Abstract
Our goal was to evaluate the feasibility, safety, and short-term outcomes of prostate artery embolization (PAE) with N-butyl cyanoacrylate (NBCA) glue as the only embolic agent in patients with benign prostatic hyperplasia (BPH)-related lower urinary tract symptoms (LUTSs). A two-center retrospective study of 50 patients (mean age, 67.6 ± 7.4 years; range, 54–85 years) treated with NBCA between 2017 and 2020 was conducted. PAE was performed using a mixture of Glubran 2 glue and Lipiodol in a 1:8 ratio, under local anesthesia, on an outpatient basis, after cone-beam computed tomography vascular mapping. Mean total injected NBCA/Lipiodol volume was 0.9 ± 0.3 mL, total injection time was 21.9 ± 7.8 s, and total radiation dose was 18,458 ± 16,397 mGy·cm. Statistically significant improvements over time occurred for the International Prostate Symptoms Score (9.9 ± 6.8 versus 20.5 ± 6.7, p = 0.0001), quality-of-life score (2.2 ± 1.5 versus 4.9 ± 1.0, p = 0.0001), prostate-specific antigen level (4.6 ± 3.0 versus 6.4 ± 3.7, p = 0.0001), and prostate volume (77.3 ± 30.5 versus 98.3 ± 40.2, p = 0.0001) at a median of 3 months versus baseline. Minor adverse events developed in 11/50 (22%) patients, but no major complications occurred. The International Index of Erectile Function did not change significantly. PAE with NBCA is feasible, safe, fast, and effective for patients with BPH-related LUTSs. Prospective comparative studies with longer follow-ups are warranted.
1. Introduction
Benign prostatic hyperplasia (BPH) is associated with lower urinary tract symptoms (LUTSs) and quality-of-life (QoL) alterations in aging men []. Transurethral resection of the prostate (TURP) remains the standard of care for most patients with failure of, or intolerance to, first-line pharmacotherapy and/or specific food supplements [,,]. However, TURP can be associated with complications such as bleeding, infection, and retrograde ejaculation []. Furthermore, advanced age or anticoagulant therapy may contraindicate TURP. Prostate artery embolization (PAE) has become a recognized and promising therapeutic option for the management of BPH, as recent level-I evidence suggests good efficacy [,,,,,,]. Despite not being recommended as first-line treatment for LUTSs due to BPH, it can be used as an alternative to standard surgical techniques, after failure to respond or intolerance to standard pharmacotherapy (α-1 adrenergic receptor antagonist and/or 5-α reductase inhibitor) [,].
Advantages of PAE compared to established surgical methods include performance under local anesthesia and absence of a need for postoperative physical rest [,]. In addition, PAE is a minimally invasive procedure that has been found safer than, and as effective as, TURP in relieving BPH-related LUTSs as measured with the International Prostate Symptom Score (IPSS) [,,]. The European Association of Urology has stated that, despite the longer procedural time compared to TURP, the lesser blood loss and shorter hospitalization time support the use of PAE []. PAE is an advanced embolization technique usually performed with nonspherical particles (polyvinyl alcohol) to occlude the prostatic arteries []. No published study has compared the various commercialized embolic agents. Most studies relied on the free-flow injection of microspheres measuring 300–500 μm in diameter. Smaller particles (100–300 μm) are not recommended due to a higher risk of adverse events [,].
Liquid adhesive agents, notably N-butyl cyanoacrylate (NBCA), have shown excellent performance in controlling active bleeding from peripheral arteries [,]. NBCA is a liquid that polymerizes upon contact with ion-rich fluids such as blood. It has several advantages over other embolic agents [,]. Its quick administration and rapid polymerization allow fast hemostasis, which is extremely useful in patients with hemodynamic instability or massive focal bleeding. Due to its liquid consistency, NBCA allows distal embolization through a flow-directed strategy, particularly of small or tortuous arteries that are difficult to catheterize []. Furthermore, NBCA remains effective in patients with coagulopathy, which is common in gastrointestinal bleeding. Before administration, NBCA must be mixed with iodized oil (Lipiodol Ultra Fluid (UF); Guerbet, Aulnay-sous-Bois, France) to make the material radiopaque and to slow the NBCA polymerization rate []. However, NBCA is considered to be at higher risk for ischemic complications compared to other embolic agents, and its safe and effective handling requires substantial experience []. No published studies have evaluated NBCA for PAE in patients with BPH.
The goal of our study was to assess the feasibility, safety, and short-term efficacy of NBCA as an embolic agent for PAE in patients with symptomatic BPH.
2. Materials and Methods
2.1. Study Population
Consecutive patients treated by PAE for disabling BPH-related LUTSs at two academic centers between November 2017 and October 2020 were included in this retrospective study. Inclusion criteria were as follows: LUTSs attributed to BPH, LUTS duration ≥6 months, failure to respond or intolerance to standard pharmacotherapy (α-1 adrenergic receptor antagonist and/or 5-α reductase inhibitor) in patients contraindicated to or who refused surgery, IPSS > 7, IPSS-related QoL score > 2, and prostate volume > 40 mL. Exclusion criteria were biopsy-confirmed prostate cancer, active urinary tract infection, advanced atherosclerosis with tortuosity of the pelvic arteries, and advanced renal failure.
Our ethics committee approved the study and waived the requirement for informed patient consent in compliance with French legislation on retrospective studies of anonymized data.
