Hypothermia Therapy for Traumatic Spinal Cord Injury: An Updated Review
Abstract
1. Introduction
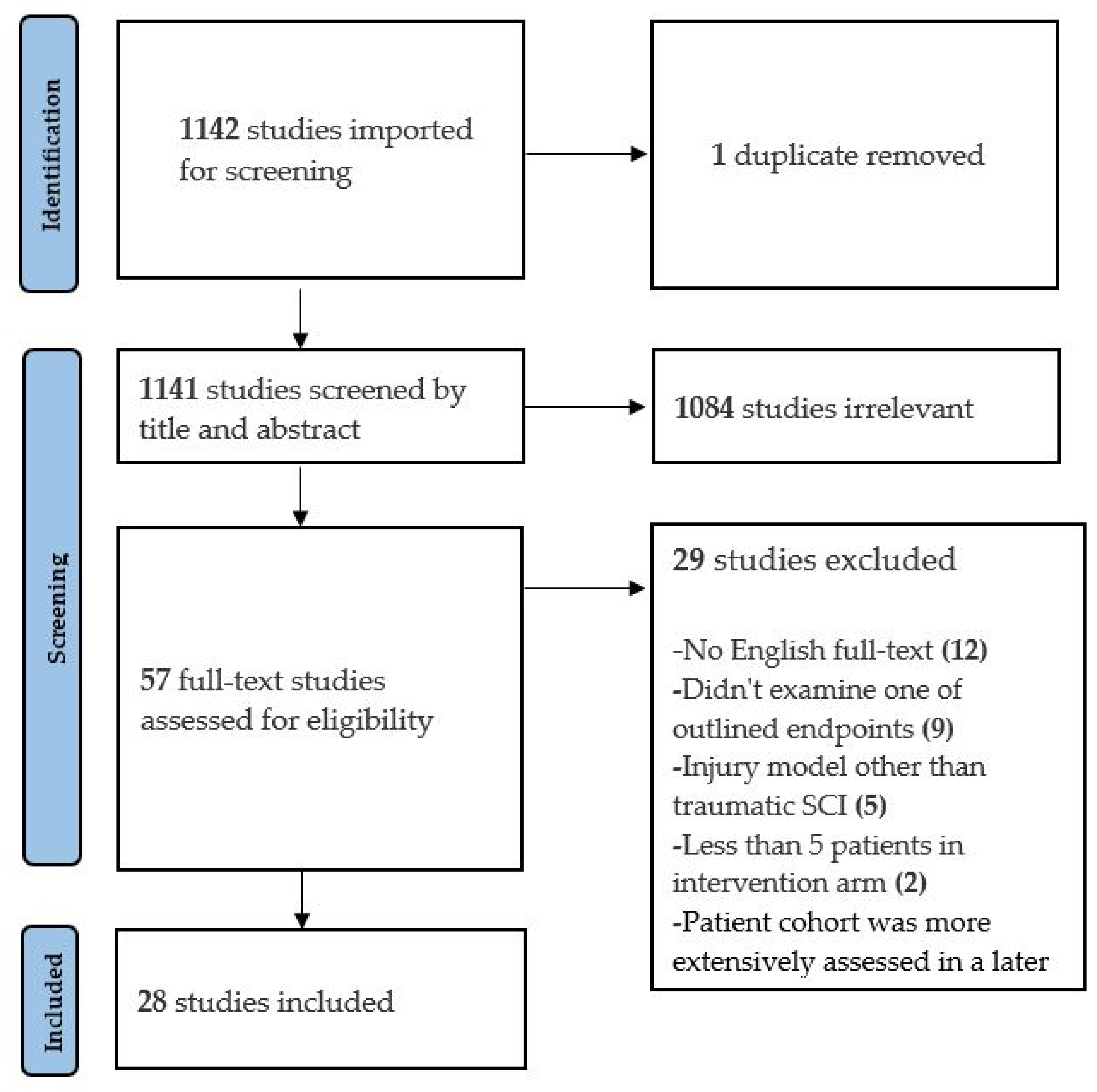
2. Methods
3. Results
3.1. Preclinical Data
3.2. Clinical Series
4. Discussion
4.1. Neuroprotective Effects of Hypothermia in Animals
4.2. New Avenues to Monitor Neurologic Injury
4.3. Safety of Hypothermia Therapy
4.4. Future Directions
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Spinal Cord Injury Statistical Center. Facts and Figures at a Glance; University of Alabama at Birmingham: Birmingham, AL, USA, 2020. [Google Scholar]
- Alkabie, S.; Boileau, A.J. The Role of Therapeutic Hypothermia After Traumatic Spinal Cord Injury—A Systematic Review. World Neurosurg. 2016, 86, 432–449. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.B.; Ayers, G.D.; Peterson, E.N.; Harris, M.B.; Morse, L.R.; O’Connor, K.C.; Garshick, E. Traumatic Spinal Cord Injury in the United States, 1993–2012. JAMA 2015, 313, 2236–2243. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.W.; Sadowsky, C. Spinal-cord injury. Lancet 2002, 359, 417–425. [Google Scholar] [CrossRef]
- Tator, C.H.; Deecke, L. Value of normothermic perfusion, hypothermic perfusion, and durotomy in the treatment of experimental acute spinal cord trauma. J. Neurosurg. 1973, 39, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Norenberg, M.D.; Smith, J.; Marcillo, A. The Pathology of Human Spinal Cord Injury: Defining the Problems. J. Neurotrauma 2004, 21, 429–440. [Google Scholar] [CrossRef]
- Yip, P.K.; Malaspina, A. Spinal cord trauma and the molecular point of no return. Mol. Neurodegener. 2012, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, C.S.; Nori, S.; Tetreault, L.; Wilson, J.; Kwon, B.; Harrop, J.; Choi, D.; Fehlings, M.G. Traumatic Spinal Cord Injury—Repair and Regeneration. Neurosurgery 2017, 80, S9–S22. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.U.; Wang, M.Y.; Levi, A.D. Hypothermia for Acute Spinal Cord Injury—A Review. World Neurosurg. 2014, 82, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Roberts, T.T.; Leonard, G.R.; Cepela, D.J. Classifications in Brief: American Spinal Injury Association (ASIA) Impairment Scale. Clin. Orthop. Relat. Res. 2017, 475, 1499–1504. [Google Scholar] [CrossRef] [PubMed]
- Steeves, J.D.; Kramer, J.K.; Fawcett, J.W.; Cragg, J.; Lammertse, D.P.; Blight, A.R.; Marino, R.J.; Ditunno, J.F.; Coleman, W.P.; Geisler, F.H.; et al. Extent of spontaneous motor recovery after traumatic cervical sensorimotor complete spinal cord injury. Spinal Cord 2011, 49, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Cappuccino, A.; Bisson, L.J.; Carpenter, B.; Marzo, J.; Dietrich, W.D.; Cappuccino, H. The Use of Systemic Hypothermia for the Treatment of an Acute Cervical Spinal Cord Injury in a Professional Football Player. Spine 2010, 35, E57–E62. [Google Scholar] [CrossRef]
- Kwon, B.K.; Mann, C.; Sohn, H.M.; Hilibrand, A.S.; Phillips, F.M.; Wang, J.C.; Fehlings, M.G. Hypothermia for spinal cord injury. Spine J. 2008, 8, 859–874. [Google Scholar] [CrossRef]
- Green, R.S.; Howes, D.W. Stock your emergency department with ice packs: A practical guide to therapeutic hypothermia for survivors of cardiac arrest. Can. Med. Assoc. J. 2007, 176, 759–762. [Google Scholar] [CrossRef][Green Version]
- Kliegel, A.; Janata, A.; Wandaller, C.; Uray, T.; Spiel, A.; Losert, H.; Kliegel, M.; Holzer, M.; Haugk, M.; Sterz, F.; et al. Cold infusions alone are effective for induction of therapeutic hypothermia but do not keep patients cool after cardiac arrest. Resuscitation 2007, 73, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, G.K.; Ogilvy, C.S.; Shuer, L.M.; Connolly, E.S.; Solomon, R.A.; Lam, A.; Kassell, N.F.; Baker, C.J.; Giannotta, S.L.; Cockroft, K.M.; et al. Comparison of Endovascular and Surface Cooling during Unruptured Cerebral Aneurysm Repair. Neurosurgery 2004, 55, 307–314; discussion 314–315. [Google Scholar] [CrossRef] [PubMed]
