Abstract
Treatment of neuropathic pain (NP) remains a challenge in clinical practice because the current treatment approaches produce satisfactory pain alleviation in only 30% of patients. This necessitates developing novel drugs or repurposing existing medications intended to manage other diseases. When the repurposing intendance is chosen, similarity in the pharmacological properties should be hosted by the candidate drugs. Herein, this review sheds light on the mechanisms of certain centrally acting skeletal muscle relaxants (CMRs), specifically tolperisone. So far, data indicate that tolperisone displays voltage-gated sodium channel (VGSC) blocking properties with modulatory effect on voltage-gated calcium channels (VGCCs). These properties have led to recent preclinical research initiatives testing tolperisone in NP, resulting in positive outcomes. Furthermore, the review highlights the currently available VGSC blockers and proposes a strategy based on combining them with VGCC blockers that have been proven for the treatment of NP. This proposal is supported by the fact that tolperisone, in combination with pregabalin, has recently been shown to acutely halt NP.
1. Introduction
Neuropathic pain (NP) is a complex and challenging condition and is a consequence of disease or lesion affecting the somatosensory nervous system according to International Association for the Study of Pain. Current drug discovery and repurposing strategies primarily focus on identifying compounds that interact with molecular targets that contribute to the development of NP.
Centrally acting skeletal muscle relaxants (CMRs), including baclofen, carisoprodol, cyclobenzaprine, diazepam, metaxalone, methocarbamol, orphenadrine, chlorzoxazone, tizanidine, and tolperisone, have been approved for the treatment of spastic conditions related to muscle damage and inflammation, such as acute low back pain, and some of them have shown varying levels of efficacy in reducing pain [1,2,3,4,5,6,7,8,9,10,11]. A population-based cross-sectional prevalence study was conducted in the US between 1988 and 1994 to assess CMRs’ use in the population [12]. This study reports on an estimated amount of 2 million adults using CMRs in the USA. Several studies have reported that the incidence of NP and spasticity reaches 50–60% and 70%, respectively, in patients with spinal cord injury (SCI) [13]. The current pharmacological approach for the treatment of individuals with SCI includes baclofen, tizanidine, benzodiazepines, clonidine, and gabapentinoids [14,15].
A recent study has evaluated the effectiveness of CMRs including baclofen, tizanidine, cyclobenzaprine, eperisone, quinine, carisoprodol, orphenadrine, chlormezanone, and methocarbamol in different pain types [3]. The outcome of the study indicates that baclofen, tizanidine, and cyclobenzaprine display strong evidence of effectiveness against trigeminal neuralgia (TGN), neck pain, and painful cramps [3]. On the other hand, the study has pointed out that in the context of fibromyalgia, low back pain, and other syndromes, these drugs are not more beneficial than placebo. Finally, the study has proposed that clinicians need to be attentive to potential adverse effects and should consider discontinuing medications if adequate pain management are not achieved. In this study, tolperisone was not included; it is a CMR that was first introduced by the Hungarian company Gedeon Richter Inc. in 1959. The clinical value of tolperisone as a muscle relaxant is underscored by its efficacy in treating muscle spasms while devoid of sedative effect associated with the use of other CMRs, as confirmed by numerous placebo-controlled double-blind studies [11,16,17,18]. Tolperisone thus quickly became a very popular CMR in Eastern Europe and countries of the former Soviet Union and Asia, especially in Japan.
The current treatment for the management of TGN includes first line medications such as carbamazepine and oxcarbazepine with strong recommendation; alternative or adjuvant medications include gabapentinoids, lamotrigine and baclofen with weak recommendation [19,20]. In general, in NP, the current pharmacological approaches encompass antidepressants, that modulate monoaminergic transmission, and drugs acting on ion channels as antiepileptics, including gabapentinoids, local anesthetics, capsaicin, and opioid analgesics, which point to the complex molecular background of neuropathy [21,22,23,24,25]. Carbamazepine and oxcarbazepine are considered as therapy for NP according to some studies; however, inconclusive results and patient intolerability that hinders dose escalation to achieve adequate treatment, due to a higher percentage of discontinuations resulting from various side effects, have been reported [25,26]. In fact, if we consider the mechanistic targets of the current medications used to manage NP, the gamma-aminobutyric acid B receptor (GABABR) is not included.
The above-mentioned CMRs for controlling muscle spasticity and related pain have different molecular mechanisms, but some of them, cyclobenzaprine, tizanidine, and tolperisone, share molecular mechanisms with the currently available drugs for the management of NP (Table 1). Both spasticity and NP have similarities in their molecular backgrounds regarding disinhibition caused by dysfunction of descending pathways or interneurons in the spinal cord, hyperexcitability of excitatory neurons, sprouting, upregulation of excitatory receptors, glial activation, and neuroinflammation [13,27,28]. The symptoms of neuropathy, including allodynia, hyperalgesia, and paresthesia (abnormal sensations without any stimuli, e.g., burning, tickling or tingling) [29], are not adequately controlled by the current medications [30]. For details of the most commonly used CMRs and drugs for NP, refer to Table 1.

Table 1.
Comparative data of CMRs and medications for neuropathic pain.
The focus of the present review is to discuss the pharmacodynamic properties of CMRs including cyclobenzaprine, tizanidine, and tolperisone that share targets with current NP medications, specifically affecting serotonergic and/or noradrenergic neurotransmission or inhibiting either voltage-gated sodium channels (VGSCs), voltage-gated calcium channels (VGCCs), or both. The review also pays attention to tolperisone per se or in combination with gabapentinoids in the context of NP, which, to the best of our knowledge, has not been reviewed thus far.
The outcome of this review may create a mechanistic rationale for the possible repurposing of the reviewed CMRs as therapeutic options for NP. Furthermore, this review brings overview on preclinical and clinical studies on these compounds in relation to analgesia that were conducted so far. Side effects and their mechanisms are also addressed as major limitations of CMR use or repurposing. Based on the presented literature data, we aim to propose further possible research in hope of translating them to clinical use.
2. Centrally Acting Skeletal Muscle Relaxants Sharing Molecular Targets with Current Neuropathic Pain Medications
2.1. Cyclobenzaprine
Cyclobenzaprine has long been described to have potent muscle relaxant effects following per os administration in animal models [32]. In this regard, its pharmacological effect was proposed to affect descending noradrenergic and serotonergic pathways among others in the central nervous system (CNS) [36]. Structurally, it displays a tricyclic structure closely related to that of tricyclic antidepressants (TCAs) (Figure 1). Before the discovery of selective serotonin reuptake inhibitor antidepressants, TCAs were the gold standard pharmacological treatment for depression, and they are still important drugs for the treatment of various other conditions related to chronic pain [24]. The close structural similarity between amitriptyline and cyclobenzaprine (Figure 1) has urged research groups to investigate its mechanism of action and efficacy in analgesic tests.
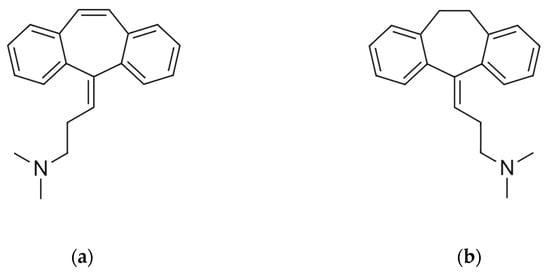
Figure 1.
The molecular structure of cyclobenzaprine (a) and amitriptyline (b). The figures were hand drawn in an art program (Clip Studio Paint), based on the 2D structure images presented on their respective PubChem pages. Cyclobenzaprine: PubChem Identifier: CID 2895, URL: https://pubchem.ncbi.nlm.nih.gov/compound/2895#section=2D-Structure (accessed on 15 December 2025). Amitriptyline: PubChem Identifier: CID 2160, URL: https://pubchem.ncbi.nlm.nih.gov/compound/2160#section=2D-Structure (accessed on 15 December 2025).
Mechanistically, cyclobenzaprine was initially reported to possess α2-adrenoceptor (AR)-mediated agonist characteristics [36,67]. Comissiong et al. also demonstrated an increase in noradrenaline metabolism in response to cyclobenzaprine treatment in the ventral horn of the spinal cord that receives dense innervation from the locus coeruleus, as opposed to no difference observed in the zona intermedia receiving no such innervation. These results indicate that cyclobenzaprine acts as an indirect inhibitor of α-motoneuron activity by increasing the noradrenergic activity in the spinal cord that originates from the locus coeruleus [68]. However, it was unclear how this increase in noradrenaline release attenuates the action of spinal motor neurons, as most studies conducted since show an α1-AR mediated facilitation of ventral horn motoneurons in response to noradrenaline [67,69]. On the other hand, it has also been shown that electrical stimulation of the locus coeruleus induces a biphasic response in the ventral horn, which consists of facilitation, followed by inhibition. The inhibition phase was naloxone-reversible, suggesting it to be an opioid-cotransmitter mediated action [70].
Later studies have underlined the principal role of the noradrenergic system in the modulation of spinal motor neuronal networks under physiological or pathophysiological conditions. In this context, α1-, α2- and β-ARs have been found to be involved in the modulation of the function of motoneurons [71]. α1-ARs have been reported to directly facilitate motoneuron excitability whereas α2-ARs decrease it [72]. In addition, after spinal nerve injury, α1-ARs become constitutively active, which contributes to motoneuronal hyperexcitability and concomitant spasms. On the other hand, activation of α2-ARs can inhibit sensory synaptic transmission to the motoneurons, thus decreasing excitatory postsynaptic potential [72]. As aforementioned, cyclobenzaprine does increase the level of noradrenaline in the spinal ventral horn through the activation of locus coeruleus neurons and by mechanisms that have not been fully elucidated. Kobayashi and colleagues have also investigated the actions of cyclobenzaprine and have reported another possible player in its mechanism of action [36]. Their study indicates that destroying noradrenergic neurons by pretreatment with 6-hydroxydopamine did not inhibit the action of cyclobenzaprine on the monosynaptic reflex; however, inducing serotonin depletion by inhibiting its synthesis with DL-p-chlorophenylalanine significantly blocked the actions of cyclobenzaprine. Furthermore, in their study, cyclobenzaprine also attenuated the action of the 5-HT2A receptor agonist, 2,5-dimethoxy-4-iodoamphetamine (DOI), belonging to psychedelic agents, which can induce both structural and functional neuroplasticity after acute administration [73]. A recent study by the Riegel research group has shown that inhibition of 5-HT2A receptor in the prefrontal cortex attenuates NP developed in rats with allodynia evoked by spared nerve injury (SNI) [74].
Taken together, results indicate that besides altering the descending noradrenergic tone in the spinal cord, cyclobenzaprine also blocks α-motorneuronal excitation by acting on descending serotonergic neurons and 5-HT2A receptor [36]. A number of 5-HT receptor subtypes are expressed on the membrane of motoneurons such as 5-HT1A, 5-HT1B, 5-HT1D, 5-HT2A, 5-HT2B, 5-HT2C, and 5-HT5A [75,76]. The activation of an individual 5-HT receptor can induce either excitation or inhibition of the motoneurons [75]. With respect to 5-HT2A receptor subtype, its activation leads to spinal motoneuron excitation [77]. Therefore, cyclobenzaprine likely blocks the effect of serotonin on motoneurons, though further studies are needed to clarify this point. Collectively, these data support that both serotonergic and noradrenergic receptors contribute to the effects of cyclobenzaprine.
Descending noradrenergic and serotoninergic pathways are important in controlling pain transmission as well. Growing data suggest the concept that chronic pain is associated with dysregulation in this pain modulatory pathway. Serotonin can produce either inhibitory or stimulatory effect, depending on the 5-HT receptor subtype undergoing activation. Thus, activation of the 5-HT1A, 5-HT1B, 5-HT1D, and 5-HT7 receptors mediates antinociception, whereas the 5-HT2A and 5-HT3 receptors can promote nociception [78,79,80]. The presence of the 5-HT2A receptor has been reported in CGRP and substance P synthesizing nociceptive neurons [81,82]. The exact role and exploitability of the 5-HT2A receptor signaling in chronic pain management models is highly controversial. With respect to NP, the picture is even more complicated with contradictory results. On one hand, 5-HT2A antagonists, ketanserin and sarpogrelate, alleviated neuropathic symptoms induced by sciatic nerve ligation (SNL) or chronic constriction injury (CCI) and, more recently, intrathecally administered α-phenyl-1-(2-phenylethyl)-4-piperidinemethanol, another 5-HT2A receptor antagonist, was shown to be effective in 2′,3′-dideoxycytidine-induced peripheral neuropathy (PN) [83,84,85]. On the other hand, evidence supports that 5-HT2A receptor activation largely participates in the alleviation of allodynia in rats [86]. Elucidating the cause of data discrepancy requires further investigation.
