Abstract
Reducing the effect of leg length discrepancy (LLD) on gait abnormalities while other abnormal conditions such as spasticity, joint contractures or weak muscle strength are exhibited is challenging. This study aimed to evaluate the impact of mild LLD on lower limb biomechanics, on participants with anatomic LLD with and without other clinical abnormalities. A motion capture system was utilized on 32 participants to measure lower limb kinematics and dynamic leg length (DLL) throughout the gait cycle, calculated as the absolute distance from the hip joint center, either to the heel, ankle joint center, or forefoot. The Pearson correlation coefficient found that LLD was associated with 5 kinematic variables only when LLD appeared with no other clinical abnormalities present (r = 0.574 – 0.846, p < 0.05). When clinical abnormalities were present, the random forest classification accuracy was lower (64% versus 80%), implying that the used kinematics are low predictors for anatomic LLD, revealing a higher asymmetrical clearance index (the difference between the maximal stance phase and the minimal contra-lateral swing phase DLL) and a different kinematic variable importance index. Clinical abnormalities in pathological gait will in all probability significantly affect gait deviations, affirming mild anatomic LLD as inconsequential. A functional measurement can offer a better estimate as to the side and extent of the functional discrepancy.
1. Introduction
Leg length discrepancy (LLD), a common orthopedic condition, may be present either due to structural deformities originating from true bony leg length differences [1], or functional deformities originating from abnormal lower limb biomechanics [2] resulting from musculoskeletal abnormalities—such as joint contracture, static or dynamic mechanical axis malalignment, muscle weakness or muscular-tendon shortening.
Recent studies have reported that gait deviations occur when LLD is <2 cm (hereafter, mild LLD) [3,4,5]; others have reported LLD as slight as 5–10 mm [6,7]. Two main methodologies evaluating gait asymmetry as a result of LLD have been described in the literature. The subjects either existed anatomical LLD [8,9] or LLD was acutely simulated with a shoe or heel lift in subjects assumed to have anatomically equal leg lengths [3,7]. Eek et al. assessed the impact of mild LLD on pathological gait deviations by correcting gait deviations using a sole lift of 12 mm among children diagnosed with spastic cerebral palsy diplegia and a relatively mild LLD of 16 mm (range 10–28) [5].
Several studies have found that LLD is compensated by dynamic strategies aimed at achieving functional equalizations [1,3,7,8], primarily when clearing the foot of the longer lower limb off the ground during the swing phase. Compensatory gait deviations can occur simultaneously in both the longer and shorter lower limb. Compensation of the shorter lower limb during the stance phase functionally elongates the limb by increasing hip and knee extension and ankle plantar flexion, whereas the longer leg utilizes deviations that functionally shorten the lower limb during the stance and swing phase with opposite kinematic deviations. According to the presence of the above asymmetric kinematic deviations, an anatomic LLD may be assumed. When assessing patients displaying neuromusculoskeletal abnormalities and exhibiting pathological gait deviations, additional clinical abnormalities such as spasticity, weak muscle strength and joint contracture deformities will either contribute to their functional LLD or limit their ability to compensate for anatomical LLD. Accordingly, the ability to measure the effect of LLD or to determine the lift height needed for correcting gait deviations is difficult. No attempt has been made to assess the impact of mild LLD on gait deviations in patients with pathological gait and its relationship to clinical abnormalities that might be present.
The primary aim of this study was to analyze kinematical asymmetry of patients with mild LLD with and without other clinical abnormalities and compare the impact of LLD on their gait deviations. The secondary aim was to assess and quantify functional discrepancy based on dynamic leg length (DLL) measurements [7,10,11]. We hypothesized that patients with only LLD would achieve dynamic equalization with asymmetric kinematics by functionally shortening the longer side, and lengthening the shorter side, respectively. However, for patients with other abnormalities, LLD would not correlate with kinematic asymmetry due to their clinical abnormalities, and they would have a higher asymmetrical DLL, i.e., higher functional discrepancies.
