Pain in Tourette Syndrome-Children’s and Parents’ Perspectives
Abstract
:1. Introduction
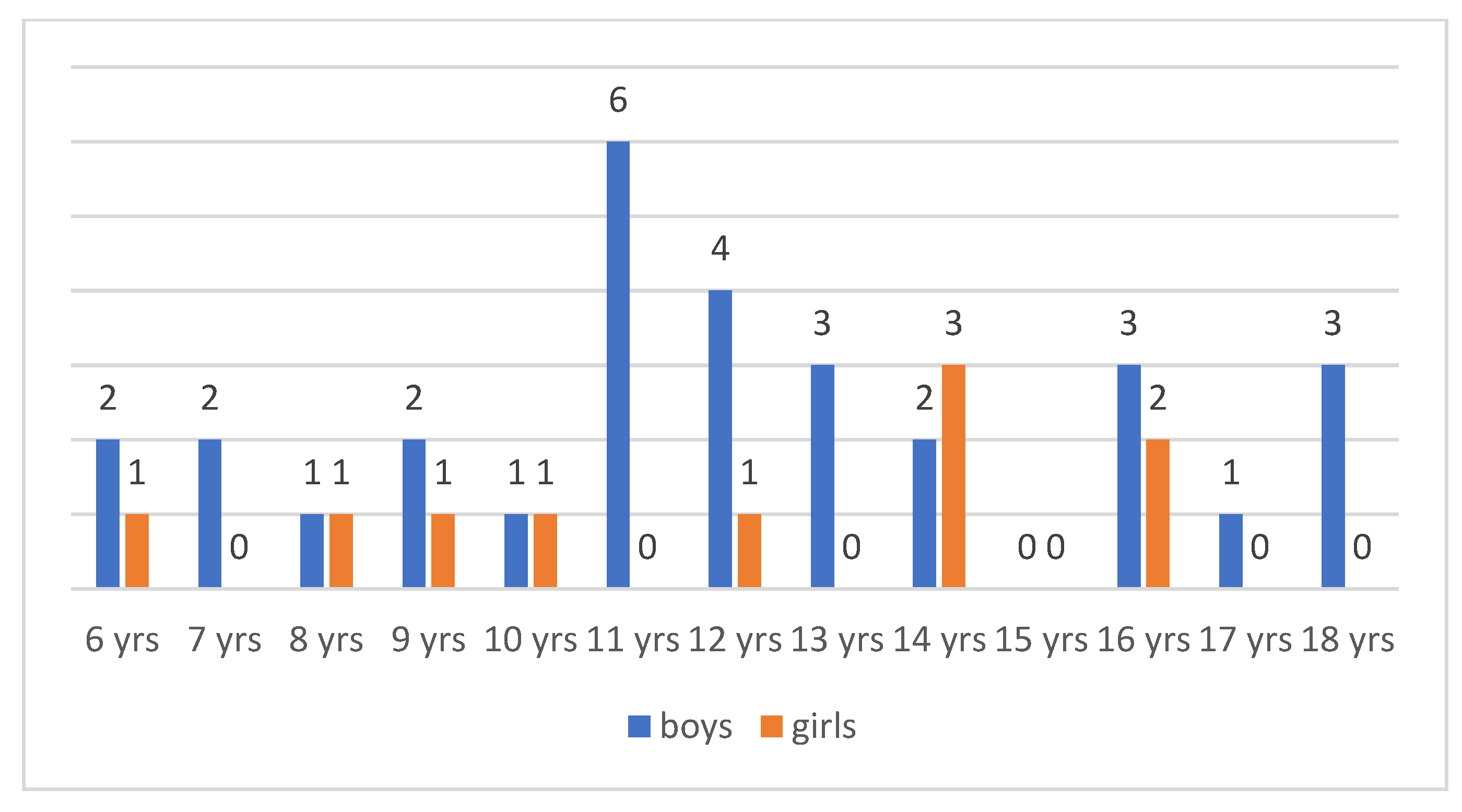
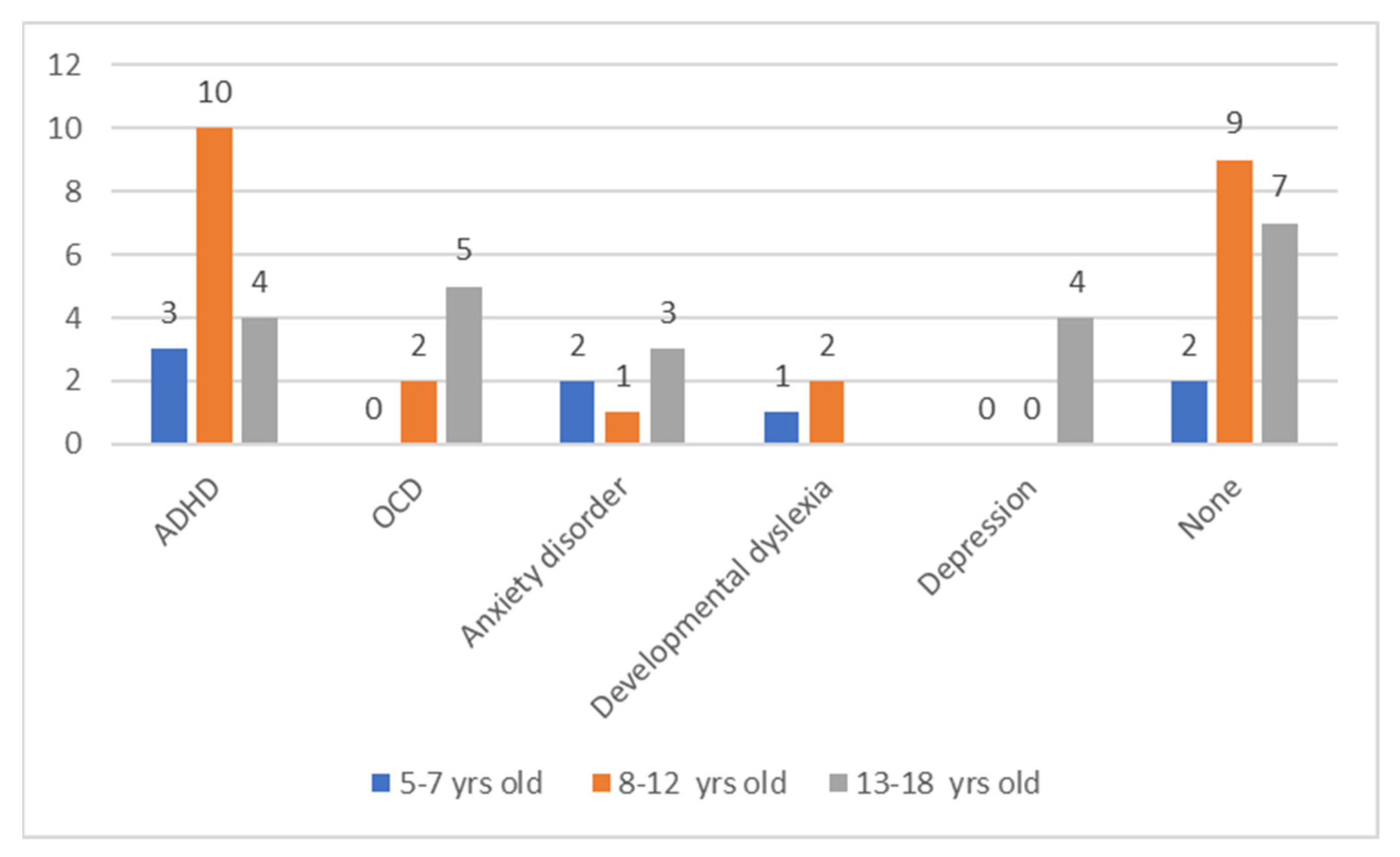
2. Materials and Methods
3. Results
3.1. Pain Severity
3.2. Location of Pain
3.3. Pain Descriptors
3.4. Pain Coping Strategies
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Robertson, M.M.; Cavanna, A. Zespół Tourette’a. Fakty; Wydawnictwo Czarno na Białym: Warszawa, Poland, 2013. [Google Scholar]
- Wolańczyk, T.; Stefanoff, P.; Komender, J. Zaburzenia tikowe. In Postępy w Diagnostyce i Leczeniu Chorób Układu Nerwowego u Dzieci, 2; Jóźwiak, S., Ed.; BiFolium: Lublin, Poland, 2000; pp. 84–100. [Google Scholar]
- Ganos, C.; Roessner, V.; Munchau, A. The functional anatomy of Gilles de la Tourette syndrome. Neurosci. Biobehav. Rev. 2013, 37, 1050–1062. [Google Scholar] [CrossRef]
- Caligiore, D.; Mannella, F.; Arbib, M.A.; Baldassarre, G. Dysfunctions of the basal ganglia-cerebellar-thalamo-cortical system produce motor tics in Tourette syndrome. PLoS Comput. Biol. 2017, 13, e1005395. [Google Scholar] [CrossRef] [PubMed]
- Cavanna, A.E.; Critchley, H.D.; Orth, M.; Stern, J.S.; Young, M.-B.; Robertson, M.M. Dissecting the Gilles de la Tourette spectrum: A factor analytic study on 639 patients. J. Neurol. Neurosurg. Psychiatry 2011, 82, 1320–1323. [Google Scholar] [CrossRef] [PubMed]
- Ludolph, A.G.; Roessner, V.; Münchau, A.; Müller-Vahl, K. Tourette Syndrome and Other Tic Disorders in Childhood, Adolescence and Adulthood. Dtsch. Aerzteblatt Int. 2012, 109, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Małek, A.; Golińska, P. Depression in Tourette Syndrome. Psychiatr. Polska 2020, 54, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Müller-Vahl, K.; Dodel, I.; Müller, N.; Münchau, A.; Reese, J.P.; Balzer-Geldsetzer, M.; Dodel, R.; Oertel, W.H. Health-related quality of life in patients with Gilles de la Tourette’s syndrome. Mov. Disord. 2010, 25, 309–314. [Google Scholar] [CrossRef]
- Lavenstein, B.; Miyares, L.; Dodge, L. Pain in Childhood Tourette Syndrome-Retrospective Analysis. Neurology 2016, 86 (Suppl. 16), 3. [Google Scholar]
