke survivors and a lower risk in older ones [24]. As the impact of obesity on stroke outcomes is still under debate, the aim of this study was to describe the patient characteristics and BMI distribution in a nation-wide cohort of patients, admitted for stroke in the U.S., and the association between BMI and mortality as well as length of hospital stay.
2. Methods
A detailed description of the study methods and the used dataset has been provided previously by our group [25].
2.1. Data Source
The data were collected from the National Inpatient Sample (NIS), the Healthcare Cost and Utilization Project (HCUP), and Agency for Healthcare Research and Quality (AHRQ) [26,27]. The NIS dataset represents an approximate 20% sample of all inpatient hospitalizations in the U.S. [28]. The database includes various patient- and hospital-level characteristics such as patient demographics, discharge diagnoses and procedural diagnoses, comorbidities and length of hospital stay (LOS). Hospital level factors include the hospital geographic region, teaching status, and bed size. National estimates are calculated using the patient-level sampling weights, provided by the HCUP.
For this study, we collected data for U.S. hospitalizations between October 2015 and December 2016. The ICD-10 coding system (International Classification of Diseases, 10th Revision, Clinical Modification—ICD-10-CM) was used from October of 2015 and thereafter to report procedural and clinical diagnoses in the NIS database. The reason we included only the data coded with ICD-10 system is that the ICD-10 codes include individual codes for BMI values and ranges.
2.2. Study Population and Variables
We included patients aged 18 years and above, with a primary diagnosis of a stroke based on one of the I63.XXX ICD-10-CM codes, who had a BMI code documentation in the secondary diagnoses. As we have described our group’s prior publication [25], we have categorized the study population into six BMI subgroups: using BMI ≤ 19 kg/m2, the under-weight group; BMI 20–25 kg/m2, normal-weight group; BMI 26–30 kg/m2, over-weight group; BMI 31–35 kg/m2, obese I group; BMI 36–39 kg/m2, obese II group; BMI ≥40 kg/m2, extremely obese group.
Different demographic parameters were obtained from the NIS dataset, including: age, sex, and race. Prior comorbidities were identified utilizing the appropriate ICD-10 codes among the secondary diagnoses in the dataset. Deyo-Charlson Comorbidity Index (Deyo-CCI) was calculated for each patient, using the 17 comorbidity conditions [29] (Appendix A Table A1 includes all the Deyo-CCI codes). The index has been used extensively in clinical studies, utilizing administrative databases, with good prognostic validity in regards to short- and long-term outcomes [30,31]. Of notice, we used age groups in the analysis, instead of using age as a continuous variable since all the patients aged 90 and above are listed as 90 years old in the database. We wanted to include the entire population of patients with stroke, not excluding the nonagenarians, hence we were forced to use age groups for accurate statistical analysis. We did include the “approximate mean age” in the results section and the abstract, however all the statistical analyses were performed with age groups for improved accuracy. The primary outcome in this study was in-hospital mortality. Length of hospital stay was the secondary outcome analyzed.
2.3. Statistical Analysis
We used the Wilcoxon Rank Sum test and chi-square (χ2) test and to compare continuous and categorical variables, respectively. The NIS dataset includes discharge sample weights, calculated within each sampling stratum as the ratio of discharges in the universe to discharges in the sample [32]. We have created a weighted logistic regression model to identify independent predictors of mortality during the hospitalization. Candidate variables included various patient clinical and demographic characteristics, Deyo-CCI and hospital-level factors. Variables, associated with primary and secondary outcomes were included in our final multivariable regression model. For all statistical analyses, we utilized SAS® software version 9.4 (SAS Institute Inc., Cary, NC, USA). A p-value < 0.05 was considered statistically significant.
3. Results
3.1. Study Cohort
A total of 16,837 hospitalizations for stoke in the U.S. were included in the analysis. After implementation of the weighting method, this hospitalizations sample represented an estimated total of 84,185 hospitalizations for stroke. There was a female predominance in the study population (55.3%), and the approximate mean age was 65.5 ± 31 years.