2. Materials and Methods
2.1. Participants
Thirty-two participants with gait deviations and LLD diagnosed by an orthopedic surgeon (using direct tape measurement) [12] were included in the study and evaluated to determine the need for a corrective heel or shoe lift. Participants were divided into two groups: Group A comprised 15 participants, average age—27 years (SD 13), mass—62 kg (SD 13) and height—169 cm (SD 13). No clinical findings known to affect their gait pattern were found in their musculoskeletal assessment. In Group A participants were diagnosed with idiopathic or post trauma LLD (n = 8), bladder exstrophy without osteotomy (n = 3), unilateral tibia vara (n = 2), Perthes’ disease (n = 1) or in-toeing gait (n = 1). Group B comprised 17 participants, average age—25 years (SD 14), mass—58 kg (SD 15) and height—160 cm (SD 10) exhibiting clinical abnormalities in their musculoskeletal assessment such as joint contractures, decreased muscle-tendon length or weak muscle strength. Diagnoses and clinical abnormalities for participants in group B are presented in Table 1. Participants of both groups had not undergone surgery, nor have they suffered any injury during the previous year; all were capable of ambulating without an assistive device and were able to walk independently in and outdoors.

Table 1.
Diagnoses and clinical abnormalities among participants in Group B.
2.2. Procedure
Gait data were recorded by a three-dimensional motion analysis system (Vicon®, Oxford Metrics, Oxford, UK), according to the PlugInGait model (PGM) [13], to measure gait deviations of the pelvis and lower extremities with a sampling rate of 120 Hz. Thirteen reflective passive skin markers were placed on the subject’s pelvis and lower limbs according to the PGM protocol. Heel and forefoot markers were also placed according to the PGM protocol [14]. A custom foot alignment device with a cross-hair laser, based on the novel device described by Wervey and Schwartz, was used to ensure proper placement of the lateral malleolus, heel and forefoot markers [15]. Participants walked barefoot at their own self-selected speed. Six gait cycles were chosen for further analysis.
Lower limb X-rays for measuring anatomic LLD were performed either by a standing calibrated X-ray using a 2.54 cm metal ball and TraumaCad® software which provided the investigator with a full set of wizards, digital measurement tools and on-screen images [16] or by supine CT scanograms. Femur length was measured from the proximal aspect of the femoral head to the distal end of the femoral condyle; tibia length was measured from the tibia plateau to the tibia plafond. All X-ray measurements were performed by an experienced physician specialized in radiographic measurements. Each group was then divided into two additional subgroups according to their anatomic LLD findings (a longer right or left lower limb). The study was approved by the Medical Center’s Ethics Committee.
Clinical evaluation was performed by the main investigator encompassing lower limb joint range of motion (ROM) and muscle-tendon length by employing a plastic goniometer, manual muscle testing [17] and muscle tone assessment with the Modified Ashworth Scale [18], when relevant.
2.3. Data Reduction and Analysis
We analyzed maximal values of the following joint kinematics at defined events of the gait cycle: frontal plane pelvic obliquity during mid-stance and mid-swing phases, hip flexion-extension during initial contact, terminal stance and mid-swing phases, hip adduction-abduction during mid-swing phase, knee flexion-extension and ankle dorsi-plantar flexion during initial contact, mid-stance, terminal stance and mid-swing phases and ankle dorsi-plantar flexion during foot off (Table 2).

Table 2.
Maximal joint kinematic values analyzed at defined gait events.
These values were chosen as they have been previously found to dynamically compensate for LLD [1,3,7,8], by a significant difference in kinematical angles measured on the longer versus the shorter lower limb. Thus, kinematic asymmetry was assessed by calculating the difference between the longer and shorter lower limb’s kinematic angles. Gait variables were normalized at 51 data points.
Throughout the gait cycle, the functional leg length was measured by three separate DLLs, measuring the distance from the hip joint center to the heel marker (HDLL), to the ankle joint center (ADDL) and to the forefoot marker (FDLL) [7,10,11] respectively (Figure 1). The PGM ascertained the virtual trajectories of the hip and ankle joint centers.
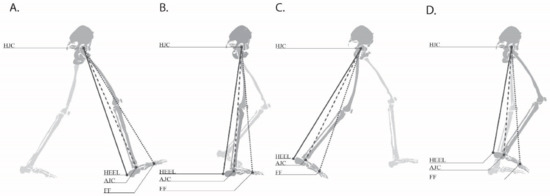
Figure 1.