Cyclobenzaprine has also been reported to increase the spinal serotoninergic tone and can cause serotonin syndrome as a side effect [87,88,89]. Thus, beside the action of cyclobenzaprine on the 5HT2A receptor, it also displays serotonin enhancer effects, which might stem from the inhibition of the reuptake of serotonin [88]. Consequently, the increased serotonin level in the spinal cord could also activate 5-HT receptors that tend to inhibit pain transmission.
At clinical level, two small studies were also conducted in order to assess the efficacy of cyclobenzaprine in myofascial pain. In one study, patients receiving cyclobenzaprine reported statistically significant improvement in symptoms compared to clonazepam or placebo [90]. In the second study, cyclobenzaprine proved to have statistically equivalent efficacy with infiltered lidocaine [91]; however, the route of administration was different, and the authors suggested that the analgesic effect of infiltrated lidocaine was superior. On the other hand, oral cyclobenzaprine was more favorable in terms of patients’ comfort and compliance because of the invasiveness of lidocaine administration [92].
The above-mentioned effect of cyclobenzaprine on the spinal monoaminergic system and its structural similarity to amitriptyline could suggest exploitable analgesic properties, though no clinical studies have been carried out to evaluate the analgesic effect of cyclobenzaprine alone or in combination with analgesics following either short- or long-term treatment in NP conditions. Nevertheless, some studies proposed treatment combinations involving cyclobenzaprine and non-steroidal anti-inflammatory drugs (NSAIDs) for back pain or painful muscle spasms [5,93]. NSAIDs are well known to produce both peripheral and central analgesic effects by inhibiting the cyclooxygenase enzymes and, consequently, the prostaglandin and other inflammatory mediator synthesis that might contribute to the peripheral sensitization of nociceptors [94]. Indeed, in clinical studies cyclobenzaprine is combined with NSAIDs to achieve analgesic effect in acute back pain; however, NSAIDs are not included in the current treatment approach of NP. In addition, cyclobenzaprine is not included in the current pharmacological approach for the treatment of individuals with SCI. Thus, novel combinations of cyclobenzaprine and compounds used in neuropathic states could be worth investigating. This is because some studies suggest that using combination-based therapy may enhance analgesic efficacy and reduce side effects.
The impact of cyclobenzaprine on VGSCs was only suggested once in the context of cardiac sodium channel blockade through a case report of ventricular tachycardia and related to its unwanted effects [95]. To the best of our knowledge, there is no study focusing on the effect of cyclobenzaprine on neuronal sodium channels, which are potential targets for the treatment of chronic pain conditions. A recent comprehensive pharmacovigilance analysis has revealed that adverse events associated with cyclobenzaprine may pose potential risks, including toxicity and suicidal behavior [96]. Further evidence of important, rare but serious adverse effects of cyclobenzaprine, including serotonin syndrome (particularly when used in combination with other serotoninergic agents) or prolongation of conduction time, arrhythmias, and tachycardia, similarly to TCAs, has also been reported [33,35,89].
2.2. Tizanidine
Tizanidine was first described in 1980 [37,38], and is a potent central α2-AR agonist with muscle relaxant properties. Structurally, tizanidine is related to clonidine, yet its antispastic efficacy is similar to that produced by baclofen while having a more favorable side effect profile [41]. In the context of analgesia, several preclinical and clinical studies have shown that tizanidine produces significant antinociceptive, anti-thermal hyperalgesic and antiallodynic effects that are mediated by α2-ARs [39,97,98,99,100,101,102]. An early autoradiographic localization study, along with others, found high densities of α2-ARs in the substantia gelatinosa of the spinal cord, the spinal trigeminal nucleus, and the locus coeruleus, indicating the involvement of α2-ARs in pain regulation [103,104]. There is also evidence on α2-ARs mediating analgesia and sedation at different sites in the CNS. Buerkle et al. found that activating spinal α2-ARs mainly causes analgesia with limited sedation, while activating α2-ARs in the brain induces strong sedation with little antinociceptive action [105]. α2-ARs can be categorized as α2A-AR, α2B-AR, and α2C-AR [106,107,108] and their effects can be selectively antagonized by BRL-44408, imiloxan, and JP-1302, respectively [109,110,111]. Several studies have been carried out with the aim of elucidating the neuroanatomical distribution of α2-ARs. An in situ hybridization study by Nicholas et al. found the mRNA of the α2A-AR subtype to be most prevalent in the locus coeruleus, ventrolateral medullary reticular formation, and the intermediolateral cell column of the thoracic spinal cord, among others. On the other hand, high levels of the α2C-AR subtype mRNA were found in the DRG [112]. Several studies have demonstrated the contribution of different α2-AR subtypes to the development of NP and its attenuation by α2-agonists [113,114]. Evidence suggests that α2-ARs play a critical role in modulating pain perception. α2-ARs activation leads to significant changes in synaptic transmission within the dorsal part of the spinal cord. Notably, this activation results in the inhibition of VGCCs and the activation of potassium channels at presynaptic and postsynaptic membranes, respectively [113]. Studies have also pointed to α2A-AR subtype contribution to the antiallodynic action of α2-AR agonists [115,116,117]. Furthermore, a study by Pei and coworkers demonstrated that intrathecal tizanidine can produce analgesic effects against mechanical and thermal hyperalgesia in neuropathic rats, which is reversible by α2A-AR antagonist, BRL-44408 [98]. These results support the contribution of α2A-AR subtype to the analgesic effect of tizanidine. All types of α2-ARs are classified within the G-protein coupled receptor (GPCR) family, and primarily coupling to the Gi/Go subfamilies [118,119].
With respect to VGSCs (Nav), studies have shown the ability of α-AR agonists such as dexmedetomidine to inhibit Nav 1.7 and Nav1.8 through the activation of Gi/o α2-ARs on the primary sensory neurons of the trigeminal ganglia [120]. Tizanidine, at supraclinical concentrations, was found to affect the cardiac rapid delayed rectifier potassium current (IKr) associated with human ether-a-go-go-related gene (HERG) channels, leading to a lengthening of the action potential duration as measured by monophasic action potential duration at 90% repolarization (MAPD90), accompanied by QTc prolongation [121]. To the best of our knowledge, there are no details regarding the direct impact of tizanidine on VGSCs. It would be of interest to investigate tizanidine in combination with blockers of VGSCs, specifically those that inhibit subtypes of channels distributed in peripheral sensory neurons.
Finally, tizanidine is included in the current SCI treatment approach; however, future studies are needed to develop further α2-AR subtypes-selective agonists, which might have different pharmacological properties related to spasticity, pain, or common adverse effects such as xerostomia and drowsiness, among others [41]. In the future, examining the combination of tizanidine with VGSC or VGCC blockers, such as tolperisone or peripheral acting new Nav 1.7, 1.8 inhibitors (see below) might show therapeutic value in NP. VGSC blockers that are devoid of sedative effect might positively or neutrally affect the side effects of tizanidine, improving side effect profile while increasing the antiallodynic effect of each other in subjects with NP.
2.3. Tolperisone
In this section, we aim to overview the proposed mechanism of tolperisone in relation to muscle-associated pain in both clinical and preclinical scenarios, emphasizing its current and future implications for NP. As mentioned in the introduction, tolperisone is a CMR and is devoid of the sedative effect, as described in several preclinical and clinical studies, in relation to pain associated with musculoskeletal disorders [16,122].
Structurally, tolperisone shows similarity to lidocaine, sharing the typical moieties necessary to the effect of local anesthetics; the lipophilic aromatic ring and the basic amine group tethered by a short linkage (Figure 2) [123]. Their chemical similarity raises the possibility of the interaction of tolperisone with VGSCs. In addition, based on the chemical structure, Ono and coworkers have attributed its measured muscle relaxant activity to sodium channels located on the axonal membranes similarly to local anesthetics [42]. In this context, Hinck and Koppenhöfer reported that tolperisone caused a significant depressive effect on the voltage-gated sodium currents, while only mildly affecting the potassium permeability, resulting in a slight increase in potassium currents at weak depolarization and a slight decrease at higher depolarization in Ranvier nodes of the sciatic nerve of Xenopus frogs [45]. In other research strategies that focus on the impact of tolperisone on calcium currents, Novales-Li and his coworkers, utilizing voltage clamping, have found that tolperisone does suppress calcium currents in a dose-dependent manner and shifted the steady state inactivation curves towards the hyperpolarizing direction [43]. In these experiments, tolperisone analogs eperisone and isoperisone showed a significantly more potent action (lower IC50 value) than tolperisone on calcium currents.
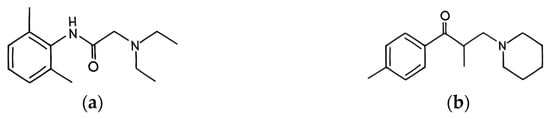
Figure 2.
The molecular structure of lidocaine (a) and tolperisone (b). The figures were hand drawn in an art program (Clip Studio Paint), based on the 2D structure images presented on their respective PubChem pages. Lidocaine: PubChem Identifier: CID 3676, URL: https://puchem.ncbi.nlm.nih.gov/compound/3676#section=2D-Structure (accessed on 15 December 2025). Tolperisone: PubChem Identifier: CID 5511, URL: https://pubchem.ncbi.nlm.nih.gov/compound/5511#section=2D-Structure (accessed on 15 December 2025).
The discovery and characterization of VGSCs, specifically Nav1 (Nav1.1–Nav1.9), have opened a new area of target research related to drugs acting on sodium channels [124,125]. Nav 1 subtype channels involved in pain are summarized in Table 2. In this regard, Hofer et al. used the two-electrode voltage clamp technique to record sodium currents corresponding to different isoforms of VGSC (Nav1.2–Nav1.8) expressed in the Xenopus laevis oocyte expression system [61]. In this study, the effects of tolperisone and lidocaine were also examined. Tolperisone was found significantly more potent than lidocaine in the inhibition of sodium channel isoforms Nav1.6, Na v1.7, and Na v1.8. Their results also indicated that the extent of tonic block induced by tolperisone was significantly stronger on the isoforms Nav1.2, Nav1.3, Nav1.7, and Nav1.8 compared to lidocaine [61]. As VGSCs are recognized to have a critical role in the pathophysiology and development of neuronal hyperexcitability following peripheral nerve injury, drugs that are able to exert a high level of tonic blockade on these channels might be useful in specific clinical scenarios, for example, in chronic pain treatment [126]. Nav1.7 is expressed in DRG neurons; however, Nav1.8 exhibits selective expression within these neurons. Nav1.3, which is upregulated in DRG neurons after injury, has garnered attention from researchers and is considered a promising target for pharmacological treatment of NP [127]. Suzetrigine, the recently introduced VGSC blocking agent for clinical use, is the first oral, nonopioid small molecule with peripheral analgesic action for acute pain and demonstrates selectivity for Nav1.8 [128]. Other selective inhibitors of Nav1.7, such as aneratrigine, have been recently developed as an alternative drug of opioid analgesics [129].

Table 2.
Nav1 subtypes and their ligands with analgesic effect.
The principal function of Nav1.7 and Nav1.8 in both the generation and maintenance of abnormal neuronal hyperexcitability of sensory neurons underscores the significance of these channels in the progression of pathological pain, including NP.
Owing to tolperisone’s molecular mechanisms, particularly the inhibition of both voltage-gated sodium and calcium channels, it is predicted that it may serve as a promising agent for reducing NP. Both sodium and calcium channels are crucial in transmitting pain signals within the CNS. Recent studies have highlighted that tolperisone’s ability to modulate these channels may effectively attenuate NP in rodents. In this regard, in a study conducted by Lakatos et al., oral tolperisone has shown acute antiallodynic effects in a rat model of NP, specifically examining mechanical allodynia (mechanical pressure stimulation) of rats with experiencing mononeuropathic pain induced by partial sciatic nerve ligation [141]. Besides suppressing mechanical allodynia, tolperisone has also been demonstrated to effectively attenuate tactile allodynia in the same model of NP [142]. In this context, Essmat et al. have shown that tolperisone can only exhibit antiallodynic effects against tactile allodynia following chronic treatment. These studies collectively underscore that tolperisone has therapeutic potential in mitigating symptoms associated with NP at a preclinical scenario.
VGCC (Cav) types, in particular, ones hosting α2δ1 subunit are hitherto described as the molecular target of gabapentin and pregabalin, which are first-line medications in the treatment of NP [52,143] (Table 1). The current drugs with calcium channel modulatory action that have been validated as effective against NP in both preclinical and clinical settings selectively bind to the α2δ-1 and α2δ-2 subunit containing VGCCs. The α2δ subunits play a crucial role in the functional assembly of VGCCs, specifically Cav2.1 and Cav2.2, which are distributed at key relay points within the pain pathways (see Table 3).
