Airway Management of Patients with Suspected or Confirmed COVID-19: Survey Results from Physicians from 19 Countries in Latin America
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). “WHO COVID-19 Dashboard,” Geneva. 2022. Available online: https://covid19.who.int/ (accessed on 14 January 2022).
- Cabrini, L.; Ghislanzoni, L.; Severgnini, P.; Landoni, G.; Baiardo Redaelli, M.; Franchi, F.; Romagnoli, S. Early versus late tracheal intubation in COVID-19 patients: A “pros/cons” debate also considering heart-lung interactions. Minerva Cardiol. Angiol. 2021, 69, 596–605. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Zhong, N.S. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Impact of COVID-19 on Health and Care Workers: A Closer Look at Deaths; World Health Organization: Geneva, Switzerland, 2021; Available online: https://apps.who.int/iris/handle/10665/345300 (accessed on 30 May 2021).
- Sabetian, G.; Moghadami, M.; Hashemizadeh Fard Haghighi, L.; Shahriarirad, R.; Fallahi, M.J.; Asmarian, N.; Sadat Moeini, Y. COVID-19 infection among healthcare workers: A cross-sectional study in southwest Iran. Virol. J. 2021, 18, 58. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.; Cimon, K.; Severn, M.; Pessoa-Silva, C.L.; Conly, J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS ONE 2012, 7, e35797. [Google Scholar] [CrossRef]
- Raboud, J.; Shigayeva, A.; McGeer, A.; Bontovics, E.; Chapman, M.; Gravel, D.; Henry, B.; Lapinsky, S.; Loeb, M.; McDonald, L.C.; et al. Risk factors for SARS transmission from patients requiring intubation: A multicentre investigation in Toronto, Canada. PLoS ONE 2010, 5, e10717. [Google Scholar] [CrossRef]
- Papoutsi, E.; Giannakoulis, V.G.; Xourgia, E.; Routsi, C.; Kotanidou, A.; Siempos, I.I. Effect of timing of intubation on clinical outcomes of critically ill patients with COVID-19: A systematic review and meta-analysis of non-randomized cohort studies. Crit. Care 2021, 25, 121. [Google Scholar] [CrossRef]
- Ferrando-Vivas, P.; Doidge, J.; Thomas, K.; Gould, D.W.; Mouncey, P.; Shankar-Hari, M.; Duncan Young, J.; Rowan, K.M.; Harrison, K.A. Prognostic factors for 30-day mortality in critically ill patients with coronavirus disease 2019: An observational cohort study. Crit. Care Med. 2021, 49, 102–111. [Google Scholar] [CrossRef]
- Granell Gil, M.; Sanchís López, N.; Aldecoa Álvarez de Santulano, C.; de Andrés Ibáñez, J.A.; Monedero Rodríguez, P.; Álvarez Escudero, J.; Rubini Puig, R.; Romero García, C.S.; en nombre del Grupo de Estudio CoV2-VIAEREA Network. Airway management of COVID-19 patients: A survey on the experience of 1125 physicians in Spain. Rev. Española Anestesiol. Reanim. 2022, 69, 12–24. [Google Scholar] [CrossRef]
