Three-Dimensional, Image-Based Evaluation of the L5 Vertebral Body and Its Ossification Center in Human Fetuses
Abstract
1. Introduction
- To quantify linear, surface, and volumetric parameters across different gestational ages and establish reference values;
- To assess potential sex-related differences;
- To determine the growth dynamics and develop mathematical models that best describe the observed relationships.
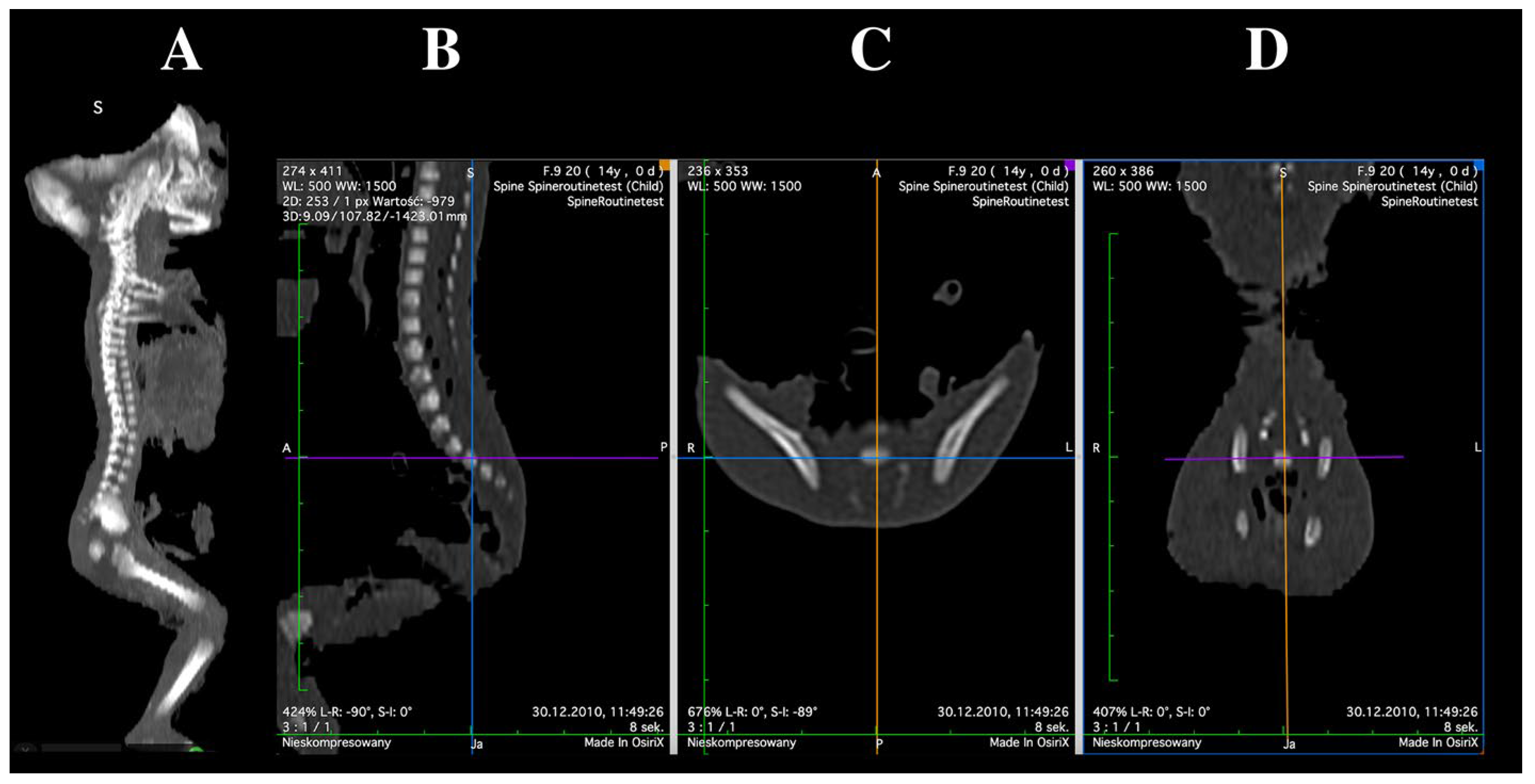
2. Materials and Methods
2.1. Examined Sample
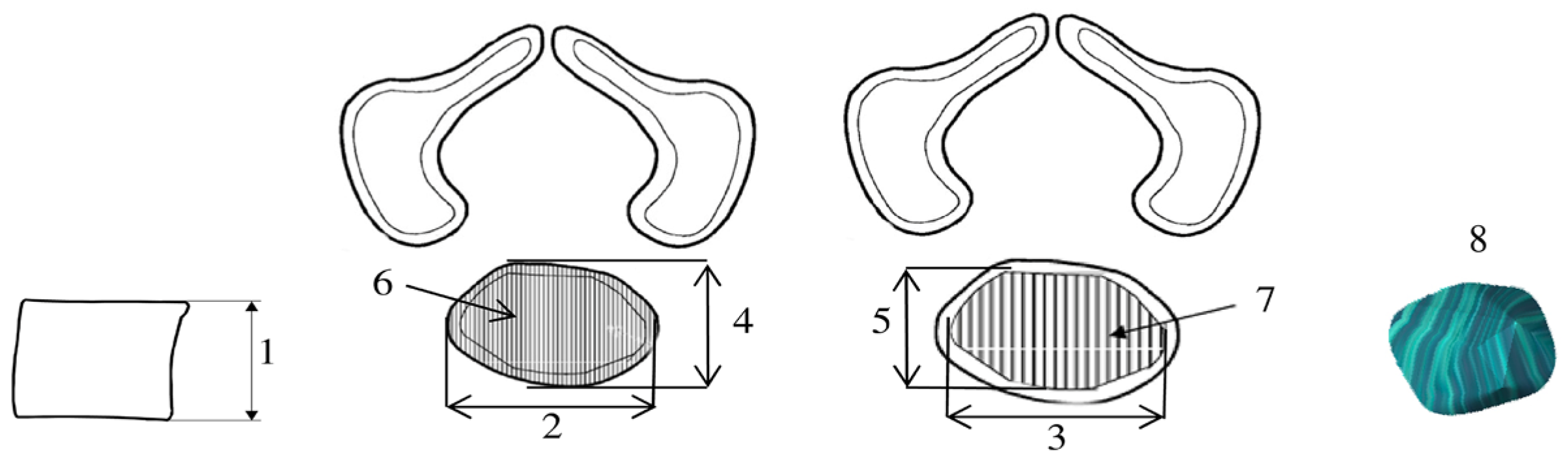
2.2. Morphometric Measurements
- Vertebral body height—the maximum distance between the superior and inferior borders of the vertebral body in the sagittal plane;
- Transverse diameter of vertebral body—the maximum distance between the lateral edges of the vertebral body in the transverse plane;
- Transverse diameter of body ossification center—the maximum distance between the lateral edges of the ossification center in the transverse plane;
- Sagittal diameter of vertebral body—the maximum distance between the anterior and posterior borders of the vertebral body in the sagittal plane;
- Sagittal diameter of body ossification center—the maximum distance between the anterior and posterior borders of the ossification center in the sagittal plane;
- Cross-sectional area of vertebral body—the area determined based on the contour of the vertebral body in the transverse plane;
- Cross-sectional area of body ossification center—the area determined based on the contour of the ossification center in the transverse plane;
- Volume of the ossification center—calculated using three-dimensional reconstruction software(OsiriX MD 3.9), taking into account spatial orientation and X-ray attenuation properties of the mineralizing tissue.
