Impact of Alcohol and Smoking on Outcomes of HPV-Related Oropharyngeal Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Demographic and Clinical Data
2.3. Treatments
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
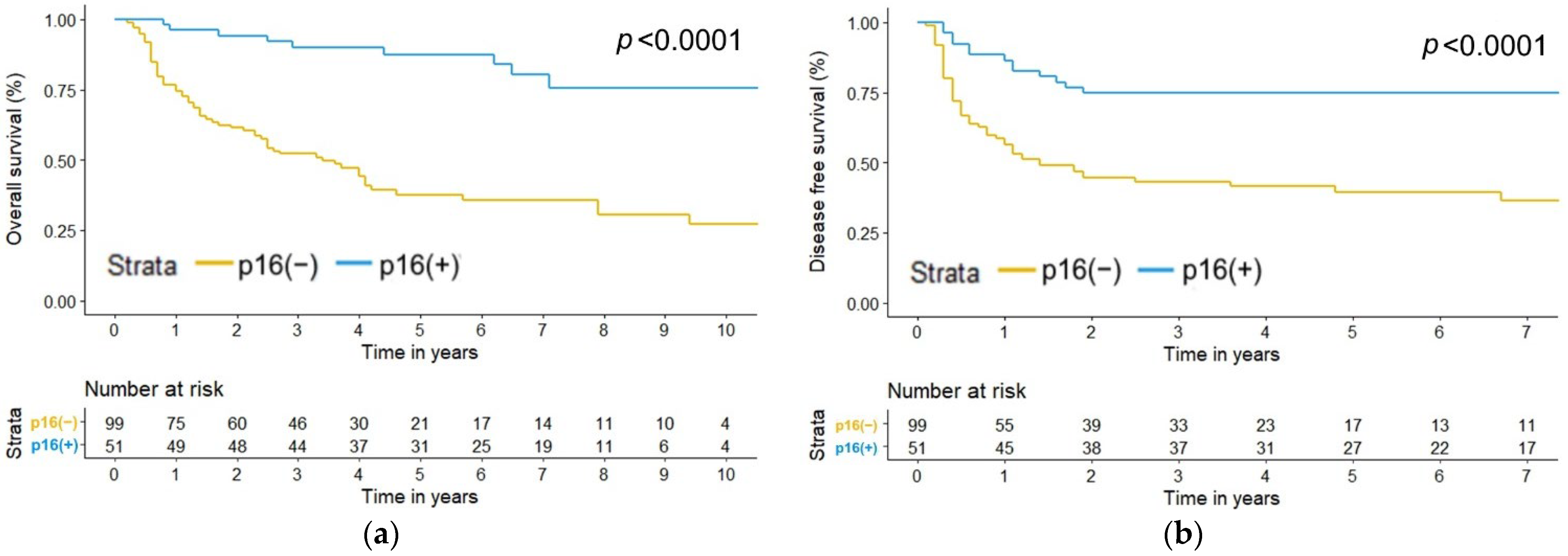
3.2. Treatment Outcomes
3.3. Factors Affecting Overall Survival (OS)
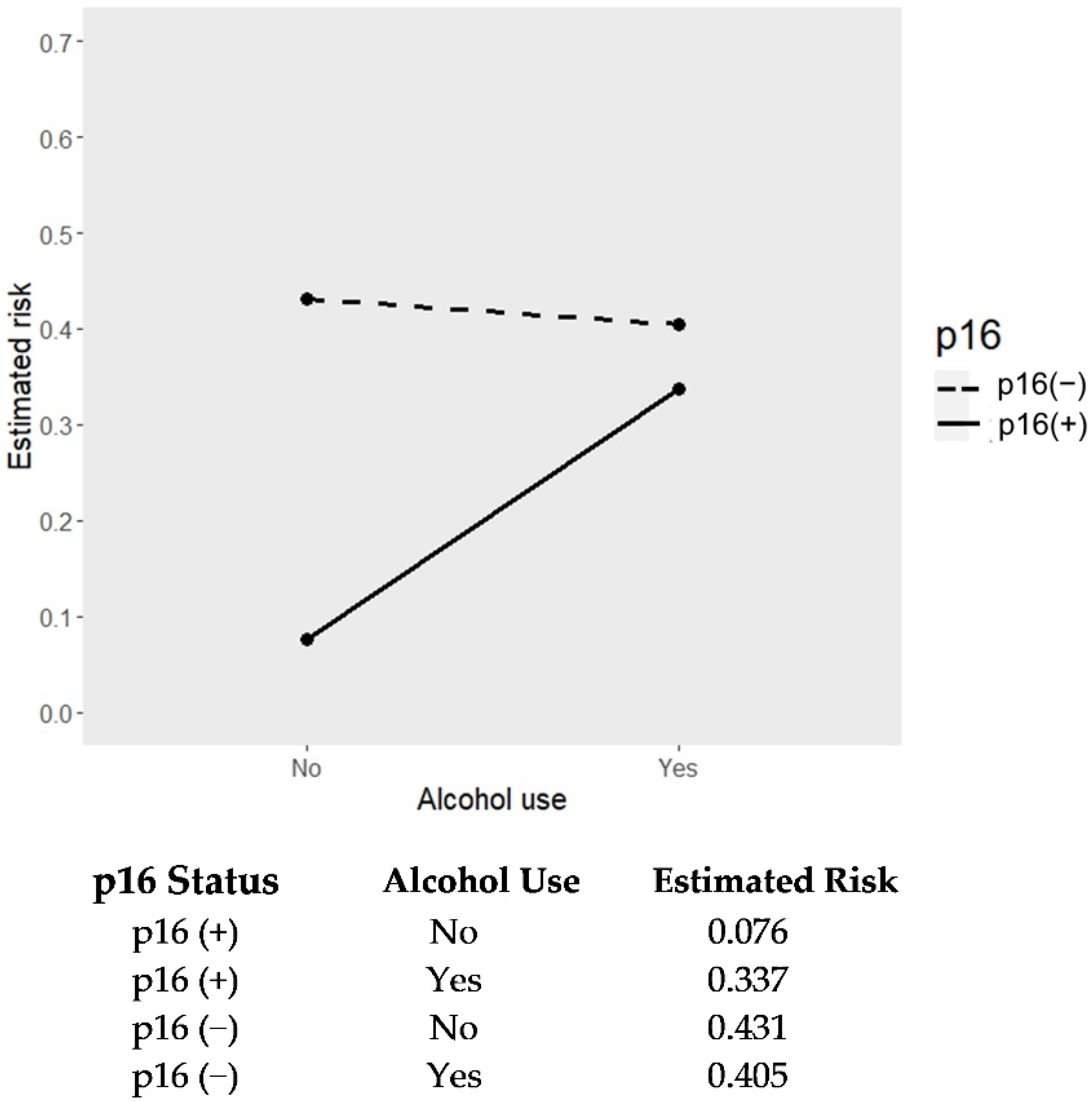
3.4. Factors Affecting Disease-Free Survival (DFS)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lechner, M.; Liu, J.; Masterson, L.; Fenton, T.R. HPV-associated oropharyngeal cancer: Epidemiology, molecular biology and clinical management. Nat. Rev. Clin. Oncol. 2022, 19, 306–327. [Google Scholar] [CrossRef]
- Carlander, A.F.; Jakobsen, K.K.; Bendtsen, S.K.; Garset-Zamani, M.; Lynggaard, C.D.; Jensen, J.S.; Grønhøj, C.; Buchwald, C.V. A Contemporary Systematic Review on Repartition of HPV-Positivity in Oropharyngeal Cancer Worldwide. Viruses 2021, 13, 1326. [Google Scholar] [CrossRef]
- Goldenberg, D.; Begum, S.; Westra, W.H.; Khan, Z.; Sciubba, J.; Pai, S.I.; Califano, J.A.; Tufano, R.P.; Koch, W.M. Cystic lymph node metastasis in patients with head and neck cancer: An HPV-associated phenomenon. Head Neck 2008, 30, 898–903. [Google Scholar] [CrossRef]
- Kreimer, A.R.; Clifford, G.M.; Boyle, P.; Franceschi, S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: A systematic review. Cancer Epidemiol. Biomark. Prev. 2005, 14, 467–475. [Google Scholar] [CrossRef]
- Scheffner, M.; Werness, B.A.; Huibregtse, J.M.; Levine, A.J.; Howley, P.M. The E6 oncoprotein encoded by human papillomavirus types 16 and 18 promotes the degradation of p53. Cell 1990, 63, 1129–1136. [Google Scholar] [CrossRef]
- Huh, K.; Zhou, X.; Hayakawa, H.; Cho, J.Y.; Libermann, T.A.; Jin, J.; Harper, J.W.; Munger, K. Human papillomavirus type 16 E7 oncoprotein associates with the cullin 2 ubiquitin ligase complex, which contributes to degradation of the retinoblastoma tumor suppressor. J. Virol. 2007, 81, 9737–9747. [Google Scholar] [CrossRef]
- McLaughlin-Drubin, M.E.; Crum, C.P.; Münger, K. Human papillomavirus E7 oncoprotein induces KDM6A and KDM6B histone demethylase expression and causes epigenetic reprogramming. Proc. Natl. Acad. Sci. USA 2011, 108, 2130–2135. [Google Scholar] [CrossRef]