2.2. Endovascular Procedure
All PAE procedures were performed by two experienced interventional radiologists (RL and FP) who were familiar with the procedure and followed the latest guidelines. PAE was performed on an outpatient basis, under local anesthesia, with no bladder catheter, usually via the femoral approach. An Artis Pheno (Siemens, Erlangen, Germany) or Allura XD 20 Clarity (Philips, Best, The Netherlands) angiography suite was used for 30 and 20 patients, respectively. A 5-French (Fr) sheath (Progreat; Terumo, Tokyo, Japan) was inserted into the right common femoral artery or left radial artery. The prostatic arterial supply was identified by selective internal iliac arteriography with a 4 Fr Cobra or Simmons type 2 catheter (Progreat; Terumo, Tokyo, Japan) on both sides. Superselective catheterization of the prostatic arteries was then performed coaxially with a 2.0–2.7 Fr microcatheter (Progreat; Terumo, Tokyo, Japan) and 0.014–0.018-inch hydrophilic guidewires. Three-dimensional (3D) rotational cone-beam computed tomography (CBCT) angiography was carried out routinely on both sides to obtain an arterial map, which avoided nontarget embolization due to anastomotic vessels.
Embolization was performed according to established techniques, bilaterally in most cases (Figure 1) []. After microcatheter positioning within the feeding artery, 2 mg of isosorbide dinitrate (Risordan, 10 mg/10 mL vial) was administered intra-arterially on each side for vasodilation. The microcatheter dead space and vascular bed of the prostatic lobe were then abundantly flushed with 10 mL of 5% dextrose solution to prevent polymerization and promote distal embolization. NBCA glue (Glubran 2, GEM; Viareggio, Italy) was diluted with iodized oil (Lipiodol Ultra Fluid; Guerbet, Aulnay-sous-Bois, France) to make the material radiopaque. A homogeneous NBCA–Lipiodol mixture was prepared immediately before the injection using two 5 mL luer-lock syringes and a three-way stopcock. A high NBCA dilution of 1:8 was used to increase mixture fluidity, thereby allowing distal embolization. Embolization was performed in free or blocked flow. Effectiveness was assessed visually during PAE, and the injection was stopped when substantial reflux occurred. The microcatheter was then promptly removed.
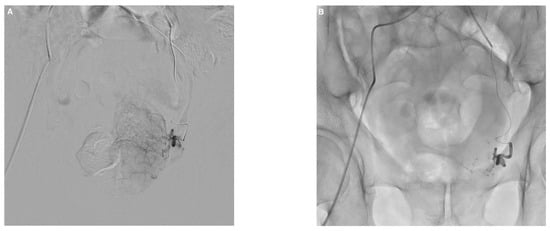
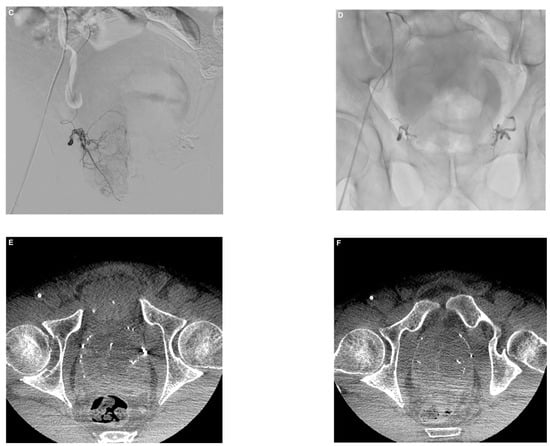
Figure 1.
Example of prostate artery embolization (PAE) with N-butyl cyanoacrylate glue in a 74-year-old patient with symptomatic benign prostatic hyperplasia. (A) Left prostatic artery angiogram before PAE showing enhancement of the left prostatic lobe. (B) Follow-up angiogram after PAE with a mixture of Glubran®2/Lipiodol in a 1:8 ratio showing total occlusion. (C) Right prostatic artery angiogram with enhancement of the right prostatic lobe. (D) Visualization of the glue/lipiodol cast in the branches of the right prostatic artery after injection of the same mixture, with complete occlusion. (E,F) Axial cone-beam computed tomography images without contrast injection after bilateral PAE showing lipiodol uptake by both prostatic lobes with distal and proximal distribution of the glue/lipiodol casts. Major improvements in lower urinary tract symptoms were noted 3 months after PAE compared to baseline (IPSS, 5 versus 24; QoL score, 2 versus 6; prostate volume, 110 versus 170 mL).
A vascular closure device was routinely placed at the puncture site (TR band (Terumo, Tokyo, Japan) for radial access and Exoseal (Cordis, Santa Clara, CA, USA) or FemoSeal (Terumo, Tokyo, Japan) for femoral access). Patients were monitored in the interventional unit for the first hour and in the ambulatory surgery department for 2 to 4 hours depending on whether access was radial or femoral. They were then discharged home with a prescription for 2 weeks of a prophylactic oral antibiotic and a nonsteroidal anti-inflammatory drug. Standard medical pharmacotherapy was continued for 2 weeks after PAE in all patients who were still under medication. Then, patients were asked to stop it.
2.3. Endpoints and Follow-Up
Data were collected before PAE (baseline) and at a scheduled follow-up visit 3 months after PAE. Clinical symptoms were assessed using the IPSS questionnaire, on which scores can range from 0 to 35 (≤7: mild symptoms; 8–19: moderate symptoms; ≥20 points: severe symptoms) and the LUTS-related IPSS-QoL score, for which responses can range from “0, delighted” to “6, terrible” [].