2.3. Statistical Analysis
3. Results
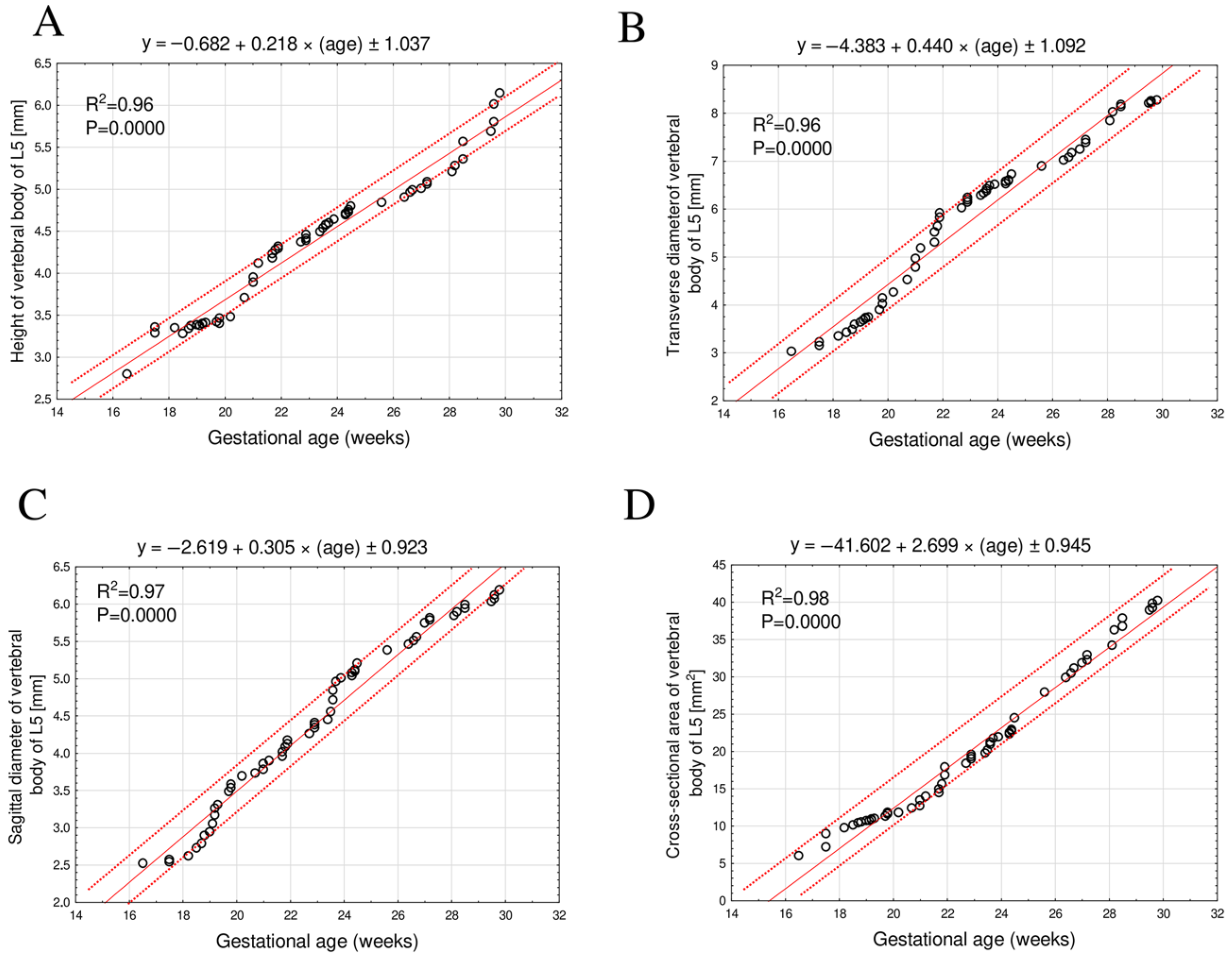
3.1. Morphometric Parameters of the L5 Vertebral Body
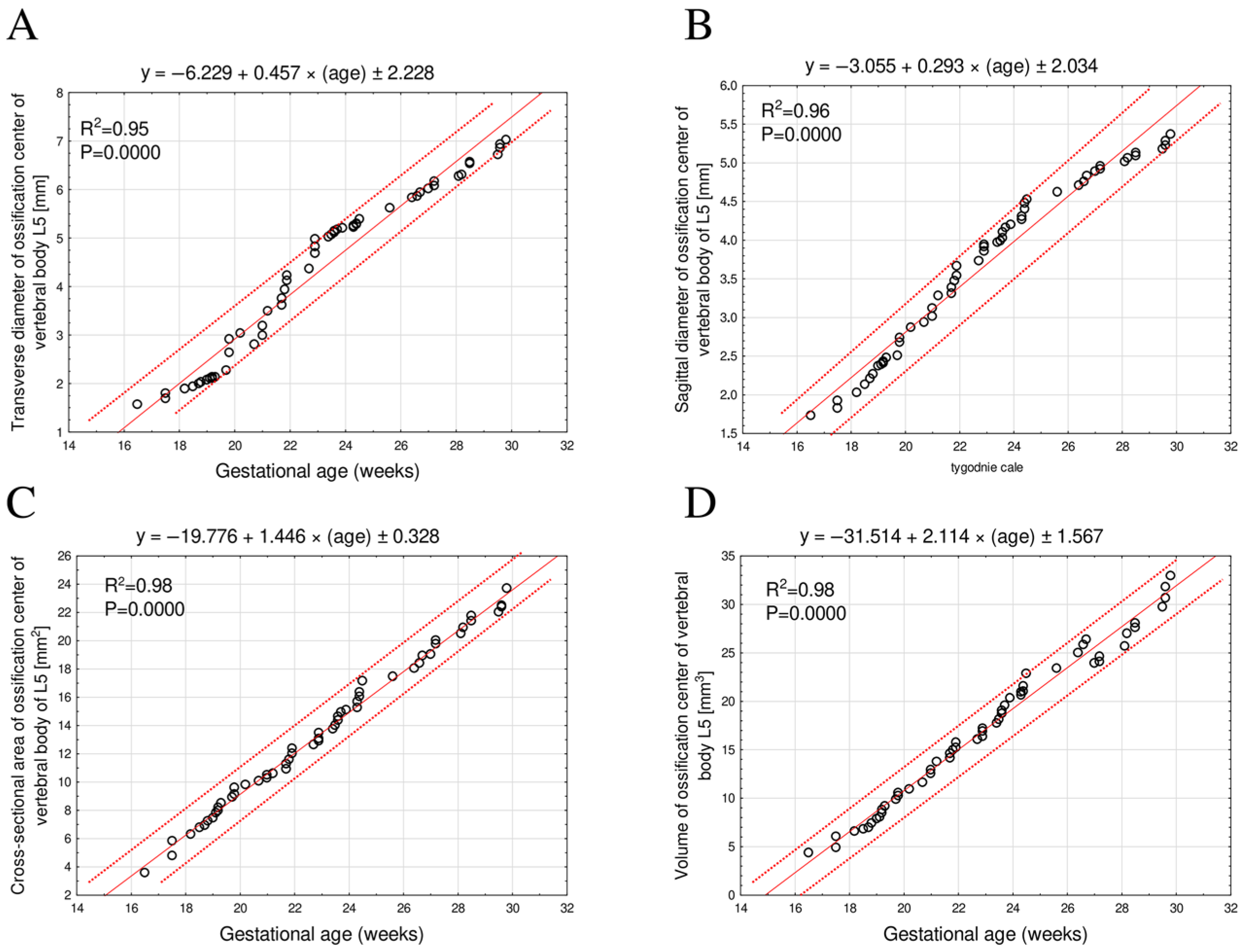
3.2. Morphometric Parameters of the L5 Ossification Center
4. Discussion
Limitations of the Study
5. Conclusions
- No sex-related differences were observed in any of the morphometric parameters of the L5 vertebral body or its ossification center.
- All analyzed morphometric parameters of the L5 vertebral body and its ossification center increased proportionally with gestational age expressed in weeks.
- The morphometric data obtained for the L5 vertebral body and its ossification center may serve as gestational age–dependent reference values, supporting fetal age assessment and ultrasound-based diagnosis of congenital anomalies. Further research on the growth patterns and morphometric characteristics of the L5 vertebra is warranted to deepen our understanding of its development and potential clinical significance.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gorincour, G.; Chaumoitre, K.; Bourliere-Najean, B.; Bretelle, F.; Sigaudy, S.; D’Ercole, C.; Philip, N.; Potier, A.; Petit, P.; Panuel, M. Fetal skeletal computed tomography: When? How? Why? Diagn. Interv. Imaging. 2014, 95, 1045–1053. [Google Scholar] [CrossRef]
- Grzonkowska, M.; Bogacz, K.; Żytkowski, A.; Szkultecka-Dębek, M.; Kułakowski, M.; Janiak, M.; Rogalska, A.; Baumgart, M. Digital Image Analysis of Vertebral Body S1 and Its Ossification Center in the Human Fetus. Brain Sci. 2025, 15, 74. [Google Scholar] [CrossRef]
- Wldjaja, E.; Whitby, E.H.; Paley, M.N.; Griffiths, P.D. Normal fetal lumbar spine on postmortem imaging. Am. J. Neuroradiol. 2006, 27, 553–559. [Google Scholar] [PubMed]
- Kaplan, K.M.; Spivak, J.M.; Bendo, J.A. Embryology of the spine and associated congenital abnormalities. Spine J. 2005, 5, 564–576. [Google Scholar] [CrossRef]
- Tsoupras, A.; Dayer, R.; Tabard-Fougère, A.; Faundez, A. Vertebral tethering’s effect on lumbar spine development in adolescent patients with sacralization of L5: A comparative case–control study. Eur. Spine J. 2025, 34, 1–8, Online ahead of printing. [Google Scholar] [CrossRef] [PubMed]