Despite the effectiveness of VGCC modulators like gabapentinoids in the management of NP, the slow onset of action has been described previously [144]. To this end, the combination-based therapies including VGSC and VGCC blockers’ combination to combat pain have been recognized as a promising strategy. In this context, a study by Hahm has shown that carbamazepine and pregabalin combination ameliorates NP of rats [145]. In a different study, the combination of carbamazepine and gabapentin resulted in better pain management for patients suffering from TGN compared to the administration of carbamazepine per se [146]. This strategy was followed by a study carried out in our previous work regarding the enhancement of tolperisone’s efficacy in NP [142]. In this regard, when tolperisone and pregabalin were administered simultaneously, a significant acute antitactile allodynic effect with fast onset was observed, reinforcing the effectiveness of combination of VGSC and VGCC blockers in managing NP [142]. The aspect of the present combination avoids concerns that have been raised regarding the combination of drugs with similar mechanisms of action, specifically the combination of TCAs with medications that positively influence serotonin levels. To the best of our knowledge, this concern is of lesser relevance in VGSC and VGCC combination, but to rule this issue out, future studies are required.

Table 3.
The distribution of VGCC hosting α2δ1 subunit in pain pathway.
Table 3.
The distribution of VGCC hosting α2δ1 subunit in pain pathway.
| Type | Channel | Voltage Activation | Peripheral Primary Afferents/Dorsal Root Ganglia | Spinal Dorsal Horn | Thalamus | Somatosensory Cortex | References |
|---|---|---|---|---|---|---|---|
| L | Cav1.1 | HVA | No | No | No | No | [147,148,149,150,151,152,153,154,155,156,157,158,159] |
| Cav1.2 | HVA | Yes (Low) | Yes | Yes | Yes | ||
| Cav1.3 | HVA | No | Yes | Yes | Yes | ||
| Cav1.4 | HVA | No | No | No | No | ||
| P/Q | Cav2.1 | HVA | Yes | Yes * | Yes | Not enough data | [157,158,159] |
| N | Cav2.2 | HVA | Yes | Yes | No | No | [159,160,161,162,163] |
| R | Cav2.3 | HVA | Yes | Yes | Yes | Yes (debated) | [164,165,166,167,168,169,170,171,172,173,174] |
| T | Cav3.1 | LVA | No | Yes | Yes | Yes | [175,176,177] |
| Cav3.2 | LVA | Yes | Yes | No | Yes | ||
| Cav3.3 | LVA | No | Yes (Low) | Yes | Yes |
*: Presynaptic distribution; HVA: High voltage activated; LVA: Low voltage activated.
The efficacy and safety of tolperisone have been evaluated earlier. A clinical study conducted in 2012 evaluated the efficacy of tolperisone in comparison with thiocolchicoside for alleviating acute low back pain. The study has demonstrated that tolperisone effectively reduced pain while offering a favorable safety profile, distinguishing it from other treatments [8]. In 1996, Pratzel et al. conducted a study to evaluate the effectiveness of tolperisone for treating patients with painful reflex muscle spasms, primarily associated with musculoskeletal conditions such as spondylarthrosis and intervertebral disc prolapse. Participants were randomly assigned to receive either 300 mg of tolperisone or a placebo daily for 21 days. The outcome of the study revealed that tolperisone significantly exceeded the placebo in alleviating muscle spasms [18]. Tolperisone also showed negligible adverse effects related to attention and cognitive brain functions, which make it preferable for stroke-affected elderly patients [17]. Thus, in a multicenter randomized double-blind placebo-controlled clinical study by Stamenova et al., the efficacy and safety of tolperisone were assessed in the treatment of muscle spasticity following cerebral stroke [16]. One hundred and twenty patients suffering from stroke-related spasticity (with a degree of spasticity being 2 or higher on the Ashworth Scale) were selected and randomized to either receive tolperisone or placebo for a total treatment time of 12 weeks. The primary endpoint of the study was muscle tone, where tolperisone proved to be significantly superior when compared to placebo in attenuating post-stroke spasticity. Interestingly adverse effects occurred less often in the tolperisone group than in the placebo group and caused no need to discontinue the therapy, further proving the preferable tolerability profile of tolperisone [16]. Because of the chiral center next to the carbonyl group in the molecular structure of tolperisone (Figure 2), stereoisomers exist. For medication purposes the racemic mixture is generally used. D-tolperisone is responsible for central skeletal muscle relaxation, while implications were raised about L-tolperisone inducing vasodilation and bronchodilation [178,179]. Fels performed a comparison of tolperisone’s structure to the biologically active conformations of lidocaine and other local anesthetics [178]. The study concluded that, because of the distance and orientation of presumed protein binding structural elements and the similar electrostatic potential pattern, tolperisone, lidocaine, and other local anesthetics could share a protein surface and binding site that can bind all ligands. It is important to also note that, while these drugs may share binding sites because of a similar conformation, the local anesthetics, but not tolperisone, can be superimposed with other, slightly different orientations; therefore, they may reach other binding sites that are unavailable to tolperisone. This could explain the lack of antiarrhythmic potential of the latter compound.
As a summary, tolperisone acts as a multi-target drug; however, its multiple molecular targets call attention to the clinical value of tolperisone in the treatment of NP. Indeed, further studies are needed to elucidate the effect of tolperisone on different chronic pain conditions of different pathological entities and to extend it to human subjects.
3. Current Knowledge on the Efficacy of CMRs in Neuropathic Pain Management
The existing literature indicates that the efficacy of CMRs in the management of NP is a subject of ongoing research. Although CMRs show promising results for several painful neuropathic conditions, there is also a significant amount of negative findings and low-quality evidence in the literature. Notably, despite the fact that a large number of painful musculoskeletal and CNS disorders are associated with muscle spasms, the efficacy of CMRs as a class is controversial. While there is evidence that, in certain conditions, the potential benefits of these agents outweigh the risks, it is important to pinpoint these conditions, as their use is limited by the almost universal side effect of sedation or, in some cases, the potential for abuse, such as in case of carisoprodol [31,180,181,182]. As an example, the European Medicines Agency (EMA) conducted a review of the safety and efficacy of tolperisone and decided to restrict its use to the treatment of post-stroke spasticity, due to insufficient evidence that its benefits outweigh the risks in treating other painful spasticities (https://www.ema.europa.eu/en/medicines/human/referrals/tolperisone accessed on 15 December 2025).
While baclofen does show promise in the treatment of TGN [51], a small clinical study published in 1985 did not demonstrate analgesic efficacy in postherpetic neuralgia (PHN) or painful diabetic neuropathy [183]. Notably, within the same cohort, the authors reported a more favorable response among patients with facial PHN, suggesting possible phenotype- or localization-dependent effects [183]. In chemotherapy-induced PN, topical treatment with an organogel containing baclofen, amitriptyline, and ketamine also failed to meet the primary endpoint of the study for symptom improvement [184].
Evidence supporting tizanidine for NP remains inconclusive, largely because adequately powered, placebo-controlled trials are scarce. Its effectiveness has been shown in clinical trials; however, these often represent low-quality studies without a placebo comparator [102].
To the best of our knowledge, despite encouraging preclinical findings, tolperisone has not been evaluated in randomized clinical trials targeting classic NP indications. Similarly, while cyclobenzaprine has demonstrated benefit over placebo in fibromyalgia, placebo-controlled trials in established NP syndromes are missing.
Taken together, the analgesic value of CMRs remains uncertain, both in NP and across their traditional spasm-related applications, where risk–benefit concerns have recently emerged. For repurposing them for NP indications, high-quality clinical trials would be necessary to better characterize their risk–benefit ratio and provide solid evidence for their clinical use. The currently available low-quality evidence also highlight a persistent gap in translation between mechanistic rationale, preclinical efficacy, and clinical outcomes.
Significant efforts have been made at both preclinical and clinical levels to enhance the therapeutic effects while simultaneously reducing adverse effects, including strategies based on combination drugs that target different molecular pathways [185]. This approach has shown promise in managing NP, particularly with the combination of VGSC and VGCC blockers, which has demonstrated efficacy in reducing the NP of rats [142]. Other earlier preclinical studies also supported this combination-based therapy. As mentioned in the former section, higher doses of the pregabalin/carbamazepine combination produced a synergistic antiallodynic effect in the NP model in rats; however, the side effects were not evaluated [145]. In addition, Essmat et al. in 2023 showed that combining tolperisone with pregabalin at low doses provided acute antiallodynic effect in rats with mononeuropathic pain. Also, the combination is devoid of adverse effects related to motor coordination or delay in the gastrointestinal transit of rats [142]. However, these studies lack data regarding pharmacokinetic interactions between the studied drugs. The use of cyclobenzaprine in combination with other medications to manage NP, particularly those that target ion channels, is limited. Although cyclobenzaprine per se or in combination, specifically with drugs for treating NP, is not well-established in the existing literature, further evaluation is necessary regarding its pharmacodynamic and pharmacokinetic interactions with current medications for NP.
Analgesic effect and NP mechanisms are known to be sex-dependent. It is impossible to rule out any sex-related variations in efficacy because most of the preclinical studies assessing CMRs have been carried out in male animals. With respect to tolperisone, two preclinical studies conducted by our research group evaluated its antiallodynic effects in rat models of NP [141,142]. However, these studies have not investigated potential sex differences in the antiallodynic efficacy of tolperisone. Therefore, potential sex-dependent differences in tolperisone efficacy remain unknown. In relation to tizanidine, a study carried out by Rodríguez-Palma et al. 2022 in discussed the sex-specific antiallodynic effects of tizanidine in experimental NP in rats [186]. The authors have shown that increasing doses of tizanidine produced a dose-dependent antiallodynic effect in neuropathic rats and the analgesic efficacy was greater in female than in male animals [186]. The authors have also highlighted the contribution of estradiol to the enhanced antiallodynic effect of tizanidine in female rats. Studies of NP should consider the underlying subject-specific mechanisms, sex, genotype, and other variables such as Nav subtype expression, sensory phenotype among others [125,187,188,189,190,191]. Only with these considerations can we hope to develop safe and effective treatments for NP.
4. Future Perspectives and Conclusions
In fact, to date, in various populations with neuropathic conditions, a single drug therapy from currently available medications is often inappropriate in NP as indicated by the high number of patients needed to treat. VGSC blockers, specifically those block Nav subtypes participating in pain modulation, are of future interest. Carbamazepine is a VGSC inhibitor, is one of the first line medications for managing TGN and also presented in the drug list composing lines of medication for the treatment of NP, however its pharmacokinetics interactions and side effect limit its use. This enforces researchers to find selective Nav subtype inhibitors or repurposing drugs acting on these channels. The gathered data support the effectiveness of selective Nav inhibitors in NP. Combining two or more drugs with different mechanisms of action has gained increasing attention in NP management and is applied in the current treatment approaches. CMRs have various chemical structures that are reflected by their multiple mechanisms of action, yet further mechanisms and effects still need to be clarified. Among the elucidated mechanisms, some are also attributed to agents currently used to treat NP including VGSC, VGCC, and spinal serotonin or noradrenergic system modulation. Despite similar pharmacological properties, at the clinical setting, the analgesic effect of CMRs is not utilized yet in NP. The use of preclinical models with high translational relevance (e.g., non-human primates) alongside the rodent pain models may provide a critical step towards clinical feasibility in the future. Based on preclinical results, a combination of CMRs with multiple modes of action related to the alleviation of neuropathic symptoms might offer great promise in overcoming the drawbacks of current treatment approaches. Nevertheless, decreasing muscle spasticity together with the inhibition of pain sensation by combining certain CMRs with drugs belonging to the available treatments for NP might be needed to achieve effective management. In this scenario, the combination of tolperisone with pregabalin can open a future avenue for research NP.
As a limitation of this review, the development of tolerance, receptor desensitization, or channel upregulation may limit the long-term utility of CMRs in the management of NP.
Author Contributions
Conceptualization, D.A.K., T.T. and M.A.-K.; data curation, J.M.K.-F.; writing—original draft preparation, D.A.K., J.M.K.-F., I.B.J., N.E. and S.K.A.; writing—review and editing, J.M.K.-F., K.K., A.R.G., N.E., T.T., Z.P.L., É.S. and M.A.-K.; visualization, J.M.K.-F. and D.A.K.; supervision, T.T. and M.A.-K.; project administration, T.T., É.S. and M.A.-K. All authors have read and agreed to the published version of the manuscript.
