Abstract
Previous studies have indicated that influenza vaccination reduces the development of lung cancer. However, the protective effects of influenza vaccination on primary liver cancer in patients with chronic kidney disease (CKD) are unclear. This cohort study identified 12,985 patients aged at least 55 years who had received a diagnosis of CKD between 1 January 2001 and 31 December 2012 from the National Health Insurance Research Database of Taiwan. The patients were classified according to vaccination status. Propensity score matching was used to reduce selection bias. Cox proportional hazards regression analysis was used to evaluate the correlation between influenza vaccination and primary liver cancer in patients with CKD. The prevalence of primary liver cancer was lower in patients with CKD who had received an influenza vaccine (adjusted hazard ratio: 0.45, 95% confidence interval [CI]: 0.35–0.58, p < 0.001). The protective effects were observed regardless of sex, age, and comorbidities. Moreover, dose-dependent protective effects were observed. In the subgroup analysis, where the patients were classified by the number of vaccinations received, the adjusted hazard ratios for 1, 2–3, and ≥4 vaccinations were 0.86 (95% CI: 0.63–1.17), 0.45 (95% CI: 0.31–0.63), and 0.21 (95% CI: 0.14–0.33), respectively. In conclusion, influenza vaccination was associated with a lower incidence of liver cancer in patients with CKD.
1. Introduction
Chronic kidney disease (CKD) includes many disorders affecting the kidney structure and function. The prevalence and mortality rate of CKD have gradually increased in recent years [1,2]. In Taiwan, the prevalence of CKD is as high as 37.2% among older adults; therefore, it has become an important public health issue [3]. The pathophysiology of CKD is diverse. For example, diabetes may cause diabetic nephropathy due to elevated advanced glycation end products and vasoactive hormones affecting the renin-angiotensin system [4]. In addition, the other risk factors of CKD include high blood pressure, heart disease, and obesity [5]. CKD is associated with many diseases, including cardiovascular diseases and end-stage renal disease, and infection [2]. Furthermore, it has been found that CKD is significantly associated with liver cancer [6,7].
Primary liver cancer is common and is the fourth-ranked cancer-specific cause of death in the world [8,9]. In 2012, the age-standardized incidence rate in Taiwan was much higher than the global average (47.11 and 9.3 cases per 100,000 in Taiwan and worldwide, respectively) [10,11]. Several risk factors have been reported for liver cancer, including hepatitis due to viral infection, aflatoxin exposure, smoking, alcohol consumption, and obesity and diabetes-associated nonalcoholic fatty liver disease [12]. Additionally, the 5-year cumulative incidence rate of primary liver cancer was higher in patients with CKD (0.90) than in the general population (0.85) [6]. Renal dysfunction also negatively affects the prognosis of primary liver cancer [7], which may be due to the shared risk factors of chronic inflammation, compromised immune status, and high uremic concentrations [13].
Seasonal influenza is a highly contagious disease. Globally, approximately 290,000 people die from influenza each year [14,15,16]. The morbidity and mortality associated with influenza are especially high in older adults and individuals with chronic diseases [15]. For instance, the infection of influenza may trigger acute exacerbations and excess hospitalizations in the patients with chronic obstructive pulmonary disease [17]. Furthermore, a previous study found that some virus infections directly and indirectly increase the risk of cancer development, such as the human papillomavirus and hepatitis B, which may induce cervical cancer and hepatocellular carcinoma, respectively [18]. Influenza infection may also have a similar effect. Therefore, the studies investigating the association between influenza and cancer are warranted.
Previous studies have demonstrated that influenza vaccination reduces the risk of infection, hospitalization, and severe disease outcomes [19]. Furthermore, statistics also showed that vaccination reduces inflammation and oxidative stress; thereby, it decreases the risk of lung cancer in patients with different chronic diseases [20]. The pathogenesis of liver cancer is similar to that of lung cancer; however, whether influenza vaccination reduces the risk of liver cancer is unclear [13]. Therefore, this cohort study was conducted to investigate the effects of influenza vaccination on the incidence of liver cancer in patients with CKD in Taiwan using data from the National Health Insurance Research Database (NHIRD).