The primary endpoint was the change from baseline to the 3-month visit in the IPSS score. Secondary endpoints included the International Index of Erectile Function form 5 (IIEF5, with scores ranging from “0, worst” to “25, best”), prostate volume as assessed by magnetic resonance imaging and/or ultrasound, and serum prostate-specific antigen (PSA) levels. Urodynamic testing was not performed routinely.
Technical success, defined as complete occlusion of at least one vascularizing prostate artery, and clinical success, defined as a QoL score <3, were also evaluated. Other procedural parameters such as procedure time, fluoroscopy time, radiation dose to the patient, total injected NBCA/Lipiodol mixture volume, and total NBCA/Lipiodol mixture injection time were recorded.
Last, adverse events during follow-up were reported according to the Society of Interventional Radiology (SIR) classification as minor (A and B) or major [,] and according to the Clavien–Dindo grading system as minor (I and II) or major (III, IV, V) [,].
2.4. Statistical Analysis
Continuous variables are described as mean ± SD (range) and qualitative/semiquantitative variables as median (interquartile range). Semiquantitative variables such as the QoL and IIEF 5 scores were handled as continuous variables given the sample size and number of modalities, after verifying the convergence of parametric and nonparametric approaches. For the IPSS score and secondary outcomes, we report only the results of the univariate analyses using the paired t-test. P values < 0.05 were considered significant. A multivariate linear regression model was built using manual backward stepwise variable selection. Several intermediate models were constructed before the optimal model was obtained. This procedure ensured the robustness of our analysis despite the exclusion of potentially interesting variables such as the center, PSA level, and number of embolized vessels. Given the small number of adverse events (all of which were minor in our study), for adjusted analyses, we dichotomized adverse events according to the SIR classification. Multivariate analysis was performed in order to find confounding factors that could have led to IPSS improvement. The statistical analyses were performed using STATA software (version 14.0, STATA, College Station, TX, USA).
3. Results
3.1. Patients
Figure 2 is the flow chart. Of the 104 consecutive patients assessed for eligibility, 6 were excluded and 48 were treated with microparticles, leaving 50 patients who underwent PAE with NBCA between November 2017 and October 2020 (Figure 2). Table 1 displays the baseline characteristics of the study patients.
Figure 2.
Flow chart of the study. PAE, prostate artery embolization; NBCA, N-butyl cyanoacrylate.

Table 1.
Demographics and baseline characteristics of the study population.
3.2. Prostate Artery Embolization Procedure
Table 2 provides technical and anatomical details. Of the 50 patients, 3 (6%) required collateral embolization or protective proximal embolization of the penile artery.

Table 2.
Technical features of PAE and short-term safety outcomes.
Post-PAE angiograms showed complete occlusion of the targeted prostatic arteries in all 50 patients, yielding a technical success of 100%.
3.3. Safety and Outcomes
All patients recovered uneventfully and were discharged on the same day. No patients had major adverse events, and 11 (22%) experienced minor adverse events (Table 2). A groin hematoma developed in 5 patients and resolved spontaneously within 1–2 weeks. Transient erectile dysfunction in 4 patients abated spontaneously 2 months after PAE. One patient was diagnosed with a urinary tract infection 3 weeks after PAE and recovered with antibiotic therapy, and another had limited penile glans mucosal necrosis after PAE that healed spontaneously within about 3 weeks.
All patients were evaluated 3 months after PAE. Table 3 reports the efficacy outcomes. By univariate analysis, significant improvements vs. baseline were noted at 3 months for the IPSS, QoL score, PSA level, and prostate volume. The IIEF5 improvement was not statistically significant.

Table 3.
PAE efficacy outcomes after 3 months.
Overall and considering any clinical improvement, 45 (90%) of the 50 patients had IPSS improvement, 2 patients had stable IPSS, and 3 had IPSS worsening, after 3 months. Last, 43 (86%) of the 50 patients were satisfied after the PAE, meaning with a QoL score < 3. At 3 months, 45 (90%) of the 50 patients treated with PAE did not need pharmacotherapy anymore.
3.4. Prognostic Factors
By multivariate linear regression analysis, the center was not significantly associated with the IPSS or QoL score improvement at 3 months. Baseline prostate volume tended to be independently associated with the IPSS improvement, whereas no associations were found with age, anticoagulant medication, or bilateral PAE. Given the number of events and our sample size, to assess potential associations of adverse events with PAE outcomes we focused on the QoL score variation, which was not significantly different between patients with adverse events and patients without adverse events. Age, baseline IIEF5, and bilateral PAE were independently associated with the IPSS-QoL score improvement. Data are summarized in Table 4 and Table 5.

Table 4.
Multivariate analysis: factors independently associated with the IPSS improvement at month 3 vs. baseline.

Table 5.
Multivariate analysis: factors independently associated with the IPSS-QoL score improvement at month 3 vs. baseline.
4. Discussion
In this retrospective study, we investigated the role of PAE with NBCA as the embolic agent for the treatment of patients with incapacitating BPH-related LUTSs. We found statistically significant improvements in the IPSS, QoL score, PSA level, and prostate volume after a median follow-up of 3 months compared to baseline. About a fifth of the patients experienced minor complications, in keeping with results obtained using microparticles [,,,,]. No major complications were recorded. To our knowledge, this is the first clinical study reporting the use of NBCA for PAE.
