Short-Term Observation of Heart Rate and Oxygen Saturation in Relation to Masticatory Muscle Activity in Temporomandibular Disorders
Abstract
1. Introduction
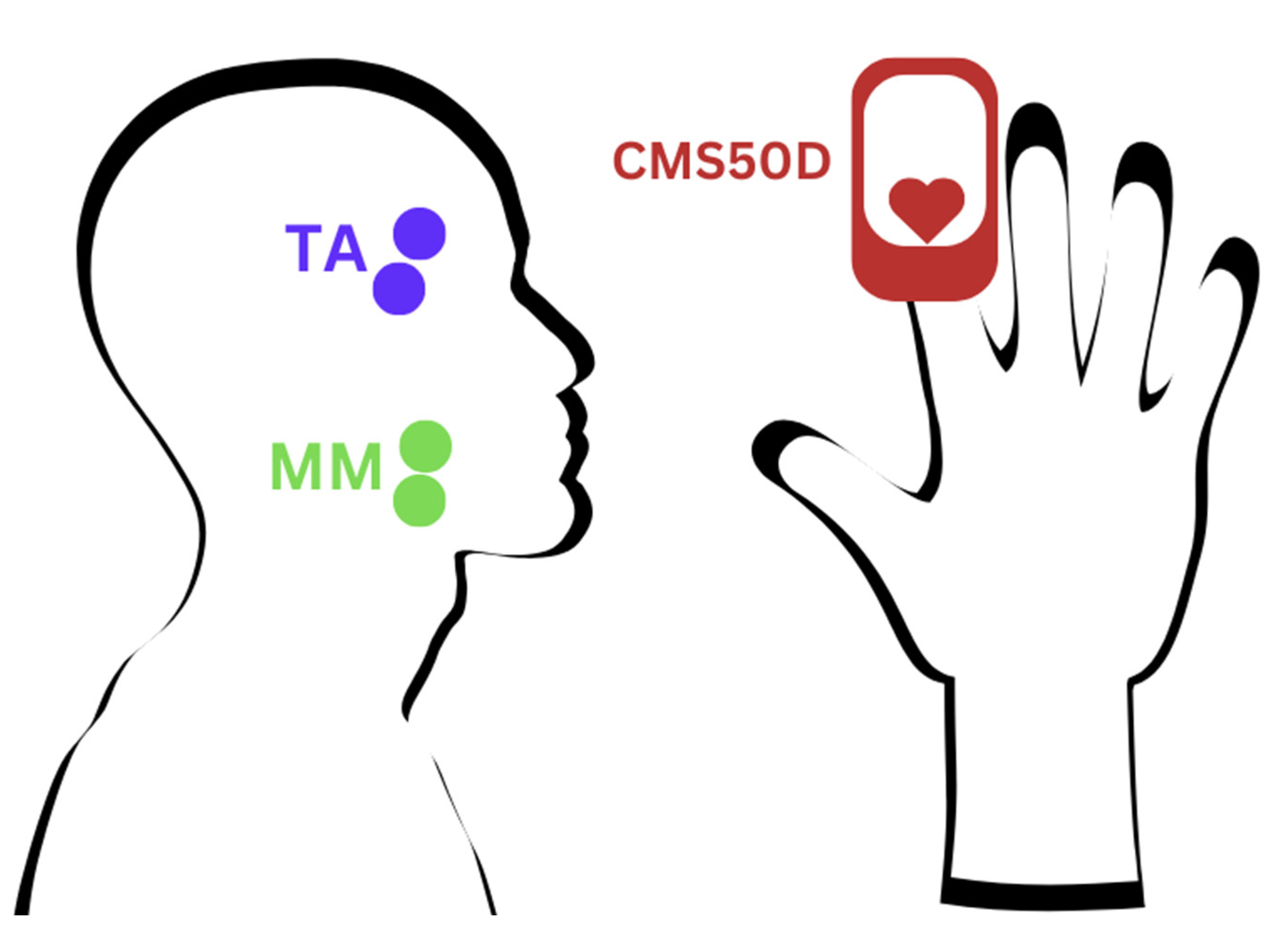
2. Materials and Methods
3. Results
4. Discussion
4.1. Interpretation of Finding
4.2. Limitations and Future Prospects
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Zieliński, G.; Pająk-Zielińska, B.; Ginszt, M. A Meta-Analysis of the Global Prevalence of Temporomandibular Disorders. J. Clin. Med. 2024, 13, 1365. [Google Scholar] [CrossRef] [PubMed]
- Warzocha, J.; Gadomska-Krasny, J.; Mrowiec, J. Etiologic Factors of Temporomandibular Disorders: A Systematic Review of Literature Containing Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) and Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) from 2018 to 2022. Healthcare 2024, 12, 575. [Google Scholar] [CrossRef]
- Zieliński, G.; Pająk-Zielińska, B.; Pająk, A.; Wójcicki, M.; Litko-Rola, M.; Ginszt, M. Global Co-Occurrence of Bruxism and Temporomandibular Disorders: A Meta-Regression Analysis. Dent. Med. Probl. 2025; online ahead of print. [Google Scholar] [CrossRef]
- Hidaka, O.; Yanagi, M.; Takada, K. Mental Stress-Induced Physiological Changes in the Human Masseter Muscle. J. Dent. Res. 2004, 83, 227–231. [Google Scholar] [CrossRef]
- Henein, M.Y.; Vancheri, S.; Longo, G.; Vancheri, F. The Impact of Mental Stress on Cardiovascular Health—Part II. J. Clin. Med. 2022, 11, 4405. [Google Scholar] [CrossRef]
- Alshak, M.N.; Das, J.M. Neuroanatomy, Sympathetic Nervous System. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Hallett, K.B.; Radford, D.J.; Seow, W.K. Oral Health of Children with Congenital Cardiac Diseases: A Controlled Study. Pediatr. Dent. 1992, 14, 224–230. [Google Scholar]
- Uğurluel, C.; Şermet Elbay, Ü.; Elbay, M.; Babaoğlu, A. Comparison of Signs and Symptoms of Temporomandibular Disorders and Parafunctions in Children with and without Cardiovascular Diseases. J. Clin. Pediatr. Dent. 2023, 47, 74–81. [Google Scholar] [CrossRef]