2. Methods
The National Health Insurance (NHI) program in Taiwan was established in 1995; it provides comprehensive healthcare coverage for more than 98% of the population [14]. In this study, we obtained the research data from the NHIRD (2001–2012). The characteristics such as age, sex, or healthcare costs were not statistically significantly different between the sample group and all the enrollees. To ensure patient privacy, all personal information from the NHIRD is delinked and deidentified; furthermore, written agreement declaring that they have no intention of obtaining information that could violate the privacy of patients or care providers must be signed by the researchers using the data. The study was approved by the Joint Institutional Review Board of Taipei Medical University (approval no. N201804043).
2.1. Patient Selection Process and the Primary Endpoint
The study cohort comprised all patients diagnosed with CKD (according to International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code 585.X) over a 12-year period (n = 32,844) from 1 January 2001 to 31 December 2012. We excluded patients without at least two outpatient department visits or at least one hospitalization in which the diagnosis was CKD in the following year (n = 9353) due to the uncertainty of their CKD diagnoses. To ensure that no patient had cancer before enrollment, we included a 1-year washout period starting on January 1, 2000. In addition, patients were excluded if they were aged less than 55 years (n = 6432) or had received an inpatient or outpatient diagnosis of cancer before the date of enrollment (n = 2780) or influenza vaccination within 6 months before the date of enrollment (n = 2097). In total, 12,985 patients were included (Figure 1). In Taiwan, the public health policy has been offering influenza vaccinations to high-risk individuals (i.e., those with chronic pulmonary diseases, cardiovascular diseases, chronic liver infection, liver cirrhosis, or type 2 diabetes mellitus) aged more than 50 years at no cost since 1998 and to all individuals aged more than 65 years since 2001 [21]. We analyzed the vaccination status by the ICD-9-CM code V048 or by the vaccine drug codes. The incidence of primary liver cancer (ICD-9-CM code 155.X) in CKD patients was indicated as the primary endpoint of our study in the follow-up years. The follow-up ended on 31 December 2012 or when the patients received a new liver cancer diagnosis, withdrew from NHI, were lost to follow-up, or died.
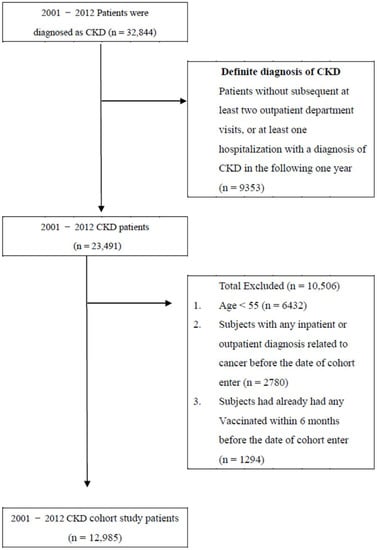
Figure 1.
Data selection Process.
2.2. Potential Confounders
The analysis of the potential confounders, such as sociodemographic characteristics (age, gender, urbanization level, and income), presence of comorbidities (Charlson comorbidity index [CCI] score, diabetes mellitus, hypertension, and dyslipidemia), and medication use (statins, metformin, renin-angiotensin-aldosterone system inhibitor [RAASI], and aspirin) was performed for each patient in this cohort.
2.3. Statistical Analysis
To estimate the effects of the vaccination and to reduce the selection bias, a propensity score matching was applied in the comparison between the vaccinated and unvaccinated groups by accounting for the covariates in a logistic regression model [22,23]. For categorical and continuous variables, we used the chi-square test and the t test, respectively. Subsequently, we calculated the hazard ratios (HRs) and 95% confidence intervals (CIs) using the Cox proportional hazards regression analysis. Furthermore, we evaluated the dose-response effect of influenza vaccination on the incidence of liver cancer. The patients with CKD were categorized into four groups according to their vaccination status: unvaccinated patients, patients with one vaccine dose, patients with two or three vaccine doses, and patients with four or more vaccine doses. We also stratified patients by age, sex, comorbidities, and medication use. Finally, we used sensitivity analysis to evaluate the differences and similarities between influenza vaccination and the risk of liver cancer in patients with CKD. All statistical analyses were performed using SPSS Statistics (version 22.0, IBM, Armonk, NY, USA) and SAS (version 9.4, SAS Institute, Cary, NC, USA). Statistical significance was indicated at a p value of <0.05.