- El-Boghdadly, K.; Wong, D.J.N.; Owen, R.; Neuman, M.D.; Pocock, S.; Carlisle, J.B.; Johnstone, C.; Andruszkiewicz, P.; Baker, P.A.; Biccard, B.M.; et al. Risks to healthcare workers following tracheal intubation of patients with COVID-19: A prospective international multicentre cohort study. Anaesthesia 2020, 75, 1437–1447. [Google Scholar] [CrossRef]
- Rivett, L.; Sridhar, S.; Sparkes, D.; Routledge, M.; Jones, N.K.; Forrest, S.; Young, J.; Pereira-Dias, J.; Hamilton, W.L.; Ferris, M.; et al. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. eLife 2020, 9, e58728. [Google Scholar] [CrossRef]
- Orser, B.A. Recommendations for Endotracheal Intubation of COVID-19 Patients. Anesth. Analg. 2020, 130, 1109–1110. [Google Scholar] [CrossRef]
- Higgs, A.; McGrath, B.A.; Goddard, C.; Rangasami, J.; Suntharalingam, G.; Gale, R.; Cook, T.M.; Society, D.A. Guidelines for the management of tracheal intubation in critically ill adults. Br. J. Anaesth. 2018, 120, 323–352. [Google Scholar] [CrossRef]
- Shallik, N.; Karmakar, A. Is it time for high flow nasal oxygen to be included in the difficult airway algorithm? Br. J. Anaesth. 2018, 121, 511–512. [Google Scholar] [CrossRef]
- Wax, R.S.; Christian, M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can. J. Anesth. 2020, 67, 568–576. [Google Scholar] [CrossRef]
- Birenbaum, A.; Hajage, D.; Roche, S.; Ntouba, A.; Eurin, M.; Cuvillon, P.; Rohn, A.; Compere, V.; Benhamou, D.; Biais, M.; et al. Effect of cricoid pressure compared with a sham procedure in the rapid sequence induction of anesthesia: The IRIS Randomized Clinical Trial. JAMA Surg. 2019, 154, 9–17. [Google Scholar] [CrossRef]
- Cook, T.M. The cricoid debate—Balancing risks and benefits. Anaesthesia 2016, 71, 721–722. [Google Scholar] [CrossRef]
- Azhar, M.N.; Bustam, A.; Poh, K.; Zahedi, A.Z.A.; Nazri, M.Z.A.M.; Ariffin, M.A.A.; Yusuf, M.H.; Zambri, A.; Chong, J.Y.; Kamarudin, A.; et al. COVID-19 aerosol box as protection from droplet and aerosol contaminations in healthcare workers performing airway intubation: A randomised cross-over simulation study. Emerg. Med. J. 2021, 38, 111–117. [Google Scholar] [CrossRef]
- Fong, S.; Li, E.; Violato, E.; Reid, A.; Gu, Y. Impact of aerosol box on intubation during COVID-19: A simulation study of normal and difficult airways. Can. J. Anesth. 2021, 68, 496–504. [Google Scholar] [CrossRef]
- Yao, W.; Wang, T.; Jiang, B.; Gao, F.; Wang, L.; Zheng, H.; Xiao, W.; Yao, S.; Mei, W.; Chen, X.; et al. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan China: Lessons learnt and international expert recommendations. Br. J. Anaesth. 2020, 125, e28–e37. [Google Scholar] [CrossRef]