- Skórzewska, A.; Grzymisławska, M.; Bruska, M.; Łupicka, J.; Woźniak, W. Ossification of the vertebral column in human foetuses: Histological and computed tomography studies. Folia Morphol. 2013, 72, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Bach, P.; Cassart, M.; Chami, M.; Garel, C.; Panuel, M. Exploration of the fetal skeleton by ultra-low-dose computed tomography: Guidelines from the fetal imaging task force of the european society of paediatric radiology. Pediatr. Radiol. 2023, 53, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Simcock, I.C.; Shelmerdine, S.C.; Langan, D.; Anna, G.; Sebire, N.J.; Arthurs, O.J. Micro-CT yields high image quality in human fetal post-mortem imaging despite maceration. BMC Med. Imaging 2021, 21, 128. [Google Scholar] [CrossRef]
- Simcock, I.C.; Arthurs, O.J.; Hutchinson, J.C.; Sebire, N.J.; Jacques, T.S.; Sekar, T.; Shelmerdine, S.C. Impact of non-invasive post-mortem micro-CT imaging on a fetal autopsy service: A single centre retrospective study. Clin. Radiol. 2024, 79, 791–798. [Google Scholar] [CrossRef]
- Dawood, Y.; Honhoff, C.; van der Post, A.-S.; Roosendaal, S.D.; Coolen, B.F.; Strijkers, G.Y.; Pajkrt, E.; de Bakker, B.S. Comparison of postmortem whole-body contrast-enhanced microfocus computed tomography and high-field magnetic resonance imaging of human fetuses. Ultrasound Obstet. Gynecol. 2022, 60, 109–117. [Google Scholar] [CrossRef]
- Winkelmann, C.T.; Wise, L.D. High-throughput micro-computed tomography imaging as a method to evaluate rat and rabbit fetal skeletal abnormalities for developmental toxicity studies. J. Pharmacol. Toxicol. Methods. 2009, 59, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Docter, D.; Dawood, Y.; Jacobs, K.; Hagoort, J.; Oostra, R.J.; van den Hoff, M.J.B.; Arthurs, O.J.; de Bakker, B.S. Microfocus computed tomography for fetal postmortem imaging: An overview. Pediatr. Radiol. 2023, 53, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Waratani, M.; Ito, F.; Tanaka, Y.; Mabuchi, A.; Mori, T.; Kitawaki, J. Prenatal diagnosis of fetal skeletal dysplasia using 3-dimensional computed tomography: A prospective study. BMC Musculoskelet. Disord. 2020, 8, 662. [Google Scholar] [CrossRef]
- Szpinda, M.; Baumgart, M.; Szpinda, A.; Woźniak, A.; Mila-Kierzenkowska, C. New patterns of the growing L3 vertebra and its 3 ossification centers in human fetuses—A CT, digital, and statistical study. Med. Sci. Monit. Basic. Res. 2013, 19, 169–180. [Google Scholar] [CrossRef][Green Version]