- Polderman, K.H. Keeping a cool head: How to induce and maintain hypothermia. Crit. Care Med. 2004, 32, 2558–2660. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Arizala, A.; Green, B.A. Hypothermia in spinal cord injury. J. Neurotrauma 1992, 9 (Suppl. 2), S497–S505. [Google Scholar] [PubMed]
- Wang, H.; Olivero, W.; Lanzino, G.; Elkins, W.; Rose, J.; Honings, D.; Rodde, M.; Burnham, J.; Wang, D. Rapid and selective cerebral hypothermia achieved using a cooling helmet. J. Neurosurg. 2004, 100, 272–277. [Google Scholar] [CrossRef]
- Albin, M.S.; White, R.J.; Acosta-Rua, G.; Yashon, D. Study of Functional Recovery Produced by Delayed Localized Cooling After Spinal Cord Injury in Primates. J. Neurosurg. 1968, 29, 113–120. [Google Scholar] [CrossRef]
- Barbosa, M.O.; Cristante, A.F.; dos Santos, G.B.; Ferreira, R.; Marcon, R.M.; Filho, T.E.P.D.B. Neuroprotective effect of epidural hypothermia after spinal cord lesion in rats. Clinics 2014, 69, 559–564. [Google Scholar] [CrossRef]
- Batchelor, P.E.; Kerr, N.F.; Gatt, A.M.; Aleksoska, E.; Cox, S.F.; Ghasem-Zadeh, A.; Wills, T.E.; Howells, D.W. Hypothermia Prior to Decompression: Buying Time for Treatment of Acute Spinal Cord Injury. J. Neurotrauma 2010, 27, 1357–1368. [Google Scholar] [CrossRef] [PubMed]
- Casas, C.E.; Herrera, L.P.; Prusmack, C.; Ruenes, G.; Marcillo, A.; Guest, J.D. Effects of epidural hypothermic saline infusion on locomotor outcome and tissue preservation after moderate thoracic spinal cord contusion in rats. J. Neurosurg. Spine 2005, 2, 308–318. [Google Scholar] [CrossRef] [PubMed]
- Dimar, J.R.; Shields, C.B.; Zhang, Y.P.; Burke, D.A.; Raque, G.H.; Glassman, S.D. The Role of Directly Applied Hypothermia in Spinal Cord Injury. Spine 2000, 25, 2294–2302. [Google Scholar] [CrossRef] [PubMed]
- Grulova, I.; Slovinska, L.; Nagyova, M.; Cizek, M.; Cizkova, D. The effect of hypothermia on sensory-motor function and tissue sparing after spinal cord injury. Spine J. 2013, 13, 1881–1891. [Google Scholar] [CrossRef] [PubMed]
- Ha, K.-Y.; Kim, Y.-H. Neuroprotective Effect of Moderate Epidural Hypothermia After Spinal Cord Injury in Rats. Spine 2008, 33, 2059–2065. [Google Scholar] [CrossRef] [PubMed]
- Hosier, H.; Peterson, D.; Tsymbalyuk, O.; Keledjian, K.; Smith, B.R.; Ivanova, S.; Gerzanich, V.; Popovich, P.G.; Simard, J.M. A Direct Comparison of Three Clinically Relevant Treatments in a Rat Model of Cervical Spinal Cord Injury. J. Neurotrauma 2015, 32, 1633–1644. [Google Scholar] [CrossRef] [PubMed]
- Jorge, A.; Fish, E.J.; Dixon, C.E.; Hamilton, K.D.; Balzer, J.; Thirumala, P. The Effect of Prophylactic Hypothermia on Neurophysiological and Functional Measures in the Setting of Iatrogenic Spinal Cord Impact Injury. World Neurosurg. 2019, 129, e607–e613. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.-H.; Chio, C.-C.; Lin, M.-T.; Yeh, C.-H. Body Cooling Ameliorating Spinal Cord Injury May Be Neurogenesis-, Anti-inflammation- and Angiogenesis-Associated in Rats. J. Trauma Inj. Infect. Crit. Care 2011, 70, 885–893. [Google Scholar] [CrossRef] [PubMed]
