Abstract
Background and Aims: The coronavirus disease 2019 (COVID-19) increases hyperinflammatory state, leading to acute lung damage, hyperglycemia, vascular endothelial damage, and a higher mortality rate. Metformin is a first-line treatment for type 2 diabetes and is known to have anti-inflammatory and immunosuppressive effects. Previous studies have shown that metformin use is associated with decreased risk of mortality among patients with COVID-19; however, the results are still inconclusive. This study investigated the association between metformin and the risk of mortality among diabetes patients with COVID-19. Methods: Data were collected from online databases such as PubMed, EMBASE, Scopus, and Web of Science, and reference from the most relevant articles. The search and collection of relevant articles was carried out between 1 February 2020, and 20 June 2021. Two independent reviewers extracted information from selected studies. The random-effects model was used to estimate risk ratios (RRs), with a 95% confidence interval. Results: A total of 16 studies met all inclusion criteria. Diabetes patients given metformin had a significantly reduced risk of mortality (RR, 0.65; 95% CI: 0.54–0.80, p < 0.001, heterogeneity I2 = 75.88, Q = 62.20, and τ2 = 0.06, p < 0.001) compared with those who were not given metformin. Subgroup analyses showed that the beneficial effect of metformin was higher in the patients from North America (RR, 0.43; 95% CI: 0.26–0.72, p = 0.001, heterogeneity I2 = 85.57, Q = 34.65, τ2 = 0.31) than in patients from Europe (RR, 0.67; 95% CI: 0.47–0.94, p = 0.02, heterogeneity I2 = 82.69, Q = 23.11, τ2 = 0.10) and Asia (RR, 0.90; 95% CI: 0.43–1.86, p = 0.78, heterogeneity I2 = 64.12, Q = 11.15, τ2 = 0.40). Conclusions: This meta-analysis shows evidence that supports the theory that the use of metformin is associated with a decreased risk of mortality among diabetes patients with COVID-19. Randomized control trials with a higher number of participants are warranted to assess the effectiveness of metformin for reducing the mortality of COVID-19 patients.
1. Introduction
1.1. Rationale
On 31 December 2019, the first outbreak of coronavirus diseases-2019 (COVID-19) started in Wuhan, China, and has since affected more than 220 countries worldwide [1]. There are no specific drugs against SARS-CoV-2 infection; however, several existing drugs have been used to manage the disease’s severity [2]. As of 7 March 2021, the total number of confirmed cases has exceeded 116 million, and the total number of deaths is more than 2.5 million (https://www.worldometers.info/coronavirus/, accessed on 5 August 2021). Previous studies have reported that patients with multiple conditions, including diabetes, hypertension, obesity, and cardiac disease, are often at increased risk of acute respiratory distress syndrome (ARDS) and mortality [3,4,5,6]. Recently, observational studies have demonstrated that metformin use, both before and after diagnosis of COVID-19, is associated with a substantially decreased risk of mortality among patients with COVID-19 [7,8].
Several biological mechanisms can explain the potential biological effect of metformin on COVID-19 mortality. First, the mortality rate for COVID-19 is substantially higher in patients with an uncontrolled glucose level. Metformin is a widely used hypoglycemic drug and helps to improve the outcome of COVID-19 patients with diabetes by controlling glucose levels. Second, metformin activates adenosine monophosphate-activated protein kinase (AMPK), which eventually increases mitochondrial metabolism and autophagy and lessens the level of the inflammatory factors [9]. Third, SARS-CoV-2 induces the secretion of interferon-gamma and increases muscular insulin resistance and circulating insulin levels, which eventually increases the response of cluster of differentiation 8 cytotoxic T-cell (CD8 + T-cell) [10]. However, metformin has a protective role in the mitochondrial electron transport chain [11] and impairs memory T-cell responses through glycolysis promotion [12]. Given the epidemiological and biological plausibility of the benefits, there is an unmet need of meta-analysis to evaluate the magnitude of the association between them.
1.2. Goal of Investigation
Currently, significant data are available in retrospective studies concerning the beneficial effects of metformin on COVID-19 that could be used to facilitate personalized decision making in patients with COVID-19. Therefore, systematically reviewed evidence from existing retrospective studies to clarify the association between metformin use and the risk of mortality among patients with COVID-19.
1.3. Hypothesis
The research questions were:
- Magnitude of the risk of mortality among COVID-19 patients with metformin and those without metformin;
- Difference of magnitude of the risk of mortality among COVID-19 patients in the various continents.
2. Methods
This study was deemed exempt from review by the Taipei Medical University Review Board. No patient informed consent was required. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, which are based on the Cochrane Handbook for Systematic Reviews of Interventions, were used to conduct this study [13,14,15].
2.1. Search Strategy
A comprehensive and systematic search was conducted in online databases such as PubMed, Scopus, Embase, and Web of Science between 1 February 2020 and 20 June 2021, with no restriction of language. The keywords used to search the most relevant articles were: “Metformin” and “coronavirus related mortality” OR “COVID-19 mortality” OR “SARS-CoV-2 virus mortality”.