The introduction of prostatic artery embolization to decrease the gland volume without surgery is a major breakthrough. Similarly, embolization of symptomatic uterine fibroids has produced comparable 5-year outcomes to those obtained with surgical excision []. Other studies of PAE in the same indication found similar IPSS improvements (evaluated at −10.6 points over time) with no major complications, notably no urinary incontinence or ejaculation dysfunction [,,,]. Few severe complications of PAE have been reported, with an incidence of 0.3% in a meta-analysis of 13 studies with 1254 patients []. None of our patients experienced major complications identified using the Clavien–Dindo or SIR classification [,,]. More specifically, no patients had dysuria, acute urinary retention, hematuria, or rectorrhagia. The five puncture-site hematomas resolved spontaneously, and conservative treatment was effective in the two patients who respectively experienced a urinary tract infection and limited glans mucosa necrosis. Bilateral embolization was not associated with the IPSS improvement but seemed to influence the QoL score, although the association fell slightly short of significance. Previous data on unilateral vs. bilateral PAE are discordant [,]. Prostate volume was not linked to symptomatic improvement in our patients, but prostate volume decreased by 21%, in keeping with the 19% reduction in one study [], whereas a greater reduction of 28% was obtained in another []. All our patients were treated on an ambulatory basis, and none required readmission for adverse events, as reported in a cohort of 486 patients []. Our higher technical and clinical success rates of 100% and 86%, respectively, may be partly explained by our small sample size resulting in limited power, and the corresponding proportions in a meta-analysis were 76.7% and 76.3% []. However, our results obtained using NBCA should be considered very promising.
The treatment of BPH-related LUTSs has changed markedly over the past 20–30 years, with a shift toward pharmacotherapy and management in primary care [,,]. Until now, patients whose LUTSs become incapacitating have typically been offered TURP and, more recently, laser prostatectomy [,]. Compared to less invasive interventions such as urethral stenting and prostatic urethral lift, PAE may provide superior urethral patency with a comparable safety profile []. Although, when assessing PAE, these minimally invasive procedures seem to be more reasonable than open surgery, no such trial has been published to date []. Moreover, no consensus exists about the relative efficacy and safety of PAE versus TURP, although both procedures are useful and seem to have a place in clinical practice [,]. Compared to TURP, for at least 12 months, PAE may provide similar improvements in urologic symptom scores and quality of life. Importantly, PAE may reduce postprocedural ejaculatory dysfunction, although few data on erectile dysfunction are available [,]. After longer follow-ups, QoL appears similar with TURP and PAE, but the need for reintervention may be higher with PAE []. PAE might be a valuable alternative for the treatment of BPH-related LUTSs in selected patients in whom the symptoms are the main reason for considering surgery []. Knowledge of predictors is helpful to identify those patients most likely to benefit from PAE, notably with NBCA [,,]. For instance, age is a crucial factor, and the risk of adverse events is significantly higher in patients older than 75 years [].
Microparticles were historically used for PAE as well as for uterine artery embolization [,,,]. Indeed, most interventional radiologists are familiar with the use of flow-directed particulate embolization for distal devascularization. Using glue for peripheral endovascular applications such as PAE requires more experience and a deep learning curve. A large proportion of interventional radiologists are unfortunately afraid of using NBCA despite many advantages. The main advantage of using NBCA is the shorter procedural time compared to particulate embolization, which decreases the fluoroscopy time and, therefore, the radiation dose to the patient. The total mixture injection time was less than 30 s in our study, and the fluoroscopy time was generally less than 30 min. Another advantage of NBCA is that the fast polymerization from surface to core avoids the opening of pre-existing vascular anastomoses, an event reported with particles, thereby potentially decreasing the risk of nontarget embolization [,,,]. In addition, NBCA can be more efficient than other embolic agents in patients with coagulopathy, since polymerization upon contact with blood anions is not dependent on coagulation function [,,,]. Our subgroup of nearly a fifth of our population treated with anticoagulant medication did not experience smaller IPSS improvements or more adverse events [,]. Moreover, smaller embolic particle size is associated with a higher adverse-event rate [,].
NBCA/Lipiodol has several other advantages [,]. Lipiodol makes the embolic material radiopaque, allowing for easier fluoroscopy guidance compared with other embolic materials that are not directly visualized, such as microparticles []. In addition, NBCA is a liquid and can therefore be used to occlude vessels in which the microcatheter cannot be advanced, according to the blocked-flow technique. This situation is particularly frequent in PAE, as the flow rate in prostatic arteries is low. Furthermore, the lipiodol is taken up by the prostate gland, and the distribution of the treated prostate territories then becomes clearly visible by CBCT or CT. This distribution could be used as a surrogate marker of clinical success, as reported for the liver []. Lastly, Glubran 2 has the advantage of being cheap in Europe by comparison with microparticles (about EUR 100 per 1 mL vial versus EUR 300 per syringe) even if added Lipiodol is needed (about EUR 250 per 10 mL vial). In the end, using glue plus lipiodol is not more expensive than using microparticles.
The risk of ischemic complications after NBCA glue embolization has always been a major concern. However, our data suggest that a mixture of NBCA and Lipiodol UF may not cause a higher number of relevant ischemic complications compared to other commonly used embolic agents such as microparticles. This finding can be explained by the characteristics of NBCA []. The NBCA/Lipiodol ratio affects the viscosity of the liquid mixture and the NBCA polymerization rate. The ratio should be adjusted to the length of the segment to be occluded [,]. This adjustment provides sufficient fluidity to ensure distal embolization of the feeding artery while keeping enough viscosity to prevent excessively distal penetration into the capillary bed, thereby preserving circulation in the distal postembolic tissue via collateral channels in the intramural microcirculation [,]. We used a high NBCA dilution ratio of 1:8 to allow very distal embolization [,]. Nontarget embolization occurred in a single patient. We routinely used CBCT, which has been reported to drastically decrease the risk of nontarget embolization [].