- Larsen, C.G.; Gyldenløve, M.; Jensen, D.H.; Therkildsen, M.H.; Kiss, K.; Norrild, B.; Konge, L.; von Buchwald, C. Correlation between human papillomavirus and p16 overexpression in oropharyngeal tumours: A systematic review. Br. J. Cancer 2014, 110, 1587–1594. [Google Scholar] [CrossRef]
- Lydiatt, W.M.; Patel, S.G.; O’Sullivan, B.; Brandwein, M.S.; Ridge, J.A.; Migliacci, J.C.; Loomis, A.M.; Shah, J.P. Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 122–137. [Google Scholar] [CrossRef]
- Ang, K.K.; Harris, J.; Wheeler, R.; Weber, R.; Rosenthal, D.I.; Nguyen-Tân, P.F.; Westra, W.H.; Chung, C.H.; Jordan, R.C.; Lu, C.; et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N. Engl. J. Med. 2010, 363, 24–35. [Google Scholar] [CrossRef]
- Fakhry, C.; Westra, W.H.; Li, S.; Cmelak, A.; Ridge, J.A.; Pinto, H.; Forastiere, A.; Gillison, M.L. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J. Natl. Cancer Inst. 2008, 100, 261–269. [Google Scholar] [CrossRef]
- Nguyen-Tan, P.F.; Zhang, Q.; Ang, K.K.; Weber, R.S.; Rosenthal, D.I.; Soulieres, D.; Kim, H.; Silverman, C.; Raben, A.; Galloway, T.J.; et al. Randomized phase III trial to test accelerated versus standard fractionation in combination with concurrent cisplatin for head and neck carcinomas in the Radiation Therapy Oncology Group 0129 trial: Long-term report of efficacy and toxicity. J. Clin. Oncol. 2014, 32, 3858–3866. [Google Scholar] [CrossRef]
- O’Sullivan, B.; Huang, S.H.; Su, J.; Garden, A.S.; Sturgis, E.M.; Dahlstrom, K.; Lee, N.; Riaz, N.; Pei, X.; Koyfman, S.A.; et al. Development and validation of a staging system for HPV-related oropharyngeal cancer by the International Collaboration on Oropharyngeal cancer Network for Staging (ICON-S): A multicentre cohort study. Lancet Oncol. 2016, 17, 440–451. [Google Scholar] [CrossRef]
- Chen, T.C.; Wu, C.T.; Ko, J.Y.; Yang, T.L.; Lou, P.J.; Wang, C.P.; Chang, Y.L. Clinical characteristics and treatment outcome of oropharyngeal squamous cell carcinoma in an endemic betel quid region. Sci. Rep. 2020, 10, 526. [Google Scholar] [CrossRef]
- Tsai, M.H.; Cheng, Y.J.; Pao, T.H.; Hsueh, W.T.; Chen, H.H.W.; Wu, Y.H. Association of Primary Treatment Modality for Advanced-Stage Oropharyngeal Squamous Cell Carcinoma With Survival Outcomes. JAMA Netw. Open 2021, 4, e2112067. [Google Scholar] [CrossRef]
- Ko, Y.C.; Chiang, T.A.; Chang, S.J.; Hsieh, S.F. Prevalence of betel quid chewing habit in Taiwan and related sociodemographic factors. J. Oral Pathol. Med. 1992, 21, 261–264. [Google Scholar] [CrossRef]