- Cook, T.M.; El-Boghdadly, K.; McGuire, B.; McNarry, A.F.; Patel, A.; Higgs, A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020, 75, 785–799. [Google Scholar] [CrossRef]
- De Jong, A.; Pardo, E.; Rolle, A.; Bodin-Lario, S.; Pouzeratte, Y.; Jaber, S. Airway management for COVID-19: A move towards universal videolaryngoscope? Lancet Respir. Med. 2020, 8, 555. [Google Scholar] [CrossRef]
- Şentürk, M.; El Tahan, M.R.; Szegedi, L.L.; Marczin, N.; Karzai, W.; Shelley, B.; Piccioni, F.; Gil, M.G.; Rex, S.; Sorbello, M.; et al. Thoracic Anesthesia of Patients With Suspected or Confirmed 2019 Novel Coronavirus Infection: Preliminary Recommendations for Airway Management by the European Association of Cardiothoracic Anaesthesiology Thoracic Subspecialty Committee. J. Cardiothorac. Vasc. Anesth. 2020, 34, 2315–2327. [Google Scholar] [CrossRef] [PubMed]
- Scott Taylor, R.; Pitzer, M.; Goldman, G.; Czysz, A.; Simunich, T.; Ashurst, J. Comparison of intubation devices in level C PPE: A cadaveric study. Am. J. Emerg. Med. 2018, 36, 922–925. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, J.Y.; Kang, S.Y.; Kwak, H.J.; Lee, D.; Lee, S.Y. Stylet angulation for routine endotracheal intubation with McGrath videolaryngoscope. Medicine 2017, 96, e6152. [Google Scholar] [CrossRef]
- Mehta, C.; Mehta, Y. Percutaneous tracheostomy. Ann. Card. Anaesth. 2017, 20, S19–S25. [Google Scholar] [CrossRef]
- Zhang, X.; Huang, Q.; Niu, X.; Zhou, T.; Xie, Z.; Zhong, Y.; Xiao, H. Safe and effective management of tracheostomy in COVID-19 patients. Head Neck 2020, 42, 1374–1381. [Google Scholar] [CrossRef]
- Miles, B.A.; Schiff, B.; Ganly, I.; Ow, T.; Cohen, E.; Genden, E.; Culliney, B.; Mehrotra, B.; Savona, S.; Wong, R.J.; et al. Tracheostomy during COV-SARS-CoV-2 pandemic: Recommendations from the New York Head and Neck Society. Head Neck 2020, 42, 1282–1290. [Google Scholar] [CrossRef]
- Alhazzani, W.; Moller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020, 48, e440–e469. [Google Scholar]
- Verbeek, J.H.; Rajamaki, B.; Ijaz, S.; Sauni, R.; Toomey, E.; Blackwood, B.; Tikka, C.; Ruotsalainen, J.; Selcen Kilinc Balci, F. PPE for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Emergencias 2021, 33, 59–61. [Google Scholar]
- Pieters, B.M.; Wilbers, N.E.; Huijzer, M.; Winkens, B.; van Zundert, A.A. Comparison of seven videolaryngoscopes with the Macintosh laryngoscope in manikins by experienced and novice personnel. Anesthesia 2016, 71, 556–564. [Google Scholar] [CrossRef]