- Bearpark, J.; Mujong, D.P.; Seri, S.; Cavanna, A.E. Headache in patients with Tourette syndrome: A systematic literature review. Cephalalgia Rep. 2020, 3, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Cha, S.; Perret, D.; Hata, J. Case report: Reduction in pain related to Tourette associated motor tic following botulinum toxin injection. J. Pain 2012, 13, 92. [Google Scholar] [CrossRef]
- Riley, D.E.; Lang, A.E. Pain in Gilles de la Tourette Syndrome and Related Tic Disorders. Can. J. Neurol. Sci. 1989, 16, 439–441. [Google Scholar] [CrossRef] [Green Version]
- Kenney, C.; Kuo, S.-H.; Jimenez-Shahed, J. Tourette’s Syndrome. Am. Fam. Phys. 2008, 77, 651–658. [Google Scholar]
- Leckman, J.F.; Riddle, M.A.; Hardin, M.T.; Ort, S.I.; Swartz, K.L.; Stevenson, J.; Cohen, D.J. The Yale Global Tic Severity Scale: Initial Testing of a Clinician-Rated Scale of Tic Severity. J. Am. Acad. Child Adolesc. Psychiatry 1989, 28, 566–573. [Google Scholar] [CrossRef]
- Stefanoff, P.; Wolańczyk, T. Rzetelność i trafność polskiej adaptacji Globalnej Skali Nasilenia Tików (YGTSS) w badaniu uczniów szkół warszawskich w wieku 12–15 lat. Prz. Epidemiol. 2005, 59, 753–762. [Google Scholar]
- Varni, J.W.; Thompson, K.L.; Hanson, V. The Varni/Thompson Pediatric Pain Questionnaire: I. Chronic musculoskeletal pain in juvenile rheumatoid arthritis. Pain 1987, 28, 27–38. [Google Scholar] [CrossRef]
- Varni, J.W.; Waldron, S.A.; Gragg, R.A.; Rapoff, M.A.; Bernstein, B.H.; Lindsley, C.B.; Newcomb, M.D. Development of the Waldron/Varni Pediatric Pain Coping Inventory. Pain 1996, 67, 141–150. [Google Scholar] [CrossRef]
- Topcu, S.Y. Relations among Pain, Pain Beliefs, and Psychological Well-Being in Patients with Chronic Pain. Pain Manag. Nurs. 2018, 19, 637–644. [Google Scholar] [CrossRef]