- Zegarowski, B. A Pilot Study of Temporomandibular Disorder (TMD) Pain and Nocturnal Autonomic Nervous System (ANS) Associated Masticatory Muscle Activity. Master’s Thesis, Oregon Health and Science University, Portland, OR, USA, 2023. [Google Scholar]
- Martynowicz, H.; Wichniak, A.; Więckiewicz, M. Sleep disorders and cardiovascular risk: Focusing on sleep fragmentation. Dent. Med. Probl. 2024, 61, 475–477. [Google Scholar] [CrossRef]
- Cutrim, R.C.; Santos-de-Araújo, A.D.; Pontes-Silva, A.; Protazio, J.B.; Anselmo-E-Silva, C.I.; Costa, C.P.S.; Gonçalves, M.C.; de Oliveira Brito Monzani, J.; de Almeida, L.V.; Filho, E.M.M.; et al. Short-Term Heart Rate Variability at Rest in Individuals with Temporomandibular Disorder: A Comparative Analysis. Clin. Oral Investig. 2023, 27, 6559–6566. [Google Scholar] [CrossRef]
- Jenzer, A.C.; Jackson, H.; Berry-Cabán, C.S. Temporomandibular Joint Pain Presentation of Myocardial Ischemia. J. Oral Maxillofac. Surg. 2018, 76, 2317.e1–2317.e2. [Google Scholar] [CrossRef]
- Greenspan, J.D.; Slade, G.D.; Bair, E.; Dubner, R.; Fillingim, R.B.; Ohrbach, R.; Knott, C.; Diatchenko, L.; Liu, Q.; Maixner, W. Pain Sensitivity and Autonomic Factors Associated With Development of TMD: The OPPERA Prospective Cohort Study. J. Pain 2013, 14, T63–T74.e6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Hasegawa, Y.; Sakagami, J.; Ono, T.; Hori, K.; Maeda, Y.; Chen, Y.-J. Effects of Unilateral Jaw Clenching on Cerebral/Systemic Circulation and Related Autonomic Nerve Activity. Physiol. Behav. 2012, 105, 292–297. [Google Scholar] [CrossRef]
- Korthuis, R.J. Exercise Hyperemia and Regulation of Tissue Oxygenation During Muscular Activity. In Skeletal Muscle Circulation; Morgan & Claypool Life Sciences: San Rafael, CA, USA, 2011. [Google Scholar]
- Noto, R.E.; Leavitt, L.; Edens, M.A. Physiology, Muscle. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Shah, N.; Melo, L.; Reid, W.D.; Cioffi, I. Masseter Deoxygenation in Adults at Risk for Temporomandibular Disorders. J. Dent. Res. 2019, 98, 666–672. [Google Scholar] [CrossRef]