3. Results
This cohort study included 12,985 patients. In total, 5495 (42.31%) patients had had an influenza vaccination, and 7490 (57.68%) patients had not had an influenza vaccination. Age, urbanization level, and income significantly differed between the two groups (Table 1). Additionally, the prevalence of comorbidities, including diabetes (p < 0.001), hypertension (p < 0.001), and dyslipidemia (p < 0.001), was higher among the patients without an influenza vaccine than in patients with an influenza vaccine. By contrast, the use of comorbidity-associated medications, such as statins, metformin, RAASI, and aspirin, was longer in patients with an influenza vaccine (Table 1).

Table 1.
Characteristics of the sample population.
Table 2 presents the incidence of liver cancer in patients with CKD with and without an influenza vaccination. After adjustment for potential confounders, the results revealed that the incidence of liver cancer was significantly lower in patients with an influenza vaccine than in those without an influenza vaccine (adjusted HR: 0.45, 95% CI: 0.35–0.58, p < 0.001). In our analysis, the protective effects of an influenza vaccination were observed regardless of sex or age and were predominant among patients aged 55–64 years (adjusted HR: 0.28, 95% CI: 0.17–0.46, p < 0.001) and among women (adjusted HR: 0.39, 95% CI: 0.26–0.60, p < 0.001, Table 2).

Table 2.
Risk of liver cancer among unvaccinated and vaccinated in study cohort.
In the sensitivity analysis, we conducted covariate adjustments to assess the association of influenza vaccinations with the risk of liver cancer in different models (Table 3). Furthermore, we used the number of vaccinations to stratify the vaccination groups. The protective effect was still observed in the subgroups of different covariates. In addition, the analysis revealed dose-dependent protective effects; the incidence of liver cancer was significantly lower in patients with ≥4 influenza vaccinations (adjusted HR: 0.21, 95% CI: 0.14–0.33, p < 0.001). Among the subgroups of patients with ≥4 vaccinations, the extent of the risk reduction in patients aged 55–64 years (adjusted HR: 0.07, 95% CI: 0.02–0.27, p < 0.001) was greater than that in patients aged ≥65 years. The female patients who had received ≥4 vaccinations were significantly protected (adjusted HR: 0.11, 95% CI: 0.04–0.27, p < 0.001). The patients with comorbidities were also protected, and the protective effects were notable among those with a CCI score of ≥3 (adjusted HR: 0.17, 95% CI: 0.09–0.32, p < 0.001). The patients taking medication for a shorter period were more protected than the patients taking medication for a longer period.

Table 3.
Sensitivity analysis of adjusted HRs of vaccination in risk reduction of liver cancer in whole season.
4. Discussion
4.1. Main Findings
In a previous retrospective cohort study, angiotensin-converting enzyme inhibitors were associated with lower incidence rates of liver cancer and cirrhosis in patients with CKD (CKD-weighted subdistribution HR: 0.15, 95% CI: 0.07–0.33, p < 0.001) [24]. The present population-based cohort study showed a similar association: (1) liver cancer was less prevalent among the patients with CKD who had received an influenza vaccination (vs. those who had not); (2) the lower prevalence was more pronounced in women than in men; (3) the protective effects of an influenza vaccination were positively correlated with the number of influenza vaccinations a patient had received; (4) the adjusted HR decreased predominantly in the patients with an influenza vaccination who were aged 55–64 years (vs. patients aged ≥65); and (5) the extent of the risk reduction was predominant in patients with a CCI score of ≥3.
4.2. Mechanism of Liver Cancer Development in Patients with CKD
CKD and liver cancer exhibit some common risk factors, including environmental toxins, hepatitis due to viral infection, and metabolic diseases [13]. A previous study found that liver cancer is more prevalent in patients with CKD (vs. patients without CKD); different possible mechanisms were proposed [25]. CKD is a general term for a group of diseases that affect the kidney structure and function; thus, multiple risk factors are involved. In patients with CKD, the accumulation of urea and urea-related metabolites (i.e., p-Cresyl sulfate) has been observed [26,27,28,29], and the concentrations of inflammatory cytokines (i.e., IL-1, IL-6, and TNF-α) are higher [30,31,32]. These factors may contribute to liver fibrosis and affect the immune system. Patients with a compromised immune system are more susceptible to hepatitis due to viral infection, and hepatitis may eventually lead to liver cancer development [26,27,28,29,30,31]. In addition, the gut microbiota is altered in patients with CKD. Endotoxins and other bacteria that enter the liver through the bloodstream contribute to the development of liver cancer [13,33,34].