- Karamouzian, S.; Akhtarshomar, S.; Saied, A.; Gholamhoseinian, A. Effects of Methylprednisolone on Neuroprotective Effects of Delay Hypothermia on Spinal Cord Injury in Rat. Asian Spine J. 2015, 9, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kuchner, E.F.; Hansebout, R.R.; Pappius, H.M. Effects of Dexamethasone and of Local Hypothermia on Early and Late Tissue Electrolyte Changes in Experimental Spinal Cord Injury. J. Spinal Disord. 2000, 13, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Lo, T.P., Jr.; Cho, K.S.; Garg, M.S.; Lynch, M.P.; Marcillo, A.E.; Koivisto, D.L.; Stagg, M.; Abril, R.M.; Patel, S.; Dietrich, W.D.; et al. Systemic hypothermia improves histological and functional outcome after cervical spinal cord contusion in rats. J. Comp. Neurol. 2009, 514, 433–448. [Google Scholar] [CrossRef]
- Maybhate, A.; Hu, C.; Bazley, F.A.; Yu, Q.; Thakor, N.V.; Kerr, C.L.; All, A.H. Potential long-term benefits of acute hypothermia after spinal cord injury: Assessments with somatosensory-evoked potentials. Crit. Care Med. 2012, 40, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Morizane, K.; Ogata, T.; Morino, T.; Horiuchi, H.; Yamaoka, G.; Hino, M.; Miura, H. A novel thermoelectric cooling device using Peltier modules for inducing local hypothermia of the spinal cord: The effect of local electrically controlled cooling for the treatment of spinal cord injuries in conscious rats. Neurosci. Res. 2012, 72, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Morochovič, R.; Chudá, M.; Talánová, J.; Cibur, P.; Kitka, M.; Vanický, I. Local Transcutaneous Cooling of the Spinal Cord in the Rat: Effects on Long-Term Outcomes After Compression Spinal Cord Injury. Int. J. Neurosci. 2008, 118, 555–568. [Google Scholar] [CrossRef] [PubMed]
- Ok, J.-H.; Kim, Y.-H.; Ha, K.-Y. Neuroprotective Effects of Hypothermia After Spinal Cord Injury in Rats. Spine 2012, 37, E1551–E1559. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.-Y.; Kim, Y.-H.; Kim, J.-W.; Kim, S.-I.; Ha, K.-Y. Effects of Therapeutic Hypothermia on Apoptosis and Autophagy After Spinal Cord Injury in Rats. Spine 2015, 40, 883–890. [Google Scholar] [CrossRef] [PubMed]
- Teh, D.B.L.; Chua, S.M.; Prasad, A.; Kakkos, I.; Jiang, W.; Yue, M.; Liu, X.; All, A.H. Neuroprotective assessment of prolonged local hypothermia post contusive spinal cord injury in rodent model. Spine J. 2018, 18, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Thienprasit, P.; Bantli, H.; Bloedel, J.R.; Chou, S.N. Effect of delayed local cooling on experimental spinal cord injury. J. Neurosurg. 1975, 42, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Westergren, H.; Farooque, M.; Olsson, Y.; Holtz, A. Motor Function Changes in the Rat Following Severe Spinal Cord Injury. Acta Neurochir. 2000, 142, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Li, N.; Zhu, L.; Zhou, Y.; Cheng, H. Beneficial effects of local profound hypothermia and the possible mechanism after experimental spinal cord injury in rats. J. Spinal Cord Med. 2015, 39, 220–228. [Google Scholar] [CrossRef][Green Version]
- Yu, C.G.; Jimenez, O.; Marcillo, A.E.; Weider, B.; Bangerter, K.; Dietrich, W.D.; Castro, S.; Yezierski, R.P. Beneficial effects of modest systemic hypothermia on locomotor function and histopathological damage following contusion-induced spinal cord injury in rats. J. Neurosurg. Spine 2000, 93, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Dididze, M.; Green, B.A.; Dietrich, W.D.; Vanni, S.; Wang, M.Y.; Levi, A.D. Systemic hypothermia in acute cervical spinal cord injury: A case-controlled study. Spinal Cord 2013, 51, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Levi, A.D.; Casella, G.; Green, B.A.; Dietrich, W.D.; Vanni, S.; Jagid, J.; Wang, M.Y. Clinical Outcomes Using Modest Intravascular Hypothermia After Acute Cervical Spinal Cord Injury. Neurosurgery 2010, 66, 670–677. [Google Scholar] [CrossRef] [PubMed]