- Ferreira, C.L.P.; Bellistri, G.; Montagna, S.; de Felício, C.M.; Sforza, C. Patients with Myogenic Temporomandibular Disorders Have Reduced Oxygen Extraction in the Masseter Muscle. Clin. Oral Investig. 2017, 21, 1509–1518. [Google Scholar] [CrossRef]
- Osiewicz, M.; Ciapała, B.; Bolt, K.; Kołodziej, P.; Więckiewicz, M.; Ohrbach, R. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): Polish Assessment Instruments. Dent. Med. Probl. 2024, 61, 5–8. [Google Scholar] [CrossRef]
- Warren, M.P.; Fried, J.L. Temporomandibular Disorders and Hormones in Women. Cells Tissues Organs 2001, 169, 187–192. [Google Scholar] [CrossRef]
- Zieliński, G.; Gawda, P. Surface Electromyography in Dentistry—Past, Present and Future. J. Clin. Med. 2024, 13, 1328. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of Recommendations for SEMG Sensors and Sensor Placement Procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Nishi, S.E.; Rahman, N.A.; Basri, R.; Alam, M.K.; Noor, N.F.M.; Zainal, S.A.; Husein, A. Surface Electromyography (sEMG) Activity of Masticatory Muscle (Masseter and Temporalis) with Three Different Types of Orthodontic Bracket. BioMed Res. Int. 2021, 2021, 6642254. [Google Scholar] [CrossRef]
- Smith, R.N.; Hofmeyr, R. Perioperative Comparison of the Agreement between a Portable Fingertip Pulse Oximeter v. a Conventional Bedside Pulse Oximeter in Adult Patients (COMFORT Trial). S. Afr. Med. J. Suid-Afr. Tydskr. Vir Geneeskd. 2019, 109, 154–158. [Google Scholar] [CrossRef]
- Mendonça, F.; Mostafa, S.S.; Morgado-Dias, F.; Ravelo-García, A.G. An Oximetry Based Wireless Device for Sleep Apnea Detection. Sensors 2020, 20, 888. [Google Scholar] [CrossRef] [PubMed]
- Konrad, P. The ABC of EMG A Practical Introduction to Kinesiological Electromyography; Noraxon U.S.A, Inc.: Scottsdale, AZ, USA, 2006; Available online: https://scholar.google.com/scholar_lookup?title=The+Abc+of+Emg%E2%80%94A+Practical+Introduction+to+Kinesiological+Electromyography&author=Konrad,+P.&publication_year=2005 (accessed on 8 January 2025).