The majority of the study population (63.1%) was white, 56.9% had Medicare coverage (Table 1). With regards to the clinical characteristics, 38% had history of diabetes mellitus, 67% had essential hypertension, 10% had peripheral vascular disease and 23% had a history of atrial fibrillation or flutter. The median BMI in the study was 34 (IQR: 29–41), while 82.4% of the patients had BMI above normal (>25 kg/m2).

Table 1.
Baseline Characteristics of the Study Population (total and per BMI groups).
3.2. Patients’ Characteristics and in-Hospital Outcomes in the Different BMI Groups
Table 1 includes the baseline characteristics of the study cohort, divided into the six predefined BMI subgroups. The BMI distribution varied significantly within the different income percentiles and country regions (p < 0.001). Female predominance was noted in the underweight and in patients with BMI ≥ 40 (extremely obese). Younger age and increased prevalence of diabetes, hypertension and heart failure were observed in the obese patient subgroups (Table 1).
Of the total population admitted for a stroke, 8.7% received thrombolytic therapy. Obese patients had higher chances to receive thrombolytic therapy during the hospitalization compared to underweight and normal weight patients, 9.3% vs. 6.2%, respectively (p < 0.001). Only 2.8% of the total study population underwent mechanical thrombectomy and 1.3% underwent in hospital carotid endarterectomy.
The average length of stay in the hospital was 5.64 ± 0.07 days. Figure 1 shows the relationship between BMI and the length of hospitalization in the study population. The correlation between BMI and LOS was a reverse J shape in nature with shorter hospital stay in overweight and obese patients, p < 0.001.
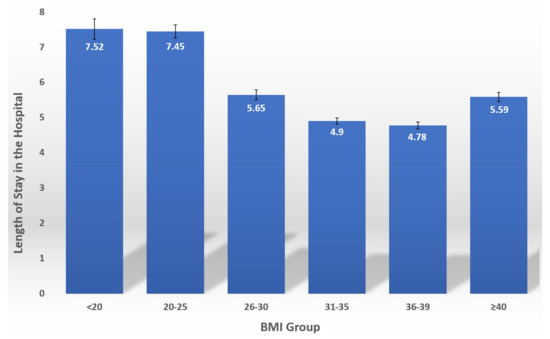
Figure 1.
The relationship between BMI and the length of hospitalization in the study.
The rate of in-hospital mortality in patients hospitalized with a stroke was documented at 3.6%. Figure 2 shows the correlation between BMI and in-hospital mortality in the study population. A reverse J-shaped relationship between the BMI and the in-hospital mortality was observed, with higher mortality in underweight and normal weight patients, p < 0.001.
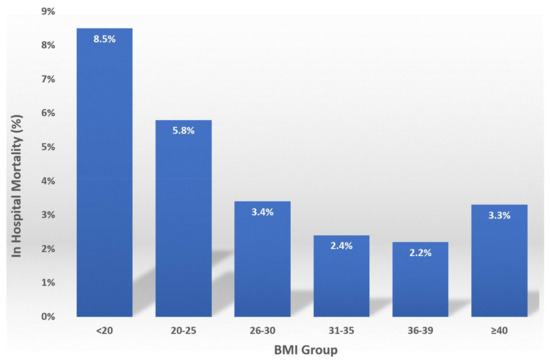
Figure 2.
The relationship between BMI and in-hospital mortality in the study.
3.3. Predictors of in-Hospital Mortality
Several parameters were found to significantly increase the odds of in-hospital mortality in an unadjusted analysis (Table 2). These included: age, white race, personal history of hypertension, renal failure, peripheral vascular disease, heart failure and atrial fibrillation/flutter (all with p < 0.01). Higher BMI as well as diabetes were associated with reduced mortality in a univariate analysis.

Table 2.
Univariate Analysis for Predictors of In-Hospital Mortality.