2.2. Eligibility Criteria
Study were included if they: (a) were restricted to epidemiological studies and evaluated the risk of mortality among COVID-19 patients with or with metformin, (b) included at least 15 participants to calculate the effect size, (c) provided clear inclusion and exclusion criteria of COVID-19 patients and metformin exposure. Studies were excluded if they had been published in the form of an editorial or review. Furthermore, we selected the most recent studies (hypothesized metformin and COVID-19 mortality) if they used similar databases.
2.3. Data Extraction
Two reviewers (M.M.I. and T.N.P.) independently screened the retrieved articles on the basis of pre-specified inclusion and exclusion criteria. Any disagreement between them was ultimately resolved through discussion with the main investigator. They first screened all the titles and abstracts, and the most relevant articles were kept for full-text revision. If the same author had published multiple papers using the same database, then the most recent study was considered for inclusion.
2.4. Statistical Analysis
The same two authors collected the effect size in term of the hazard ratio (HR) or odds ratio (OR) for each study, with a 95% CI. The random-effect model was used to calculate the risk ratio (RR) for the outcome of interest (COVID-19 mortality), with 95% CI. The I2 and Q statistics were also calculated to measure heterogeneity. The I2 value was also classified into four groups (0~25: very low, 25~50: low, 50~75: moderate, and >75: high). Forest plots were drawn to show the effect size for all associations. A funnel plot was constructed to present publication bias. However, all analyses were conducted using statistical software (Comprehensive Meta-Analysis, version 2.0, Biostat Inc. 14 North Dean Street, Englewood, NJ, USA).
3. Results
3.1. Literature Search
The online databases search yielded 228 articles. After reviewing all the titles and abstracts, 205 were excluded. A total of 23 articles went for full-text review, and 16 articles finally met all inclusion criteria [7,8,16,17,18,19,20,21,22,23,24,25,26,27,28,29] (Supplementary Figure S1).
3.2. Study Characteristics
Table 1 shows the baseline characteristics of the included studies. All of the studies used a retrospective study design. The percentage of male patient was between 35.1 and 97.3. Six studies were conducted in North America, five studies were from Europe, and five studies were from Asia. All patients had type-2 diabetes, and the number of metformin users were between 9 and 1,800,005. All studies reported in-hospital mortality, except for one.

Table 1.
Characteristics of included studies.
3.3. Primary Analysis
3.3.1. Metformin Use and COVID-19 Mortality
A total of 16 studies assessed the association between metformin use and the risk of mortality among patients with COVID-19. Metformin use was associated with a 35% decreased in risk of mortality among patients with COVID-19 (RR, 0.65, 95%CI: 0.54–0.80, p < 0.001) (Figure 1). There was a significant heterogeneity between the studies (I2 = 75.88, Q = 62.20, and τ2 = 0.06, p < 0.001).
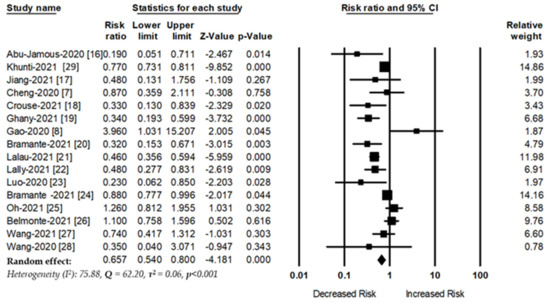
Figure 1.
Association between metformin use and COVID-19 mortality.
3.3.2. Subgroup Analysis
Subgroup analyses were also conducted to examine the magnitude of their association from different perspectives (Table 2). Eight studies used a nation-wide database, and eight studies used hospital-based data to evaluate the risk of COVID-19 mortality among patients with metformin. The overall risk of COVID-19 mortality with metformin were RR, 0.74 (95%CI: 0.60–0.89) and RR, 0.45 (95%CI: 0.27–0.74), respectively.

Table 2.
Summary of subgroup analyses.
There were no associations between metformin and COVID-19 mortality in the Asian population (RR, 0.90, 95%CI: 0.43–1.86). However, the beneficial effect of metformin was observed in the patients from Europe and North America (RR, 0.67, 95%CI: 0.47–0.94 vs. RR, 0.43, 95%CI: 0.26–0.72).