4.3. Mechanism Underlying the Association between Incidence of Liver Cancer and Influenza Vaccination
The vaccines against human papillomavirus and hepatitis B have been demonstrated to prevent cervical cancer and liver cancer, respectively. Influenza vaccination was also related to a decline in the incidence of lung cancer in a recent study [20]. Infection with influenza leads to the activation of inflammatory cells and an increase in pro-inflammatory cytokines such as IL-1, IL-6, and TNF-α. These may affect the immune regulation of the liver. In addition, the dysregulation of pro- and anti-inflammatory cytokines can cause liver necrosis and may also activate oncogenic signaling cascades [13,35]. Moreover, influenza infection compromises the immune system by, for example, suppressing the natural killer cell, which plays an important immune role in the liver [36,37]. Additionally, influenza infection alters the gut microbiota composition, similarly to CKD [38,39]. Patients with influenza are more susceptible to microbial attacks, which can lead to the release of endotoxins and bacteria into the bloodstream and ultimately lead to liver fibrosis and hepatoma [13]. The number of times a patient is infected with influenza is positively correlated with the formation of reactive oxygen species, which are associated with cellular damage and the activation of proto-oncogenes [20,40]. Furthermore, influenza infection may decrease kidney function. Influenza infection increases the accumulation of uremic toxins and the risks of liver fibrosis and liver cancer [41]. Consequently, by reducing or preventing the risk factors associated with influenza, influenza vaccination reduces the incidence of liver cancer.
4.4. Effect of Influenza Vaccination in Patients with Different Characteristics
In this study, the protective effect of influenza vaccination was predominant in patients aged 55–64 years (vs. patients aged ≥65 years). The reason may be that the immune system declines with age, especially with regard to the activity of the thymus function. In addition, the responses of CD4+ and CD8+ T cells are reduced, and the function of antigen-presenting cells is decreased, in turn affecting the effect of the vaccine [42]. Furthermore, the protective effect of influenza vaccination was predominant in patients with a CCI score ≥3 (vs. patients with a lower score), possibly because higher CCI scores are associated with more fragile liver function. Finally, liver cancer was less prevalent in the vaccinated women than in the vaccinated men. Previous studies have found that estrogen is associated with lower concentrations of serum IL-6 [43]. As mentioned earlier, elevated IL-6 concentrations are a risk factor for liver cancer. Estrogen and influenza vaccines may have synergistic effects.
5. Limitations
This study has some limitations. First, the diagnosis of CKD was based on ICD-9-CM codes; the accuracy of the diagnoses was unclear. However, the NHI administration randomly verifies medical records, and we only selected patients with at least two outpatient visits or one hospitalization with a diagnosis of CKD in the following year. Second, the higher level of antibody production may be related to a better prevention effect of liver cancer. However, the NHIRD lacks biochemical data such as the estimated glomerular filtration rate (eGFR) and the level of antibody and demographic data such as smoking habits and alcohol consumption. Because the data of these potential confounders were not available, we used propensity score matching to reduce the bias. Third, to reduce the effects of the influenza vaccination policy in Taiwan, this study only included patients aged ≥55 years. Future studies can be designed to incorporate younger patients. Fourth, we were unable to obtain information on the type of the liver cancer. If we could classify the types of liver cancer, such as hepatocellular carcinoma or cholangiocarcinoma, we might be able to measure the effects of vaccination comprehensively. Fifth, the composition of the flu vaccine may vary from year to year. These components might also affect the protective effect of the vaccine in the study. Finally, although the results of this study were significant, this study was not a prospective randomized blinded study. Additional research is required to investigate the precise cause–effect relationship between influenza vaccination and liver cancer in patients with CKD.
6. Conclusions
This is the first population-based cohort study to investigate the effect of influenza vaccination on the incidence of liver cancer in patients with CKD. Influenza vaccination was associated with a lower incidence of liver cancer; therefore, regular and planned vaccination may be suitable for patients with CKD. Further research is warranted to explore the underlying mechanisms. In addition, the patients with liver cirrhosis are also closely related to liver cancer. More research is worthwhile to explore the effect of influenza vaccination in this population.