After adjusting for potential confounders, most of the above (except peripheral vascular disease) remained an independent predictor of in-hospital mortality in a multivariable analysis (Table 3). Higher BMI and diabetes were independent predictors of improved survival. Deyo Comorbidity index of ≥2 was also an independent predictor of mortality in patients hospitalized for stroke, OR-2.39 (1.94–2.94), p < 0.001.

Table 3.
Multivariable Analysis for Predictors of In-Hospital Mortality.
4. Discussion
Using the NIS database, we analyzed a weighted total of 84,185 hospitalizations for a stroke, during the study period of Oct. 2015 to Dec. 2016. This nation-wide data analysis showed a reverse J-shaped association between the BMI and mortality in hospital, in the study population. Elevated BMI was found to be an independent predictor of lower in-hospital mortality and length of hospital stay in patients admitted for a stroke during the study period.
In this study, we aimed to analyze the relationship between BMI and in-hospital outcomes in a nation-wide population of patients, admitted in the US following a cerebrovascular event, in order to overcome the potential biases of the prior, smaller studies. In addition, we wanted to improve the differentiation between the different obese patients BMI subgroups, dividing them into mild (30 < BMI ≤ 35), moderate (35 < BMI < 40) and extremely obese (BMI ≥ 40) groups. The different sociodemographic and clinical characteristics of our study population were comparable with prior publications on stroke patients as to their age and comorbidities such as hypertension, diabetes mellitus, atrial fibrillation and others [16,19,24].
A recent systematic review of 25 studies (299,750 patients) showed that a vast majority of these studies reported a survival benefit for obese study participants, suffering from a stroke. However, due to methodological limitations, study design, lacking adjustment for comorbidities, selection bias and survival bias, it was difficult to draw firm conclusions as to the real-world relationship between BMI and outcomes in post stroke patients [9].
The effect of elevated BMI on the risk for stroke can be explained by elevated prevalence of risk factors such as diabetes, hyperlipidemia and hypertension in the obese patients. However, prospective studies did not show that these co-morbidities necessarily modify the relationship between BMI and stroke [11,12]. In our study increased BMI was documented to have an independent, positive effect on the mortality, despite an almost doubling of the diabetes prevalence in patients with elevated BMI, when compared to the underweight and normal weight patients. The positive effect of the BMI possibly drove the counterintuitive correlation between diabetes and improved survival, documented in this study OR-0.76 (0.69–0.83), p < 0.001.
The data presented here reveals a reverse J-shaped relationship between the body mass index and in-hospital mortality in stroke patients, while the mild and moderately obese patient subgroups (BMI 31–39) exhibited the lowest in-hospital mortality in this study. Prior studies have suggested that the “obesity paradox”, described in various cardiovascular conditions including in myocardial infarction, heart failure and sudden death, may apply to patients admitted with a stroke, resulting in lower mortality in obese patients [15,16,17,18,19]. Importantly, many of the prior investigations clustered all patients with BMI > 30 into one study group, showing improved outcomes. We have further subdivided the obese patients in three groups, as described in the methods section. We documented decreased mortality only in the first two of these subgroups (30 < BMI ≤ 35 and 35 < BMI < 40), while in extremely obese patients (BMI ≥ 40), the documented mortality was higher than in patients with BMI between 31–39 kg/m2 (Figure 2).
Interestingly, patients suffering from overweight and obesity were shown to be younger, a fact that could have theoretically contributed to better survival in these patients. Niedziela et al, has described this observation in the past, showing that in 20 out of 26 reports included in his meta-analysis of the “obesity paradox” in myocardial infarction studies, patients suffering from overweight and obesity were younger compared to patients in other subgroups [33].
Several protective pathophysiological mechanisms have been suggested to play a role in improving the survival of critically ill patients, including the potential benefit of nutritional reserves in obese patients [34,35,36] and neurohormonal mechanisms linked to higher leptin levels in obese individuals [37,38,39]. We assume that similar mechanisms may have played a role in stroke patients who are exposed to an intense continuous metabolic stress associated with the acute cerebrovascular event and hospitalization. As expected, patients with higher body mass index suffered from high prevalence of cardiovascular risk factors such as HTN and DM. It seems that the adverse effects of these cardiovascular risk factors on patients’ outcomes are counterbalanced by the protective mechanisms that improve the survival in obese individuals hospitalized with a stroke, many of whom suffer from HTN and DM.