- Hansebout, R.R.; Hansebout, C.R. Local cooling for traumatic spinal cord injury: Outcomes in 20 patients and review of the literature. J. Neurosurg. Spine 2014, 20, 550–561. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, M.J.; Hogg, F.R.A.; Kearney, S.; Kopp, M.; Blex, C.; Serdani, L.; Sherwood, O.; Schwab, J.M.; Zoumprouli, A.; Papadopoulos, M.C.; et al. Effects of local hypothermia–rewarming on physiology, metabolism and inflammation of acutely injured human spinal cord. Sci. Rep. 2020, 10, 8125. [Google Scholar] [CrossRef] [PubMed]
- Geisler, F.H.; Coleman, W.P.; Grieco, G.; Poonian, D. The Sygen® Multicenter Acute Spinal Cord Injury Study. Spine 2001, 26 (Suppl. 24), S87–S98. [Google Scholar] [CrossRef] [PubMed]
- Steeves, J.D.; Lammertse, D.; Curt, A.; Fawcett, J.; Tuszynski, M.H.; Ditunno, J.F.; Ellaway, P.H.; Fehlings, M.; Guest, J.D.; Kleitman, N.; et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP panel: Clinical trial outcome measures. Spinal Cord 2007, 45, 206–221. [Google Scholar] [CrossRef] [PubMed]
- Van Middendorp, J.J.; Hosman, A.J.; Pouw, M.H.; Van de Meent, H. ASIA impairment scale conversion in traumatic SCI: Is it related with the ability to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord 2009, 47, 555–560. [Google Scholar]
- Aarabi, B.; Hesdorffer, D.C.; Ahn, E.S.; Aresco, C.; Scalea, T.M.; Eisenberg, H.M. Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J. Neurosurg. 2006, 104, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Tao, Y.; Marsons, L.; Dee, P.; Yu, D.; Guan, Y.; Zhou, X. The effectiveness of early prophylactic hypothermia in adult patients with traumatic brain injury: A systematic review and meta-analysis. Aust. Crit. Care 2020, 34, 83–91. [Google Scholar] [CrossRef]
- Clifton, G.L.; Allen, S.; Barrodale, P.; Plenger, P.; Berry, J.; Koch, S.; Fletcher, J.; Hayes, R.L.; Choi, S.C. A Phase II Study of Moderate Hypothermia in Severe Brain Injury. J. Neurotrauma 1993, 10, 263–271; discussion 273. [Google Scholar] [CrossRef] [PubMed]
- Marion, D.W.; Obrist, W.D.; Earlier, P.M.; Penrod, L.E.; Darby, J.M. The use of moderate therapeutic hypothermia for patients with severe head injuries: A preliminary report. J. Neurosurg. 1993, 79, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Marion, D.W.; Penrod, L.E.; Kelsey, S.F.; Obrist, W.D.; Kochanek, P.; Palmer, A.M.; Wisniewski, S.; DeKosky, S. Treatment of Traumatic Brain Injury with Moderate Hypothermia. N. Engl. J. Med. 1997, 336, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Clifton, G.L.; Jiang, J.Y.; Lyeth, B.G.; Jenkins, L.W.; Hamm, R.J.; Hayes, R.L. Marked Protection by Moderate Hypothermia after Experimental Traumatic Brain Injury. J. Cereb. Blood Flow Metab. 1991, 11, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Carney, N.; Totten, A.M.; O’Reilly, C.; Ullman, J.S.; Hawryluk, G.W.J.; Bell, M.J.; Bratton, S.L.; Chesnut, R.; Harris, O.A.; Kissoon, N.; et al. Guidelines for Management of Severe Traumatic Brain Injury, 4th ed.; Brain Trauma Foundation: New York, NY, USA, 2016. [Google Scholar]
- Michenfelder, J.D.; Milde, J.H. The effect of profound levels of hypothermia (below 14 degrees C) on canine cerebral metabolism. J. Cereb. Blood Flow Metab. 1992, 12, 877–880. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, S.; Miyamoto, O.; Janjua, N.A.; Itano, T.; Mori, S.; Norimatsu, H. Post-traumatic moderate systemic hypothermia reduces TUNEL positive cells following spinal cord injury in rat. Spinal Cord 2004, 42, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Duz, B.; Kaplan, M.; Bilgic, S.; Korkmaz, A.; Kahraman, S. Does Hypothermic Treatment Provide an Advantage After Spinal Cord Injury Until Surgery? An Experimental Study. Neurochem. Res. 2008, 34, 407–410. [Google Scholar] [CrossRef] [PubMed]