Funding
This work has been supported by the Higher Education Institutional Excellence Programme of the Ministry of Human Capacities in Hungary, within the framework of the Neurology Thematic Programme of Semmelweis University (TKP 2021 EGA-25) and the “Competitiveness and Excellence Cooperations” project (2018-1.3.1-VKE-2018-00030) provided by the National Research, Development, and Innovation Fund of Hungary, Hungary.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AR | Adrenoceptor |
| CCI | Chronic constriction injury |
| CINP | Chemotherapy-induced neuropathic pain |
| CMR | Centrally acting skeletal muscle relaxant |
| CNS | Central nervous system |
| DRG | Dorsal root ganglion |
| ECG | Electrocardiogram |
| GABABR | gamma-aminobutyric acid B receptor |
| GPCR | G-protein coupled receptor |
| HERG | Human ether-a-go-go-related gene |
| h | Hour |
| HVA | High-voltage-activated |
| IC50 | Half-maximal inhibitory concentration |
| IKr | Rapid delayed rectifier potassium current |
| Ip. | Intraperitoneal |
| Iv. | Intravenous |
| LVA | Low-voltage-activated |
| MAPD90 | Monophasic action potential duration at 90% repolarization |
| NMDAR | N-methyl-D-aspartate-receptor |
| NP | Neuropathic pain |
| NSAID | Non-steroidal anti-inflammatory drug |
| PHN | postherpetic neuralgia |
| PN | Peripheral neuropathy |
| Po. | Per os |
| SCI | Spinal cord injury |
| SNI | Spared nerve injury |
| SNL | Spinal nerve ligation |
| TCA | Tricyclic antidepressant |
| TGN | Trigeminal neuralgia |
| TRPV1 | Transient Receptor Potential Vanilloid 1 |
| TTX-R | Tetrodotoxin-resistant |
| TTX-S | Tetrodotoxin-sensitive |
| VGCC | Voltage-gated calcium channel |
| VGSC | Voltage-gated sodium channel |
| WDR | Wide dynamic range |
References
- Witenko, C.; Moorman-Li, R.; Motycka, C.; Duane, K.; Hincapie-Castillo, J.; Leonard, P.; Valaer, C. Considerations for the Appropriate Use of Skeletal Muscle Relaxants for the Management of Acute Low Back Pain. Pharm. Ther. 2014, 39, 427. [Google Scholar]
- Zhu, L.L.; Wang, Y.H.; Zhou, Q. Tizanidine: Advances in Pharmacology & Therapeutics and Drug Formulations. J. Pain Res. 2024, 17, 1257–1271. [Google Scholar] [CrossRef]
- Oldfield, B.J.; Gleeson, B.; Morford, K.L.; Adams, Z.; Funaro, M.C.; Becker, W.C.; Merlin, J.S. Long-Term Use of Muscle Relaxant Medications for Chronic Pain: A Systematic Review. JAMA Netw. Open 2024, 7, e2434835. [Google Scholar] [CrossRef]
- Nielsen, R.V.; Fomsgaard, J.S.; Siegel, H.; Martusevicius, R.; Mathiesen, O.; Dahl, J.B. The Effect of Chlorzoxazone on Acute Pain after Spine Surgery. A Randomized, Blinded Trial. Acta Anaesthesiol. Scand. 2016, 60, 1152–1160. [Google Scholar] [CrossRef]
- Borenstein, D.G.; Lacks, S.; Wiesel, S.W. Cyclobenzaprine and Naproxen versus Naproxen Alone in the Treatment of Acute Low Back Pain and Muscle Spasm. Clin. Ther. 1990, 12, 125–131. [Google Scholar]
- Tüzün, F.; Ünalan, H.; Öner, N.; Özgüzel, H.; Kirazli, Y.; Içaǧasioǧlu, A.; Kuran, B.; Tüzün, Ş.; Başar, G. Multicenter, Randomized, Double-Blinded, Placebo-Controlled Trial of Thiocolchicoside in Acute Low Back Pain. Jt. Bone Spine 2003, 70, 356–361. [Google Scholar] [CrossRef]
- Pillastrini, P.; Gardenghi, I.; Bonetti, F.; Capra, F.; Guccione, A.; Mugnai, R.; Violante, F.S. An Updated Overview of Clinical Guidelines for Chronic Low Back Pain Management in Primary Care. Jt. Bone Spine 2012, 79, 176–185. [Google Scholar] [CrossRef]
- Rao, R.; Panghate, A.; Chandanwale, A.; Sardar, I.; Ghosh, M.; Roy, M.; Banerjee, B.; Goswami, A.; Kotwal, P.P. Clinical Comparative Study: Efficacy and Tolerability of Tolperisone and Thiocolchicoside in Acute Low Back Pain and Spinal Muscle Spasticity. Asian Spine J. 2012, 6, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Soonawalla, D.F.; Joshi, N. Efficacy of Thiocolchicoside in Indian Patients Suffering from Low Back Pain Associated with Muscle Spasm. J. Indian Med. Assoc. 2008, 106, 331–335. [Google Scholar] [PubMed]
- Hoiriis, K.T.; Pfleger, B.; McDuffie, F.C.; Cotsonis, G.; Elsangak, O.; Hinson, R.; Verzosa, G.T. A Randomized Clinical Trial Comparing Chiropractic Adjustments to Muscle Relaxants for Subacute Low Back Pain. J. Manip. Physiol. Ther. 2004, 27, 388–398. [Google Scholar] [CrossRef] [PubMed]
- Quasthoff, S.; Möckel, C.; Zieglgänsberger, W.; Schreibmayer, W. Tolperisone: A Typical Representative of a Class of Centrally Acting Muscle Relaxants with Less Sedative Side Effects. CNS Neurosci. Ther. 2008, 14, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Dillon, C.; Paulose-Ram, R.; Hirsch, R.; Gu, Q. Skeletal Muscle Relaxant Use in the United States: Data from the Third National Health and Nutrition Examination Survey (NHANES III). Spine 2004, 29, 892–896. [Google Scholar] [CrossRef]
- Finnerup, N.B. Neuropathic Pain and Spasticity: Intricate Consequences of Spinal Cord Injury. Spinal Cord 2017, 55, 1046–1050. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.M.; Ma, C.L.; Xu, J.; He, J.P. Reduction in Post-Spinal Cord Injury Spasticity by Combination of Peripheral Nerve Grafting and Acidic Fibroblast Growth Factor Infusion in Monkeys. J. Int. Med. Res. 2021, 49, 03000605211022294. [Google Scholar] [CrossRef]
- Cabahug, P.; Pickard, C.; Edmiston, T.; Lieberman, J.A. A Primary Care Provider’s Guide to Spasticity Management in Spinal Cord Injury. Top. Spinal Cord Inj. Rehabil. 2020, 26, 157–165. [Google Scholar] [CrossRef]
- Stamenova, P.; Koytchev, R.; Kuhn, K.; Hansen, C.; Horvath, F.; Ramm, S.; Pongratz, D. A Randomized, Double-Blind, Placebo-Controlled Study of the Efficacy and Safety of Tolperisone in Spasticity Following Cerebral Stroke. Eur. J. Neurol. 2005, 12, 453–461. [Google Scholar] [CrossRef]
- Dulin, J.; Kovacs, L.; Ramm, S.; Horvath, F.; Ebeling, L.; Kohnen, R. Evaluation of Sedative Effects of Single and Repeated Doses of 50 Mg and 150 Mg Tolperisone Hydrochloride. Results of a Prospective, Randomized, Double-Blind, Placebo-Controlled Trial. Pharmacopsychiatry 1998, 31, 137–142. [Google Scholar] [CrossRef]
- Pratzel, H.G.; Alken, R.G.; Ramm, S. Efficacy and Tolerance of Repeated Oral Doses of Tolperisone Hydrochloride in the Treatment of Painful Reflex Muscle Spasm: Results of a Prospective Placebo-Controlled Double-Blind Trial. Pain 1996, 67, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Chong, M.S.; Bahra, A.; Zakrzewska, J.M. Guidelines for the Management of Trigeminal Neuralgia. Clevel. Clin. J. Med. 2023, 90, 355–362. [Google Scholar] [CrossRef]
- Zhao, X.; Ge, S. The Efficacy and Safety of Gabapentin vs. Carbamazepine in Patients with Primary Trigeminal Neuralgia: A Systematic Review and Meta-Analysis. Front. Neurol. 2023, 14, 1045640. [Google Scholar] [CrossRef]
- Nickel, F.T.; Seifert, F.; Lanz, S.; Maihöfner, C. Mechanisms of Neuropathic Pain. Eur. Neuropsychopharmacol. 2012, 22, 81–91. [Google Scholar] [CrossRef]
- Zeng, L.; Alongkronrusmee, D.; van Rijn, R.M. An Integrated Perspective on Diabetic, Alcoholic, and Drug-Induced Neuropathy, Etiology, and Treatment in the US. J. Pain Res. 2017, 10, 219–228. [Google Scholar] [CrossRef]
- Mendlik, M.T.; Uritsky, T.J. Treatment of Neuropathic Pain. Curr. Treat. Options Neurol. 2015, 17, 50. [Google Scholar] [CrossRef]
- Al-Khrasani, M.; Mohammadzadeh, A.; Balogh, M.; Király, K.; Barsi, S.; Hajnal, B.; Köles, L.; Zádori, Z.S.; Harsing, L.G., Jr. Glycine Transporter Inhibitors: A New Avenue for Managing Neuropathic Pain. Brain Res. Bull. 2019, 152, 143–158. [Google Scholar] [CrossRef]
- Finnerup, N.B.; Attal, N.; Haroutounian, S.; McNicol, E.; Baron, R.; Dworkin, R.H.; Gilron, I.; Haanpää, M.; Hansson, P.; Jensen, T.S.; et al. Pharmacotherapy for Neuropathic Pain in Adults: A Systematic Review and Meta-Analysis. Lancet Neurol. 2015, 14, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, G.; La Cesa, S.; Truini, A.; Cruccu, G. Natural History and Outcome of 200 Outpatients with Classical Trigeminal Neuralgia Treated with Carbamazepine or Oxcarbazepine in a Tertiary Centre for Neuropathic Pain. J. Headache Pain 2014, 15, 34. [Google Scholar] [CrossRef] [PubMed]
- Zavvarian, M.M.; Hong, J.; Fehlings, M.G. The Functional Role of Spinal Interneurons Following Traumatic Spinal Cord Injury. Front. Cell. Neurosci. 2020, 14, 127. [Google Scholar] [CrossRef] [PubMed]
- Kopach, O.; Medvediev, V.; Krotov, V.; Borisyuk, A.; Tsymbaliuk, V.; Voitenko, N. Opposite, Bidirectional Shifts in Excitation and Inhibition in Specific Types of Dorsal Horn Interneurons Are Associated with Spasticity and Pain Post-SCI. Sci. Rep. 2017, 7, 5884. [Google Scholar] [CrossRef]
- Woolf, C.J.; Mannion, R.J. Neuropathic Pain: Aetiology, Symptoms, Mechanisms, and Management. Lancet 1999, 353, 1959–1964. [Google Scholar] [CrossRef]
- Al-Khrasani, M.; Essmat, N.; Boldizsár, I.; Varga, B.T.; Chalabiani, Y.; Abbood, S.K.; Ernyey, A.J.; Király, K.; Máté, A.; Riba, P.; et al. Do Vitamins Halt the COVID-19-Evoked pro-Inflammatory Cytokines Involved in the Development of Neuropathic Pain? Biomed. Pharmacother. 2025, 189, 118346. [Google Scholar] [CrossRef]
- Waldman, H.J.; Waldman, S.D.; Kidder, K.A. Centrally Acting Skeletal Muscle Relaxants and Associated Drugs. In Pain Management, 2nd ed.; National Library of Medicine: Bethesda, MD, USA, 2011. [Google Scholar]
- Share, N.N.; McFarlane, C.S. Cyclobenzaprine: A Novel Centrally Acting Skeletal Muscle Relaxant. Neuropharmacology 1975, 14, 675–684. [Google Scholar] [CrossRef]