| Variable | Mean | SD | CI 95 Inf | CI 95 Sup |
|---|---|---|---|---|
| Age | 41, 91 | 10, 26 | 41, 5 | 42, 31 |
| Seniority | 21, 19 | 16, 88 | 20, 51 | 21, 86 |
| Number of COVID-19 confirmed intubated patients | 11, 90 | 21, 18 | 11, 06 | 12, 75 |
| Number of COVID-19 suspected intubated patients | 20, 67 | 40, 00 | 19, 08 | 22, 27 |
| Items of the Questionnaire | n (%) | * p Value |
|---|---|---|
| Which is the most accurate description of the hospital where you normally work? | <0.001 | |
| Public hospital | 1109 (46%) | |
| Private hospital | 618 (25.6%) | |
| Public–private hospital | 684 (28.4%) | |
| What is your medical specialty in where you have had experience with airway management in COVID-19 patients? | <0.001 | |
| Anesthesiology | 1475 (61.2%) | |
| Critical Care Medicine | 179 (7.4%) | |
| Emergency Medicine | 53 (2.2%) | |
| Internal Medicine | 13 (0.5%) | |
| Other | 691 (28.7%) | |
| In your clinical experience, where have you intubated more COVID-19 patients? | <0.001 | |
| Emergencies/out-of-hospital emergencies | 44 (1.8%) | |
| Hospital emergency department | 279 (11.6%) | |
| Intensive care unit | 600 (24.9%) | |
| Urgent surgery | 1002 (41.5%) | |
| Scheduled surgery | 361 (15%) | |
| Hospitalization ward | 125 (5.2%) | |
| As a front line exposure professional, have you been infected by COVID-19? | <0.001 | |
| Yes, I have been diagnosed positive by PCR or serology | 365 (15.1%) | |
| No, I have been diagnosed negative by PCR or serology | 1347 (55.9%) | |
| I have never been tested because I have been asymptomatic | 648 (26.9%) | |
| I have never been tested, although I have had symptoms | 51 (2.1%) |
| Items of the Questionnaire | n (%) | * p Value |
|---|---|---|
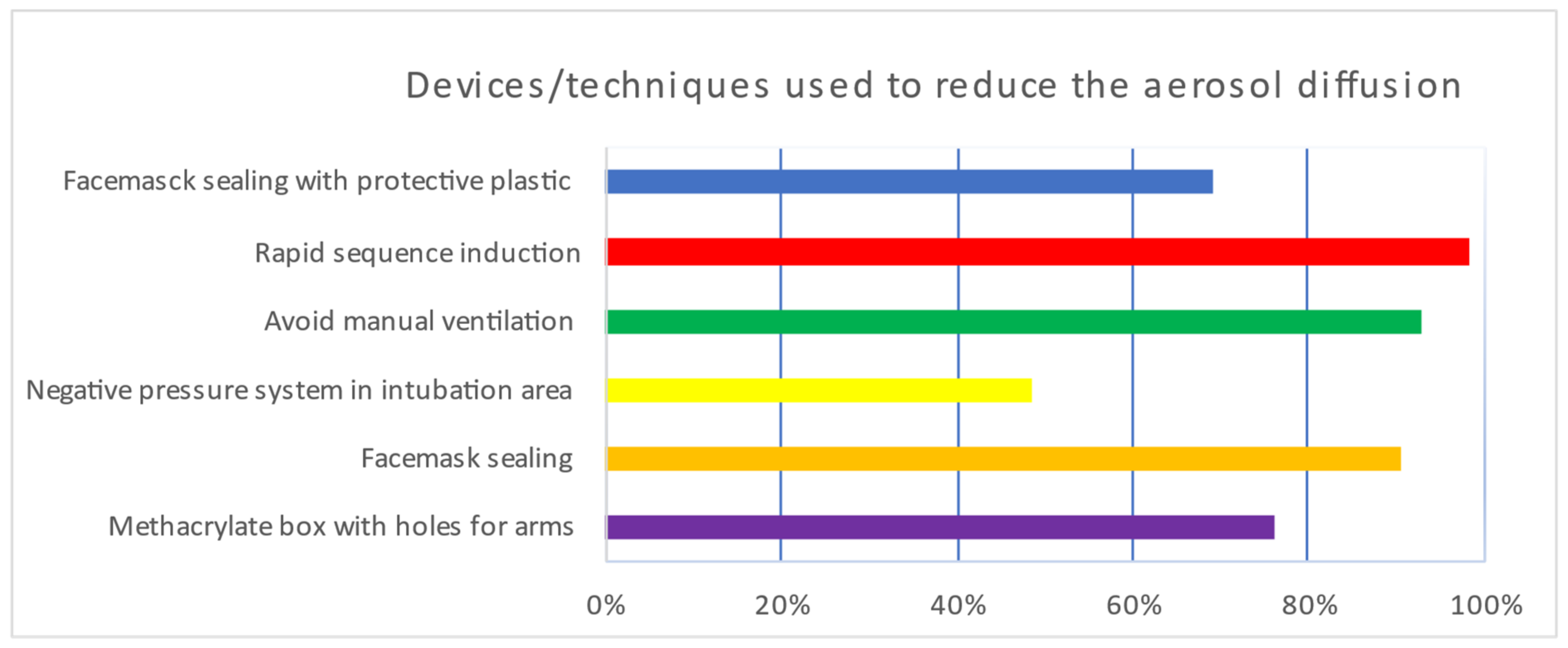
| What do you think about the following systems for the reduction of diffusion of aerosols? 6-point Likert scale (from 1 = strongly disagree to 6 = strongly agree; percentage scoring 6: n (%)). | ||
| Methacrylate box with holes for arms | 543 (22.5%) | <0.001 |
| Face mask sealing | 622 (25.8%) | <0.001 |
| Negative pressure system in intubation area | 601 (24.9%) | <0.001 |
| Avoid manual ventilation | 654 (27.1%) | <0.001 |
| Rapid sequence induction | 803 (33.3%) | <0.001 |
| Face mask sealing with protective plastic | 483 (20%) | <0.001 |
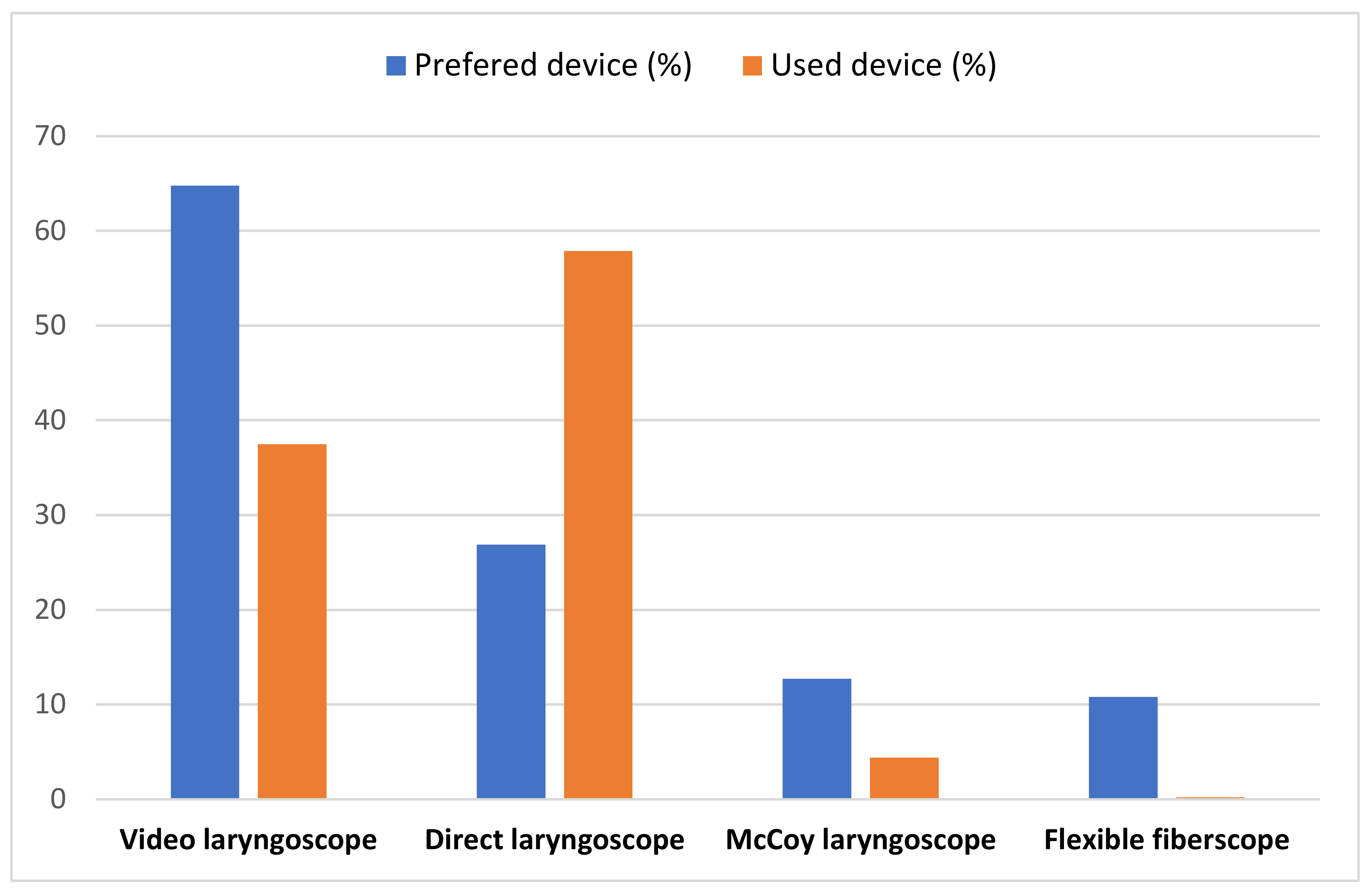
| Based on your COVID-19 patients’ experience, what is the optimal device for intubation? 6-point Likert scale. Percentage scoring 6. n (%). | Number n (%) | |
| Video laryngoscope | 1562 (64.8 %) | <0.001 |
| Direct laryngoscope | 649 (26.9%) | <0.001 |