DLLs during the gait cycle phases measured from hip joint center (HJC) to the heel marker (HEEL), to the ankle joint center (AJC) and to the forefoot marker (FF) ((A) initial contact, (B) mid stance, (C) pre-swing, (D) mid swing).
Clearance index was defined as the difference between the maximal DLLs measured during stance phase (right or left) and the minimal DLLs measured during the contralateral swing phase (left or right) [7]. Mid to terminal stance was defined as the stance phase; mid-swing was defined as the swing phase. These values are most critical in the gait cycle where the maximal functional leg length during stance is required to clear the contralateral side while the minimal functional length during the swing phase is required to clear the foot off the ground. A higher index value occurs during the longer limb swing phase due to excessive functional shortening and/or functional elongation of the shorter limb during the stance phase [7]. A lower index value may be present due to excessive functional shortening of the longer limb during the stance phase and/or decreased functional shortening of the shorter limb during the swing phase [7]. Thus, the clearance index allows quantifying the functional discrepancy, which is the difference between the right and left clearance index. The clearance index was identified according to the side of the swing limb and was found to be symmetrical among the 40 healthy participants evaluated in the same gait laboratory (Figure 2) [7,11].
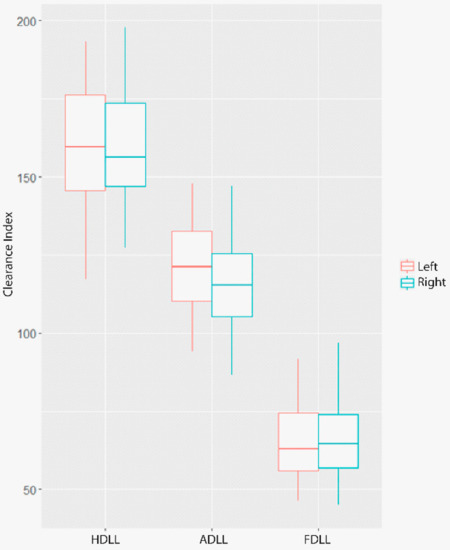
Figure 2.
A boxplot representation of the differences (in mm) between maximal DLLs throughout the stance phase and the contralateral minimal DLLs throughout the swing phase among 40 healthy controls from prior analysis made in the same gait laboratory.
2.4. Statistical Analysis and Interpretation
The relationship between LLD and kinematic asymmetry was evaluated by the Pearson product-moment asymmetry. Kinematic asymmetry was defined as the difference between the longer and shorter lower limbs’ kinematical angles at the predefined gait event (Table 2). To evaluate the relationship between anatomic LLD and their kinematics in both groups, and to point out the kinematics that are most correlated with anatomic LLD, we fitted a random forest model for supervised classification to each group separately. Groups A and B were classified into subgroups according to whether the individual exhibited a longer anatomic left or right lower limb, based on a set of predictor variables (gait kinematics). Subsequently, we used the random forest algorithm to extract the variable importance for classification from the Gini importance index, which evaluates variables importance by their impact on classification accuracy when their values are reallocated randomly. The random forest method is considered to be superior to most existing classifiers [19,20] and does not require assumptions regarding data distribution.
Although this method does not produce explicit thresholds for variables’ significance, one can still notice the most influencing variables. However, the variables in the model and their distribution are of interest to clinicians. Thus, we then proceeded to evaluate the differences in clearance indices between each pair of subgroups categorized with the same anatomic LLD.
All kinematics variables, for each group, were tested for holding the normality assumption by the Shapiro-Wilk test, and adjusted to the Bonferroni correction for multiple comparisons. Analysis was performed using R software version 3.2.4.
3. Results
Each group was divided according to their anatomic LLD findings: 1. Group A1: 6 participants, Right > Left by 12.66 mm (2.28–23.04); 2. Group A2: 9 participants, Left > Right by 17.4 mm (6.69–28.10); 3. Group B1: 10 participants, Right > Left by 13.2 mm (5.89–20.5) and 4. Group B2: 7 participants, Left > Right by 17.4 mm (3.84–31) (average (95% CI)). The correlation analysis demonstrated that LLD was correlated with 5 kinematic variables in Group A, with only anatomic LLD as clinical findings (Figure 3). No correlation was found between kinematic asymmetry and anatomic LLD in Group B with other clinical abnormalities.