- Spiller, H.A.; Winter, M.L.; Mann, K.V.; Borys, D.J.; Muir, S.; Krenzelok, E.P. Five-Year Multicenter Retrospective Review of Cyclobenzaprine Toxicity. J. Emerg. Med. 1995, 13, 781–785. [Google Scholar] [CrossRef]
- Browning, R.; Jackson, J.L.; O’Malley, P.G. Cyclobenzaprine and Back Pain: A Meta-Analysis. Arch. Intern. Med. 2001, 161, 1613–1620. [Google Scholar] [CrossRef] [PubMed]
- Bebarta, V.S.; Maddry, J.; Borys, D.J.; Morgan, D.L. Incidence of Tricyclic Antidepressant-like Complications after Cyclobenzaprine Overdose. Am. J. Emerg. Med. 2011, 29, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Hasegawa, Y.; Ono, H. Cyclobenzaprine, a Centrally Acting Muscle Relaxant, Acts on Descending Serotonergic Systems. Eur. J. Pharmacol. 1996, 311, 29–35. [Google Scholar] [CrossRef]
- Sayers, A.C.; Bürki, H.R.; Eichenberger, E. The Pharmacology of 5-Chloro-4-(2-Imidazolin-2-Yl-Amino)-2,1,3-Benzothiadiazole (DS 103-282), a Novel Myotonolytic Agent. Arzneimittelforschung 1980, 30, 793–803. [Google Scholar]
- Sie, O.G.; Lakke, J.P.W.F. The Spasmolytic Properties of 5-Chloro-4-(2-Imidazolin-2-Yl-Amino)-2, 1, 3-Benzothiadiazole Hydrochloride (DS 103-282): A Pilot Study. Clin. Neurol. Neurosurg. 1980, 82, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Kameyama, T.; Nabeshima, T.; Matsuno, K.; Sugimoto, A. Comparison of α-Adrenoceptor Involvement in the Antinociceptive Action of Tizanidine and Clonidine in the Mouse. Eur. J. Pharmacol. 1986, 125, 257–264. [Google Scholar] [CrossRef]
- Klimscha, W.; Chiari, A.; Krafft, P.; Plattner, O.; Taslimi, R.; Mayer, N.; Weinstabl, C.; Schneider, B.; Zimpfer, M. Hemodynamic and Analgesic Effects of Clonidine Added Repetitively to Continuous Epidural and Spinal Blocks. Anesth. Analg. 1995, 80, 322–327. [Google Scholar] [CrossRef]
- Wagstaff, A.J.; Bryson, H.M. Tizanidine: A Review of Its Pharmacology, Clinical Efficacy and Tolerability in the Management of Spasticity Associated with Cerebral and Spinal Disorders. Drugs 1997, 53, 435–452. [Google Scholar] [CrossRef]
- Ono, H.; Fukuda, H.; Kudo, Y. Mechanisms of Depressant Action of Muscle Relaxants on Spinal Reflexes: Participation of Membrane Stabilizing Action. J. Pharmacobio-Dyn. 1984, 7, 171–176. [Google Scholar] [CrossRef]
- Novales-Li, P.; Sun, X.-P.; Takeuchi, H. Suppression of Calcium Current in a Snail Neurone by Eperisone and Its Analogues. Eur. J. Pharmacol. 1989, 168, 299–305. [Google Scholar] [CrossRef]
- Melka, A.; Tekle-Haimanot, R.; Lambien, F. Symptomatic Treatment of Neurolathyrism with Tolperisone HCL (Mydocalm): A Randomized Double Blind and Placebo Controlled Drug Trial. Ethiop. Med. J. 1997, 35, 77–91. [Google Scholar]
- Hinck, D.; Koppenhöfer, E. Tolperisone-A Novel Modulator of Ionic Currents in Myelinated Axons. Gen. Physiol. Biophys. 2001, 20, 413–429. [Google Scholar] [PubMed]
- Vaughan, S.A.; Torres, K.; Kaye, R. RESUME-1: A Phase III Study of Tolperisone in the Treatment of Painful, Acute Muscle Spasms of the Back. Pain Manag. 2021, 12, 25–33. [Google Scholar] [CrossRef]
- Bae, J.W.; Kim, M.J.; Park, Y.S.; Myung, C.S.; Jang, C.G.; Lee, S.Y. Considerable Interindividual Variation in the Pharmacokinetics of Tolperisone HC. Int. J. Clin. Pharmacol. Ther. 2007, 45, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Wuis, E.W.; Dirks, M.J.M.; Vree, T.B.; Van der Kleijn, E. Pharmacokinetics of Baclofen in Spastic Patients Receiving Multiple Oral Doses. Pharm. Weekbl. Sci. 1990, 12, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Bowery, N.G.; Hill, D.R.; Hudson, A.L.; Doble, A.; Middlemiss, D.N.; Shaw, J.; Turnbull, M. (-)Baclofen Decreases Neurotransmitter Release in the Mammalian CNS by an Action at a Novel GABA Receptor. Nature 1980, 283, 92–94. [Google Scholar] [CrossRef]
- Hulme, A.; MacLennan, W.J.; Ritchie, R.T.; John, V.A.; Shotton, P.A. Baclofen in the Elderly Stroke Patient Its Side-Effects and Pharmacokinetics. Eur. J. Clin. Pharmacol. 1985, 29, 467–469. [Google Scholar] [CrossRef]
- Fromm, G.H.; Terrence, C.F.; Chattha, A.S. Baclofen in the Treatment of Trigeminal Neuralgia: Double-blind Study and Long-term Follow-up. Ann. Neurol. 1984, 15, 240–244. [Google Scholar] [CrossRef]
- Attal, N. Pharmacological Treatments of Neuropathic Pain: The Latest Recommendations. Rev. Neurol. 2019, 175, 46–50. [Google Scholar] [CrossRef]
- Bennett, M.I.; Simpson, K.H. Gabapentin in the Treatment of Neuropathic Pain. Palliat. Med. 2004, 18, 5–11. [Google Scholar] [CrossRef]
- Serpell, M.G. Gabapentin in Neuropathic Pain Syndromes: A Randomised, Double-Blind, Placebo-Controlled Trial. Pain 2002, 99, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Kukkar, A.; Bali, A.; Singh, N.; Jaggi, A.S. Implications and Mechanism of Action of Gabapentin in Neuropathic Pain. Arch. Pharm. Res. 2013, 36, 237–251. [Google Scholar] [CrossRef] [PubMed]
- Martins, D.F.; Prado, M.R.B.; Daruge-Neto, E.; Batisti, A.P.; Emer, A.A.; Mazzardo-Martins, L.; Santos, A.R.S.; Piovezan, A.P. Caffeine Prevents Antihyperalgesic Effect of Gabapentin in an Animal Model of CRPS-I: Evidence for the Involvement of Spinal Adenosine A1 Receptor. J. Peripher. Nerv. Syst. 2015, 20, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, R.H.; O’Connor, A.B.; Backonja, M.; Farrar, J.T.; Finnerup, N.B.; Jensen, T.S.; Kalso, E.A.; Loeser, J.D.; Miaskowski, C.; Nurmikko, T.J.; et al. Pharmacologic Management of Neuropathic Pain: Evidence-Based Recommendations. Pain 2007, 132, 237–251. [Google Scholar] [CrossRef]
- Gupta, S.; Nihalani, N.; Masand, P. Duloxetine: Review of Its Pharmacology, and Therapeutic Use in Depression and Other Psychiatric Disorders. Ann. Clin. Psychiatry 2007, 19, 125–132. [Google Scholar] [CrossRef]
- Lunn, M.P.T.; Hughes, R.A.C.; Wiffen, P.J. Duloxetine for Treating Painful Neuropathy, Chronic Pain or Fibromyalgia. Cochrane Database Syst. Rev. 2014, 2014, CD007115. [Google Scholar] [CrossRef]
- Bryson, H.M.; Wilde, M.I. Amitriptyline. A Review of Its Pharmacological Properties and Therapeutic Use in Chronic Pain States. Drugs Aging 1996, 8, 459–476. [Google Scholar] [CrossRef]
- Hofer, D.; Lohberger, B.; Steinecker, B.; Schmidt, K.; Quasthoff, S.; Schreibmayer, W. A Comparative Study of the Action of Tolperisone on Seven Different Voltage Dependent Sodium Channel Isoforms. Eur. J. Pharmacol. 2006, 538, 5–14. [Google Scholar] [CrossRef]
- Mao, J.; Chen, L.L. Systemic Lidocaine for Neuropathic Pain Relief. Pain 2000, 87, 7–17. [Google Scholar] [CrossRef]
- Haeseler, G.; Foadi, N.; Ahrens, J.; Dengler, R.; Hecker, H.; Leuwer, M. Tramadol, Fentanyl and Sufentanil but Not Morphine Block Voltage-Operated Sodium Channels. Pain 2006, 126, 234–244. [Google Scholar] [CrossRef]
- Marincsák, R.; Tóth, B.I.; Czifra, G.; Szabó, T.; Kovács, L.; Bíró, T. The Analgesic Drug, Tramadol, Acts as an Agonist of the Transient Receptor Potential Vanilloid-1. Anesth. Analg. 2008, 106, 1890–1896. [Google Scholar] [CrossRef] [PubMed]
- Hara, K.; Minami, K.; Sata, T. The Effects of Tramadol and Its Metabolite on Glycine, γ-Aminobutyric AcidA, and N-Methyl-D-Aspartate Receptors Expressed in Xenopus Oocytes. Anesth. Analg. 2005, 100, 1400–1405. [Google Scholar] [CrossRef] [PubMed]
- Ambrósio, A.F.; Soares-da-Silva, P.; Carvalho, C.M.; Carvalho, A.P. Mechanisms of Action of Carbamazepine and Its Derivatives, Oxcarbazepine, BIA 2-093, and BIA 2-024. Neurochem. Res. 2002, 27, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Fung, S.J.; Manzoni, D.; Chan, J.Y.H.; Pompeiano, O.; Barnes, C.D. Locus Coeruleus Control of Spinal Motor Output. Prog. Brain Res. 1991, 88, 395–409. [Google Scholar]
- Commissiong, J.W.; Karoum, F.; Reiffenstein, R.J.; Neff, N.H. Cyclobenzaprine: A Possible Mechanism of Action for Its Muscle Relaxant Effect. Can. J. Physiol. Pharmacol. 1981, 59, 37–44. [Google Scholar] [CrossRef]
- Hirayama, T.; Ono, H.; Fukuda, H. Effects of Adrenergic Agents on Ventral Horn Cells in Rat Spinal Cord Slices. Biomed. Res. 1988, 9, 343–351. [Google Scholar] [CrossRef]
- Fung, S.J.; Chan, J.Y.H.; Manzoni, D.; White, S.R.; Lai, Y.Y.; Strahlendorf, H.K.; Zhuo, H.; Liu, R.H.; Reddy, V.K.; Barnes, C.D. Cotransmitter-Mediated Locus Coeruleus Action on Motoneurons. Brain Res. Bull. 1994, 35, 423–432. [Google Scholar] [CrossRef]
- Tartas, M.; Morin, F.; Barrière, G.; Goillandeau, M.; Lacaille, J.C.; Cazalets, J.R.; Bertrand, S.S. Noradrenergic Modulation of Intrinsic and Synaptic Properties of Lumbar Motoneurons in the Neonatal Rat Spinal Cord. Front. Neural Circuits 2010, 4, 1243. [Google Scholar] [CrossRef]
- Rank, M.M.; Murray, K.C.; Stephens, M.J.; D’Amico, J.; Gorassini, M.A.; Bennett, D.J. Adrenergic Receptors Modulate Motoneuron Excitability, Sensory Synaptic Transmission and Muscle Spasms after Chronic Spinal Cord Injury. J. Neurophysiol. 2011, 105, 410–422. [Google Scholar] [CrossRef]
- Olson, D.E. Psychoplastogens: A Promising Class of Plasticity-Promoting Neurotherapeutics. J. Exp. Neurosci. 2018, 12, 1179069518800508. [Google Scholar] [CrossRef]
- Vizcarra, V.S.; Barber, K.R.; Franca-Solomon, G.; Majuta, L.; Smith, A.; Langlais, P.R.; Largent-Milnes, T.M.; Vanderah, T.W.; Riegel, A.C. Targeting 5-HT2A Receptors and Kv7 Channels in PFC to Attenuate Chronic Neuropathic Pain in Rats Using a Spared Nerve Injury Model. Neurosci. Lett. 2022, 789, 136864. [Google Scholar] [CrossRef]
- Perrier, J.-F.; Rasmussen, H.; Christensen, R.; Petersen, A. Modulation of the Intrinsic Properties of Motoneurons by Serotonin. Curr. Pharm. Des. 2013, 19, 4371–4384. [Google Scholar] [CrossRef] [PubMed]