- Baumgart, M.; Grzonkowska, M.; Kułakowski, M. Digital image analysis of vertebral body L4 and its ossification centre in the human foetus. Folia Morphol. 2025, 84, 406–417. [Google Scholar] [CrossRef]
- Bhat, N.; Rao, L.; Shetty, A.; Das, S.; Naik, N.B.K.; Nayak, V.; Prabhath, S.; Alapatt, K.; Sumalatha, S. Morphometric analysis of the fifth lumbar vertebra (L5): Anatomical dimensions and clinical implications in South Indian population. Transl. Res. Anat. 2025, 39, 100392. [Google Scholar] [CrossRef]
- Chano, T.; Matsumoto, K.; Ishizawa, M.; Morimoto, S.; Hukuda, S.; Okabe, H.; Kato, H.; Fujino, S. Analysis of the presence of osteocalcin, S-100 protein, and proliferating cell nuclear antigen in cells of various types of osteosarcomas. Eur. J. Histochem. 1996, 40, 189–198. [Google Scholar] [PubMed]
- Duarte, W.R.; Shibata, T.; Takenaga, K.; Takahashi, E.; Kubota, K.; Ohya, K.; Ishikawa, I.; Yamauchi, M.; Kasugai, S. S100A4: A novel negative regulator of mineralization and osteoblast differentiation. J. Bone Miner. Res. 2003, 18, 493–501. [Google Scholar] [CrossRef]
- Czyż, M.; Kędzia, A. Geometrical assessment of the foetal lumbar vertebral column—Clinical implications. Folia Morphol. 2004, 63, 431–438. [Google Scholar]
- Sagi, H.C.; Jarvis, J.G.; Uhthoff, H.K. Histomorphic analysis of the development of the pars interarticularis and its association with isthmic spondylosis. Spine 1998, 23, 1635–1639; discussion 1640. [Google Scholar] [CrossRef]
- Kim, J.K.; Chang, M.C.; Park, W.T.; Lee, G.W. Identification of L5 vertebra on lumbar spine radiographs using deep learning. J. Int. Med. Res. 2024, 52, 03000605231223881. [Google Scholar] [CrossRef] [PubMed]
- Sabnis, A.; Nakhate, M. A study of prevalence of sacralization of L5 vertebra. Int. J. Anat. Res. 2020, 8, 7399–7402. [Google Scholar] [CrossRef]
- Szpinda, M.; Baumgart, M.; Szpinda, A.; Woźniak, A.; Mila-Kierzenkowska, C. Cross-sectional study of C1-S5 vertebral bodies in human fetuses. Med. Sci. Monit. Basic. Res. 2015, 11, 174–189. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Yuan, X.; Peng, Z.; Jian, N.; Tian, M.; Feng, X.; Lin, X.; Wang, X. Normal fetal development of the cervical, thoracic, and lumbar spine: A postmortem study based on magnetic resonance imaging. Prenat. Diagn. 2021, 41, 989–997. [Google Scholar] [CrossRef]