This implication of obesity and improved survival after a stroke should be by no means interpreted as supporting weight gain. Elevated body weight index has been documented to be an independent risk factor for several cardiovascular conditions such as ischemic heart disease, myocardial infarction, heart failure, cardiac arrhythmia (both atrial and ventricular), sudden cardiac arrest and stroke [35,40]. The evidence in favor of preventive strategies to fight obesity is unequivocal and our findings should not be misinterpreted as suggesting otherwise.
Our study has several limitations. The National Inpatient Sample database is an administrative retrospective database, containing discharge-level records, hence, it is susceptible to potential coding errors. The lack of patient identifiers in the NIS database does not allow us to analyze other outcomes such as 30-day mortality. We could only document events occurring during the hospitalization, with no longer term follow up. We also cannot rule out that some of the hospitalizations were “readmissions” of the same patients with another cerebrovascular event. Several important parameters are not collected into the NIS database such as additional patient characteristics, chronic medical therapy, laboratory tests etc. Therefore, we cannot completely rule out residual confounding of the correlation we observed in this study. These limitations are counterbalanced by the nation-wide, real-world nature of the data, lack of selection bias and the absence of reporting bias introduced by selective publication from specialized centers.
In conclusion, a reverse J-shaped correlation between the body mass index and in-hospital mortality was documented in patients hospitalized for a stroke in the U.S. during this study period. The presented findings support the existence of an “obesity paradox” in patients hospitalized following a stroke, similar to that described in other cardiovascular conditions.
Author Contributions
Conceptualization, G.R., G.E.-G. and O.A.; methodology, G.R., G.E.-G. and O.A.; formal analysis, G.R. and G.E.-G.; investigation, G.R. and G.E.-G.; resources, G.R. and G.E.-G.; data curation, G.R. and G.E.-G.; writing—original draft preparation, G.R., G.E.-G. and G.M.; writing—review and editing, I.M., E.K.H., J.N.R., S.C., A.R., E.Y.B. and O.A.; supervision, O.A.; project administration, O.A.; funding acquisition, O.A. and E.Y.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The data in the National Inpatient Sample dataset is de-identified; therefore, the Human Research Committee exempted this study from institutional review.
Informed Consent Statement
Patient consent was waived in this nation-wide de-identified database by the Healthcare Cost and Utilization Project (HCUP).
Data Availability Statement
The Healthcare Cost and Utilization Project (HCUP) Data Use Agreement doesn’t allow us to make the data from the NIS database, used for this study, available to other. The NIS database is available for purchase by the public and our detailed and transparent description of methods used for the data analysis allows anyone who wishes to do so to reproduce our results.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
ICD-10 codes used in the study.
Table A1.
ICD-10 codes used in the study.