- Mara, C.A.; Kashikar-Zuck, S.; Cunningham, N.; Goldschneider, K.R.; Huang, B.; Dampier, C.; Sherry, D.D.; Crosby, L.; Miller, J.F.; Barnett, K.; et al. Development and Psychometric Evaluation of the PROMIS Pediatric Pain Intensity Measure in Children and Adolescents with Chronic Pain. J. Pain 2021, 22, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Benestad, B.; Vinje’, O.; Veiernrd, M.B.; Vandvik, H. Quantitative and Qualitative Assessments of Pain in Children with Juvenile Chronic Arthritis Based on the Norwegian Version of the Pediatric Pain Questionnaire. Scand. J. Rheumatol 1996, 25, 293–299. [Google Scholar] [CrossRef]
- Jaaniste, T.; Noel, M.; von Baeyer, C.L. Young children’s ability to report on past, future, and hypothetical pain states. Pain 2016, 157, 2399–2409. [Google Scholar] [CrossRef] [PubMed]
- Wiesenfeld-Hallin, Z. Sex differences in pain perception. Gend. Med. 2005, 2, 137–145. [Google Scholar] [CrossRef]
- Failo, A.; Beals-Erickson, S.E.; Venuti, P. Coping strategies and emotional well-being in children with disease-related pain. J. Child Health Care 2017, 22, 84–96. [Google Scholar] [CrossRef]
- Hay, I.; Oates, J.; Giannini, A.; Berkowitz, R.; Rotenberg, B. Pain Perception of Children Undergoing Nasendoscopy for Investigation of Voice and Resonance Disorders. J. Voice 2009, 23, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Twycross, A. Pain: A Bio-Psycho-Social Phenomenon. In Managing Pain in Children: A Clinical Guide for Nurses and Healthcare Professionals; Twycross, A., Dowden, S., Bruce, E., Eds.; Wiley-Blackwell: Chichester, UK, 2014; pp. 36–47. [Google Scholar]
- Gil, K.M.; Thompson, R.G., Jr.; Keith, B.R.; Tota-Faucette, M.; Noll, S.; Kinney, T.R. Sickle Cell Disease Pain in Children and Adolescents: Change in Pain Frequency and Coping Strategies Over Time. J. Pediatr. Psychol. 1993, 18, 621–637. [Google Scholar] [CrossRef]
- Hermann, C.; Hohmeister, J.; Zohsel, K.; Ebinger, F.; Flor, H. The assessment of pain coping and pain-related cognitions in children and adolescents: Current methods and further development. J. Pain 2007, 8, 802–813. [Google Scholar] [CrossRef]