Precautions must be taken to minimize the complication rate. Flushing the microcatheter before the injection with dextrose to remove all ionic solutions and promptly pulling the catheter back after the injection to avoid adhesion to the vessel and trapping of NBCA are important [,]. Histoacryl is the most widely used NBCA glue, although it has not received the European Community (EC) mark and is not approved by the Food and Drug Administration. We used Glubran 2 (GEM Srl, Viareggio, Italy), the only EC-marked glue for endovascular administration. In Glubran 2, the comonomer methacryloxysulfolane is added to produce a more pliable and stable polymer with a lower polymerization temperature and less cytotoxicity than Histoacryl [,]. Thus, Glubran 2 may result in less inflammation and, therefore, in less pain. Finally, as indicated above, the use of CBCT decreases the risk of nontarget embolization.
In the present study, no comparison was performed in terms of outcomes between patients with a large intravesical median lobe and those with a nonlarge one. Maron et al. showed no significant differences in early outcomes in PAE between patients with severe (≥10 mm) and nonsevere (<10 mm) intravesical prostatic protrusion [], meaning that selection of patients should not be focused on this specific feature. However, previous studies indicated a greater impact of PAE-induced ischemia in the adenomatous than in the stromal element of the prostate gland []. Most authors agree nowadays that the mechanism by which PAE resolves dynamic obstruction in patients with BPH is the shrinkage of the enlarged prostate gland as a result of PAE-induced ischemic infarction [].
Over the last two decades, arterial embolization has gained acceptance for several indications in the urological field, either as a minimally invasive alternative to surgery or as a complementary therapeutic tool to surgery [,,,]. Indeed, arterial embolization can be used as a first-line therapy for the treatment of bleedings following partial nephrectomy, as a prophylactic therapy for large renal angiomyolipomas, or as a preoperative tool before radical nephrectomy in order to facilitate surgical intervention by decreasing intraoperative bleeding [,,]. It can also be used as a palliative treatment of hemorrhage from bladder or prostate cancer []. The use of these minimally invasive techniques, in urological surgery as well as in interventional radiology, allows for the reduction in the risk of surgical site infection by comparison with a traditional approach. In addition, minimally invasive surgery or intervention is usually associated with better perioperative outcomes and a lower rate of overall complications []. Surgical or interventional site complication is one of the main risks of such approaches. In terms of wound infection, it has been shown that sutures reduce postoperative pain and improve the grade of satisfaction with the cosmetic outcome as compared to staples []. In interventional radiology, the systematic use of vascular closure devices can reduce puncture-site-related complications as well.
Our study has several limitations. First, the retrospective design may have led to missing data. Second, PAE with NBCA was not compared to another intervention or embolic agent. Third, although two centers contributed to patient recruitment, our sample size of only 50 patients may have limited our ability to detect significant differences and may explain some discrepancies with earlier studies. Fourth, PAE was performed by two senior interventional radiologists who had considerable experience with PAE and NBCA embolization, one in each center, resulting in a risk of bias. Fifth, the short follow-up of 3 months is a limitation, given that later recanalization has been reported after PAE with microparticles []. However, our goal was to report the first clinical data to date to our knowledge on PAE with NBCA to treat BPH-related LUTSs. Further studies with longer follow-ups and comparisons of embolic agents are needed. Finally, we did not have uroflowmetry or postvoid residual volume data.
5. Conclusions
PAE with NBCA is a feasible, safe, fast, and effective procedure with promising results in patients with BPH-related LUTSs. Further prospective comparative studies with longer follow-ups are warranted to identify the best embolic agent and the patients most likely to benefit from PAE to treat BPH-related LUTSs.
Author Contributions
Conceptualization, R.L. and F.P.; methodology, K.G. and E.S.; software, K.G. and E.S.; validation, R.L. and F.P.; formal analysis, C.M. and M.M.; investigation, P.-O.C., N.G., O.C., and R.L.; resources, O.C.; data curation, M.M.; writing—original draft preparation, R.L., K.G., E.S., N.G., and F.P.; writing—review and editing, R.L.; K.G., C.M., O.C., N.G., and F.P.; visualization, R.L.; supervision, R.L. and F.P.; project administration, M.M.; funding acquisition, K.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded solely by institutional and departmental resources: no external funding was used.
Institutional Review Board Statement
Ethical review and approval were waived for this study, as it consisted in the retrospective assessment of anonymized data.
Informed Consent Statement
The need for informed patient consent was waived by the ethics committee that approved the study, as the study consisted in the retrospective assessment of anonymized data.
Data Availability Statement
All the study data are reported in this article.
Acknowledgments
We thank Ludwig-Serge Aho-Glélé for his help in statistical analyses.
Conflicts of Interest
None of the authors have any conflicts of interest to declare.
