Abstract
Background: This study was conducted to identify the predictive factors for survival and favorable neurological outcome in patients with emergency department cardiac arrest (EDCA). Methods: ED patients who suffered from in-hospital cardiac arrest (IHCA) from July 2014 to June 2019 were enrolled. The electronic medical records were retrieved and data were extracted according to the IHCA Utstein-style guidelines. Results: The cardiac arrest survival post-resuscitation in-hospital (CASPRI) score was associated with survival, and the CASPRI scores were lower in the survival group. Three components of the CASPRI score were associated with favorable neurological survival, and the CASPRI scores were lower in the favorable neurological survival group of patients who were successfully resuscitated. The independent predictors of survival were presence of hypotension/shock, metabolic illnesses, short resuscitation time, receiving coronary angiography, and TTM. Receiving coronary angiography and low CASPRI score independently predicted favorable neurological survival in resuscitated patients. The performance of a low CASPRI score for predicting favorable neurological survival was fair, with an AUROCC of 0.77. Conclusions: The CASPRI score can be used to predict survival and neurological status of patients with EDCA. Post-cardiac arrest care may be beneficial for IHCA, especially in patients with EDCA.
1. Introduction
Patients who have had an in-hospital cardiac arrest (IHCA) have a high mortality rate [1,2,3,4,5], and the etiology and treatment strategy for these patients differ from those of patients with out-of-hospital cardiac arrest (OHCA). Cardiac arrest in the emergency department (ED) comprises about 10–19% of IHCA events [2,5,6] and is linked with a higher chance of shockable initial rhythms and a higher survival rate compared with patients sustaining cardiac arrest in other locations in the hospital [2]. However, ED cardiac arrest (EDCA) is rarely examined as a distinct group [2,5,7], and the risks of survival and neurological outcome are rarely discussed. Knowledge of the risk factors related to survival and neurological outcome may help to optimize the treatment strategy, including prevention, resuscitation efforts, and post-cardiac arrest care in EDCA.
The cardiac arrest survival post-resuscitation in-hospital (CASPRI) score has been used to predict favorable neurological survival [8]. This score has been validated in an Asian population [9], and is recommended as a good tool for estimation of survival to hospital discharge, with a favorable neurological outcome in patients with return of spontaneous circulation after in-hospital cardiac arrest [4]. It is not known whether the CASPRI score can be applied to EDCA for prognosis prediction. We performed this retrospective study to identify the predictive factors of survival and favorable neurological outcome in patients with EDCA. We also evaluated whether the CASPRI scoring system could be used in EDCA.
2. Materials and Methods
Taichung Veterans General Hospital (TCVGH) is a medical center located in central Taiwan. It has 1500 beds and an annual ED volume of 66,000 visits. We retrospectively retrieved information from electronic medical records (EMR) of ED patients in TCVGH, who received cardiopulmonary resuscitation (CPR) from 1 July 2014 to 30 June 2019. Patients who visited the ED for trauma, for out-of-hospital cardiac arrest (OHCA), or had signed a “do-not-resuscitate (DNR)” order were excluded. We also excluded patients who were younger than 18 years old, pregnant, a prisoner, had a psychiatric disease, or had human immune deficiency virus (HIV) infection. Patients who were transferred to another hospital after being resuscitated were also excluded. We did not exclude the patients who had been successfully resuscitated from an OHCA event in other hospitals, and were transferred to our ED with spontaneous circulation on arrival. All identifiable patient information was deleted before data analysis.
Two research assistants, both qualified nursing practitioners with at least 5 years of experience in emergency medicine, reviewed the medical records and abstracted the data on a structured data sheet using the Utstein-style elements of in-hospital cardiac arrest [10]. In addition to accessing the EMR of the ED information system, the research assistants also queried the inpatient information system for records related to post-resuscitation care and outcomes. Two board-certified emergency physicians confirmed the quality of the data using established criteria.
The CASPRI predictors were grouped if they had the same CASPRI score, and the CASPRI scores were grouped to avoid small numbers (fewer than 4 cases) in each group. Candidate predictive factors for survival to discharge, as well as favorable neurological outcome (defined as a cerebral performance category score of 1 or 2) were analyzed. Continuous data were expressed as mean ± standard deviation (SD). Categorical data were expressed as number and percentage. Chi-square tests or Fisher’s exact test were used to compare categorical features, and unpaired t test was used to compare continuous features. p values < 0.05 were considered statistically significant. Variables with a p value of <0.20 in the univariate analysis were entered into a logistic regression model. We used the area under the receiver operating characteristic curve (AUROCC) to evaluate the predictive powers of the CASPRI scoring system. Analyses were performed using the Statistical Package for the Social Science (IBM SPSS version 22.0; International Business Machines Corp, New York, NY, USA).