- Chaleat-Valayer, E.; Roumenoff, F.; Bard-Pondarre, R.; Ganne, C.; Verdun, S.; Lucet, A.; Bernard, J.-C. Pain coping strategies in children with cerebral palsy. Dev. Med. Child Neurol. 2019, 61, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Branson, S.M.; Craig, K.D. Children’s spontaneous strategies for coping with pain: A review of the literature. Can. J. Behav. Sci. Rev. Can. Sci. Comport. 1988, 20, 402–412. [Google Scholar] [CrossRef]
- Emerson, N.D.; Bursch, B. Communicating with Youth about Pain: Developmental Considerations. Children 2020, 7, 184. [Google Scholar] [CrossRef]
- McGrath, P.J.; Craigh, K.D. Developmental and Psychological Factors in Children’s Pain. Pediatr. Clin. N. Am. 1989, 36, 823–836. [Google Scholar] [CrossRef]
- Evans, J.; Seri, S.; Cavanna, A.E. The effects of Gilles de la Tourette syndrome and other chronic tic disorders on quality of life across the lifespan: A systematic review. Eur. Child Adolesc. Psychiatry 2016, 25, 939–948. [Google Scholar] [CrossRef] [Green Version]
- Nelson, S.; Moorman, E.; Farrell, M.; Cunningham, N. Irritability is Common and is Related to Poorer Psychosocial Outcomes in Youth with Functional Abdominal Pain Disorders (FAPD). Children 2018, 5, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piacentini, J.; Woods, D.W.; Scahill, L.; Wilhelm, S.; Peterson, A.L.; Chang, S.; Ginsburg, G.S.; Deckersbach, T.; Dziura, J.; Levi-Pearl, S.; et al. Behavior Therapy for Children with Tourette Disorder. JAMA 2010, 303, 1929–1937. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tilling, F.; Cavanna, A.E. Relaxation therapy as a treatment for tics in patients with Tourette syndrome: A systematic literature review. Neurol. Sci. 2019, 41, 1011–1017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheng, J.; Liu, S.; Wang, Y.; Cui, R.; Zhang, X. The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plast. 2017, 2017, 9724371. [Google Scholar] [CrossRef] [PubMed]
- Apkarian, A.V.; Bushnell, M.C.; Treede, R.-D.; Zubieta, J.-K. Human brain mechanisms of pain perception and regulation in health and disease. Eur. J. Pain 2005, 9, 463. [Google Scholar] [CrossRef] [PubMed]
| Type of Pain | |
|---|---|
| Exertional | Muscular pain due to excessive contraction |