- De Biasio, P.; Ginocchio, G.; Aicardi, G.; Ravera, G.; Venturini, P.L.; Vignolo, M. Ossification timing of sacra vertebrae by ultrasound in the mid-second trimester of pregnancy. Prenat. Diagn. 2003, 23, 1056–1059. [Google Scholar] [CrossRef]
- Macé, G.; Sonigo, P.; Cormier-Daire, V.; Aubry, M.C.; Martinovic, J.; Elie, C.; Gonzales, M.; Carbonne, B.; Dumez, Y.; Le Merrer, M.; et al. Three-dimensional helical computed tomography in prenatal diagnosis of fetal skeletal dysplasia. Ultrasound Obstet. Gynecol. 2013, 42, 161–168. [Google Scholar] [CrossRef]
- Victoria, T.; Epelman, M.; Coleman, B.G.; Horii, S.C.; Oliver, E.R.; Mahboubi, S.; Khalek, N.; Kasperski, S.; Edgar, J.C.; Jaramillo, D. Low-dose fetal CT in the prenatal evaluation of skeletal dysplasias and other severe skeletal abnormalities. Am. J. Roentgenol. 2013, 200, 989–1000. [Google Scholar] [CrossRef]
- Nemec, U.; Nemec, S.F.; Krakow, D.; Brugger, P.C.; Malinger, G.; Graham, J.M., Jr.; Rimoin, D.L.; Prayer, D. The skeleton and musculature on foetal MRI. Insights Imaging 2011, 2, 309–318. [Google Scholar] [CrossRef][Green Version]
- Gottlieb, A.G.; Galan, H.L. Nontraditional sonographic pearls in estimating gestational age. Semin. Perinatol. 2008, 32, 154–160. [Google Scholar] [CrossRef]
- Salomon, L.J.; Alfirevic, Z.; Da Silva Costa, F.; Deter, R.L.; Figueras, F.; Ghi, T.; Glanc, P.; Khalil, A.; Lee, W.; Napolitano, R.; et al. ISUOG Practice Guidelines: Ultrasound assessment of fetal biometry and growth. Ultrasound Obstet. Gynecol. 2019, 53, 715–723. [Google Scholar] [CrossRef]
- Lees, C.C.; Stampalija, T.; Baschat, A.A.; Da Silva Costa, F.; Ferrazzi, E.; Figueras, F.; Hecher, K.; Kingdom, J.; Poon, L.C.; Salomon, L.J.; et al. ISUOG Practice Guidelines: Diagnosis and management of small-for-gestational-age fetus and fetal growth restriction. Ultrasound Obstet. Gynecol. 2020, 56, 298–312. [Google Scholar] [CrossRef]
- Onn-Margalit, L.; Weissbach, T.; Gafner, M.; Fried, S.; Wandel, A.; Ziv-Baran, T.; Katorza, E. An association between fetal subarachnoid space and various pathologies using MR imaging. Diagnostics 2024, 14, 2535. [Google Scholar] [CrossRef]
| Gestational Age | Crown-Rump Length (mm) | Number of Fetuses | Sex | ||||
|---|---|---|---|---|---|---|---|
| Weeks (Hbd-Life) | Mean | SD | Min. | Max. | ♂ | ♀ | |
| 17 | 115.00 | - | 115.00 | 115.00 | 1 | 0 | 1 |
| 18 | 133.33 | 5.77 | 130.00 | 140.00 | 3 | 1 | 2 |
| 19 | 149.50 | 3.82 | 143.00 | 154.00 | 8 | 3 | 5 |
| 20 | 161.00 | 2.71 | 159.00 | 165.00 | 4 | 2 | 2 |