- Hsu, W.L.; Chien, Y.C.; Chiang, C.J.; Yang, H.I.; Lou, P.J.; Wang, C.P.; Yu, K.J.; You, S.L.; Wang, L.Y.; Chen, S.Y.; et al. Lifetime risk of distinct upper aerodigestive tract cancers and consumption of alcohol, betel and cigarette. Int. J. Cancer 2014, 135, 1480–1486. [Google Scholar] [CrossRef]
- Auguste, A.; Deloumeaux, J.; Joachim, C.; Gaete, S.; Michineau, L.; Herrmann-Storck, C.; Duflo, S.; Luce, D. Joint effect of tobacco, alcohol, and oral HPV infection on head and neck cancer risk in the French West Indies. Cancer Med. 2020, 9, 6854–6863. [Google Scholar] [CrossRef]
- Kumar, R.; Rai, A.K.; Das, D.; Das, R.; Kumar, R.S.; Sarma, A.; Sharma, S.; Kataki, A.C.; Ramteke, A. Alcohol and Tobacco Increases Risk of High Risk HPV Infection in Head and Neck Cancer Patients: Study from North-East Region of India. PLoS ONE 2015, 10, e0140700. [Google Scholar] [CrossRef]
- Fakhry, C.; Westra, W.H.; Wang, S.J.; van Zante, A.; Zhang, Y.; Rettig, E.; Yin, L.X.; Ryan, W.R.; Ha, P.K.; Wentz, A.; et al. The prognostic role of sex, race, and human papillomavirus in oropharyngeal and nonoropharyngeal head and neck squamous cell cancer. Cancer 2017, 123, 1566–1575. [Google Scholar] [CrossRef]
- Marur, S.; Li, S.; Cmelak, A.J.; Gillison, M.L.; Zhao, W.J.; Ferris, R.L.; Westra, W.H.; Gilbert, J.; Bauman, J.E.; Wagner, L.I.; et al. E1308: Phase II Trial of Induction Chemotherapy Followed by Reduced-Dose Radiation and Weekly Cetuximab in Patients With HPV-Associated Resectable Squamous Cell Carcinoma of the Oropharynx- ECOG-ACRIN Cancer Research Group. J. Clin. Oncol. 2017, 35, 490–497. [Google Scholar] [CrossRef] [PubMed]
- Hegde, J.V.; Shaverdian, N.; Felix, C.; Wang, P.C.; Veruttipong, D.; Hsu, S.; Riess, J.W.; Rao, S.D.; Daly, M.E.; Chen, A.M. Functional Outcomes After De-escalated Chemoradiation Therapy for Human Papillomavirus-Positive Oropharyngeal Cancer: Secondary Analysis of a Phase 2 Trial. Int. J. Radiat. Oncol. Biol. Phys. 2018, 100, 647–651. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.M.; Felix, C.; Wang, P.C.; Hsu, S.; Basehart, V.; Garst, J.; Beron, P.; Wong, D.; Rosove, M.H.; Rao, S.; et al. Reduced-dose radiotherapy for human papillomavirus-associated squamous-cell carcinoma of the oropharynx: A single-arm, phase 2 study. Lancet Oncol. 2017, 18, 803–811. [Google Scholar] [CrossRef]