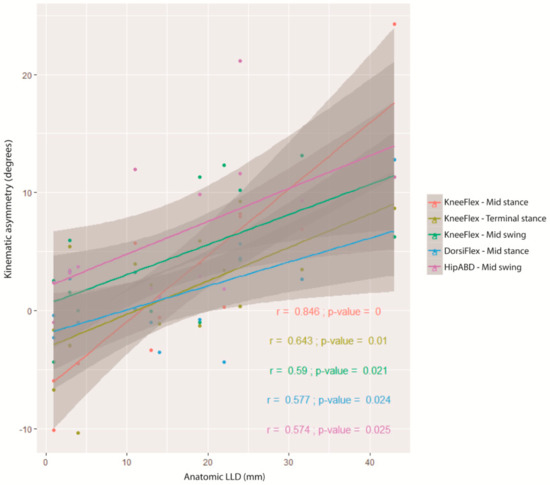
Figure 3.
The correlations between kinematic asymmetry and anatomic LLD (with a 95% confidence interval of the regression line).
Random forest classification accuracy was 80% for Group A versus 64% accuracy for Group B (Table 3), which implies that the kinematic variables used are more adequate predictors for anatomic LLD in group A. Based on the Gini importance index, different kinematic variables were ranked as the 14 most important kinematics variables which influence the classification of participants as to a longer left or right lower limb (Figure 4). In Group A, three participants were erroneously classified. All were diagnosed with idiopathic LLD; 2 with a LLD of 3 mm and 1 with a LLD of 11 mm. In Group B, 6 participants were erroneously classified due to significant clinical abnormalities. Patient 1 with severe right hip joint ROM limitations, patient 3 with severe knee flexion contracture, patient 5 with a paralytic right foot, limited ankle dorsi and plantar flexion ROM, patient 12 with limited dorsi flexion, short hamstrings and weak dorsi flexors, patient 13 with short hamstrings and limited hip ROM and patient 15 with limited hip, knee and ankle ROM with weak plantar flexors.

Table 3.
Classifier performance.
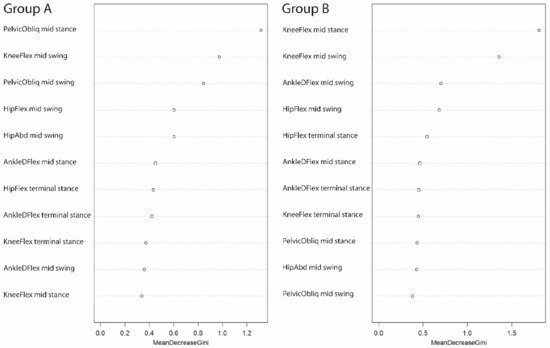
Figure 4.
Utilizing the two group classification random forest models. The variable list extracted by the Gini importance index when classifying individuals exhibiting a longer left or right anatomic lower limb (on the left—group A, on the right—group B). A high value indicates the great importance of a variable for accurate classification.
The clearance index was highest in both groups on the longer limb (when the right lower limb was at swing phase), except for Group A (Left > Right), which was relatively symmetrical (Figure 5). When comparing the clearance indices between the groups according to their anatomic LLD, Group B exhibited a higher clearance index difference between sides as opposed to Group A. A difference in clearance index between sides was found to be higher than FDLL in HDLL and ADLL in both groups.
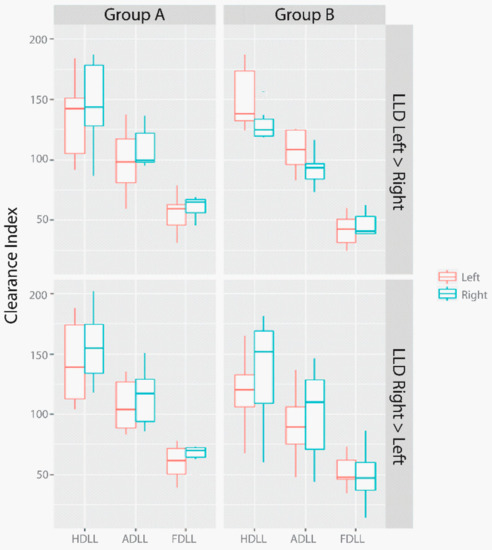
Figure 5.