| 21 | 174.75 | 2.87 | 171.00 | 178.00 | 4 | 3 | 1 |
| 22 | 185.00 | 1.41 | 183.00 | 186.00 | 4 | 1 | 3 |
| 23 | 197.60 | 2.61 | 195.00 | 202.00 | 5 | 2 | 3 |
| 24 | 208.67 | 3.81 | 204.00 | 213.00 | 9 | 5 | 4 |
| 25 | 214.00 | - | 214.00 | 214.00 | 1 | 0 | 1 |
| 26 | 229.00 | 5.66 | 225.00 | 233.00 | 2 | 1 | 1 |
| 27 | 237.50 | 3.33 | 233.00 | 241.00 | 6 | 6 | 0 |
| 28 | 249.50 | 0.71 | 249.00 | 250.00 | 2 | 0 | 2 |
| 29 | 253.00 | 0.00 | 253.00 | 253.00 | 2 | 0 | 2 |
| 30 | 263.25 | 1.26 | 262.00 | 265.00 | 4 | 3 | 1 |
| Total | 55 | 27 | 28 | ||||
| Parameters of the L5 Vertebral Body | ICC |
|---|---|
| Height | 0.994 * |
| Transverse diameter | 0.994 * |
| Sagittal diameter | 0.996 * |
| Cross-sectional area | 0.997 * |
| Parameters of the ossification center of the L5 vertebral body | |
| Transverse diameter | 0.996 * |
| Sagittal diameter | 0.997 * |
| Cross-sectional area | 0.997 |
| Volume | 0.9937 |
| Gestational Age (Weeks) | N | Vertebral Body L5 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Height (mm) | Transverse Diameter (mm) | Sagittal Diameter (mm) | Cross-Sectional Area (mm2) | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| 17 | 1 | 2.80 | 3.02 | 2.52 | 6.04 | ||||
| 18 | 3 | 3.33 | 0.04 | 3.24 | 0.10 | 2.58 | 0.04 | 8.66 | 1.30 |
| 19 | 8 | 3.37 | 0.04 | 3.63 | 0.12 | 3.02 | 0.22 | 10.67 | 0.29 |
| 20 | 4 | 3.44 | 0.04 | 4.08 | 0.16 | 3.57 | 0.09 | 11.62 | 0.25 |
| 21 | 4 | 3.92 | 0.17 | 4.86 | 0.28 | 3.82 | 0.08 | 13.12 | 0.70 |
| 22 | 5 | 4.26 | 0.05 | 5.64 | 0.24 | 4.07 | 0.08 | 15.94 | 1.42 |
| 23 | 5 | 4.42 | 0.05 | 6.17 | 0.10 | 4.37 | 0.07 | 19.21 | 0.52 |
| 24 | 9 | 4.65 | 0.08 | 6.49 | 0.10 | 4.94 | 0.19 | 21.82 | 0.91 |
| 25 | 1 | 4.80 | 6.72 | 5.20 | 24.46 | ||||
| 26 | 2 | 4.87 | 0.04 | 6.96 | 0.09 | 5.42 | 0.06 | 28.86 | 1.40 |
| 27 | 5 | 5.02 | 0.05 | 7.26 | 0.15 | 5.68 | 0.14 | 31.73 | 0.97 |
| 28 | 2 | 5.25 | 0.05 | 7.93 | 0.13 | 5.87 | 0.04 | 35.20 | 1.46 |
| 29 | 2 | 5.47 | 0.15 | 8.16 | 0.04 | 5.97 | 0.04 | 37.32 | 0.76 |
| 30 | 4 | 5.91 | 0.20 | 8.24 | 0.03 | 6.10 | 0.07 | 39.54 | 0.58 |
| Gestational Age (Weeks) | N | Ossification Center L5 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Transverse Diameter (mm) | Sagittal Diameter (mm) | Cross-Sectional Area (mm2) | Volume (mm3) | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| 17 | 1 | 1.56 | 1.73 | 3.60 | 4.36 | ||||