| Medical Condition. | ICD-10 CM Codes | Score |
|---|---|---|
| Myocardial infarction | I22.xx, I21.xx, I25.2 | 1 |
| Congestive heart failure | I09.9, I11.0, I13.0, I13.2, I25.5, I42.0, I42.5-I42.9, I43.x, I50.x, P29.0 | 1 |
| Peripheral vascular disease | I70.x, I71.x, I73.1, I73.8, I73.9, I77.1, I79.0, I79.2, K55.1, K55.8, K55.9, Z95.8, Z95.9 | 1 |
| Cerebrovascular disease | G45.x, G46.x, H34.0, I60.x-I69.x | 1 |
| Dementia | F00.x-F03.x, F05.1, G30.x, G31.1 | 1 |
| Chronic pulmonary disease | I27.8, I27.9, J40.x-J47.x, J60.x-J67.x, J68.4, J70.1, J70.3 | 1 |
| Rheumatologic disease | M05.x, M06.x, M31.5, M32.x-M34.x, M35.1, M35.3, M36.0 | 1 |
| Peptic ulcer disease | K25.x-K28.x | 1 |
| Mild liver disease | B18.x, K70.0-K70.3, K70.9, K71.3-K71.5, K71.7, K73.x, K74.x, K76.0, K76.2-K76.4, K76.8, K76.9, Z94.4 | 1 |
| Diabetes | E10.0, E10.l, E10.6, E10.8, E10.9, E11.0, E11.1, E11.6, E11.8, E11.9, E12.0, E12.1, E12.6, E12.8, E12.9, E13.0, E13.1, E13.6, E13.8, E13.9, E14.0, E14.1, E14.6, E14.8, E14.9 | 1 |
| Diabetes with chronic complications | E10.2-E10.5, E10.7, E11.2-E11.5, E11.7, E12.2-E12.5, E12.7, E13.2-E13.5, E13.7, E14.2-E14.5, E14.7 | 2 |
| Hemiplegia or paraplegia | G04.1, G11.4, G80.1, G80.2, G81.x, G82.x, G83.0-G83.4, G83.9 | 2 |
| Renal disease | I12.0, I13.1, N03.2-N03.7, N05.2-N05.7, N18.x, N19.x, N25.0, Z49.0-Z49.2, Z94.0, Z99.2 | 2 |
| Any malignancy including leukemia and lymphoma | C00.x-C26.x, C30.x-C34.x, C37.x-C41.x, C43.x, C45.x-C58.x, C60.x-C76.x, C81.x-C85.x, C88.x, C90.x-C97.x | 2 |
| Moderate or severe liver disease | I85.0, I85.9, I86.4, I98.2, K70.4, K71.1, K72.1, K72.9, K76.5, K76.6, K76.7 | 3 |
| Metastatic solid tumor | C77.x-C80.x | 6 |
| Acquired Immunodeficiency syndrome (AIDS) | B20.x-B22.x, B24.x | 6 |
References
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 15 November 2021).
- Bhattacharya, J.; Bundorf, M.K. The incidence of the healthcare costs of obesity. J. Health Econ. 2009, 28, 649–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flegal, K.M.; Carroll, M.D.; Kuczmarski, R.J.; Johnson, C.L. Overweight and obesity in the United States: Prevalence and trends, 1960–1994. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 39–47. [Google Scholar] [CrossRef] [Green Version]
- Flegal, K.M.; Carroll, M.D.; Ogden, C.L.; Curtin, L.R. Prevalence and trends in obesity among US adults, 1999–2008. JAMA 2010, 303, 235–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flegal, K.M.; Kruszon-Moran, D.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA 2016, 315, 2284–2291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gortmaker, S.L.; Must, A.; Perrin, J.M.; Sobol, A.M.; Dietz, W.H. Social and economic consequences of overweight in adolescence and young adulthood. N. Engl. J. Med. 1993, 329, 1008–1012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feigin, V.L.; Nguyen, G.; Cercy, K.; Johnson, C.O.; Alam, T.; Parmar, P.G.; Abajobir, A.A.; Abate, K.H.; Abd-Allah, F.; et al.; GBD 2016 Lifetime Risk of Stroke Collaborators Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N. Engl. J. Med. 2018, 379, 2429–2437. [Google Scholar] [CrossRef] [PubMed]
- GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar] [CrossRef] [Green Version]
- Oesch, L.; Tatlisumak, T.; Arnold, M.; Sarikaya, H. Obesity paradox in stroke—Myth or reality? A systematic review. PLoS ONE 2017, 12, e0171334. [Google Scholar] [CrossRef]
- Bazzano, L.A.; Gu, D.; Whelton, M.R.; Wu, X.; Chen, C.S.; Duan, X.; Chen, J.; Chen, J.C.; He, J. Body mass index and risk of stroke among Chinese men and women. Ann. Neurol. 2010, 67, 11–20. [Google Scholar] [CrossRef] [Green Version]