3.3.3. Sensitivity Analysis
To confirm the robustness of our findings, we categorized studies into three groups based on the number of metformin users with COVID-19 (<1000, 1000–10,000, and >10,000). Eleven studies included less than 1000 metformin users, and the risk of COVID-19 related mortality was significantly lower among metformin users (RR, 0.53 (95%CI: 0.32–0.81, p = 0.004)) (Supplementary Figure S2). There was a moderate significant heterogeneity among the studies (I2 = 69.31, Q = 32.58, and τ2 = 0.35, p < 0.001). Three studies included metformin users between 1000 and 10,000 and there was a insignificant reduction in mortality among metformin users (RR, 0.78 (95%CI: 0.47–1.29, p = 0.34)) (Supplementary Figure S3). There was a higher significant heterogeneity among the studies (I2 = 91.80, Q = 24.40, and τ2 = 0.17, p <0.001). Two studies included more than 10,000 metformin users with COVID-19, and there was a significant reduction in mortality among metformin users (RR, 0.77 (95%CI: 0.73–0.81, p < 0.001)) (Supplementary Figure S4). There was no heterogeneity between the studies (I2 = 0.00, Q = 0.01, and τ2 = 0, p = 0.89).
3.4. Secondary Analysis:
Metformin Use and Acute Respiratory Distress Syndrome Risk
Three studies evaluated the association between metformin use and Acute Respiratory Distress Syndrome (ARDS) risk. The overall pooled effect shows that metformin use was associated with a decreased risk of ARDS among COVID-19 patients with diabetes (RR, 0.39; 95%CI: 0.20–0.76, p = 0.006, I2 = 79.15, Q = 9.59, τ2 = 0.28) (Figure 2).
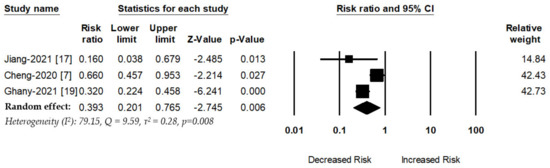
Figure 2.
Association between metformin use and ARDS risk.
3.5. Publication Bias
In Figure 3, the funnel plot shows no publication bias between the studies. Egger’s regression test was utilized to assess the funnel asymmetry, which indicated no publication bias (p = 0.20).
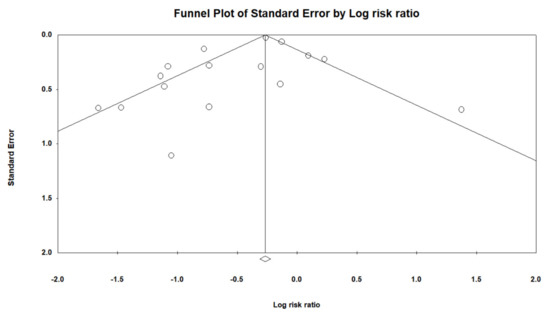
Figure 3.
Funnel plot.
4. Discussion
Our meta-analysis was designed to clarify the association between metformin use and risk of mortality in patients with COVID-19. The findings of our study show that metformin was associated with a decreased risk of mortality among COVID-19 patients, both before and after use. The beneficial effects of metformin was lower in the Asian population than in the non-Asian counterparts (North American and European). Genetic susceptibility and variation of β-cell function may influence their response to metformin treatment [30,31].
Our study findings are pertinent with four previous meta-analysis (Table 3) [32,33,34,35]. Lukito et al. [35] aimed to show the positive effect of metformin use on mortality in hospitalized COVID-19 patients, and nine studies met inclusion criteria. Metformin use was associated with a 36% reduced risk of mortality among hospitalized COVID-19 patients. However, they did not provide any subgroup analysis and sensitivity analysis. Scheen et al. [34] conducted a meta-analysis using only four studies, showing that metformin consumption was associated with a reduced risk of mortality among patients with COVID-19 (OR, 0.75, 95% CI: 0.67–0.85).

Table 3.
Comparison of effect size with other studies.
Several biological possibilities can explain the beneficial mechanism of metformin in COVID-19 patients (Table 4). Previous studies have shown that tumor necrosis factor-α (TNFα) has a significant role in COVID-19 pathology; it activates macrophage, increases cytokine release, and worsens the patient’s condition (Figure 4). However, metformin helps decrease cytokine release [Interleukin 6 (IL-6), TNFα], decreases thrombosis, reduces glycaemia, and increases the neutrophil to lymphocyte ration through angiotensin-converting enzyme 2 (ACE2) receptor modulation. There was a reduced level of inflammatory mediators, IL-6 and TNFα, in both diabetes and non-diabetes patients while using metformin. Moreover, metformin shows the significant positive effect on reducing the neutrophil counts, and decreasing neutrophil extracellular traps [36,37]. Metformin helps to increase ACE-2 expression via adenosine monophosphate-activated protein kinase (AMPK) activation, which leads to reduced cytokine response. It is reported that the direct entry of SAR-CoV-2 increase endoplasmic reticulum stress; however, metformin suppress the ER stress through activation of the 5-AMPK-phosphatidylinositol 3 kinase (PI3K)-c-Jun NH2 pathway [38].

Table 4.
The beneficial mechanism of metformin against COVID-19.