- Perrier, J.F.; Cotel, F. Serotonergic Modulation of Spinal Motor Control. Curr. Opin. Neurobiol. 2015, 33, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bayliss, D.A.; Umemiya, M.; Berger, A.J. Inhibition of N- and P-type Calcium Currents and the After-hyperpolarization in Rat Motoneurones by Serotonin. J. Physiol. 1995, 485, 635–647. [Google Scholar] [CrossRef]
- Nadeson, R.; Goodchild, C.S. Antinociceptive Role of 5-HT1A Receptors in Rat Spinal Cord. Br. J. Anaesth. 2002, 88, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Cortes-Altamirano, J.L.; Olmos-Hernandez, A.; Jaime, H.B.; Carrillo-Mora, P.; Bandala, C.; Reyes-Long, S.; Alfaro-Rodríguez, A. Review: 5-HT1, 5-HT2, 5-HT3 and 5-HT7 Receptors and Their Role in the Modulation of Pain Response in the Central Nervous System. Curr. Neuropharmacol. 2018, 16, 210–221. [Google Scholar] [CrossRef]
- Brenchat, A.; Nadal, X.; Romero, L.; Ovalle, S.; Muro, A.; Sánchez-Arroyos, R.; Portillo-Salido, E.; Pujol, M.; Montero, A.; Codony, X.; et al. Pharmacological Activation of 5-HT7 Receptors Reduces Nerve Injury-Induced Mechanical and Thermal Hypersensitivity. Pain 2010, 149, 483–494. [Google Scholar] [CrossRef]
- Bardin, L. The Complex Role of Serotonin and 5-HT Receptors in Chronic Pain. Behav. Pharmacol. 2011, 22, 390–404. [Google Scholar] [CrossRef]
- Okamoto, K.; Imbe, H.; Morikawa, Y.; Itoh, M.; Sekimoto, M.; Nemoto, K.; Senba, E. 5-HT2A Receptor Subtype in the Peripheral Branch of Sensory Fibers Is Involved in the Potentiation of Inflammatory Pain in Rats. Pain 2002, 99, 133–143. [Google Scholar] [CrossRef]
- Van Steenwinckel, J.; Brisorgueil, M.J.; Fischer, J.; Vergé, D.; Gingrich, J.A.; Bourgoin, S.; Hamon, M.; Bernard, R.; Conrath, M. Role of Spinal Serotonin 5-HT2A Receptor in 2′,3′-Dideoxycytidine-Induced Neuropathic Pain in the Rat and the Mouse. Pain 2008, 137, 66–80. [Google Scholar] [CrossRef]
- Wang, D.; Gao, Y.; Ji, H.; Hong, Y. Topical and Systemic Administrations of Ketanserin Attenuate Hypersensitivity and Expression of CGRP in Rats with Spinal Nerve Ligation. Eur. J. Pharmacol. 2010, 627, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Nitanda, A.; Yasunami, N.; Tokumo, K.; Fujii, H.; Hirai, T.; Nishio, H. Contribution of the Peripheral 5-HT2A Receptor to Mechanical Hyperalgesia in a Rat Model of Neuropathic Pain. Neurochem. Int. 2005, 47, 394–400. [Google Scholar] [CrossRef]
- Dupuis, A.; Wattiez, A.S.; Pinguet, J.; Richard, D.; Libert, F.; Chalus, M.; Aissouni, Y.; Sion, B.; Ardid, D.; Marin, P.; et al. Increasing Spinal 5-HT2A Receptor Responsiveness Mediates Anti-Allodynic Effect and Potentiates Fluoxetine Efficacy in Neuropathic Rats. Evidence for GABA Release. Pharmacol. Res. 2017, 118, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Day, L.T.; Jeanmonod, R.K. Serotonin Syndrome in a Patient Taking Lexapro and Flexeril: A Case Report. Am. J. Emerg. Med. 2008, 26, 1069.e1–1069.e3. [Google Scholar] [CrossRef] [PubMed]
- Mestres, J.; Seifert, S.A.; Oprea, T.I. Linking Pharmacology to Clinical Reports Cyclobenzaprine and Its Possible Association with Serotonin Syndrome. Clin. Pharmacol. Ther. 2011, 90, 662–665. [Google Scholar] [CrossRef]
- Keegan, M.T.; Brown, D.R.; Rabinstein, A.A. Serotonin Syndrome from the Interaction of Cyclobenzaprine with Other Serotoninergic Drugs. Anesth. Analg. 2006, 103, 1466–1468. [Google Scholar] [CrossRef]
- Herman, C.R.; Schiffman, E.L.; Look, J.O.; Rindal, D.B. The Effectiveness of Adding Pharmacologic Treatment with Clonazepam or Cyclobenzaprine to Patient Education and Self-Care for the Treatment of Jaw Pain upon Awakening: A Randomized Clinical Trial. J. Orofac. Pain 2002, 16, 1. [Google Scholar]
- Furtado, R.N.V.; Carazzato, S.; Farias, C.A.; Chamlian, T.R.; Masiero, D. Myofascial Syndrome: Comparison between Infiltration of Trigger Points Treatment and Oral Medication (Cyclobenzaprine). Acta Fisiátr. 2002, 9, 117–126. [Google Scholar] [CrossRef]
- Leite, F.M.G.; Atallah, Á.N.; El Dib, R.; Grossmann, E.; Januzzi, E.; Andriolo, R.B.; Da Silva, E.M.K. Cyclobenzaprine for the Treatment of Myofascial Pain in Adults. Cochrane Database Syst. Rev. 2009, 2017, CD006830. [Google Scholar] [CrossRef]
- Friedman, B.W.; Dym, A.A.; Davitt, M.; Holden, L.; Solorzano, C.; Esses, D.; Bijur, P.E.; Gallagher, E.J. Naproxen with Cyclobenzaprine, Oxycodone/Acetaminophen, or Placebo for Treating Acute Low Back Pain: A Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2015, 314, 1572–1580. [Google Scholar] [CrossRef]
- Cohen, S.P.; Mullings, R.; Abdi, S. The Pharmacologic Treatment of Muscle Pain. Anesthesiology 2004, 101, 495–526. [Google Scholar] [CrossRef]
- Chua-Tuan, J.L.; Cao, D.; Iwanicki, J.L.; Hoyte, C.O. Cardiac Sodium Channel Blockade after an Intentional Ingestion of Lacosamide, Cyclobenzaprine, and Levetiracetam: Case Report. Clin. Toxicol. 2015, 53, 565–568. [Google Scholar] [CrossRef]
- Tu, J.; Zhang, C.; Xie, S.; He, J.; Zhang, H. Cyclobenzaprine-Related Adverse Events: A Comprehensive Pharmacovigilance Analysis Using the FDA Adverse Event Reporting System. Front. Med. 2025, 12, 1574395. [Google Scholar] [CrossRef] [PubMed]
- Kameyama, T.; Nabeshima, T.; Sugimoto, A.; Matsuno, K.; Yamada, S. Antinociceptive Action of Tizanidine in Mice and Rats. Naunyn Schmiedebergs Arch. Pharmacol. 1985, 330, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Pei, W.; Zou, Y.; Wang, W.; Wei, L.; Zhao, Y.; Li, L. Tizanidine Exerts Anti-Nociceptive Effects in Spared Nerve Injury Model of Neuropathic Pain through Inhibition of TLR4/NF-ΚB Pathway. Int. J. Mol. Med. 2018, 42, 3209–3219. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, R.J.; Kroin, J.S.; Lubenow, T.R.; Penn, R.D.; Ivankovich, A.D. Effect of Intrathecal Tizanidine on Antinociception and Blood Pressure in the Rat. Pain 1990, 40, 333–338. [Google Scholar] [CrossRef]
- Kawamata, T.; Omote, K.; Kawamata, M.; Iwasaki, H.; Namiki, A. Antinociceptive Interaction of Intrathecal A2-Adrenergic Agonists, Tizanidine and Clonidine, with Lidocaine in Rats. Anesthesiology 1997, 87, 436–448. [Google Scholar] [CrossRef]
- Hord, A.H.; Chalfoun, A.G.; Denson, D.D.; Azevedo, M.I. Systemic Tizanidine Hydrochloride (ZanaflexTM) Relieves Thermal Hyperalgesia in Rats with an Experimental Mononeuropathy. Anesth. Analg. 2001, 93, 1310–1315. [Google Scholar] [CrossRef]
- Semenchuk, M.R.; Sherman, S. Effectiveness of Tizanidine in Neuropathic Pain: An Open-Label Study. J. Pain 2000, 1, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Young, W.S.; Kuhar, M.J. Noradrenergic A1 and A2 Receptors: Light Microscopic Autoradiographic Localization. Proc. Natl. Acad. Sci. USA 1980, 77, 1696–1700. [Google Scholar] [CrossRef]
- Brightwell, J.J.; Taylor, B.K. Noradrenergic Neurons in the Locus Coeruleus Contribute to Neuropathic Pain. Neuroscience 2009, 160, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Buerkle, H.; Yaksh, T.L. Pharmacological Evidence for Different Alpha2-Adrenergic Receptor Sites Mediating Analgesia and Sedation in the Rat. Br. J. Anaesth. 1998, 81, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Gyires, K.; Zádori, Z.S.; Török, T.; Mátyus, P. A2-Adrenoceptor Subtypes-Mediated Physiological, Pharmacological Actions. Neurochem. Int. 2009, 55, 447–453. [Google Scholar] [CrossRef]
- Bylund, D.B. Sub Types of A2-Adrenoceptors: Pharmacological and Molecular Biological Evidence Converg. Trends Pharmacol. Sci. 1988, 9, 356–361. [Google Scholar] [CrossRef]
- Hein, L.; Kobilka, B.K. Adrenergic Receptor Signal Transduction and Regulation. Neuropharmacology 1995, 34, 357–366. [Google Scholar] [CrossRef]
- Shujaa, N.; Al-Khrasani, M.; Zádori, Z.S.; Rossi, M.; Mátyus, P.; Németh, J.; Hein, L.; Gyires, K. α(2)-Adrenoceptor Agonist-Induced Inhibition of Gastric Motor Activity Is Mediated by α(2A)-Adrenoceptor Subtype in the Mouse. Neurochem. Int. 2011, 58, 708–713. [Google Scholar] [CrossRef]
- Michel, A.D.; Loury, D.N.; Whiting, R.L. Assessment of Imiloxan as a Selective α(2B)-Adrenoceptor Antagonist. Br. J. Pharmacol. 1990, 99, 560–564. [Google Scholar] [CrossRef]
- Sallinen, J.; Höglund, I.; Engström, M.; Lehtimäki, J.; Virtanen, R.; Sirviö, J.; Wurster, S.; Savola, J.M.; Haapalinna, A. Pharmacological Characterization and CNS Effects of a Novel Highly Selective α 2C-Adrenoceptor Antagonist JP-1302. Br. J. Pharmacol. 2007, 150, 391–402. [Google Scholar] [CrossRef]
- Nicholas, A.P.; Pieribone, V.; Hökfelt, T. Distributions of MRNAs for Alpha-2 Adrenergic Receptor Subtypes in Rat Brain: An in Situ Hybridization Study. J. Comp. Neurol. 1993, 328, 575–594. [Google Scholar] [CrossRef]
- Bahari, Z.; Meftahi, G.H. Spinal A2-Adrenoceptors and Neuropathic Pain Modulation; Therapeutic Target. Br. J. Pharmacol. 2019, 176, 2366–2381. [Google Scholar] [CrossRef]
- Malmberg, A.B.; Hedley, L.R.; Jasper, J.R.; Hunter, J.C.; Basbaum, A.I. Contribution of a 2 Receptor Subtypes to Nerve Injury-Induced Pain and Its Regulation by Dexmedetomidine. Br. J. Pharmacol. 2001, 132, 1827–1836. [Google Scholar] [CrossRef]
- Pertovaara, A. The Noradrenergic Pain Regulation System: A Potential Target for Pain Therapy. Eur. J. Pharmacol. 2013, 716, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Costa-Pereira, J.T.; Ribeiro, J.; Martins, I.; Tavares, I. Role of Spinal Cord A2-Adrenoreceptors in Noradrenergic Inhibition of Nociceptive Transmission During Chemotherapy-Induced Peripheral Neuropathy. Front. Neurosci. 2020, 13, 1413. [Google Scholar] [CrossRef]