| Skeletal or joint pain | |
| Neuropathic pain (due to spinal cord, radicular or peripheral nerve compression) | |
| Traumatic | Pain in a body part struck by a moving limb |
| Pain in a moving body part striking something nearby | |
| Self-mutilation (including biting) | |
| Pain from compulsive touching of hot or sharp objects | |
| Pain inflicted on others from tics or compulsions | |
| Pain Caused by Suppression of Tics | |
| Pain Relieving Tics |
| YGTSS | ||
|---|---|---|
| Child | Present pain | 0.860 * |
| Worst pain | 0.744 * | |
| Parent | Present pain | 0.843 * |
| Worst pain | 0.772 * |
| Child (n = 40) Median (Mean, SD) | Parent (n = 57) Median (Mean, SD) | p | |
|---|---|---|---|
| Present pain | 1.0 (2.0; 2.5) | 1.0 (2.2; 2.6) | 0.720 |
| Worst pain | 3.0 (3.1; 2.9) | 4.0 (3.9; 3.3) | 0.265 |
| Boys (n = 31) Median (Mean, SD) | Girls (n = 9) Median (Mean, SD) | p | |
|---|---|---|---|
| Present pain | 1.0 (1.9; 2.3) | 1.0 (2.5; 3.1) | 0.726 |
| Worst pain | 3.0 (3.1; 2.9) | 2.5 (3.2; 3.2) | 0.824 |
| Mothers (n = 35) Median (Mean, SD) | Fathers (n = 22) Median (Mean, SD) | p | |
|---|---|---|---|
| Present pain | 1.0 (2.3; 2.8) | 1.0 (1.9; 2.1) | 0.940 |
| Worst pain | 4.0 (3.7; 3.3) | 3.5 (3.9; 3.3) | 0.561 |
| Pain Descriptors (%) | |
|---|---|
| Child | sharp (84) |
| stinging (75) | |
| burning (63) | |
| pressure (54) | |
| exhausting (42) | |
| stabbing (29) | |
| tingling (17) | |
| Parent | sharp (72) |
| stinging (56) | |
| stabbing (54) | |
| pressure (39) | |
| nagging (21) |
| Child (5–12 years) (n = 9) (%) | Parent (n = 17) (%) | ||
|---|---|---|---|
| Pain Coping Strategies | Wish for it to go away | 60.9 | 70.0 |
| Try not to think about the pain or ignore the pain | 56.5 | 55.5 | |
| Try to be brave and not say anything | 56.5 | 63.0 | |
| Tell my mother or father | 56.5 | 62.9 | |
| Play a game | 52.2 | 37.0 | |
| Have my mother, father or a friend sit with me | 47.8 | 55.5 | |
| Imagine I can make the pain or hurt disappear by myself | 47.8 | 25.9 | |
| Know that I can ask for something that will make the pain or hurt feel better | 47.8 | 55.6 | |