| 18 | 3 | 1.79 | 0.10 | 1.93 | 0.10 | 5.64 | 0.77 | 5.84 | 0.84 |
| 19 | 8 | 2.06 | 0.07 | 2.34 | 0.12 | 7.62 | 0.62 | 7.96 | 0.85 |
| 20 | 4 | 2.71 | 0.34 | 2.70 | 0.15 | 9.39 | 0.41 | 10.38 | 0.45 |
| 21 | 4 | 3.12 | 0.29 | 3.09 | 0.15 | 10.36 | 0.25 | 12.73 | 0.86 |
| 22 | 5 | 3.93 | 0.26 | 3.47 | 0.14 | 11.64 | 0.57 | 14.94 | 0.59 |
| 23 | 5 | 4.77 | 0.26 | 3.88 | 0.09 | 13.16 | 0.44 | 16.86 | 0.66 |
| 24 | 9 | 5.19 | 0.08 | 4.22 | 0.16 | 15.16 | 0.77 | 20.00 | 1.19 |
| 25 | 1 | 5.39 | 4.53 | 17.13 | 22.89 | ||||
| 26 | 2 | 5.73 | 0.15 | 4.67 | 0.06 | 17.76 | 0.39 | 24.20 | 1.11 |
| 27 | 5 | 6.01 | 0.12 | 4.87 | 0.08 | 19.23 | 0.64 | 24.97 | 1.06 |
| 28 | 2 | 6.29 | 0.03 | 5.04 | 0.04 | 20.73 | 0.30 | 26.33 | 0.88 |
| 29 | 2 | 6.55 | 0.03 | 5.11 | 0.03 | 21.56 | 0.27 | 27.81 | 0.32 |
| 30 | 4 | 6.88 | 0.13 | 5.27 | 0.08 | 22.64 | 0.73 | 31.28 | 1.42 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grzonkowska, M.; Kułakowski, M.; Elster, K.; Dzięcioł-Anikiej, Z.; Zwierko, B.; Kierońska-Siwak, S.; Konieczna-Brazis, M.; Banasiak, M.; Orkisz, S.; Baumgart, M. Three-Dimensional, Image-Based Evaluation of the L5 Vertebral Body and Its Ossification Center in Human Fetuses. Brain Sci. 2025, 15, 1229. https://doi.org/10.3390/brainsci15111229
Grzonkowska M, Kułakowski M, Elster K, Dzięcioł-Anikiej Z, Zwierko B, Kierońska-Siwak S, Konieczna-Brazis M, Banasiak M, Orkisz S, Baumgart M. Three-Dimensional, Image-Based Evaluation of the L5 Vertebral Body and Its Ossification Center in Human Fetuses. Brain Sciences. 2025; 15(11):1229. https://doi.org/10.3390/brainsci15111229
Chicago/Turabian StyleGrzonkowska, Magdalena, Michał Kułakowski, Karol Elster, Zofia Dzięcioł-Anikiej, Beata Zwierko, Sara Kierońska-Siwak, Magdalena Konieczna-Brazis, Michał Banasiak, Stanisław Orkisz, and Mariusz Baumgart. 2025. "Three-Dimensional, Image-Based Evaluation of the L5 Vertebral Body and Its Ossification Center in Human Fetuses" Brain Sciences 15, no. 11: 1229. https://doi.org/10.3390/brainsci15111229
APA StyleGrzonkowska, M., Kułakowski, M., Elster, K., Dzięcioł-Anikiej, Z., Zwierko, B., Kierońska-Siwak, S., Konieczna-Brazis, M., Banasiak, M., Orkisz, S., & Baumgart, M. (2025). Three-Dimensional, Image-Based Evaluation of the L5 Vertebral Body and Its Ossification Center in Human Fetuses. Brain Sciences, 15(11), 1229. https://doi.org/10.3390/brainsci15111229