Author Contributions
Conceptualization, W.-R.H., C.-C.C. (Chun-Chao Chen); methodology, T.-Y.Y. and W.-R.H.; validation, K.-J.L. and C.-C.C. (Chun-Chao Chen) and C.-C.C. (Chun-Chih Chiu); formal analysis, Y.-A.F.; investigation, Y.-A.F. and W.J.; resources, J.-C.L.; data curation, M.-H.L., H.-T.Y. and M.-H.H.; writing—original draft preparation, N.-H.C., W.-R.H. and C.-C.C. (Chun-Chao Chen); writing—review and editing, W.-R.H. and C.-C.C. (Chun-Chao Chen), supervision, J.-C.L.; project administration, H.-C.J. and J.-Q.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financially supported of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan, Taipei Medical University-National Taiwan University Hospital Joint Research Program, (111-TMU085), and 111FRP-02 from the Taipei Medical University-Shuang Ho Hospital, Ministry of Health and Welfare.
Institutional Review Board Statement
The study was approved by the Joint Institutional Review Board of Taipei Medical University (approval no. N201804043).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data supporting the findings of this research were sourced from NHIRD in Taiwan. Owing to the legal restrictions imposed by the Government of Taiwan related to the Personal Information Protection Act, the database cannot be made publicly available.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Xie, Y.; Bowe, B.; Mokdad, A.H.; Xian, H.; Yan, Y.; Li, T.; Maddukuri, G.; Tsai, C.; Floyd, T.; Al-Aly, Z. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018, 94, 567–581. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Coresh, J. Chronic kidney disease. Lancet 2012, 379, 165–180. [Google Scholar] [CrossRef]
- Wen, C.P.; Cheng, T.Y.; Tsai, M.K.; Chang, Y.C.; Chan, H.T.; Tsai, S.P.; Chiang, P.H.; Hsu, C.C.; Sung, P.K.; Hsu, Y.H.; et al. All-cause mortality attributable to chronic kidney disease: A prospective cohort study based on 462 293 adults in Taiwan. Lancet 2008, 371, 2173–2182. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Cooper, M.E. Pathogenesis of diabetic nephropathy. J. Diabetes Investig. 2011, 2, 243–247. [Google Scholar] [CrossRef]
- Kazancioğlu, R. Risk factors for chronic kidney disease: An update. Kidney Int. Suppl. 2013, 3, 368–371. [Google Scholar] [CrossRef]
- Na, S.Y.; Sung, J.Y.; Chang, J.H.; Kim, S.; Lee, H.H.; Park, Y.H.; Chung, W.; Oh, K.H.; Jung, J.Y. Chronic kidney disease in cancer patients: An independent predictor of cancer-specific mortality. Am. J. Nephrol. 2011, 33, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Fabrizi, F.; Cerutti, R.; Alfieri, C.M.; Ridruejo, E. An Update on Hepatocellular Carcinoma in Chronic Kidney Disease. Cancers 2021, 13, 3617. [Google Scholar] [CrossRef]
- Lafaro, K.J.; Demirjian, A.N.; Pawlik, T.M. Epidemiology of hepatocellular carcinoma. Surg. Oncol. Clin. N. Am. 2015, 24, 1–17. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Chiang, C.-J.; Lo, W.-C.; Yang, Y.-W.; You, S.-L.; Chen, C.-J.; Lai, M.-S. Incidence and survival of adult cancer patients in Taiwan, 2002–2012. J. Formos. Med. Assoc. 2016, 115, 1076–1088. [Google Scholar] [CrossRef]
- Dasgupta, P.; Henshaw, C.; Youlden, D.R.; Clark, P.J.; Aitken, J.F.; Baade, P.D. Global Trends in Incidence Rates of Primary Adult Liver Cancers: A Systematic Review and Meta-Analysis. Front. Oncol. 2020, 10, 171. [Google Scholar] [CrossRef]
- Yang, J.D.; Hainaut, P.; Gores, G.J.; Amadou, A.; Plymoth, A.; Roberts, L.R. A global view of hepatocellular carcinoma: Trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 589–604. [Google Scholar] [CrossRef]
- Yeh, H.; Chiang, C.C.; Yen, T.H. Hepatocellular carcinoma in patients with renal dysfunction: Pathophysiology, prognosis, and treatment challenges. World J. Gastroenterol. 2021, 27, 4104–4142. [Google Scholar] [CrossRef]
- Fang, Y.A.; Chen, C.I.; Liu, J.C.; Sung, L.C. Influenza Vaccination Reduces Hospitalization for Heart Failure in Elderly Patients with Chronic Kidney Disease: A Population-Based Cohort Study. Acta Cardiol. Sin. 2016, 32, 290–298. [Google Scholar] [CrossRef]
- Smetana, J.; Chlibek, R.; Shaw, J.; Splino, M.; Prymula, R. Influenza vaccination in the elderly. Hum. Vaccines Immunother. 2018, 14, 540–549. [Google Scholar] [CrossRef]
- World Health Organization. Influenza (Seasonal). 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (accessed on 27 June 2022).