- Vickers, A.J.; Steineck, G. Prognosis, Effect Modification, and Mediation. Eur. Urol. 2018, 74, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Principe, D.R.; Kamath, S.D.; Korc, M.; Munshi, H.G. The immune modifying effects of chemotherapy and advances in chemo-immunotherapy. Pharmacol. Ther. 2022, 236, 108111. [Google Scholar] [CrossRef]
- Clark, G.M. Prognostic factors versus predictive factors: Examples from a clinical trial of erlotinib. Mol. Oncol. 2008, 1, 406–412. [Google Scholar] [CrossRef]
- Lee, W.T.; Hsiao, J.R.; Ou, C.Y.; Huang, C.C.; Chang, C.C.; Tsai, S.T.; Chen, K.C.; Huang, J.S.; Wong, T.Y.; Lai, Y.H.; et al. The Influence of Prediagnosis Alcohol Consumption and the Polymorphisms of Ethanol-Metabolizing Genes on the Survival of Head and Neck Cancer Patients. Cancer Epidemiol. Biomark. Prev. 2019, 28, 248–257. [Google Scholar] [CrossRef]
- Bouland, C.; Dequanter, D.; Lechien, J.R.; Hanssens, C.; De Saint Aubain, N.; Digonnet, A.; Javadian, R.; Yanni, A.; Rodriguez, A.; Loeb, I.; et al. Prognostic Significance of a Scoring System Combining p16, Smoking, and Drinking Status in a Series of 131 Patients with Oropharyngeal Cancers. Int. J. Otolaryngol. 2021, 2021, 8020826. [Google Scholar] [CrossRef]
- Saito, Y.; Yoshida, M.; Ushiku, T.; Omura, G.; Ebihara, Y.; Shimono, T.; Fukayama, M.; Yamasoba, T.; Asakage, T. Prognostic value of p16 expression and alcohol consumption in Japanese patients with oropharyngeal squamous cell carcinoma. Cancer 2013, 119, 2005–2011. [Google Scholar] [CrossRef]
- Sinha, P.; Logan, H.L.; Mendenhall, W.M. Human papillomavirus, smoking, and head and neck cancer. Am. J. Otolaryngol. 2012, 33, 130–136. [Google Scholar] [CrossRef]
- Anantharaman, D.; Muller, D.C.; Lagiou, P.; Ahrens, W.; Holcátová, I.; Merletti, F.; Kjærheim, K.; Polesel, J.; Simonato, L.; Canova, C.; et al. Combined effects of smoking and HPV16 in oropharyngeal cancer. Int. J. Epidemiol. 2016, 45, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Gillison, M.L.; Zhang, Q.; Jordan, R.; Xiao, W.; Westra, W.H.; Trotti, A.; Spencer, S.; Harris, J.; Chung, C.H.; Ang, K.K. Tobacco smoking and increased risk of death and progression for patients with p16-positive and p16-negative oropharyngeal cancer. J. Clin. Oncol. 2012, 30, 2102–2111. [Google Scholar] [CrossRef] [PubMed]