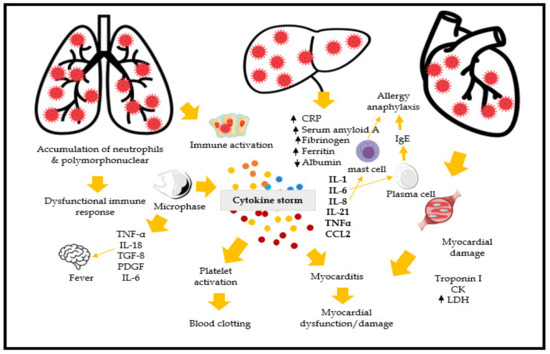
Figure 4.
Biological mechanism of COVID-19. (Note: CRP: C-reactive protein; CCL2: chemokine ligand 2; TNF- α: tumor necrosis factor-α; IL-1, 6, 8, 18, 21: Interleukin-1, 6, 8, 18, 21; TGF-8: Transforming growth factor 8; PDGF: Platelet-derived growth factor; LDH: Lactate dehydrogenase, IgE: Immunoglobulin E).
In addition, metformin help to reduce the release of inflammatory markers by affecting the MTOR and NF-kappa B pathways [39]. Previous studies have demonstrated that SARS-CoV-2 activates several cellular responses, including cellular stress responses such as unfolded protein response (UPR) and autophagy, through the inhibition of mTOR [40]. The biological mechanism of UPR and autophagy are involved in cellular and tissue homeostasis, apoptosis, and innate immunity modulation. However, metformin has great potential to inhibit protein synthesis, inhibit UPR, and activate the immune system [41]. It also appears that the physical condition of patients with SARS-CoV-2 is more likely to deteriorate due to multiple comorbidities, including cardiovascular diseases. Invasion of SARS-CoV-2 is associated with advanced vascular endothelial glycocalyx damage, especially in elderly patients [42]. However, deterioration of vascular endothelial glycocalyx can be a potent mechanism for the development of life-threatening complications, including acute kidney injury, among COVID-19 patients [43]. Multiples studies have shown that metformin induces endothelial glycocalyx restoration and protects the cardiovascular system [44,45].
Other molecular pathways common to diabetes and SARS-CoV-2 infection can be used to explain the potential benefit of metformin. Viral-induced interferon-gamma secretion has been demonstrated to increase muscular insulin resistance and circulating insulin levels, which, in turn, increases the cluster of differentiation 8 cytotoxic T-cell (CD8 + T-cell) responses.
Our study has several strengths. First, it is an updated meta-analysis of 17 studies that evaluated the beneficial effect of metformin on COVID-19 mortality. Second, we have shown a broad subgroup analysis of the association between them. Third, we have shown several possible mechanisms of how metformin plays a protective role in COVID-19 mortality.
Our study has some limitations that need to be addressed. First, our study shows metformin was associated with a decreased risk of mortality but the duration of metformin use and reduced risk of mortality was not reported due to data unavailability. Second, we are unable to show gender-specific mortality among COVID-19 patients with or without mortality. Third, we are also unable to show what would be the optimal dose for a protective effect against COVID-19. Fourth, our analyses were only based on retrospective observational studies. The quality of retrospective observational studies is generally poor and contains some risk of bias. However, there were no randomized controlled trials (RCTs) available while conducting this study. In future, RCTs should be conducted to confirm or refute their association. Fifth, there was also significant heterogeneity of the pooled studies, although we did use random effect models to reduce the bias of studies due to heterogeneity. Finally, our study could not provide any information about the risk of mortality of COVID-19 patients with continuation or discontinuation of metformin use until admission due to lack of data.
5. Conclusions
Our updated meta-analysis shows that metformin use is associated with a reduced risk of mortality among patients with COVID-19. However, the possibility of confounding factors cannot be excluded. Clinicians also need to carefully evaluate the actual benefits of metformin for patients who are currently taking it and who are also at risk of COVID-19 mortality. A large prospective RCT is warranted to assess the beneficial effects of metformin treatment in COVID-19, especially in nondiabetic patients.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10163507/s1, Figure S1: Searching strategy, Figure S2: Metformin use and the risk of mortality of patients with COVID-19 (Studies included metformin users less than 1000 participants), Figure S3: Metformin use and the risk of mortality of patients with COVID-19 (Studies included metformin users between 1000 and 10,000 participants), Figure S4: Metformin use and the risk of mortality of patients with COVID-19 (Studies included metformin users more than 10,000 participants).