- Jou, I.M. Effects of core body temperature on changes in spinal somatosensory-evoked potential in acute spinal cord compression injury: An experimental study in the rat. Spine 2000, 25, 1878–1885. [Google Scholar] [CrossRef] [PubMed]
- Dalkilic, T.; Fallah, N.; Noonan, V.K.; Elizei, S.S.; Dong, K.; Belanger, L.; Ritchie, L.; Tsang, A.; Bourassa-Moreau, E.; Heran, M.K.; et al. Predicting Injury Severity and Neurological Recovery after Acute Cervical Spinal Cord Injury: A Comparison of Cerebrospinal Fluid and Magnetic Resonance Imaging Biomarkers. J. Neurotrauma 2018, 35, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Buttram, S.D.; Wisniewski, S.; Jackson, E.K.; Adelson, P.D.; Feldman, K.; Bayir, H.; Berger, R.P.; Clark, R.S.; Kochanek, P. Multiplex Assessment of Cytokine and Chemokine Levels in Cerebrospinal Fluid following Severe Pediatric Traumatic Brain Injury: Effects of Moderate Hypothermia. J. Neurotrauma 2007, 24, 1707–1718. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, S.L.; Myers, T.J.; Baldini, M.G. Disseminated intravascular coagulation during rewarming following hypothermia. JAMA 1981, 245, 2517–2518. [Google Scholar] [CrossRef]
- Reuler, J.B. Hypothermia: Pathophysiology, Clinical Settings, and Management. Ann. Intern. Med. 1978, 89, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Simosa, H.F.; Petersen, D.J.; Agarwal, S.K.; Burke, P.A.; Hirsch, E.F. Increased Risk of Deep Venous Thrombosis with Endovascular Cooling in Patients with Traumatic Head Injury. Am. Surg. 2007, 73, 461–464. [Google Scholar] [CrossRef] [PubMed]
- Phang, I.; Zoumprouli, A.; Saadoun, S.; Papadopoulos, M. Safety profile and probe placement accuracy of intraspinal pressure monitoring for traumatic spinal cord injury: Injured Spinal Cord Pressure Evaluation study. J. Neurosurg. Spine 2016, 25, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Sanossian, N.; Ohanian, A.G.; Saver, J.L.; Kim, L.I.; Ovbiagele, B. Frequency and Determinants of Nonpublication of Research in the Stroke Literature. Stroke 2006, 37, 2588–2592. [Google Scholar] [CrossRef]
| Study | Animal | Injury Method | Level of Injury | Hypothermia Method | Treatment Temp/Rate | Target Temp | Treatment Onset | Duration | Other Therapy | Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| Albin et al., 1968 | Rhesus monkeys (n = 14) | Weight drop (300 g/cf) | T10 | Local: subarachnoid heat exchanger | 2–5 °C | 10 °C | 4 h after injury | 3 h | None | No deleterious effects were noted. 13 of 14 treated monkeys achieved complete functional recovery. |
| Barbosa et al., 2014 | Wistar rats (n = 15 per group) | NYU impactor (25 g/fc) | T9–10 | Local: epidural cold solution perfusion | 9–10 °C | 25 °C | Immediately after injury | 20 min | None | No difference in motor outcomes (BBB) were seen between groups. |
| Batchelor et al., 2010 | Female Fischer rats (n = 16 per group) | Spinal cord impactor (150 kdyn) and canal spacer | T8 | Systemic: surface cooling | NR | 33 °C | 30 min after injury | 7.5 h | Spacer decompression (0, 2, or 8 h after injury) | Hypothermia significantly improved (p < 0.005) BBB and ladder-stepping scores in rats decompressed after 8 h. |
| Casas et al., 2005 | Female Sprague-Dawley rats (n = 14 per group) | NYU impactor (12.5 g·cm) | T10 | Local: epidural saline perfusion | 4 °C | 20, 30, or 37.5 °C | 30 min after injury | 3 h | None | No differences in motor outcomes (BBB) were observed between groups. |