References
- Burnett, A.L.; Wein, A.J. Benign prostatic hyperplasia in primary care: What you need to know. J. Urol. 2006, 175, S19–S24. [Google Scholar] [CrossRef]
- Parsons, J.K.; Dahm, P.; Köhler, T.S.; Lerner, L.B.; Wilt, T.J. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2020. J. Urol. 2002, 204, 799–804. [Google Scholar] [CrossRef] [PubMed]
- Cormio, L.; Calò, B.; Falagario, U.; Iezzi, M.; Lamolinara, A.; Vitaglione, P.; Silecchia, G.; Carrieri, G.; Fogliano, V.; Iacobelli, S.; et al. Improvement of urinary tract symptoms and quality of life in benign prostate hyperplasia patients associated with consumption of a newly developed whole tomato-based food supplement: A phase II prospective, randomized double-blinded, placebo-controlled study. Transl. Med. 2021, 19, 24. [Google Scholar] [CrossRef]
- Geevarghese, R.; Harding, J.; Parsons, N.; Hutchinson, C.; Parsons, C. The relationship of embolic particle size to patient outcomes in prostate artery embolisation for benign prostatic hyperplasia: A systematic review and meta-regression. Clin. Radiol. 2020, 75, 366–374. [Google Scholar] [CrossRef]
- Maclean, D.; Harris, M.; Drake, T.; Maher, B.; Modi, S.; Dyer, J.; Somani, B.; Hacking, N.; Bryant, T. Factors predicting a good symptomatic outcome after prostate artery embolisation (PAE). Cardiovasc. Interv. Radiol. 2018, 41, 1152–1159. [Google Scholar] [CrossRef]
- Wang, M.; Guo, L.; Duan, F.; Yuan, K.; Zhang, G.; Li, K.; Yan, J.; Wang, Y.; Kang, H. Prostatic arterial embolization for the treatment of lower urinary tract symptoms caused by benign prostatic hyperplasia: A comparative study of medium- and large-volume prostates. BJU Int. 2016, 117, 155–164. [Google Scholar] [CrossRef]
- Zumstein, V.; Betschart, P.; Vetterlein, M.W.; Kluth, L.A.; Hechelhammer, L.; Mordasini, L.; Engeler, D.S.; Kessler, T.M.; Schmid, H.P.; Abt, D. Prostatic artery embolization versus standard surgical treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia: A systematic review and meta-analysis. Eur. Urol. Focus 2019, 5, 1091–1100. [Google Scholar] [CrossRef]
- Russo, G.I.; Kurbatov, D.; Sansalone, S.; Lepetukhin, A.; Dubsky, S.; Sitkin, I.; Salamone, C.; Fiorino, L.; Rozhivanov, R.; Cimino, S.; et al. Prostatic arterial embolization vs open prostatectomy: A 1-year matched-pair analysis of functional outcomes and morbidities. Urology 2015, 86, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, F.C.; Iscaife, A.; Yoshinaga, E.M.; Moreira, A.M.; Antunes, A.A.; Srougi, M. Transurethral resection of the prostate (TURP) versus original and PErFecTED prostate artery embolization (PAE) due to benign prostatic hyperplasia (BPH): Preliminary results of a single center, prospective, urodynamic-controlled analysis. Cardiovasc. Interv. Radiol. 2016, 39, 44–52. [Google Scholar] [CrossRef] [PubMed]
- DeMeritt, J.S.; Elmasri, F.F.; Esposito, M.P.; Rosenberg, G.S. Relief of benign prostatic hyperplasia-related bladder outlet obstruction after transarterial polyvinyl alcohol prostate embolization. J. Vasc. Interv. Radiol. 2000, 11, 767–770. [Google Scholar] [CrossRef]
- Abt, D.; Hechelhammer, L.; Müllhaupt, G.; Markart, S.; Güsewell, S.; Kessler, T.M.; Schmid, H.P.; Engeler, D.S.; Mordasini, L. Comparison of prostatic artery embolisation (PAE) versus transurethral resection of the prostate (TURP) for benign prostatic hyperplasia: Randomised, open label, non-inferiority trial. BMJ 2018, 361, k2338. [Google Scholar] [CrossRef]
- Ray, A.F.; Powell, J.; Speakman, M.J.; Longford, N.T.; DasGupta, R.; Bryant, T.; Modi, S.; Dyer, J.; Harris, M.; Carolan-Rees, G.; et al. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: An observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int. 2018, 122, 270–282. [Google Scholar] [CrossRef]
- Carnevale, F.C.; Moreira, A.M.; de Assis, A.M.; Antunes, A.A.; Cristina de Paula Rodrigues, V.; Srougi, M.; Cerri, G.G. Prostatic artery embolization for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: 10 years’ experience. Radiology 2020, 296, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Gravas, S.; Cornu, J.N.; Gacci, M.; Gratzke, C.; Herrmann, T.R.W.; Mamoulakis, C.; Rieken, M.; Speakman, M.J.; Tikkinen, K.A.O. Management of non-neurogenic male LUTS. EAU Guidelines Edn presented at the EAU Annual Congress Amsterdam 2020 [Internet]. EAU. 2020. Available online: http://uroweb.org/guidelines/compilations-of-all-guidelines/ (accessed on 9 July 2021).