- Zieliński, G.; Gawda, P. Analysis of the Use of Sample Size and Effect Size Calculations in a Temporomandibular Disorders Randomised Controlled Trial—Short Narrative Review. J. Pers. Med. 2024, 14, 655. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988; ISBN 978-0-203-77158-7. [Google Scholar]
- Eze-Nliam, C.M.; Quartana, P.J.; Quain, A.M.; Smith, M.T. Nocturnal Heart Rate Variability Is Lower in Temporomandibular Disorder Patients than in Healthy, Pain-Free Individuals. J. Orofac. Pain 2011, 25, 232–239. [Google Scholar]
- Michalek-Zrabkowska, M.; Martynowicz, H.; Wieckiewicz, M.; Smardz, J.; Poreba, R.; Mazur, G. Cardiovascular Implications of Sleep Bruxism—A Systematic Review with Narrative Summary and Future Perspectives. J. Clin. Med. 2021, 10, 2245. [Google Scholar] [CrossRef]
- Carnagarin, R.; Kiuchi, M.G.; Ho, J.K.; Matthews, V.B.; Schlaich, M.P. Sympathetic Nervous System Activation and Its Modulation: Role in Atrial Fibrillation. Front. Neurosci. 2019, 12, 1058. [Google Scholar] [CrossRef]
- DeLalio, L.J.; Sved, A.F.; Stocker, S.D. Sympathetic Nervous System Contributions to Hypertension: Updates and Therapeutic Relevance. Can. J. Cardiol. 2020, 36, 712–720. [Google Scholar] [CrossRef]
- Mulder, A.L.M.; van Golde, J.C.; Prinzen, F.W.; Blanco, C.E. Cardiac Output Distribution in Response to Hypoxia in the Chick Embryo in the Second Half of the Incubation Time. J. Physiol. 1998, 508, 281–287. [Google Scholar] [CrossRef]
- Giussani, D.A. The Fetal Brain Sparing Response to Hypoxia: Physiological Mechanisms. J. Physiol. 2016, 594, 1215–1230. [Google Scholar] [CrossRef]
- Kiyatkin, E.A. Functional Role of Peripheral Vasoconstriction: Not Only Thermoregulation but Much More. J. Integr. Neurosci. 2021, 20, 755–764. [Google Scholar] [CrossRef]
- Delong, C.; Sharma, S. Physiology, Peripheral Vascular Resistance. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538308/ (accessed on 8 January 2025).
- Cabrales, P.; Tsai, A.G.; Intaglietta, M. Balance between vasoconstriction and enhanced oxygen delivery. Transfusion 2008, 48, 2087–2095. [Google Scholar] [CrossRef]
- Amarante, E.d.L.; de Lima, J.A.S.; Bandeira, R.N.; de Moura, A.P.A.; Pessoa, L.S.d.F.; Pernambuco, L.d.A.; Alves, G.Â.d.S. Masseter Muscle Surface Electromyography in College Students with a High Degree of Anxiety and Temporomandibular Disorder. Rev. CEFAC 2018, 20, 44–52. [Google Scholar] [CrossRef][Green Version]
- Crincoli, V.; De Biase, C.; Cazzolla, A.P.; Campobasso, A.; Dioguardi, M.; Piancino, M.G.; Mattia, L.; Ribatti, D.; Di Comite, M. Effects of Contact Sports on Temporomandibular Disorders: An Observational Study. Dent. J. 2022, 10, 180. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, G.; Ginszt, M.; Zawadka, M.; Rutkowska, K.; Podstawka, Z.; Szkutnik, J.; Majcher, P.; Gawda, P. The Relationship between Stress and Masticatory Muscle Activity in Female Students. J. Clin. Med. 2021, 10, 3459. [Google Scholar] [CrossRef]
- Yoshimura, S.; Hori, K.; Uehara, F.; Hori, S.; Yamaga, Y.; Hasegawa, Y.; Akazawa, K.; Ono, T. Relationship between Body Mass Index and Masticatory Factors Evaluated with a Wearable Device. Sci. Rep. 2022, 12, 4117. [Google Scholar] [CrossRef]