| McCoy laryngoscope | 307 (12.7%) | <0.001 |
| Flexible fiberscope | 260 (10.8%) | <0.001 |
| What type of video laryngoscopy would you prefer to intubate a COVID-19 patient? 6-point Likert scale. Percentage scoring 6. n (%). | ||
| C-MAC | 808 (33.5%) | <0.001 |
| King Vision | 629 (26.1%) | <0.001 |
| McGrath | 594 (24.6%) | <0.001 |
| Glidescope | 562 (23.3%) | <0.001 |
| Airtraq | 271 (11.2%) | <0.001 |
| Direct laryngoscope | 690 (28.6%) | <0.001 |
| Others | 235 (9.7%) | <0.001 |
| In COVID-19 patients, what type of video laryngoscope blade do you prefer to use? | <0.001 | |
| Reusable | 398 (16.5%) | |
| Disposable | 1191 (49.4%) | |
| Indifferent | 317 (13.2%) | |
| I do not have experience | 505 (20.9%) | |
| What type of video laryngoscope blade do you prefer to use? | <0.001 | |
| With channel | 835 (34.6%) | |
| Without channel | 581 (24.1%) | |
| Indifferent | 464 (19.3%) | |
| I do not have experience | 531 (22%) | |
| In COVID-19 patients, what type of video laryngoscope blade do you prefer to use? | <0.001 | |
| Macintosh blade | 1234 (51.2%) | |
| Hypercurved blade | 565 (23.4%) | |
| Indifferent | 349 (14.5%) | |
| I do not have experience | 263 (10.9%) | |
| In COVID 19 patients, what type of video laryngoscope image display monitor do you prefer to use? | <0.001 | |
| Video laryngoscope attachment | 842 (34.9%) | |
| Separate/remote from video laryngoscope | 856 (35.5%) | |
| Indifferent | 387(16.1%) | |
| I do not have experience | 326 (13.5%) | |
| What disadvantages of video laryngoscopes consider the most detrimental. 6-point Likert scale. Percentage scoring 6: n (%). | ||
| Annoying light reflections on the video laryngoscope screen | 262 (10.9%) | <0.001 |
| Difficulty introducing into the mouth | 269 (11.2%) | <0.001 |
| Need for proximity to the patient’s upper airways | 311 (12.9%) | <0.001 |
| Difficulty inserting the tube through the vocal cords | 291 (12.1%) | <0.001 |
| Lack of practical experience with any of the video laryngoscopes used | 589 (24.4%) | <0.001 |
| What type of device do you usually use to facilitate intubation? 6-point Likert scale. Percentage scoring 6: n (%). | ||
| Frova guide | 529 (21.6%) | <0.001 |
| Eschmann guide | 825 (34.2%) | <0.001 |
| Flexible stylet inside the orotracheal tube | 735 (31.9%) | <0.001 |
| Fiberscope | 418 (17.3%) | <0.001 |
| VAMA | 155 (6.4%) | <0.001 |
| None | 124 (5.1%) | <0.001 |
| In the case of a predicted or known difficult airway of a COVID-19 patient, how do you prefer to perform the intubation? 6-point Likert scale. Percentage scoring 6: n (%). | ||
| Flexible fiberscope | 761 (31.6%) | <0.001 |