This study was approved by the institutional review board (IRB) of Taichung Veterans General Hospital (IRB number: SE20226A).
3. Results
We collected a total of 322 patients with non-traumatic cardiac arrest in the ED. Male gender was predominant (68.6%), and 16 (5.0%) had had an initial OHCA event, and was referred to the ED after successful resuscitation in other hospital. The pre-arrest cerebral performance category (CPC) scores of 1, 2, 3, and 4 accounted for 33.5%, 34.8%, 21.7%, and 7.8% of the patients, respectively. Most of the cardiac arrests occurred in the resuscitation room (71.7%), followed by the observation room (20.5%), and the imaging room (3.4%). Six (1.9%) cardiac arrest events occurred outside of the ED when patients were transferred to scope rooms or radiology department for diagnostic/interventional procedures. The most common initial rhythms were pulseless electrical activity (68.1%), followed by asystole (18.3%), ventricular fibrillation (6.5%), and pulseless ventricular tachycardia (6.5%). One hundred and sixty-eight patients (52.2%) were successfully resuscitated (defined as recovery of spontaneous circulation (ROSC) for at least 20 min), and in 3 patients the resuscitation effort was stopped due to DNR order before or after this event. Eighty-nine patients (27.6%) survived to discharge, while 36 patients (11.2%) had favorable neurological outcomes (CPC of 1 or 2) at discharge. A total of 44 patients (13.7%) survived for more than one year, and the majority of these patients (32, 72.7%) had favorable neurological outcomes. A flowchart of baseline characteristics and outcomes is illustrated in Figure 1.
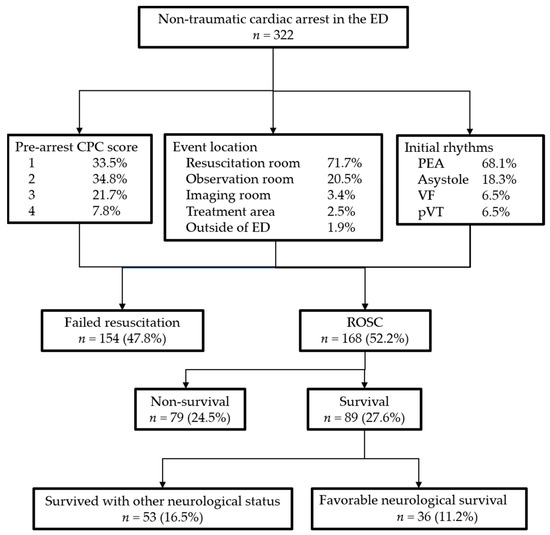
Figure 1.
A flowchart of baseline characteristics and outcomes. Abbreviations: CPC: Cerebral performance category; ED: Emergency Department; PEA: pulseless electrical activity; VF: ventricular fibrillation; pVT: pulseless ventricular tachycardia; ROSC: return of spontaneous circulation.
Survival of EDCA was associated with presence of preexisting conditions (heart failure, myocardial infarct, hepatic failure, hypotension/shock, metabolic illnesses, diabetes mellitus, sepsis, and renal failure), non-respiratory causes of cardiac arrest, initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia, receiving coronary angiography (urgent or delayed), attempts of coronary reperfusion, and targeted temperature management (TTM). The cardiac arrest survival post-resuscitation in-hospital (CASPRI) score was also associated with survival, and the CASPRI scores were lower in the survival group (mean ± SD, 15.3 ± 6.4 vs. 19.4 ± 5.4, p < 0.001) (Table 1).

Table 1.
Clinical characteristics and Utstein style elements of survival and non-survival IHCA patients.