- Cerda, C.; Lezcano, M.F.; Marinelli, F.; Alarcón, J.; Fuentes, R. Determination of Mandibular Position and Mouth Opening in Healthy Patients and Patients with Articular and/or Muscular Pathology: A Pilot Study with 3D Electromagnetic Articulography and Surface Electromyography. J. Clin. Med. 2023, 12, 4822. [Google Scholar] [CrossRef]
- Colonna, A.; Noveri, L.; Ferrari, M.; Bracci, A.; Manfredini, D. Electromyographic Assessment of Masseter Muscle Activity: A Proposal for a 24 h Recording Device with Preliminary Data. J. Clin. Med. 2022, 12, 247. [Google Scholar] [CrossRef]
- Zieliński, G.; Wójcicki, M.; Rapa, M.; Matysik-Woźniak, A.; Baszczowski, M.; Ginszt, M.; Litko-Rola, M.; Szkutnik, J.; Różyło-Kalinowska, I.; Rejdak, R.; et al. Masticatory Muscle Thickness and Activity Correlates to Eyeball Length, Intraocular Pressure, Retinal and Choroidal Thickness in Healthy Women versus Women with Myopia. J. Pers. Med. 2022, 12, 626. [Google Scholar] [CrossRef]
- Marin, T.; Moore, J. Understanding Near-Infrared Spectroscopy. Adv. Neonatal Care 2011, 11, 382–388. [Google Scholar] [CrossRef]
- Mizukoshi, K.; Hamanaka, Y.; Niwayama, M. Investigation of Oxygen Saturation in Regions of Skin by near Infrared Spectroscopy. Skin Res. Technol. 2022, 28, 695–702. [Google Scholar] [CrossRef]
- Cody, N.; Bradbury, I.; McMullan, R.R.; Quinn, G.; O’Neill, A.; Ward, K.; McCann, J.; McAuley, D.F.; Silversides, J.A. Physiologic Determinants of Near-Infrared Spectroscopy-Derived Cerebral and Tissue Oxygen Saturation Measurements in Critically Ill Patients. Crit. Care Explor. 2024, 6, e1094. [Google Scholar] [CrossRef]
- Stell, D.; Noble, J.J.; Kay, R.H.; Kwong, M.T.; Jeffryes, M.J.R.; Johnston, L.; Glover, G.; Akinluyi, E. Exploring the Impact of Pulse Oximeter Selection within the COVID-19 Home-Use Pulse Oximetry Pathways. BMJ Open Respir. Res. 2022, 9, e001159. [Google Scholar] [CrossRef] [PubMed]
- Chattrattrai, T.; Janal, M.N.; Lobbezoo, F.; Raphael, K.G. The Association between Sleep Bruxism and Awake Bruxism: Polysomnographic and Electromyographic Recordings in Women with and without Myofascial Pain. J. Oral Rehabil. 2023, 50, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Camparis, C.M.; Formigoni, G.; Teixeira, M.J.; Bittencourt, L.R.A.; Tufik, S.; de Siqueira, J.T.T. Sleep Bruxism and Temporomandibular Disorder: Clinical and Polysomnographic Evaluation. Arch. Oral Biol. 2006, 51, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Wieckiewicz, M.; Smardz, J.; Martynowicz, H.; Wojakowska, A.; Mazur, G.; Winocur, E. Distribution of Temporomandibular Disorders among Sleep Bruxers and Non-Bruxers-A Polysomnographic Study. J. Oral Rehabil. 2020, 47, 820–826. [Google Scholar] [CrossRef]
- Zieliński, G.; Pająk, A.; Wójcicki, M. Global Prevalence of Sleep Bruxism and Awake Bruxism in Pediatric and Adult Populations: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 4259. [Google Scholar] [CrossRef]
- Wilson, S.; Cecins, N.; Jenkins, S.; Melang, M.; Singh, B.; Hill, K. Comparing Finger and Forehead Sensors to Measure Oxygen Saturation in People with Chronic Obstructive Pulmonary Disease. Respirology 2013, 18, 1143–1147. [Google Scholar] [CrossRef]