| Tell myself to be brave | 43.4 | 55.5 | |
| Tell myself that it will be alright | 43.4 | 55.5 | |
| Go to sleep until it feels better | 43.4 | 59.2 | |
| Go to bed | 39.1 | 55.5 | |
| Ask for medicine | 39.1 | 33.3 | |
| Ask for a hug or kiss | 39.1 | 51.8 | |
| Rub the sore spot | 39.1 | 40.7 |
| Adolescent (13–18 years) (n = 15) (%) | Parent (n = 24) (%) | ||
|---|---|---|---|
| Pain Coping Strategies | Go to bed | 76.5 | 76.7 |
| Ask to be left alone | 76.5 | 46.7 | |
| Lie down | 70.6 | 70.0 | |
| Sleep it off | 70.6 | 77.7 | |
| Try to be strong and not say anything | 70.6 | 76.6 | |
| Wish for it to go away | 70.6 | 70.0 | |
| Visit with my friends | 64.7 | 53.3 | |
| Play a game | 64.7 | 63.4 | |
| Try not to think about the pain or ignore the pain | 64.7 | 70.0 | |
| Tell myself that it will be alright | 58.8 | 66.7 | |
| Watch TV | 58.8 | 70.0 | |
| Rub the sore spot | 58.8 | 50.0 | |
| Imagine I can make the pain disappear by myself | 52.9 | 46.6 | |
| Cry or yell | 35.5 | 40.0 | |
| Get angry, irritable, or cranky | 58.8 | 60.0 | |
| Tell myself I can handle it | 56.6 | 56.6 | |
| Have my mother, father or a friend sit with me | 47.1 | 63.3 | |
| Breathe deeply | 47.0 | 53.3 | |
| Tell my parent(s) | 52.7 | 66.7 | |
| Know that I can ask for something that will make the pain feel better | 29.4 | 60.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Małek, A. Pain in Tourette Syndrome-Children’s and Parents’ Perspectives. J. Clin. Med. 2022, 11, 460. https://doi.org/10.3390/jcm11020460
Małek A. Pain in Tourette Syndrome-Children’s and Parents’ Perspectives. Journal of Clinical Medicine. 2022; 11(2):460. https://doi.org/10.3390/jcm11020460
Chicago/Turabian StyleMałek, Agnieszka. 2022. "Pain in Tourette Syndrome-Children’s and Parents’ Perspectives" Journal of Clinical Medicine 11, no. 2: 460. https://doi.org/10.3390/jcm11020460
APA StyleMałek, A. (2022). Pain in Tourette Syndrome-Children’s and Parents’ Perspectives. Journal of Clinical Medicine, 11(2), 460. https://doi.org/10.3390/jcm11020460