In patients successfully resuscitated, favorable neurological survival was associated with absence of hypotension/shock, non-respiratory cause of cardiac arrest, receiving coronary angiography, and attempts of coronary reperfusion (Table 2). Three components of CASPRI score (initial rhythm of witnessed or non-witnessed ventricular fibrillation/pulseless ventricular tachycardia, pre-arrest CPC score of 1 or 2, and absence of factors of mechanical ventilation/sepsis/hypotension or hepatic failure/malignancy prior to arrest) were also associated with favorable neurological survival, and the CASPRI scores were lower in the favorable neurological survival group (mean ± SD, 11.1 ± 5.6 vs. 17.8 ± 6.1, p < 0.001) (Table 3).

Table 2.
Utstein style elements and favorable neurological survival in resuscitated patients.

Table 3.
The Cardiac Arrest Survival Post-Resuscitation In-hospital (CASPRI) predictors and favorable neurological survival in resuscitated patients.
Multivariate logistic regression analysis showed that the independent predictors of survival were presence of hypotension/shock, metabolic illnesses, short resuscitation time, receiving coronary angiography, and TTM. In resuscitated patients, the independent predictors of favorable neurological survival were receiving coronary angiography (urgent vs. other groups: OR, 95% confidence interval of 5.5, 1.8–16.8), and low CASPRI score (0–9 vs. other groups: OR, 95% confidence interval of 9.2, 2.2–37.4, 10–14 vs. other groups: OR, 95% confidence interval of 7.7, 2.1–28.2, respectively). The AUROCC of low CASPRI score for predicting favorable neurological survival was 0.77 (95% confidence interval: 0.68–0.85) (Table 4).

Table 4.
Multivariate logistic regression and AUROCC.
4. Discussion
One of the components of in-hospital cardiac arrest that distinguishes it from out-of-hospital arrest is that the former may result from progressively worsening underlying disease, whereas the latter is often sudden and unpredictable [4]. The mixture of characteristics in out-of-hospital and in-hospital arrest populations explains why cardiac arrest in the ED has a higher survival rate compared with arrest in other locations of the hospital. However, it also raises the question as to whether the predictive factors of survival and favorable neurological outcome in patients with IHCA are applicable to EDCA.
The presence of pre-existing co-morbidities has been shown to be associated with poor survival in patients sustaining IHCA [11,12,13], but our study found that presence of hepatic failure, hypotension/shock, metabolic illnesses, diabetes mellitus, sepsis, or renal failure predicted survival after EDCA, and presence of hypotension/shock and metabolic illnesses were also independent predictors of survival. Patients with these medical conditions presenting with cardiac arrest in the ED might be in the early stage of time-sensitive deterioration in their disease process, which allows early recognition and immediate treatment in the ED setting, and leads to a higher chance of survival. Patients without these medical conditions might lack the reversibility by agile response in the ED, and had lower survival rates than their counterparts.
However, our study showed that absence of hypotension/shock predicted favorable neurological outcome. The absence of factors of mechanical ventilation/sepsis/hypotension or hepatic failure/malignancy prior to arrest, which is one of the components of the CASPRI score, was also associated with favorable neurological survival. Only eleven of one hundred and sixty-eight resuscitated patients received TTM in our study. Further research is warranted to clarify the role of this neuroprotective treatment for EDCA in patients with these medical conditions.
IHCA survival improved from 13.7% in 2000 to 26.7% in 2019 [1,3], but decisions pertaining to not attempting resuscitation and termination of cardiopulmonary resuscitation remain a challenge for clinicians and patients’ families [14]. Systems designed to predict survival and neurological outcome, such as the CASPRI score, could be used to optimize medical resources and enhance communication with patients and families. The strength of the CASPRI scoring system is that it focuses on the 10% of patients successfully resuscitated from an in-hospital cardiac arrest who have a >70% probability of favorable neurological survival to discharge [8]. The CASPRI scoring system was developed using the United States’ Get With the Guideline (GWTG) registry. The total score is calculated by summing the scores of eleven variables, including age, initial arrest rhythm or time to defibrillation, pre-arrest cerebral performance category score, hospital location, duration of resuscitation, presence of mechanical ventilation, renal insufficiency, hepatic insufficiency, sepsis, malignancy, and hypotension prior to the arrest. Although the original model of the CASPRI score did not include patients with EDCA, we found that the CASPRI score can be used to predict the survival and neurological status of patients with EDCA. The CASPRI score was associated with survival, and the CASPRI scores were lower in the survival group in all patients. CASPRI scores were lower in the favorable neurological survival group of patients who were successfully resuscitated, and the multivariate logistic regression analysis showed that CASPRI score was an independent predictor of favorable neurological survival in resuscitated patients. The performance of low CASPRI score for predicting favorable neurological survival was fair, with an AUROCC of 0.77. The application of the CASPRI score as a predictive tool for EDCA could provide accurate prognostication based on precise information about the likelihood of survival and neurological outcome, and may provide critical information to facilitate shared decision-making for cardiopulmonary resuscitation [15,16], such as decisions related to choosing an end-of-life plan, or other aggressive resuscitation efforts.