- Hong, A.M.; Martin, A.; Chatfield, M.; Jones, D.; Zhang, M.; Armstrong, B.; Lee, C.S.; Harnett, G.; Milross, C.; Clark, J.; et al. Human papillomavirus, smoking status and outcomes in tonsillar squamous cell carcinoma. Int. J. Cancer 2013, 132, 2748–2754. [Google Scholar] [CrossRef] [PubMed]
- Hafkamp, H.C.; Manni, J.J.; Haesevoets, A.; Voogd, A.C.; Schepers, M.; Bot, F.J.; Hopman, A.H.; Ramaekers, F.C.; Speel, E.J. Marked differences in survival rate between smokers and nonsmokers with HPV 16-associated tonsillar carcinomas. Int. J. Cancer 2008, 122, 2656–2664. [Google Scholar] [CrossRef]
- Lassen, P.; Lacas, B.; Pignon, J.P.; Trotti, A.; Zackrisson, B.; Zhang, Q.; Overgaard, J.; Blanchard, P. Prognostic impact of HPV-associated p16-expression and smoking status on outcomes following radiotherapy for oropharyngeal cancer: The MARCH-HPV project. Radiother. Oncol. 2018, 126, 107–115. [Google Scholar] [CrossRef]
- Chen, S.Y.; Massa, S.; Mazul, A.L.; Kallogjeri, D.; Yaeger, L.; Jackson, R.S.; Zevallos, J.; Pipkorn, P. The association of smoking and outcomes in HPV-positive oropharyngeal cancer: A systematic review. Am. J. Otolaryngol. 2020, 41, 102592. [Google Scholar] [CrossRef]
- Chidambaram, S.; Nakken, E.R.; Kennedy, W.; Thorstad, W.L.; Chen, S.Y.; Pipkorn, P.; Zevallos, J.P.; Mazul, A.L. Prognostic Significance of Smoking in Human Papillomavirus-Positive Oropharyngeal Cancer Under American Joint Committee on Cancer Eighth Edition Stage. Laryngoscope 2020, 130, 1961–1966. [Google Scholar] [CrossRef]
- Chen, S.Y.; Last, A.; Ettyreddy, A.; Kallogjeri, D.; Wahle, B.; Chidambaram, S.; Mazul, A.; Thorstad, W.; Jackson, R.S.; Zevallos, J.P.; et al. 20 pack-year smoking history as strongest smoking metric predictive of HPV-positive oropharyngeal cancer outcomes. Am. J. Otolaryngol. 2021, 42, 102915. [Google Scholar] [CrossRef]
- Huang, S.H.; Xu, W.; Waldron, J.; Siu, L.; Shen, X.; Tong, L.; Ringash, J.; Bayley, A.; Kim, J.; Hope, A.; et al. Refining American Joint Committee on Cancer/Union for International Cancer Control TNM stage and prognostic groups for human papillomavirus-related oropharyngeal carcinomas. J. Clin. Oncol. 2015, 33, 836–845. [Google Scholar] [CrossRef]
- Vawda, N.; Banerjee, R.N.; Debenham, B.J. Impact of Smoking on Outcomes of HPV-related Oropharyngeal Cancer Treated with Primary Radiation or Surgery. Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 1125–1131. [Google Scholar] [CrossRef]