- Bilhim, T.; Pisco, J.; Pereira, J.A.; Costa, N.V.; Fernandes, L.; Campos Pinheiro, L.; Duarte, M.; Oliveira, A.G. Predictors of clinical outcome after prostate artery embolization with spherical and nonspherical polyvinyl alcohol particles in patients with benign prostatic hyperplasia. Radiology 2016, 281, 289–300. [Google Scholar] [CrossRef] [PubMed]
- Abdulmalak, G.; Chevallier, O.; Falvo, N.; Di Marco, L.; Bertaut, A.; Moulin, B.; Abi-Khalil, C.; Gehin, S.; Charles, P.E.; Latournerie, M.; et al. Safety and efficacy of transcatheter embolization with Glubran®2 cyanoacrylate glue for acute arterial bleeding: A single-center experience with 104 patients. Abdom Radiol. 2018, 43, 723–733. [Google Scholar] [CrossRef]
- Loffroy, R.; Desmyttere, A.S.; Mouillot, T.; Pellegrinelli, J.; Facy, O.; Drouilllard, A.; Falvo, N.; Charles, P.E.; Bardou, M.; Midulla, M.; et al. Ten-year experience with arterial embolization for peptic ulcer bleeding: N-butyl cyanoacrylate glue versus other embolic agents. Eur. Radiol. 2021, 31, 3015–3026. [Google Scholar] [CrossRef] [PubMed]
- Loffroy, R.; Guiu, B.; Cercueil, J.P.; Krausé, D. Endovascular therapeutic embolisation: An overview of occluding agents and their effects on embolised tissues. Curr. Vasc. Pharm. 2009, 7, 250–263. [Google Scholar] [CrossRef]
- Barry, M.J.; Williford, W.O.; Chang, Y.; Machi, M.; Jones, K.M.; Walker-Corkery, E.; Lepor, H. Benign prostatic hyperplasia specific health status measures in clinical research: How much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? J. Urol. 1995, 154, 1770–1774. [Google Scholar] [CrossRef]
- Sacks, D.; McClenny, T.E.; Cardella, J.F.; Lewis, C.A. Society of Interventional Radiology clinical practice guidelines. J. Vasc. Interv. Radiol. 2003, 14, S199–S202. [Google Scholar] [CrossRef]
- Khalilzadeh, O.; Baerlocher, M.O.; Shyn, P.B.; Connolly, B.L.; Devane, A.M.; Morris, C.S.; Cohen, A.M.; Midia, M.; Thornton, R.H.; Gross, K.; et al. Proposal of a new adverse event classification by the Society of Interventional Radiology standards of practice committee. J. Vasc. Interv. Radiol. 2017, 28, 1432–1437.e3. [Google Scholar] [CrossRef]
- Ayyagari, R.; Powell, T.; Staib, L.; Chapiro, J.; Perez-Lozada, J.C.; Bhatia, S.; Chai, T.; Schoenberger, S.; Devito, R. Prostatic artery embolization in nonindex benign prostatic hyperplasia patients: Single-center outcomes for urinary retention and gross prostatic hematuria. Urology 2020, 136, 212–217. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Moss, J.G.; Cooper, K.G.; Khaund, A.; Murray, L.S.; Murray, G.D.; Wu, O.; Craig, L.E.; Lumsden, M.A. Randomised comparison of uterine artery embolisation (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5-year results. BJOG 2011, 118, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Kuang, M.; Vu, A.; Athreya, S. A systematic review of prostatic artery embolization in the treatment of symptomatic benign prostatic hyperplasia. Cardiovasc. Interv. Radiol. 2017, 40, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Malling, B.; Røder, M.A.; Brasso, K.; Forman, J.; Taudorf, M.; Lönn, L. Prostate artery embolisation for benign prostatic hyperplasia: A systematic review and meta-analysis. Eur. Radiol. 2019, 29, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Bilhim, T.; Pisco, J.; Rio Tinto, H.; Fernandes, L.; Campos Pinheiro, L.; Duarte, M.; Pereira, J.A.; Oliveira, A.G.; O’Neill, J. Unilateral versus bilateral prostatic arterial embolization for lower urinary tract symptoms in patients with prostate enlargement. Cardiovasc. Interv. Radiol. 2013, 36, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Pyo, J.S.; Cho, W.J. Systematic review and meta-analysis of prostatic artery embolisation for lower urinary tract symptoms related to benign prostatic hyperplasia. Clin. Radiol. 2017, 72, 16–22. [Google Scholar] [CrossRef]
- Jiang, Y.L.; Qian, L.J. Transurethral resection of the prostate versus prostatic artery embolization in the treatment of benign prostatic hyperplasia: A meta-analysis. BMC Urol. 2019, 19, 11. [Google Scholar] [CrossRef]
- Jung, J.H.; McCutcheon, K.A.; Borofsky, M.; Young, S.; Golzarian, J.; Reddy, B.; Shin, T.Y.; Kim, M.H.; Narayan, V.; Dahm, P. Prostatic arterial embolization for the treatment of lower urinary tract symptoms in men with benign prostatic hyperplasia. Cochrane Database Syst. Rev. 2020, 12, CD012867. [Google Scholar] [CrossRef][Green Version]
- Wang, M.Q.; Wang, Y.; Yan, J.Y.; Yuan, K.; Zhang, G.D.; Duan, F.; Li, K. Prostatic artery embolization for the treatment of symptomatic benign prostatic hyperplasia in men ≥75 years: A prospective single-center study. World J. Urol. 2016, 34, 1275–1283. [Google Scholar] [CrossRef] [PubMed]