The management in the post–cardiac arrest period of IHCA should focus on the precipitating cause, hemodynamic and respiratory support, and neuroprotective care [4]. However, this concept is generally derived from evidence obtained from studies on OHCA. Coronary angiography is well known to be associated with superior outcomes in survivors of OHCA [17,18,19], but its role in IHCA has rarely been discussed. Our study found that receiving coronary angiography (urgent or delayed), attempts of coronary reperfusion, and TTM were associated with survival, and receiving coronary angiography and TTM were also independent predictors of survival for all patients. Receiving coronary angiography and attempts of coronary reperfusion were associated with favorable neurological survival, and receiving coronary angiography was also an independent predictor of favorable neurological outcome in successfully resuscitated patients. These findings appear to support the benefits of post-cardiac arrest care for IHCA, especially in patients with EDCA.
Targeted temperature management after cardiac arrest remains the primary neuroprotective approach following out-of-hospital cardiac arrest [20], but results regarding use of TTM in IHCA are inconsistent. Chan et al. found that use of TTM was associated with a lower likelihood of survival to hospital discharge and a lower likelihood of favorable neurological survival in patients with IHCA [21], while other researchers found that the beneficial effects of TTM for patients with IHCA were not significantly different from OHCA, especially when baseline factors were matched [22,23,24]. In our study, TTM was favorable for survival in EDCA, but it was not predictive of favorable neurological outcome in resuscitated patients. Although not every individual component of the CASPRI score was associated with favorable neurological survival, a summation score of all components showed a significantly predictive value in our study. Development of a summation score of post-resuscitation processes may be warranted in future research.
Survival from cardiac arrest was higher in EDs than cardiac arrests in intensive care units (ICU-CA), but their risks factors of survival and favorable neurological outcome seem be similar. Treating ICU-CA as unique entity, Roedl and colleagues found that the SOFA score and liver failure after ICU-CA are independent predictors of mortality [25]. Leloup and colleagues found that six-month survival with no or moderate functional sequelae was correlated with a number of organ failures ≤2 when cardiac arrest occurred, resuscitation time ≤5 min, shockable rhythm cardiac arrests, etiology related to the life-sustaining devices in place, absence of preexisting disability or disease deemed fatal within 5 years, and sedation [26]. Our study showed that survival of EDCA was associated with causes of cardiac arrest, shockable rhythm, and short resuscitation time. We also found that post-resuscitation processes (coronary angiography and TTM) were also associated survival, which was not mentioned in researches of ICU-CA.
Generalization of the results of this study might be limited since it was retrospective and information was collected from a single institution. The chart review method used in this study is subject to various potential shortcomings, including inaccuracy and incompleteness in vital sign measurements and the recording of medical events, and inconsistent criteria for ordering certain examinations and identifying abnormalities during these examinations. We attempted to minimize the limitations of the retrospective medical chart review by asking experienced nursing practitioners to retrieve the data from medical information systems, and having board-certified emergency physicians confirm the quality of the data.
5. Conclusions
The independent predictors of survival were presence of hypotension/shock, metabolic illnesses, short resuscitation time, receiving coronary angiography, and TTM. The independent predictors of favorable neurological survival in resuscitated patients were receiving coronary angiography and low CASPRI score. The CASPRI score can be used to predict survival and neurological status of patients with EDCA. The performance of a low CASPRI score for predicting favorable neurological survival was fair. Post-cardiac arrest care may be beneficial for IHCA, especially in patients with EDCA.