- Mallia, P.; Johnston, S.L. Influenza infection and COPD. Int. J. Chronic Obstr. Pulm. Dis. 2007, 2, 55–64. [Google Scholar] [CrossRef]
- Read, S.A.; Douglas, M.W. Virus induced inflammation and cancer development. Cancer Lett. 2014, 345, 174–181. [Google Scholar] [CrossRef]
- Rondy, M.; El Omeiri, N.; Thompson, M.G.; Levêque, A.; Moren, A.; Sullivan, S.G. Effectiveness of influenza vaccines in preventing severe influenza illness among adults: A systematic review and meta-analysis of test-negative design case-control studies. J. Infect. 2017, 75, 381–394. [Google Scholar] [CrossRef]
- Chen, C.C.; Wu, C.H.; Lin, C.H.; Chiu, C.C.; Yang, T.Y.; Lei, M.H.; Yeh, H.T.; Jian, W.; Fang, Y.A.; Hao, W.R.; et al. Influenza Vaccination and Risk of Lung Cancer in Patients with Chronic Kidney Disease: A Nationwide, Population-Based Cohort Study. Cancers 2022, 14, 2926. [Google Scholar] [CrossRef]
- 2021 Government-Funded Influenza Vaccination Program. 17 September 2021. Available online: http://at.cdc.tw/GV3J16 (accessed on 23 January 2022).
- Rosenbaum, P.R.; Rubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- D’Agostino, R.B., Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat. Med. 1998, 17, 2265–2281. [Google Scholar] [CrossRef]
- Zhang, X.; Wong, G.L.; Yip, T.C.; Tse, Y.K.; Liang, L.Y.; Hui, V.W.; Lin, H.; Li, G.L.; Lai, J.C.; Chan, H.L.; et al. Angiotensin-converting enzyme inhibitors prevent liver-related events in nonalcoholic fatty liver disease. Hepatology 2022, 76, 469–482. [Google Scholar] [CrossRef] [PubMed]
- Stengel, B. Chronic kidney disease and cancer: A troubling connection. J. Nephrol. 2010, 23, 253–262. [Google Scholar] [PubMed]
- Sun, C.-Y.; Chang, S.-C.; Wu, M.-S. Uremic Toxins Induce Kidney Fibrosis by Activating Intrarenal Renin–Angiotensin–Aldosterone System Associated Epithelial-to-Mesenchymal Transition. PLoS ONE 2012, 7, e34026. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Chen, Y.; Zhu, Z.; Su, X.; Ni, J.; Du, R.; Zhang, R.; Jin, W. p-Cresyl sulfate promotes the formation of atherosclerotic lesions and induces plaque instability by targeting vascular smooth muscle cells. Front. Med. 2016, 10, 320–329. [Google Scholar] [CrossRef]
- Nitta, T.; Kim, J.-S.; Mohuczy, D.; Behrns, K.E. Murine cirrhosis induces hepatocyte epithelial mesenchymal transition and alterations in survival signaling pathways. Hepatology 2008, 48, 909–919. [Google Scholar] [CrossRef]
- Wells, R.G. The epithelial to mesenchymal transition in liver fibrosis: Here today, gone tomorrow? Hepatology 2010, 51, 737–740. [Google Scholar] [CrossRef]
- Descamps-Latscha, B.; Herbelin, A.; Nguyen, A.T.; Roux-Lombard, P.; Zingraff, J.; Moynot, A.; Verger, C.; Dahmane, D.; de Groote, D.; Jungers, P.; et al. Balance between IL-1 beta, TNF-alpha, and their specific inhibitors in chronic renal failure and maintenance dialysis. Relationships with activation markers of T cells, B cells, and monocytes. J. Immunol. 1995, 154, 882–892. [Google Scholar]