| Dimar et al., 2000 | Male Sprague-Dawley rats (n = 8 per group) | NYU impactor (25 g·cm), 50% canal spacer, or both | T10 | Local: epidural cooling apparatus | 19 °C | NR | Immediately after injury | 2 h | Spacer decompression (2 h after insertion) | Hypothermia significantly (p < 0.05) improved motor (BBB) outcomes in the spacer-only group at 5 weeks post-injury. |
| Grulova et al., 2013 | Male Wistar rats (n > 11 per group) | Balloon catheter compression | T8–9 | Systemic: surface cooling | NR | 31–32 °C | Immediately after injury | 30 min | None | Hypothermia improved (p < 0.01) urinary scores within 5 days of injury. No difference in motor (BBB) outcomes was observed. |
| Ha et al., 2008 | Male Sprague-Dawley rats (n = 8 per group) | NYU impactor (25 g·cm) | T9 | Local: epidural saline perfusion | 18 °C | 30 °C | Immediately after injury | 48 h | None | Hypothermia improved (p < 0.01) motor function (Gale) and incline plane scores 7 days after injury. |
| Hosier et al., 2015 | Female Long-Evans rats (n > 7 per group) | Spinal cord impactor (25 g·cm) | C8; left unilateral | Systemic: surface cooling | −8 °C/h | 33 °C | 5 min after injury | 4 h | None | Hypothermia improved (p < 0.05) motor scores 7 days after injury. Beam balance, accelerating rotarod, and BBB scores were greater (p < 0.05) in the hypothermia group 6 weeks after injury. |
| Jorge et al., 2019 | Female Sprague-Dawley rats (n > 5 per group) | Spinal cord impactor (200 kdyn) | T8 | Systemic: surface cooling | NR | 32 °C | Beginning of surgery | 2 h | None | Hypothermia-treated rats had significantly higher (p < 0.01) BBB scores 6 weeks after injury. |
| Kao et al., 2011 | Male Sprague-Dawley rats (n = 8 per group) | Aneurysm clip (55 g) | T8–9 | Systemic: surface cooling | 31 °C | 33 °C | Immediately after injury | 2 h | None | Hypothermia group had significantly higher (p < 0.05) BBB scores 4 days after injury. |
| Karamouzian et al., 2015 | Male Wistar rats (n = 20 per group) | Weight drop (25 g·cm) | T8–9 | Systemic: surface cooling | NR | 33–34 °C | 30 min (early) or 3.5 h (late) after injury | 3 h | Methylprednisolone (30 mg/kg immediately after injury) | Groups treated with early/late hypothermia, methylprednisolone, or both achieved significantly higher (p = 0.05) BBB scores than controls 2–3 weeks after injury. No motor differences were seen among treatment groups. |
| Kuchner et al., 2000 | Female mongrel dogs (n > 15 per group) | Epidural balloon inflation (160 mm·Hg) | T13 | Local: epidural heat exchanger | NR | 3–9 °C | 15 min (hypothermia only) or 3.5 h (hypothermia and dexamethasone) after Injury | 4 h | Dexamethasone (0.24 mg/kg/day) | Hypothermia (p < 0.05), steroid (p < 0.05), and dual-therapy (p < 0.01) groups had significantly higher motor scores compared to controls at 7 weeks post-injury. |
| Lo et al., 2009 | Female Fischer rats (n = 15 per group) | OSU electromagnetic SCI device (3 kdyn) | C5 | Systemic: surface cooling | NR | 33 °C | After injury | 4 h | None | Hypothermia did not improve BBB or incline plane test scores. Hypothermia significantly increased forelimb gripping (p < 0.05) and self-supported hanging (p < 0.01) 8 weeks after injury |
| Maybhate et al., 2012 | Female Lewis rats (n = 10 per group) | NYU impactor (12.5 g·cm) | T8 | Systemic: surface cooling | NR | 32 °C | 2 h after injury | 2 h | None | Hypothermia significantly improved (p < 0.00004) BBB scores at 4 weeks post-injury. |
| Morizane et al., 2012 | Female Wistar rats (n > 8 per group) | NYU impactor (25 g·cm) | T4 | Local: extracorpeal thermoelectric cooling device | NR | 33 °C | Immediately after injury | 48 h | None | Hypothermia-treated rats had significantly better (p < 0.01) BBB scores at 8 weeks post-injury |