Author Contributions
Conceptualization, methodology, software, resources, data curation, and writing—original draft preparation, T.N.P., Y.-C.W., M.-C.L., M.-H.H. and M.M.I.; writing—review and editing and supervision, Y.-C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
This research was funded in part by the Ministry of Education (MOE) under grants MOE 109-6604-001-400 and DP2-109-21121-01-A-01 and the Ministry of Science and Technology (MOST) under grant MOST 109-2823-8-038-004.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Yao, X.; Ye, F.; Zhang, M.; Cui, C.; Huang, B.; Niu, P.; Liu, X.; Zhao, L.; Dong, E.; Song, C. In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin. Infect. Dis. 2020, 71, 732–739. [Google Scholar] [CrossRef] [Green Version]
- Poly, T.N.; Islam, M.M.; Yang, H.C.; Lin, M.C.; Jian, W.-S.; Hsu, M.-H.; Li, Y.-C.J. Obesity and Mortality Among Patients Diagnosed With COVID-19: A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 620044. [Google Scholar] [CrossRef]
- Lippi, G.; Wong, J.; Henry, B.M. Hypertension and its severity or mortality in Coronavirus Disease 2019 (COVID-19): A pooled analysis. Pol. Arch. Intern. Med. 2020, 130, 304–309. [Google Scholar] [CrossRef] [Green Version]
- Kumar, A.; Arora, A.; Sharma, P.; Anikhindi, S.A.; Bansal, N.; Singla, V.; Khare, S.; Srivastava, A. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Pranata, R.; Huang, I.; Lim, M.A.; Wahjoepramono, E.J.; July, J. Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19–systematic review, meta-analysis, and meta-regression. J. Stroke Cerebrovasc. Dis. 2020, 29, 104949. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Liu, Y.-M.; Li, H.; Zhang, X.; Lei, F.; Qin, J.-J.; Chen, Z.; Deng, K.-Q.; Lin, L.; Chen, M.-M.; et al. Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Pre-existing Type 2 Diabetes. Cell Metab. 2020, 32, 537–547.e533. [Google Scholar] [CrossRef]
- Gao, Y.; Liu, T.; Zhong, W.; Liu, R.; Zhou, H.; Huang, W.; Zhang, W. Risk of Metformin in Patients with Type 2 Diabetes with COVID-19: A Preliminary Retrospective Report. Clin. Transl. Sci. 2020, 13, 1055–1059. [Google Scholar] [CrossRef] [PubMed]
- Foretz, M.; Guigas, B.; Viollet, B. Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus. Nat. Rev. Endocrinol. 2019, 15, 569–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Šestan, M.; Marinović, S.; Kavazovic, I.; Cekinović, Đ.; Wueest, S.; Wensveen, T.T.; Brizić, I.; Jonjic, S.; Konrad, D.; Wensveen, F.; et al. Virus-Induced Interferon-γ Causes Insulin Resistance in Skeletal Muscle and Derails Glycemic Control in Obesity. Immunity 2018, 49, 164–177.e166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrzejewski, S.; Siegel, P.M.; St-Pierre, J. Metabolic profiles associated with metformin efficacy in cancer. Front. Endocrinol. 2018, 9, 372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siska, P.J.; Rathmell, J.C. T cell metabolic fitness in antitumor immunity. Trends Immunol. 2015, 36, 257–264. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Islam, M.; Iqbal, U.; Walther, B.; Atique, S.; Dubey, N.K.; Nguyen, P.-A.; Poly, T.N.; Masud, J.H.B.; Li, Y.-C.; Shabbir, S.-A. Benzodiazepine Use and Risk of Dementia in the Elderly Population: A Systematic Review and Meta-Analysis. Neuroepidemiology 2016, 47, 181–191. [Google Scholar] [CrossRef]
- Wu, C.C.; Lee, A.J.; Su, C.H.; Huang, C.Y.; Islam, M.; Weng, Y.C. Statin Use Is Associated with a Decreased Risk of Mortality among Patients with COVID-19. J. Clin. Med. 2021, 10, 1450. [Google Scholar] [CrossRef]
- Abu-Jamous, B.; Anisimovich, A.; Baxter, J.; Mackillop, L.; Vizcaychipi, M.P.; McCarthy, A.; Khan, R.T. Associations of comorbidities and medications with COVID-19 outcome: A retrospective analysis of real-world evidence data. medRxiv 2020. [Google Scholar] [CrossRef]
- Jiang, N.; Chen, Z.; Liu, L.; Yin, X.; Yang, H.; Tan, X.; Wang, J.; Li, H.; Tian, M.; Lu, Z.; et al. Association of metformin with mortality or ARDS in patients with COVID-19 and type 2 diabetes: A retrospective cohort study. Diabetes Res. Clin. Pr. 2021, 173, 108619. [Google Scholar] [CrossRef] [PubMed]