- Shuster, A.; Gunnarsson, T.; Klurfan, P.; Larrazabal, R. N-butyl cyanoacrylate proved beneficial to avoid a nontarget embolization of the ophthalmic artery in endovascular management of epistaxis. A neurointerventional report and literature review. Interv. Neuroradiol. 2011, 17, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.J.; Barthes-Biesel, D.; Salsac, A.V. Polymerization kinetics of n-butyl cyanoacrylate glues used for vascular embolization. J. Mech. Behav. Biomed. Mater. 2017, 69, 307–317. [Google Scholar] [CrossRef]
- Li, Y.J.; Barthes-Biesel, D.; Salsac, A.V. Polymerization kinetics of a mixture of Lipiodol and Glubran 2 cyanoacrylate glue upon contact with a proteinaceous solution. J. Mech. Behav. Biomed. Mater. 2017, 74, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Loffroy, R.; Mouillot, T.; Bardou, M.; Chevallier, O. Current role of cyanoacrylate glue transcatheter embolization in the treatment of acute nonvariceal gastrointestinal bleeding. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 975–984. [Google Scholar] [CrossRef] [PubMed]
- Kurbatov, D.; Russo, G.I.; Lepetukhin, A.; Dubsky, S.; Sitkin, I.; Morgia, G.; Rozhivanov, R.; Cimino, S.; Sansalone, S. Prostatic artery embolization for prostate volume greater than 80 cm3: Results from a single-center prospective study. Urology 2014, 84, 400–404. [Google Scholar] [CrossRef]
- Loffroy, R.; Lin, M.D.; Yenokyan, G.; Rao, P.P.; Bhagat, N.; Noordhoek, N.; Radaelli, N.; Blijd, J.; Liapi, E.; Geschwind, J.F. Intraprocedural C-arm dual-phase cone-beam CT: Can it be used to predict short-term response to TACE with drug-eluting beads in patients with hepatocellular carcinoma? Radiology 2013, 266, 636–648. [Google Scholar] [CrossRef]
- Tanaka, F.; Kawai, N.; Sato, M.; Minamiguchi, H.; Nakai, M.; Nakata, K.; Sanda, H.; Sonomura, T.; Matuzaki, I.; Murata, S. Effect of transcatheter arterial embolization with a mixture of n-butyl cyanoacrylate, lipiodol, and ethanol on the vascular wall: Macroscopic and microscopic studies. Jpn. J. Radiol. 2015, 33, 404–409. [Google Scholar] [CrossRef]
- Jae, H.J.; Chung, J.W.; Kim, H.C.; So, Y.H.; Lim, H.G.; Lee, W.; Kim, B.K.; Park, J.H. Experimental study on acute ischemic small bowel changes induced by superselective embolization of superior mesenteric artery branches with N-butyl cyanoacrylate. J. Vasc. Interv. Radiol. 2008, 19, 755–763. [Google Scholar] [CrossRef]
- Wang, M.Q.; Duan, F.; Yuan, K.; Zhang, G.D.; Yan, J.; Wang, Y. Benign prostatic hyperplasia: Cone-beam CT in conjunction with DSA for identifying prostatic arterial anatomy. Radiology 2017, 282, 271–280. [Google Scholar] [CrossRef]
- Maron, S.Z.; Sher, A.; Kim, J.; Lookstein, R.A.; Rastinehad, A.R.; Fischman, A. Effect of median lobe enlargement on early prostatic artery embolization outcomes. J. Vasc. Interv. Radiol. 2020, 31, 370–377. [Google Scholar] [CrossRef]
- Stamatiou, K. The impact of prostate artery embolization (PAE) on the physical history and pathophysiology of benign prostatic hyperplasia (BPH). Arch. Ital. Urol. 2018, 90, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Loffroy, R.; Chevallier, O.; Gehin, S.; Midulla, M.; Berthod, P.E.; Galland, C.; Briche, P.; Duperron, C.; Majbri, N.; Mousson, C.; et al. Endovascular management of arterial injuries after blunt or iatrogenic renal trauma. Quant. Imaging Med. Surg. 2017, 7, 434–442. [Google Scholar] [CrossRef]
- Bardin, F.; Chevallier, O.; Bertaut, A.; Delorme, E.; Moulin, M.; Pottecher, P.; Di Marco, L.; Gehin, S.; Mourey, E.; Cormier, L.; et al. Selective arterial embolization of symptomatic and asymptomatic renal angiomyolipomas: A retrospective study of safety, outcomes and tumor size reduction. Quant. Imaging Med. Surg. 2017, 7, 8–23. [Google Scholar] [CrossRef] [PubMed]
- Cochetti, G.; Del Zingaro, M.; Boni, A.; Allegritti, M.; De Vermandois, J.A.R.; Paladini, A.; Egidi, M.G.; Poli, G.; Ursi, P.; Cirocchi, R.; et al. Renal artery embolization before radical nephrectomy for complex renal tumour: Which are the true advantages? Open Med. 2019, 14, 797–804. [Google Scholar] [CrossRef]
- Loffroy, R.; Pottecher, P.; Cherblanc, V.; Favelier, S.; Estivalet, L.; Koutlidis, N.; Moulin, M.; Cercueil, J.P.; Cormier, L.; Krausé, D. Current role of transcatheter arterial embolization for bladder and prostate hemorrhage. Diagn. Interv. Imaging 2014, 95, 1027–1034. [Google Scholar] [CrossRef]
- De Vermandois, J.A.R.; Cochetti, G.; Del Zingaro, M.; Santoro, A.; Panciarola, M.; Boni, A.; Marsico, M.; Gaudio, G.; Paladini, A.; Guiggi, P.; et al. Evaluation of surgical site infection in mini-invasive urological surgery. Open Med. 2019, 14, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Cochetti, G.; Abraha, I.; Randolph, J.; Montedori, A.; Boni, A.; Arezzo, A.; Mazza, E.; De Vermandois, J.A.R.; Cirocchi, R.; Mearini, E.; et al. Surgical wound closure by staples or sutures?: Systematic review. Medicine 2020, 99, e20573. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).