- Rapa, S.F.; Di Iorio, B.R.; Campiglia, P.; Heidland, A.; Marzocco, S. Inflammation and Oxidative Stress in Chronic Kidney Disease—Potential Therapeutic Role of Minerals, Vitamins and Plant-Derived Metabolites. Int. J. Mol. Sci. 2019, 21, 263. [Google Scholar] [CrossRef]
- Gupta, J.; Mitra, N.; Kanetsky, P.A.; Devaney, J.; Wing, M.R.; Reilly, M.; Shah, V.O.; Balakrishnan, V.S.; Guzman, N.J.; Girndt, M.; et al. Association between albuminuria, kidney function, and inflammatory biomarker profile in CKD in CRIC. Clin. J. Am. Soc. Nephrol. 2012, 7, 1938–1946. [Google Scholar] [CrossRef]
- Zitvogel, L.; Galluzzi, L.; Viaud, S.; Vétizou, M.; Daillère, R.; Merad, M.; Kroemer, G. Cancer and the gut microbiota: An unexpected link. Sci. Transl. Med. 2015, 7, ps271. [Google Scholar] [CrossRef]
- Yamada, S.; Takashina, Y.; Watanabe, M.; Nagamine, R.; Saito, Y.; Kamada, N.; Saito, H. Bile acid metabolism regulated by the gut microbiota promotes non-alcoholic steatohepatitis-associated hepatocellular carcinoma in mice. Oncotarget 2018, 9, 9925–9939. [Google Scholar] [CrossRef]
- Chai, E.Z.; Siveen, K.S.; Shanmugam, M.K.; Arfuso, F.; Sethi, G. Analysis of the intricate relationship between chronic inflammation and cancer. Biochem. J. 2015, 468, 1–15. [Google Scholar] [CrossRef]
- Jost, S.; Quillay, H.; Reardon, J.; Peterson, E.; Simmons, R.P.; Parry, B.A.; Bryant, N.N.P.; Binder, W.D.; Altfeld, M. Changes in Cytokine Levels and NK Cell Activation Associated with Influenza. PLoS ONE 2011, 6, e25060. [Google Scholar] [CrossRef]
- Krueger, P.D.; Lassen, M.G.; Qiao, H.; Hahn, Y.S. Regulation of NK cell repertoire and function in the liver. Crit. Rev. Immunol. 2011, 31, 43–52. [Google Scholar] [CrossRef]
- Sencio, V.; Barthelemy, A.; Tavares, L.P.; Machado, M.G.; Soulard, D.; Cuinat, C.; Queiroz-Junior, C.M.; Noordine, M.L.; Salomé-Desnoulez, S.; Deryuter, L.; et al. Gut Dysbiosis during Influenza Contributes to Pulmonary Pneumococcal Superinfection through Altered Short-Chain Fatty Acid Production. Cell Rep. 2020, 30, 2934–2947.e2936. [Google Scholar] [CrossRef]
- Gu, S.; Chen, Y.; Wu, Z.; Chen, Y.; Gao, H.; Lv, L.; Guo, F.; Zhang, X.; Luo, R.; Huang, C.; et al. Alterations of the Gut Microbiota in Patients With Coronavirus Disease 2019 or H1N1 Influenza. Clin. Infect. Dis. 2020, 71, 2669–2678. [Google Scholar] [CrossRef]
- Azad, N.; Rojanasakul, Y.; Vallyathan, V. Inflammation and lung cancer: Roles of reactive oxygen/nitrogen species. J Toxicol Environ. Health B Crit. Rev. 2008, 11, 1–15. [Google Scholar] [CrossRef]
- Watanabe, T. Renal complications of seasonal and pandemic influenza A virus infections. Eur. J. Pediatr. 2013, 172, 15–22. [Google Scholar] [CrossRef]
- Pawelec, G. Age and immunity: What is “immunosenescence”? Exp. Gerontol. 2018, 105, 4–9. [Google Scholar] [CrossRef]
- Prieto, J. Inflammation, HCC and sex: IL-6 in the centre of the triangle. J. Hepatol. 2008, 48, 380–381. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).