- Sudo, R.T.; do Amaral, R.V.; da Silva Monteiro, C.E.; Pitta, I.d.R.; Lima, M.d.C.; Montes, G.C.; Ririe, D.G.; Hayashida, K.; Zapata-Sudo, G. Antinociception Induced by a Novel A2A Adrenergic Receptor Agonist in Rodents Acute and Chronic Pain Models. Eur. J. Pharmacol. 2017, 815, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Limbird, L.E. Receptors Linked to Inhibition of Adenylate Cyclase: Additional Signaling Mechanisms. FASEB J. 1988, 2, 2686–2695. [Google Scholar] [CrossRef]
- Gilsbach, R.; Hein, L. Are the Pharmacology and Physiology of α 2adrenoceptors Determined by α 2-Heteroreceptors and Autoreceptors Respectively? Br. J. Pharmacol. 2012, 165, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Im, S.T.; Jo, Y.Y.; Han, G.; Jo, H.J.; Kim, Y.H.; Park, C.K. Dexmedetomidine Inhibits Voltage-Gated Sodium Channels via α 2-Adrenoceptors in Trigeminal Ganglion Neurons. Mediat. Inflamm. 2018, 2018, 1782719. [Google Scholar] [CrossRef]
- Kaddar, N.; Vigneault, P.; Pilote, S.; Patoine, D.; Simard, C.; Drolet, B. Tizanidine (Zanaflex): A Muscle Relaxant That May Prolong the QT Interval by Blocking I Kr. J. Cardiovasc. Pharmacol. Ther. 2012, 17, 102–109. [Google Scholar] [CrossRef]
- Svensson, P.; Wang, K.; Arendt-Nielsen, L. Effect of Muscle Relaxants on Experimental Jaw-Muscle Pain and Jaw-Stretch Reflexes: A Double-Blind and Placebo-Controlled Trial. Eur. J. Pain 2003, 7, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.; McLeod, G. Basic Pharmacology of Local Anaesthetics. BJA Educ. 2020, 20, 34–41. [Google Scholar] [CrossRef]
- Yu, F.H.; Catterall, W.A. Overview of the Voltage-Gated Sodium Channel Family. Genome Biol. 2003, 4, 207. [Google Scholar] [CrossRef]
- Xie, Y.F. Nav1.8 and Chronic Pain: From Laboratory Animals to Clinical Patients. Biomolecules 2025, 15, 694. [Google Scholar] [CrossRef]
- Lai, J.; Porreca, F.; Hunter, J.C.; Gold, M.S. Voltage-Gated Sodium Channels and Hyperalgesia. Annu. Rev. Pharmacol. Toxicol. 2004, 44, 371–397. [Google Scholar] [CrossRef]
- Dib-Hajj, S.D.; Cummins, T.R.; Black, J.A.; Waxman, S.G. Sodium Channels in Normal and Pathological Pain. Annu. Rev. Neurosci. 2010, 33, 325–347. [Google Scholar] [CrossRef]
- Bertoch, T.; D’Aunno, D.; McCoun, J.; Solanki, D.; Taber, L.; Urban, J.; Oswald, J.; Swisher, M.W.; Tian, S.; Miao, X.; et al. Suzetrigine, a Nonopioid NaV1.8 Inhibitor for Treatment of Moderate-to-Severe Acute Pain: Two Phase 3 Randomized Clinical Trials. Anesthesiology 2025, 142, 1085–1099. [Google Scholar] [CrossRef] [PubMed]
- Cha, K.I.; Kim, G.E.; Seol, J.H.; Kim, D.W.; Lee, S. Enhancing Chemical Stability and Bioavailability of Aneratrigine Capsules via Dry Granulation: Addressing Stability Challenges in Sodium Bicarbonate-Containing Formulations for Clinical Development. Pharmaceutics 2025, 17, 1047. [Google Scholar] [CrossRef] [PubMed]
- Niu, H.L.; Liu, Y.N.; Xue, D.Q.; Dong, L.Y.; Liu, H.J.; Wang, J.; Zheng, Y.L.; Zou, A.R.; Shao, L.M.; Wang, K.W. Inhibition of Nav1.7 Channel by a Novel Blocker QLS-81 for Alleviation of Neuropathic Pain. Acta Pharmacol. Sin. 2021, 42, 1235–1247. [Google Scholar] [CrossRef]
- Zhang, B.; Shi, X.; Liu, X.; Liu, Y.; Li, X.; Wang, Q.; Huang, D.; Zhao, W.; Cui, J.; Cao, Y.; et al. Discovery of E0199: A Novel Compound Targeting Both Peripheral NaV and KV7 Channels to Alleviate Neuropathic Pain. J. Pharm. Anal. 2025, 15, 101132. [Google Scholar] [CrossRef]
- Jarvis, M.F.; Honore, P.; Shieh, C.C.; Chapman, M.; Joshi, S.; Zhang, X.F.; Kort, M.; Carroll, W.; Marron, B.; Atkinson, R.; et al. A-803467, a Potent and Selective Nav1.8 Sodium Channel Blocker, Attenuates Neuropathic and Inflammatory Pain in the Rat. Proc. Natl. Acad. Sci. USA 2007, 104, 8520–8525. [Google Scholar] [CrossRef]
- McGaraughty, S.; Chu, K.L.; Scanio, M.J.C.; Kort, M.E.; Faltynek, C.R.; Jarvis, M.F. A Selective Nav1.8 Sodium Channel Blocker, A-803467 [5-4-Chlorophenyl-N-(3,5-Dimethoxyphenyl)Furan-2-Carboxamide], Attenuates Spinal Neuronal Activity in Neuropathic Rats. J. Pharmacol. Exp. Ther. 2008, 324, 1204–1211. [Google Scholar] [CrossRef]
- Gilchrist, J.M.; Yang, N.D.; Jiang, V.; Moyer, B.D. Pharmacologic Characterization of LTGO-33, a Selective Small Molecule Inhibitor of the Voltage-Gated Sodium Channel NaV1.8 with a Unique Mechanism of ActionS. Mol. Pharmacol. 2024, 105, 233–249. [Google Scholar] [CrossRef]
- Su, M.; Ouyang, X.; Zhou, P.; Dong, L.; Shao, L.; Wang, K.; Liu, Y. Inhibition of TTX-S Na+ Currents by a Novel Blocker QLS-278 for Antinociception. J. Pharmacol. Exp. Ther. 2025, 392, 100030. [Google Scholar] [CrossRef]
- Xue, D.; Liu, Y.; Zheng, Y.; Niu, H.; Dong, L.; Ouyang, X.; Song, S.; Zhang, D.; Ge, Q.; Wang, K.; et al. Design and Synthesis of Novel α-Aminoamides Derivatives as Nav1.7 Inhibitors for Antinociception. Chin. Chem. Lett. 2022, 33, 1643–1646. [Google Scholar] [CrossRef]
- McCoun, J.; Winkle, P.; Solanki, D.; Urban, J.; Bertoch, T.; Oswald, J.; Swisher, M.W.; Taber, L.A.; Healey, T.; Jazic, I.; et al. Suzetrigine, a Non-Opioid NaV1.8 Inhibitor With Broad Applicability for Moderate-to-Severe Acute Pain: A Phase 3 Single-Arm Study for Surgical or Non-Surgical Acute Pain. J. Pain. Res. 2025, 18, 1569–1576. [Google Scholar] [CrossRef] [PubMed]
- Zakrzewska, J.M.; Palmer, J.; Morisset, V.; Giblin, G.M.; Obermann, M.; Ettlin, D.A.; Cruccu, G.; Bendtsen, L.; Estacion, M.; Derjean, D.; et al. Safety and Efficacy of a Nav1.7 Selective Sodium Channel Blocker in Patients with Trigeminal Neuralgia: A Double-Blind, Placebo-Controlled, Randomised Withdrawal Phase 2a Trial. Lancet Neurol. 2017, 16, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Mueller, A.; Starobova, H.; Morgan, M.; Dekan, Z.; Cheneval, O.; Schroeder, C.I.; Alewood, P.F.; Deuis, J.R.; Vetter, I. Antiallodynic Effects of the Selective NaV1.7 Inhibitor Pn3a in a Mouse Model of Acute Postsurgical Pain: Evidence for Analgesic Synergy with Opioids and Baclofen. Pain 2019, 160, 1766–1780. [Google Scholar] [CrossRef]
- Deuis, J.R.; Wingerd, J.S.; Winter, Z.; Durek, T.; Dekan, Z.; Sousa, S.R.; Zimmermann, K.; Hoffmann, T.; Weidner, C.; Nassar, M.A.; et al. Analgesic Effects of GpTx-1, PF-04856264 and CNV1014802 in a Mouse Model of NaV1.7-Mediated Pain. Toxins 2016, 8, 78. [Google Scholar] [CrossRef] [PubMed]
- Lakatos, P.P.; Karádi, D.Á.; Galambos, A.R.; Essmat, N.; Király, K.; Laufer, R.; Geda, O.; Zádori, Z.S.; Tábi, T.; Al-Khrasani, M.; et al. The Acute Antiallodynic Effect of Tolperisone in Rat Neuropathic Pain and Evaluation of Its Mechanism of Action. Int. J. Mol. Sci. 2022, 23, 9564. [Google Scholar] [CrossRef]
- Essmat, N.; Galambos, A.R.; Lakatos, P.P.; Karádi, D.Á.; Mohammadzadeh, A.; Abbood, S.K.; Geda, O.; Laufer, R.; Király, K.; Riba, P. Pregabalin–Tolperisone Combination to Treat Neuropathic Pain: Improved Analgesia and Reduced Side Effects in Rats. Pharmaceuticals 2023, 16, 1115. [Google Scholar] [CrossRef]
- Field, M.J.; Cox, P.J.; Stott, E.; Melrose, H.; Offord, J.; Su, T.Z.; Bramwell, S.; Corradini, L.; England, S.; Winks, J.; et al. Identification of the A2-δ-1 Subunit of Voltage-Calcium Calcium Channels as a Molecular Target for Pain Mediating the Analgesic Actions of Pregabalin. Proc. Natl. Acad. Sci. USA 2006, 103, 17537–17542. [Google Scholar] [CrossRef]
- Moore, R.A.; Straube, S.; Wiffen, P.J.; Derry, S.; McQuay, H.J.; Moore, M. Pregabalin for Acute and Chronic Pain in Adults. Cochrane Database Syst. Rev. 2009, CD007076. [Google Scholar] [CrossRef] [PubMed]
- Hahm, T.S.; Ahn, H.J.; Ryu, S.; Gwak, M.S.; Choi, S.J.; Kim, J.K.; Yu, J.M. Combined Carbamazepine and Pregabalin Therapy in a Rat Model of Neuropathic Pain. Br. J. Anaesth. 2012, 109, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Mariam, A.; Tahir, N.; Rasheed, N.; Khan, N.; Fazal, S.; Naseer, R. Comparison of Carbamazepine Alone and in Combination with Gabapentin as Medical Therapy to Control Pain Associated with Trigeminal Neuralgia. Found. Univ. J. Dent. 2024, 4, 37–41. [Google Scholar] [CrossRef]
- Striessnig, J.; Pinggera, A.; Kaur, G.; Bock, G.; Tuluc, P. L-Type Ca2+ Channels in Heart and Brain. Wiley Interdiscip. Rev. Membr. Transp. Signal. 2014, 3, 15–38. [Google Scholar] [CrossRef]
- Isensee, J.; van Cann, M.; Despang, P.; Araldi, D.; Moeller, K.; Petersen, J.; Schmidtko, A.; Matthes, J.; Levine, J.D.; Hucho, T. Depolarization Induces Nociceptor Sensitization by Cav1.2-Mediated PKA-II Activation. J. Cell Biol. 2021, 220, e202002083. [Google Scholar] [CrossRef]
- Antunes, F.T.T.; Campos, M.M.; Carvalho, V.d.P.R.; da Silva Junior, C.A.; Magno, L.A.V.; de Souza, A.H.; Gomez, M.V. Current Drug Development Overview: Targeting Voltage-Gated Calcium Channels for the Treatment of Pain. Int. J. Mol. Sci. 2023, 24, 9223. [Google Scholar] [CrossRef]
- Radwani, H.; Lopez-Gonzalez, M.J.; Cattaert, D.; Roca-Lapirot, O.; Dobremez, E.; Bouali-Benazzouz, R.; Eiríksdóttir, E.; Langel, Ü.; Favereaux, A.; Errami, M.; et al. Cav1.2 and Cav1.3 L-Type Calcium Channels Independently Control Short- and Long-Term Sensitization to Pain. J. Physiol. 2016, 594, 6607–6626. [Google Scholar] [CrossRef] [PubMed]
- Ertel, E.A.; Campbell, K.P.; Harpold, M.M.; Hofmann, F.; Mori, Y.; Perez-Reyes, E.; Schwartz, A.; Snutch, T.P.; Tanabe, T.; Birnbaumer, L.; et al. Nomenclature of Voltage-Gated Calcium Channels. Neuron 2000, 25, 533–535. [Google Scholar] [CrossRef]
- Hell, J.W.; Westenbroek, R.E.; Warner, C.; Ahlijanian, M.K.; Prystay, W.; Gilbert, M.M.; Snutch, T.P.; Catterall, W.A. Identification and Differential Subcellular Localization of the Neuronal Class C and Class D L-Type Calcium Channel A1 Subunits. J. Cell Biol. 1993, 123, 949–962. [Google Scholar] [CrossRef]