- Hu, G.; Tuomilehto, J.; Silventoinen, K.; Sarti, C.; Mannisto, S.; Jousilahti, P. Body mass index, waist circumference, and waist-hip ratio on the risk of total and type-specific stroke. Arch. Intern. Med. 2007, 167, 1420–1427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurth, T.; Gaziano, J.M.; Berger, K.; Kase, C.S.; Rexrode, K.M.; Cook, N.R.; Buring, J.E.; Manson, J.E. Body mass index and the risk of stroke in men. Arch. Intern. Med. 2002, 162, 2557–2562. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.M.; Sung, J.; Davey Smith, G.; Ebrahim, S. Body mass index and ischemic and hemorrhagic stroke: A prospective study in Korean men. Stroke 2004, 35, 831–836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strazzullo, P.; D’Elia, L.; Cairella, G.; Garbagnati, F.; Cappuccio, F.P.; Scalfi, L. Excess body weight and incidence of stroke: Meta-analysis of prospective studies with 2 million participants. Stroke 2010, 41, e418–e426. [Google Scholar] [CrossRef] [Green Version]
- Andersen, K.K.; Olsen, T.S. The obesity paradox in stroke: Lower mortality and lower risk of readmission for recurrent stroke in obese stroke patients. Int. J. Stroke 2015, 10, 99–104. [Google Scholar] [CrossRef]
- Doehner, W.; Schenkel, J.; Anker, S.D.; Springer, J.; Audebert, H.J. Overweight and obesity are associated with improved survival, functional outcome, and stroke recurrence after acute stroke or transient ischaemic attack: Observations from the TEMPiS trial. Eur. Heart J. 2013, 34, 268–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassan, A.E.; Chaudhry, S.A.; Jani, V.; Grigoryan, M.; Khan, A.A.; Adil, M.M.; Qureshi, A.I. Is there a decreased risk of intracerebral hemorrhage and mortality in obese patients treated with intravenous thrombolysis in acute ischemic stroke? J. Stroke Cerebrovasc. Dis. 2013, 22, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Olsen, T.S.; Dehlendorff, C.; Petersen, H.G.; Andersen, K.K. Body mass index and poststroke mortality. Neuroepidemiology 2008, 30, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Vemmos, K.; Ntaios, G.; Spengos, K.; Savvari, P.; Vemmou, A.; Pappa, T.; Manios, E.; Georgiopoulos, G.; Alevizaki, M. Association between obesity and mortality after acute first-ever stroke: The obesity-stroke paradox. Stroke 2011, 42, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffman, H.; Jalal, M.S.; Furst, T.; Chin, L.S. The Obesity Paradox in Spontaneous Intracerebral Hemorrhage: Results from a Retrospective Analysis of the Nationwide Inpatient Sample. Neurocrit. Care 2020, 32, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Lee, S.H.; Ryu, W.S.; Kim, C.K.; Lee, J.; Yoon, B.W. Paradoxical longevity in obese patients with intracerebral hemorrhage. Neurology 2011, 76, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Persaud, S.R.; Lieber, A.C.; Donath, E.; Stingone, J.A.; Dangayach, N.S.; Zhang, X.; Mocco, J.; Kellner, C.P. Obesity Paradox in Intracerebral Hemorrhage. Stroke 2019, 50, 999–1002. [Google Scholar] [CrossRef]
- Funada, S.; Shimazu, T.; Kakizaki, M.; Kuriyama, S.; Sato, Y.; Matsuda-Ohmori, K.; Nishino, Y.; Tsuji, I. Body mass index and cardiovascular disease mortality in Japan: The Ohsaki Study. Prev. Med. 2008, 47, 66–70. [Google Scholar] [CrossRef]
- Towfighi, A.; Ovbiagele, B. The impact of body mass index on mortality after stroke. Stroke 2009, 40, 2704–2708. [Google Scholar] [CrossRef] [PubMed]
- Rozen, G.; Elbaz-Greener, G.; Marai, I.; Heist, E.K.; Ruskin, J.N.; Carasso, S.; Birati, E.Y.; Amir, O. The relationship between the body mass index and in-hospital mortality in patients admitted for sudden cardiac death in the United States. Clin. Cardiol. 2021, 44, 1673–1682. [Google Scholar] [CrossRef] [PubMed]
- HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). In 2012–2013. Agency for Healthcare Research and Quality. Available online: www.hcup-us.ahrq.gov/nisoverview.jsp (accessed on 7 January 2022).