| Morochovic et al., 2008 | Male Sprague-Dawley rats (n = 10 per group) | Epidural balloon catheter | T8–9 | Local: surface cooling | −1.4 °C/min | 30 °C | 25 min after injury | 60 min | None | No difference in locomotor performance (BBB) was detected between groups. |
| Ok et al., 2012 | Male Sprague-Dawley rats (n = 8 per group) | NYU impactor (25 g·cm) | T9 | A. Local: epidural water infusion B. Systemic: cold air chamber | A. 20 °C B. −0.25 °C/min | A. 28 °C B. 32 °C | A. After injury B. After waking from anesthesia | 48 h | None | 6 weeks after SCI, both local and systemic hypothermia groups had significantly higher (p < 0.05) BBB scores. |
| Seo et al., 2015 | Male Sprague-Dawley rats (n = 27 per group) | NYU impactor (25 g·cm) | T9 | Systemic: surface cooling | NR | 30–32 °C | After injury | 4 h | None | 6 weeks after SCI, hypothermia groups had significantly better (p < 0.05) BBB scores than control. |
| Tator et al., 1973 | Rhesus monkeys (n = 10 per group) | Inflatable cuff (350–400·mm Hg) | T9 | Local: subarachnoid cold solution perfusion | 5 °C | NR | 3 h after injury and immediately after durotomy | 3 h | Durotomy (immediately before hypothermia) | Normothermia-durotomy group recovered significantly better than nonperfused no durotomy group after 400 mm·Hg injury. Hypothermia treatment did not have this effect. |
| Teh et al., 2018 | Sprague-Dawley rats (n = 7 per group) | NYU impactor (12.5 g·cm) | T8 | Local: epidural heat exchange | −0.5 °C/min | 30 °C | 2 h after injury | 5 or 8 h | None | BBB scores were significantly higher in both 5 h (p = 0.001) and 8 h (p = 0.006) hypothermia groups compared to control after 6 weeks. |
| Thienprasit et al., 1975 | Adult cats (n > 5 per group) | Balloon catheter inflation | L2 | Local: epidural saline perfusion | 15 °C | NR | 6 h after injury | 2 h | Decompressive laminectomy (6 h after injury but before cooling) | Animals whose cortical-evoked responses failed to reappear within 6 h of injury had significantly better recovery (p < 0.01) after hypothermia and laminectomy compared to laminectomy alone. |
| Westergren et al., 2000 | Male Sprague-Dawley rats (n > 5 per group) | Blocking weight technique (50 g) | T7–8 | Systemic: surface cooling | NR | 30 °C | After injury | 2 h | None | Animals treated with hypothermia performed better on inclined plane test at 2 weeks post-injury. No differences in motor function (Gale) scores were detected. |
| Xu et al., 2016 | Male Sprague-Dawley rats (n = 7 per group) | Aneurysm clip (10 g) | T10 | Local: epidural saline infusion | 4 °C | 18 °C | Immediately after injury | 2 h | None | Hypothermia group achieved significantly higher (p < 0.05) BBB scores than control up to 3 weeks after injury. |
| Yu et al., 2000 | Female Sprague-Dawley rats (n > 7 per group) | NYU impactor (12.5 g·cm) | T10 | Systemic: surface cooling | NR | 32 °C | 30 min after injury | 4 h | None | BBB scores were significantly higher (p = 0.0024) 6 weeks after injury in hypothermia group compared to normothermia. |
| Study | Design | Total Patients | Inclusion Criteria | Exclusion Criteria | Hypothermia Method | Treatment Temp/Rate | Target Temp | Time to Treatment | Duration | Additional Therapy | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|
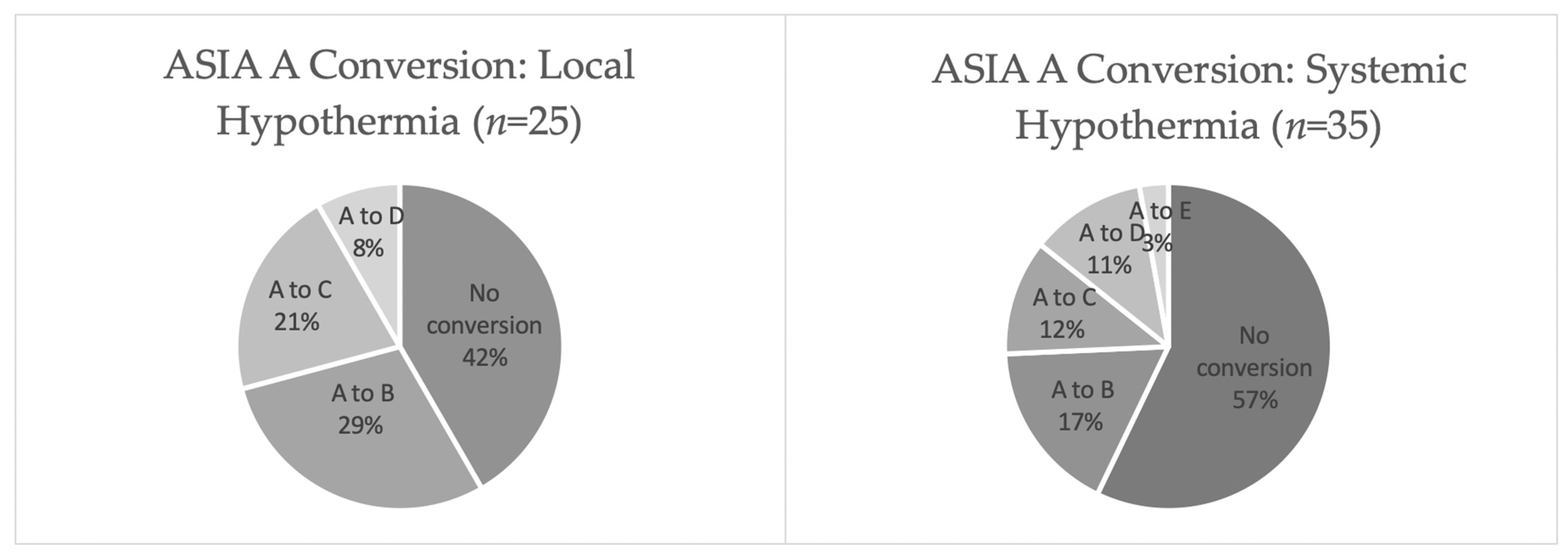
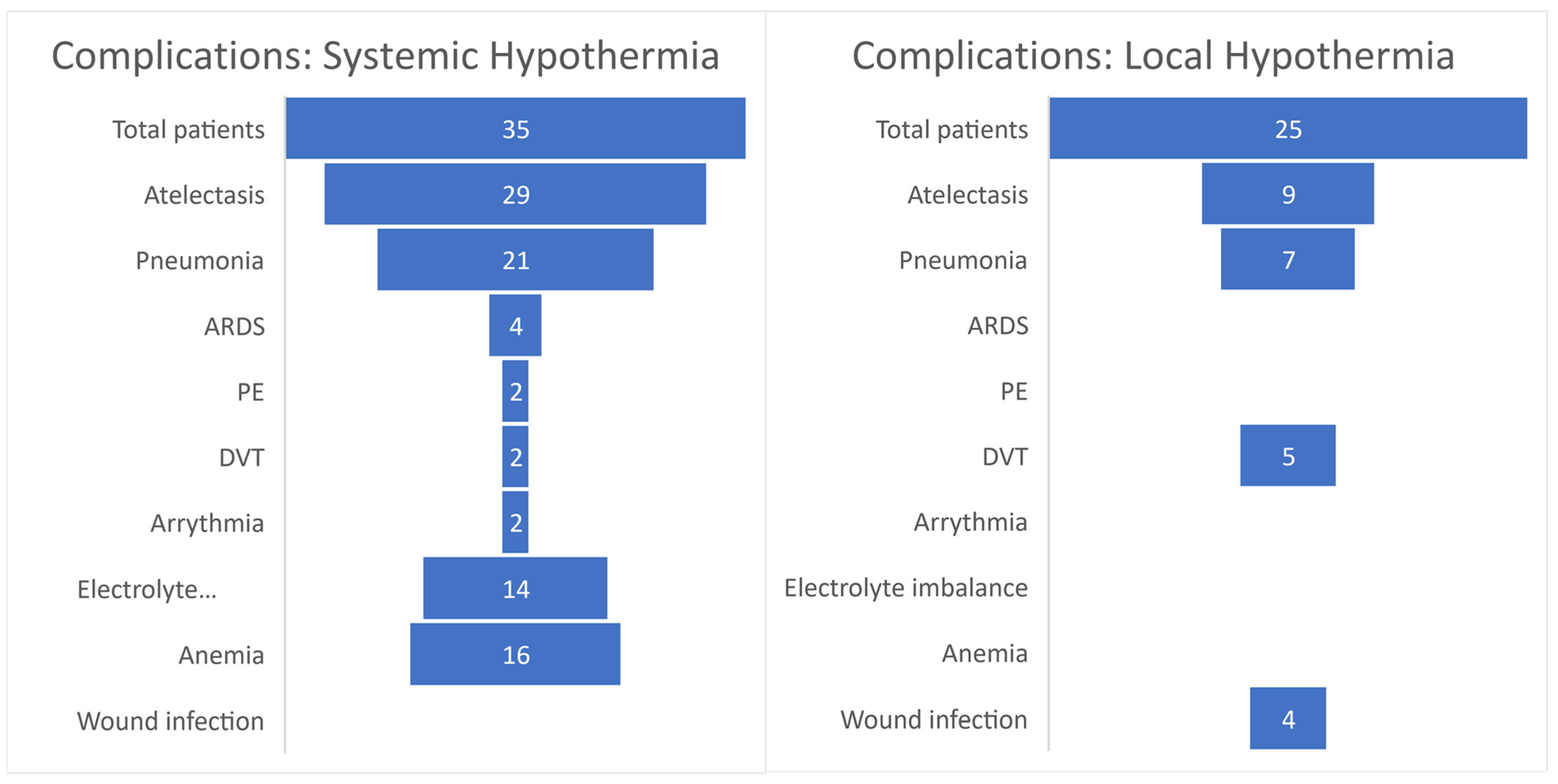