Author Contributions
Conceptualization, J.C.-H.T.; methodology, J.C.-H.T., J.-W.M. and S.-Y.H.; software, S.-C.L.; validation, J.-W.M. and S.-Y.H.; formal analysis, J.C.-H.T. and S.-C.L.; investigation, J.C.-H.T., J.-W.M. and S.-Y.H.; resources, J.C.-H.T.; data curation, T.-C.L.; writing—original draft preparation, J.C.-H.T.; writing—review and editing, J.C.-H.T. and S.-Y.H.; visualization, J.C.-H.T. and S.-Y.H.; supervision, T.-C.L.; project administration, J.C.-H.T., J.-W.M. and S.-Y.H.; funding acquisition, J.C.-H.T. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by Taichung Veterans General Hospital, Puli Branch (grant number PL-2020001), in which the APC was included.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Taichung Veterans General Hospital (IRB number: SE20226A).
Informed Consent Statement
Patient consent was waived due to no additional risk/harm in a retrospective medical record review, and all identifiable patient information was deleted before data analysis.
Data Availability Statement
Readers could access the data and material supporting the conclusions of the study by contacting Jeffrey Che-Hung Tsai at erdr2181@gmail.com.
Acknowledgments
We would like to thank the Clinical Informatics Research & Development Center and Biostatistics Task Force of Taichung Veterans General Hospital. Thank Nurse Specialist Practitioners, Hui-Yuan Hsieh and Kuei-Ling Hsu, to review the medical records and abstracted the data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Girotra, S.; Nallamothu, B.K.; Spertus, J.A.; Li, Y.; Krumholz, H.M.; Chan, P.S. Trends in survival after in-hospital cardiac arrest. N. Engl. J. Med 2012, 367, 1912–1920. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kayser, R.G.; Ornato, J.P.; Peberdy, M.A. Cardiac arrest in the Emergency Department: A report from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 2008, 78, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.W.; Holmberg, M.J.; Berg, K.M.; Donnino, M.W.; Granfeldt, A. In-Hospital Cardiac Arrest: A Review. JAMA 2019, 321, 1200–1210. [Google Scholar] [CrossRef]
- Donoghue, A.J.; Abella, B.S.; Merchant, R.; Praestgaard, A.; Topjian, A.; Berg, R.; Nadkarni, V.; American Heart Association’s Get with the Guidelines-Resuscitation Investigators. Cardiopulmonary resuscitation for in-hospital events in the emergency department: A comparison of adult and pediatric outcomes and care processes. Resuscitation 2015, 92, 94–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, M.T.; Huang, W.C.; Yen, D.H.T.; Yeh, E.H.; Wu, S.Y.; Liao, H.H. The Potential Risk Factors for Mortality in Patients After In-Hospital Cardiac Arrest: A Multicenter Study. Front. Cardiovasc. Med. 2021. [Google Scholar] [CrossRef]
- Tan, S.C.; Leong, B.S. Cardiac arrests within the emergency department: An Utstein style report, causation and survival factors. Eur. J. Emerg. Med. 2018, 25, 12–17. [Google Scholar] [CrossRef]
- Chan, P.S.; Spertus, J.A.; Krumholz, H.M.; Berg, R.A.; Li, Y.; Sasson, C.; Nallamothu, B.K. A Validated Prediction Tool for Initial Survivors of In-Hospital Cardiac Arrest. Arch. Intern. Med. 2012, 172, 947–953. [Google Scholar] [CrossRef]
- Wang, C.H.; Chang, W.T.; Huang, C.H.; Tsai, M.S.; Yu, P.H.; Wu, Y.W.; Chen, W.J. Validation of the Cardiac Arrest Survival Postresuscitation In-hospital (CASPRI) score in an East Asian population. PLoS ONE 2018, 13, e0202938. [Google Scholar] [CrossRef]
- Nolan, J.P.; Berg, R.A.; Andersen, L.W.; Bhanji, F.; Chan, P.S.; Donnino, M.W.; Lim, S.H.; Ma, M.H.; Nadkarni, V.M.; Starks, M.A.; et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Template for In-Hospital Cardiac Arrest: A Consensus Report from a Task Force of the International Liaison Committee on Resuscitation. Circulation 2019, 140, e746–e757. [Google Scholar] [CrossRef] [Green Version]
- Larkin, G.L.; Copes, W.S.; Nathanson, B.H.; Kaye, W. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: A report from the National Registry for Cardiopulmonary Resuscitation. Resuscitation 2010, 81, 302–311. [Google Scholar] [CrossRef]