| Video laryngoscope | 1487 (61.7%) | <0.001 |
| Direct laryngoscope | 475 (19.7%) | <0.001 |
| McCoy laryngoscope | 336 (13.9%) | <0.001 |
| Laryngeal mask | 153 (6.3%) | <0.001 |
| Tracheal intubation through the laryngeal mask | 177 (7.3%) | <0.001 |
| Tracheostomy | 175 (7.3%) | <0.001 |
| In the case of unpredicted or unknown difficult airway of COVID-19 patient, how do you prefer to perform the intubation? 6-point Likert scale. Percentage scoring 6. n (%). | ||
| Flexible fiberscope | 411 (17%) | <0.001 |
| Video laryngoscope | 1536 (63.7%) | <0.001 |
| Direct laryngoscope | 581 (24.1%) | <0.001 |
| McCoy laryngoscope | 401 (16.6%) | <0.001 |
| Laryngeal mask | 252 (10.5%) | 0.281 |
| Tracheal intubation through the laryngeal mask | 252 (10.5%) | 0.066 |
| Items of the Questionnaire | n (%) | * p Value |
|---|---|---|
| Did you perform preoxygenation prior to intubation/tracheostomy? | <0.001 | |
| Yes, for at least 5 min | 707 (29.3 %) | |
| Yes, for 3–5 min | 1117 (46.3 %) | |
| Yes, for less than 1 min | 331 (13.7 %) | |
| No, the patient’s conditions did not allow delay | 163 (6.8 %) | |
| No, context/stress of the situation did not permit us to preoxygenate | 93 (3.9 %) | |
| What is the most frequently used device for intubation in COVID-19 patients? | <0.001 | |
| Video laryngoscope | 905 (37.5%) | |
| Direct laryngoscopy | 1395 (57.9%) | |
| McCoy laryngoscope | 107 (4.4%) | |
| Fiberscope | 4 (0.2%) | |
| What kind of video laryngoscope have you used most frequently for intubation in COVID-19 patients? | <0.001 | |
| C-MAC | 334 (13.9%) | |
| King Vision | 293 (12.2%) | |
| McGrath | 460 (19.1%) | |
| Glidescope | 186 (7.7%) | |
| Airtraq | 59 (2.4%) | |
| Not available | 673 (27.9%) | |
| They prefer direct laryngoscopy even if they have video laryngoscope | 406 (16.8%) | |
| Please answer “yes” if you have used these video laryngoscopes. | “Yes” n (%) | |
| C-MAC | 1203 (49.9%) | <0.001 |
| King Vision | 1207 (50.1%) | <0.001 |
| McGrath | 1129 (46.8%) | <0.001 |
| Glidescope | 1039 (43.1%) | <0.001 |
| Airtraq | 1087 (45.1%) | <0.001 |
| Others | 1319 (54.7%) | <0.001 |
| In COVID-19 patients, what type of video laryngoscope blade do you use most frequently? | <0.001 | |
| Reusable | 1144 (47.4%) | |
| Disposable | 640 (26.5%) | |
| Indifferent | 461 (19.2%) | |
| I do not have experience | 166 (6.9%) | |
| Please answer yes if you have used these devices/techniques | Yes; n (%) | <0.001 |
| Methacrylate box with holes for arms | 1832 (76%) | |
| Facemask sealing | 2187 (90.7%) | |
| Negative pressure system in intubation area | 1174 (48.7%) | |
| Avoid manual ventilation | 2234 (92.7%) | |