- Hsiao, J.R.; Huang, C.C.; Ou, C.Y.; Chang, C.C.; Lee, W.T.; Tsai, S.T.; Huang, J.S.; Chen, K.C.; Lai, Y.H.; Wu, Y.H.; et al. Investigating the health disparities in the association between lifestyle behaviors and the risk of head and neck cancer. Cancer Sci. 2020, 111, 2974–2986. [Google Scholar] [CrossRef] [PubMed]
| Variable | p16 (−), n = 99 | p16 (+), n = 51 | p-Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Male, n, % | 93 | 93.94 | 37 | 72.55 | <0.001 |
| Female, n, % | 6 | 6.06 | 14 | 27.45 | <0.001 |
| Age, mean, SD | 53.3 | 9.22 | 56.7 | 9.71 | 0.036 |
| Age, n, % | 0.085 | ||||
| <50 | 36 | 36.36 | 10 | 19.61 | |
| 50–59 | 35 | 35.35 | 20 | 39.22 | |
| ≥60 | 28 | 28.28 | 21 | 41.18 | |
| Cigarette smoking, n, % | 91 | 91.92 | 26 | 50.98 | <0.001 |
| Smoking age (pack-years), mean, SD | 31.8 | 26.8 | 14.4 | 17.9 | <0.001 |
| Smoking age (pack-years), n, % | <0.001 | ||||
| 0 | 8 | 8.08 | 25 | 49.02 | |
| 1–9 | 7 | 7.07 | 3 | 5.88 | |
| 10–19 | 14 | 14.14 | 0 | 0.00 | |
| 20–29 | 18 | 18.18 | 10 | 19.61 | |
| ≥30 | 52 | 52.53 | 13 | 25.49 | |
| Alcohol use, n, % | 86 | 86.87 | 26 | 50.98 | <0.001 |
| Betel quid chewing, n, % | 76 | 76.77 | 10 | 19.61 | <0.001 |
| ABC concomitant use, n, % | <0.001 | ||||
| 3 | 70 | 70.7 | 9 | 17.65 | |
| 2 of 3 | 20 | 20.2 | 12 | 23.53 | |
| Tumor subsite, n, % | 0.002 | ||||
| Tonsil | 47 | 47.47 | 40 | 78.43 | |
| Soft palate | 22 | 22.22 | 6 | 11.76 | |
| Tongue base | 23 | 23.23 | 5 | 9.80 | |
| Posterior pharyngeal wall | 7 | 7.07 | 0 | 0.00 | |
| Clinical stage (AJCC 7th ed.), n, % | 0.041 | ||||
| Stage I | 2 | 2.02 | 1 | 1.96 | |
| Stage II | 7 | 7.07 | 0 | 0.00 | |
| Stage III | 6 | 6.06 | 9 | 17.65 | |
| Stage IVA | 68 | 68.69 | 37 | 72.55 | |
| Stage IVB | 16 | 16.16 | 4 | 7.84 | |
| Clinical stage (AJCC 8th ed.), n, % | <0.001 | ||||
| Stage I | 2 | 2.02 | 26 | 50.98 | |
| Stage II | 7 | 7.07 | 15 | 29.41 | |
| Stage III | 5 | 5.05 | 10 | 19.61 | |
| Stage IVA | 55 | 55.56 | 0 * | 0.00 * | |
| Stage IVB | 30 | 30.3 | 0 * | 0.00 * | |
| Initial treatment, n, % | 0.024 | ||||
| Surgery | 32 | 32.32 | 7 | 13.73 | |
| RT-based therapy | 67 | 67.68 | 44 | 86.27 | |
| CCRT | 66 | 66.67 | 40 | 78.43 | |
| RT only | 1 | 1.01 | 4 | 7.84 | |
| Disease relapse, n, % | 58 | 58.59 | 13 | 25.49 | <0.001 |
| LRR | 25 | 25.25 | 6 | 11.76 | |