- Ebell, M.H.; Afonso, A.M. Pre-arrest predictors of failure to survive after in-hospital cardiopulmonary resuscitation: A meta-analysis. Fam. Pract. 2011, 28, 505–515. [Google Scholar] [CrossRef] [Green Version]
- Piscator, E.; Hedberg, P.; Goransson, K.; Djarv, T. Survival after in-hospital cardiac arrest is highly associated with the Age-combined Charlson Co-morbidity Index in a cohort study from a two-site Swedish University hospital. Resuscitation 2016, 99, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.C.; Lugton, J.; Spiller, J.A.; Carduff, E. CPR decision-making conversations in the UK: An integrative review. BMJ Supportive Palliat. Care 2019, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Elwyn, G.; Frosch, D.; Thomson, R.; Joseph-Williams, N.; Lloyd, A.; Kinnersley, P.; Cording, E.; Tomson, D.; Dodd, C.; Rollnick, S.; et al. Shared Decision Making: A Model for Clinical Practice. J. Gen. Intern. Med. 2012, 27, 1361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- You, J.J.; Jayaraman, D.; Swinton, M.; Jiang, X.; Heyland, D.K. Supporting shared decision-making about cardiopulmonary resuscitation using a video-based decision-support intervention in a hospital setting: A multisite before–after pilot study. CMAJ Open 2019, 7, E630. [Google Scholar] [CrossRef] [Green Version]
- Camuglia, A.C.; Randhawa, V.K.; Lavi, S.; Walters, D.L. Cardiac catheterization is associated with superior outcomes for survivors of out of hospital cardiac arrest: Review and meta-analysis. Resuscitation 2014, 85, 1533–1540. [Google Scholar] [CrossRef]
- Zanuttini, D.; Armellini, I.; Nucifora, G.; Carchietti, E.; Trillò, G.; Spedicato, L.; Bernardi, G.; Proclemer, A. Impact of emergency coronary angiography on in-hospital outcome of unconscious survivors after out-of-hospital cardiac arrest. Am. J. Cardiol. 2012, 110, 1723–1728. [Google Scholar] [CrossRef]
- Larsen, J.M.; Ravkilde, J. Acute coronary angiography in patients resuscitated from out-of-hospital cardiac arrest—A systematic review and meta-analysis. Resuscitation 2012, 83, 1427–1433. [Google Scholar] [CrossRef]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef]
- Chan, P.S.; Berg, R.A.; Tang, Y.; Curtis, L.H.; Spertus, J.A. Association Between Therapeutic Hypothermia and Survival After In-Hospital Cardiac Arrest. JAMA 2016, 316, 1375–1382. [Google Scholar] [CrossRef]
- Chen, C.T.; Chen, C.H.; Chen, T.Y.; Yen, D.H.; How, C.K.; Hou, P.C. Comparison of in-hospital and out-of-hospital cardiac arrest patients receiving targeted temperature management: A matched case-control study. J. Chin. Med. Assoc. 2020, 83, 858–864. [Google Scholar] [CrossRef] [PubMed]
- Engsig, M.; Søholm, H.; Folke, F.; Gadegaard, P.J.; Wiis, J.T.; Molin, R.; Mohr, T.; Engsig, F.N. Similar long-term survival of consecutive in-hospital and out-of-hospital cardiac arrest patients treated with targeted temperature management. Clin. Epidemiol. 2016, 8, 761–768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chien, Y.S.; Tsai, M.S.; Huang, C.H.; Lai, C.H.; Huang, W.C.; Chan, L.; Kuo, L.K. Outcomes of Targeted Temperature Management for In-Hospital and Out-Of-Hospital Cardiac Arrest: A Matched Case-Control Study Using the National Database of Taiwan Network of Targeted Temperature Management for Cardiac Arrest (TIMECARD) Registry. Med. Sci. Monit. 2021, 27, e931203. [Google Scholar] [CrossRef]
- Roedl, K.; Jarczak, D.; Blohm, R.; Winterland, S.; Müller, J.; Fuhrmann, V.; Westermann, D.; Söffker, G.; Kluge, S. Epidemiology of intensive care unit cardiac arrest: Characteristics, comorbidities, and post-cardiac arrest organ failure—A prospective observational study. Resuscitation 2020, 156, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Leloup, M.; Briatte, I.; Langlois, A.; Cariou, A.; Lesieur, O.; ACIR Study Group. Unexpected cardiac arrests occurring inside the ICU: Outcomes of a French prospective multicenter study. Intensive Care Med. 2020, 46, 1005–1015. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).