- Healthcare Cost and Utilization Project (HCUP). 2000–2011. In Agency for Healthcare Research and Quality. Available online: www.hcup-us.ahrq.gov/nisoverview.jsp (accessed on 7 January 2022).
- Steiner, C.; Elixhauser, A.; Schnaier, J. The healthcare cost and utilization project: An overview. Eff. Clin. Pract. 2002, 5, 143–151. [Google Scholar] [PubMed]
- Deyo, R.A.; Cherkin, D.C.; Ciol, M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef]
- Chu, Y.T.; Ng, Y.Y.; Wu, S.C. Comparison of different comorbidity measures for use with administrative data in predicting short- and long-term mortality. BMC Health Serv. Res. 2010, 10, 140. [Google Scholar] [CrossRef] [Green Version]
- Radovanovic, D.; Seifert, B.; Urban, P.; Eberli, F.R.; Rickli, H.; Bertel, O.; Puhan, M.A.; Erne, P.; Investigators, A.p. Validity of Charlson Comorbidity Index in patients hospitalised with acute coronary syndrome. Insights from the nationwide AMIS Plus registry 2002–2012. Heart 2014, 100, 288–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosseini, S.M.; Moazzami, K.; Rozen, G.; Vaid, J.; Saleh, A.; Heist, K.E.; Vangel, M.; Ruskin, J.N. Utilization and in-hospital complications of cardiac resynchronization therapy: Trends in the United States from 2003 to 2013. Eur. Heart J. 2017, 38, 2122–2128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niedziela, J.; Hudzik, B.; Niedziela, N.; Gasior, M.; Gierlotka, M.; Wasilewski, J.; Myrda, K.; Lekston, A.; Polonski, L.; Rozentryt, P. The obesity paradox in acute coronary syndrome: A meta-analysis. Eur. J. Epidemiol. 2014, 29, 801–812. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Horwich, T.B.; Oreopoulos, A.; Kovesdy, C.P.; Younessi, H.; Anker, S.D.; Morley, J.E. Risk factor paradox in wasting diseases. Curr. Opin. Clin. Nutr. Metab. Care 2007, 10, 433–442. [Google Scholar] [CrossRef]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O. Obesity and cardiovascular disease: Risk factor, paradox, and impact of weight loss. J. Am. Coll. Cardiol. 2009, 53, 1925–1932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oliveros, H.; Villamor, E. Obesity and mortality in critically ill adults: A systematic review and meta-analysis. Obesity 2008, 16, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, S.R.; Licinio, J.; Tauchnitz, R.; Engelmann, L.; Negrao, A.B.; Gold, P.; Chrousos, G.P. Plasma leptin levels are increased in survivors of acute sepsis: Associated loss of diurnal rhythm, in cortisol and leptin secretion. J. Clin. Endocrinol. Metab. 1998, 83, 280–283. [Google Scholar] [CrossRef] [PubMed]
- DeLany, J. Leptin hormone and other biochemical influences on systemic inflammation. J. Bodyw. Mov. Ther. 2008, 12, 121–132. [Google Scholar] [CrossRef]
- Noriko, I.; Lam, Q.L.; Lu, L.; Matarese, G.; La Cava, A. Leptin and Inflammation. Curr. Immunol. Rev. 2008, 4, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.J.; Braun, W.; Enderle, J.; Bosy-Westphal, A. Beyond BMI: Conceptual Issues Related to Overweight and Obese Patients. Obes. Facts 2016, 9, 193–205. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).