| DM | 18 | 18.18 | 5 | 9.80 | |
| LRR + DM | 15 | 15.15 | 2 | 3.92 | |
| Mortality, n, % | 61 | 61.62 | 9 | 17.65 | <0.001 |
| DOD | 47 | 47.47 | 5 | 9.80 | |
| Dead, other reason | 14 | 14.14 | 4 | 7.84 | |
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Stepwise Selection * | Selected Predictors # | |||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Covariate | ||||||
| p16 (ref. = negative) | 0.18 | (0.09, 0.37) | 0.08 | (0.02, 0.35) | 0.09 | (0.02, 0.44) |
| Gender (ref. = male) | 0.15 | (0.04, 0.60) | 0.52 | (0.12, 2.33) | ||
| Age (5-year increments) | 0.89 | (0.78, 1.02) | ||||
| Clinical stage (ref. = stage I–III) & | ||||||
| Stage IVA | 2.69 | (1.07, 6.76) | 2.55 | (1.00, 6.49) | 2.72 | (1.05, 7.00) |
| Stage IVB | 12.11 | (4.41, 33.26) | 16.26 | (5.76, 45.86) | 15.62 | (5.29, 46.13) |
| Tumor subsite (ref. = other sites than tonsil) | 0.46 | (0.28, 0.73) | 0.77 | (0.45, 1.33) | ||
| Initial treatment (ref. = surgery) | 0.88 | (0.52, 1.48) | 1.02 | (0.58, 1.81) | ||
| Smoking age (ref. = <20 pack-years) | ||||||
| 20–29 | 1.78 | (0.85, 3.70) | 0.96 | (0.41, 2.23) | 1.15 | (0.46, 2.90) |
| ≥30 | 2.98 | (1.67, 5.32) | 1.90 | (1.02, 3.54) | 2.05 | (1.05, 4.00) |
| Alcohol use (ref. = none) | 3.19 | (1.58, 6.44) | 0.90 | (0.39, 2.08) | ||
| Betel quid chewing (ref. = none) | 2.35 | (1.40, 3.96) | 0.85 | (0.45, 1.61) | ||
| Interaction term | ||||||
| p16: Smoking age (20–29 pack-years) | 8.00 | (1.16, 55.01) | 5.74 | (0.79, 41.53) | ||
| p16: Smoking age (≥30 pack-years) | 2.94 | (0.43, 19.93) | 2.53 | (0.36, 17.85) | ||
| p16: Alcohol use | ||||||
| p16: Betel quid chewing | ||||||
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Stepwise Selection * | Selected Predictors # | |||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Covariate | ||||||
| p16 (ref. = negative) | 0.31 | (0.17, 0.56) | 0.12 | (0.03–0.58) | 0.10 | (0.02, 0.49) |
| Gender (ref. = male) | 0.32 | (0.12, 0.88) | 1.12 | (0.36, 3.42) | ||
| Age (5-year increments) | 0.98 | (0.87, 1.11) | 1.12 | (0.97–1.28) | ||
| Clinical stage (ref. = stage I–III) & | ||||||
| Stage IVA | 2.75 | (1.09, 6.90) | 3.6 | (1.37–9.45) | 2.87 | (1.11, 7.41) |
| Stage IVB | 10.68 | (3.88, 29.41) | 12.35 | (4.09–37.26) | 8.43 | (2.83, 25.08) |
| Tumor subsite (ref. = other sites than tonsil) | 0.34 | (0.21, 0.55) | 0.49 | (0.26–0.83) | 0.46 | (0.27, 0.80) |