- Crouse, A.B.; Grimes, T.; Li, P.; Might, M.; Ovalle, F.; Shalev, A. Metformin Use Is Associated with Reduced Mortality in a Diverse Population with COVID-19 and Diabetes. Front. Endocrinol. 2021, 11, 600439. [Google Scholar] [CrossRef]
- Ghany, R.; Palacio, A.; Dawkins, E.; Chen, G.; McCarter, D.; Forbes, E.; Chung, B.; Tamariz, L. Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Bramante, C.T.; Buse, J.; Tamaritz, L.; Palacio, A.; Cohen, K.; Vojta, D.; Liebovitz, D.; Mitchell, N.; Nicklas, J.; Lingvay, I.; et al. Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity. J. Med. Virol. 2021, 93, 4273–4279. [Google Scholar] [CrossRef]
- Lalau, J.-D.; Al-Salameh, A.; Hadjadj, S.; Goronflot, T.; Wiernsperger, N.; Pichelin, M.; Allix, I.; Amadou, C.; Bourron, O.; Duriez, T.; et al. Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19. Diabetes Metab. 2021, 47, 101216. [Google Scholar] [CrossRef] [PubMed]
- Lally, M.A.; Tsoukas, P.; Halladay, C.W.; O’Neill, E.; Gravenstein, S.; Rudolph, J.L. Metformin is associated with decreased 30-day mortality among nursing home residents infected with SARS-CoV2. J. Am. Med Dir. Assoc. 2021, 22, 193–198. [Google Scholar] [CrossRef]
- Luo, P.; Qiu, L.; Liu, Y.; Liu, X.-l.; Zheng, J.-l.; Xue, H.-y.; Liu, W.-h.; Liu, D.; Li, J. Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis. Am. J. Trop. Med. Hyg. 2020, 103, 69–72. [Google Scholar] [CrossRef]
- Bramante, C.T.; Ingraham, N.E.; Murray, T.A.; Marmor, S.; Hovertsen, S.; Gronski, J.; McNeil, C.; Feng, R.; Guzman, G.; Abdelwahab, N.; et al. Metformin and risk of mortality in patients hospitalised with COVID-19: A retrospective cohort analysis. Lancet Health Longev. 2021, 2, e34–e41. [Google Scholar] [CrossRef]
- Oh, T.K.; Song, I.-A. Metformin use and risk of COVID-19 among patients with type II diabetes mellitus: An NHIS-COVID-19 database cohort study. Acta Diabetol. 2021, 58, 771–778. [Google Scholar] [CrossRef]
- Pérez-Belmonte, L.M.; Torres-Peña, J.D.; López-Carmona, M.D.; Ayala-Gutiérrez, M.M.; Fuentes-Jiménez, F.; Huerta, L.J.; Muñoz, J.A.; Rubio-Rivas, M.; Madrazo, M.; Garcia, M.G.; et al. Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: A nationwide cohort study. BMC Med. 2020, 18, 359. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Cooper, J.M.; Gokhale, K.; Acosta-Mena, D.; Dhalla, S.; Byne, N.; Chandan, J.S.; Anand, A.; Okoth, K.; Subramanian, A.; et al. Association of Metformin with Susceptibility to COVID-19 in People with Type 2 Diabetes. J. Clin. Endocrinol. Metab. 2021, 106, 1255–1268. [Google Scholar] [CrossRef]
- Wang, B.; Van Oekelen, O.; Mouhieddine, T.H.; Del Valle, D.M.; Richter, J.; Cho, H.J.; Richard, S.; Chari, A.; Gnjatic, S.; Merad, M.; et al. A tertiary center experience of multiple myeloma patients with COVID-19: Lessons learned and the path forward. J. Hematol. Oncol. 2020, 13, 94. [Google Scholar] [CrossRef] [PubMed]
- Khunti, K.; Knighton, P.; Zaccardi, F.; Bakhai, C.; Barron, E.; Holman, N.; Kar, P.; Meace, C.; Sattar, N.; Sharp, S.; et al. Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: A nationwide observational study in England. Lancet Diabetes Endocrinol. 2021, 9, 293–303. [Google Scholar] [CrossRef]
- Cai, X.-L.; Ji, L.-N. Treatment response between Asian and non-Asian patients with type 2 diabetes: Is there any similarity or difference? Chin. Med. J. 2019, 132, 1. [Google Scholar] [CrossRef]
- Di Xiao, J.Y.; Zhang, S.M.; Liu, R.R.; Yin, J.Y.; Han, X.Y.; Li, X.; Zhang, W.; Chen, X.P.; Zhou, H.H.; Ji, L.N.; et al. A Two-Stage Study Identifies Two Novel Polymorphisms in PRKAG2 Affecting Metformin Response in Chinese Type 2 Diabetes Patients. Pharm. Pers. Med. 2021, 14, 745. [Google Scholar] [CrossRef]
- Hariyanto, T.I.; Kurniawan, A. Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection. Obes. Med. 2020, 19, 100290. [Google Scholar] [CrossRef] [PubMed]
- Kow, C.S.; Hasan, S. Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis. J. Med. Virol. 2021, 93, 695–697. [Google Scholar] [CrossRef] [PubMed]
- Scheen, A.J. Metformin and COVID-19: From cellular mechanisms to reduced mortality. Diabetes Metab. 2020, 46, 423–426. [Google Scholar] [CrossRef]