The differences between maximal DLLs throughout the stance phase and the contralateral minimal DLLs throughout the swing phase in both groups, classified according to anatomic LLD.
4. Discussion
Our study demonstrates that anatomic LLD is correlated with compensatory kinematic asymmetry only when no additional clinical abnormalities are present. The presence of clinical abnormalities, such as joint contractures, muscle-tendon shortening and weak muscle strength will most probably have more of an effect on gait, making the mild anatomic LLD of <2 cm inconsequential. In pathological gait deviations, a functional measurement based on DLL might assist in assessing functional LLD during gait. When examining the relationship between kinematic symmetry for movements known to compensate for LLD and anatomic LLD measured by X-ray, no correlation was found in Group B with pathological gait and clinical abnormalities. However, a high correlation was found in five kinematic parameters in Group A that had only LLD as a clinical finding, consistent with others [1,3,4,8]. This suggests that kinematic asymmetry in pathological gait where clinical abnormalities were present, was not associated with LLD.
Group A exhibited a uniform gait pattern, demonstrating that a higher classification accuracy attained by the random forest method might suggest that LLD was the main factor influencing their gait deviations. An 80% accuracy level obtained by the classifier in Group A is considered high. It is well-known that decision-making in pathological gait is variable [21]. Both groups presented different classification variables for LLD displaying a different kinematic profile, despite a similarity in LLD. In addition, evaluating the 3 cases in group B which were incorrectly classified by the model, revealed that they were relatively “normal” subjects: two with an LLD of 3 mm and one with an LLD of 11 mm, which seems reasonable to be classified incorrectly. However, in group B, the model incorrectly classified 6 subjects, with significant clinical abnormalities leading to difficulty in classifying them according to their gait pattern.
The clearance index, based on the relationship between maximal stance and contralateral minimal swing phase DLL revealed several differences between the groups. A relatively different clearance index between sides was seen in group B, which might be related to their clinical abnormalities since the two groups did not differ in their anatomic LLD. Group A achieved compensatory asymmetry in their gait pattern which equalized their DLL. The asymmetry in their anatomic LLD was associated with their clearance index, except for Group A with longer left lower limb, where a relative symmetry was found despite the anatomic LLD. This might be due to the fact that some subjects with LLD were able to—or chose to—compensate for their LLD and change their DLL, while others are not able to—or do not to—compensate. This might depend on the amount of LLD or factors that we are still not aware of. However, group B exhibited a pathological gait with significant clinical abnormalities affecting their DLL, leading to an asymmetrical clearance index, unrelated to their anatomic leg length. In addition, Group B with longer right lower limb presented higher asymmetry in their HDLL and ADLL, which may imply that this group was severe with significantly more clinical abnormalities that affect gait and lead to asymmetry. FDLL performed differently and presented a relatively symmetrical DLL, which might be due to its dependency on ankle joint movement [11] due to compensation strategies used along with the clinical abnormalities.
The effect of the functional discrepancy, as a result of the clinical abnormalities, considerably affects gait more than LLD, and thus, this should be the basis on which asymmetry is quantified and equalization determined.
Although this research was methodically planned, the authors are aware of its limitations. The polyvalence of the primary diagnosis of the patients demonstrates a potential limitation which may have produced some inconclusive results. Despite the imperfect accuracy of marker placement in the suggested method, this approach offers the best estimate of functional discrepancy and a solid ground for intervention. One can argue that the location of the lift is dependent on the timing of the functional discrepancy; a higher discrepancy in FDLL will necessitate a foot sole lift compensation. However, if the functional discrepancy is HDLL or ADLL, then a heel lift might be suggested. The extent of the correction might be half of the functional discrepancy measured, since compensation is generated by both lower limbs. However, this should be validated in further studies.
5. Conclusions
We question the implication of mid anatomic LLD in patients with pathological gait patterns and clinical abnormalities in order to analyze their gait deviations. The role of mild anatomic LLD in pathological gait when additional clinical abnormalities are present might be limited based on their kinematic profile. Currently, no method has yet attempted to detect and quantify functional LLD. A functional measurement method taking into account the anatomic leg length and kinematic deviations was thus applied, offering a better estimation as to the side and extent of the functional discrepancy. Further studies are recommended to validate this process.