| Initial treatment (ref. = surgery) | 1.05 | (0.62, 1.78) | 1.21 | (0.68, 2.16) | ||
| Smoking age (ref. = <20 pack-years) | ||||||
| 20–29 | 1.43 | (0.71, 2.88) | 1.69 | (0.77–3.70) | 1.64 | (0.74, 3.63) |
| ≥30 | 2.07 | (1.20, 3.55) | 1.88 | (1.01–3.49) | 1.99 | (1.06, 3.75) |
| Alcohol use (ref. = none) | 2.68 | (1.37, 5.23) | 0.66 | (0.27–1.62) | 0.57 | (0.23, 1.39) |
| Betel quid chewing (ref. = none) | 1.77 | (1.08, 2.92) | 0.91 | (0.48, 1.72) | ||
| Interaction term | ||||||
| p16: Smoking age (20–29 pack-years) | ||||||
| p16: Smoking age (≥30 pack-years) | ||||||
| p16: Alcohol use | 4.4 | (0.78–24.7) | 6.00 | (1.03, 35.01) | ||
| p16: Betel quid chewing | ||||||
| Smoking Age | Follow-Up | p16 (+) | |
|---|---|---|---|
| Absolute Risk (95% CI) | Absolute Risk (95% CI) | ||
| Alcohol (−) | Alcohol (+) | ||
| <20 pack-years | 3 years | 0.12 (0.11, 0.14) | 0.33 (0.24, 0.39) |
| 5 years | 0.14 (0.12, 0.15) | 0.35 (0.26, 0.42) | |
| 20–29 pack-years | 3 years | 0.19 (0.18, 0.20) | 0.45 (0.35, 0.51) |
| 5 years | 0.21 (0.20, 0.21) | 0.47 (0.37, 0.54) | |
| ≥30 pack-years | 3 years | 0.22 (0.21, 0.24) | 0.50 (0.38, 0.57) |
| 5 years | 0.24 (0.22, 0.25) | 0.52 (0.41, 0.59) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lai, Y.-H.; Su, C.-C.; Wu, S.-Y.; Hsueh, W.-T.; Wu, Y.-H.; Chen, H.H.W.; Hsiao, J.-R.; Liu, C.-H.; Tsai, Y.-S. Impact of Alcohol and Smoking on Outcomes of HPV-Related Oropharyngeal Cancer. J. Clin. Med. 2022, 11, 6510. https://doi.org/10.3390/jcm11216510
Lai Y-H, Su C-C, Wu S-Y, Hsueh W-T, Wu Y-H, Chen HHW, Hsiao J-R, Liu C-H, Tsai Y-S. Impact of Alcohol and Smoking on Outcomes of HPV-Related Oropharyngeal Cancer. Journal of Clinical Medicine. 2022; 11(21):6510. https://doi.org/10.3390/jcm11216510
Chicago/Turabian StyleLai, Yu-Hsuan, Chien-Chou Su, Shang-Yin Wu, Wei-Ting Hsueh, Yuan-Hua Wu, Helen H. W. Chen, Jenn-Ren Hsiao, Ching-Hsun Liu, and Yi-Shan Tsai. 2022. "Impact of Alcohol and Smoking on Outcomes of HPV-Related Oropharyngeal Cancer" Journal of Clinical Medicine 11, no. 21: 6510. https://doi.org/10.3390/jcm11216510
APA StyleLai, Y.-H., Su, C.-C., Wu, S.-Y., Hsueh, W.-T., Wu, Y.-H., Chen, H. H. W., Hsiao, J.-R., Liu, C.-H., & Tsai, Y.-S. (2022). Impact of Alcohol and Smoking on Outcomes of HPV-Related Oropharyngeal Cancer. Journal of Clinical Medicine, 11(21), 6510. https://doi.org/10.3390/jcm11216510