- Lukito, A.A.; Pranata, R.; Henrina, J.; Lim, M.A.; Lawrensia, S.; Suastika, K. The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 patients: A systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 2177–2183. [Google Scholar] [CrossRef] [PubMed]
- Zangiabadian, M.; Nejadghaderi, S.A.; Zahmatkesh, M.M.; Hajikhani, B.; Mirsaeidi, M.; Nasiri, M.J. The Efficacy and Potential Mechanisms of Metformin in the Treatment of COVID-19 in the Diabetics: A Systematic Review. Front. Endocrinol. 2021, 12, 263. [Google Scholar] [CrossRef]
- Sukumar, M.; Liu, J.; Ji, Y.; Subramanian, M.; Crompton, J.G.; Yu, Z.; Roychoudhuri, R.; Palmer, D.C.; Muranski, P.; Karoly, E.D.; et al. Inhibiting glycolytic metabolism enhances CD8+ T cell memory and antitumor function. J. Clin. Investig. 2013, 123, 4479–4488. [Google Scholar] [CrossRef]
- Jung, T.W.; Lee, M.W.; Lee, Y.J.; Kim, S.M. Metformin prevents endoplasmic reticulum stress-induced apoptosis through AMPK-PI3K-c-Jun NH2 pathway. Biochem. Biophys. Res. Commun. 2012, 417, 147–152. [Google Scholar] [CrossRef]
- Isoda, K.; Young, J.L.; Zirlik, A.; MacFarlane, L.A.; Tsuboi, N.; Gerdes, N.; Schonbeck, U.; Libby, P. Metformin inhibits proinflammatory responses and nuclear factor-κB in human vascular wall cells. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 611–617. [Google Scholar] [CrossRef] [Green Version]
- Siri, M.; Dastghaib, S.; Zamani, M.; Rahmani-Kukia, N.; Geraylow, K.R.; Fakher, S.; Keshvarzi, F.; Mehrbod, P.; Ahmadi, M.; Mokarram, P. Autophagy, Unfolded Protein Response, and Neuropilin-1 Cross-Talk in SARS-CoV-2 Infection: What Can Be Learned from Other Coronaviruses. Int. J. Mol. Sci. 2021, 22, 5992. [Google Scholar] [CrossRef]
- Kaneto, H.; Kimura, T.; Obata, A.; Shimoda, M.; Kaku, K. Multifaceted Mechanisms of Action of Metformin Which Have Been Unraveled One after Another in the Long History. Int. J. Mol. Sci. 2021, 22, 2596. [Google Scholar] [CrossRef] [PubMed]
- Groen, B.B.L.; Hamer, H.M.; Snijders, T.; Van Kranenburg, J.; Frijns, D.; Vink, H.; van Loon, L.J. Skeletal muscle capillary density and microvascular function are compromised with aging and type 2 diabetes. J. Appl. Physiol. 2014, 116, 998–1005. [Google Scholar] [CrossRef] [Green Version]
- Yamaoka-Tojo, M. Endothelial glycocalyx damage as a systemic inflammatory microvascular endotheliopathy in COVID-19. Biomed. J. 2020, 43, 399–413. [Google Scholar] [CrossRef] [PubMed]
- Eskens, B.J.M.; Zuurbier, C.J.; Van Haare, J.; Vink, H.; Van Teeffelen, J.W.G.E. Effects of two weeks of metformin treatment on whole-body glycocalyx barrier properties in db/db mice. Cardiovasc. Diabetol. 2013, 12, 175. [Google Scholar] [CrossRef] [Green Version]
- Targosz-Korecka, M.; Malek-Zietek, K.E.; Kloska, D.; Rajfur, Z.; Stepien, E.Ł.; Grochot-Przeczek, A.; Szymonski, M. Metformin attenuates adhesion between cancer and endothelial cells in chronic hyperglycemia by recovery of the endothelial glycocalyx barrier. Biochim. Biophys. Acta (BBA) Gen. Subj. 2020, 1864, 129533. [Google Scholar] [CrossRef]
- Ceriello, A. Hyperglycemia and the worse prognosis of COVID-19. Why a fast blood glucose control should be mandatory. Diabetes Res. Clin. Pract. 2020, 163, 108186. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A.; De Nigris, V.; Prattichizzo, F. Why is hyperglycaemia worsening COVID-19 and its prognosis? Diabetes Obes. Metab. 2020, 22, 1951–1952. [Google Scholar] [CrossRef]
- Chen, Y.; Gu, F.; Guan, J.-L. Metformin Might Inhibit Virus through Increasing Insulin Sensitivity. Chin. Med. J. 2018, 131, 376–377. [Google Scholar] [CrossRef]
- Sharma, S.; Ray, A.; Sadasivam, B. Metformin in COVID-19: A possible role beyond diabetes. Diabetes Res. Clin. Pr. 2020, 164, 108183. [Google Scholar] [CrossRef]
- Jing, Y.; Wu, F.; Li, D.; Yang, L.; Li, Q.; Li, R. Metformin improves obesity-associated inflammation by altering macrophages polarization. Mol. Cell. Endocrinol. 2018, 461, 256–264. [Google Scholar] [CrossRef]