Author Contributions
Methodology, S.K.; Investigation, S.K. and B.D.; Writing—Original Draft Preparation, S.K.; Writing-Review & Editing, S.K.; Supervision, E.C. and D.O.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Walsh, M.; Connolly, P.; Jenkinson, A.; O’Brien, T. Leg length discrepancy—An experimental study of compensatory changes in three dimensions using gait analysis. Gait Posture 2000, 12, 156–161. [Google Scholar] [CrossRef]
- Baylis, W.J.; Rzonca, E.C. Functional and structural limb length discrepancies: Evaluation and treatment. Clin. Podiatr. Med. Surg. 1988, 5, 509–520. [Google Scholar] [PubMed]
- Resende, R.A.; Kirkwood, R.N.; Deluzio, K.J.; Cabral, S.; Fonseca, S.T. Biomechanical strategies implemented to compensate for mild leg length discrepancy during gait. Gait Posture 2016, 46, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Resende, R.A.; Kirkwood, R.N.; Deluzio, K.J.; Morton, A.M.; Fonseca, S.T. Mild leg length discrepancy affects lower limbs, pelvis and trunk biomechanics of individuals with knee osteoarthritis during gait. Clin. Biomech. 2016, 38, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Eek, M.N.; Zugner, R.; Stefansdottir, I.; Tranberg, R. Kinematic gait pattern in children with cerebral palsy and leg length discrepancy: Effects of an extra sole. Gait Posture 2017, 55, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Carmeli, E. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait Posture 2017, 57, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Carmeli, E. The effect of simulated leg length discrepancy on lower limb biomechanics during gait. Gait Posture 2017, 61, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Song, K.M.; Halliday, S.E.; Little, D.G. The effect of limb-length discrepancy on gait. J Bone Jt. Surg. Am. Vol. 1997, 79, 1690–1698. [Google Scholar] [CrossRef]
- Seeley, M.K.; Umberger, B.R.; Clasey, J.L.; Shapiro, R. The relation between mild leg-length inequality and able-bodied gait asymmetry. J. Sports Sci. Med. 2010, 9, 572–579. [Google Scholar] [PubMed]
- Khamis, S.; Carmeli, E. A new concept for measuring leg length discrepancy. J. Orthop. 2017, 14, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Danino, B.; Hayek, S.; Carmeli, E. Measuring clearance mechanics based on dynamic leg length. Meas. Phys. Educ. Exerc. Sci. 2017, 22, 1–9. [Google Scholar] [CrossRef]
- Jamaluddin, S.; Sulaiman, A.R.; Imran, M.K.; Juhara, H.; Ezane, M.A.; Nordin, S. Reliability and accuracy of the tape measurement method with a nearest reading of 5 mm in the assessment of leg length discrepancy. Singap. Med. J. 2011, 52, 681–684. [Google Scholar]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 1990, 8, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.B.; Ounpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Wervey, R.; Schwartz, M. A new device for improving foot marker alignment. In Proceedings of the 8th Annual GCMAS Meeting 2003, Wilmington, DE, USA, 7–10 May 2003. [Google Scholar]
- Segev, E.; Hemo, Y.; Wientroub, S.; Ovadia, D.; Fishkin, M.; Steinberg, D.M.; Hayek, S. Intra- and interobserver reliability analysis of digital radiographic measurements for pediatric orthopedic parameters using a novel pacs integrated computer software program. J. Child. Orthop. 2010, 4, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, U.; Sherman, A. Muscle strength grading. In Statpearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2017. [Google Scholar]
- Bohannon, R.W.; Smith, M.B. Interrater reliability of a modified ashworth scale of muscle spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef] [PubMed]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Wu, B.; Abbott, T.; Fishman, D.; McMurray, W.; Mor, G.; Stone, K.; Ward, D.; Williams, K.; Zhao, H. Comparison of statistical methods for classification of ovarian cancer using mass spectrometry data. Bioinformatics 2003, 19, 1636–1643. [Google Scholar] [CrossRef] [PubMed]
- Skaggs, D.L.; Rethlefsen, S.A.; Kay, R.M.; Dennis, S.W.; Reynolds, R.A.; Tolo, V.T. Variability in gait analysis interpretation. J. Pediatr. Orthop. 2000, 20, 759–764. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).