- Hetzenauer, A.; Sinnegger-Brauns, M.J.; Striessnig, J.; Singewald, N. Brain Activation Pattern Induced by Stimulation of L-Type Ca2+-Channels: Contribution of CaV1.3 and CaV1.2 Isoforms. Neuroscience 2006, 139, 1005–1015. [Google Scholar] [CrossRef]
- Zanetti, L.; Kilicarslan, I.; Netzer, M.; Babai, N.; Seitter, H.; Koschak, A. Function of Cone and Cone-Related Pathways in CaV1.4 IT Mice. Sci. Rep. 2021, 11, 2732. [Google Scholar] [CrossRef] [PubMed]
- Bibollet, H.; Kramer, A.; Bannister, R.A.; Hernández-Ochoa, E.O. Advances in CaV1.1 Gating: New Insights into Permeation and Voltage-Sensing Mechanisms. Channels 2023, 17, 2167569. [Google Scholar] [CrossRef] [PubMed]
- Alves, V.S.; Alves-Silva, H.S.; Orts, D.J.B.; Ribeiro-Silva, L.; Arcisio-Miranda, M.; Oliveira, F.A. Calcium Signaling in Neurons and Glial Cells: Role of Cav1 Channels. Neuroscience 2019, 421, 95–111. [Google Scholar] [CrossRef]
- Llinás, R.R.; Choi, S.; Urbano, F.J.; Shin, H.S. γ-Band Deficiency and Abnormal Thalamocortical Activity in P/Q-Type Channel Mutant Mice. Proc. Natl. Acad. Sci. USA 2007, 104, 17819–17824. [Google Scholar] [CrossRef]
- Meuth, S.; Budde, T.; Pape, H.C. Differential Control of High-Voltage Activated Ca2+ Current Components by a Ca2+-Dependent Inactivation Mechanism in Thalamic Relay Neurons. Thalamus Relat. Syst. 2001, 1, 31–38. [Google Scholar] [CrossRef]
- Ferron, L.; Harding, E.K.; Gandini, M.A.; Brideau, C.; Stys, P.K.; Zamponi, G.W. Functional Remodeling of Presynaptic Voltage-Gated Calcium Channels in Superficial Layers of the Dorsal Horn during Neuropathic Pain. iScience 2024, 27, 109973. [Google Scholar] [CrossRef]
- Nieto-Rostro, M.; Ramgoolam, K.; Pratt, W.S.; Kulik, A.; Dolphin, A.C. Ablation of α 2 δ-1 Inhibits Cell-Surface Trafficking of Endogenous N-Type Calcium Channels in the Pain Pathway in Vivo. Proc. Natl. Acad. Sci. USA 2018, 115, E12043–E12052. [Google Scholar] [CrossRef]
- Ohashi, N.; Uta, D.; Ohashi, M.; Hoshino, R.; Baba, H. Omega-Conotoxin MVIIA Reduces Neuropathic Pain after Spinal Cord Injury by Inhibiting N-Type Voltage-Dependent Calcium Channels on Spinal Dorsal Horn. Front. Neurosci. 2024, 18, 1366829. [Google Scholar] [CrossRef]
- Smith, M.T.; Cabot, P.J.; Ross, F.B.; Robertson, A.D.; Lewis, R.J. The Novel N-Type Calcium Channel Blocker, AM336, Produces Potent Dose-Dependent Antinociception after Intrathecal Dosing in Rats and Inhibits Substance P Release in Rat Spinal Cord Slices. Pain 2002, 96, 119–127. [Google Scholar] [CrossRef]
- Nebe, J.; Vanegas, H.; Schaible, H.G. Spinal Application of ω-Conotoxin GVIA, an N-Type Calcium Channel Antagonist, Attenuates Enhancement of Dorsal Spinal Neuronal Responses Caused by Intra-Articular Injection of Mustard Oil in the Rat. Exp. Brain Res. 1998, 120, 61–69. [Google Scholar] [CrossRef]
- de Amorim Ferreira, M.; Ferreira, J. Role of Cav2.3 (R-Type) Calcium Channel in Pain and Analgesia: A Scoping Review. Curr. Neuropharmacol. 2023, 22, 1909–1922. [Google Scholar] [CrossRef]
- Le Pichon, C.E.; Chesler, A.T. The Functional and Anatomical Dissection of Somatosensory Subpopulations Using Mouse Genetics. Front. Neuroanat. 2014, 8, 21. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Hwang, J.H.; Kim, J.S.; Jung, S.J.; Oh, S.B. R-Type Calcium Channel Isoform in Rat Dorsal Root Ganglion Neurons. Korean J. Physiol. Pharmacol. 2010, 14, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Park, C.K.; Hai, Y.L.; Hyun, Y.K.; Park, S.H.; Sung, J.J.; Joong, S.K.; Monteil, A.; Seog, B.O.; Miller, R.J. Molecular Basis of Cav2.3 Calcium Channels in Rat Nociceptive Neurons. J. Biol. Chem. 2007, 282, 4757–4764. [Google Scholar] [CrossRef]
- Murakami, M.; Suzuki, T.; Nakagawasai, O.; Murakami, H.; Murakami, S.; Esashi, A.; Taniguchi, R.; Yanagisawa, T.; Tan-No, K.; Miyoshi, I.; et al. Distribution of Various Calcium Channel A1 Subunits in Murine DRG Neurons and Antinociceptive Effect of ω-Conotoxin SVIB in Mice. Brain Res. 2001, 903, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.; Ibrahim, M.; Gomez, K.; Yu, J.; Cai, S.; Chew, L.A.; Bellampalli, S.S.; Moutal, A.; Largent-Milnes, T.; Porreca, F.; et al. Conotoxin Contulakin-G Engages a Neurotensin Receptor 2/R-Type Calcium Channel (Cav2.3) Pathway to Mediate Spinal Antinociception. Pain 2022, 163, 1751–1762. [Google Scholar] [CrossRef]
- Saegusa, H.; Kurihara, T.; Zong, S.; Minowa, O.; Kazuno, A.A.; Han, W.; Matsuda, Y.; Yamanaka, H.; Osanai, M.; Noda, T.; et al. Altered Pain Responses in Mice Lacking A1E Subunit of the Voltage-Dependent Ca2+ Channel. Proc. Natl. Acad. Sci. USA 2000, 97, 6132–6137. [Google Scholar] [CrossRef]
- Westenbroek, R.E.; Hoskins, L.; Catterall, W.A. Localization of Ca2+ Channel Subtypes on Rat Spinal Motor Neurons, Interneurons, and Nerve Terminals. J. Neurosci. 1998, 18, 6319–6330. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, F.X.; Huang, F.; Lu, Y.J.; Li, G.D.; Bao, L.; Xiao, H.S.; Zhang, X. Peripheral Nerve Injury Induces Trans-Synaptic Modification of Channels, Receptors and Signal Pathways in Rat Dorsal Spinal Cord. Eur. J. Neurosci. 2004, 19, 871–883. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, C.T.; Westenbroek, R.E.; Hell, J.W.; Soong, T.W.; Snutch, T.P.; Catterall, W.A. Biochemical Properties and Subcellular Distribution of the Neuronal Class E Calcium Channel A1 Subunit. J. Neurosci. 1995, 15, 6419–6432. [Google Scholar] [CrossRef]
- Tadic, V.P.; Timic Stamenic, T.; Todorovic, S.M. CaV2.3 Channels in the Mouse Central Medial Thalamic Nucleus Are Essential for Thalamocortical Oscillations and Spike Wave Discharges. Sci. Rep. 2025, 15, 4966. [Google Scholar] [CrossRef]
- Talley, E.M.; Cribbs, L.L.; Lee, J.H.; Daud, A.; Perez-Reyes, E.; Bayliss, D.A. Differential Distribution of Three Members of a Gene Family Encoding Low Voltage-Activated (T-Type) Calcium Channels. J. Neurosci. 1999, 19, 1895–1911. [Google Scholar] [CrossRef]
- Zhang, Y.; Mori, M.; Burgess, D.L.; Noebels, J.L. Mutations in High-Voltage-Activated Calcium Channel Genes Stimulate Low-Voltage-Activated Currents in Mouse Thalamic Relay Neurons. J. Neurosci. 2002, 22, 6362–6371. [Google Scholar] [CrossRef]
- Na, H.S.; Choi, S.; Kim, J.; Park, J.; Shin, H.S. Attenuated Neuropathic Pain in CaV3.1 Null Mice. Mol. Cells 2008, 25, 242–246. [Google Scholar] [CrossRef]
- Fels, G. Tolperisone: Evaluation of the Lidocaine-like Activity by Molecular Modeling. Arch. Pharm. 1996, 329, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, T.S.; Fukuda, K.I.; Mori, S.; Ogawa, M.; Nagasawa, K. Determination of Tolperisone Enantiomers in Plasma and Their Disposition in Rats. Chem. Pharm. Bull. 1992, 40, 272–274. [Google Scholar] [CrossRef]
- Kumar, M.; Kumar, M.; Freund, J.M.; Dillon, G.H. A Single Amino Acid Residue at Transmembrane Domain 4 of the α Subunit Influences Carisoprodol Direct Gating Efficacy at GABAa Receptors. J. Pharmacol. Exp. Ther. 2017, 362, 395–404. [Google Scholar] [CrossRef]
- Reeves, R.R.; Burke, R.S. Carisoprodol: Abuse Potential and Withdrawal Syndrome. Curr. Drug Abuse. Rev. 2010, 3, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Reeves, R.R.; Pinkofsky, H.B.; Carter, O.S. Carisoprodol: A Drug of Continuing Abuse. J. Am. Osteopath. Assoc. 1997, 97, 723. [Google Scholar] [CrossRef]
- Terrence, C.F.; Fromm, G.H.; Tenicela, R. Baclofen as an Analgesic in Chronic Peripheral Nerve Disease. Eur. Neurol. 1985, 24, 380–385. [Google Scholar] [CrossRef]
- Barton, D.L.; Wos, E.J.; Qin, R.; Mattar, B.I.; Green, N.B.; Lanier, K.S.; Bearden, J.D.; Kugler, J.W.; Hoff, K.L.; Reddy, P.S.; et al. A Double-Blind, Placebo-Controlled Trial of a Topical Treatment for Chemotherapy-Induced Peripheral Neuropathy: NCCTG Trial N06CA. Support. Care Cancer 2011, 19, 833–841. [Google Scholar] [CrossRef]
- Boccella, S.; De Filippis, L.; Giorgio, C.; Brandolini, L.; Jones, M.; Novelli, R.; Amorizzo, E.; Leoni, M.L.G.; Terranova, G.; Maione, S.; et al. Combination Drug Therapy for the Management of Chronic Neuropathic Pain. Biomolecules 2023, 13, 1802. [Google Scholar] [CrossRef]
- Rodríguez-Palma, E.J.; Castelo-Flores, D.G.; Caram-Salas, N.L.; Salinas-Abarca, A.B.; Centurión, D.; De la Luz-Cuellar, Y.E.; Granados-Soto, V. Sex-Dependent Antiallodynic Effect of A2 Adrenergic Receptor Agonist Tizanidine in Rats with Experimental Neuropathic Pain. Eur. J. Pharmacol. 2022, 920, 174855. [Google Scholar] [CrossRef]
- Belfer, I. Pain Genetics and Personalized Spine Care. Glob. Spine J. 2014, 4, s-0034-1376743. [Google Scholar] [CrossRef]
- Kwon, M.; Kim, K.; Eum, Y.J.; Nan, G.; Kim, L.; Park, H.; Kim, U.J.; Sohn, J.H.; Cheong, C.; Cho, J.H.; et al. Sex Differences in Pain Perception and Modulation in the Brain: Effects of Insular Cortex Stimulation on Chronic Pain Relief. Brain Commun. 2025, 7, fcaf362. [Google Scholar] [CrossRef]
- Marchesini, M.; Fornasari, D.; Natoli, S.; Vegni, E.; Cuomo, A. Sex-Related Differences in Chronic Pain: A Narrative Review by a Multidisciplinary Task Force. Medicina 2025, 61, 1172. [Google Scholar] [CrossRef]
- Minett, M.S.; Falk, S.; Santana-Varela, S.; Bogdanov, Y.D.; Nassar, M.A.; Heegaard, A.M.; Wood, J.N. Pain without Nociceptors? Nav1.7-Independent Pain Mechanisms. Cell Rep. 2014, 6, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Diaz, M.M.; Caylor, J.; Strigo, I.; Lerman, I.; Henry, B.; Lopez, E.; Wallace, M.S.; Ellis, R.J.; Simmons, A.N.; Keltner, J.R. Toward Composite Pain Biomarkers of Neuropathic Pain—Focus on Peripheral Neuropathic Pain. Front. Pain Res. 2022, 3, 869215. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.