- Desai, N.; Roman, A.; Rochelson, B.; Gupta, M.; Xue, X.; Chatterjee, P.K.; Tam, H.T.; Metz, C.N. Maternal metformin treatment decreases fetal inflammation in a rat model of obesity and metabolic syndrome. Am. J. Obstet. Gynecol. 2013, 209, 136.e131–136.e139. [Google Scholar] [CrossRef]
- El-Arabey, A.A.; Abdalla, M. Metformin and COVID-19: A novel deal of an old drug. J. Med. Virol. 2020, 92, 2293–2294. [Google Scholar] [CrossRef]
- Seifarth, C.; Schehler, B.; Schneider, H.J. Effectiveness of Metformin on Weight Loss in Non-Diabetic Individuals with Obesity. Exp. Clin. Endocrinol. Diabetes 2012, 121, 27–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ansari, G.; Mojtahedzadeh, M.; Kajbaf, F.; Najafi, A.; Khajavi, M.R.; Khalili, H.; Rouini, M.R.; Ahmadi, H.; Abdollahi, M. How does blood glucose control with metformin influence intensive insulin protocols? Evidence for involvement of oxidative stress and inflammatory cytokines. Adv. Ther. 2008, 25, 681–702. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Liu, X.; Ye, S. Effects of metformin on blood and urine pro-inflammatory mediators in patients with type 2 diabetes. J. Inflamm. 2016, 13, 34. [Google Scholar] [CrossRef] [PubMed]
- Algire, C.; Moiseeva, O.; Deschênes-Simard, X.; Amrein, L.; Petruccelli, L.; Birman, E.; Viollet, B.; Ferbeyre, G.; Pollak, M.N. Metformin Reduces Endogenous Reactive Oxygen Species and Associated DNA Damage. Cancer Prev. Res. 2012, 5, 536–543. [Google Scholar] [CrossRef] [Green Version]
- Ouslimani, N.; Peynet, J.; Bonnefont-Rousselot, D.; Thérond, P.; Legrand, A.; Beaudeux, J.-L. Metformin decreases intracellular production of reactive oxygen species in aortic endothelial cells. Metabolism 2005, 54, 829–834. [Google Scholar] [CrossRef]
- Hou, X.; Song, J.; Li, X.-N.; Zhang, L.; Wang, X.; Chen, L.; Shen, Y.H. Metformin reduces intracellular reactive oxygen species levels by upregulating expression of the antioxidant thioredoxin via the AMPK-FOXO3 pathway. Biochem. Biophys. Res. Commun. 2010, 396, 199–205. [Google Scholar] [CrossRef]
- Malhotra, A.; Hepokoski, M.; McCowen, K.C.; Shyy, J.Y.-J. ACE2, Metformin, and COVID-19. iScience 2020, 23, 101425. [Google Scholar] [CrossRef]
- Nesti, L.; Natali, A. Metformin effects on the heart and the cardiovascular system: A review of experimental and clinical data. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 657–669. [Google Scholar] [CrossRef]
- Borges, C.M.; Fujihara, C.K.; Malheiros, D.M.A.C.; De Ávila, V.F.; Formigari, G.P.; De Faria, J.B.L. Metformin arrests the progression of established kidney disease in the subtotal nephrectomy model of chronic kidney disease. Am. J. Physiol. Physiol. 2020, 318, F1229–F1236. [Google Scholar] [CrossRef]
- Sturmlechner, I.; Durik, M.; Sieben, C.J.; Baker, D.J.; Van Deursen, J.M. Cellular senescence in renal ageing and disease. Nat. Rev. Nephrol. 2016, 13, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Christensen, M.; Schiffer, T.; Gustafsson, H.; Krag, S.P.; Nørregaard, R.; Palm, F. Metformin attenuates renal medullary hypoxia in diabetic nephropathy through inhibition uncoupling protein-2. Diabetes/Metab. Res. Rev. 2019, 35, e3091. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Ruan, X.-l.; Xue, Y.-x.; Yang, S.; Shi, M.; Wang, L.-n. Metformin reduces the senescence of renal tubular epithelial cells in diabetic nephropathy via the MBNL1/miR-130a-3p/STAT3 pathway. Oxidative Med. Cell. Longev. 2020, 2020, 8708236. [Google Scholar] [CrossRef] [PubMed]
- Dalan, R. Metformin, neutrophils and COVID-19 infection. Diabetes Res. Clin. Pract. 2020, 164, 108230. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, H.; Nomura, N.; Shoda, W.; Isobe, K.; Kikuchi, H.; Yamamoto, K.; Fujimaru, T.; Ando, F.; Mori, T.; Okado, T.; et al. Metformin increases urinary sodium excretion by reducing phosphorylation of the sodium-chloride cotransporter. Metabolism 2018, 85, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Liu, L.; Xu, L.; Xing, Y.; Ye, S. Metformin alleviates renal injury in diabetic rats by inducing Sirt1/FoxO1 autophagic signal axis. Clin. Exp. Pharmacol. Physiol. 2020, 47, 599–608. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).