| Dididze et al., 2013 | Case-controlled study | 35 (14 from Levi et al., 2010) | 1. 18–65 years of age 2. AIS grade A 3. GCS = 15 4. Non-penetrating injury 5. Required urgent surgical reduction | 1. Age < 18 or >65 years 2. AIS grade B, C or D 3. Hyperthermia (>37 °C) on admission 4. Severe systemic injury 5. Cord transection 6. Intubation and sedation before initial neurological exam 7. Improved neurological exam within 12 h of injury 8. Other major comorbidities | Systemic: intravascular heat exchange catheter | −2.5 °C/h | 33 °C | Average = 7.76 ± 1.09 h | 48 h | None | 15 out of 35 total patients (43%) improved at least one AIS grade. When excluding patients who converted from AIS A within 24 h, 35.5% (11 out of 31) improved at least one grade. A similar number of respiratory complications occurred in both retrospective (n = 14) and prospective (n = 21) groups. Overall, 14.2% of patients experienced thromboembolic complications. |
| Hansebout and Hansebout, 2014 | Prospective case series | 20 | 1. Age 16–65 years 2. Alert and cooperative 3. Clinically complete cord injury | 1. Motor or sensory function below the level of cord injury 2. Perianal sensation 3. Anal sphincter contraction | Local: epidural cooling unit | 3 °C | Dural temp = 6 °C | Average = 7.1 h | Average = 3.7 h | Dexamethasone (6 mg every 6 h for 11 days) | All patients initially had AIS grade A impairment. Of the 20 total patients, 13 (65%) improved at least one AIS score. The most frequent complications were respiratory in nature (45% atelectasis and 35% pneumonia). The overall incidence of thromboembolic events was 25%. |
| Gallagher et al., 2020 | Prospective cohort study | 5 | 1. AIS grade A–C 2. Age 18–70 years 3. Surgery within 72 h of injury 4. Thoracic injuries | 1. Other major comorbidities or concurrent injuries 2. Penetrating TSCI 3. No consent | Local: epidural cooling catheter | −0.8 °C/h | Dural temp = 33 °C | Average = 70.4 ± 9.3 h | 12 h | None | The study was terminated after 3 out of 5 total patients experienced delayed wound infections. Four patients were initially AIS grade A on admission, of which only 1 improved to AIS B. |
| Levi et al., 2010 | Retrospective comparative case series | 14 | 1. Age 16–65 years 2. AIS grade A 3. Nonpenetrating injury 4. Patients requiring immediate surgical reduction | 1. AIS grade B, C, or D 2. Hyperthermia on admission (>38.5 °C) 3. Severe systemic injury 4. Spinal cord transection 5. Improvement in neurologic exam within 12 h of injury 6. Other major comorbidities | Systemic: intravascular heat exchange catheter | −0.5 °C/h | 33 °C | Average = 9.17 ± 2.24 h | Average = 47.6 ± 3.1 h | None | 6 of the 14 (42.8%) total patients improved their AIS scores. The most frequent complications were respiratory in nature. No thromboembolic complications were reported. A similar number of complications were observed in 14 case-matched control TSCI patients. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ransom, S.C.; Brown, N.J.; Pennington, Z.A.; Lakomkin, N.; Mikula, A.L.; Bydon, M.; Elder, B.D. Hypothermia Therapy for Traumatic Spinal Cord Injury: An Updated Review. J. Clin. Med. 2022, 11, 1585. https://doi.org/10.3390/jcm11061585
Ransom SC, Brown NJ, Pennington ZA, Lakomkin N, Mikula AL, Bydon M, Elder BD. Hypothermia Therapy for Traumatic Spinal Cord Injury: An Updated Review. Journal of Clinical Medicine. 2022; 11(6):1585. https://doi.org/10.3390/jcm11061585
Chicago/Turabian StyleRansom, Seth C., Nolan J. Brown, Zachary A. Pennington, Nikita Lakomkin, Anthony L. Mikula, Mohamad Bydon, and Benjamin D. Elder. 2022. "Hypothermia Therapy for Traumatic Spinal Cord Injury: An Updated Review" Journal of Clinical Medicine 11, no. 6: 1585. https://doi.org/10.3390/jcm11061585
APA StyleRansom, S. C., Brown, N. J., Pennington, Z. A., Lakomkin, N., Mikula, A. L., Bydon, M., & Elder, B. D. (2022). Hypothermia Therapy for Traumatic Spinal Cord Injury: An Updated Review. Journal of Clinical Medicine, 11(6), 1585. https://doi.org/10.3390/jcm11061585