| Rapid sequence induction | 2373 (98.4%) | |
| Sellick’s maneuver | 1557 (64.6%) | |
| Facemasck sealing with protective plastic | 1664 (69%) | |
| In patients with suspected or positive COVID-19 diagnosis, how many clinicians experienced with airway, including you were on stage? | <0.001 | |
| One | 926 (38.4%) | |
| Two | 1299 (53.9%) | |
| Three or more | 186 (7.7%) | |
| Even if you knew perfectly the sequence and approach of the airway and the preparation of the COVID-19 patient to minimize risks, do you think at any time that you had forgotten any safety steps due to the stress of the situation? | <0.001 | |
| Never | 278 (11.5%) | |
| A few times | 1677 (69.6%) | |
| Almost always | 415 (17.2%) | |
| Always | 41 (1.7%) | |
| Being in close proximity of the airway of COVID-19 positive patient, which caused more stress for you? | <0.001 | |
| Failure of intubation and patient deterioration | 742 (30.8%) | |
| Finding an unexpected difficult airway | 753 (31.2%) | |
| Fear of contagion | 916 (38%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Granell, M.; Sanchis, N.; Delgado, C.; Lozano, M.; Pinho, M.; Sandoval, C.; Romero, C.S.; Aldecoa, C.; Cata, J.P.; Neira, J.; et al. Airway Management of Patients with Suspected or Confirmed COVID-19: Survey Results from Physicians from 19 Countries in Latin America. J. Clin. Med. 2022, 11, 4731. https://doi.org/10.3390/jcm11164731
Granell M, Sanchis N, Delgado C, Lozano M, Pinho M, Sandoval C, Romero CS, Aldecoa C, Cata JP, Neira J, et al. Airway Management of Patients with Suspected or Confirmed COVID-19: Survey Results from Physicians from 19 Countries in Latin America. Journal of Clinical Medicine. 2022; 11(16):4731. https://doi.org/10.3390/jcm11164731
Chicago/Turabian StyleGranell, Manuel, Nerea Sanchis, Carlos Delgado, Manuel Lozano, Marcio Pinho, Cecilia Sandoval, Carolina S. Romero, Cesar Aldecoa, Juan P. Cata, Jorge Neira, and et al. 2022. "Airway Management of Patients with Suspected or Confirmed COVID-19: Survey Results from Physicians from 19 Countries in Latin America" Journal of Clinical Medicine 11, no. 16: 4731. https://doi.org/10.3390/jcm11164731
APA StyleGranell, M., Sanchis, N., Delgado, C., Lozano, M., Pinho, M., Sandoval, C., Romero, C. S., Aldecoa, C., Cata, J. P., Neira, J., De Andres, J., Herreros-Pomares, A., Navarro, G., & The COV2-VIAEREA Network Study Group. (2022). Airway Management of Patients with Suspected or Confirmed COVID-19: Survey Results from Physicians from 19 Countries in Latin America. Journal of Clinical Medicine, 11(16), 4731. https://doi.org/10.3390/jcm11164731