- Kim, H.; Lee, J.; Kim, J. Electromyography-Signal-Based Muscle Fatigue Assessment for Knee Rehabilitation Monitoring Systems. Biomed. Eng. Lett. 2018, 8, 345–353. [Google Scholar] [CrossRef]

| TMDs Subjects | Healthy Subjects | Z | p | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Pain-free opening | 48 | 8 | 50 | 6 | 0.59 | 0.55 |
| Maximum unassisted opening | 51 | 6 | 50 | 6 | −0.58 | 0.56 |
| Maximum assisted opening | 54 | 6 | 53 | 6 | −1.36 | 0.17 |
| Mandibular movement to the right | 10 | 2 | 9 | 2 | −0.89 | 0.38 |
| Mandibular movement to the left | 11 | 2 | 10 | 2 | −2.99 | 0.00 |
| Protrusion | 9 | 2 | 9 | 2 | −0.83 | 0.41 |
| TMDs Subjects | Healthy Subjects | Z | p | ES | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| SpO2 (%) | 97.97 | 1.44 | 98.03 | 1.70 | −0.66 | 0.51 | 0.05 |
| HR (bpm) | 73.35 | 13.48 | 73.09 | 17.68 | 0.96 | 0.34 | 0.07 |
| TA (μV) | 2.83 | 1.95 | 2.45 | 1.59 | 1.17 | 0.24 | 0.09 |
| MM (μV) | 2.39 | 1.42 | 2.23 | 1.07 | −0.01 | 0.99 | 0.00 |
| SpO2 (%) | Mean | SD | R | t(N-2) | p | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | ||||||
| 97.99 | 1.55 | TA (μV) | 2.67 | 1.81 | 0.09 | 1.27 | 0.21 |
| MM (μV) | 2.32 | 1.28 | 0.01 | 0.10 | 0.92 | ||
| HR (bpm) | |||||||
| Mean | SD | ||||||
| 73.24 | 15.36 | TA (μV) | 2.67 | 1.81 | −0.01 | −0.18 | 0.86 |
| MM (μV) | 2.32 | 1.28 | −0.03 | −0.35 | 0.73 | ||
| R | t(N-2) | p | |
|---|---|---|---|
| SpO2 (%) | |||
| TA (μV) | 0.20 | 2.06 | 0.04 * |
| MM (μV) | 0.15 | 1.47 | 0.14 |
| HR (bpm) | |||
| TA (μV) | −0.13 | −1.36 | 0.18 |
| MM (μV) | 0.04 | 0.44 | 0.66 |
| R | t(N-2) | p | |
|---|---|---|---|
| SpO2 (%) | |||
| TA (μV) | −0.04 | −0.34 | 0.73 |
| MM (μV) | −0.22 | −1.96 | 0.05 |
| HR (bpm) | |||
| TA (μV) | 0.13 | 1.11 | 0.27 |
| MM (μV) | −0.14 | −1.23 | 0.22 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zieliński, G.; Ginszt, M.; Wójcicki, M.; Szkutnik, J.; Litko-Rola, M.; Gawda, P. Short-Term Observation of Heart Rate and Oxygen Saturation in Relation to Masticatory Muscle Activity in Temporomandibular Disorders. Brain Sci. 2025, 15, 361. https://doi.org/10.3390/brainsci15040361
Zieliński G, Ginszt M, Wójcicki M, Szkutnik J, Litko-Rola M, Gawda P. Short-Term Observation of Heart Rate and Oxygen Saturation in Relation to Masticatory Muscle Activity in Temporomandibular Disorders. Brain Sciences. 2025; 15(4):361. https://doi.org/10.3390/brainsci15040361
Chicago/Turabian StyleZieliński, Grzegorz, Michał Ginszt, Marcin Wójcicki, Jacek Szkutnik, Monika Litko-Rola, and Piotr Gawda. 2025. "Short-Term Observation of Heart Rate and Oxygen Saturation in Relation to Masticatory Muscle Activity in Temporomandibular Disorders" Brain Sciences 15, no. 4: 361. https://doi.org/10.3390/brainsci15040361
APA StyleZieliński, G., Ginszt, M., Wójcicki, M., Szkutnik, J., Litko-Rola, M., & Gawda, P. (2025). Short-Term Observation of Heart Rate and Oxygen Saturation in Relation to Masticatory Muscle Activity in Temporomandibular Disorders. Brain Sciences, 15(4), 361. https://doi.org/10.3390/brainsci15040361








